Abstract
Purpose
The prevalence of burnout in intensive care unit (ICU) professionals is difficult to establish due to the variety of survey instruments used, the heterogeneity of the targeted population, the design of the studies, and the differences among countries regarding ICU organization.
Methods
We performed a systematic review and meta-analysis examining the prevalence of high-level burnout in physicians and nurses working in adult ICUs, including only studies that use the Maslach Burnout Inventory (MBI) as a tool to evaluate burnout and involving at least 3 different ICUs.
Results
Twenty-five studies with a combined population of 20,723 healthcare workers from adult ICUs satisfied the inclusion criteria. Combining 18 studies including 8187 ICU physicians, 3660 of them reported a high level of burnout (prevalence 0.41, range 0.15–0.71, 95% CI [0.33; 0.5], I2 97.6%, 95% CI [96.9%; 98.1%]). The heterogeneity can be at least in part explained by the definition of burnout used and the response rate as confirmed by the multivariable metaregression done. In contrast, there was no significant difference regarding other factors such as the study period (before or during the coronavirus disease 2019 (COVID-19) pandemic), the income of the countries, or the Healthcare Access and Quality (HAQ) index. Combining 20 studies including 12,536 ICU nurses, 6232 of nurses were reporting burnout (prevalence 0.44, range 0.14–0.74, [95% CI 0.34; 0.55], I2 98.6% 95% CI [98.4%; 98.9%]). The prevalence of high-level burnout in ICU nurses for studies performed during the COVID-19 pandemic was higher than that reported for studies performed before the COVID-19 pandemic (0.61 [95% CI, 0.46; 0.75] and 0.37 [95% CI, 0.26; 0.49] respectively, p = 0.003). As for physicians, the heterogeneity is at least in part explained by the definition used for burnout using the MBI but not by the number of participants. When compared, the prevalence of high-level burnout was not different between ICU physicians and ICU nurses. However, the proportion of ICU nurses with a high level of emotional exhaustion was higher than for ICU physicians (0.42 [95% CI, 0.37; 0.48] and 0.28 [0.2; 0.39], respectively, p = 0.022).
Conclusion
According to this meta-analysis, the prevalence of high-level burnout is higher than 40% in all ICU professionals. However, there is a great heterogeneity in the results. To evaluate and to compare preventive and therapeutic strategies, there is the need to use a consensual definition of burnout when using the MBI instrument.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00134-023-07025-8.
Keywords: Burnout, MBI, COVID-19, Nurses, Physicians
Take-home message
| Twenty-five studies with a combined population of 20,723 healthcare workers (8187 physicians and 12,536 nurses) from adult intensive care units (ICUs) have been included in this meta-analysis. A high level of burnout has been observed in 41% of the ICU physicians and in 44% of the ICU nurses. The coronavirus disease 2019 pandemic was associated with an increase in the prevalence of high-level burnout only in ICU nurses. |
Introduction
Burnout is an occupational phenomenon that has been described by Maslach et al. [1] as a condition in which professionals “lose all concern, all emotional feeling for the people they work with, and come to treat them in a detached or even dehumanized way”. Professional burnout is a psychological syndrome arising in response to chronic emotional and interpersonal stressors on the job [2] and is characterized by three different features: emotional exhaustion, depersonalization, and lack of personal and professional completion [3]. Burnout has been recently identified as an “occupational phenomenon” in the World Health Organization’s (WHO) International Classification of Diseases, 11th Revision. WHO (2019) which described burnout as follows: “Burnout is a syndrome conceptualized as resulting from chronic workplace stress that has not been successfully managed.” Intensive care unit (ICU) professionals are at high risk of experiencing burnout due to the high density of ICU professionals, mainly intensivists and critical care nurses (but also respiratory therapists, pharmacists and others who spend time in the ICU), the presence of patients with life-threatening illnesses, the observed discrepancies in job demands, responsibility overload, workload, end-of-life issues, perception of futility and staff unwillingness to withdraw life sustaining treatment, and interpersonal conflicts all constituting potential stressors [4]. The consequences of burnout in ICU providers are substantial, with implications for workplace morale, quality of care delivered, patient safety, and also costs of care, including those related to ICU professionals staff turnover [5, 6].
The prevalence of burnout in ICU professionals has been extensively studied for 15 years. However, a precise estimation of its prevalence is difficult due to the variety of survey instruments used, the heterogeneity of the targeted population, the design of the studies, the period of the study (pre-coronavirus disease (COVID-19) era or COVID-19 era), and differences among countries regarding ICU organization. Burnout is mostly diagnosed by using the Maslach Burnout Inventory (MBI) [7]. The MBI is a 22-item, self-report questionnaire that requests respondents to indicate on a seven-point Likert scale the frequency with which they experience certain feelings related to their job. The MBI has been shown to be reproducible and valid [1–3] and is the most widely used instrument to asses burnout in healthcare workers. Due to these heterogeneities, the main objective of this systematic review and meta-analysis was to estimate the prevalence of high-level burnout in physicians and nurses working in adult ICUs, only including studies using the MBI as a tool to evaluate burnout and involving at least 3 different ICUs.
Methods
Protocol and registration
The protocol of this study was preregistered on PROSPERO (CRD42022340015). This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines (supplementary Table S1).
Search strategy and selection criteria
The MEDLINE via PubMed (including In-Process and Epub ahead of print) and Embase databases and the Cochrane Central Register of Controlled Trials database were systematically searched without language restrictions or period limitations. Trial registries including ClinicalTrials.gov were also considered to identify completed and ongoing trials. The electronic search for relevant theoretical references was carried out in May 2022 (more recent publications were considered until September 2022). We searched for studies referring to the following subject index terms: (burnout[Title/Abstract]) AND (ICU[Title/Abstract). To limit heterogeneity, which is reported in meta-analyses related to physicians/nurses [8, 9], we used strict criteria. Therefore, cohort studies or randomized controlled trials involving at least 3 ICUs and including ICU physicians and/or nurses were included. These studies had to provide the prevalence of high-level burnout separately for ICU physicians and ICU nurses, using the MBI instrument [9]. Determination of the level of burnout had to be a primary or a secondary objective of the included studies. Studies focused solely on residents/interns or only involving paediatric ICUs or neonatal ICUs and studies performed in selected ICU patients (post-Do Not Resuscitate orders, trauma….) were not included. Moreover, we excluded papers that provided overall burnout prevalence in groups of healthcare workers (including ICU professionals) but did not give specific data on the burnout of ICU physicians and nurses. Studies published only in abstract form were also excluded.
