Abstract
Little work has focused on the underlying mechanisms that may link financial strain and smoking processes. The current study tested the hypothesis that financial strain would exert an indirect effect on cognitive-based smoking processes via depressive symptoms. Three clinically significant dependent variables linked to the maintenance of smoking were evaluated: negative affect reduction motives, negative mood abstinence expectancies, and perceived barriers for quitting. Participants included 102 adult daily smokers (Mage = 33.0 years, SD = 13.60; 35.3% female) recruited from the community to participate in a self-guided (unaided; no psychological or pharmacological intervention) smoking cessation study. Results indicated that depressive symptoms explain, in part, the relation between financial strain and smoking motives for negative affect reduction, negative mood abstinence expectancies, and perceived barriers for quitting. Results indicate that smoking interventions for individuals with high levels of financial strain may potentially benefit from the addition of therapeutic tactics aimed at reducing depression.
Keywords: Financial strain, Depression, Smoking cessation, Treatment, Social determinants of health
Financial strain, reflecting an unfavorable asset-to-needs ratio, affects individuals of any SES strata who experience debt that exceeds their economic capacities and impacts their ability to afford basic necessities, such as food, clothing, housing, major household items, and other bills (Siahpush, Borland, & Scollo, 2003). Financial strain has also been found to be related to increased risk of smoking (Falba, Teng, Sindelar, & Gallo, 2005; Murayama et al., 2013; Nelson, Lust, Story, & Ehlinger, 2008; Shaw, Agahi, & Krause, 2011). Research has found that financial strain is associated with a higher probability of being a current smoker, greater smoking rate, and lower success in quitting (Kendzor et al., 2010; Reitzel, Langdon, Nguyen, & Zvolensky, 2015; Siahpush & Carlin, 2006). Smokers with more financial strain are more likely to report greater interest in quitting, but are less likely to attempt to quit (Siahpush, Yong, Borland, Reid, & Hammond, 2009).
There is a large empirical literature linking depressive symptoms and disorders to the onset and maintenance of smoking (Hitsman et al., 2013). Negative reinforcement expectancies have been found to be associated with higher levels of negative affect/emotional vulnerability in smokers (Copeland, Brandon, & Quinn, 1995). Additionally, studies have found financial strain is related to greater psychological distress, including depressive symptoms (Chou & Chi, 2000; Dijkstra-Kersten, Biesheuvel-Leliefeld, Wouden, Penninx, & Marwijk, 2015; Price, VanRyn, & Vinokur, 1992). However, depressive symptoms have not been directly explored in relation to financial strain and smoking processes. Theoretically, smokers with greater financial strain may be more apt to experience depressed mood, which, in turn, may be related to a corresponding tendency to engage in negative reinforcement smoking behavior to manage such aversive states, increased expectations of experiencing negative mood states during periods of brief (24-hour) smoking abstinence, and greater perceptions of difficulties in quitting.
The current study tested the hypothesis that financial strain would exert an indirect effect on cognitive-based smoking processes via depressive symptoms. Specifically, financial strain was expected to positively relate with depressive symptoms, which in turn, would be associated with negative affect reduction motives, negative mood abstinence expectancies, and perceived barriers for quitting (Brandon, 1994; Copeland & Brandon, 2000; Zvolensky et al., 2007).
1. Method
1.1. Participants
Participants included 102 adult daily smokers (Mage = 33.0 years, SD = 13.60; 35.3% female) recruited from communities in Burlington, Vermont and Houston, Texas. Inclusion criteria for the current study were: (1) being between 18- and 65 years of age; (2) being interested in making a serious, unaided, quit attempt; and (3) smoking a minimum of 5 cigarettes per day. Exclusion criteria were: (1) pregnancy or the possibility of being pregnant (by self-report); (2) current use of nicotine replacement therapy and/or smoking cessation counseling; (3) current or past history of psychotic-spectrum symptoms or disorders; or (4) current suicidality. The racial/ethnic distribution of this sample was as follows: 85.3% White/Caucasian; 7.8% Black/Non-Hispanic; 2.9% Hispanic; 1.0% Asian; 1.0% American Indian/Alaska Native; 2.9% Multi-racial; and 2.0% ‘Others’. On average, participants reported smoking 15.6 cigarettes per day (SD = 6.76), smoking their first cigarette at 17.4 years of age (SD = 3.43), and reported being a daily smoker for an average of 14.9 years (SD = 12.93).
