Abstract
We describe changes in the comprehensiveness of services delivered by family physicians in 4 Canadian provinces (British Columbia, Manitoba, Ontario, Nova Scotia) during the periods 1999-2000 and 2017-2018 and explore if changes differ by years in practice. We measured comprehensiveness using province-wide billing data across 7 settings (home, long-term care, emergency department, hospital, obstetrics, surgical assistance, anesthesiology) and 7 service areas (pre/postnatal care, Papanicolaou [Pap] testing, mental health, substance use, cancer care, minor surgery, palliative home visits). Comprehensiveness declined in all provinces, with greater changes in number of service settings than service areas. Decreases were no greater among new-to-practice physicians.
Key words: comprehensive health care, scope of practice, primary care, family medicine, cohort effect, Canada
INTRODUCTION
Declining comprehensiveness of family physician practice has been documented across multiple jurisdictions,1-8 with accompanying speculation that this is driven by lack of interest or inadequate training among more recent cohorts of family physicians.1,9-17 Supporting this speculation are data showing that physicians who have recently entered practice participate in a narrower range of services and/or practice settings than those in established practice.2,8,14,18
An accurate understanding of changes in comprehensiveness is needed to inform policy responses. If more recent cohorts are delivering less comprehensive care than more experienced physicians, targeted interventions during formative stages of training and in the early career process might be needed. We used population-based linked administrative data from 4 Canadian provinces to test the hypothesis that any decline in comprehensiveness over time is greater among physicians within their first 10 years of practice than among physicians in practice for >10 years.
METHODS
Data and Measures
Our team includes researchers and family physicians in each of 4 Canadian provinces (British Columbia [BC], Manitoba [MB], Ontario [ON], and Nova Scotia [NS]). We used administrative data for billing and shadow-billing information submitted by all practicing family physicians to describe comprehensiveness of care at 2 points in time (1999-2000 and 2017-2018, the oldest and most recent years for which data comparable across provinces were available) in BC, MB, ON, and NS. We accessed similar databases, developed comparable definitions for all variables, and conducted parallel analyses for each province. Further details on these data are published elsewhere,19-27 and complete methods are available in Supplemental Appendix 1. We obtained ethics approval for each jurisdiction.
Comprehensiveness
We identified 7 settings (home, long-term care, emergency department, hospital, obstetrics, surgical assistance, and anesthesiology) and 7 service areas of office-based practice (pre/postnatal care, Papanicolaou [Pap] testing, mental health, substance use, cancer care, minor surgery, and palliative home visits) that could be tracked consistently over time for each of the 4 study provinces [Supplemental Table 1]). These align with settings and domains of care in the College of Family Physicians of Canada’s Family Medicine Profile28 and Residency Training Profile29 and build on an approach previously published using administrative data in Ontario.18
Physician characteristics
We used data from provincial regulatory colleges to classify the physician population on the basis of years in practice, sex, and location of training (Canada, international, or unknown).20 Urban/rural practice location was assigned on the basis of the location of residence of patients seen by the family physician.30 We counted the number of patient contacts per year as a measure of practice volume. The physician populations included in the analysis are described in Supplemental Table 2.
Analysis
We used generalized estimating equations (Poisson distribution and log link) to examine changes in count of service settings and service areas for 1999-2000 and 2017-2018. We tested the hypothesis that there was a significant interaction between year and years in practice, adjusting for physician sex, urban/rural practice location, and location of training (Canada, international, unknown) and confirmed results were consistent with and without adjustment for practice volume.
RESULTS
The mean number of service settings in which physicians had contacts decreased in all provinces by 1.0 to 1.7 settings, and the number of service areas decreased by 0.3 to 0.5 areas. In 1999-2000, physicians in their first 10 years practiced in fewer service settings on average than physicians in practice for 10-29 years (Figure 1). In 2017-2018, patterns changed such that physicians in their first 10 years had similar or more mean service settings than physicians in practice for ≥10 years.
Figure 1.