Data extraction
Article selection was first performed by two independent reviewers based on titles and abstracts (LP&SH). They then independently reviewed the full texts of studies that appeared potentially relevant to determine their eligibility for inclusion. Data extraction was also performed by the two independent reviewers (LP&SH) with the use of a data collection form. Disagreements were resolved by a third reviewer who had the deciding vote (LB). General and specific characteristics of each study were obtained, including the year of publication, the country, the study design, the number of physicians/nurses involved, the gender, the response rate, the MBI definition used, the study period (pre-COVID-19 or COVID-19), the number of subjects with a high level of burnout and the MBI features. In order to consider differences across countries, the World Bank country classification was used to rank countries according to their income level. It assigns the world’s economies to four income groups (low, lower-middle, upper-middle, and high-income countries) according to Gross National Index (GNI) per capita. The Healthcare Access and Quality (HAQ) Index was used to measure personal health-care access and quality across countries [10]. This index is measured on a scale from 0 (worst) to 100 (best), based on death rates from 32 causes of death that could be avoided by timely and effective medical care (also known as 'amenable mortality').
Quality assessment
A quality assessment was performed by two independent reviewers (LP&LB) at both the individual study level and outcome level. The Joanna Briggs Institute (JBI) critical appraisal checklist for studies reporting prevalence data was used to assess the methodological quality of a study and to determine the extent to which a study has addressed the possibility of bias in its design, conduct and analysis [11].
Data analysis
The primary outcome was the proportion of ICU physicians and the proportion of ICU nurses (analysed separately) presenting with a high-level of burnout according to the MBI. The MBI is a 22-item self-report questionnaire that evaluates the three domains of burnout in independent subscales: emotional exhaustion, depersonalization, and personal accomplishment. The MBI is used (and validated) in many languages including English, French, German, Portuguese, Chinese, and Korean. Additional outcomes included the prevalence of the three different features of burnout: high levels of emotional exhaustion and/or depersonalization and/or low level of personal accomplishment in ICU physicians and in ICU nurses. Prevalence estimates of burnout were calculated by pooling the study-specific estimates using random-effects meta-analyses and inverse variance method. Because of the high level of heterogeneity, Hartung-Knapp method of pooling and estimating 95% confidence intervals were used to account for uncertainty in the variance estimate [12].
Heterogeneity was assessed using the Higgins’ inconsistency test (I2) and the Cochran Q statistic. The I2 was interpreted as follows: values < 25% indicate low; 25–75%, moderate; and > 75%, considerable heterogeneity [13, 14].
The potential sources of heterogeneity were investigated by arranging groups of studies according to potentially relevant characteristics into subgroups and univariable meta-regression analyses. The factors that were individually examined included the following: the MBI definition used > − 9 vs. other thresholds, physicians vs. nurses, COVID-19 vs. non-COVID-19 period, upper-middle income countries vs. high-income countries, sex ratio, sample size (according to different thresholds: 50, 100 and 200 participants), response rates and HAQ index. The factors associated with heterogeneity at P < 0.10 were subsequently included in multivariable meta-regression models [15].
Sensitivity analyses were performed by serially excluding each study to determine the implications of individual studies for the pooled estimates [16]. Sensitivity analyses for risk of bias was done based on two categories for the total score of JBI (> 50% vs. ≤ 50%) [17].
Potential publication bias was assessed by visual inspection of funnel plots, and plot asymmetry was considered suggestive of a reporting bias [18]. Plot asymmetry was tested using Egger’s test based on a weighted linear regression of the treatment effect on its standard error [19].
All analyses were performed using R statistical software version 4.1.3 with the ‘meta’ package [20]. All significance tests were 2-tailed, with P < 0.05 considered statistically significant.
Role of the funding source
This study had no funding source. The corresponding author had full access to all study data and had the final responsibility for the decision to submit this article for publication.
Results
Study characteristics
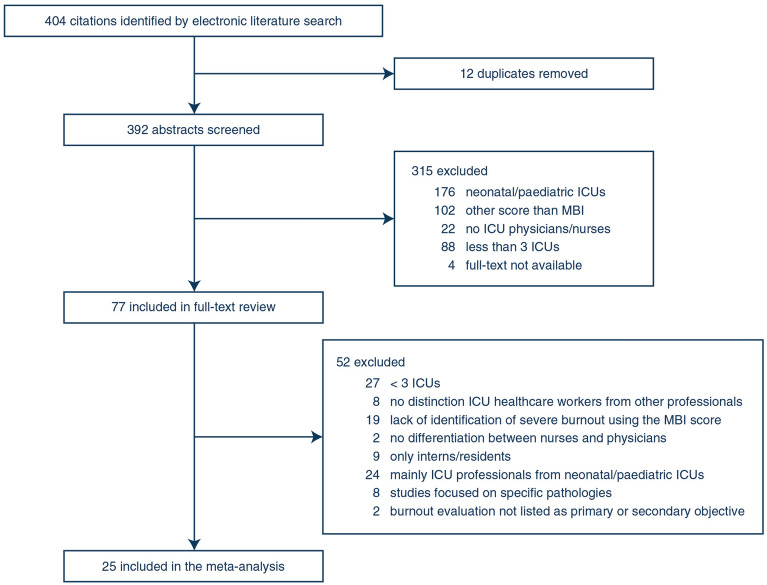
The electronic search recovered 404 citations, 77 of which were selected for full-text assessment (Fig. 1). Twenty-five studies with a combined population of 20,723 healthcare workers (8187 physicians and 12,536 nurses) from adult ICUs satisfied the inclusion criteria [21–45]. These studies were published between 2007 to 2021. Only two articles were published before 2010 [37, 45]. Regarding the journal field of the included studies, 13 were published in the critical care field [23, 24, 28, 29, 31, 32, 34–39, 44], 6 were published in the nursing field [21, 22, 27, 43, 45, 46], 3 were published in the anaesthesiology field [30, 33, 40], 2 were published in the general medical journals field [25, 42] and 1 was published in the field of ethics [41]. The characteristics of the selected articles are presented in Table 1, including the year of study, country, high-level burnout definition, sample size, participation rate, and prevalence of high-level burnout. Fourteen of these 25 studies came from Europe [22, 24, 27, 29, 33, 34, 36, 37, 39–41, 43–45]. Six studies were done, at least in part, during the COVID-19 pandemic [22–24, 27–29]. Three [27–29] of these 6 studies had two inclusion periods (pre- and during COVID-19 pandemic) which were considered separately (Table 1) initially. However, after careful evaluation of the factors contributing to heterogeneity, we only have taken into account the COVID-19 period of these three surveys [27–29]. In 10 studies, a high level of burnout was defined by a cumulative MBI score higher than–9 [23–25, 28, 29, 36–39, 44]. Reported response rates varied from 15 to 98.8% [21–45]. The quality assessment of the included studies is presented in supplementary Table S2.