1.2. Measures
Demographics Questionnaire.
Demographic data included gender (0 = male, 1 = female), age, race (0 = race other than White; 1 = White), and education (1 = grade 6 or less to 8 = completed graduate or professional school). Collected demographic information was used to describe the sample and gender, age, race and education were included as covariates.
Structured Clinical Interview-Non-Patient Version for DSM-IV (SCID-N/ P; First, Spitzer, Gibbon, & Williams, 2007).
Axis I psychopathology assessments were performed using the SCID-N/P.
Financial Strain Questionnaire (FSQ; Pearlin, Lieberman, Menaghan, & Mullan, 1981).
The FSQ consists of 8 items adapted from an economic strain measure that assesses current perceived financial difficulty in terms of the ability to afford food, clothing, housing, major items (e.g., car), furniture/household equipment, leisure activities, and bills according to a 3-point Likert scale (Pearlin et al., 1981).
Inventory of Depression and Anxiety Symptoms (IDAS; Watson et al., 2007) Depression Subscale.
The IDAS is a 64-item self-report instrument that assesses distinct affect symptom dimensions. The IDAS depression symptom subscale (IDAS-DEP; 20 items) was utilized (Cronbach’s α = 0.91).
Wisconsin Inventory of Smoking Dependence Motives (WISDM; Piper et al., 2004) Negative Affect Subscale.
The WISDM comprises 68 items designed to assess 13 different theoretically-derived motivational domains on a 7-point Likert scale ranging from 1 (“Not true of me at all”) to 7 (“Extremely true of me”). We elected to focus our hypothesis only on the WISDM negative affect subscale (WISDM-NA; 6 items).
Smoking Abstinence Expectancies Questionnaire (SAEQ; Abrams, Zvolensky, Dorman, Gonzalez, & Mayer, 2011).
The SAEQ has good psychometric properties, including internal consistency, convergent and discriminant validity, and test–retest reliability (Abrams et al., 2011).
Barriers to Cessation Scale (BCS; Macnee & Talsma, 1995).
The BCS is a 19-item self-report measure of perceived barriers associated with quitting smoking. The BCS total score was utilized.
Smoking History Questionnaire (SHQ; Brown, Lejuez, Kahler, & Strong, 2002; Garey et al., in press).
The SHQ is a self-report questionnaire used to assess smoking history (e.g. smoking rate, age of onset of initiation), pattern (e.g. number of cigarettes consumed per day), and strategies used to quit, and problematic symptoms experienced during past quit attempts (e.g., weight gain, nausea, irritability, and anxiety).
Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988).
The PANAS is a self-report measure that assesses the extent to which participants experienced 20 different feelings and emotions on a scale ranging from 1 (“Very slightly or not at all”) to 5 (“Extremely”). The PANAS negative affect subscale (PANAS-NA; 10 items) was used.
1.3. Procedure
Adult daily smokers were recruited from the community through flyers, newspaper ads, and radio announcements to participate in a self-guided quit study examining barriers to successful smoking cessation (Langdon, Farris, Hogan, Grover, & Zvolensky, 2016; Langdon, Farris, Øverup, & Zvolensky, 2015). Interested participants were scheduled for an in-person baseline assessment to determine study eligibility. Following written informed consent, participants were interviewed using the SCID-I/NP and completed a computerized self-report battery of questionnaires. Participants were compensated $20 for participating in the baseline assessment, regardless of study eligibility. The current study is based on baseline (pre-cessation data) for a sub-set of the sample, which was selected on the basis of available data on all studied variables. The study protocol was approved by the University of Houston Institutional Review Board.
1.4. Analytic strategy
Regression analyses were conducted using bootstrapping techniques through PROCESS, a conditional modeling program that utilizes an ordinary least squares-based path analytical framework to test for both direct and indirect effects (Hayes, 2013). Bootstrapping is the recommended approach when data distribution is non-normal or unknown (Kelley, 2005; Kirby & Gerlanc, 2013). An indirect effect is the product of path a and path b and is assumed to be significant if the confidence intervals (CIs) around their product do not include zero (Preacher & Hayes, 2008; Zhao, Lynch, & Chen, 2010). Kappa-squared (κ2) was used as an indicator of effect size (Preacher & Kelley, 2011). Three models were conducted with (1) smoking motives for negative affect reduction, (2) negative mood abstinence expectancies, and (3) perceived barriers for quitting as criterion variables.
