Abstract
Background
Digital health interventions such as smartphone applications (mHealth) or Internet resources (eHealth) are increasingly used to improve the management of chronic conditions, such as type 2 diabetes mellitus. These digital health interventions can augment or replace traditional health services and may be paid for using healthcare budgets. While the impact of digital health interventions for the management of type 2 diabetes on health outcomes has been reviewed extensively, less attention has been paid to their economic impact.
Objective
This study aims to critically review existing literature on the impact of digital health interventions for the management of type 2 diabetes on health and social care utilisation and costs.
Methods
Studies that assessed the impact on health and social care utilisation of digital health interventions for type 2 diabetes were included in the study. We restricted the digital health interventions to information provision, self-management and behaviour management. Four databases were searched (MEDLINE, EMBASE, PsycINFO and EconLit) for articles published between January 2010 and March 2021. The studies were analysed using a narrative synthesis approach. The risk of bias and reporting quality were appraised using the ROBINS-I checklist.
Results
The review included 22 studies. Overall, studies reported mixed evidence on the impact of digital health interventions on health and social care utilisation and costs, and suggested this impact differs according to the healthcare utilisation component. For example, digital health intervention use was associated with lower medication use and fewer outpatient appointments, whereas evidence on general practitioner visits and inpatient admissions was mixed. Most reviewed studies focus on a single component of healthcare utilisation.
Conclusions
The review shows no clear evidence of an impact of digital health interventions on health and social care utilisation or costs. Further work is needed to assess the impact of digital health interventions across a broader range of care utilisation components and settings, including social and mental healthcare services.
Clinical Trial Registration
The study protocol was registered on PROSPERO before searches began in April 2021 (registration number: CRD42020172621).
Key Points for Decision Makers
| In this paper, we critically review and describe studies that assess the impact of digital health interventions in type 2 diabetes mellitus on healthcare utilization and cost. |
| We found that the impact of digital health may differ according to the care sector, such as medications or different types of appointments. |
| Drawing on the findings of this review, we propose some areas for further work, including an assessment of the impact of digital health interventions across a broader range of care utilisation components and settings, such as social and mental healthcare services. |
Introduction
The number of digital health interventions (DHIs) delivered through devices such as smartphones, tablets or computers has increased exponentially [1]. Such DHIs have been used to facilitate remote access to effective treatments, improve the management of chronic conditions and promote healthy behaviours. Previous systematic reviews have synthesised evidence about the impact of DHIs on health outcomes and patient experience [2, 3]. However, the economic impact of DHIs is less well understood. On the one hand, one might expect DHIs to be cost saving because they may help deliver healthcare more efficiently. On the other hand, the implementation of DHIs may imply large investments by the health system, for example, restructuring care pathways and health services, implementation costs and staff training and upskilling. While economic evidence is rapidly emerging, the overall direction and magnitude of the economic impact of DHIs is unclear.
One of the areas where DHIs have received considerable attention is the management of type 2 diabetes [4]. Digital health interventions are particularly valuable in this context because they can facilitate the management of the condition and encourage behavioural change (e.g. diet and exercise) [5]. Studying the economic impact of DHIs in type 2 diabetes is crucial because the burden of disease is large [6], and hence, there is ample scope to deliver more health gains from scarce health and social care resources. A recent study [7] reviewed cost-effectiveness analyses of DHIs for the prevention and control of type 2 diabetes but the focus was on DHIs delivered through smartphones and included decision-analytical modelling studies.
Our study aims to critically review the impact of DHIs for the management of type 2 diabetes across a broad range of health and social care services and their associated costs. The review focuses on DHIs that seek to promote or manage health and well-being through supporting behavioural change and decision making of the patient diagnosed with type 2 diabetes, sometimes in combination with a healthcare professional. In this population, DHIs may be used for the management of the long-term condition. Such interventions are typically interactive, personalised, based on user input and may be provided at the individual or population level. This review aims to generate a deeper understanding of the economic impacts (on individuals and health systems) of more complex types of DHIs. Simpler forms of DHIs, such as diagnostic and monitoring devices, are much closer to the nature of conventional medical devices, and their economic impact has been reviewed elsewhere [8]. While we focus on a single long-term condition, we anticipate a similar economic impact of DHIs that support behavioural change and decision making across other chronic conditions, such as arthritis or heart disease.
Methods
The review protocol was registered on PROSPERO (CRD42020172621) [9]. The review includes quantitative assessments of the economic impact of DHIs for type 2 diabetes.
Studies met the inclusion criteria for this review if:
they included a population of adults (aged 18 years and above) with type 2 diabetes who had received a DHI for information provision, self-management or behaviour management;
comparators were standard care, or information provision or group information sessions, no comparator or other DHIs;
the outcomes considered were health and social care utilisation and cost;
they were evaluations undertaken in a public or private clinical setting internationally; and
they were reported in journal articles published in English.
Studies were excluded if they were studying a patient population with type 1 diabetes, gestational or other rarer forms of diabetes, or the DHI was focussed on comorbidities or complications of type 2 diabetes. They were also excluded if clinicians alone used the interventions, for example decision-support systems, and if the study outcomes were only cost-effectiveness modelling (not including patient-level data) or patient experience or satisfaction alone, not including reporting of health and social care utilisation and costs.