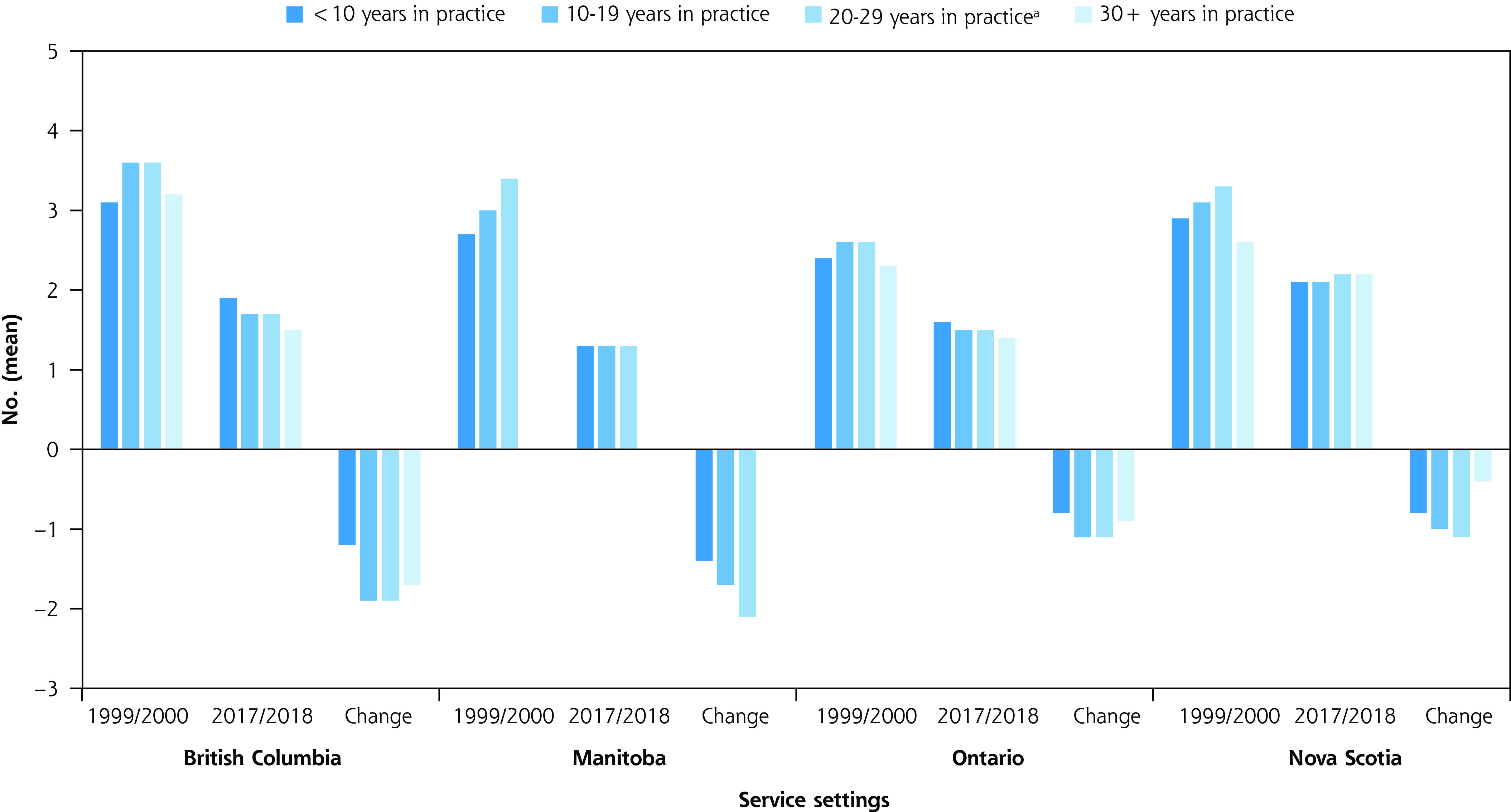
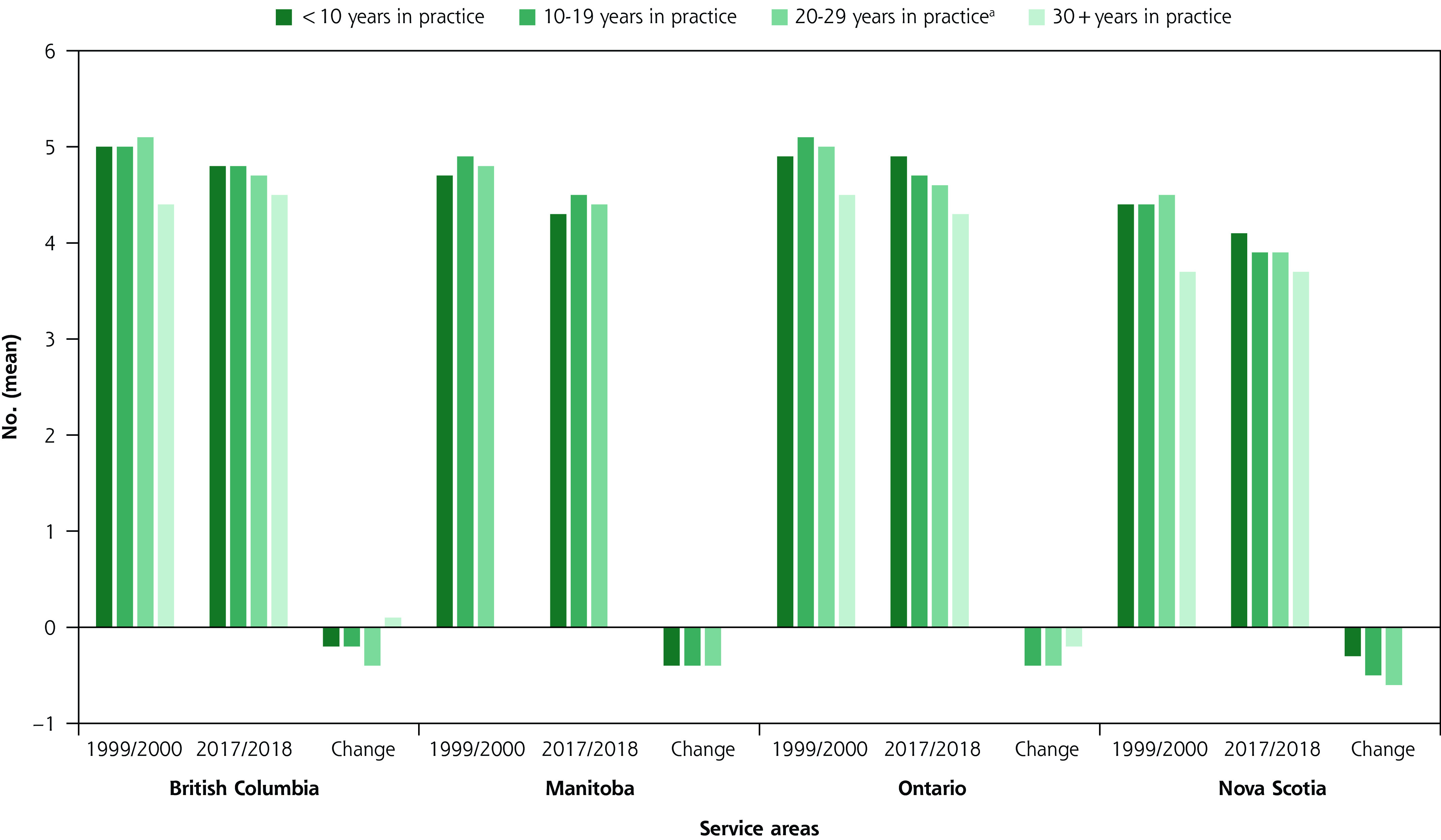
Mean number of service settings and service areas in 1999-2000 and 2017-2018 and changes over time, by years in practice.
a In Manitoba this category includes all physicians in practice ≥20 years.
The average number of service areas varied less by years in practice than did service settings. For both years, physicians in their first 10 years had similar mean service areas to those in practice longer (Figure 1).
In both unadjusted and adjusted regression analyses, physicians in practice <10 years practiced in fewer service settings (rate ratios <1) compared to those in practice 10 to 19 years, and the number of settings decreased from 1999-2000 to 2017-2018 (Table 1). The interaction effects for year and <10 years in practice showed that any decrease in service setting was less among physicians in practice <10 years (BC, ON, NS) or not significantly different (MB) from those in practice 10 to 19 years.
Table 1.
