Abstract
Background
In Saudi Arabia, stay-at-home orders to address the coronavirus disease 2019 (COVID-19) pandemic between March 15 and 23, 2020 and eased on May 28, 2020. We conducted a scoping review to systematically describe physical activity and sedentary behavior in Saudi Arabia associated with the timing of the lockdown.
Methods
We searched six databases on December 13, 2021 for articles published in English or Arabic from 2018 to the search date. Studies must have reported data from Saudi Arabia for any age and measured physical activity or sedentary behavior.
Results
Overall, 286 records were found; after excluding duplicates, 209 records were screened, and 19 studies were included in the review. Overall, 15 studies were cross-sectional, and 4 studies were prospective cohorts. Three studies included children and adolescents (age: 2–18 years), and 16 studies included adults (age: 15–99 years). Data collection periods were < = 5 months, with 17 studies collecting data in 2020 only, one study in 2020–2021, and one study in 2021. The median analytic sample size was 363 (interquartile range 262–640). Three studies of children/adolescents collected behaviors online at one time using parental reporting, with one also allowing self-reporting. All three studies found that physical activity was lower during and/or following the lockdown than before the lockdown. Two studies found screen time, television watching, and playing video games were higher during or following the lockdown than before the lockdown. Sixteen adult studies assessed physical activity, with 15 utilizing self-reporting and one using accelerometry. Physical activity, exercise, walking, and park visits were all lower during or following the lockdown than before the lockdown. Six adult studies assessed sedentary behavior using self-report. Sitting time (4 studies) and screen time (2 studies) were higher during or following the lockdown than before the lockdown.
Conclusions
Among children, adolescents, and adults, studies consistently indicated that in the short-term, physical activity decreased and sedentary behavior increased in conjunction with the movement restrictions. Given the widespread impact of the pandemic on other health behaviors, it would be important to continue tracking behaviors post-lockdown and identify subpopulations that may not have returned to their physical activity and sedentary behavior to pre-pandemic levels to focus on intervention efforts.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-023-15422-3.
Keywords: COVID-19, Physical activity, Middle East region, Saudi Arabia, Sedentary behavior, Surveillance
Background
On March 11, 2020, the World Health Organization declared coronavirus disease 2019 (COVID-19) a pandemic. To tackle viral spread, person-to-person exposure was limited by imposing public movement restrictions. As a result, individuals' physical activity was impacted; there was a drastic change in exercising, walking, and bicycling for transportation and leisure [1]. Sedentary behavior often replaced time spent engaging in physical activity, as the stay-at-home restrictions reduced such opportunities. Even when restrictions were lifted, public facilities (indoor and outdoor) were closed or limited to curtail crowding [2].
The immediate impact of stay-at-home orders on physical activity has been documented through self-reported and device-based metrics. For example, in a convenience sample of 13,503 adults from 14 countries, self-reported moderate-to-vigorous physical activity declined by 41% following pandemic-related restrictions [3]. The decline was greater for work activities than leisure activities, for those with more baseline physical activity compared to those with lesser physical activity, and for younger adults compared to older adults. Other studies using activity trackers indicated immediate declines in step counts (i.e., an indicator of walking levels) attributable to the pandemic in Japan [4], Singapore [5], the United States [6], and worldwide [7–10], although the magnitude of results varied between countries. There is evidence of similar impacts on physical activity among children [1, 11].
The immediate impact of stay-at-home orders has also been documented for sedentary behaviors, characterized as activities while awake with an energy expenditure of 1.5 metabolic equivalents or less while sitting, reclining, or lying [12]. A systematic review found five studies of apparently healthy children and 26 studies of apparently healthy adults, all of which reported increased sedentary behavior primarily due to the pandemic [11]. Another review included 19 studies of children/adolescents and 45 studies of adults and found consistent increases in sedentary behavior during the pandemic period, with larger gains among children compared to adults [13]. The acute global declines in physical activity and increases in sedentary behavior are of concern since engagement in physical activity improves bone health and weight status for children (age 3 to 5 years), improves cognitive function for children/adolescents (age 6 to 13 years), and reduces the risk of mortality, chronic diseases (e.g., certain cancers, cardiovascular disease, obesity), excessive weight gain, fall-related injuries, and dementia for adults [14]. Engagement in sedentary behavior acutely induces vascular dysfunction [15] and, in the long term, increases the risk of mortality, cardiovascular disease, and type 2 diabetes [14, 16].
Physical activity is one of the priority goals of Saudi Arabia’s Vision 2030 given its importance in chronic disease prevention and health benefits [17]. The Saudi Sports for All Federation outlines the vision, framework, goals, and corresponding strategies to help people of all ages become more physically active [18]. The 2021 Household Sports Practice Survey indicated that 48% of the Saudi Arabia population engaged in at least 30 min/week of physical activity, which was higher than the 2019 prevalence of 45% [19]. Two reviews that included studies through early 2018 found that the prevalence of physical inactivity in Saudi Arabia ranged from 55%-96% among children/adolescents, 73%-91% among female adults, and 50%-85% among male adults [20]. A third review included studies published between 2018–2021 that used population-based sampling in the Saudi Arabia population [21]. Among children and adolescents, approximately 80–90% did not attain at least 60 min/day of moderate-to-vigorous physical activity, while for adults approximately 50–95% had a low or insufficient physical activity that did not meet the World Health Organization’s recommendations [22, 23]. In this same review, about 50–80% of children and adolescents engaged in at least two hours/day of screen time or sedentary behavior, while for adults about half had a sitting time of five hours/day or more.
Due to the COVID-19 pandemic, in Saudi Arabia stay-at-home orders were implemented on March 15, 2020, with a suspension of travel for non-essential work, followed by a nationwide curfew from March 23 to April 5, 2020 [24]. The curfews were extended until May 28, 2020, when most regions began easing the curfews. We conducted a scoping review to systematically describe physical activity and sedentary behavior (i.e., physical behaviors) among people of all ages in Saudi Arabia from the pre-COVID-19 pandemic period to the post-movement restriction period. A review focused on Saudi Arabia can bring an understanding of the impact of the pandemic on physical behaviors, identify groups that may not have returned to their pre-pandemic levels, and highlight potential needs for future research and surveillance.
Methods
Search methods
The scoping review protocol was developed in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) statement [25]. Since this review focused on documenting the pandemic-induced change in the prevalence of physical activity and sedentary behavior, and was a scoping rather than a systematic review [26], the protocol was not required to be registered with any platforms. The completed PRISMA-ScR checklist can be found in Supplement 1 [25].
We searched six databases (Cochrane Library, Global Health [EBSCO], PubMed, Scopus, SPORTDiscus [EBSCO], and the World Health Organization Global Index Medicus) on March 3, 2022, with the search strategy detailed in Supplement 2. After manually removing duplicate citations with reference management software, two authors independently screened all titles/abstracts and full-text articles for inclusion using Covidence systematic review software (www.covidence.org; Veritas Health Innovation; Melbourne, Australia), with discrepancies resolved by consensus.
Inclusion and exclusion criteria
Inclusion criteria were studies that either assessed physical activity or sedentary behavior before and during the pandemic, or asked participants to recall how their physical behaviors changed due to the pandemic. We included studies published between March 1, 2020 and March 3, 2022 that reported on physical activity or sedentary behavior in Saudi Arabia. We included observational studies published in either English or Arabic. Both self-reported and device-based measures of physical activity and sedentary behavior were included in the review.
We excluded studies that did not collect data from March 2020 to March 2022 or did not report the impact of the COVID-19 pandemic on physical behaviors. We also excluded studies that did not report data specifically for Saudi Arabia. We excluded studies that did not include a measure of physical activity or sedentary behavior. For example, studies that discussed “intention to exercise” were excluded since that was not a direct measure of physical behaviors, such as in Alshareef et al. [27]. We excluded studies of hospitalized or institutionalized adults. Grey literature, dissertations, commentaries, and conference proceedings were also excluded.
Abstraction and analysis
Once the study inclusion was confirmed, one rater abstracted study details and a second rater checked the abstraction, with discrepancies resolved by consensus. The abstraction tool included the study name, study purpose, data collection period, region, sampling methods, target population, inclusion and exclusion criteria, and sample size. Information abstracted on the sample included age, gender, and nationality. We classified age groups based on the predominant age included in the study: children 1 to 12 years, adolescents 13 to 17 years, and adults 18 years and older [28]. For physical activity and sedentary behavior, we collected results at various time points (e.g., before and during lockdown) and the methods used (e.g., questionnaire and definitions).
The quality of each study was assessed to identify strengths and weaknesses. This was performed by having two reviewers answer ten questions about each study, with disagreements between the raters resolved by consensus. We used the Joanna Briggs Institute Prevalence Critical Appraisal Tool Checklist for Prevalence Studies to assess study quality [29], making modifications and additions to fit the purposes of this review (Supplement 3). In recognition that objective quality assessment tools treat each threat to validity equally, [30] we did not intend to provide a total score for each study. Instead, we used the quality assessment results to focus on the specific threats to validity identified across the included studies.
Results
A total of 286 records were found; after manually removing 77 duplicates across databases, 209 records were screened for inclusion (Fig. 1). In the title and abstract screening stage, 162 records were excluded as irrelevant. After a full-text review of 47 reports, we included 19 studies [24, 31–48], all published in English.