Four databases, MEDLINE, EMBASE, PsycINFO and EconLit, were searched for articles published between January 2010 and March 2021. A search strategy was developed in MEDLINE with the help of an information specialist to ensure proper use of search terms. This strategy was adapted for use in the other databases. Appendix 1 shows the search strategy for all databases. It combined key terms about DHIs, type 2 diabetes and the economic impact in terms of health and social care utilisation and costs.
The database searches were run in April 2021. Duplicates were removed using the Rayyan web application [10] and Endnote referencing software [11]. The first reviewer screened all the records using Microsoft Excel. A second reviewer screened 20% of the included abstracts and full texts for eligibility. Any disputes were discussed between the first and second reviewers. If the conflicts remained, they were referred to a third reviewer.
Templates for data extraction were piloted and adapted to enable key data to be extracted from the included papers. Information was extracted on the characteristics of the studies (i.e. number of participants and participant characteristics, country, study type, length of follow-up, key outcome measures reported and their results), the impact on health and social care utilisation (e.g. self-reported or administrative data source changes in several types of health and social care utilisation) and the resulting impact on costs (e.g. how cost had changed in the reported follow-up period). The data extraction was reviewed by the third reviewer for quality assurance. The review results were analysed using a narrative synthesis approach, in which themes were identified within the study results that related to the aims of the study [12]. Because of the heterogeneity of the study designs and outcomes measures, it was not possible to perform a meta-analysis.
The ROBINS-I tool [13] was used to appraise all papers by the first reviewer and all studies were also appraised by a second reviewer. It is a quality assessment checklist designed to assess the overall risk of biases in the study design and analysis, including aspects related to: (1) confounding; (2) sample selection; (3) classification and measurement error; (4) deviations from study protocol; (4) missing data; and (5) reporting. Within each of these components, studies can be rated as ‘low risk of bias’ (comparable to a well-conducted randomised controlled trial [RCT]), ‘moderate risk of bias’ (sound for a non-randomised trial, but not comparable to a RCT), ‘serious risk of bias’ (the study has some significant issues that may affect the validity of the results), ‘critical risk of bias’ (too problematic to provide any useful evidence) and ‘no information’ (no information on which to base a judgement) if the design or analysis component has not been reported.
Results
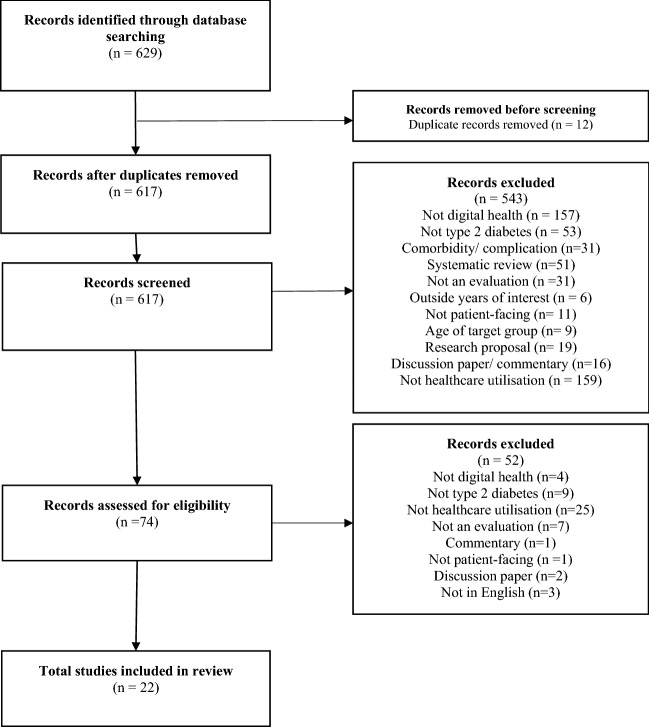
The results of the searches are shown in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart (Fig. 1). The database searches identified 617 papers after removing duplicates. These papers were then screened and assessed for eligibility. The reasons for papers to be excluded are outlined in the PRISMA flowchart. During abstract screening, many studies were excluded because they focused on a non-relevant DHI (n = 157). For example, they did not consider a DHI at all, or focused on medical devices for type 2 diabetes and interventions that were targeted at clinicians such as decision support systems. Others were excluded because they did not consider impacts on healthcare utilisation and costs (n = 159), focused on other types of diabetes or targeted complications (e.g. foot ulcers) of type 2 diabetes (n = 53). Systematic reviews synthesising the impact of DHIs on health outcomes and patient experience were also excluded (n = 51).
Fig. 1.
Preferred reporting items for systematic reviews and meta-analyses (PRISMA) flowchart
At full-text screening, studies were excluded mainly because they did not evaluate the impact on healthcare utilisation and costs (n = 25), did not focus on type 2 diabetes (n = 9) or were not an impact study (n = 7). Twenty-two studies were included in the review.
Study Characteristics
The key study characteristics are shown in Table 1. Most studies (n = 16, 73%) had over 100 participants and were conducted in North America (n = 8, 36%) or Europe (n = 9, 41%). Over half of the studies (n = 13, 59%) were conducted alongside RCTs. Almost half of the studies (n = 10, 45%) involved a comparison of DHI with treatment as usual, although this meant a variety of face-to-face services across a range of settings (e.g. primary and secondary care). Most studies considered relatively short follow-up periods: five (23%) had a follow-up of up to 6 months and 14 studies (64%) had a follow-up of 6–12 months.
Table 1.
