Abstract
This short review aimed at (i) providing an update on the health benefits associated with melatonin supplementation, while (ii) considering future potential research directions concerning melatonin supplementation use relative to Coronavirus disease of 2019 (COVID-19). A narrative review of the literature was undertaken to ascertain the effect of exogenous melatonin administration on humans. Night-time melatonin administration has a positive impact on human physiology and mental health. Indeed, melatonin (i) modulates the circadian components of the sleep-wake cycle; (ii) improves sleep efficiency and mood status; (iii) improves insulin sensitivity; and (iv) reduces inflammatory markers and oxidative stress. Melatonin has also remarkable neuroprotective and cardioprotective effects and may therefore prevent deterioration caused by COVID-19. We suggest that melatonin could be used as a potential therapy in the post-COVID-19 syndrome, and therefore call for action the research community to investigate on the potential use of exogenous melatonin to enhance the quality of life in patients with post-COVID-19 syndrome.
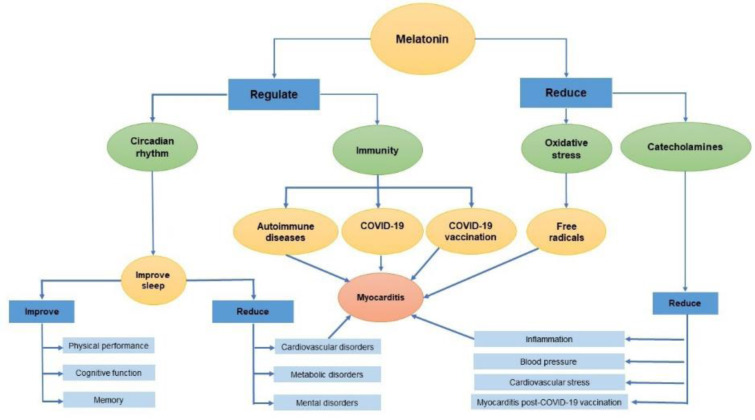
See also Figure 1(Fig. 1).
Keywords: antioxidant status, cytokines, dose, free radicals, stress
Introduction
Melatonin is an indoleamine produced by the pineal gland in humans (Ackermann and Stehle, 2006[4]; Arendt, 2006[16]; Zawilska et al., 2006[160]). Its regulation is impacted by dark-light and both seasonal, and lunar cycles (Arendt and Broadway, 1987[17]; Dergaa et al., 2019[40]; Dergaa et al., 2021[42]; Nelson et al., 2015[109]). Melatonin secretion decreases progressively with advancing age, resulting in a reduction in sleep duration (Iguchi et al., 1982[69]). Endogenous melatonin levels are known to decrease substantially after 40 years, and this decline can be causally linked to lowered sleep efficacy (Haimov et al., 1994[66]; Pierpaoli et al., 1995[117]), eventually affecting physical and mental health (Karasek, 2004[73]). Exogenous melatonin supplementation may potentially have beneficial effects on sleep as well as age-related diseases (Karasek, 2004[73]). Therefore, the potential role of melatonin supplementation in the prevention and/or treatment of insomnia and age-related diseases is promising. Importantly, at least for short regimens, melatonin supplementation in humans is safe, as demonstrated by preclinical and clinical data (Colella et al., 2016[30]; Minich et al., 2022[103]; Sánchez-Barceló et al., 2010[131]).
Interestingly, the high levels of melatonin concentration in children may be a contributing factor to their high protection against the coronavirus disease of 2019 (COVID-19) (Shneider et al., 2020[134]). Indeed, endogenous melatonin seems to play a key role in suppressing COVID-19 infections. Therefore, melatonin supplementation may have a variety of health benefits, including improved quality of life and cost savings in healthcare, and may help prevent complications associated with COVID-19 (Giri et al., 2021[62]; Ramos et al., 2021[120]). However, for years, data obtained in animals have been uncritically extrapolated to humans (Kennaway, 2019[74]).
Thus, the purposes of this narrative review were to (i) summarize recent findings regarding melatonin supplementation in humans and its clinical implications; and (ii) provide some suggestions on what future research in the field should focus on.
Treatment of Sleep Disorders with Exogenous Melatonin
The primary physiological function of melatonin is to inform the human body about the diurnal light/dark cycle and to synchronize the central and peripheral oscillators located in tissues and organs (Khullar, 2012[75]; Rong et al., 2020[129]). Melatonin secretion is widely regarded as the best known indicator of the circadian body clock's state (Folkard, 2008[56]). Importantly, the circadian clock system is critical for homeostasis and human health maintenance (Pickel and Sung, 2020[116]; Van Someren, 2000[152]). Specifically, melatonin exerts chronobiotic effects by stimulating G protein-dependent receptors types 1 and 2 (Khullar, 2012[75]; Slominski et al., 2012[135]). This function is critical because disruptions in circadian rhythm can increase the risk of metabolic, cardiovascular, and/or mental diseases, as well as result in poorer health outcomes (Aly and Rizk, 2018[9]; Hacışevki and Baba, 2018[65]).
Consequently, exogenous melatonin supplementation has been proven to be effective at restoring sleep-wake cycles and enhancing sleep quality, and is frequently used as a medication to treat sleep disorders, such as sleeplessness and jet lag syndrome (Laudon and Frydman-Marom, 2014[82]). Melatonin increases sleepiness and shortens sleep onset latency by exerting its sedative effect on the central nervous system (Gandolfi et al., 2020[58]; Marseglia et al., 2015[98]; Souissi et al., 2020[140], 2022[138]).
Can Melatonin Improve Cognitive Function?
It has been shown that 1 mg of exogenous melatonin administered at night may be effective in improving sleep quality, memory, and cognitive functioning in elderly people (Peck et al., 2004[114]). It seems that exogenous melatonin is also a useful therapeutic agent in the treatment of mental impairment associated with aging (Peck et al., 2004[114]). In fact, exogenous melatonin is particularly effective in reversing age-related cognitive decline when decreased endogenous melatonin secretion has been detected in patients (Pandi-Perumal et al., 2005[111]).
Endogenous melatonin secretion is decreased in people of advanced age, for instance (Burgess and Fogg, 2008[24]), or lower in those who are blind (Warman et al., 2011[156]), or in patients with neurodegenerative disorders (Rajpoot, 2020[119]). Consequently, melatonin treatment in these populations resulted in a significant improvement of the clinical and neurophysiological aspects of rapid eye movement and sleep behavior disorders in blind populations (Warman et al., 2011[156]), and in elderly patients with underlying neurodegenerative disorders (St Louis and Boeve, 2017[142]; Videnovic et al., 2020[154]). In the same context, meta-analysis studies reported that melatonin treatment improved sleep quality in patients with Alzheimer and Parkinson diseases, and it may be used as an exclusive or adjunctive therapy in patients with neurodegenerative disorders and associated behavioral and cognitive function disorders (Ferracioli-Oda et al., 2013[54]; Zhang et al., 2016[163]).