Fig. 1.
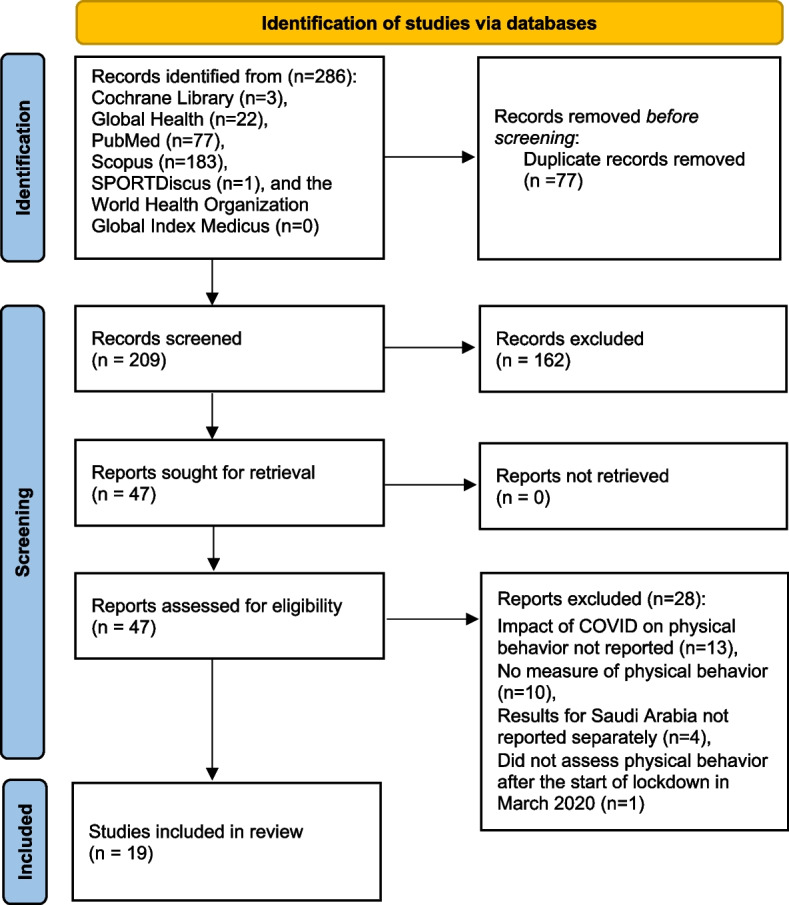
PRISMA flow diagram of the search strategy and results for the scoping review. From: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/
Most studies were cross-sectional in design, except for four studies that collected data at two [35, 36, 45] or seven [43] time points (Table 1). Data collection mainly occurred in 2020, except for the study by Abdulaziz et al.[32] (data collection: September 2020 to February 2021) and Almugti et al. [38] (data collection: July 2021 to August 2021). Most data collection occurred for three months or fewer, except for Abdulaziz et al. [32] that collected data over five months. Analytic sample sizes ranged from 65 [46] to 30,134 [43], with a median of 363 (interquartile range 262 to 640).
Table 1.
Description of each study included in the review (n = 19)
| First Author, Year | Dates of Data Collection | Data Collection Period in Months | Data Collection Time Points | Location in Saudi Arabia | Sampling Procedure | Analytic Sample Size | Age in Years Mean (SD) or Median [IQR] | Age Range in years | Female Percent | Nationality Percent |
|---|---|---|---|---|---|---|---|---|---|---|
| Children/Adolescents | ||||||||||
| Almugti, 2021 [38] | July to August 2021 | 2 | 1 | Jizan 30.0% Riyadh 19.4%, Eastern Province 12.7%, Medina 11.4%, Asir 9.8%, Makkah 8.6%, Bahah 4.1%, Qassim 1.8%, Hail 0.7%, Najran 0.5%, Tabuk 0.5%, Al Jawf 0.3%, Northern Borders 0.2% | Through social media in Saudi Arabia (e.g., Twitter, WhatsApp, and Facebook) | 651 | 9 (4) | 3 to 15 | 41.0% | All parents were Saudi |
| Hanbazaza, 2021 [44] | June 22 to July 22, 2020 | 1 | 1 | All different regions across Saudi Arabia | Conducted using online survey distributed via social media (WhatsApp, Twitter, and Snapchat) in Arabic | 280 | NR | 6 to 15 | 48.9% | NR |
| Al Agha, 2021 [34] | April 2020 to June 2020 | 3 | 1 | Jeddah | Patients with type 1 diabetes were contacted via an online virtual pediatric endocrine outpatient clinic | 150 | 12.5 (4.6) | 2 to 18 | 72.0% | NR |
| Adults | ||||||||||
| Abd El-Fatah, 2021 [31] | October 2020 | 1 | 1 | Makkah region 69.7%, Eastern region 20.4%, Riyadh region 9.9% | Mass email via collaborating authors networks, social media engagement (WhatsApp and Twitter), and snowball sampling | 363 | 36.3 (8.5) | 20 to 59 | 65.6% | NR |
| Abdulaziz, 2021 [32] | September 2020 through February 2021 | 5 | 1 | Qassim province (cities of Buraidah, Unaizah, and AlRass) | Each city selected 10% of the PHCC in each city using simple random sampling (10P HCCs total; 5 from Buraidah, 3 from Unaizah, and 2 from AlRass). An average of 20 attendees were selected daily at each PHCC and interviewed | 299 | 38.6 (13.1) | 18 to missing | 72.6% | NR |
| Abdulsalam, 2021 [33] | NR | NR | 1 | Jeddah | Online questionnaire was distributed using social media (Facebook, Twitter, Instagram, and WhatsApp) and email communication | 472 | NR | 18 to 59 | 68.0% | NR |
| Al Fagih, 2020 [35] | Pre-lockdown (February 2 to March 12, 2020) and lockdown (March 12 to April 19, 2020) | 2 pre and 2 post | 2 | Riyadh | Contacted patients at a cardiac center | 82 | 65 [58 to 72] | NR | 35.4% | NR |
| Alfawaz, 2021 [24] | Two weeks during and after Ramadan (May 11 to June 6, 2020) | 1 | 1 | NR, implies all regions | Online questionnaire was cascaded to different social media outlets throughout Saudi Arabia | 1965 | 35.2 (13.1) | 15 to 75 | 53.0% | 83.1% Saudi, 16.9% non-Saudi |
| Al-Musharaf, 2021 [36] | Pre-lockdown (February to April 2019) and lockdown (April to May 2020) | 3 pre and 2 post | 2 | Riyadh | Randomly selected women aged between 19 and 30 years with no history of medical issues from several colleges | 297 | 20.7 (1.4) | 19 to 30 | 100.0% | All Saudi |
| Alharthi, 2021 [37] | NR | NR | 1 | All regions | NR; enrolled only Saudis between the ages of 18 and 60 | 384 | NR | 18 to 60 | 50.6% | All Saudi |
| Alotaibi, 2021 [39] | March 1 to April 30, 2020 | 2 | 1 | All regions* | Canvassing on social media, local radio stations, and through university mailing lists | 22,053 | NR | 18 to 40 | 44.5% | NR |
| Alqurashi, 2021 [40] | March to May 2020 | 3 | 1 | Region: Eastern 60.1%, Western 23.5%, Central 15.9%, Northern 0.5% | Google forms of the questionnaire were sent to participants to complete via email and social media platforms (Twitter, Telegram, and WhatsApp) | 208 | NR | 18 to 56 | 88.9% | Saudi 99.5%, Non-Saudi 0.5% |
| Bakhsh, 2021 [41] | Two week period between June and early July 2020 | 1 | 1 | Region: Western 70%, Central 16%, Eastern 8%, Southern 5%, Northern 1% | Online questionnaire distributed on various platforms (WhatsApp, Twitter, and email). Questionnaire link was sent to the authors’ relatives, friends, and neighbors to participate in the study and to share the link with their contacts | 2,255 | NR | 18 to missing | 64.0% | Saudi 91%, Non-Saudi 9% |
| Barwais, 2020 [42] | April 9 to April 25, 2020 | 1 | 1 | Region: Makkah 73.4% and Medinah 26.6% | Convenience sample recruited through email invitations and on social media sites (Twitter, Telegram, and WhatsApp groups) | 244 | 33.8 (7.7) | 18 to 50 | 36.9% | NR |
| BinDhim, 2021 [43] | Total of 7 waves of collection in 2020 | grouped into 4 waves of ~ 3 months each | 7 waves; grouped into 4 quarters | All 13 administrative regions | Proportional quota sampling using phone interviews with an age- and gender-stratified random selection of phone numbers from a list generated from the Sharik Association for Health Research (a database of > 80,000 individuals interested in participating in health research, covering all 13 administrative regions) | 30,134 over all waves; Quarter 1 = 7050, Quarter 2 = 11,289, Quarter 3 = 5183, Quarter 4 = 6612 | 36.5 (13.5) | 18 to 99 | 51.2% overall | All Saudi |
| Jalal, 2021 [45] | Before lockdown (March 2020) and during lockdown (June 2020) | 1 pre and 1 post | 2 | Al-Ahsa | Students of undergraduate programs were selected from their registration numbers by using a simple random technique | 628 | 20.5 (1.9) | 18 to 30 | 70.9% | NR |
| Magliah, 2021 [46] | Three days after the lockdown ended in Saudi Arabia (June 21–23, 2020) | 1 | 1 | Jeddah | Web survey (Google Forms) distributed via social media to patients who were actively attending the specialized insulin pump clinic | 65 | 30 (7.9) | 18 to missing | 70.8% | All Saudi |
| Šagát, 2020 [47] | May 10 to May 17, 2020 | 1 | 1 | Riyadh | Simple randomization to select 1000 potential participants on the Riyadh municipality forum groups that were available on social media who were then sent the online questionnaire | 463 | 35.6 (9.8) | 18 to 64 | 44.1% | 71% Saudi citizens and 29% foreigners |
| Sultan, 2021 [48] | August to September 2020 | 2 | 1 | NR, implies all regions | Non-probability convenient sample; online survey distributed using social media | 338 | 40 [IQR not reported] | 30 to 44 | 79.0% | NR |
Abbreviations: IQR Interquartile range, NA Not applicable, NR Not reported, PHCC Primary health care clinics, SD Standard deviation
*obtained directly from authors
Studies were conducted in certain regions of Saudi Arabia such as Al-Ahsa [45], Jeddah [33, 34, 46], Qassim [32], Riyadh [35, 36, 47], or in multiple regions [31, 40–42]. Other studies included participants from the entire country, either stated explicitly [37, 38, 43, 44] or implied [24, 39, 48]. The most common sampling procedure was some combination of convenience sampling through social media platforms, email, radio, or mailing lists [24, 31, 33, 38–42, 44, 46, 48]. Other studies used country-level proportional quota [43] or simple random sampling through health clinics [32, 34, 35], universities [36, 45], or municipal forum groups [47]. The sampling technique was not reported for one study [37].