Fig. 1.
Flow diagram of study selection
Table 1.
Characteristics of the included studies
| Embriaco et al. [37], 2007 | Frade Mera et al. [45], 2009 | Voultsos et al. [33], 2010 | Merlani et al. [39], 2011 | Karanikola et al. [43], 2012 | Giannini et al. [44], 2013 | Teixeira et al. [40], 2013 | Burghi et al. [38], 2014 | Teixeira et al. [41], 2014 | Zhang et al. [42], 2014 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Country | France | Spain | Greece, Cyprus | Switzerland | Greece | Italy | Portugal | Uruguay | Portugal | China |
| Multicenter | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Study carried out during the pre-COVID-19 era | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Physicians, N | 978 | – | 80 | 459 | – | 71 | 73 | 82 | 82 | – |
| Female gender, N | 244 | – | 49 | 193 | 37 | – | – | – | – | |
| Nurses, N | – | 123 | – | 2415 | 152 | 127 | 194 | 282 | 218 | 426 |
| Female gender, N | – | – | – | 2018 | 119 | 33 | – | – | – | 377 |
| Definition of high-level burnout | Total > − 9 | EE > 24 + DP ≥ 9 + PA < 33 | EE ≥ 27 or DP ≥ 10 or PA ≤ 33 | Total > − 9 | EE ≥ 31 + DP ≥ 11 + PA ≤ 35 | Total > − 9 | EE ≥ 25 + DP ≥ 10 + PA ≤ 32 | Total > − 9 | EE ≥ 25 + DP ≥ 10 + PA ≤ 32 | EE ≥ 27 + DP ≥ 10 + PA ≤ 33 |
| Response rate, % | 82 | 73 | 81.6 | 76 | 21 | 89 | 67 | 88 | – | 98.8 |
| Garrouste et al. [36], 2015 | Awajeh et al. [21], 2018 | See et al. [35], 2018 | Vincent et al. [34], 2019 | Rosa et al. [25], 2019 | Azoulay et al. [24], 2020 | Azoulay et al. [23], 2021 | Bruyneel et al. [22], 2021 | Butera et al. [27], 2021 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Country | France | Saudi Arabia | Asia | UK | Brazil | International | France | Belgium | Belgium | |
| Multicenter | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Study carried out during the pre-COVID-19 era | Yes | Yes | Yes | Yes | Yes | No (1st wave) | No (2nd wave) | No (1st wave) | Yes | No (1st wave) |
| Physicians, N | 330 | – | 992 | 766 | 50 | 846 | 175 | – | – | – |
| Female gender, N | 138 | – | 283 | 235 | – | 290 | – | – | – | – |
| Nurses, N | – | 270 | 3100 | 157 | 85 | – | 412 | 1135 | 283 | 1189 |
| Female gender, N | – | 262 | 2700 | 125 | – | – | – | 892 | – | – |
| Definition of high-level burnout | Total > − 9 | EE ≥ 27 + DP ≥ 10 + PA ≤ 33 | EE ≥ 28 or DP ≥ 11 | EE ≥ 27 ± DP ≥ 10 ± PA ≤ 33 | Total > − 9 | Total > − 9 | Total > − 9 | EE ≥ 27 or DP ≥ 10 or PA ≤ 33 | EE ≥ 27 or DP ≥ 10 or PA ≤ 33 | EE ≥ 27 or DP ≥ 10 or PA ≤ 33 |
| Response rate, % | 82 | 90 | 66 | – | 89 | 15 | 70.2 | – | 46 | 68 |
| Hu et al. [31], 2021 | Kok et al. [29], 2021 | Moll et al. [28], 2021 | Wang et al. [32], 2021 | Yildiz et al. [26], 2021 | Omar et al. [30], 2022 | |||
|---|---|---|---|---|---|---|---|---|
| Country | China | The Netherlands | US | China | Turkey | Qatar | ||
| Multicenter | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Study carried out during the pre-COVID-19 era | Yes | Yes | No (1st wave) | Yes | No (2nd wave) | No (1st wave) | Yes | Yes |
| Physicians, N | 1122 | 53 | 49 | 43 | 59 | 1813 | – | 160 |
| Female gender, N | 484 | – | – | 9 | 16 | 673 | – | – |
| Nurses, N | 1289 | 199 | 184 | 425 | 453 | – | 164 | 201 |
| Female gender, N | 1172 | – | – | 323 | 372 | – | 112 | – |
| Definition of high-level burnout | EE ≥ 27 or DP ≥ 13 or PA ≤ 31 | Total > − 9 | Total > − 9 | Total > − 9 | Total > − 9 | EE ≥ 27 + DP ≥ 10 or PA ≤ 33 | EE ≥ 18 or DP ≥ 10 or PA ≤ 21 | EE ≥ 27 ± DP ≥ 13 ± PA ≤ 33 |
| Response rate, % | 31.3 | 53.3 | 53.3 | 46.5 | 49.9 | 90.7 | 68 | 36.4 |
