Abstract
Patient: Male, 9-year-old
Final Diagnosis: Epidermoid cyst
Symptoms: Perianal lesions • perianal pain
Clinical Procedure: —
Specialty: Pediatrics and Neonatology • Surgery
Objective:
Rare disease
Background:
Lowe syndrome, also known as oculocerebrorenal syndrome, is a rare genetic condition caused by an X-linked mutation of the OCRL1 gene, with an estimated prevalence in the general population of approximately 1 in 500 000. It is a multisystem disorder most commonly affecting the eyes, central nervous system, and kidneys. These commonly manifest as congenital cataracts, intellectual disability, and proximal renal dysfunction (Fanconi-type). Epidermal lesions are an uncommon manifestation of this condition, and the association is not completely understood.
Case Report:
Here we present a case of a 9-year-old boy with Lowe syndrome who presented with multiple cystic masses found in the perianal region. An excision was then performed to remove the masses and found that the lesions were epidermal cysts, which are infrequently found in Lowe syndrome. After excision, the patient recovered uneventfully without complications.
Conclusions:
While epidermal cysts are an uncommon manifestation that have been documented, our case remains unique given the location and associated symptoms of the lesions. At presentation, the constellation of pain and peri-anal masses was concerning for a malignant etiology. However, after diagnostic imaging was performed, these lesions were found to be epidermal cysts, an infrequent manifestation of Lowe syndrome. Few previous case reports described cystic lesions in association with Lowe syndrome, and none, to our knowledge, have described multiple symptomatic perianal lesions. This case is important to consider because epidermal cystic lesions can be found with this presentation and should be considered on differential diagnoses for dermatologic findings in Lowe syndrome patients.
Keywords: Epidermal Cyst, Oculocerebrorenal Syndrome, Pediatrics
Background
Lowe syndrome, also known as oculocerebrorenal syndrome, is a rare genetic disorder with an estimated prevalence in the general population of approximately 1 in 500 000. It is a multisystem disorder characterized by abnormalities in the eye, nervous system, and kidneys [1]. These commonly manifest as congenital cataracts, intellectual disability, and proximal renal dysfunction (Fanconi-type). Other cardinal features include isolated kidney dysfunction, severe progressive growth retardation, neonatal hypotonia, areflexia, seizures, arthropathy, and behavioral problems [2]. Less-commonly described manifestations of Lowe syndrome include epidermal cysts. In this case report we report multiple perianal epidermal cysts found in a 9-year-old boy, an uncommon presentation of Lowe syndrome, not previously described in the literature to our knowledge [3,4].
Case Report
This is a case of a 9-year-old boy with a history of Lowe syndrome, congenital cataracts, hypotonic cerebral palsy, developmental delay, epilepsy, congenital dysplasia of the hips, and neurogenic bowel and bladder who presented with multiple perianal masses that were suspected of being epidermal cysts, an uncommon manifestation in Lowe syndrome. The diagnosis of Lowe syndrome was confirmed in June of 2020 via whole-exome sequencing, which found a hemizygous variant in the classically associated OCRL1 gene. The mother reported that there had been a large perianal lesion for 2–3 years followed by 6–8 months of 2 smaller perianal lesions appearing. The lesions caused intermittent pain and discomfort, but the mother denied any erythema, changes to skin, bleeding, or discharge. Physical exam revealed 3 bulging perianal masses with the largest being at the left inferior position and 2 smaller lesions superiorly, near the gluteal cleft (Figure 1).
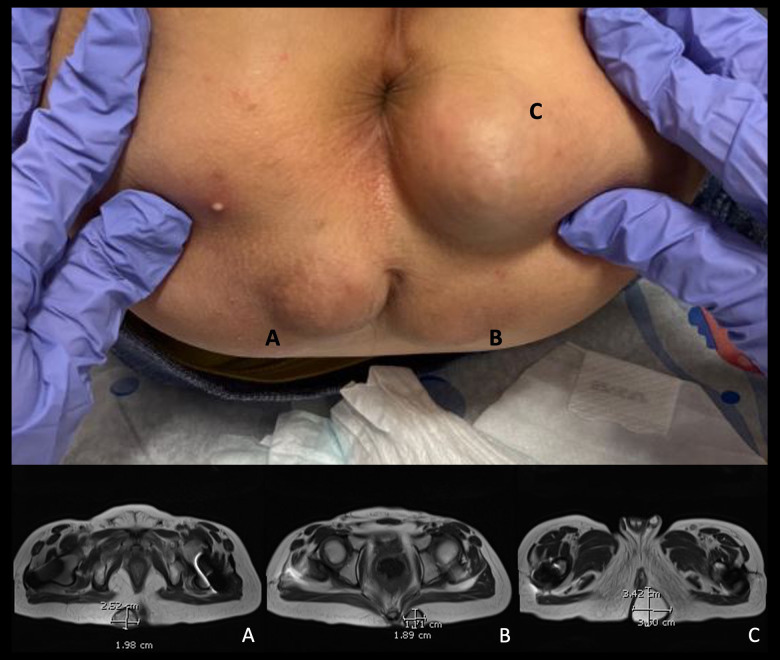
Figure 1.