Three studies included children and adolescents [34, 38, 44], 1 study included participants aged 15 to 75 years (which we assigned to the adult group) [24], and the remaining 15 studies included adults at least 18 years of age [31–33, 35–37, 39–43, 45–48]. All studies enrolled both males and females, except Al-Musharaf et al. [36] who enrolled females only. Some studies enrolled only participants of Saudi nationality [36–38, 43, 46], while others included Saudi and non-Saudi nationalities residing in the country [24, 40, 41, 47]. Ten studies did not report the nationality of participants [31–35, 39, 42, 44, 45, 48].
Impact on physical behaviors of children/adolescents
Three studies recruited children/adolescents through social media platforms [38, 44] or a pediatric endocrine clinic [34]. The age range was wide for all three studies, from a minimum age of 2 [34], 3 [38], or 6 [44] to a maximum age of 15 [38, 44] or 18 years [34]. All relied on parental reports, although one study also allowed self-reporting [34] (Table 2). The questionnaires were administered online and asked about the daily duration of physical activity [34], daily duration of moderate-to-vigorous physical activity [38], or frequency of participation in physical activity [44] before and during the lockdown. All three studies conducted measurements at a single time point.
Table 2.
Physical activity results from the scoping review (n = 19)
| First Author, Year | Physical Activity Assessment Method | Physical Activity Definitions Used | Physical Activity Before Lockdown | Physical Activity During and/or Following Lockdown | Change Reported | Summary |
|---|---|---|---|---|---|---|
| Children/Adolescents | ||||||
| Almugti, 2021 [38] | Parent-reported questionnaire modified by an expert panel | Based on Canadian 24-Hour Movement Guidelines for Children and Youth: At least 1 h/day of MVPA | MVPA < 1 h/day 29%, ≥ 1 h/day 71% | MVPA < 1 h/day 49%, ≥ 1 h/day 51% | P for difference 0.001 | Decreased MVPA |
| Hanbazaza, 2021 [44] | Parent-reported questionnaire | Change in children’s PA (increased, decreased, or remained unchanged); The number of d/wk their children participated in PA before and during lockdown (5 response options ranging from “None at all” to “5–6 times a week”) with PA categorized as ≤ 4 times/week as "not physically active" and ≥ 5 times a week as "physically active" | 19.3% were physically active | 16.1% were physically active | Proportion of physically active decreased 3.2% but was not statistically significant (p = 0.30) | Decreased PA |
| Al Agha, 2021 [34] | Parent- or self-reported questionnaire | Duration of PA | Daily duration of PA before lockdown: < 30 min 40.5%, 30–60 min 28.0%, Not practicing 27.4%, missing 4.1%* | NR | PA during lockdown: Decreased 66.1%, Increased 19.0%, Not affected 14.9% | Decreased PA |
| Adults | ||||||
| Abd El-Fatah, 2021 [31] | IPAQ-SF | Changes in PA reported as no change, positive change, or negative change, see footnote below table for definitions | Median PA 380 min/wk; Low 62.3%, Moderate 37.5%, High 0.3% | Median PA 320 min/wk; Low 63.6%, Moderate 34.2%, High 2.2% | Moderate PA days/wk: No change 54.5%, Positive change (increased PA) 25.1%, Negative change (decreased PA) 20.4%; Moderate PA min/day: No change 48.2%, Positive change 32.2%, Negative change 19.6% | Decreased median PA |
| Abdulaziz, 2021 [32] | Questionnaire | Engagement in any PA, such as walking, going to the gym, and playing sports | NR | 58.9% engaging in PA | Change in exercise: Increased 14.0%, Decreased 30.1%, No change 37.8%; Change in park visits: Increased 4.7%, Decreased 76.7%, No change 18.6% | Decreased exercise; Decreased park visits |
| Abdulsalam, 2021 [33] | Questionnaire translated, tested, and validated by experts at the university | Categorized PA hr/week and PA level per day | Usual daily PA level very low 11.7%, low 17.4%, normal 51.5%, high 17.8%, very high 1.7% | Usual daily PA level very low 22.2%, low 29.0%, normal 34.7%, high 13.1%, very high 0.8% | Usual daily PA level and PA in hr/wk significantly decreased during the COVID-19 period | Decreased usual daily PA level; decreased PA hr/wk |
| Al Fagih, 2020 [35] | Uniaxial accelerometer embedded in patients' cardiac implantable device (Medtronic ICD/CRT) | PA defined in h/day | Median 2.4 h/day PA | Median 1.8 h/day PA | 27.1% decline in PA; change in PA occurred in the first week of March 2020 which coincides with the implementation of social distancing measures | Decreased total PA |
| Alfawaz, 2021 [24] | Questionnaire designed/revised by multidisciplinary experts and piloted | Categorized daily walking, home physical activities, weight lifting, and swimming: never, 1–2, 3–4, or > 4 days | Daily walking never 21.0%, 1–2 d/wk 23.6%, 3–4 d/wk 24.9%, > 4 d/wk 30.5%; Home PA never 42.8%, 1–2 d/wk 19.0%, 3–4 d/wk 18.0%, > 4 d/wk 20.1% | Daily walking never 23.6%, 1–2 d/wk 22.9%, 3–4 d/wk 24.4%, > 4 d/wk 29.1%; Home PA never 44.6%, 1–2 d/wk 18.8%, 3–4 d/wk 17.1%, > 4 d/wk 19.5% | Significant changes in walking, home physical activities with weights, and swimming (p values < 0.001) | Decreased daily walking; Decreased home activities; Increased swimming |
| Al-Musharaf, 2021 [36] | GPAQ Arabic version | Meeting recommendation of ≥ 600 MET-min/week | 47.5% meeting recommendations | 40.7% meeting recommendations | Test for difference in meeting PA recommendations p = 0.08 | Decreased meeting PA recommendations |
| Alharthi, 2021 [37] | Modified IPAQ (New Zealand PAQ) | Reported did or did not do exercise | Did exercise 64.2% | Did exercise 48.9% | Increased exercise 48.9% (p = 0.01) | Decreased "did exercise" |
| Alotaibi, 2021 [39] | Questionnaire | Active or inactive based on the WHO guidelines (150–300 min/week of moderate or 75–150 min/week of vigorous intensity PA, or some equivalent combination). MVPA further divided into < 3 d/wk or ≥ 3 d/wk | Inactive 77.1%, Active 22.9%; MVPA > 3 times/wk 13.0%, < 3 times/wk 9.9% | Inactive 80.0%, Active 20.0%; MVPA > 3 times/wk 10.2%, < 3 times/wk 9.8% | Inactive + 2.9%, Active -2.9%; > 3 times/wk -2.9%, < 3 times/wk -0.09% | Decreased active group; increased inactive group |
| Alqurashi, 2021 [40] | Questionnaire developed and piloted | PA before and during lockdown, asking about: 1) engagement in PA or sports before the pandemic, 2) their gym attendance, 3) whether they exercised at home during the lockdown, 4) whether their time spent exercising increased during the quarantine | Engaged in PA before pandemic 59.1%; exercised at a gym before pandemic 28.8% | Practice exercise at home during lockdown: never 36.5%, 1–3 times/wk 39%, 4–6 times/wk 10.1%, every day 14.4% | During the quarantine period, increased exercise time at home: strongly agree 27.5%, agree 25.5%, neutral 29.8%, disagree 12.5% | Increased time in exercise at home |
| Bakhsh, 2021 [41] | Questionnaire | Asked participants about changes in their level of PA, weekly frequency of PA, duration of PA per day, and types of PA performed during quarantine | NR | Frequency of PA: none 40%, 1–2 d/wk 22%, 3 d/wk 11%, 4–6 d/wk 14%, daily 13%; Duration of PA: none 40%, < 30 min/d 13%, 30 min/d 15%, 1 h/d 24%, > 1 h/d 8%; Type of PA: walking 65% (most common), cardiorespiratory exercise 11%, and resistance training 7% | Change in PA level: increased 27%, decreased 52%, no change 21% | Decreased PA |
| Barwais, 2020 [42] | IPAQ-SF | Total MET-min/wk | Mean 903 (SD 755.6) MET-min/wk | Mean 387 (SD 397.8) MET-min/wk | p for paired difference 0.001 with a large effect size (d = 0.89); Social contexts: significant decreases in PA performed alone (p < 0.001), with family (p < 0.05), with friends (p < 0.05), and with groups (p < 0.001) | Decreased PA overall and for men and women |
| BinDhim, 2021 [43] | Questionnaire refined through linguistic validation, reliability testing, and focus group evaluation | WHO/US PA Guidelines: low level of PA or acceptable PA level (≥ 150 min/wk of MPA and/or ≥ 75 min/wk VPA) | Acceptable PA level Q1 (January to mid-March) 41.0% | Acceptable PA level Q2 (mid-March to June) 26.5%, Q3 (July to September) 24.6%, Q4 (October to December) 24.6% | Significant decline in prevalence odds of having an acceptable PA level between Q1 and each of Q2-4 (all p < 0.001) for both unadjusted and adjusted (age, gender, and region) analysis | Decreased PA |
| Jalal, 2021 [45] | GPAQ | Meeting recommendation of > = 600 total MET-min/wk | Total PA mean 1149.2 (SD 120.08) MET-min/week; Attaining ≥ 600 MET-min/wk 52.1% | Total PA mean 1116.5 (SD 125.3) MET-min/week; Attaining ≥ 600 MET-min/wk 47.9% | differences: MET-min/week p = 0.0001, attaining ≥ 600 MET-min/wk p = 0.03 | Decreased total PA; Decreased meet PA recommendations |