EE emotional exhaustion, DP depersonalisation, PA personal accomplishment
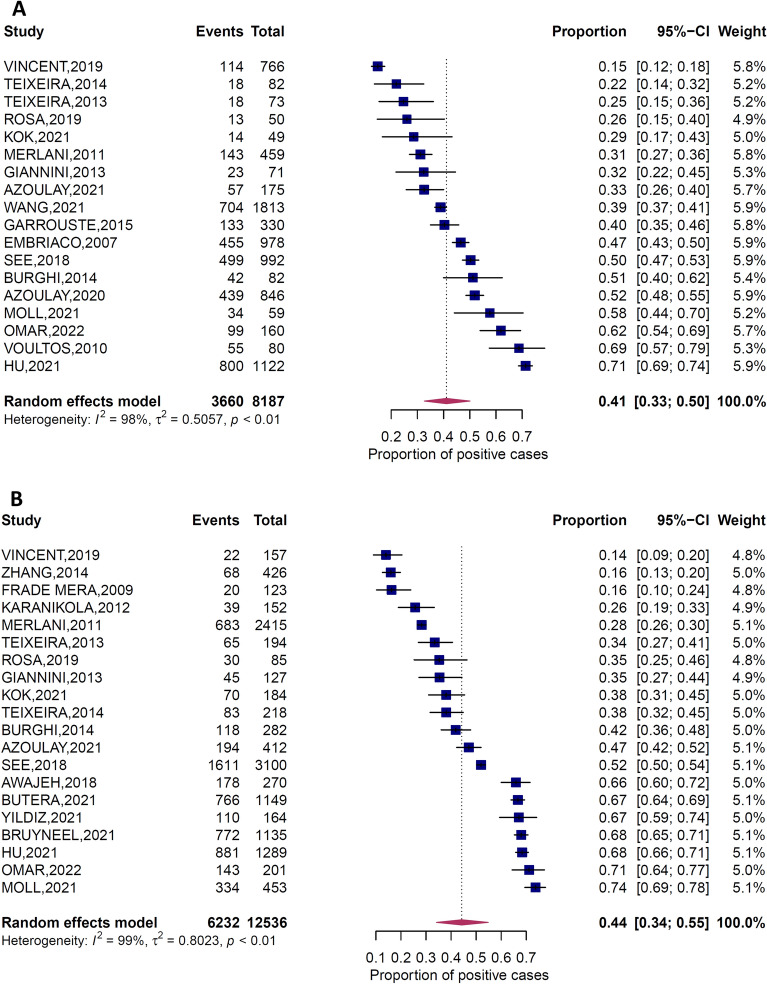
Prevalence of high-level burnout in ICU physicians
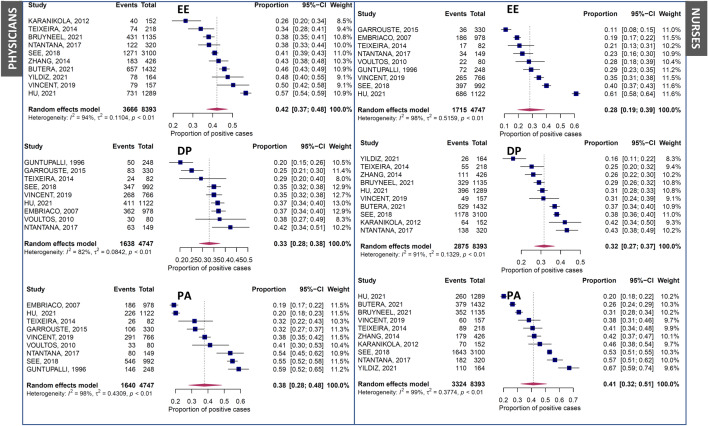
The prevalence of high-level burn out ranged from 0.15 to 0.71 across 18 primary studies totalling 8187 ICU physicians, 3660 of them were presenting with a high level of burnout (random effects model, proportion (prevalence 0.41, range 0.15–0.71, 95% CI [0.33; 0.5], I2 97.6%, 95% CI [96.9%; 98.1%]) (Fig. 2A). The proportion of ICU physicians with a high level of emotional exhaustion was 0.28 [95% CI 0.2; 0.39] (Fig. 3), slightly lower than the proportion of ICU physicians with a high level of depersonalisation (0.33 [95% CI 0.28; 0.38]) (Fig. 3) while the proportion of subjects reporting low personal accomplishment was the highest (0.38 [95% CI 0.28; 0.48]) (Fig. 3).
Fig. 2.
Forest plots representing the prevalence of high-level burnout in ICU physicians (A) and in ICU nurses (B)
Fig. 3.
Forest plots representing the prevalence of high-level of emotional exhaustion (EE), depersonalization (DP) and low personal accomplishment (PA) in ICU physicians (left panel)) and in ICU nurses (right panel)
The associated funnel plots were globally symmetrical for the different outcomes (supplementary Figure S1A). The P values of Egger’s regression intercept were all > 0.05.
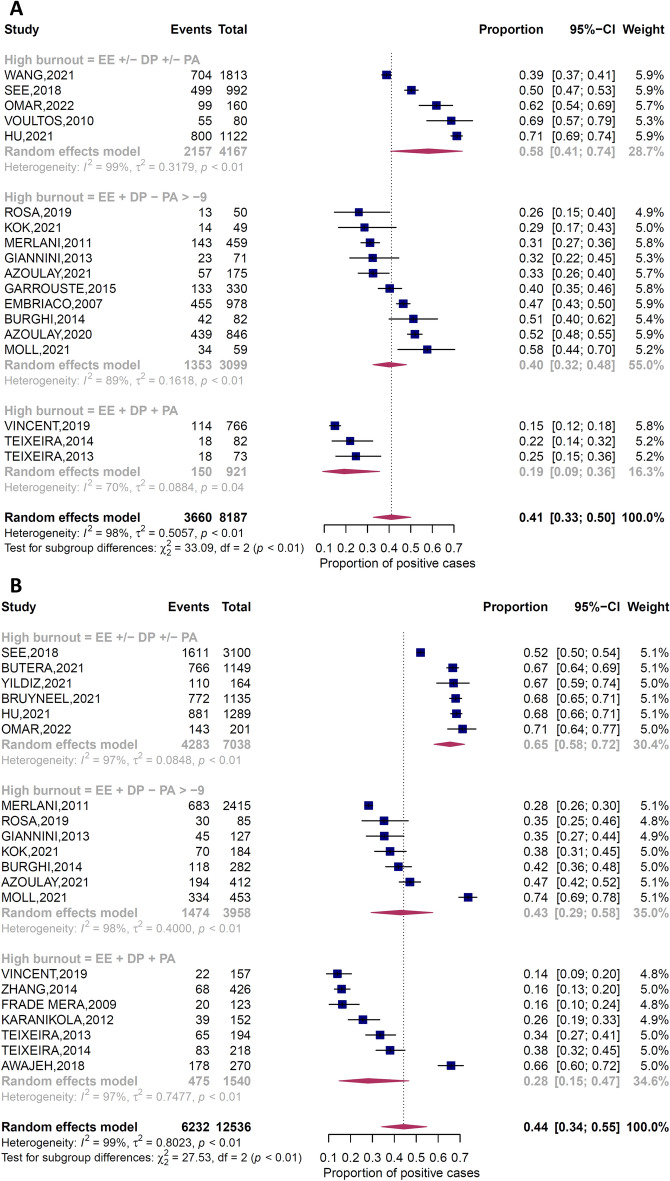
The sub-group analysis (supplementary Figure S2) according to the study period (during the COVID-19 pandemic or not) revealed that there was no significant difference regarding the prevalence of high-level of burnout in ICU physicians (0.47 [95% CI, 0.29; 0.65] for studies performed during the COVID-19 pandemic and 0.39 [95% CI, 0.29; 0.51] for studies performed before the COVID-19 pandemic (p = 0.38). Another sub-group analysis was performed according to country income and there was no difference in burnout prevalence between the upper-middle income countries (4 studies) compared with those from high-income countries (13 studies) (burnout prevalence in ICU physicians, 0.47 [95% CI, 0.20; 0.77] and 0.38 [95% CI, 0.28; 0.49] respectively, p = 0.43). An additional analysis evaluated the relationship between the definition of high-level burnout using a combined score of the MBI instrument (total score > − 9) compared to two alternate definitions (e.g. using only one or two domains of the MBI or using the three domains). There was a statistical difference in reported burnout between these different definition groups: 0.58 [95% CI 0.41; 0.74] (EE ± DP ± PA), 0.40 [95% CI 0.33; 0.48] (EE + DP—PA > − 9) and 0.19 [95% CI 0.09; 0.36] (EE + DP + PA), p < 0.0001 (Fig. 4A). There was also a statistical difference (p = 0.0005) according to the sample size with lower prevalence in sample size ≤ 50 participants (0.27 [95% CI 0.14; 0.46]) vs. > 50 participants (0.43 [95% CI 0.33; 0.53]). Meta-regression reported no influence of the sex ratio (− 0.19, [95% CI, − 1.01;0.63], p = 0.61), the response rate (− 0.01 [95% CI, − 0.03;0.00], p = 0.07) and the HAQ index (− 0.02 [95% CI, − 0.05; 0.01, p = 0.27) regarding the prevalence of high-level burnout in ICU physicians (supplementary Figure S3A). The multivariable metaregression results showed that the association was significant for the definition of high-level burnout (EE ± DP ± PA vs. EE + DP—PA > − 9: 0.54 [95% CI 0.04; 1.04], p = 0.04) and the response rate: − 0.01 [95% CI, − 0.02; − 0.04], p = 0.04). Sensitivity analyses based on a serial exclusion process for each study did not change the effect on the various studied endpoints, confirming the robustness of our findings (supplementary Figure S4). The comparison between the two categories for the total score of JBI (> 50% vs. ≤ 50%) did not show any statistical difference (p = 0.69).