Summary of study characteristics
| Number of participants | Number of studies (n = 22) | Percentage of studies (%) |
|---|---|---|
| < 50 | 4 | 18 |
| 50–100 | 2 | 9 |
| 101–200 | 7 | 32 |
| > 200 | 9 | 41 |
| Country | ||
| Europe | 9 | 41 |
| North America | 8 | 36 |
| Other | 5 | 23 |
| Study design | ||
| RCT | 12 | 55 |
| Non-randomised study | 10 | 45 |
| Length of follow-up (months) | ||
| <6 | 5 | 23 |
| 6–12 | 14 | 64 |
| >12 | 3 | 14 |
| Control group | ||
| TAU/standard care | 12 | 55 |
| Other DHI | 3 | 14 |
| None | 7 | 32 |
| Economic outcome* | ||
| Health and social care utilisation | 18 | 82 |
| Cost | 7 | 32 |
| Care component | ||
| Medication | 8 | 36 |
| Hospital episode | 3 | 14 |
| Multiple items | 11 | 50 |
| DHI type | ||
| Self-management | 8 | 36 |
| Behaviour management | 8 | 36 |
| Other | 6 | 27 |
Most studies considered the impact of DHIs on a single component of healthcare utilisation or costs. For example, eight studies reported the impact on medication utilisation (e.g. metformin or insulin) [14–21]. A measurement of HbA1c over 6.5% corresponds to a diagnosis of type 2 diabetes, and management of the condition includes targeting a level of HbA1c below 7%. Five of these were studies in which most patients had HbA1c levels between 7 and 9% [14–18] and the rest had populations where the mean HbA1c level was higher. In the studies where the time since onset was recorded, patients varied from ‘newly diagnosed’ to later stages of the disease requiring insulin or treatment intensification.
Very few studies (n = 3, 17%) reported an impact across several primary and secondary care utilisation components [22–24], which included a mix of hospital, general practitioner (GP) and community diabetes-related services. Eight (36%) of the studies were based on self-management (patients monitoring their lifestyle and condition alone) [14, 16, 22, 24–28] and eight more on behaviour management (patients and professionals managing patients’ lifestyle and condition) [15, 17, 20, 21, 29–32]. Four (18%) were based on self-management and information provision together [18, 19, 33, 34], one (5%) on behaviour and self-management [23], and another on behaviour management and information provision [35].
Summary of Study Results
The study results are summarised in Table 2. Overall, the direction of the impact of DHIs on health and social care utilisation was mixed, irrespective of the mode of delivery of the DHIs. Four (18%) studies reported an increase in healthcare utilisation [20–22, 33], seven (32%) studies suggested a reduction in care utilisation [16, 18, 24, 27, 28, 30, 34], and five (23%) studies reported both positive and negative economic impacts [17, 25, 26, 31, 32]. Of those studies that reported costs (n = 7, 31%), six suggested a decrease in costs [15, 19, 24, 28, 29, 35], and one reported increased costs [23]. The magnitude of the cost impact in these studies was relatively small, usually less than $500 saving per patient over a time horizon of 6–12 months.
Table 2.
Summary of study results
| First author (year) | Country | N | Study design | Follow-up | Intervention approach | Mode of delivery | Control | Health and social care utilisation category | Effect on health are utilisation | Effect on cost |
|---|---|---|---|---|---|---|---|---|---|---|
| Agarwal (2019) | Canada | 223 | RCT | 3 months | Self-management | App | Usual care | Primary, outpatient, emergency and inpatient | Mixed | |
| Al Hayek (2021) | Saudi Arabia | 105 | Prospective observational | 12 weeks | Self-management | App | None | Total healthcare | Increase | |
| Arora (2014) | USA | 128 | RCT | Self-management | Text | Usual care | Primary and emergency | Mixed | ||
| Fico (2020) | Italy, Czech Republic, Spain | 7* | Prospective observational | 4 weeks | Self-management | Web | None | Medication | No difference | |
| Fountoulakis (2015) | Greece | 105 | RCT | 12 months | Behaviour management | Web | Usual care | Outpatient | Decrease | |
| Gilmer (2019) | Mexico | 301 | RCT and simulation model | 5, 10, 15 and 20 years | Behaviour management/self-management | App | Usual care | Total healthcare | Increase | |
| Gordon (2014) | Australia | 120 | RCT | 6 months | Behaviour management | Mobile and web | Usual care | Medication | Decrease | |
| Katz (2012) | USA | 32 | Prospective observational | 56 weeks treatment group, 10 weeks control group | Self-management | App | None | Emergency and inpatient | Decrease | |
| Kempf (2017) | Germany | 202 | RCT | 12 months | Self-management | Web | Other DHI | Medication | Decrease | |