2. Results
2.1. Descriptive analyses
Zero-order correlations among all study variables are presented in Table 1. Financial strain and depressive symptoms were positively correlated (r = 0.35; 12% shared variance). Depressive symptoms were positively related to all criterion measures (r’s = 0.34–0.37). Financial strain was uncorrelated to all criterion measures (all p’s > 0.05).
Table 1.
Descriptive statistics and bivariate correlations between study variables (n = 102).
| Variable | Mean/n (SD/%) | Observed range | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| 1. Gendera | 36 (35.3) | – | 1 | ||||||||||
| 2. Agea | 32.96 (13.60) | (18–65) | 0.03 | 1 | |||||||||
| 3. Racea | 87 (85.3) | – | −0.16 | −0.11 | 1 | ||||||||
| 4. Educationa | 4.39 (1.34) | (2–8) | −0.14 | 0.23* | 0.04 | 1 | |||||||
| 5. PANAS-NAa | 19.94 (7.03) | (10–46) | 0.17 | −0.14 | −0.02 | 0.08 | 1 | ||||||
| 6. CPDa | 15.62 (6.76) | (5–40) | 0.03 | 0.26** | −0.09 | 0.01 | −0.02 | 1 | |||||
| 7. FSQb | 17.14 (4.48) | (8–24) | −0.20* | −0.06 | −0.07 | −0.09 | 0.26** | 0.09 | 1 | ||||
| 8. IDAS-DEPc | 41.22 (12.51) | (21–76) | 0.11 | −0.14 | −0.11 | −0.03 | 0.63*** | 0.01 | 0.35*** | 1 | |||
| 9. WISDM-NAd | 4.56 (1.33) | (1.33–7) | 0.21* | −0.14 | 0.10 | −0.01 | 0.35*** | 0.17 | 0.13 | 0.37*** | 1 | ||
| 10. SAEQ-NMd | 24.60 (10.17) | (0–42) | 0.27** | 0.03 | 0.10 | 0.25* | 0.31** | 0.17 | −0.001 | 0.34** | 0.51*** | 1 | |
| 11. BCSd | 26.62 (10.48) | (3–53) | 0.26** | 0.08 | −0.12 | −0.03 | 0.37*** | 0.13 | 0.07 | 0.37*** | 0.36*** | 0.35*** | 1 |
Note. N = 102; gender: % listed as females (coded: 0 = male and 1 = female); race: % listed as White (coded: 0 = other than White and 1 = White); PANAS-NA = Positive and Negative Affect Schedule-Negative Affect Subscale; CPD = cigarettes per day; FSQ = Financial Strain Questionnaire; IDAS-DEP = Inventory of Depression and Anxiety-Depression Subscale; WISDM-NA = Wisconsin Inventory of Smoking Dependence Motives-Negative Affect Subscale; SAEQ-NM = Smoking Abstinence Expectancies Questionnaire-Negative Mood Subscale; BCS = Barriers to Cessation Scale.
p < 0.05.
p < 0.01.
p < 0.001.
Covariate.
Predictor.
Indirect explanatory variable.
Criterion.