What Is the Beneficial Role of Melatonin in Physical Performance?
The association between physical exercise and melatonin secretion has been well discussed (Escames et al., 2012[49]). Melatonin concentration increases temporarily in the blood during exercise (Carr et al., 1981[27]; Ronkainen et al., 1986[130]; Theron et al., 1984[148]), suggesting that melatonin plays a role during physical exercise (Souissi et al., 2022[137]). However, melatonin supplementation may be beneficial or useless depending on the type of physical exercise (López-Flores et al., 2018[89]).
Sleep and recovery are key components of athletes' health and performance enhancements (Gander et al., 2008[57]; Walsh et al., 2021[155]). According to a recent study (Kruk et al., 2021[78]), athletes frequently use sleep-enhancing supplements. In this regard, melatonin is among the most commonly used supplement due to its wide-range effects on the organism, including, but not limited to, its antioxidant properties that protect muscles and mitochondria from oxidative stress (Liesa and Shirihai, 2013[86]). Furthermore, exogenous melatonin has been proven to be an effective antioxidant and anti-inflammatory agent, eventually maintaining mitochondrial function (Hu et al., 2019[68]), as well as muscular strength and adaptability during heavy exercise (Borges et al., 2015[22]; Ochoa et al., 2011[110]; Trionfante et al., 2017[151]). It has been recently shown that melatonin supplementation during congested training periods can enhance antioxidant status and glucose resistance in different types of training, including soccer training camps and resistance training athletes (Farjallah et al., 2022[52]; Leonardo-Mendonça et al., 2017[84]; Souissi et al., 2022[136]).
Endurance exercise consumes glucose, resulting in a decrease in muscle and liver glycogen stores (Trefts et al., 2015[150]). For ATP synthesis, melatonin can partly shift glucose metabolism from anaerobic glycolysis to aerobic mitochondrial oxidative phosphorylation, and consequently result in decreased lactate production (Mazepa et al., 1999[100]; Sayed et al., 2018[133]). Therefore, pre-exercise melatonin administration can enhance lipid utilization as a substrate energy source (Mazepa et al., 1999[100]; Souissi et al., 2022[136]; Trionfante et al., 2017[151]). Future studies should investigate the relationship between melatonin secretion/supplementation and the body mass index, and why not considering melatonin as a potential way to help patients with obesity to optimize the outcome of their exercise programs.
Can Melatonin Improve Mood Status?
Environmental disruptions of circadian rhythms, including the sleep-wake cycle, can result in mood-related perturbations in susceptible people (Altun and Ugur‐Altun, 2007[7]; Germain and Kupfer, 2008[59]; Ghazel et al., 2022[60]; Monteleone and Maj, 2008[105]), and in athletes (Romdhani et al., 2019[127]). Indeed, numerous preclinical and clinical findings have suggested a strong link between circadian rhythms, melatonin secretion dysregulation, and mood regulation (Altun and Ugur‐Altun, 2007[7]; Etain et al., 2011[50]; Germain and Kupfer, 2008[59]; Lanfumey et al., 2013[81]; Lerner and Nordlund, 1978[85]; McClung, 2011[101]; Monteleone and Maj, 2008[105]; Monteleone et al., 2011[106]; Munk-Jørgensen, 2014[108]).
Exogenous melatonin ingestion has a favorable clinical response for reducing sleep difficulties or improving health problems associated with circadian rhythms disruption, which may be prevalent in the symptomatology of mood disorders (Coogan and Thome, 2011[31]; Maldonado et al., 2009[94]). A prospective observational study identified that exogenous melatonin consumption improved sleep and mood (Livianos et al., 2012[88]). This suggests that its use may be part of a therapeutic toolkit for the treatment of anxiety and depression related to sleep deprivation (Quera Salva and Hartley, 2012[118]; Robillard et al., 2018[124]). In this context, a recent study revealed that salivary melatonin levels were negatively correlated with the severity of depression (Sundberg et al., 2016[146]) and suggested that melatonin could become a clinically useful biomarker of stress, anxiety and depression (Chojnowska et al., 2021[29]; Kudo et al., 2021[79]; Sundberg et al., 2016[146]). The effects of melatonin ingestion on depressive symptoms may represent an interesting area of research in the future.
Can Melatonin Reduce Cardiovascular Risk?
Low blood melatonin levels have been found in a variety of clinical diseases, such as arterial hypertension (Dominguez-Rodriguez et al., 2014[46]; Jonas et al., 2003[71]; Koziróg et al., 2011[77]), heart failure (Dominguez-Rodriguez et al., 2016[45]; Dzida et al., 2013[48]; Girotti et al., 2003[63]; Kimak et al., 2014[76]), ischemic and heart diseases (Altun et al., 2002[8]; Brugger et al., 1995[23]; Domínguez‐Rodríguez et al., 2002[44]), and cardiovascular related risk conditions such as diabetes mellitus and obesity (Mäntele et al., 2012[97]; McMullan et al., 2013[102]). In this context, exogenous melatonin has been shown to be beneficial to reduce the internal carotid arteries' pulsatility index and blood clotting (Del Zar et al., 1990[33][34]), and to decrease catecholamine levels in the blood (Arangino et al., 1999[15]; Souissi et al., 2021[139]). Indeed, a negative correlation between endogenous melatonin levels and cardiovascular diseases has been reported (Dominguez‐Rodriguez et al., 2010[47]). The potential therapeutic involvement of melatonin in the pathophysiology of coronary artery disease is being increasingly acknowledged (Jiki et al., 2018[70]; Pandi-Perumal et al., 2016[112]). Furthermore, due to its direct free radical scavenging activity, melatonin appears to have cardioprotective benefits (Dominguez-Rodriguez, 2012[43]; Paulis and Šimko, 2007[113]; Reiter et al., 2010[123]; Sun et al., 2016[145]). The cardiovascular protective action of melatonin supplementation is particularly promising for cardiovascular disorders (Jiki et al., 2018[70]) and exercise-induced cardiovascular fatigue (Souissi et al., 2021[139]) amongst others.
Additionally, we would like to highlight that the sudden cardiac arrests caused by COVID-19 infection depend primarily on the damage inflammation and the cytokine storm induced by the host immune reaction (Tan and Reiter, 2022[147]; Zhang et al., 2020[161]). In this case, melatonin could be used to downregulate the overreaction of the immune system, potentially suppressing/dampening the inflammation and reducing the risk of mortality (Tan and Reiter, 2022[147]). Larger clinical trials are therefore needed to determine the efficacy of melatonin supplementation as a novel preventive intervention in cardiovascular disorders (in the pathophysiology of coronary artery disorder, arterial hypertension, congestive heart failure, COVID-19, and cardiovascular fatigue induced by exercise) in humans.
Can Melatonin Be Utilized to Treat Respiratory Disease and Viral Infections?