Rate Ratios (95% CI) for Comprehensiveness of Service Settings
| British Columbia | Manitoba | Ontario | Nova Scotia | |||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Intercept | NA | 3.72 (3.54-3.91) |
NA | 3.26 (2.92-3.63) |
NA | 3.1 (2.9-3.21) |
NA | 2.26 (2.06-2.47) |
| Years since MD (reference = 10-19 years) | ||||||||
| <10 | 0.92 (0.88-0.96) |
0.9 (0.86-0.94) |
0.86 (0.78-0.94) |
0.89 (0.81-0.97) |
0.92 (0.89-0.94) |
0.95 (0.92-0.99) |
0.92 (0.85-0.98) |
0.96 (0.88-1.04) |
| 20-29 (MB: ≥20) | 0.9 (0.86-0.93) |
1.02 (0.98-1.06) |
0.89 (0.79-0.99) |
1.05 (0.95-1.16) |
0.96 (0.93-0.98) |
0.96 (0.93-1.0) |
0.96 (0.89-1.03) |
1.0 (0.93-1.04) |
| ≥30 | 0.63 (0.6-0.67) |
0.95 (0.9-1.01) |
NA | NA | 0.8 (0.77-0.82) |
0.89 (0.85-0.93) |
0.77 (0.72-0.83) |
0.86 (0.77-0.95) |
| Year | ||||||||
| 2017-2018 (vs 1999-2000) | 0.49 (0.47-0.5) |
0.52 (0.49-0.56) |
0.45 (0.42-0.48) |
0.48 (0.42-0.56) |
0.6 (0.59-0.62) |
0.65 (0.62-0.68) |
0.69 (0.67-0.73) |
0.76 (0.96-0.84) |
| Interaction | ||||||||
| Year, <10 | NA | 1.25 (1.15-1.37) |
NA | 1.13 (0.96-1.34) |
NA | 1.13 (1.06-1.2) |
NA | 1.07 (0.94-1.23) |
| Year, 20-29 (MB: ≥20) | NA | 0.95 (0.86-1.03) |
NA | 0.92 (0.76-1.12) |
NA | 1.0 (0.95-1.06) |
NA | 0.94 (0.83-1.08) |
| Year, ≥30 | NA | 0.87 (0.78-0.96) |
NA | NA | NA | 0.99 (0.9-1.05) |
NA | 1.09 (0.94-1.26) |
| Covariates | ||||||||
| Male (vs female) | 1.29 (1.24-1.34) |
1.11 (1.07-1.16) |
1.69 (1.54-1.84) |
1.27 (1.17-1.37) |
1.4 (1.37-1.43) |
1.22 (1.19-1.25) |
1.14 (1.08-1.2) |
0.99 (0.95-1.06) |
| Urban (vs rural) | 0.75 (0.72-0.77) |
0.72 (0.7-0.75) |
0.56 (0.52-0.6) |
0.54 (0.5-0.57) |
0.54 (0.53-0.56) |
0.55 (0.53-0.56) |
0.9 (0.85-0.96) |
1.0 (0.95-1.06) |
| Number of contacts (per 100 contacts) | 1.01 (1.0-1.01) |
1.0 (1.0-1.0) |
1.01 (1.0-1.01) |
1.0 (1.0-1.01) |
1.0 (1.0-1.0) |
1.0 (1.0-1.0) |
1.01 (1.01-1.01) |
1.01 (1.0-1.01) |
| International MD (vs Canadian MD) | 0.86 (0.83-0.9) |
0.9 (0.87-0.94) |
0.91 (0.84-0.98) |
0.79 (0.73-0.84) |
NA | NA | NA | NA |
| Unknown MD (vs Canadian MD) | 0.76 (0.66-0.87) |
0.83 (0.73-0.95) |
1.22 (0.92-1.62) |
1.38 (1.26-1.52) |
NA | NA | NA | NA |
MB = Manitoba; MD = Doctor of Medicine; NA = not applicable.
Note: There were missing data on place of graduation in Nova Scotia and incomplete data in Ontario; therefore, this variable was excluded from modeling in these provinces.
There were no significant differences in the number of service areas between physicians in practice <10 years and those in practice 10 to 19 years (Table 2). The interaction between year and years in practice was not significant, or as in Ontario indicated that physicians in practice <10 years practiced in slightly more service areas than would be predicted by years in practice and year alone.
Table 2.