2.2. Indirect effect analyses
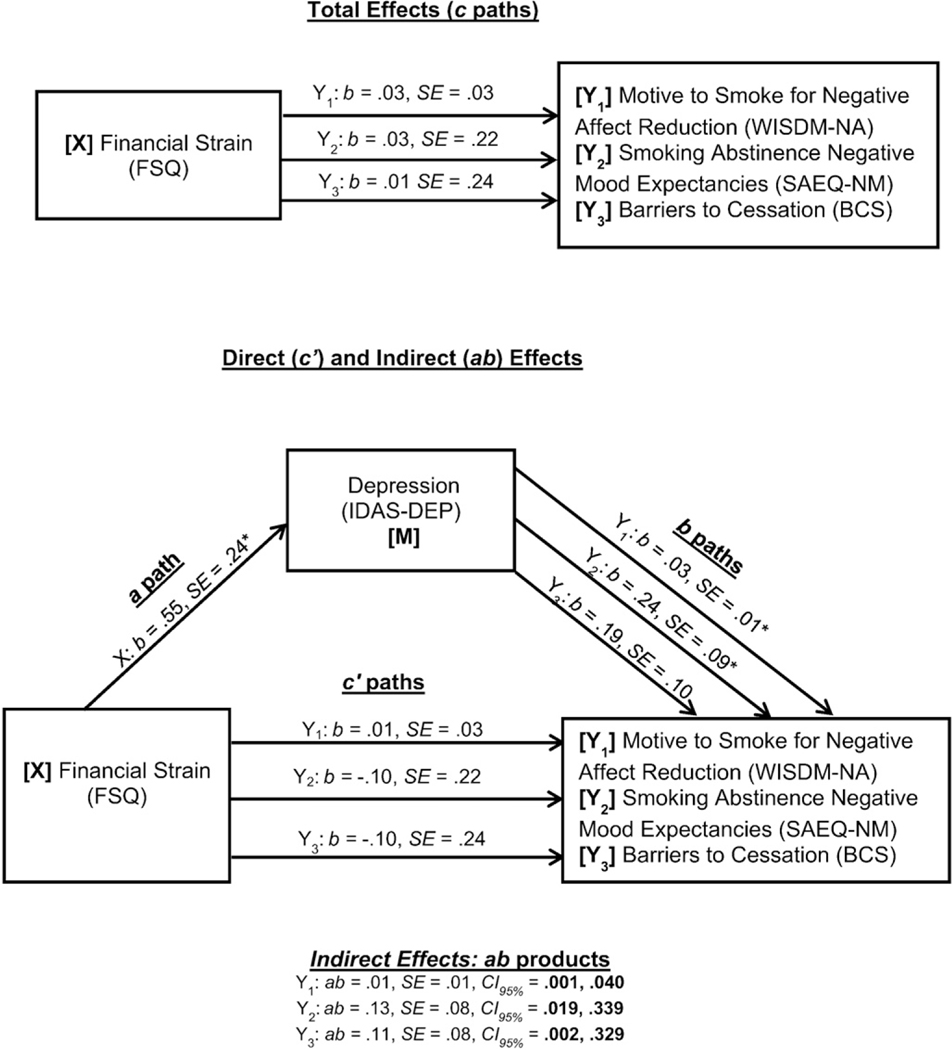
Regression results for paths a, b, c, and c′ are presented in Fig. 1. For smoking motives for negative affect reduction, the total effect model accounted for significant variance (R2 = 0.22, F[7, 94] = 3.77, p = 0.001). The direct effect model that included depressive symptoms accounted for greater variance in smoking motives for negative affect reduction (R2 = 0.25, F[8, 93] = 3.92, p = 0.001). The independent indirect effect of financial strain on smoking motives for negative affect reduction through depressive symptoms was significant (ab = 0.01, SE = 0.009, CI95% = 0.001, 0.040). Specifically, greater financial strain was significantly associated with increased depressive symptoms, which was subsequently associated with greater expectancy that smoking will alleviate negative affect. The effect size for this pathway was in the small to medium range (κ2 = 0.05).
Fig. 1.
Conceptual model of the indirect effect (ab) of financial strain on smoking motives for negative affect reduction, and negative mood abstinence expectancies, and perceived barriers to quitting through depressive symptoms. Note: N = 102; *p < 0.05. a path = Effect of X on M; b paths = Effect of M on Yi; c paths = Total effect of X on Yi; c′ paths = Direct effect of X on Yi controlling for M. Three separate paths were conducted (Y1–3) with the predictor (X). Covariates included gender, age, race, education, negative affectivity (PANAS-NA), and cigarettes smoked per day (SHQ).