Melatonin has been successfully used to treat respiratory disease and viral infections (Reiter et al., 2020[122]), with its beneficial effects on acute respiratory stress caused by viruses and bacteria being identified (Wu et al., 2019[158]; Yip et al., 2013[159]). Although melatonin is not viricidal, it has indirect anti-viral actions (Reiter et al., 2020[122]) owing to its antioxidative, anti-inflammatory, and immune-enhancing properties (Anderson et al., 2015[13]; Boga et al., 2012[20]; Lee and Glickman, 2021[83]; Reiter et al., 2020[121]). Melatonin use resulted in lowered viremia, decreased viral load, and decreased paralysis and death (Bonilla et al., 2004[21]). Moreover, melatonin has been proven to suppress the effects of viral infections in several conditions (Bahrampour Juybari et al., 2020[19]). In previous respiratory syncytial virus models, melatonin ingestion resulted in a downregulation of acute lung oxidative injury, pro-inflammatory cytokine release, and inflammatory cell recruitment (Zhang et al., 2020[162]). These findings, along with those summarized by Reiter et al. (2020[122]), support the rationale use of melatonin supplementation for respiratory viral diseases.
Can Melatonin Boost the Immune Response?
The ability of melatonin to influence the immune response is one of its most intriguing properties (Carrillo-Vico et al., 2013[28]; Kurhaluk and Tkachenko, 2020[80]). Some decades ago, the first evidence that melatonin could boost antibody production and reverse the immunosuppressive impact of corticosteroids and/or acute stress was reported (Maestroni et al., 1987[91]; Maestroni, 2001[92]). The immunoregulatory role of melatonin has recently been well established (Kurhaluk and Tkachenko, 2020[80]; Mańka and Majewska, 2016[96]). Melatonin may operate as an immunological buffer, boosting the immune response in basal or immunosuppressive situations or acting as an anti-inflammatory agent in the context of excessive immune responses (Carrillo-Vico et al., 2013[28]; Mortezaee et al., 2019[107]). Although, it has been recently shown that melatonin could be used to treat some autoimmune diseases, such as multiple sclerosis (Farez et al., 2016[51]) and autoimmune thyroid diseases (D'Angelo et al., 2016[32]), more investigations are warranted to confirm its potential promising therapeutic use (Zhao et al., 2019[164]).
Interestingly, exogenous melatonin treatment may significantly enhance the strength and persistence of the immunological response elicited by the severe COVID-19 (Wichniak et al., 2021[157]). Additionally, it has been shown that the antioxidant properties of melatonin and its pleiotropic effect on the immune system may help reduce some of the deleterious side effects of the COVID-19 vaccination (Maestroni, 2020[90]). It would be possible that melatonin treatment could be more beneficial in elderly people with sleep disorders. So far, the available information suggests that melatonin has a broad capacity to increase both cell-mediated and humoral immune responses regardless of sex or age (Maestroni, 2020[90]).
Can Melatonin Aid Mitigate the Harmful Effects of the COVID-19 Epidemic?
COVID-19, designated a public health emergency and a global threat of international concern by the World Health Organization, is one of the most worrisome diseases in recent history, with a clear 2020-lockdowns disruption observed in most countries globally (Dergaa et al., 2022[41][39]; Ghram et al., 2021[61]; Mohammed, 2020[104]; Varma et al., 2021[153]). As of January 23, 2022, severe acute respiratory syndrome coronavirus 2 is estimated to have infected globally approximately 663640386 people so far, with 6713093 estimated deaths (https://covid19.who.int/). The stringent public health measures, although effective in reducing person-to-person transmission of COVID-19 (Dergaa et al., 2021[36], 2022[37][38][41][39]) have been shown to negatively impact individuals' lifestyle behaviors (eg; physical activity levels, sleep/wake behaviors, diet) (Ammar et al., 2020[10], 2021[11]; Dergaa et al., 2022[37][41]; Romdhani et al., 2022[125][126][128]; Trabelsi et al., 2021[149]), their mental wellbeing and mood state (Akbari et al., 2021[6]).
Since, endogenous melatonin levels were reduced in patients with COVID-19 infection (Anderson and Reiter, 2020[14]; Attademo and Bernardini, 2021[18]), melatonin has been researched for its potential role in COVID-19 infected patients (Golombek et al., 2022[64]; Zhang et al., 2020[162]). Indeed, melatonin treatment may help mitigate the harmful effects of the COVID-19 epidemic on sleep and mental health (Lee and Glickman, 2021[83]; Wichniak et al., 2021[157]). In addition, the anti-inflammation, antioxidant, and immune enhancing actions of melatonin potential support its potential attenuation of COVID-19 infection (Zhang et al., 2020[162]). Melatonin seems to play a key role in suppressing COVID-19 infection (Martín Giménez et al., 2020[99]). The results of the research projects regarding the melatonin effect on COVID-19 patients are indeed very promising.
Can Melatonin Reduce the Severity of Post-COVID-19 Syndrome?
Importantly, it has been shown that more than 60 % of COVID-19 survivors experienced post-COVID-19 syndrome (PC19S) (Fernández-de-Las-Peñas et al., 2021[53]). However, contrary to the symptoms and complications of acute COVID-19 that are well established, the sequelae induced by the PC19S need more studies (Malik et al., 2022[95]). So far, patients with PC19Ss have been reported to have persistent symptoms and a poor quality of life (Malik et al., 2022[95]). The exact pathophysiological mechanisms explaining the PC19S are not well understood due to their multifactorial properties. However, since the major serious persistent symptoms highlighted after the infections were sleep disturbance, fatigue, anxiety, depression and/or mental impairment (Malik et al., 2022[95]), one could speculate that endogenous melatonin disturbance is a potential factor contributing to the long-term consequences of COVID-19 infection (Magdy et al., 2022[93]).
Furthermore, it has been recently shown that severe PC19S was associated with radiological evidence of cardiac damage (myocarditis: cause of mortality) (Dennis et al., 2021[35]). Mechanisms explaining myocarditis in patients with PC19S remain unclear (Ackermann et al., 2020[5]; Dennis et al., 2021[35]). However, it is evident that myocarditis has been associated with several factors, particularly with older age (Dennis et al., 2021[35]). In fact, aging is associated with increased oxidative stress (Abete et al., 1999[3]; Ferrucci and Fabbri, 2018[55]), and decreased endogenous protective mechanisms (Abete et al., 1997[1], 2001[2]), including decreased melatonin production (Dominguez‐Rodriguez et al., 2010[47]). Briefly, inflammaging (chronic inflammation in aging) is the main factor of myocarditis (Ferrucci and Fabbri, 2018[55]; Soysal et al., 2020[141]). Therefore, inflammaging associated with PC19S are potential factors for increasing the risk of myocarditis and weakening the immune system efficiency (Soysal et al., 2020[141]).