| Magliah, 2021 [46] | Web survey (Google Forms) with a section asking about the impact of lockdown on different self-management behaviors, which included rating their ability to maintain PA in comparison with the pre-lockdown period | Report change in PA during vs before lockdown in five categories (Greatly decreased to greatly increased) | NR | NR | Greatly decreased 41.5%, somewhat decreased 26.2%, no change 9.2%, somewhat increased 15.4%, greatly increased 7.7% | Decreased PA |
| Šagát, 2020 [47] | Questionnaire | Categorize their weekly frequency of PA before and after the pandemic: none, once, 2–3 times, 4–5 times, or 6–7 times per week | Did not practice PA 7.3%, PA 1 time/wk 10.3%, PA 2–3 times/wk 35.6%, PA 4–5 times/wk 24.1%, PA 6–7 times/wk 22.7% | Did not practice PA 20.0%, PA 1 time/wk 15.2%, PA 2–3 times/wk 25.1%, PA 4–5 times/wk 25.8%, PA 6–7 times/wk 13.9% | Significant differences in proportions who "did not practice PA" (p = 0.001; increase), "practiced PA once a wk" (p = 0.02; increase), "practiced PA 2–3 times a wk" (p = 0.001; decrease), and "practiced PA 6–7 time a wk" (p < 0.001; decrease) | Decreased PA |
| Sultan, 2021 [48] | Questionnaire developed after a literature review; tested reliability | Categorized participants as not active, light activity, active, or very active (categories not further defined) | Not active 5.3%, light activity 31.2%, active 54.9%, very active 6.8% | Not active 19.0%, light activity 36.2%, active 37.4%, very active 7.4% | "Not active" category increased significantly p < 0.001 | Increased "not active" category |
Abbreviations: d days, ICD/CRT Implantable cardioverter-defibrillator / cardiac resynchronization therapy, IPAQ International PA Questionnaire, GPAQ Global PA Questionnaire, MET Metabolic equivalent of task, min minutes, MPA Moderate PA, MVPA Moderate to vigorous PA, NA Not applicable, NR Not reported, PA Physical activity, wk week, VPA Vigorous physical activity, WHO World Health Organization
IPAQ-SF November 2005 scoring protocol: Low [not moderate or high]; Moderate [either A) ≥ 3 days of vigorous activity of ≥ 20 min/day, B) ≥ 5 days of moderate-intensity activity or walking of ≥ 30 min/day, or C) ≥ 5 days of any combination of walking, moderate-intensity or vigorous intensity activities achieving ≥ 600 MET-min/week]; High [either A) vigorous-intensity activity on ≥ 3 days achieving ≥ 1500 MET-min/week or B) ≥ 7 days of any combination of walking, moderate-intensity or vigorous intensity activities achieving ≥ 3000 MET-min/week]
*obtained directly from authors
The lockdown was associated with a 20-percentage point decrease in moderate-to-vigorous physical activity of at least one hour/day [38] and a three-percentage point decrease in the percent classified as physically active [44]. The third study among participants aged 2 to 18 years with diabetes reported that the lockdown was associated with decreased physical activity for 66.1% of the sample, increased physical activity for 19.0%, and no change for 14.9% [34].
Two studies assessed sedentary behavior by asking parents to report time on digital screens [38] or time spent playing video games and watching television [44] (Table 3). Compared to the pre-lockdown period, the lockdown period was associated with 24.0, 35.0, and 22.5 percentage point increases in the proportion of children/adolescents on screens for > 2 h/day [38], video games for > = 3 h/day [44], and watching television for > = 4 h/day [44], respectively.
Table 3.
Sedentary behavior results from the scoping review (n = 8)
| First Author, Year | Sedentary Behavior Assessment Method | Sedentary Behavior Definitions Used | Sedentary Behavior Before Lockdown | Sedentary Behavior During and or Following Lockdown | Change Reported | Summary |
|---|---|---|---|---|---|---|
| Children/Adolescents | ||||||
| Almugti, 2021 [38] | Parent-reported questionnaire modified by expert panel | How much time their child spent viewing digital screens, including TV, tablets, and phones; categories based on Canadian 24-Hour Movement Guidelines for Children and Youth: < = 2 h/day of screen time | Use of screens ≤ 2 h/day 37%, > 2 h/day 63% | Use of screens ≤ 2 h/day 13%, > 2 h/day 87% | difference p = 0.001 | Increased screen time |
| Hanbazaza, 2021 [44] | Parent-reported questionnaire | How long child played video games and watched TV per day; categorized as > = 3 h/day playing video games (considered high) and > = 4 h/day watching TV (considered high) | Playing video games > = 3 h/day 40.4%; watching TV > = 4 h/day 21.1% | Playing video games > = 3 h/day 75.4%; watching TV > = 4 h/day 43.6% | Significant increases (p-values < 0.001) in proportions that were playing video games > = 3 h/day and were watching TV > = 4 h/day | Increased video game time, Increased TV time |
| Adults | ||||||
| Abd El-Fatah, 2021 [31] | IPAQ-SF | Routine sitting in the day as no change, positive change, or negative change | Daily sitting: 1–2 h/day 20.4%, 3–4 h/day 27%, 5–6 h/day 21.5%, More than 6 h/day 31.1%, | Daily sitting: 1–2 h/day 12.9%, 3–4 h/day 13.8%, 5–6 h/day 18.2%, More than 6 h/day 55.1%, | Daily sitting in h/day: No change 45.5%, Decrease 8.3%, Increase 46.2% | Increased sitting time |
| Abdulsalam, 2021 [33] | Questionnaire translated, tested, and validated by experts at the university | Time spent in front of the computer, mobile devices, television, etc | < 1 h/day 9.1%, 1–2 h/day 24.2%, 3–4 h/day 33.1%, 5–6 h/day 21.2%, > 6 h/day 12.5% | < 1 h/day 4.7%, 1–2 h/day 7.6%, 3–4 h/day 20.3%, 5–6 h/day 31.1%, > 6 h/day 36.2% | Significant increase (e.g., before 12.5% spent > 6 h/day, but during the pandemic it became the most prevalent category (36.2%) | Increased screen time |
| Al-Musharaf, 2021 [36] | GPAQ Arabic version | Continuous min/day sitting or reclining | Mean 451.4 (SD 242.1) min/day | Mean 484.9 (SD 257.2) min/day | Test for difference p = 0.07 | Increase sitting time |
| Jalal, 2021 [45] | GPAQ | Continuous min/day sitting or reclining | Mean 448.7 (SD 73.6) min/day | Mean 517.8 (SD 83.0) min/day | Differences in min/day p = 0.0001 | Increased sitting time |
| Šagát, 2020 [47] | Questionnaire | Asked to categorize their physical behavior at their job/occupation | Occupation: sitting always or most of the time 30.5%, sitting and moving equally 27.9%, moving always or most of the time 42.4% | Occupation: sitting always or most of the time 50.9%, sitting and moving equally 24.2%, moving always or most of the time 24.9% | Significant differences in proportions "sitting always or most of the time" (p < 0.001; increase) and "moving always or most of the time" (p < 0.001; decrease) during their job/occupation | Increased sitting time at work |
| Sultan, 2021 [48] | Questionnaire tested for reliability | Daily screen time categorized as < 1 h/day, 1–3 h/day, 4–5 h/day, or ≥ 6 h/day | < 1 h/day 13.4%, 1–3 h/day 48.7%, 4–5 h/day 23.1%, ≥ 6 h/day 14.8% | < 1 h/day 7.1%, 1–3 h/day 29.4%, 4–5 h/day 28.2%, ≥ 6 h/day 35.3% | Increases in proportions with ≥ 6 h/day of screen time and of social media time (p ≤ 0.001 for both) | Increased screen time |
Abbreviations: GPAQ Global Physical Activity Questionnaire, IPAQ -SF International Physical Activity Questionnaire short form, h hours, min minutes, SD Standard deviation, TV Television
*obtained directly from authors
Impact on physical behaviors of adults
Three studies recruited adults through health clinics [32, 35], and the remaining studies recruited through social media platforms [24, 31, 33, 39–42, 46, 48], universities [36, 45], municipal forum groups [47], proportional quota sampling from throughout the country [43], or was not reported [37]. All but one study relied on self-reported physical activity assessed using questionnaires (Table 2). These included the International Physical Activity Questionnaire [31, 37], the Global Physical Activity Questionnaire [36, 45], or some other questionnaires that experts designed and pilot tested [24, 33, 40, 43], assessed for reliability [48], or not pilot tested (or unreported as such) [32, 39, 41, 46, 47]. The exception was Al Fagih et al. study [35] that enrolled patients with cardiac implantable devices and relied on the accelerometer embedded in those devices for assessing the duration of physical activity for just over a month immediately before and after lockdown. Among 82 patients, median total physical activity declined from pre-lockdown (2.4 h/day) to lockdown (1.8 h/day). The other clinic-oriented study found that 30.1% and 76.7% reported decreases in exercise and park visits, respectively, during the lockdown than before the lockdown [32].