Gross and MRI images of 3 perianal cystic masses. A) Lesion located to the right of the coccyx. B) The most superior lesion located to the left of the coccyx. C) The largest, most inferior lesion located in the left perirectal region of the buttocks.
A pelvis MRI with and without contrast was ordered to further define the masses. The imaging found 3 well-circumscribed, rounded lesions in the soft tissue adjacent to the gluteal cleft. The largest, most inferior lesion was found in the left perirectal region and measured 3.3×2.5×3.8 cm, with a cystic appearance. The most superior lesion was found to the left of the coccyx and measured 1.8×1.6×2.4 cm. The third lesion was found to the right of the coccyx and measured 2.4×2.0×2.4 cm. The 2 relatively smaller lesions appeared to be marginally heterogenous in comparison to the larger, simpler lesion (Figure 1). Given that the lesions appeared amenable to complete excision, it was deemed reasonable to consider excisional biopsy rather than fine-needle aspiration, which may not have been helpful given the cystic nature of the lesions.
The patient was then scheduled for a surgical excision of the 3 subcutaneous masses. Specimens consisted of an inferior perianal mass measuring 4.5×4×2.5 cm, a left gluteal mass measuring 3×2.5×1.5 cm, and a right gluteal mass measuring 2.5×2×1.5 cm. Postoperatively, the patient had an uneventful course and was discharged to home in good condition on the same day.
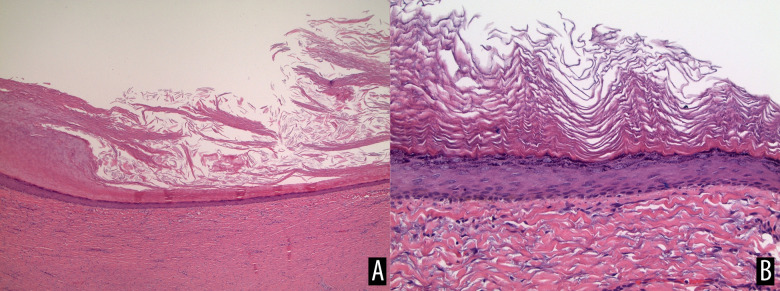
The pathology report was significant for 3 epidermal (infundibular) cysts. The left inferior perianal mass weighed 29.4 grams, the left superior gluteal mass weighed 9.5 grams, and the right superior gluteal mass weighed 7.2 grams. All 3 masses were well-encapsulated cystic structures with a smooth outer surface, and upon opening revealed a hollowed cystic structure with a smooth inner lining. The masses were all filled with a thick gray keratinaceous material (Figure 2).
Figure 2.
Pathological examination of the perianal cystic masses. (A) H&E stain at 40× magnification displaying fibrotic cystic wall with a keratinizing stratified squamous lining. (B) H&E stain at 200× magnification displaying epithelial lining of one of the cysts.
Two subsequent clinic follow-ups at 1 week and 2 months revealed 3 well-healing incisions with no signs of infection or lesion recurrence. The patient’s mother was then informed that they could follow-up as needed.
Discussion
The primary cause of Lowe syndrome is a mutation of the OCRL1 gene localized at Xq26. It is inherited in an X-linked recessive fashion but has also been attributed to de novo mutations at this locus [5]. Normally, the gene encodes a lipid phosphatase known as phosphatidylinositol 4, 5-bisphosphate-5-phosphatase (OCRL1) [6]. This phosphatase is localized in the Golgi network, with very diverse roles, dependent on the cell type it is localized in [7]. These include membrane trafficking, phagocytosis, cell adhesion and migration, cell polarity, ciliogenesis, cytokinesis, and intracellular signaling. A common theme exists, in that most processes affected by the loss of OCRL1 protein are actin-dependent [8]. This coincides with the primary underlying diagnosis of our patient due to the mutation in the OCRL1 gene being identified on a previous genetic analysis.