Specific to negative mood abstinence expectancies, the total effect model accounted for significant variance (R2 = 0.27, F[7, 94] = 4.96, p < 0.001). The direct effect model that included depressive symptoms accounted for greater variance in negative mood abstinence expectancies (R2 = 0.32, F[8, 93] = 5.46, p < 0.001). The independent indirect effect of financial strain on negative mood abstinence expectancies through depressive symptoms was significant (ab = 0.13, SE = 0.08, CI95% = 0.019, 0.339). Specifically, greater financial strain was significantly associated with increased depressive symptoms, which was subsequently associated with greater negative mood abstinence expectancies. The effect size for this pathway was in the small to medium range (κ2 = 0.06).
Regarding perceived barriers to cessation, the total effect model accounted for significant variance (R2 = 0.21, F[7, 94] = 3.50, p = 0.002). The direct effect model that included depressive symptoms accounted for greater variance in perceived barriers to cessation (R2 = 0.24, F[8, 93] = 3.60, p < 0.001). The independent indirect effect of financial strain on perceived barriers to cessation through depressive symptoms was significant (ab = 0.11, SE = 0.08, CI95% = 0.002, 0.329). Specifically, greater financial strain was significantly associated with increased depressive symptoms, which was subsequently associated with more perceived barriers to cessation. The effect size for this pathway was in the small to medium range (κ2 = 0.05).
2.3. Specificity analyses
To further strengthen interpretation of results, financial strain and depressive symptoms variables were reversed for each of the three models tested (Preacher & Hayes, 2004); specifically, depressive symptoms was the predictor, financial strain was the explanatory variable, and all were criterion variables remained the same. Tests of the indirect effects in these models were estimated based on 10,000 bootstrap resamples. All results of the reversed models were non-significant (smoking motives for negative affect reduction: ab = 0.001, SE = 0.004, CI95% = −0.006, 0.012; negative mood abstinence expectancies: ab = −0.01, SE = 0.03, CI95% = −0.076, 0.033; and perceived barriers for quitting: ab = −0.01, SE = 0.03, CI95% = −0.080, 0.035).
3. Discussion
Consistent with expectation, depressive symptoms played an explanatory role in the relation between financial strain and smoking motives for negative affect reduction, negative mood abstinence expectancies, and perceived barriers for quitting. Importantly, effect sizes were examined in the form of kappa-squared, which were utilized to indicate the effect size of the indirect effects of financial strain via depression on the studied dependent variables. Results indicated that effect sizes on the dependent variables were in the small to medium range (0.05–0.06). Notably, the indirect effects were evident over and above sociodemographic factors (gender, age, race, and education), depressive states on (negative affectivity), and smoking dependence (number of cigarettes per day). Such results are broadly consistent with past work indicating that both financial strain (Reitzel et al., 2015) and depressive symptoms (Dijkstra-Kersten et al., 2015) are related to the maintenance of smoking and uniquely extends this work to indicate that depressive symptoms may serve as a mechanistic construct in these relations. Additionally, the alternative models tested, showed no significant indirect effects, suggesting that the effect was specific to depression, and that financial strain is associated with depressed mood, which in turn, is related to cognitive-based smoking processes.
The present data suggest that the experience of financial strain may be related to cognitive-based smoking maintenance processes by virtue of heightened depressive symptoms. The present findings have implications for improving intervention programming for smoking cessation that involves social determinants of health processes, such as financial strain. For example, clinically, the results indicate that smoking interventions for those with high levels of financial strain may potentially benefit from the addition of therapeutic tactics aimed at reducing depressive symptoms (e.g., behavioral activation; mindfulness- and acceptance-based approaches). Prospective studies are needed to examine the effects of financial strain, depressive symptoms and smoking maintenance processes over time to more comprehensively assess the directionality of these observed relations.
There are several interpretive caveats to the present study. First, the cross-sectional nature of these data precludes causal attributions. The present tests were based on a theoretical framework supported by extant empirical data, but did not allow for testing of temporal sequencing. Future prospective studies are necessary to determine the directional effects of these relations. Second, our sample consisted of community-recruited daily cigarette smokers with moderate levels of nicotine dependence. Additionally, participants in the present study were also treatment-seeking smokers, which may contribute to biased findings. Future studies may benefit by sampling from lighter and heavier smoking populations, as well as non-treatment seeking smokers, to ensure the generalizability of the results to the general smoking population. Third, as the key variables were assessed via self-report, there is the possibility that the observed relations were, in part, a function of shared method variance. Future research may benefit from employing a multi-method assessment approach to cross-index the nature of the relations observed in the current report. Fourth, the present study did not collect information on nicotine dependence levels. Future studies may benefit from collecting these data to examine whether effects are consistent at different levels of smoking dependence. Fifth, the present study did not collect participant income data. Although, as in past work, education was used as an indicator of social economic status (Reitzel et al., 2015), future studies may benefit from additionally adjusting for income. Lastly, although bootstrapped confidence intervals were estimated around the mediation coefficient, this robust technique was not employed when estimating other parameters. Thus, future work could benefit from utilizing sophisticated precision techniques, such as bootstrapping, to increase the confidence in observed effects.