| Li (2018) | UK | 374 | RCT | 12 months | Self-management | Web | Other DHI | Total healthcare | Decrease | Decrease |
| Lorig (2016) | USA | 1242 | Prospective observational | 12 months | Self-management/ information provision | Web | Face-to-face | Diagnostic tests | Increase | |
| Lu (2020) | China | 120 | RCT | 6 months | Self-management/information provision | Web | Usual care | Medication | Decrease | |
| Luley (2011) | Germany | 70 | RCT | 6 months | Behaviour management | Web | Usual care | Medication | Mixed | |
| Maxwell (2016) | USA | 26 | Prospective observational | 6 months | Behaviour management | Web | None | Medication | Increase | |
| McGloin (2020) | USA | 40 | Prospective observational | 12 weeks | Behaviour management | Web | None | Primary, outpatient and inpatient | Decrease | |
| Menon (2017) | Australia | 103 | Retrospective observational | 1 month | Behaviour management | Web | Face-to-face | Medication | Increase | |
| Musacchio (2011) | Italy | 1004 | Retrospective observational | 12 months | Behaviour management | Web | None | Medication and outpatient | Mixed | |
| Nicolucci (2015) | Italy | 302 | RCT | 12 months | Self-management/information provision | Web | Usual care | Outpatient | Decrease | |
| Roelofsen (2016) | The Netherlands | 633 | Prospective observational | 12 months | Self-management/information provision | Web | Other DHI | Medication | Decrease | |
| Warren (2018) | Australia | 126 | RCT | 6 months | Behaviour management/information provision | Tablet and web | Usual care | Primary, outpatient, emergency and inpatient | Decrease | Decrease |
| Wild (2016) | UK | 307 | RCT | 9 months | Behaviour management | Web | Usual care | Primary and emergency | Mixed | |
| Yu (2020) | Taiwan | 97 | Prospective observational | 8 months | Self-management | App | None | Medication, primary and outpatient | Decrease | Decrease |
DHI digital health intervention, RCT randomised controlled trial
The reviewed studies suggest that the impact of DHIs might differ according to the component of healthcare utilisation. For example, DHIs were mostly associated with lower medication use [14–21, 28, 31, 36] and fewer outpatient visits [25, 28–32, 34, 35]. In the studies where the time since onset was recorded, patients varied from ‘newly diagnosed’ to later stages of the disease requiring insulin or treatment intensification. Whereas, the impact of DHIs on GP visits [25, 26, 28, 30, 32, 35], hospital accident and emergency [25–27, 32] and inpatient admission [25, 27, 30, 35] was mixed. In studies that reported impacts across multiple healthcare components and settings of care, the evidence was also mixed [22–24, 35]. None of the studies reported impacts on social care or mental healthcare utilisation.
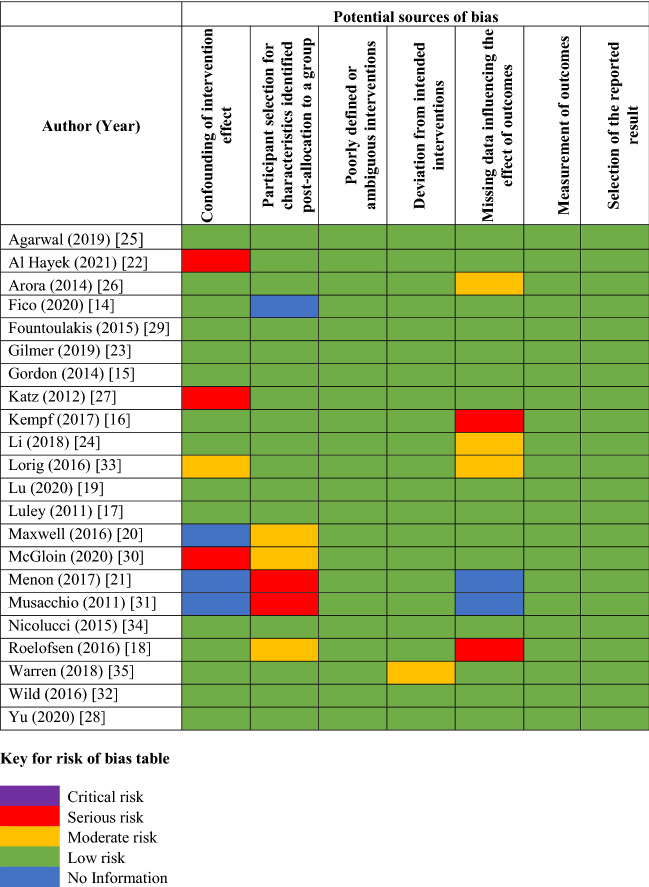
Quality Assessment
Results of the quality assessment are shown in Table 3. Overall, the risk of bias was relatively low across the reviewed studies [13]. Across the studies included, the most common issues were a lack of appropriate analysis methods for confounding, and missing data (lack of follow-up data for much of the original sample because of a high dropout, or a lack of information about methods for adjusting for missing data).
Table 3.
Risk of bias
Twelve (55%) RCTs were included in the analysis [15–17, 19, 23–26, 29, 32, 34, 35] with the vast majority being judged ‘low risk’ in all categories. The remaining ten (45%) [14, 18, 20–22, 27, 28, 30, 31, 33] studies were non-randomised, with three of them being rated ‘high risk’ because of potential issues with confounding [22, 27, 30]. Two studies were judged as having ‘moderate risk’ [20, 30] because of sample selection issues. Two of the observational studies provided insufficient information on missing data [21, 31] and were classified as ‘no information’.
Discussion
Summary of Findings
This study critically assessed published evidence on the economic impact of DHIs for type 2 diabetes on health and social care utilisation and costs. Overall, the review suggests that the direction of the impact of DHIs on healthcare utilisation is mixed and might differ according to the healthcare utilisation component. In particular, DHIs seem to be associated with a reduction in medication and fewer diabetes-related outpatient appointments. The vast majority of studies evaluating the impact of DHIs on healthcare costs reported a decrease in costs. The overall risk of biases in the reviewed studies is relatively low; the vast majority of the non-randomised studies was rated ‘low’ or ‘moderate’ risk across most bias components.