Rate Ratios (95% CI) for Comprehensiveness of Service Areas
| British Columbia | Manitoba | Ontario | Nova Scotia | |||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Intercept | NA | 4.56 (4.46-4.65) |
NA | 4.57 (4.36-4.78) |
NA | 4.99 (4.86-5.13) |
NA | 3.72 (3.55-3.9) |
| Years since MD (reference = 10-19 years) | ||||||||
| <10 | 0.99 (0.98-1.01) |
1.02 (1.0-1.04) |
0.96 (0.93-0.99) |
1.01 (0.98-1.05) |
1.0 (0.98-1.01) |
0.99 (0.97-1.02) |
1.02 (0.98-1.05) |
1.03 (0.99-1.07) |
| 20-29 (MB: ≥20) | 0.98 (0.97-0.99) |
0.99 (0.97-1.01) |
0.94 (0.9-0.97) |
1.02 (0.97-1.06) |
0.97 (0.96-0.99) |
0.97 (0.95-1.0) |
0.98 (0.95-1.01) |
0.98 (0.95-1.02) |
| ≥30 | 0.89 (0.88-0.91) |
0.92 (0.89-0.95) |
NA | NA | 0.89 (0.87-0.9) |
0.9 (0.88-0.93) |
0.87 (0.84-0.9) |
0.87 (0.81-0.93) |
| Year | ||||||||
| 2017-2018 (vs 1999-2000) | 0.93 (0.93-0.94) |
0.99 (0.97-1.01) |
0.9 (0.88-0.92) |
0.97 (0.93-1.02) |
0.93 (0.92-0.94) |
0.95 (0.93-0.98) |
0.89 (0.87-0.91) |
0.95 (0.9-1.0) |
| Interaction | ||||||||
| Year, <10 | NA | 1.0 (0.97-1.03) |
NA | 0.97 (0.92-1.02) |
NA | 1.06 (1.02-1.1) |
NA | 1.04 (0.97-1.11) |
| Year, 20-29 (MB: ≥20) | NA | 0.98 (0.95-1.0) |
NA | 0.92 (0.86-0.99) |
NA | 1.0 (0.96-1.03) |
NA | 0.98 (0.92-1.05) |
| Year, ≥30 | NA | 1.01 (0.97-1.05) |
NA | NA | NA | 1.04 (1.0-1.08) |
NA | 1.07 (0.98-1.16) |
| Covariates | ||||||||
| Male (vs female) | 1.03 (1.02-1.04) |
0.97 (0.96-0.98) |
1.02 (0.99-1.04) |
0.92 (0.9-0.95) |
1.01 (1.0-1.02) |
0.96 (0.95-0.98) |
0.99 (0.97-1.02) |
0.91 (0.89-0.94) |
| Urban (vs rural) | 0.96 (0.94-0.97) |
0.92 (0.91-0.93) |
0.93 (0.9-0.95) |
0.88 (0.85-0.9) |
0.89 (0.88-0.91) |
0.88 (0.86-0.9) |
0.91 (0.89-0.94) |
0.96 (0.93-0.98) |
| Number of contacts (per 100 contacts) | 1.0 (1.0-1.0) |
1.0 (1.0-1.0) |
1.0 (1.0-1.0) |
1.0 (1.0-1.0) |
1.0 (1.0-1.0) |
1.0 (1.0-1.0) |
1.0 (1.0-1.0) |
1.0 (1.0-1.01) |
| International MD (vs Canadian MD) | 1.03 (1.02-1.04) |
1.01 (1.00-1.02) |
1.0 (0.97-1.03) |
0.94 (0.92-0.96) |
NA | NA | NA | NA |
| Unknown MD (vs Canadian MD) | 0.97 (0.93-1.01) |
0.95 (0.91-0.99) |
1.0 (0.85-1.16) |
1.01 (0.86-1.19) |
NA | NA | NA | NA |
MB = Manitoba; MD = Doctor of Medicine; NA = not applicable.
Note: There were missing data on place of graduation in Nova Scotia and incomplete data in Ontario; therefore, this variable was excluded from modeling in these provinces.
DISCUSSION
We found declining comprehensiveness across 4 provinces, with greater changes in service settings than areas of office-based practice, but no evidence that comprehensiveness declined faster among physicians in their first 10 years of practice. Our measure of comprehensiveness was limited to service settings and areas that could be consistently measured with administrative data over time and across provinces. Each province has its own system of fee codes and billing requirements, yet findings were consistent across provinces. Our analysis does not speak to whether services delivered were in line with population needs. Given that some physicians focus on specific settings (ie, providing hospitalist care or working in emergency departments or in long-term care), declining physician-level comprehensiveness might not reflect declining total service volumes among all family physicians.