HIGHLIGHTS.
It is posited that financial strain will exert an indirect effect on cognitive-based smoking processes via depressive signs
Depressive symptoms explained link between financial strain and negative affect reduction smoking motives
Depressive symptoms explained link between financial strain and negative mood abstinence expectancies
Depressive symptoms explained link between financial strain and perceived barriers for quitting
Results have implications for improving intervention programs for smoking cessation involving financial strain
Role of funding sources
This work was supported by a National Institutes of Health grant awarded to Dr. Kirsten J. Langdon (1F31DA026634-01).
Footnotes
Conflicts of interest
None of the authors have any conflicts of interest to report.
References
- Abrams K, Zvolensky MJ, Dorman L, Gonzalez A, & Mayer M. (2011). Development and validation of the smoking abstinence expectancies questionnaire. Nicotine & Tobacco Research, 12(12), 1296–1304. [DOI] [PubMed] [Google Scholar]
- Brandon TH (1994). Negative affect as motivation to smoke. Current Directions in Psychological Science, 3(2), 33–37. [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, & Strong DR (2002). Distress tolerance and duration of past smoking cessation attempts. Journal of Abnormal Psychology, 111(1), 180. [PubMed] [Google Scholar]
- Chou KL, & Chi I. (2000). Stressful events and depressive symptoms among old women and men: A longitudinal study. International Journal of Aging and Human Development, 51(4), 275–293. [DOI] [PubMed] [Google Scholar]
- Copeland AL, & Brandon TH (2000). Testing the causal role of expectancies in smoking motivation and behavior. Addictive Behaviors, 25(3), 445–449. [DOI] [PubMed] [Google Scholar]
- Copeland A, Brandon T, & Quinn E. (1995). The Smoking Consequences Questionnaire-Adult: Measurement of smoking outcome expectancies of experienced smokers. Psychological Assessment, 7, 484–494. 10.1037/1040-3590.7.4.484. [DOI] [Google Scholar]
- Dijkstra-Kersten S, Biesheuvel-Leliefeld K, Wouden J, Penninx B, & Marwijk H. (2015). Associations of financial strain and income with depressive and anxiety disorders. Journal of Epidemiology and Community Health. [DOI] [PubMed] [Google Scholar]
- Falba T, Teng HM, Sindelar JL, & Gallo WT (2005). The effect of involuntary job loss on smoking intensity and relapse. Addiction, 100(9), 1330–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JB (2007). Structured clinical interview for DSM-IV-TR Axis I disorders, research version, non-patient edition (SCIDI/NP). New York, NY: Biometrics Research, New York State Psychiatric Institute. [Google Scholar]
- Garey L, Jardin C, Kauffman BY, Sharp C, Neighbors C, Schmidt NB, & Zvolensky MJ (2016). (in press). Psychometric evaluation of the barriers to cessation scale. Psychological Assessment. 10.1037/pas0000379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Methodology in the social sciences. New York, NY: The Guilford Press. [Google Scholar]
- Hitsman B, Papandonatos G, McChargue D, DeMott A, Herrera M, Spring B, ... Niaura R. (2013). Past major depression and smoking cessation outcome: A systematic review and meta-analysis update. Addiction, 108(2), 294–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley K. (2005). The effects of nonnormal distributions on confidence intervals around the standardized mean difference: Bootstrap and parametric confidence intervals. Educational and Psychological Measurement, 65(1), 51–69. [Google Scholar]
- Kendzor D, Businelle M, Costello T, Castro Y, Reitzel L, Cofta-Woerpel L, ... Wetter D. (2010). Financial strain and smoking cessation among racially/ethnically diverse smokers. American Journal of Public Health, 100(4), 702–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KN, & Gerlanc D. (2013). BootES: An R package for bootstrap confidence intervals on effect sizes. Behavior Research Methods, 45(4), 905–927. [DOI] [PubMed] [Google Scholar]