Contributions
This is the first study to comprehensively review the economic impact of DHIs for type 2 diabetes. Overall, our review suggests that the case for an economic benefit is not as clear as the clinical benefit shown in previous systematic reviews [3, 37]. The study also shows that the existing evidence base is limited because of the short follow-ups of many studies evaluating interventions for type 2 diabetes, and the difficulty in comparing heterogeneous results for the impact on service utilisation and costs. We have also shown that studies report a limited number of cost dimensions and do not show a benefit as clearly in the costliest types of care (e.g. hospital admissions). However, the studies have included participants at a range of various stages of the disease in terms of the time since diagnosis and the duration of type 2 diabetes symptoms (which may or may not be linked).
A recent study [7] reviewed the cost-effectiveness evidence on mHealth interventions for type 2 diabetes and suggested that, overall, these tend to provide good value for money. This does not necessary mean that the mHealth interventions considered in that study led to lower costs as they can be cost effective even if they are more costly than the comparator. However, this review [7] focused on (modelling-based) cost-effectiveness analyses, and interventions delivered through smartphones, whereas our study included a broader range of DHIs and all types of economic impact evaluations. By reviewing a more comprehensive range of impact studies, we find that the economic impact of DHIs may not be as well understood as suggested by the previous review.
Our review also found that the economic impact of DHIs might differ across the different types of healthcare utilisation. In fact, it suggests that potential economic benefits are most likely to materialise in certain care components such as medication and insulin use, or outpatient attendances [15, 16, 18, 19, 29, 34]. Unlike previous reviews [7], our study considered the impact of DHIs on both health and social care utilisation and costs, but found no evidence on the impact on social, community and informal care services.
Limitations
One of the limitations of this review is that it did not consider grey literature or studies published in languages other than English. It was deemed important to include high-quality evidence and full evaluations such as RCTs and large observational studies on the impacts of digital health, which are less likely to be reported outside journal articles.
Our study was not able to disentangle potential drivers of the impact of DHIs on health and social care utilisation and costs. Characteristics such as age, duration of disease, ethnicity or gender may have an impact on clinical and economic outcomes, but the reviewed studies have not considered whether the economic impact of DHIs varies across these factors. One notable exception is the evaluation of the HeLP-Diabetes programme, which adjusted for age and disease duration in the economic analysis [24]. Poduval et al.’s qualitative analysis as part of the same study finds that the shorter the duration of diabetes since diagnosis, the greater the likelihood of completing an intervention [38], and hence the higher the costs incurred.
The mix of results found in this review may have been partially explained by differences in care pathways and health financing systems across the different countries included in the review. However, this review was not able to disentangle this, and determine whether the findings are generalisable across jurisdictions. In addition, this review was not able to dissect whether the economic impact of DHIs differs according to whether the DHI complements or substitutes face-to-face health services. The heterogeneity of DHI types in terms of their function (self-management or behaviour management as defined previously) did not appear to have a clear effect on the impact of DHIs. However, the proportion of DHIs reducing service use or cost was slightly higher in DHIS for self-management (seven out of 12) [16, 18, 19, 24, 27, 28, 34] than when service users used the DHIs with healthcare professionals [15, 29, 30, 35].
Implications for Future Research
This review has identified some gaps in the literature about the impact of digital health for type 2 diabetes on healthcare utilisation. First, DHIs are likely lead to a broad range of health and non-health cost impacts, including those outside the healthcare sector [39]. Hence, studies should account for the potential economic impact across a broader range of sectors, such as social and community care settings, informal care and productivity impacts. Second, DHI software updates and iterations are an important consideration that has received little attention in the reviewed studies. Because digital health is a rapidly moving field, DHIs are likely to be updated during an evaluation. As a result, the interventions themselves may change during an evaluation and it will be important to assess the extent to which the evolving nature of DHIs impacts on health and social care utilisation. Third, further work is warranted to explore which type of patients benefit most from these DHIs and which elements of the DHIs drive this (e.g. therapeutic elements or dose), and how this heterogeneity may impact health and social care utilisation. This is important so that adaptations and iterations of DHIs target the populations that are most likely to benefit from the DHIs and lead to greater savings to the health system.
Conclusions
The review found mixed evidence on the economic impact of DHIs. Reviewed studies suggested that this impact might differ according to the care component, with DHIs being associated with a reduction in medication and diabetes-related outpatient appointments, but not GP visits or hospital admissions. Future work should consider exploring the economic impact of DHIs across a broader range of care components and settings, and whether this impact is mediated by patient or contextual factors.
Appendix 1: Search strategies
MEDLINE
"diabetes mellitus, type 2"/ or "adult onset diabetes mellitus".mp. or "type 2 diabetes".mp. or "t2dm".mp.
"Mobile applications"/ or "Telemedicine"/ or "Mobile application*".mp. or "Telemedicine".mp. or "Digital Health".mp. or "App* on prescription".mp. or "app".mp. or "Digital prescribing".mp. or "Wearable*".mp. or "Digital Therapeutic*".mp. or ("Digital" adj5 "Medicine").mp. or "blood glucose monitoring".mp. or "internet".mp. or "mHealth".mp. or "eHealth".mp. or "remote delivery".mp. or "online".mp. or "website".mp.