Melatonin ingestion could reduce the severity of PC19S-inducing myocarditis by attenuating aging and inhibiting the production of inflammatory cytokines (Su et al., 2022[144]). Furthermore, it has been shown that melatonin supplementation significantly improved coxsackie-virus B3-inducing myocarditis in mouse hearts (Sang et al., 2018[132]). Sang et al. (2018[132]) suggested that melatonin could be a promising new therapeutic approach against viral myocarditis. It would be interesting in the future to assay the effect of melatonin supplementation against COVID-19-inducing myocarditis in human hearts.
On the other hand, numerous studies have demonstrated the beneficial effects of exogenous melatonin on mental health and sleep (Lim et al., 2022[87]). Effective sleep disturbance management and early sensorium correction are reported to be critical in preventing post-intensive care syndrome and lowering morbidity (Hashmi et al., 2017[67]). Although evidence regarding the impact of exogenous melatonin on PC19S is lacking, its efficacy and safety have been repeatedly demonstrated in humans (Buscemi et al., 2006[25]), and we expect that its use by patients with PC19Ss would be highly beneficial. The present review is therefore a call to action for public health to explore the effect of exogenous melatonin on PC19S patients.
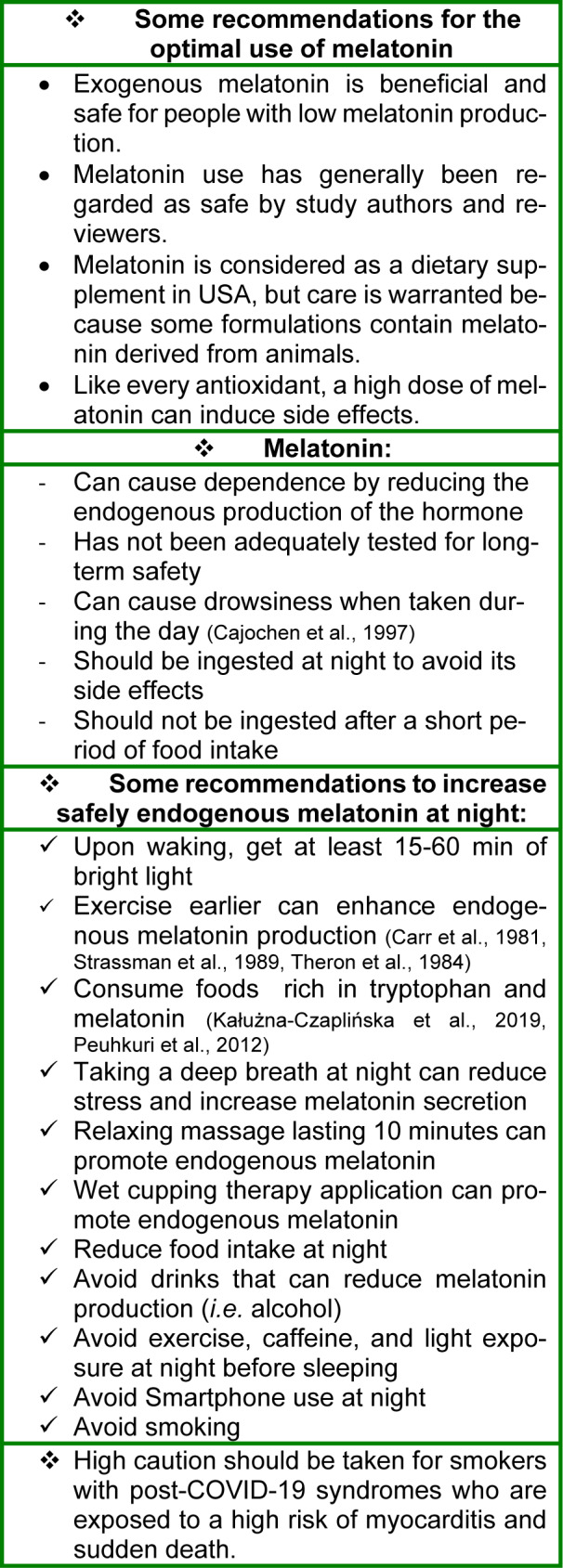
Finally, we highlight that exogenous melatonin may present some side effects for some populations (pregnant and breast-feeding women) (Andersen et al., 2016[12]), and should not be consumed at high doses and/or for long time as we do not know the long-term endocrine effects of melatonin administration (Minich et al., 2022[103]). Therefore, it is important that we suggest some recommendations based on expert knowledge and scientific research for optimizing health and offer concrete steps for increasing endogenous melatonin (Table 1(Tab. 1); References in Table 1: Cajochen et al., 1997[26]; Carr et al., 1981[27]; Kałużna-Czaplińska et al., 2019;[72] Peuhkuri et al., 2012[115]; Strassman et al., 1989[143]; Theron et al., 1984[148]).
Table 1. Fight Coronavirus disease of 2019 (COVID-19) and boost immunity by increasing endogenous melatonin levels. Concrete tips for increasing endogenous melatonin and promoting sleep.
Conclusions
Exogenous melatonin supplementation may improve sleep efficiency, mood status, and cognitive performance. In addition, it may have potential therapeutic use in mental health and cardiovascular disorders. At present, melatonin is known to potentially attenuate the COVID-19 infection through its anti-inflammatory, antioxidant, and immune-enhancing properties. We call for research on the potential beneficial use of melatonin in patients with PC19S.
Notes
Mohamed Romdhani and Amine Ghram contributed equally as third author.
Karim Chamari and Helmi Ben Saad contributed equally as last author.
Conflict of interest
The authors declare that they have no competing interests.
Figure 1. Graphical abstract.