Fig. 4.
Forest plots representing the prevalence of high-level burnout in ICU physicians (A) and in ICU nurses (B) according to the definition used. EE emotional exhaustion, DP Depersonalization, PA low Personal Accomplishment
Prevalence of high-level burnout in ICU nurses
The prevalence of high-level burnout ranged from 0.14 to 0.74 across 20 primary studies totalling 12,536 ICU nurses, 6232 of them were presenting with burnout (random effects model, proportion (prevalence 0.44, range 0.14–0.74, [95% CI 0.34; 0.55], I2 98.6% 95% CI [98.4%; 98.9%]) (Fig. 2). The proportion of ICU nurses with a high level of emotional exhaustion was high (0.42 [95% CI, 0.37; 0.48]) (Fig. 3) and comparable to the proportion of subjects reporting low personal accomplishment (0.41 [95% CI, 0.32; 0.51]) (Fig. 3). The proportion of ICU nurses with a high level of depersonalisation was slightly lower (0.32 [95% CI, 0.27; 0.37]) (Fig. 3).
The associated funnel plots were globally symmetrical for the different outcomes (supplementary Figure S1B). The P values of Egger’s regression intercept were all > 0.05.
The sub-group analysis (supplementary Figure S5) according to the study period (during COVID-19 pandemic compared to pre-COVID-19) performed in ICU nurses showed that the prevalence of high-level burnout in ICU nurses for studies performed during the COVID-19 pandemic was higher compared to studies performed before the COVID-19 pandemic (0.61 [95% CI, 0.46; 0.75] and 0.37 [95% CI, 0.26; 0.49] respectively, p = 0.003).
A sub-group analysis evaluating the relationship between country income and reported burnout in nurses did not show any difference between upper-middle income countries (5 studies) compared to high-income countries (15 studies) (burnout prevalence in ICU nurses, 0.47 [95%CI, 0.19; 0.75] and 0.44 [95%CI, 0.32; 0.56] respectively, p = 0.83). Like physicians, there was a difference (p < 0.0001) in reported burnout in nurses by definition: 0.65 [95% CI, 0.58; 0.72] for (EE ± DP ± PA) definition, 0.43 [95% CI, 0.29; 0.58] for (EE + DP—PA > − 9) definition and 0.28 [95% CI, 0.15; 0.47] for (EE + DP + PA) definition (Fig. 4B). There was also a statistical difference (p = 0.0169) according to the sample size with lower prevalence when the sample size was ≤ 200 participants (0.32 [95% CI, 0.2; 0.47]) vs. when there were > 200 participants (0.53 [95% CI, 0.4; 0.66]). Meta-regression reported no influence of the sex ratio (− 0.17, [95% CI, − 1.16; 0.82], p = 0.71), the response rate (− 0.01 [95% CI, − 0.03; 0], p = 0.17) and the HAQ index (− 0.02 [95% CI, − 0.06; 0.03, p = 0.47) regarding the prevalence of high-level burnout in ICU nurses (supplementary Figure S3B). As for physicians, the multivariable metaregression results showed that the association was significant for the definition of high-level burnout (EE ± DP ± PA vs. EE + DP—PA > − 9: 0.81 [95% CI, 0.05;1.57], p = 0.04), but not with the number of participants. Sensitivity analyses based on a serially exclusion process for each study did not change the effect on the various studied endpoints, confirming the robustness of our findings (supplementary Figure S3). The comparison between the two categories for the total score of JBI (> 50% vs. ≤ 50%) did not show any statistical difference (p = 0.98).