Studies found that fewer adults met recommendations for physical activity [36, 39, 45] or fewer classified themselves as “active or very active” compared to before the lockdown [48]. Studies also found that the lockdown was associated with lower daily or weekly physical activity levels [31, 33, 41–43, 45–47], lower exercise [37], and less daily walking and participation in household activities [24]. Other studies found an increase in swimming [24] and an increase in time spent exercising at home [40] associated with the lockdown. One study explored the results by gender and found that lower physical activity during the lockdown compared to the pre-lockdown period was similar for both women (n = 90) and men (n = 154) [42].
Six studies assessed sedentary behavior using a questionnaire (Table 3). They found that sitting time increased, both overall [31, 33, 36, 45] and while at work [47], and daily screen time increased, all attributable to the lockdown [48]. Specifically, two studies using continuous measures reported an increase in sitting time of 33.5 min/day [36] or 69.1 min/day [45]. Three studies using a categorical measure reported that the proportion of adults with > 6 or ≥ 6 h/day of sitting time [31] or screen time [33, 48] increased by 20.5 to 24.0 percentage points.
Quality assessment
The quality assessment tool, comprising ten questions and applied to the 19 studies, is provided in Table 4, with the corresponding questions itemized in Supplement 3. All studies had data analysis with sufficient coverage (n = 19, question 5), and most measured physical behaviors in a standard way for all participants (n = 17, question 8). Most studies described study subjects and the setting in adequate detail (n = 14, question 6) and used a valid method to assess the volume of physical behaviors (n = 13, question 7). Twelve studies summarized physical behaviors using appropriate analytic methods (question 10), and about half of the studies provided sample size justification (n = 10, question 3). However, few studies sampled participants appropriately (n = 4, question 2) or provided an appropriate sampling frame to address the target population (n = 1, question 1), with most studies recruiting participants through social media platforms, professional networks, health clinics, or universities. Few studies also assessed physical behaviors at least once before and once after lockdown (n = 4, question 9) or reported an adequate response rate or appropriately managed non-response (n = 3, question 4; 15 did not report on response rate).
Table 4.
Quality assessment results with studies listed in alphabetical order by the first author's last name (n = 19)
| First Author, Year | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Children/Adolescents | ||||||||||
| Almugti, 2021 [38] | N | N | N | U | Y | Y | Y | Y | N | Y |
| Hanbazaza, 2021 [44] | N | N | Y | U | Y | Y | N | Y | N | Y |
| Al Agha, 2021 [34] | N | U | N | U | Y | N | N | N | N | Y |
| Adults | ||||||||||
| Abd El-Fatah, 2021 [31] | N | N | Y | U | Y | Y | Y | Y | N | N |
| Abdulaziz, 2021 [32] | N | Y | Y | Y | Y | Y | U | U | N | U |
| Abdulsalam, 2021 [33] | N | N | N | U | Y | Y | Y | Y | N | Y |
| Al Fagih, 2020 [35] | N | Y | N | U | Y | N | Y | Y | Y | Y |
| Alfawaz, 2021 [24] | N | N | Y | U | Y | Y | Y | Y | N | Y |
| Al-Musharaf, 2021 [36] | N | Y | N | U | Y | Y | Y | Y | Y | N |
| Alharthi, 2021 [37] | U | U | Y | U | Y | Y | Y | Y | N | N |
| Alotaibi, 2021 [39] | N | N | N | U | Y | Y | N | Y | N | Y |
| Alqurashi, 2021 [40] | N | N | N | U | Y | Y | Y | Y | N | Y |
| Bakhsh, 2021 [41] | N | N | Y | U | Y | Y | Y | Y | N | Y |
| Barwais, 2020 [42] | N | N | N | U | Y | Y | Y | Y | N | N |
| BinDhim, 2021 [43] | Y | Y | Y | N | Y | N | Y | Y | Y | Y |
| Jalal, 2021 [45] | N | U | Y | U | Y | N | Y | Y | Y | N |
| Magliah, 2021 [46] | N | N | N | Y | Y | Y | N | Y | N | Y |
| Šagát, 2020 [47] | N | N | Y | Y | Y | N | N | Y | N | Y |
| Sultan, 2021 [48] | N | N | Y | U | Y | Y | Y | Y | N | U |
| Total Yes | 1 | 4 | 10 | 3 | 19 | 14 | 13 | 17 | 4 | 12 |
| Total Unclear | 1 | 3 | 0 | 15 | 0 | 0 | 1 | 1 | 0 | 2 |
| Total No | 17 | 12 | 9 | 1 | 0 | 5 | 5 | 1 | 15 | 5 |
The quality assessment is available in Supplement 3 of this paper
Abbreviations: N No, U Unclear, Y Yes
Discussion
This scoping review, based on 19 studies from Saudi Arabia, found consistent evidence across the available literature indicating that physical activity declined and sedentary behavior increased during the COVID-19 lockdown period compared with before. This was most consistent for children, adolescents, and adults across all studies, and was similar for men and women, as reported in one study [42]. For adults, physical activity was lower with the lockdown by approximately 5 to 15 percentage points when considering the studies that classified the proportion as either “active” or “meeting physical activity guidelines” and sedentary behavior was higher by approximately 20 to 25 percentage points for studies that classified the proportion with ~ 6 h/day or more of sitting or screen time.
For children/adolescents, all three studies indicated lower physical activity or moderate-to-vigorous physical activity with the lockdown [34, 38, 44], while two studies indicated a higher proportion of children/adolescents spent time on digital screens [38], playing video games [44], and watching television during the lockdown [44].
There were a couple of notable exceptions among adults, wherein the lockdown was associated with a self-reported increase in swimming [24] and an increase in time spent exercising at home [40]. The higher time spent exercising at home was expected, since time for exercising elsewhere may have been spent at home. Another study reported home exercise among adults but found fewer home activities with the lockdown [24].
We identified four reviews of the global impact of COVID-19 on physical behaviors to compare our results. These reviews found that studies consistently reported lower self-report or device-measured physical activity [1, 11, 49] and higher sedentary behavior [1, 11, 13] associated with lockdown policies. People who were more active prior to the pandemic had larger declines in physical activity [11]. As noted by Stockwell et al.[11], these findings are despite health practitioners and various government organizations guiding how to stay active in self-quarantine and during a lockdown.
The detrimental impact of the lockdown on physical activity was also documented among children/adolescent patients with diabetes [34] and adult patients with heart failure [35] in Saudi Arabia. Other reviews identified studies from different countries that indicated similar declines in physical activity as a result of the lockdown among patients with diabetes, heart failure, congenital heart disease, obesity, and neuromuscular disease [1, 11, 49].
Our review findings are also consistent with an online cross-sectional survey of 2970 adults conducted in April 2020 from the Middle East and North Africa (MENA) region, wherein no physical activity engagement increased from before the pandemic (34.9%) to during the pandemic (39.1%) [50]. Additionally, they found other adverse health impacts over the short term, including weight gain, longer sleep time, and higher reporting of irritability, physical and emotional exhaustion, and tension. Other studies in Saudi Arabia or the MENA region found detrimental impacts of the pandemic on physical health, including changes in eating habits [51], weight gain [51, 52], diabetes [27, 34, 53], and mental health [54–56]. Awareness of increasing physical activity is needed for children, adolescents, and adults in Saudi Arabia [21] since there has been a recent upward trend in obesity and diabetes [57–59]. Taken together with the findings from this review, there is concern over the long-term impact of these observations on physical behaviors. Increasing physical activity and decreasing sedentary behavior is a worthwhile endeavor, given its potential benefit in reducing hospitalizations, admission to an intensive care unit, and death among those with COVID-19 [60, 61].