References
- 1.Abete P, Ferrara N, Cacciatore F, Madrid A, Bianco S, Calabrese C, et al. Angina-induced protection against myocardial infarction in adult and elderly patients: a loss of preconditioning mechanism in the aging heart? J Am Coll Cardiol. 1997;30:947–954. doi: 10.1016/s0735-1097(97)00256-8. [DOI] [PubMed] [Google Scholar]
- 2.Abete P, Ferrara N, Cacciatore F, Sagnelli E, Manzi M, Carnovale V, et al. High level of physical activity preserves the cardioprotective effect of preinfarction angina in elderly patients. J Am Coll Cardiol. 2001;38:1357–1365. doi: 10.1016/s0735-1097(01)01560-1. [DOI] [PubMed] [Google Scholar]
- 3.Abete P, Napoli C, Santoro G, Ferrara N, Tritto I, Chiariello M, et al. Age-related decrease in cardiac tolerance to oxidative stress. J Mol Cell Cardiol. 1999;31:227–236. doi: 10.1006/jmcc.1998.0862. [DOI] [PubMed] [Google Scholar]
- 4.Ackermann K, Stehle JH. Melatonin synthesis in the human pineal gland: advantages, implications, and difficulties. Chronobiol Int. 2006;23:369–379. doi: 10.1080/07420520500464379. [DOI] [PubMed] [Google Scholar]
- 5.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020;383:120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akbari H, Pourabbas M, Yoosefi M, Briki W, Attaran S, Mansoor H, et al. How physical activity behavior affected well-being, anxiety and sleep quality during COVID-19 restrictions in Iran. Eur Rev Med Pharmacol Sci. 2021;25:7847–7857. doi: 10.26355/eurrev_202112_27632. [DOI] [PubMed] [Google Scholar]
- 7.Altun A, Ugur‐Altun B. Melatonin: therapeutic and clinical utilization. Int J Clin Pract. 2007;61:835–845. doi: 10.1111/j.1742-1241.2006.01191.x. [DOI] [PubMed] [Google Scholar]
- 8.Altun A, Yaprak M, Aktoz M, Vardar A, Betul U-A, Ozbay G. Impaired nocturnal synthesis of melatonin in patients with cardiac syndrome X. Neurosci Lett. 2002;327:143–145. doi: 10.1016/s0304-3940(02)00368-3. [DOI] [PubMed] [Google Scholar]
- 9.Aly HF, Rizk MZ. Melatonin and its indisputable effects on the health state. melatonin-molecular biology, clinical and pharmaceutical approaches. London: IntechOpen; 2018. [Google Scholar]
- 10.Ammar A, Mueller P, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Psychological consequences of COVID-19 home confinement: The ECLB-COVID19 multicenter study. PloS One. 2020;15(11):e0240204. doi: 10.1371/journal.pone.0240204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ammar A, Trabelsi K, Brach M, Chtourou H, Boukhris O, Masmoudi L, et al. Effects of home confinement on mental health and lifestyle behaviours during the COVID-19 outbreak: insights from the ECLB-COVID19 multicentre study. Biol Sport. 2021;38(1):9–21. doi: 10.5114/biolsport.2020.96857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andersen LP, Gögenur I, Rosenberg J, Reiter RJ. The safety of melatonin in humans. Clin Drug Invest. 2016;36:169–175. doi: 10.1007/s40261-015-0368-5. [DOI] [PubMed] [Google Scholar]
- 13.Anderson G, Maes M, Markus RP, Rodriguez M. Ebola virus: melatonin as a readily available treatment option. J Med Virol. 2015;87:537–543. doi: 10.1002/jmv.24130. [DOI] [PubMed] [Google Scholar]
- 14.Anderson G, Reiter RJ. Melatonin: roles in influenza, Covid‐19, and other viral infections. Rev Med Virol. 2020;30(3):e2109. doi: 10.1002/rmv.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arangino S, Cagnacci A, Angiolucci M, Vacca AM, Longu G, Volpe A, et al. Effects of melatonin on vascular reactivity, catecholamine levels, and blood pressure in healthy men. Am J Cardiol. 1999;83:1417–1419. doi: 10.1016/s0002-9149(99)00112-5. [DOI] [PubMed] [Google Scholar]
- 16.Arendt J. Melatonin and human rhythms. Chronobiol Int. 2006;23:21–37. doi: 10.1080/07420520500464361. [DOI] [PubMed] [Google Scholar]
- 17.Arendt J, Broadway J. Light and melatonin as zeitgebers in man. Chronobiol Int. 1987;4:273–282. doi: 10.3109/07420528709078534. [DOI] [PubMed] [Google Scholar]
- 18.Attademo L, Bernardini F. Are dopamine and serotonin involved in COVID-19 pathophysiology? Eur J Psychiatry. 2021;35(1):62. doi: 10.1016/j.ejpsy.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bahrampour Juybari K, Pourhanifeh MH, Hosseinzadeh A, Hemati K, Mehrzadi S. Melatonin potentials against viral infections including COVID-19: Current evidence and new findings. Virus Res. 2020;287:198108. doi: 10.1016/j.virusres.2020.198108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boga JA, Coto‐Montes A, Rosales‐Corral SA, Tan DX, Reiter RJ. Beneficial actions of melatonin in the management of viral infections: a new use for this “molecular handyman”? Rev Med Virol. 2012;22:323–338. doi: 10.1002/rmv.1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bonilla E, Valero N, Chacín‐Bonilla L, Medina‐Leendertz S. Melatonin and viral infections. J Pineal Res. 2004;36(2):73–79. doi: 10.1046/j.1600-079X.2003.00105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Borges LdS, Dermargos A, Junior EPdS, Weimann E, Lambertucci RH, Hatanaka E. Melatonin decreases muscular oxidative stress and inflammation induced by strenuous exercise and stimulates growth factor synthesis. J Pineal Res. 2015;58:166–172. doi: 10.1111/jpi.12202. [DOI] [PubMed] [Google Scholar]
- 23.Brugger P, Marktl W, Herold M. Impaired nocturnal secretion of melatonin in coronary heart disease. Lancet. 1995;345(8962):1408. doi: 10.1016/s0140-6736(95)92600-3. [DOI] [PubMed] [Google Scholar]
- 24.Burgess HJ, Fogg LF. Individual differences in the amount and timing of salivary melatonin secretion. PloS One. 2008;3(8):e3055. doi: 10.1371/journal.pone.0003055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buscemi N, Vandermeer B, Hooton N, Pandya R, Tjosvold L, Hartling L, et al. Efficacy and safety of exogenous melatonin for secondary sleep disorders and sleep disorders accompanying sleep restriction: meta-analysis. BMJ. 2006;332(7538):385–393. doi: 10.1136/bmj.38731.532766.F6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cajochen C, Kräuchi K, Wirz-Justice A. The acute soporific action of daytime melatonin administration: effects on the EEG during wakefulness and subjective alertness. J Biol Rhythms. 1997;12:636–643. doi: 10.1177/074873049701200619. [DOI] [PubMed] [Google Scholar]