Comparison of the prevalence of high-level burnout in ICU physicians and ICU nurses
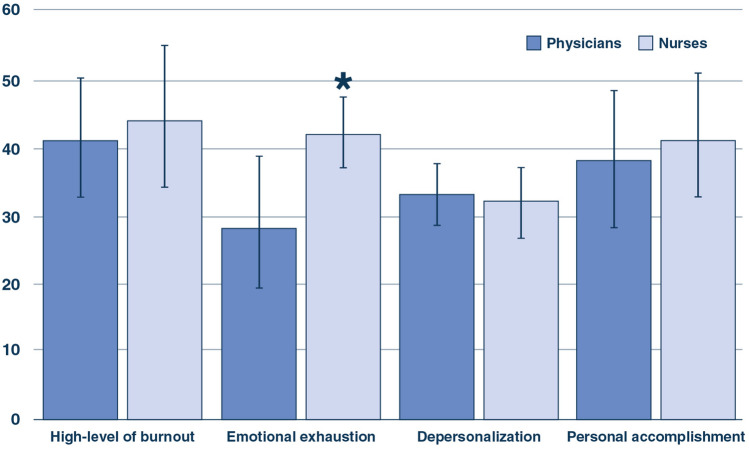
The analysis of the 20,723 included ICU professionals revealed that the prevalence of a high level of burnout was not different (p = 0.63) between ICU physicians (0.41 [95% CI, 0.33; 0.5] and ICU nurses 0.44 [95% CI, 0.34; 0.55]. However, the proportion of ICU professionals with a high level of emotional exhaustion was higher in ICU nurses than in ICU physicians (0.42 [95% CI, 0.37; 0.48] and 0.28 [0.2; 0.39], respectively, p = 0.022). In contrast, there was no difference between ICU nurses and physicians regarding both the proportion of those with a high level of depersonalisation and the proportion of subjects reporting a low personal accomplishment (Fig. 5).
Fig. 5.
Comparison of the proportions (expressed as percentages) of positive cases between ICU physicians and ICU nurses (*p = 0.022)
Discussion
This systematic review and meta-analysis of 25 studies (total N = 20,617 healthcare workers from adult ICUs) showed that the prevalence of ICU physicians and ICU nurses with a high level of burnout were 42 and 45% respectively without any significant differences between them apart from higher reported emotional exhaustion in ICU nurses. The results should however be interpreted considering the large amount of heterogeneity presented in many comparisons despite certain precautions such as using a single instrument (MBI), targeting only ICU professionals (and studying separately nurses and physicians), discarding specialized ICUs and studies involving less than 3 ICUs.
It has been reported that the prevalence of burnout in all ICU professionals ranges from 6 to 47% [47]. Burnout is generally assessed by the Maslach Burnout Inventory (MBI) which is considered the standard instrument for measuring the severity of burnout. However, several methods exist to define the burnout level using the MBI. In the present study, we have reported that there was no influence of the method used to evaluate the prevalence of high-level burnout when using the MBI in both ICU physicians and nurses.
In a meta-analysis including four studies with a sample of 1,986 ICU nurses, the meta-analytic estimate prevalence for high emotional exhaustion was 31% (95% CI, 8–59%), for high depersonalization was 18% (95% CI, 8–30%), and for low personal accomplishment was 46% (95% CI, 20–74%) [48]. We reported an increased level of EE in ICU nurses as compared with doctors. High levels of EE are related to personal factors, as well as work factors such as long working days, high workload, and poor quality of work life [49]. An adequate work environment, with good working relationships and support by the institution, have been reported as protective factors [50].
Due to its associated increased work intensity, high degree of difficulty with regards to patient disease status, and imposition of high emotional stress on both family members and patients, the high prevalence of (high-level) burnout in ICU professionals reported here seems consistent.
A higher level of burnout among healthcare professionals including ICU workers has been reported to be associated with negative outcomes, such as depressive symptoms [51], higher staff turnover, lower job satisfaction, and heart disease [52]. Therefore, not only may burnout decrease the physical and psychological conditions of healthcare professionals, but it also may compromise the health care institutions at which they are employed.
Many factors have been reported to be associated with burnout such as age, sex, marital status, personality traits, work experience in an ICU, work environment, workload and shift work, ethical issues, and end-of-life decision-making [47]. Quality of the relationships between ICU nurses and ICU physicians is considered as an important factor associated with the burnout level [37, 49]. Another frequently reported factor is when the staff does not have enough time to provide adequate care for each patient [53].
Given that the health system of each country has its own characteristics, competencies in the nursing area, training programs, workload, and costs of care, the levels of burnout can be diverse [54, 55]. An intervention for ICU nurses that included education, role-play, and debriefing resulted in a lower prevalence of job strain at 6 months associated with a reduction in both the absenteeism and the turnover when compared with nurses who did not undergo this program [56].
Limitations
Despite using strict inclusion criteria, the reported heterogeneity is important, mainly related to the various methods to define a high level of burnout using the MBI instrument. However, there is the need to reach a consensus to define a high level of burnout using the MBI instrument in ICU healthcare workers to be able to evaluate and to compare preventive strategies. The present study shows that using the three components of the MBI contributes to limit this heterogeneity.
Despite extracting and analysing the rawest available data in each included study, standardising these data using effect size, and then performing meta-regressions and sensitivity analyses to validate the findings, some degree of imprecision is still possible in the pooled effect sizes related to variations in the aggregate data used. Using individual participant data in future research could considerably improve the precision of the effect sizes.
Although our results revealed a certain heterogeneity, it is worth noting that the prevalence of a high level of burnout in healthcare workers was always higher than 14%, thus highlighting the presence of a substantial problem across the globe. Even if the MBI instrument evaluates burnout as a job-related incident, it is not able to individualize symptoms directly related to work stress from nonwork stress, or from a combination of the two. Though burnout is generally considered as related to interindividual relations, a possible increase in the prevalence of burnout among physicians could be due to other causes such as an increasing volume of non–patient-focused work (administrative tasks, electronic files to complete or other activities without direct interactions with patients or staff). Finally, important variables such as staff involvement in the study and whether non-participation occurred randomly or not were not available and could explain part of the heterogeneity.
Both organizational and individual interventions bring value to managing work-related stress, improving well-being at work, and alleviating fatigue and moral distress, thereby allowing to decrease the prevalence of burnout in ICU professionals [57]. High resilience capacities and strong perceived support from the hospital have also been shown to be associated with lower odds of burnout and turnover intention while the presence of burnout increased turnover intention [58]. To promote a policy of reduction of psychosocial risks in the ICU environment, some scientific societies have initiated a call to action to enhance the critical care community’s interest in reducing the prevalence of BOS and promoting a healthy work environment in the ICU [7].
Conclusion
Identifying preventive measures for decreasing the burnout level appears crucial. There is also an urgent need for intervention trials evaluating strategies to improve the well-being at work of ICU caregivers. However, to evaluate and to compare preventive and therapeutic strategies, there is an urgent need to reach a consensus regarding how to define a high-level of burnout in studies related to ICU healthcare workers when using the worldwide used MBI instrument.
Supplementary Information
Below is the link to the electronic supplementary material.
Author's contributions
LP and LB conceived and coordinated the study; SH and LP extracted the data; LP wrote the manuscript. MH and LB critically reviewed the manuscript; LB and AL performed the statistical analyses. All authors revised the manuscript and approved the final version.