The present findings reinforce the concept that whereas comprehensiveness has declined over time among physicians entering practice (as has been observed elsewhere),11,15 this decline occurs across all career stages for the periods assessed.1,5,18 Our findings were remarkably consistent across the 4 provinces examined, given that each has their own provincially administered health insurance systems and varying models of primary care delivery and physician payment. Any efforts to enhance or maintain comprehensiveness of care delivered by family physicians should address the service delivery contexts in which all physicians are practicing rather than on interventions in training or early practice.
Supplementary Material
Footnotes
Conflicts of interest: authors report none.
Read or post commentaries in response to this article.
Funding support: This study received funding from the Canadian Institutes of Health Research (Project Grant 155965). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; or decision to submit the manuscript for publication. The statements expressed herein are solely those of the authors and do not necessarily reflect those of the funder, and no endorsements are intended or should be inferred.
Data support:
British Columbia: Access to data provided by the Data Steward(s) is subject to approval but can be requested for research projects via the Data Steward(s) or their designated service providers. All inferences, opinions, and conclusions drawn in this publication are those of the author(s) and do not reflect the opinions or policies of the Data Steward(s).
Ontario: This study was supported by the Institute for Clinical Evaluative Sciences, which is funded by an annual grant from the Ontario Ministry of Health and the Ministry of Long-Term Care. Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information. The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
Nova Scotia: Portions of the data used in this report were made available by Health Data Nova Scotia of Dalhousie University (#2017-EGM-001). Although this research analysis is based on data obtained from the Nova Scotia Department of Health and Wellness, the observations and opinions expressed are those of the authors and do not represent those of either Health Data Nova Scotia or the Department of Health and Wellness.
Manitoba: The authors acknowledge the Manitoba Centre for Health Policy for use of data contained in the Manitoba Population Research Data Repository under project #2020-026 (HIPC# 2020/2021-10). The results and conclusions are those of the authors, and no official endorsement by the Manitoba Centre for Health Policy, Manitoba Health, or other data providers is intended or should be inferred. Data used in this study are from the Manitoba Population Research Data Repository housed at the Manitoba Centre for Health Policy, University of Manitoba, and were derived from data provided by Manitoba Health.
Ethics: This project received research ethics approval from the University of British Columbia-Simon Fraser University Harmonized Behavioral Research Ethics Board (H18-03291), Ontario Tech University Ethics Board (14867), Nova Scotia Health Authority Ethics Board (1023561), and the University of Manitoba Ethics Board (HS23897 [H2020:208]).
References
- 1.Chan BTB. The declining comprehensiveness of primary care. CMAJ. 2002; 166(4): 429-434. [PMC free article] [PubMed] [Google Scholar]
- 2.Chen FM, Huntington J, Kim S, Phillips WR, Stevens NG.. Prepared but not practicing: declining pregnancy care among recent family medicine residency graduates. Fam Med. 2006; 38(6): 423-426. [PubMed] [Google Scholar]
- 3.Cohen D, Coco A.. Declining trends in the provision of prenatal care visits by family physicians. Ann Fam Med. 2009; 7(2): 128-133. 10.1370/afm.916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xierali IM, Puffer JC, Tong ST, Bazemore AW, Green LA.. The percentage of family physicians attending to women’s gender-specific health needs is declining. J Am Board Fam Med. 2012; 25(4): 406-407. 10.3122/jabfm.2012.04.110290 [DOI] [PubMed] [Google Scholar]
- 5.Lavergne MR, Peterson S, McKendry R, Sivananthan S, McGrail K.. Full-service family practice in British Columbia: policy interventions and trends in practice, 1991-2010. Healthc Policy. 2014; 9(4): 32-47. [PMC free article] [PubMed] [Google Scholar]