- 27.Carr D, Reppert S, Bullen B, Skrinar G, Beitins I, Arnold M, et al. Plasma melatonin increases during exercise in women. J Clin Endocrinol Metab. 1981;53(1):224–225. doi: 10.1210/jcem-53-1-223. [DOI] [PubMed] [Google Scholar]
- 28.Carrillo-Vico A, Lardone PJ, Álvarez-Sánchez N, Rodríguez-Rodríguez A, Guerrero JM. Melatonin: buffering the immune system. Int J Mol Sci. 2013;14:8 638–8 683. doi: 10.3390/ijms14048638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chojnowska S, Ptaszyńska-Sarosiek I, Kępka A, Knaś M, Waszkiewicz N. Salivary biomarkers of stress, anxiety and depression. J Clin Med. 2021;10(3):517. doi: 10.3390/jcm10030517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Colella M, Biran V, Baud O. Melatonin and the newborn brain. Early Hum Dev. 2016;102:1–3. doi: 10.1016/j.earlhumdev.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 31.Coogan AN, Thome J. Chronotherapeutics and psychiatry: setting the clock to relieve the symptoms. World J Biol Psychiatry. 2011;12(Suppl 1):40–43. doi: 10.3109/15622975.2011.598389. [DOI] [PubMed] [Google Scholar]
- 32.D’Angelo G, Marseglia L, Manti S, Colavita L, Cuppari C, Impellizzeri P, et al. Atopy and autoimmune thyroid diseases: melatonin can be useful? Ital J Pediatrics. 2016;42(1):95. doi: 10.1186/s13052-016-0305-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Del Zar MdlM, Martinuzzo M, Cardinali DP, Carreras LO, Vacas MI. Diurnal variation in melatonin effect on adenosine triphosphate and serotonin release by human platelets. Eur J Endocrinol. 1990;123:453–458. doi: 10.1530/acta.0.1230453. [DOI] [PubMed] [Google Scholar]
- 34.Del Zar MM, Martinuzzo M, Falcón C, Cardinali DP, Carreras LO, Vacas MI. Inhibition of human platelet aggregation and thromboxane-B2 production by melatonin: evidence for a diurnal variation. J Clin Endocrinol Metab. 1990;70:246–251. doi: 10.1210/jcem-70-1-246. [DOI] [PubMed] [Google Scholar]
- 35.Dennis A, Wamil M, Alberts J, Oben J, Cuthbertson DJ, Wootton D, et al. Multiorgan impairment in low-risk individuals with post-COVID-19 syndrome: a prospective, community-based study. BMJ Open. 2021;11(3):e048391. doi: 10.1136/bmjopen-2020-048391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dergaa I, Abdelrahman H, Varma A, Yousfi N, Souissi A, Ghram A, et al. COVID-19 vaccination, herd immunity and the transition toward normalcy: challenges with the upcoming sports events. Ann Appl Sport Sci. 2021;9(3):10. [Google Scholar]
- 37.Dergaa I, Abubakera M, Souissi A, Mohammed AR, Varmaa A, Musa S, et al. Age and clinical signs as predictors of COVID-19 symptoms and cycle threshold value. Libyan J Med. 2022;17(1):2010337. doi: 10.1080/19932820.2021.2010337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dergaa I, Ammar A, Souissi A, Fessi MS, Trabelsi K, Glenn JM, et al. COVID-19 lockdown: impairments of objective measurements of selected physical activity, cardiorespiratory and sleep parameters in trained fitness coaches. EXCLI J. 2022;21:1084–1098. doi: 10.17179/excli2022-4986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dergaa I, Ben Saad H, Souissi A, Musa S, Abdulmalik MA, Chamari K. Olympic Games in COVID-19 times: lessons learned with special focus on the upcoming FIFA World Cup Qatar 2022. Br J Sports Med. 2022;56:654–656. doi: 10.1136/bjsports-2021-105276. [DOI] [PubMed] [Google Scholar]
- 40.Dergaa I, Fessi MS, Chaabane M, Souissi N, Hammouda O. The effects of lunar cycle on the diurnal variations of short-term maximal performance, mood state, and perceived exertion. Chronobiol Int. 2019;36:1249–1257. doi: 10.1080/07420528.2019.1637346. [DOI] [PubMed] [Google Scholar]
- 41.Dergaa I, Musa S, Romdhani M, Souissi A, Abdulmalik M, Chamari K, et al. FIFA World Cup 2022: What can we learn from the inspiring Tokyo 2020 Olympic Games held in COVID-19 times? Biol Sport. 2022;39:1073–1080. doi: 10.5114/biolsport.2022.113293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dergaa I, Romdhani M, Fessi MS, Ben Saad H, Varma A, Ben Salem A, et al. Does lunar cycle affect biological parameters in young healthy men? Chronobiol Int. 2021;38:933–940. doi: 10.1080/07420528.2021.1897609. [DOI] [PubMed] [Google Scholar]
- 43.Dominguez-Rodriguez A. Melatonin in cardiovascular disease. Expert Opin Invest Drugs. 2012;21:1593–1596. doi: 10.1517/13543784.2012.716037. [DOI] [PubMed] [Google Scholar]
- 44.Domínguez‐Rodríguez A, Abreu‐González P, García MJ, Sanchez J, Marrero F, Armas‐Trujillo Dd. Decreased nocturnal melatonin levels during acute myocardial infarction. J Pineal Res. 2002;33:248–252. doi: 10.1034/j.1600-079x.2002.02938.x. [DOI] [PubMed] [Google Scholar]
- 45.Dominguez-Rodriguez A, Abreu-Gonzalez P, Piccolo R, Galasso G, Reiter RJ. Melatonin is associated with reverse remodeling after cardiac resynchronization therapy in patients with heart failure and ventricular dyssynchrony. Int J Cardiol. 2016;221:359–363. doi: 10.1016/j.ijcard.2016.07.056. [DOI] [PubMed] [Google Scholar]
- 46.Dominguez-Rodriguez A, Abreu-Gonzalez P, Reiter RJ. The potential usefulness of serum melatonin level to predict heart failure in patients with hypertensive cardiomyopathy. Int J Cardiol. 2014;174:415–417. doi: 10.1016/j.ijcard.2014.04.044. [DOI] [PubMed] [Google Scholar]
- 47.Dominguez‐Rodriguez A, Abreu‐Gonzalez P, Sanchez‐Sanchez JJ, Kaski JC, Reiter RJ. Melatonin and circadian biology in human cardiovascular disease. J Pineal Res. 2010;49:14–22. doi: 10.1111/j.1600-079X.2010.00773.x. [DOI] [PubMed] [Google Scholar]
- 48.Dzida G, Prystupa A, Lachowska-Kotowska P, Kardas T, Kamienski P, Kimak E, et al. Alteration in diurnal and nocturnal melatonin serum level in patients with chronic heart failure. Ann Agric Environ Med. 2013;20:745–748. [PubMed] [Google Scholar]
- 49.Escames G, Ozturk G, Baño‐Otálora B, Pozo MJ, Madrid JA, Reiter RJ, et al. Exercise and melatonin in humans: reciprocal benefits. J Pineal Res. 2012;52(1):1–11. doi: 10.1111/j.1600-079X.2011.00924.x. [DOI] [PubMed] [Google Scholar]
- 50.Etain B, Milhiet V, Bellivier F, Leboyer M. Genetics of circadian rhythms and mood spectrum disorders. Eur Neuropsychopharmacol. 2011;21:S676–S682. doi: 10.1016/j.euroneuro.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 51.Farez MF, Calandri IL, Correale J, Quintana FJ. Anti‐inflammatory effects of melatonin in multiple sclerosis. BioEssays. 2016;38:1016–1026. doi: 10.1002/bies.201600018. [DOI] [PubMed] [Google Scholar]