Physical activity is impacted by the physical environment, including built and natural surroundings [62]. For example, parks provide a crucial place for physical activity and general recreation, particularly in more temperate areas of Saudi Arabia and seasonably cooler times of the year. In our review, one study in the Qassim region found that adults self-reported fewer park visits during the lockdown than before the lockdown [32]. A prospective study in the United States found an increase in park visits at the start of the pandemic, followed by a marked decline in lockdown near closed parks but not near open parks [63]. Once closed parks opened again, their usage increased to levels found at the start of the pandemic. From a worldwide perspective, park visits increased with the start of the pandemic and were lower when the government levied stay-at-home restrictions [2]. If park observation or usage data exist in Saudi Arabia, it would be valuable to investigate whether the patterns followed global trends. Furthermore, an investigation into the impact of the built environment on changing physical behaviors during the pandemic would be worthwhile [64].
Limitations of the studies included
We found several notable limitations in the current literature that were reviewed, both from the quality assessment (Table 4) and from our observations. First, most studies were cross-sectional, relying on participants to self-report activities before and during the lockdown. Recency bias is a threat to these studies, whereby activities occurring more recently might be easier to report than those occurring more distant in time. Prospective measurement, accomplished in four studies, reduces the risk of bias [35, 36, 43, 45]. This limitation is especially pertinent for two studies that collected data in 2021 [32, 38]. Second, many studies used convenience and nonrepresentative samples, particularly relying on social media platforms for recruitment. While these studies offer the advantage of lower costs and quick access to participants, they also limit participation to those without access to social media platforms and those unwilling to participate using those recruitment channels. This further limits the generalizability of the results.
Third, assessments were mostly based on self-reporting or parental-reporting using a wide variety of questionnaires, precluding our ability to summarize findings with meta-analytic techniques accurately. In fact, many questionnaires appeared non-standardized and did not provide information about the total volume of physical activity. Using valid and reliable metrics for this population would be preferred. Fourth, many studies lacked information on the nationality of their sample, and most studies did not report findings by potential modifiers, such as gender, age, socioeconomic status, region of the country, nationality, or health-associated metrics, possibly due to sample sizes. Fifth, since the period before the COVID-19 pandemic and during the lockdown were not the same seasons of the year, seasonality could confound the relationships observed. Finally, although we included three studies on children and adolescents, the age range was wide and primarily based on parental reporting, which is limited [65]. It would be helpful to document the impacts by narrower age groups to discern any differences that might have a lasting effect on physical behaviors in the future. However, despite these limitations, the findings of the lockdown’s impact on physical behaviors were largely consistent. Future studies are needed to prospectively document physical activity and sedentary behavior changes from pre-pandemic to post-lockdown.
Strengths and limitations of this review
This scoping review was comprehensive, with searches conducted in six databases, which included Arabic studies, although there were none. To our knowledge, this is the first review to describe the impacts of the COVID-19 pandemic on physical activity and sedentary behavior in Saudi Arabia among children, adolescents, and adults [66]. Based on our inclusion criteria, we accepted all papers regardless of study quality but quantified study quality using a previously developed tool. Despite the strengths of this review, several limitations also exist. The questionnaires used across studies were heterogeneous, as was how they were analyzed, limiting our ability to meta-analyze findings to summarize results. The lack of reporting of findings by sociodemographic and health-related metrics also precluded our ability to summarize across subpopulations.
Conclusions
In 2021, the Saudi Sports for All Federation set a target to decrease the prevalence of physical inactivity by 30% in adults by 2030 [18]. The findings from this scoping review stress the need to improve physical activity and curtail sedentary behavior in Saudi Arabia, particularly in light of the apparent decline in physical activity and increase in sedentary behavior during and following the COVID-19 lockdown period. This is in agreement with recent worldwide reports on physical activity among children, adolescents, and adults [67–69]. Colleagues have identified the global pattern of unhealthy lifestyle behaviors (including physical behaviors) and the COVID-19 pandemic as a “syndemic”, wherein two or more health conditions or diseases negatively interact [70].
Major areas of focus to support physical activity were designated by the World Health Organization [71] and the International Society for Physical Activity and Health [72]. Some of the Gulf Cooperation Council countries have national policies and strategies to promote physical activity, but implementation is generally low [73]. Others have called for a coordinated regional effort to promote physical activity and reduce sedentary behavior [73]. Consideration should also be given to the specific barriers and facilitators of physical activity and sedentary behavior in Saudi Arabia [74, 75] and the socio-ecologic correlates relevant to this unique time period [76]. Given the widespread impact of the COVID-19 pandemic on other health behaviors, it would be important to continue tracking behaviors and identify subpopulations that may not have returned their physical activity and sedentary behavior to pre-pandemic levels to focus on intervention efforts.
Supplementary Information
Additional file 1: Table S1. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist. Table S2. Databases searched, search structure, and search terms. Table S3. Quality assessment tool applied to each included study.
Acknowledgements
The authors thank Rekha Menon (World Bank) and Issam Abousleiman (World Bank) for their input and support on the manuscript.
Role of the funding/sponsor
The funders of this study had no role in this scoping review.
Abbreviations
- COVID-19
Coronavirus disease 2019
- MENA
Middle East and North Africa
- PRISMA-ScR
Preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews
Authors’ contributions
KRE conceptualized and drafted the paper. CCM led the systematic search for papers and organized the Covidence and Endnote databases. KRE, CCM, and MH participated in study selection. CCM and MH abstracted the studies, while KRE provided input. All authors reviewed and approved the final manuscript.
Funding
This work was supported by King Faisal Specialist Hospital and Research Center and the Health, Nutrition and Population Reimbursable Advisory Services Program between the World Bank and the Ministry of Finance in Saudi Arabia (#P172148 and #P179873). The content is solely the responsibility of the authors and does not necessarily represent the official views of the King Faisal Specialist Hospital and Research Center and World Bank.
Availability of data and materials
All data generated or analyzed during this study are referenced in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Park AH, Zhong S, Yang H, Jeong J, Lee C. Impact of COVID-19 on physical activity: A rapid review. J Glob Health. 2022;12:05003. doi: 10.7189/jogh.12.05003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geng DC, Innes J, Wu W, Wang G. Impacts of COVID-19 pandemic on urban park visitation: a global analysis. J For Res (Harbin) 2022;32(2):553–67. doi: 10.1007/s11676-020-01249-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilke J, Mohr L, Tenforde AS, Edouard P, Fossati C, Gonzalez-Gross M, Sanchez Ramirez C, Laino F, Tan B, Pillay JD, et al. A Pandemic within the Pandemic? Physical Activity Levels Substantially Decreased in Countries Affected by COVID-19. Int J Environ Res Public Health. 2021;18(5):2235. doi: 10.3390/ijerph18052235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Obuchi SP, Kawai H, Ejiri M, Ito K, Murakawa K. Change in outdoor walking behavior during the coronavirus disease pandemic in Japan: A longitudinal study. Gait Posture. 2021;88:42–46. doi: 10.1016/j.gaitpost.2021.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ong JL, Lau T, Massar SAA, Chong ZT, Ng BKL, Koek D, Zhao W, Yeo BTT, Cheong K, Chee MWL. COVID-19-related mobility reduction: heterogenous effects on sleep and physical activity rhythms. Sleep. 2021;44(2):zsaa179. doi: 10.1093/sleep/zsaa179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hunter RF, Garcia L, de Sa TH, Zapata-Diomedi B, Millett C, Woodcock J, Pentland A, Moro E. Effect of COVID-19 response policies on walking behavior in US cities. Nat Commun. 2021;12(1):3652. doi: 10.1038/s41467-021-23937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tison GH, Avram R, Kuhar P, Abreau S, Marcus GM, Pletcher MJ, Olgin JE. Worldwide Effect of COVID-19 on Physical Activity: A Descriptive Study. Ann Intern Med. 2020;173(9):767–770. doi: 10.7326/M20-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.FItbit News. The impact of Coronavirus on Global Activity. Published March 23, 2020. Accessed at https://blog.fitbit.com/covid-19-global-activity/.
- 9.The Effect of the Global Pandemic on Active Lifestyles. Written April 9, 2020. Accessed at https://www.garmin.com/en-US/blog/general/the-effect-of-the-global-pandemic-on-active-lifestyles/
- 10.2020: How Garmin Users Prioritized Movement in a Global Pandemic. Published February 1, 2021. Accessed at https://www.garmin.com/en-GB/blog/2020-how-garmin-users-prioritized-movement-in-a-global-pandemic/
- 11.Stockwell S, Trott M, Tully M, Shin J, Barnett Y, Butler L, McDermott D, Schuch F, Smith L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open Sport Exerc Med. 2021;7(1):e000960. doi: 10.1136/bmjsem-2020-000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sedentary Behaviour Research Network Standardized use of the terms "sedentary" and "sedentary behaviours". Appl Physiol Nutr Metab. 2012;37:540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 13.Runacres A, Mackintosh KA, Knight RL, Sheeran L, Thatcher R, Shelley J, McNarry MA. Impact of the COVID-19 pandemic on sedentary time and behaviour in children and adults: a systematic review and meta-analysis. Public Health. 2021;18(21):11286. doi: 10.3390/ijerph182111286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.US Department of Health and Human Services: Physical Activity Guidelines for Americans. 2nd edition. Washington, DC: US Department of Health and Human Services. 2018. Accessed at https://health.gov/paguidelines/second-edition/.