- Langdon KJ, Farris SG, Hogan JB, Grover KW, & Zvolensky MJ (2016). Anxiety sensitivity in relation to quit day dropout among adult daily smokers recruited to participate in a self-guided cessation attempt. Addictive Behaviors, 58, 12–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langdon KJKJ, Farris SGSG, Øverup CSCS, & Zvolensky MJMJ (2015). ssociations between anxiety sensitivity, negative affect, and smoking during a self-guided smoking cessation attempt. Nicotine & Tobacco Research, 18(5), 1188–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macnee CL, & Talsma A. (1995). Development and testing of the barriers to cessation scale. Nursing Research, 44(4), 214–219. [PubMed] [Google Scholar]
- Murayama H, Bennett JM, Shaw BA, Liang J, Krause N, Kobayashi E, & Shinkai S. (2013). Does Social Support Buffer the Effect of Financial Strain on the Trajectory of Smoking in Older Japanese? A 19-Year Longitudinal Study. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 70(3), 367–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson MC, Lust K, Story M, & Ehlinger E. (2008). Credit card debt, stress and key health risk behaviors among college students. American Journal of Health Promotion, 22, 400–407. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, & Mullan JT (1981). The stress process. Journal of Health and Social Behavior, 22, 337–356. [PubMed] [Google Scholar]
- Piper ME, Piasecki TM, Federman EB, Bolt DM, Smith SS, Fiore MC, & Baker TB (2004). A multiple motives approach to tobacco dependence: The Wisconsin inventory of smoking dependence motives (WISDM-68). Journal of Consulting and Clinical Psychology, 72(2), 139–154. 10.1037/0022-006X.72.2.139. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36(4), 717–731. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Kelley K. (2011). Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods, 16(2), 93. [DOI] [PubMed] [Google Scholar]
- Price RH, VanRyn M, & Vinokur AD (1992). Impact of a preventive job search intervention on the likelihood of depression among the unemployed. Journal of Health and Social Behavior, 33, 158–167. [PubMed] [Google Scholar]
- Reitzel LR, Langdon KJ, Nguyen NT, & Zvolensky MJ (2015). Financial strain and smoking cessation among men and women within a self-guided quit attempt. Addictive Behaviors, 47, 66–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw B, Agahi N, & Krause N. (2011). Are changes in financial strain associated with changes in alcohol use and smoking among older adults? Journal of Studies on Alcohol and Drugs, 72(6), 917–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siahpush M, & Carlin JB (2006). Financial stress, smoking cessation and relapse: Results from a prospective study of an Australian national sample. Addiction, 101(1), 121–127. [DOI] [PubMed] [Google Scholar]
- Siahpush M, Borland R, & Scollo M. (2003). Smoking and financial stress. Tobacco Control, 12, 60–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siahpush M, Yong H, Borland R, Reid J, & Hammond D. (2009). Smokers with financial stress are more likely to want to quit but less likely to try or succeed: Findings from the International Tobacco Control (ITC) Four Country Survey. Addiction, 104(8), 1382–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A. (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Kotov R, Simms LJ, Chmielewski M, McDade-Montez EA, ... Stuart S. (2007). Development and validation of the inventory of depression and anxiety symptoms (IDAS). Psychological Assessment, 19(3), 253–268. [DOI] [PubMed] [Google Scholar]
- Zhao X, Lynch JG, & Chen Q. (2010). Reconsidering Baron and Kenny: Myths and truths about mediation analysis. Journal of Consumer Research, 37(2), 197–206. [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Miller MO, Bernstein A, Yartz AR, Gregor KL, ... Gibson, L. E. (2007). Incremental validity of anxiety sensitivity in terms of motivation to quit, reasons for quitting, and barriers to quitting among community-recruited daily smokers. Nicotine & Tobacco Research, 9(9), 965–975. [DOI] [PubMed] [Google Scholar]