- 52.Farjallah MA, Ghattassi K, Kamoun A, Graja A, Ben Mahmoud L, Driss T, et al. Melatonin supplementation alleviates cellular damage and physical performance decline induced by an intensive training period in professional soccer players. PloS One. 2022;17(9):e0273719. doi: 10.1371/journal.pone.0273719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fernández-de-Las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, Florencio LL, Cuadrado ML, Plaza-Manzano G, et al. Prevalence of post-COVID-19 symptoms in hospitalized and non-hospitalized COVID-19 survivors: A systematic review and meta-analysis. Eur J Intern Med. 2021;92:55–70. doi: 10.1016/j.ejim.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ferracioli-Oda E, Qawasmi A, Bloch MH. Meta-analysis: melatonin for the treatment of primary sleep disorders. PloS One. 2013;8(5):e63773. doi: 10.1371/journal.pone.0063773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ferrucci L, Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol. 2018;15:505–522. doi: 10.1038/s41569-018-0064-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Folkard S. Do permanent night workers show circadian adjustment? A review based on the endogenous melatonin rhythm. Chronobiol Int. 2008;25:215–224. doi: 10.1080/07420520802106835. [DOI] [PubMed] [Google Scholar]
- 57.Gander P, Millar M, Webster C, Merry A. Sleep loss and performance of anaesthesia trainees and specialists. Chronobiol Int. 2008;25:1077–1091. doi: 10.1080/07420520802551428. [DOI] [PubMed] [Google Scholar]
- 58.Gandolfi JV, Di Bernardo APA, Chanes DAV, Martin DF, Joles VB, Amendola CP, et al. the effects of melatonin supplementation on sleep quality and assessment of the serum melatonin in icu patients: a randomized controlled trial. Crit Care Med. 2020;48:e1286–e1e93. doi: 10.1097/ccm.0000000000004690. [DOI] [PubMed] [Google Scholar]
- 59.Germain A, Kupfer DJ. Circadian rhythm disturbances in depression. Hum Psychopharmacol. 2008;23:571–585. doi: 10.1002/hup.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ghazel N, Souissi A, Chtourou H, Aloui G, Souissi N. The effect of music on short-term exercise performance during the different menstrual cycle phases in female handball players. Res Sports Med. 2022;30:50–60. doi: 10.1080/15438627.2020.1860045. [DOI] [PubMed] [Google Scholar]
- 61.Ghram A, Bragazzi NL, Briki W, Jenab Y, Khaled M, Haddad M, et al. COVID-19 pandemic and physical exercise: lessons learnt for confined communities. Front Psychol. 2021;12:618585. doi: 10.3389/fpsyg.2021.618585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Giri A, Srinivasan A, Sundar IK. COVID-19: Sleep, circadian rhythms and immunity–repurposing drugs and chronotherapeutics for SARS-CoV-2. Front Neurosci. 2021;15:674204. doi: 10.3389/fnins.2021.674204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Girotti L, Lago M, Ianovsky O, Elizari MV, Dini A, Lloret SP, et al. Low urinary 6-sulfatoxymelatonin levels in patients with severe congestive heart failure. Endocrine. 2003;22:245–248. doi: 10.1385/ENDO:22:3:245. [DOI] [PubMed] [Google Scholar]
- 64.Golombek D, Pandi-Perumal S, Rosenstein RE, Lundmark PO, Spence DW, Cardinali DP, et al. Dysregulated light/dark cycle impairs sleep and delays the recovery of patients in intensive care units: A call for action for COVID-19 treatment. Chronobiol Int. 2022;39:903–906. doi: 10.1080/07420528.2022.2056477. [DOI] [PubMed] [Google Scholar]
- 65.Hacışevki A, Baba B. An overview of melatonin as an antioxidant molecule: a biochemical approach. In: Dragoi CM, Crenguta Nicolae A, editors. Melatonin. Molecular biology, clinical and pharmaceutical approaches. London: IntechOpen; 2018. pp. 59–85. [Google Scholar]
- 66.Haimov I, Laudon M, Zisapel N, Souroujon M. The relationship between urinary 6-sulphatoxymelatonin rhythm and insomnia in old age. Adv Pineal Res. 1994;8:433. [Google Scholar]
- 67.Hashmi AM, Han JY, Demla V. Intensive care and its discontents: psychiatric illness in the critically ill. Psychiatric Clin. 2017;40:487–500. doi: 10.1016/j.psc.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 68.Hu L, Zhang S, Wen H, Liu T, Cai J, Du D, et al. Melatonin decreases M1 polarization via attenuating mitochondrial oxidative damage depending on UCP2 pathway in prorenin-treated microglia. PloS One. 2019;14(2):e0212138. doi: 10.1371/journal.pone.0212138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Iguchi H, Kato K-I, Ibayashi H. Age-dependent reduction in serum melatonin concentrations in healthy human subjects. J Clin Endocrinol Metab. 1982;55:27–29. doi: 10.1210/jcem-55-1-27. [DOI] [PubMed] [Google Scholar]
- 70.Jiki Z, Lecour S, Nduhirabandi F. Cardiovascular benefits of dietary melatonin: a myth or a reality? Front Physiol. 2018;9(528) doi: 10.3389/fphys.2018.00528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jonas M, Garfinkel D, Zisapel N, Laudon M, Grossman E. Impaired nocturnal melatonin secretion in non-dipper hypertensive patients. Blood Press. 2003;12:19–24. [PubMed] [Google Scholar]
- 72.Kałużna-Czaplińska J, Gątarek P, Chirumbolo S, Chartrand MS, Bjørklund G. How important is tryptophan in human health? Crit Rev Food Sci Nutr. 2019;59:72–88. doi: 10.1080/10408398.2017.1357534. [DOI] [PubMed] [Google Scholar]
- 73.Karasek M. Melatonin, human aging, and age-related diseases. Exp Gerontol. 2004;39:1723–1729. doi: 10.1016/j.exger.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 74.Kennaway DJ. Melatonin research in mice: a review. Chronobiol Int. 2019;36:1167–1183. doi: 10.1080/07420528.2019.1624373. [DOI] [PubMed] [Google Scholar]
- 75.Khullar A. The role of melatonin in the circadian rhythm sleep-wake cycle: a review of endogenous and exogenous melatonin. Psychiatric Times. 2012;29(7):26. [Google Scholar]
- 76.Kimak E, Dzida G, Duma D, Prystupa A, Halabis M, Kimak A, et al. Association between concentration of melatonin, and lipoproteins, LPO, hsCRP, NTproBNP in chronic heart failure patients. Curr Issues Pharm Med Sci. 2014;3:159–164. [Google Scholar]