Funding
No financial support.
Availability of data and material
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
LP received consultancy fees from Air Liquide MS, Faron and MSD. AL has no conflicts of interest. SH received consultancy fees from Pfizer. MSH has no conflicts of interest LB received consultancy fees from Lundbeck and Janssen.
Ethics approval
Not applicable. All studies have been independently reviewed and approved by the local Institutional Review Board.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3. Palo Alto: Consulting Psychologists Press; 1996. [Google Scholar]
- 2.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 3.Maslach C, Jackson SE. The measurement of experienced burnout. J Occup Behav. 1981;2:99–113. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- 4.Papazian L, Sylvestre A, Herridge M. Should all ICU clinicians regularly be tested for burnout? Yes. Intensive Care Med. 2018;44:681–683. doi: 10.1007/s00134-018-5094-z. [DOI] [PubMed] [Google Scholar]
- 5.Moss M, Good VS, Gozal D, et al. A critical care societies collaborative statement: burnout syndrome in critical care health-care professionals. A call for action. Am J Respir Crit Care Med. 2016;194:106–113. doi: 10.1164/rccm.201604-0708ST. [DOI] [PubMed] [Google Scholar]
- 6.Hodkinson A, Zhou A, Johnson J, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ. 2022;378:e070442. doi: 10.1136/bmj-2022-070442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moss M, Good VS, Gozal D, et al. An official critical care societies collaborative statement-burnout syndrome in critical care health-care professionals: a call for action. Chest. 2016;150:17–26. doi: 10.1016/j.chest.2016.02.649. [DOI] [PubMed] [Google Scholar]
- 8.Hodkinson A, Zhou A, Johnson J, et al. Associations of physician burnout with career engagement and quality of patient care: systematic review and meta-analysis. BMJ. 2022;2:e070442. doi: 10.1136/bmj-2022-070442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320:1131. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.GBD Healthcare Access and Quality Collaborators (2018) Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet. 2016;391:2236–2271. doi: 10.1016/S0140-6736(18)30994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Munn Z, Moola S, Lisy K, et al. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13:147–153. doi: 10.1097/XEB.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 12.IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014;14:25. doi: 10.1186/1471-2288-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins J, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta-analyses. BMJ. 2003 doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins J, Thompson S. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 15.Thiese MS, Ronna B, Ott U. P value interpretations and considerations. J Thorac Dis. 2016;8:928–931. doi: 10.21037/jtd.2016.08.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patsopoulos NA, Evangelou E, Ioannidis JPA. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37:1148–1157. doi: 10.1093/ije/dyn065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glasgow MJ, Edlin R, Harding JE. Comparison of risk-of-bias assessment approaches for selection of studies reporting prevalence for economic analyses. BMJ Open. 2020;10:e037324. doi: 10.1136/bmjopen-2020-037324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54:1046–1055. doi: 10.1016/s0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 19.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwarzer G. Meta: an R package for meta-analysis. R News. 2007;7:40–45. [Google Scholar]
- 21.Awajeh AM, Issa MR, Rasheed AM, Amirah MF. Burnout among critical care nurses in king Saud medical city (KSMC) J Nurs Care. 2018;450:2. [Google Scholar]
- 22.Bruyneel A, Smith P, Tack J, Pirson M. Prevalence of burnout risk and factors associated with burnout risk among ICU nurses during the COVID-19 outbreak in French speaking Belgium. Intensive Crit Care Nurs. 2021;65:103059. doi: 10.1016/j.iccn.2021.103059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Azoulay E, Pochard F, Reignier J, et al. Symptoms of mental health disorders in critical care physicians facing the second COVID-19 wave: a cross-sectional study. Chest. 2021;160:944–955. doi: 10.1016/j.chest.2021.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Azoulay E, De Waele J, Ferrer R, et al. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care. 2020;10:110. doi: 10.1186/s13613-020-00722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rosa RG, Falavigna M, da Silva DB, et al. Effect of flexible family visitation on delirium among patients in the intensive care unit: the ICU visits randomized clinical trial. JAMA. 2019;322:216–228. doi: 10.1001/jama.2019.8766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yıldız E. Psychopathological factors associated with burnout in intensive care nurses: a cross-sectional study. J Am Psychiatr Nurses Assoc. 2021 doi: 10.1177/1078390321999725. [DOI] [PubMed] [Google Scholar]
- 27.Butera S, Brasseur N, Filion N, et al. Prevalence and associated factors of burnout risk among intensive care and emergency nurses before and during the coronavirus disease 2019 pandemic: a cross-sectional study in Belgium. J Emerg Nurs. 2021;47:879–891. doi: 10.1016/j.jen.2021.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moll V, Meissen H, Pappas S, et al. The coronavirus disease 2019 pandemic impacts burnout syndrome differently among multiprofessional critical care clinicians—a longitudinal survey study. Crit Care Med. 2022;50:440–448. doi: 10.1097/CCM.0000000000005265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kok N, van Gurp J, Teerenstra S, et al. Coronavirus disease 2019 immediately increases burnout symptoms in ICU professionals: a longitudinal cohort study. Crit Care Med. 2021;49:419–427. doi: 10.1097/CCM.0000000000004865. [DOI] [PubMed] [Google Scholar]
- 30.Omar AS, Labib A, Hanoura SE, et al. Impact of extracorporeal membrane oxygenation service on burnout development in eight intensive care units. A national cross-sectional study. J Cardiothorac Vasc Anesth. 2022;36:2891–2899. doi: 10.1053/j.jvca.2022.02.018. [DOI] [PubMed] [Google Scholar]
- 31.Hu Z, Wang H, Xie J, et al. Burnout in ICU doctors and nurses in mainland China—a national cross-sectional study. J Crit Care. 2021;62:265–270. doi: 10.1016/j.jcrc.2020.12.029. [DOI] [PubMed] [Google Scholar]