"Health Resources"/ or "health expenditures"/ or "health care use".mp. or "health care utili?ation".mp. or "health service use".mp. or "health service utili?ation".mp. or "social care use".mp. or "social care utili?ation".mp. or "social service use".mp. or "health care cost*".mp. or "health care expenditure".mp. or "medical cost*".mp. or "medical expenditure".mp. or "primary care cost*".mp. or "hospital care cost*".mp. or "health care visit*".mp. or "medical consultation*".mp. or "medical appointment*".mp. or "doctor visit*".mp. or "GP visit*".mp. or "hospital outpatient visit*".mp. or "hospital admission*".mp. or "specialist visit*".mp. or "specialist referral*".mp. or "help-seeking".mp. or "medication".mp. or "insulin use".mp. or "diabetic medicine*".mp. or "blood glucose-lowering drug*".mp. or "blood sugar-lowering drug*".mp.
1 and 2 and 3
limit 4 to dt=20100101-20210331
limit 5 to (english language and humans)
limit 6 to journal article
remove duplicates from 7
EMBASE
"Type 2 Diabetes".ti,ab,kw. or "Non Insulin Dependent Diabetes Mellitus"/ or "Adult Onset Diabetes".ti,ab,kw. or "t2dm". ti,ab,kw.
"Mobile application"/ or "Mobile application*".ti,ab,kw. or "Telemedicine*".ti,ab,kw. or "Telemedicine"/ or "Digital Health".ti,ab,kw. or "app".ti,ab,kw. or "App* on prescription".ti,ab,kw. or "Digital prescribing".ti,ab,kw. or "Wearable*".ti,ab,kw. or "Digital Therapeutic*".ti,ab,kw. or ("Digital" adj5 "Medicine").ti,ab,kw. or "blood glucose monitoring".ti,ab,kw. or "mHealth".ti,ab,kw. or "eHealth".ti,ab,kw. or "remote delivery".ti,ab,kw. or "online".ti,ab,kw. or "website".ti,ab,kw. or "internet".ti,ab,kw.
"health care utilisation"/ or "health care delivery"/ or "health care cost"/ or "healthcare expenditure*".ti,ab,kw. or "health care use".ti,ab,kw. or "health care utili#ation".ti,ab,kw. or "health care cost*".ti,ab,kw. or "health expenditure*".ti,ab,kw. or "health service use".ti,ab,kw. or "health care utili#ation".ti,ab,kw. or "social care use".ti,ab,kw. or "social care utili#ation".ti,ab,kw. or "social service use".ti,ab,kw. or "health care expenditure*".ti,ab,kw. or "medical cost*".ti,ab,kw. or "medical expenditure*".ti,ab,kw. or "primary care cost*".ti,ab,kw. or "hospital care cost*".ti,ab,kw. or "health care visit*".ti,ab,kw. or "medical consultation*".ti,ab,kw. or "medical appointment*".ti,ab,kw. or "doctor visit*".ti,ab,kw. or "GP visit*".ti,ab,kw. or "hospital outpatient visit*".ti,ab,kw. or "hospital admission*".ti,ab,kw. or "specialist visit*".ti,ab,kw. or "specialist referral*".ti,ab,kw. or "help-seeking".ti,ab,kw. or "medication*".ti,ab,kw. or "insulin use".ti,ab,kw. or "diabetic medicine*".ti,ab,kw. or "blood glucose-lowering drug*".ti,ab,kw. or "blood sugar-lowering drug*".ti,ab,kw. or "medical spending".ti,ab,kw. or "service use".ti,ab,kw. or "health resource*".ti,ab,kw.
1 and 2 and 3
limit 4 to dc=20100101-20210331
limit 5 to (human and english language)
limit 6 to (article and journal)
remove duplicates from 7
PsychInfo
exp "Type 2 Diabetes"/ or "Adult Onset Diabetes".mp. or "diabetes mellitus type 2".mp. or "type 2 diabetes".mp. or "t2dm".mp.
exp "Mobile Applications"/ or "Mobile Application*".mp. or exp "Computer Applications"/ or "Telemedicine".mp. or exp "Telemedicine"/ or "Digital Health".mp. or exp "Digital Interventions"/ or "Digital Prescribing".mp. or exp "Wearable Devices"/ or " App* on prescription ".mp. or " app".mp. or "Digital Therapeutic*".mp. or ("Digital" adj5 "Medicine").mp. or "blood glucose monitoring".mp. or "internet".mp. or "mHealth".mp. or "eHealth".mp. or "remote delivery".mp. or "online".mp. or "website".mp.
exp "Health Care Utilization"/ or exp "Health Care Services"/ or exp "Health Care Costs"/ or "Health Care Cost*".mp. or "health expenditure*".mp. or "medical spending".mp. or "Health Resource*".mp. or "health care use".mp. or "health service use".mp. or "health service utili#ation".mp. or "social care use".mp. or "social care utili#ation".mp. or "social service use".mp. or "health care expenditure*".mp. or "medical cost*".mp. or "medical expenditure*".mp. or "primary care cost*".mp. or "hospital care cost*".mp. or "health care visit*".mp. or "medical consultation*".mp. or "medical appointment*".mp. or "doctor visit*".mp. or "GP visit*".mp. or "hospital outpatient visit*".mp. or "hospital admission*".mp. or "specialist visit*".mp. or "specialist referral*".mp. or "help-seeking".mp. or "medication*".mp. or "insulin use".mp. or "diabetic medicine*".mp. or "blood glucose-lowering drug*".mp. or "blood sugar-lowering drug*".mp.