- 6.Cohidon C, Cornuz J, Senn N.. Primary care in Switzerland: evolution of physicians’ profile and activities in twenty years (1993-2012). BMC Fam Pract. 2015; 16: 107. 10.1186/s12875-015-0321-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bitton A. The necessary return of comprehensive primary health care. Health Serv Res. 2018; 53(4): 2020-2026. 10.1111/1475-6773.12817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hedden L, Lavergne MR, McGrail KM, et al. Trends in providing out-of-office, urgent after-hours, and on-call care in British Columbia. Ann Fam Med. 2019; 17(2): 116-124. 10.1370/afm.2366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong E, Stewart M.. Predicting the scope of practice of family physicians. Can Fam Physician. 2010; 56(6): e219-e225. [PMC free article] [PubMed] [Google Scholar]
- 10.Ladouceur R. What has become of family physicians? Can Fam Physician. 2012; 58(12): 1322. [PMC free article] [PubMed] [Google Scholar]
- 11.Freeman TR, Boisvert L, Wong E, Wetmore S, Maddocks H.. Comprehensive practice: normative definition across 3 generations of alumni from a single family practice program, 1985 to 2012. Can Fam Physician. 2018; 64(10): 750-759. [PMC free article] [PubMed] [Google Scholar]
- 12.Rowland K. The voice of the new generation of family physicians. Ann Fam Med. 2014; 12(1): 6-7. 10.1370/afm.1614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glauser W, Tepper J.. Can family medicine meet the expectations of millennial doctors? Healthy Debate. Published May 26, 2016. Accessed Jan 3, 2023. www.healthydebate.ca/2016/05/topic/young-doctors-family-medicine
- 14.Jaakkimainen RL, Schultz SE, Glazier RH, Abrahams C, Verma S.. Tracking family medicine graduates. Where do they go, what services do they provide and whom do they see? BMC Fam Pract. 2012; 13: 26. 10.1186/1471-2296-13-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weidner AKH, Chen FM.. Changes in preparation and practice patterns among new family physicians. Ann Fam Med. 2019; 17(1): 46-48. 10.1370/afm.2337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saultz J. Comprehensive practice. Fam Med. 2017; 49(2): 89-90. [PubMed] [Google Scholar]
- 17.Saultz J. The importance of being comprehensive. Fam Med. 2012; 44(3): 157-158. [PubMed] [Google Scholar]
- 18.Schultz SE, Glazier RH.. Identification of physicians providing comprehensive primary care in Ontario: a retrospective analysis using linked administrative data. CMAJ Open. 2017; 5(4): E856-E863. 10.9778/cmajo.20170083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lavergne MR, Goldsmith LJ, Grudniewicz A, et al. Practice patterns among early-career primary care (ECPC) physicians and workforce planning implications: protocol for a mixed methods study. BMJ Open. 2019; 9(9): e030477. 10.1136/bmjopen-2019-030477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.British Columbia Ministry of Health . 2018: Medical services plan practitioner file. v2. Population Data BC. College of Physicians and Surgeons of BC. Published 2019. https://www.popdata.bc.ca/data [Google Scholar]
- 21.British Columbia Ministry of Health . 2019: PharmaNet. v2. Population Data BC. Data Stewardship Committee. Published 2019. https://www.popdata.bc.ca/data [Google Scholar]
- 22.British Columbia Ministry of Health . 2018: Medical services plan (MSP) payment information file. v2. Population Data BC. Published 2019. https://www.popdata.bc.ca/data
- 23.British Columbia Ministry of Health . 2019: Consolidation file (MSP registration & premium billing). v2. Population Data BC. Published 2019. https://www.popdata.bc.ca/data
- 24.British Columbia Ministry of Health . 2019: Vital events deaths. v2. Population Data BC. Published 2019. https://www.popdata.bc.ca/data
- 25.Canadian Institute for Health Information . 2019: Discharge abstract database (hospital separations). v2. Population Data BC. Published 2019. https://www.popdata.bc.ca/data
- 26.Canadian Institute for Health Information . 2019: National ambulatory care reporting system. v2. Population data BC. Published 2019. https://www.popdata.bc.ca/data
- 27.WorkSafeBC . 2018: WorkSafeBC claims and firm level files. v2. Population data BC. Published 2019. https://www.popdata.bc.ca/data
- 28.The College of Family Physicians of Canada . Family Medicine Professional Profile. The College of Family Physicians of Canada; 2018. Accessed Jan 3, 2023. https://www.cfpc.ca/CFPC/media/Resources/Education/FM-Professional-Profile.pdf [Google Scholar]
- 29.Fowler N, Wyman R, eds. Residency Training Profile for Family Medicine and Enhanced Skills Programs Leading to Certificates of Added Competence; Outcomes of Training Project. The College of Family Physicians of Canada; May 2021. Accessed Jan 3, 2023. https://www.cfpc.ca/CFPC/media/Resources/Education/Residency-Training-Profile-ENG.pdf [Google Scholar]
- 30.Statistics Canada . Statistical Area Classification (SAC). Published Sep 17, 2018. Accessed Sep 21, 2021. https://www150.statcan.gc.ca/n1/pub/92-195-x/2011001/other-autre/sac-css/sac-css-eng.htm
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