- 32.Wang J, Hu B, Peng Z, et al. Prevalence of burnout among intensivists in mainland China: a nationwide cross-sectional survey. Crit Care. 2021;25:8. doi: 10.1186/s13054-020-03439-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Voultsos P, Koungali M, Psaroulis K, Boutou AK. Burnout syndrome and its association with anxiety and fear of medical errors among intensive care unit physicians: a cross-sectional study. Anaesth Intensive Care. 2020;48:134–142. doi: 10.1177/0310057X20902780. [DOI] [PubMed] [Google Scholar]
- 34.Vincent L, Brindley PG, Highfield J, et al. Burnout syndrome in UK intensive care unit staff: data from all three burnout syndrome domains and across professional groups, genders and ages. J Intensive Care Soc. 2019;20:363–369. doi: 10.1177/1751143719860391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.See KC, Zhao MY, Nakataki E, et al. Professional burnout among physicians and nurses in Asian intensive care units: a multinational survey. Intensive Care Med. 2018;44:2079–2090. doi: 10.1007/s00134-018-5432-1. [DOI] [PubMed] [Google Scholar]
- 36.Garrouste-Orgeas M, Perrin M, Soufir L, et al. The Iatroref study: medical errors are associated with symptoms of depression in ICU staff but not burnout or safety culture. Intensive Care Med. 2015;41:273–284. doi: 10.1007/s00134-014-3601-4. [DOI] [PubMed] [Google Scholar]
- 37.Embriaco N, Azoulay E, Barrau K, et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007;175:686–692. doi: 10.1164/rccm.200608-1184OC. [DOI] [PubMed] [Google Scholar]
- 38.Burghi G, Lambert J, Chaize M, et al. Prevalence, risk factors and consequences of severe burnout syndrome in ICU. Intensive Care Med. 2014;40:1785–1786. doi: 10.1007/s00134-014-3454-x. [DOI] [PubMed] [Google Scholar]
- 39.Merlani P, Verdon M, Businger A, et al. Burnout in ICU caregivers: a multicenter study of factors associated to centers. Am J Respir Crit Care Med. 2011;184:1140–1146. doi: 10.1164/rccm.201101-0068OC. [DOI] [PubMed] [Google Scholar]
- 40.Teixeira C, Ribeiro O, Fonseca AM, Carvalho AS. Burnout in intensive care units—a consideration of the possible prevalence and frequency of new risk factors: a descriptive correlational multicentre study. BMC Anesthesiol. 2013;13:38. doi: 10.1186/1471-2253-13-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Teixeira C, Ribeiro O, Fonseca AM, Carvalho AS. Ethical decision making in intensive care units: a burnout risk factor? Results from a multicentre study conducted with physicians and nurses. J Med Ethics. 2014;40:97–103. doi: 10.1136/medethics-2012-100619. [DOI] [PubMed] [Google Scholar]
- 42.Zhang XC, Huang DS, Guan P, SUBLIN Study Team Job burnout among critical care nurses from 14 adult intensive care units in Northeastern China: a cross-sectional survey. BMJ Open. 2014;4:e004813. doi: 10.1136/bmjopen-2014-004813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Karanikola MNK, Papathanassoglou EDE, Mpouzika M, Lemonidou C. Burnout syndrome indices in Greek intensive care nursing personnel. Dimens Crit Care Nurs. 2012;31:94–101. doi: 10.1097/DCC.0b013e3182445fd2. [DOI] [PubMed] [Google Scholar]
- 44.Giannini A, Miccinesi G, Prandi E, et al. Partial liberalization of visiting policies and ICU staff: a before-and-after study. Intensive Care Med. 2013;39:2180–2187. doi: 10.1007/s00134-013-3087-5. [DOI] [PubMed] [Google Scholar]
- 45.FradeMera MJ, Vinagre Gaspar R, Zaragoza García I, et al. Burnout syndrome in different intensive care units. Enferm Intensiva. 2009;20:131–140. doi: 10.1016/s1130-2399(09)73221-3. [DOI] [PubMed] [Google Scholar]
- 46.Yildiz Y, Oztas DM, Ulukan MO, et al. Application of hybrid extracorporeal membrane oxygenation for the treatment of subsequent shock following acute respiratory distress syndrome developing after firearm injury. Case Rep Med. 2019;2019:3120912. doi: 10.1155/2019/3120912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chuang C-H, Tseng P-C, Lin C-Y, et al. Burnout in the intensive care unit professionals: a systematic review. Medicine. 2016;95:e5629. doi: 10.1097/MD.0000000000005629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ramírez-Elvira S, Romero-Béjar JL, Suleiman-Martos N, et al. Prevalence, risk factors and burnout levels in intensive care unit nurses: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18:11432. doi: 10.3390/ijerph182111432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Poncet MC, Toullic P, Papazian L, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175:698–704. doi: 10.1164/rccm.200606-806OC. [DOI] [PubMed] [Google Scholar]
- 50.Koinis A, Giannou V, Drantaki V, et al. The impact of healthcare workers job environment on their mental-emotional health. Coping strategies: the case of a local general hospital. Health Psychol Res. 2015;3:1984. doi: 10.4081/hpr.2015.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Embriaco N, Hraiech S, Azoulay E, et al. Symptoms of depression in ICU physicians. Ann Intensive Care. 2012;2:34. doi: 10.1186/2110-5820-2-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Embriaco N, Papazian L, Kentish-Barnes N, et al. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care. 2007;13:482–488. doi: 10.1097/MCC.0b013e3282efd28a. [DOI] [PubMed] [Google Scholar]
- 53.Moss M, Good VS, Gozal D, et al. An official critical care societies collaborative statement: burnout syndrome in critical care healthcare professionals: a call for action. Crit Care Med. 2016;44:1414–1421. doi: 10.1097/CCM.0000000000001885. [DOI] [PubMed] [Google Scholar]
- 54.Hämmig O. Explaining burnout and the intention to leave the profession among health professionals—a cross-sectional study in a hospital setting in Switzerland. BMC Health Serv Res. 2018;18:785. doi: 10.1186/s12913-018-3556-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Moloney W, Boxall P, Parsons M, Cheung G. Factors predicting registered nurses’ intentions to leave their organization and profession: a job demands-resources framework. J Adv Nurs. 2018;74:864–875. doi: 10.1111/jan.13497. [DOI] [PubMed] [Google Scholar]
- 56.El Khamali R, Mouaci A, Valera S, et al. Effects of a multimodal program including simulation on job strain among nurses working in intensive care units: a randomized clinical trial. JAMA. 2018;320:1988–1997. doi: 10.1001/jama.2018.14284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kleinpell R, Moss M, Good VS, et al. The critical nature of addressing burnout prevention: results from the critical care societies collaborative’s national summit and survey on prevention and management of burnout in the ICU. Crit Care Med. 2020;48:249–253. doi: 10.1097/CCM.0000000000003964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kuriyama A, Sakuraya M, Kinjo M, et al. Burnout and turnover intention in critical care professionals during the COVID-19 pandemic in Japan: a cross-sectional survey. Ann Am Thorac Soc. 2022 doi: 10.1513/AnnalsATS.202201-029OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.