1 and 2 and 3
limit 4 to up="20100101-20210331"
limit 5 to (human and english language)
limit 6 to journal article
remove duplicates from 7
EconLit
TX diabetes mellitus type 2 or type 2 diabetes or t2dm or adult-onset diabetes
TX mobile application? or telemedicine or mobile application? or app or mobile app? or mhealth or ehealth or digital health or digital medicine or digital prescribing or wearable* or digital therapeutic* or digital medicine or blood glucose monitoring
TX health resource utili?ation or health care service? or health resource? or medical spending or service use or healthcare utili?ation or health care cost? or outpatient visit? or health care use or health service use or health service utili?ation or social care use or social care utili?ation or social service use or health care expenditure? or medical cost? or medical expenditure? or primary care cost? or hospital care cost? or health care visit? or medical consultation? or medical appointment? or doctor visit? or GP visit? hospital outpatient visit? or hospital admission? or specialist visit? or specialist referral? or help-seeking or medication or insulin use or diabetic medicine or blood glucose-lowering drug? or blood sugar-lowering drug?
SR1 OR S2 OR S3
Limiters - Published Date: 20100101-20210331
Declarations
Funding
Tiyi Morris has been funded through a National Institute for Health Research Applied Research Collaborations North Thames PhD studentship. The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
Conflicts of interest/competing interests
Tiyi Morris, Fiona Aspinal, Jean Ledger, Keyi Li and Manuel Gomes have no conflicts of interest that are directly relevant to the content of this article.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Authors’ contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by TM, FA, KL and MG. The first draft of the manuscript was written by TM and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Contributor Information
Tiyi Morris, Email: tiyi.morris@ucl.ac.uk.
Fiona Aspinal, Email: f.aspinal@ucl.ac.uk.
Jean Ledger, Email: j.ledger@ucl.ac.uk.
Keyi Li, Email: keyi.li.19@ucl.ac.uk.
Manuel Gomes, Email: m.gomes@ucl.ac.uk.
References
- 1.Thomason J. Big tech, big data and the new world of digital health. Glob Health J. 2021;5(4):165–168. doi: 10.1016/j.glohj.2021.11.003. [DOI] [Google Scholar]
- 2.Wang Y, et al. Effectiveness of mobile health interventions on diabetes and obesity treatment and management: systematic review of systematic reviews. JMIR Mhealth Uhealth. 2020;8(4):e15400. doi: 10.2196/15400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cui M, et al. T2DM self-management via smartphone applications: a systematic review and meta-analysis. PLoS One. 2016;11(11):e0166718. doi: 10.1371/journal.pone.0166718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kerr D, King F, Klonoff DC. Digital health interventions for diabetes: everything to gain and nothing to lose. Diabetes Spectr. 2019;32(3):226. doi: 10.2337/ds18-0085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Villalobos N, Vela FS, Hernandez LM. Digital healthcare intervention to improve self-management for patients with type 2 diabetes: a scoping review. J Sci Innov Med. 2020;3(3), p.21
- 6.Seuring T, Archangelidi O, Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics. 2015;33(8):811–831. doi: 10.1007/s40273-015-0268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rinaldi G, Hijazi A, Haghparast-Bidgoli H. Cost and cost-effectiveness of mHealth interventions for the prevention and control of type 2 diabetes mellitus: a systematic review. Diabetes Res Clin Pract. 2020;162:108084. doi: 10.1016/j.diabres.2020.108084. [DOI] [PubMed] [Google Scholar]
- 8.Drummond M. Economic evaluation of medical devices. In: Hamilton JH, editor. Oxford encyclopedia of economics and finance. Oxford: Oxford University Press; 2018.
- 9.Morris T, Ledger J, Aspinal F, et al. The impact of digital health innovations for the management of type II diabetes: a systematic review. PROSPERO 2020 CRD42020172621. 2020. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD4202017262. Accessed 11 May 2020.
- 10.Ouzzani M, et al. Rayyan: a web and mobile app for systematic reviews. Syst Rev. 2016;5(210):1–10. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The EndNote Team. EndNote. Philadelphia: Clarivate; 2013.
- 12.Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC Methods Programme. 2006, DOI: 10.13140/2.1.1018.4643
- 13.Sterne JA, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fico G, et al. User centered design to improve information exchange in diabetes care through eHealth: results from a small scale exploratory study. J Med Syst. 2020;44(1):2. doi: 10.1007/s10916-019-1472-5. [DOI] [PubMed] [Google Scholar]
- 15.Gordon LG, et al. A cost-effectiveness analysis of a telephone-linked care intervention for individuals with type 2 diabetes. Diabetes Res Clin Pract. 2014;104(1):103–111. doi: 10.1016/j.diabres.2013.12.032. [DOI] [PubMed] [Google Scholar]
- 16.Kempf K, et al. Efficacy of the telemedical lifestyle intervention program TeLiPro in advanced stages of type 2 diabetes: a randomized controlled trial. Diabetes Care. 2017;40(7):863–871. doi: 10.2337/dc17-0303. [DOI] [PubMed] [Google Scholar]
- 17.Luley C, et al. Weight loss in obese patients with type 2 diabetes: effects of telemonitoring plus a diet combination: the Active Body Control (ABC) Program. Diabetes Res Clin Pract. 2011;91(3):286–292. doi: 10.1016/j.diabres.2010.11.020. [DOI] [PubMed] [Google Scholar]