Manifestations of this condition are characterized by the triad of abnormalities within the eyes, nervous system, and the kidneys. Skin lesions have also been associated with this syndrome, but the relationship is poorly understood. Some clinicians have suggested that the mutation in Lowe syndrome also provokes cyst formation, but cysts are not currently considered a clinical feature of Lowe syndrome [3]. A single-institution case series by Kim et al described the clinical features of 12 male patients with confirmed diagnosis of Lowe syndrome [4]; all 12 of their patients had growth failure and developmental delay, and 11 of the 12 had congenital cataracts. Additionally, seizures occurred in 50% of their patients. Our patient also displayed these symptoms, supporting the underlying diagnosis of Lowe syndrome.
The child described in our case had the classic triad of abnormalities for Lowe syndrome, along with multiple epidermal cystic lesions, an uncommon manifestation of Lowe syndrome not previously described as localizing to the perianal area and being symptomatic (Table 1) [3,4,9,10]. Won et al reported a case of a 6-year-old boy with multiple asymptomatic cystic lesions found on the temporal and occipital scalp [3]. The histologic description of the cystic masses described in their paper closely resemble the perianal cystic masses found in our case. Kim et al also found that 5 of the 12 patients they reported with Lowe syndrome developed epidermal cysts, but they did not report perianal manifestations [4]. Other reported cutaneous cystic lesions described in Lowe syndrome include vellus hair cysts [9]. Therefore, the presentation of multiple symptomatic perianal cystic masses found in our case, to our knowledge, has not been previously described in the literature (Table 1) [3,4,8–10]. This is important to consider due to the fact that the original presentation led our team to consider malignant etiologies. After diagnostic imaging was performed, however, it became clear that these masses were in fact benign-appearing cystic masses.
Table 1.
Reviewed articles of cystic lesions in cases of Lowe syndrome.
| Article reviewed | Presentation | Signs and symptoms | Location of cyst(s) |
|---|---|---|---|
| Won et al [3] | 6-year-old male | Asymptomatic | Temporal and occipital scalp |
| Kim et al [4] | 18-year-old male | Not mentioned | Back or buttocks |
| 16-year-old male | Not mentioned | Back or buttocks | |
| 23-year-old male | Not mentioned | Back or buttocks | |
| 24-year-old male | Not mentioned | Back or buttocks | |
| 1-year-old male | Not mentioned | Back or buttocks | |
| Nandedkar et al [9] | 20-year-old male | Asymptomatic | Midchest |
| Ikehara et al [10] | 9-year-old male | Asymptomatic | Occipital scalp |
The exact mechanism of cystic lesions formation is unknown, but some studies have suggested that it is related to abnormal levels of extracellular lysosomal enzymes [11]. Nandekar et al reported a case of eruptive vellus hair cysts that displayed abnormally high levels of these extracellular lysosomal enzymes. It is suggested that the loss of cellular control due to accumulation of PIP2 and extracellular release of lysosomal enzymes leads to cyst formation. The cysts are believed to appear as a local defense against destructive enzymes that accumulate as a result of extracellular lysosomal enzymes [9].
Akin to the technique described in Won et al, the epidermal lesions in this case were similarly removed via excision [3]. Despite cyst removal, a study suggested that recurrence of cutaneous cysts to be as high as 42% [4]. Of note, when excision is performed, hemostasis may be difficult to achieve due to platelet dysfunction [11]. Recker et al reported that tranexamic acid improves platelet function in patients with Lowe syndrome, so it can be considered perioperatively [9]. Despite an increased risk of bleeding, our patient tolerated the procedure well without the need for additional therapies to support hemostasis. On follow-up with the patient, no evidence of recurrence has been detected.
There are some reasons why these cysts with an unusual presentation in Lowe syndrome should be considered. The first is that effective management through excision is available, as stated previously. Another is due to the fact that, although rare, malignant transformation is possible [12]. Possible transformations include squamous cell carcinoma, basal cell carcinoma, and Merkel cell carcinoma [12]. Each of these malignancies carry its own set of risks, so identification of these cysts is important for effective management of patients with Lowe syndrome.