- 15.Carter S, Hartman Y, Holder S, Thijssen DH, Hopkins ND. Sedentary behavior and cardiovascular disease risk: mediating mechanisms. Exerc Sport Sci Rev. 2017;45(2):80–86. doi: 10.1249/JES.0000000000000106. [DOI] [PubMed] [Google Scholar]
- 16.Katzmarzyk PT, Powell KE, Jakicic JM, Troiano RP, Piercy K, Tennant B. Physical activity guidelines advisory c: sedentary behavior and health: update from the 2018 physical activity guidelines advisory committee. Med Sci Sports Exerc. 2019;51(6):1227–1241. doi: 10.1249/MSS.0000000000001935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vision 2030. Accessed May 12, 2022 at https://www.vision2030.gov.sa/
- 18.Saudi Sports for All Federation: Sports for All: Overall Strategy. Accessed at www.sportsforall.com.sa. 2021: 1–29.
- 19.Kingdom of Saudi Arabia, General Authority for Statistics: According to Households Sport Practice Survey in Saudi Arabia. Accessed June 27, 2022 at https://www.stats.gov.sa/en/news/315. 2022.
- 20.Alasqah I, Mahmud I, East L, Usher K. Patterns of physical activity and dietary habits among adolescents in Saudi Arabia: A systematic review. Int J Health Sci (Qassim) 2021;15(2):39–48. [PMC free article] [PubMed] [Google Scholar]
- 21.Evenson KR, Alhusseini N, Moore CC, Hamza MM, Al-Qunaibet A, Rakic S, Alsukait RF, Herbst CH, AlAhmed R, Al-Hazzaa HM, Alqahtani SA: Scoping review of population-based studies of physical activity and sedentary behavior in Saudi Arabia. J Phys Act Health 2023:in press. [DOI] [PubMed]
- 22.Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, Carty C, Chaput JP, Chastin S, Chou R, et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization: WHO Guidelines on Physical Activity and Sedentary Behavior. Accessed at https://apps.who.int/iris/bitstream/handle/10665/336656/9789240015128-eng.pdf. In. Geneva, Switzerland: World Health Organization; 2020: 1–531.
- 24.Alfawaz H, Amer OE, Aljumah AA, Aldisi DA, Enani MA, Aljohani NJ, Alotaibi NH, Alshingetti N, Alomar SY, Khattak MNK, et al. Effects of home quarantine during COVID-19 lockdown on physical activity and dietary habits of adults in Saudi Arabia. Sci Rep. 2021;11(1):5904. doi: 10.1038/s41598-021-85330-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 26.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alshareef R, Al Zahrani A, Alzahrani A, Ghandoura L. Impact of the COVID-19 lockdown on diabetes patients in Jeddah. Saudi Arabia Diabetes Metab Syndr. 2020;14(5):1583–1587. doi: 10.1016/j.dsx.2020.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Christiansen S, Iverson C, Flanagin A, al. e: AMA Manual of Style: A Guide for Authors and Editors. Accessed August 31, 2022 at https://www.amamanualofstyle.com/, 11th edn: Oxford University Press; 2020.
- 29.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13:147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 30.Savitz DA, Wellenius GA, Trikalinos TA. The Problem with mechanistic risk of bias assessments in evidence synthesis of observational studies and a practical alternative: assessing the impact of specific sources of potential bias. Am J Epidemiol. 2019;188(9):1581–1585. doi: 10.1093/aje/kwz131. [DOI] [PubMed] [Google Scholar]
- 31.Abd El-Fatah NK, Alshehri AA, Alsulami FH, Alasmari N, Osman NA. Association between mental health outcomes and changes in lifestyle behavior index among saudi adults 16 weeks after COVID-19 pandemic lockdown release. Front Public Health. 2021;9:728117. doi: 10.3389/fpubh.2021.728117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abdulaziz A, Kalevaru CS. Lifestyle changes of attendees at primary health care centers during the COVID-19 pandemic in qassim province, Saudi Arabia. J Family Med Primary Care. 2021;10(10):3838–3844. doi: 10.4103/jfmpc.jfmpc_930_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abdulsalam NM, Khateeb NA, Aljerbi SS, Alqumayzi WM, Balubaid SS, Almarghlani AA, Ayad AA, Williams LL. Assessment of dietary habits and physical activity changes during the full COVID-19 curfew period and its effect on weight among adults in Jeddah, Saudi Arabia. Int J Environ Res Public Health. 2021;18(16):8580. doi: 10.3390/ijerph18168580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al Agha AE, Alharbi RS, Almohammadi OA, Yousef SY, Sulimani AE, Alaama RA. Impact of COVID-19 lockdown on glycemic control in children and adolescents. Saudi Med J. 2021;42(1):44–48. doi: 10.15537/smj.2021.1.25620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al Fagih A, Al Onazi M, Al Basiri S, Al-Kaf F, Dagriri K, Al Hebaishi Y, Samargandy S, Al Shengeiti L. Remotely monitored inactivity due to COVID-19 lockdowns: Potential hazard for heart failure patients. Saudi Med J. 2020;41(11):1211–1216. doi: 10.15537/smj.2020.11.25449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al-Musharaf S, Aljuraiban G, Bogis R, Alnafisah R, Aldhwayan M, Tahrani A. Lifestyle changes associated with COVID-19 quarantine among young Saudi women: A prospective study. PLoS ONE. 2021;16(4 April):e0250625. doi: 10.1371/journal.pone.0250625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alharthi MH. Weight control practices among the Saudi Arabian population during the Covid-19 lockdown. J Family Med Prim Care. 2021;10(10):3797–3802. doi: 10.4103/jfmpc.jfmpc_702_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Almugti HS, Alotaibi A, Almohammed A, Abuhadi R, Baeshen R, Alharthi Z, Alsharari A, Alotaibi S, Omar Y, Alturki N, et al. Impact of COVID-19 on Saudi Children: Special Focus on Behavioral, Social, and Emotional Aspects, 2020–2021. Cureus. 2021;13(11):e19856. doi: 10.7759/cureus.19856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alotaibi AS, Boukelia B. The effect of pre-quarantine physical activity on anxiety and depressive symptoms during the covid-19 lockdown in the kingdom of saudi arabia. Int J Environ Res Public Health. 2021;18(15):7771. doi: 10.3390/ijerph18157771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alqurashi RM. Changes in Nutritional Habits and lifestyles during the COVID-19 Lockdown period in Saudi Arabia: A Cross-Sectional Study. Current Res Nutr Food Sci. 2021;9(3):934–944. doi: 10.12944/CRNFSJ.9.3.20. [DOI] [Google Scholar]
- 41.Bakhsh MA, Khawandanah J, Naaman RK, Alashmali S. The impact of COVID-19 quarantine on dietary habits and physical activity in Saudi Arabia: a cross-sectional study. BMC Public Health. 2021;21(1):1487. doi: 10.1186/s12889-021-11540-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barwais FA. Physical activity at home during the covid-19 pandemic in the two mostaffected cities in Saudi Arabia. Open Public Health Journal. 2020;13(1):470–476. doi: 10.2174/1874944502013010470. [DOI] [Google Scholar]
- 43.BinDhim NF, Althumiri NA, Basyouni MH, AlMousa N, AlJuwaysim MF, Alhakbani A, Alrashed N, Almahmoud E, AlAloula R, Alqahtani SA. Exploring the Impact of COVID-19 Response on Population Health in Saudi Arabia: Results from the "Sharik" Health Indicators Surveillance System during 2020. Int J Environ Res Public Health. 2021;18(10):5291. doi: 10.3390/ijerph18105291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hanbazaza M, Wazzan H. Changes in eating habits and lifestyle during COVID-19 curfew in children in Saudi Arabia. Nutr Res Pract. 2021;15(Suppl 1):S41–s52. doi: 10.4162/nrp.2021.15.S1.S41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jalal SM, Beth MRM, Al-Hassan HJM, Alshealah NMJ. Body mass index, practice of physical activity and lifestyle of students during COVID-19 lockdown. J Multidiscip Healthc. 2021;14:1901–1910. doi: 10.2147/JMDH.S325269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Magliah SF, Zarif HA, Althubaiti A, Sabban MF. Managing Type 1 diabetes among Saudi adults on insulin pump therapy during the COVID-19 lockdown. Diabetes Metab Syndr. 2021;15(1):63–68. doi: 10.1016/j.dsx.2020.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Šagát P, Bartík P, González PP, Tohănean DI, Knjaz D. Impact of COVID-19 quarantine on low back pain intensity, prevalence, and associated risk factors among adult citizens residing in Riyadh (Saudi Arabia): a cross-sectional study. Int J Environ Res Public Health. 2020;17(19):7302. doi: 10.3390/ijerph17197302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sultan I, Alobaidi RA, Sewaid KK, Bader MU, Almuwallad NT, Mohammed RA. Assessment of the effect of the COVID-19 pandemic on the lifestyle of the population in saudi arabia: a cross-sectional online survey study. Cureus. 2021;13(11):e19796. doi: 10.7759/cureus.19796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Caputo EL, Reichert FF. Studies of physical activity and covid-19 during the pandemic: a scoping review. J Phys Act Health. 2020;17(12):1275–1284. doi: 10.1123/jpah.2020-0406. [DOI] [PubMed] [Google Scholar]