- 18.Roelofsen Y, et al. Demographical, clinical, and psychological characteristics of users and nonusers of an online platform for T2DM patients (e-VitaDM-3/ZODIAC-44) J Diabetes Res. 2016;2016:6343927. doi: 10.1155/2016/6343927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu Z, et al. Internet-based medication management services improve glycated hemoglobin levels in patients with type 2 diabetes. Telemed J E Health. 2021;27(6):686–693. doi: 10.1089/tmj.2020.0123. [DOI] [PubMed] [Google Scholar]
- 20.Maxwell LG, et al. Evaluation of the impact of a pharmacist-led telehealth clinic on diabetes-related goals of therapy in a veteran population. Pharmacotherapy. 2016;36(3):348–356. doi: 10.1002/phar.1719. [DOI] [PubMed] [Google Scholar]
- 21.Menon A, et al. A comparison of characteristics of patients seen in a tertiary hospital diabetes telehealth service versus specialist face-to-face outpatients. J Telemed Telecare. 2017;23(10):842–849. doi: 10.1177/1357633X17733295. [DOI] [PubMed] [Google Scholar]
- 22.Al Hayek A, Robert AA, Al DM. Impact of the FreeStyle Libre flash glucose monitoring system on diabetes: self-management practices and glycemic control among patients with type 2 diabetes in Saudi Arabia: a prospective study. Diabetes Metab Syndr. 2021;15(2):557–563. doi: 10.1016/j.dsx.2021.02.027. [DOI] [PubMed] [Google Scholar]
- 23.Gilmer T, et al. Cost-effectiveness of a technology-enhanced diabetes care management program in Mexico. Value Health Reg Issues. 2019;20:41–46. doi: 10.1016/j.vhri.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 24.Li J, et al. Cost-effectiveness of facilitated access to a self-management website, compared to usual care, for patients with type 2 diabetes (help-diabetes): randomized controlled trial. J Med Internet Res. 2018;20(6):e9256. doi: 10.2196/jmir.9256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agarwal P, et al. Mobile App for improved self-management of type 2 diabetes: multicenter pragmatic randomized controlled trial. JMIR mHealth uHealth. 2019;7(1):e10321. doi: 10.2196/10321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arora S, et al. Trial to examine text message-based mHealth in emergency department patients with diabetes (TExT-MED): a randomized controlled trial. Ann Emerg Med. 2014;63(6):745–54.e6. doi: 10.1016/j.annemergmed.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 27.Katz R, Mesfin T, Barr K. Lessons from a community-based mHealth diabetes self-management program: "It's not just about the cell phone". J Health Commun. 2012;17(Suppl. 1):67–72. doi: 10.1080/10810730.2012.650613. [DOI] [PubMed] [Google Scholar]
- 28.Yu K, et al. Longitudinal effects of an intergenerational mHealth program for older type 2 diabetes patients in rural Taiwan. Diabetes Educator. 2020;46(2):206–216. doi: 10.1177/0145721720907301. [DOI] [PubMed] [Google Scholar]
- 29.Fountoulakis S, et al. Impact and duration effect of telemonitoring on EtabA1c, BMI and cost in insulin-treated diabetes mellitus patients with inadequate glycemic control: a randomized controlled study. Hormones. 2015;14(4):632–643. doi: 10.14310/horm.2002.1603. [DOI] [PubMed] [Google Scholar]
- 30.McGloin H, et al. Patient empowerment using electronic telemonitoring with telephone support in the transition to insulin therapy in adults with type 2 diabetes: observational, pre-post, mixed methods study. J Med Internet Res. 2020;22(5):e16161. doi: 10.2196/16161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Musacchio N, et al. Impact of a chronic care model based on patient empowerment on the management of type 2 diabetes: effects of the SINERGIA programme. Diabet Med. 2011;28(6):724–730. doi: 10.1111/j.1464-5491.2011.03253.x. [DOI] [PubMed] [Google Scholar]
- 32.Wild S, et al. The impact of supported telemetric monitoring in people with type 2 diabetes: study protocol for a randomised controlled trial. Trials. 2013;14:198. doi: 10.1186/1745-6215-14-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lorig K, et al. Benefits of diabetes self-management for health plan members: a 6-month translation study. J Med Internet Res. 2016;18(6):e164. doi: 10.2196/jmir.5568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nicolucci A, et al. A randomized trial on home telemonitoring for the management of metabolic and cardiovascular risk in patients with type 2 diabetes. Diabetes Technol Ther. 2015;17(8):563–570. doi: 10.1089/dia.2014.0355. [DOI] [PubMed] [Google Scholar]
- 35.Warren R, et al. Effects of telemonitoring on glycaemic control and healthcare costs in type 2 diabetes: a randomised controlled trial. J Telemed Telecare. 2018;24(9):586–595. doi: 10.1177/1357633X17723943. [DOI] [PubMed] [Google Scholar]
- 36.Majithia AR, et al. Glycemic outcomes in adults with type 2 diabetes participating in a continuous glucose monitor-driven virtual diabetes clinic: prospective trial. J Med Internet Res. 2020;22(8):e21778. doi: 10.2196/21778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carpenter R, DiChicchio T, Barker K. Interventions for self-management of type 2 diabetes: an integrative review. Int J Nurs Sci. 2019;6:70–91. doi: 10.1016/j.ijnss.2018.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Poduval S, et al. Feasibility, acceptability, and impact of a web-based structured education program for type 2 diabetes: real-world study. JMIR Diabetes. 2020;5(1):e15744. doi: 10.2196/15744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gomes M, Murray E, Raftery, J. Economic Evaluation of Digital Health Interventions: Methodological Issues and Recommendations for Practice. PharmacoEconomics 40, 367–378 (2022). 10.1007/s40273-022-01130-0 [DOI] [PMC free article] [PubMed]