Therefore, epidermal cysts are an association of Lowe syndrome. However, the perianal location and symptomatic nature of these cysts are rare. Our primary goal with this paper was to reiterate that unusual locations of epidermal cyst can be seen with this syndrome. Thus, epidermal cysts should be kept in the list of differential diagnoses if unusual cysts are encountered in patients with Lowe syndrome.
Conclusions
The novelty of our case is the presentation of multiple symptomatic perianal epidermal cystic lesions. At presentation, the constellation of pain and perianal masses was concerning for a malignant etiology. However, after diagnostic imaging was performed, these lesions were found to be epidermal cysts, which is an uncommon manifestation of Lowe syndrome. Previous case reports have described cystic lesions in association with Lowe syndrome, but none, to our knowledge, have described multiple symptomatic perianal lesions. This case highlights the effectiveness of excision in treating patients with cutaneous manifestations from Lowe syndrome, with relatively low morbidity. Proper identification of epidermal cysts in patients with Lowe syndrome can assist in effective management and treatment options and help prevent possible negative outcomes for similar cases. Therefore, it is important to consider these lesions in the differential diagnosis of unusual cystic masses in Lowe syndrome because, with timely identification and excision, patients may be relieved of discomfort in a safe and efficient approach.
Footnotes
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Loi M. Lowe syndrome. Orphanet J Rare Dis. 2006;1:16. doi: 10.1186/1750-1172-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ma X, Ning K, Jabbehdari S, et al. Oculocerebrorenal syndrome of Lowe: Survey of ophthalmic presentations and management. Eur J Ophthalmol. 2020;30(5):966–73. doi: 10.1177/1120672120920544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Won JH, Lee MJ, Park JS, et al. Multiple epidermal cysts in lowe syndrome. Ann Dermatol. 2010;22(4):444–46. doi: 10.5021/ad.2010.22.4.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim HK, Kim JH, Kim YM, et al. Lowe syndrome: A single center’s experience in Korea. Korean J Pediatr. 2014;57(3):140–48. doi: 10.3345/kjp.2014.57.3.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bokenkamp A, Ludwig M. The oculocerebrorenal syndrome of Lowe: An update. Pediatr Nephrol. 2016;31(12):2201–12. doi: 10.1007/s00467-016-3343-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tatsi P, Papanikolaou GE, Chartomatsidou T, et al. Lowe syndrome identified in the offspring of an oocyte donor who was an unknown carrier of a de novo mutation: A case report and review of the literature. J Med Case Rep. 2019;13(1):325. doi: 10.1186/s13256-019-2263-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dressman MA, Olivos-Glander IM, Nussbaum RL, Suchy SF. Ocrl1, a PtdIns(4,5) P(2) 5-phosphatase, is localized to the trans-Golgi network of fibroblasts and epithelial cells. J Histochem Cytochem. 2000;48(2):179–90. doi: 10.1177/002215540004800203. [DOI] [PubMed] [Google Scholar]
- 8.Mehta ZB, Pietka G, Lowe M. The cellular and physiological functions of the Lowe syndrome protein OCRL1. Traffic. 2014;15(5):471–87. doi: 10.1111/tra.12160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nandedkar MA, Minus H, Nandedkar MA. Eruptive vellus hair cysts in a patient with Lowe syndrome. Pediatr Dermatol. 2004;21(1):54–57. doi: 10.1111/j.0736-8046.2004.21112.x. [DOI] [PubMed] [Google Scholar]
- 10.Ikehara S, Utani A. Multiple protrusive epidermal cysts on the scalp of a Lowe syndrome patient. J Dermatol. 2017;44(1):105–7. doi: 10.1111/1346-8138.13444. [DOI] [PubMed] [Google Scholar]
- 11.Recker F, Reutter H, Ludwig M. Lowe syndrome/Dent-2 disease: A comprehensive review of known and novel aspects. J Pediatr Genet. 2013;2(2):53–68. doi: 10.3233/PGE-13049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wollina U, Langner D, Tchernev G, et al. Epidermoid cysts – a wide spectrum of clinical presentation and successful treatment by surgery: A retrospective 10-year analysis and literature review. Open Access Maced J Med Sci. 2018;6(1):28–30. doi: 10.3889/oamjms.2018.027. [DOI] [PMC free article] [PubMed] [Google Scholar]