- 50.Cheikh Ismail L, Osaili TM, Mohamad MN, Al Marzouqi A, Jarrar AH, Zampelas A, Habib-Mourad C, Omar Abu Jamous D, Ali HI, Al Sabbah H, et al. Assessment of eating habits and lifestyle during the coronavirus 2019 pandemic in the Middle East and North Africa region: a cross-sectional study. Br J Nutr. 2021;126(5):757–766. doi: 10.1017/S0007114520004547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mumena W. Impact of COVID-19 Curfew on Eating Habits, Eating Frequency, and Weight According to Food Security Status in Saudi Arabia: A Retrospective Study. Progress in Nutrition. 2021;22(4):1–9. [Google Scholar]
- 52.Alshahrani SM, Alghannam AF, Taha N, Alqahtani SS, Al-Mutairi A, Al-Saud N, Alghnam S. The impact of COVID-19 pandemic on weight and body mass index in Saudi Arabia: A longitudinal study. Front Public Health. 2021;9:775022. doi: 10.3389/fpubh.2021.775022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Alsalman AA, Aldossari MR, Alomani ZD, Alkhunaizi SI, Aljardah ZA, Almousa FA, Kalalah ZA. Impact of coronavirus disease lockdown on children with type 1 diabetes mellitus in Al-Khobar, Saudi Arabia. Cureus. 2022;14(1):e21350. doi: 10.7759/cureus.21350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alzahrani F, Alshahrani NZ, Abu Sabah A, Zarbah A, Abu Sabah S, Mamun MA. Prevalence and factors associated with mental health problems in Saudi general population during the coronavirus disease 2019 pandemic: A systematic review and meta-analysis. Psych J. 2022;11(1):18–29. doi: 10.1002/pchj.516. [DOI] [PubMed] [Google Scholar]
- 55.Al Dhaheri AS, Bataineh MF, Mohamad MN, Ajab A, Al Marzouqi A, Jarrar AH, Habib-Mourad C, Abu Jamous DO, Ali HI, Al Sabbah H, et al. Impact of COVID-19 on mental health and quality of life: Is there any effect? A cross-sectional study of the MENA region. PLoS ONE. 2021;16(3):e0249107. doi: 10.1371/journal.pone.0249107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Almhizai RA, Almogren SH, Altwijery NA, Alanazi BA, Al Dera NM, Alzahrani SS, Alabdulkarim SM. Impact of COVID-19 on children's and adolescent's mental health in Saudi Arabia. Cureus. 2021;13(11):e19786. doi: 10.7759/cureus.19786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Al-Quwaidhi AJ, Pearce MS, Critchley JA, Sobngwi E, O'Flaherty M. Trends and future projections of the prevalence of adult obesity in Saudi Arabia, 1992–2022. East Mediterr Health J. 2014;20(10):589–595. doi: 10.26719/2014.20.10.589. [DOI] [PubMed] [Google Scholar]
- 58.GBD Eastern Mediterranean Region Obesity Collaborators Burden of obesity in the Eastern Mediterranean Region: findings from the Global Burden of Disease 2015 study. Int J Public Health. 2018;63(Suppl 1):165–176. doi: 10.1007/s00038-017-1002-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Salem V, AlHusseini N, Razack H, Naoum A, Sims O, Alqahtani S. Prevalence, risk factors, and interventions for obesity in Saudi Arabia: A systematic review. Obes Rev. 2022;23(7):e13448. doi: 10.1111/obr.13448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sallis R, Young DR, Tartof SY, Sallis JF, Sall J, Li Q, Smith GN, Cohen DA. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. Br J Sports Med. 2021;55(19):1099–1105. doi: 10.1136/bjsports-2021-104080. [DOI] [PubMed] [Google Scholar]
- 61.Cho DH, Lee SJ, Jae SY, Kim WJ, Ha SJ, Gwon JG, Choi J, Kim DW, Kim JY. Physical activity and the risk of COVID-19 infection and mortality: a nationwide population-based case-control study. J Clin Med. 2021;10(7):1539. doi: 10.3390/jcm10071539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Aytur S, Jones S, Stransky M, Evenson K. Measuring physical activity in outdoor community recreational environments: Implications for research, policy, and practice. Curr Cardiovasc Risk Rep. 2015;9(423):1–13. doi: 10.1007/s12170-014-0423-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Volenec ZM, Abraham JO, Becker AD, Dobson AP. Public parks and the pandemic: How park usage has been affected by COVID-19 policies. PLoS ONE. 2021;16(5):e0251799. doi: 10.1371/journal.pone.0251799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gu X, Keller J, Zhang T, Dempsey D, Roberts H, Jeans K, Stevens W, Borchard J, VanPelt J, Tulchin-Francis K. Disparity in built environment and its impacts on youths' physical activity behaviors during COVID-19 pandemic restrictions. J Racial Ethn Disparities. 2022;14:1–11. doi: 10.1007/s40615-022-01341-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chinapaw MJ, Mokkink LB, van Poppel MN, van Mechelen W, Terwee CB. Physical activity questionnaires for youth: a systematic review of measurement properties. Sports Med (Auckland, NZ. 2010;40(7):539–563. doi: 10.2165/11530770-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 66.Zhang F, Zhang Y, Yu Y, Lu W, Zhang H. Bibliometric analysis of the top-50 cited articles on COVID-19 and physical activity. Front Public Health. 2022;10:926244. doi: 10.3389/fpubh.2022.926244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ramirez Varela A, Hallal PC, Mejia Grueso J, Pedisic Z, Salvo D, Nguyen A, Klepac B, Bauman A, Siefken K, Hinckson E, et al. Status and trends of physical activity surveillance, policy, and research in 164 countries: findings from the global observatory for physical activity-GoPA! 2015 and 2020 surveys. J Phys Act Health. 2023;20(2):112–128. doi: 10.1123/jpah.2022-0464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Reilly JJ, Barnes J, Gonzalez S, Huang WY, Manyanga T, Tanaka C, Tremblay MS. Recent secular trends in child and adolescent physical activity and sedentary behavior internationally: analyses of active healthy kids global alliance global matrices 1.0 to 4.0. J Phys Activity Health. 2022;19(11):729–736. doi: 10.1123/jpah.2022-0312. [DOI] [PubMed] [Google Scholar]
- 69.Aubert S, Barnes JD, Demchenko I, Hawthorne M, Abdeta C, Abi Nader P, Adsuar Sala JC, Aguilar-Farias N, Aznar S, Bakalar P, et al. Global matrix 4.0 physical activity report card grades for children and adolescents: results and analyses from 57 countries. J Phys Activity Health. 2022;19(11):700–728. doi: 10.1123/jpah.2022-0456. [DOI] [PubMed] [Google Scholar]
- 70.Arena R, Pronk NP, Laddu D, Whitsel LP, Sallis JF, Lavie CJ, Network H-P. Mapping one million COVID-19 deaths and unhealthy lifestyle behaviors in the United States: recognizing the syndemic pattern and taking action. Am J Med. 2022;135(11):1288–1295. doi: 10.1016/j.amjmed.2022.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.World Health Organization: Global Status Report on Physical Activity Edited by the world health organization. Geneva, Switzerland. 2022;2022:1–112. [Google Scholar]
- 72.Milton K, Cavill N, Chalkley A, Foster C, Gomersall S, Hagstromer M, Kelly P, Kolbe-Alexander T, Mair J, McLaughlin M, et al. Eight investments that work for physical activity. J Phys Act Health. 2021;18(6):625–630. doi: 10.1123/jpah.2021-0112. [DOI] [PubMed] [Google Scholar]
- 73.Al-Hazzaa HM. Physical activity research in the gulf cooperation council countries: progress made but work still to do. J Phys Act Health. 2022;19(11):769–770. doi: 10.1123/jpah.2022-0484. [DOI] [PubMed] [Google Scholar]
- 74.Alqahtani AS, Baattaiah BA, Alharbi MD, Khan F, Aldhahi MI. Barriers and facilitators affecting physical activity among adults in Saudi Arabia during COVID-19 quarantine. Health Promot Int 2021;daab191. 10.1093/heapro/daab191. [DOI] [PubMed]
- 75.Chaabane S, Chaabna K, Doraiswamy S, Mamtani R, Cheema S. Barriers and facilitators associated with physical activity in the middle east and north africa region: a systematic overview. Int J Environ Res Public Health. 2021;18(4):1647. doi: 10.3390/ijerph18041647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Knight RL, McNarry MA, Sheeran L, Runacres AW, Thatcher R, Shelley J, Mackintosh KA. Moving forward: understanding correlates of physical activity and sedentary behaviour during Covid-19-an integrative review and socioecological approach. Int J Environ Res Public Health. 2021;18(20):10910. doi: 10.3390/ijerph182010910. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) Checklist. Table S2. Databases searched, search structure, and search terms. Table S3. Quality assessment tool applied to each included study.
Data Availability Statement
All data generated or analyzed during this study are referenced in this published article.