- 77.Koziróg M, Poliwczak AR, Duchnowicz P, Koter‐Michalak M, Sikora J, Broncel M. Melatonin treatment improves blood pressure, lipid profile, and parameters of oxidative stress in patients with metabolic syndrome. J Pineal Res. 2011;50:261–266. doi: 10.1111/j.1600-079X.2010.00835.x. [DOI] [PubMed] [Google Scholar]
- 78.Kruk J, Aboul-Enein BH, Duchnik E. Exercise-induced oxidative stress and melatonin supplementation: current evidence. J Physiol Sci. 2021;71(1):1–19. doi: 10.1186/s12576-021-00812-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kudo N, Shinohara H, Kagabu S, Kodama H. Evaluation of salivary melatonin concentrations as a circadian phase maker of morning awakening and their association with depressive mood in postpartum mothers. Chronobiol Int. 2021;38:1409–1420. doi: 10.1080/07420528.2021.1930028. [DOI] [PubMed] [Google Scholar]
- 80.Kurhaluk N, Tkachenko H. Melatonin and alcohol-related disorders. Chronobiol Int. 2020;37:781–803. doi: 10.1080/07420528.2020.1761372. [DOI] [PubMed] [Google Scholar]
- 81.Lanfumey L, Mongeau R, Hamon M. Biological rhythms and melatonin in mood disorders and their treatments. Pharmacol Ther. 2013;138:176–184. doi: 10.1016/j.pharmthera.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 82.Laudon M, Frydman-Marom A. Therapeutic effects of melatonin receptor agonists on sleep and comorbid disorders. Int J Mol Sci. 2014;15:15924–15950. doi: 10.3390/ijms150915924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lee RU, Glickman GL. Sleep, circadian health and melatonin for mitigating COVID-19 and optimizing vaccine efficacy. Front Neurosci. 2021;15:711605. doi: 10.3389/fnins.2021.711605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Leonardo-Mendonça RC, Ocaña-Wilhelmi J, de Haro T, de Teresa-Galván C, Guerra-Hernández E, Rusanova I, et al. The benefit of a supplement with the antioxidant melatonin on redox status and muscle damage in resistance-trained athletes. Appl Physiol Nutr Metab. 2017;42:700–707. doi: 10.1139/apnm-2016-0677. [DOI] [PubMed] [Google Scholar]
- 85.Lerner AB, Nordlund JJ. Melatonin: clinical pharmacology. In: Nir I, Reiter RJ, Wurtman RJ, editors. The pineal gland; Proceedings of the International Symposium, Jerusalem, November 14-17, 1977; Vienna: Springer; 1978. pp. 339–345. [Google Scholar]
- 86.Liesa M, Shirihai OS. Mitochondrial dynamics in the regulation of nutrient utilization and energy expenditure. Cell Metab. 2013;17:491–506. doi: 10.1016/j.cmet.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lim S, Park S, Koyanagi A, Yang JW, Jacob L, Yon DK, et al. Effects of exogenous melatonin supplementation on health outcomes: An umbrella review of meta-analyses based on randomized controlled trials. Pharmacol Res. 2022;176:106052. doi: 10.1016/j.phrs.2021.106052. [DOI] [PubMed] [Google Scholar]
- 88.Livianos L, Sierra P, Arques S, García A, Rojo L. Is melatonin an adjunctive stabilizer? Psychiatry Clin Neurosci. 2012;66:82–83. doi: 10.1111/j.1440-1819.2011.02288.x. [DOI] [PubMed] [Google Scholar]
- 89.López-Flores M, Luque-Nieto R, Costa Moreira O, Suárez-Iglesias D, Villa-Vicente JG. Effects of melatonin on sports performance: A systematic review. J Exerc Physiol Online. 2018;21:121–138. [Google Scholar]
- 90.Maestroni G. Exogenous melatonin as potential adjuvant in anti-SarsCov2 vaccines. J Neuroimm Pharmacol. 2020;15:572–573. doi: 10.1007/s11481-020-09956-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Maestroni G, Conti A, Pierpaoli W. Role of the pineal gland in immunity: II. Melatonin enhances the antibody response via an opiatergic mechanism. Clin Exp Immunol. 1987;68:384–391. [PMC free article] [PubMed] [Google Scholar]
- 92.Maestroni GJ. The immunotherapeutic potential of melatonin. Exp Opin Invest Drugs. 2001;10:467–476. doi: 10.1517/13543784.10.3.467. [DOI] [PubMed] [Google Scholar]
- 93.Magdy R, Elmazny A, Soliman SH, Elsebaie EH, Ali SH, Abdel Fattah AM, et al. Post-COVID-19 neuropsychiatric manifestations among COVID-19 survivors suffering from migraine: a case–control study. J Headache Pain. 2022;23(1):1–10. doi: 10.1186/s10194-022-01468-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Maldonado MD, Reiter RJ, Pérez‐San‐Gregorio MA. Melatonin as a potential therapeutic agent in psychiatric illness. Hum Psychopharmacol. 2009;24:391–400. doi: 10.1002/hup.1032. [DOI] [PubMed] [Google Scholar]
- 95.Malik P, Patel K, Pinto C, Jaiswal R, Tirupathi R, Pillai S, et al. Post‐acute COVID‐19 syndrome (PCS) and health‐related quality of life (HRQoL)—A systematic review and meta‐analysis. J Med Virol. 2022;94:253–262. doi: 10.1002/jmv.27309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mańka S, Majewska E. Immunoregulatory action of melatonin. The mechanism of action and the effect on inflammatory cells. Postepy Hig Med Dosw (Online) 2016;70(0):1059–1067. doi: 10.5604/17322693.1221001. [DOI] [PubMed] [Google Scholar]
- 97.Mäntele S, Otway DT, Middleton B, Bretschneider S, Wright J, Robertson MD, et al. Daily rhythms of plasma melatonin, but not plasma leptin or leptin mRNA, vary between lean, obese and type 2 diabetic men. PloS One. 2012;7(5):e37123. doi: 10.1371/journal.pone.0037123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Marseglia L, D'Angelo G, Manti S, Aversa S, Arrigo T, Reiter RJ, et al. Analgesic, anxiolytic and anaesthetic effects of melatonin: new potential uses in pediatrics. Int J Mol Sci. 2015;16:1209–1220. doi: 10.3390/ijms16011209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Martín Giménez VM, Prado N, Diez E, Manucha W, Reiter RJ. New proposal involving nanoformulated melatonin targeted to the mitochondria as a potential COVID-19 treatment. Nanomedicine (Lond) 2020;15:2819–2821. doi: 10.2217/nnm-2020-0371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mazepa R, Cuevas M, Collado P, González-Gallego J. Melatonin increases muscle and liver glycogen content in nonexercised and exercised rats. Life Sci. 1999;66:153–160. doi: 10.1016/s0024-3205(99)00573-1. [DOI] [PubMed] [Google Scholar]
- 101.McClung CA. Circadian rhythms and mood regulation: insights from pre-clinical models. Eur Neuropsychopharmacol. 2011;21:S683–S693. doi: 10.1016/j.euroneuro.2011.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.McMullan CJ, Schernhammer ES, Rimm EB, Hu FB, Forman JP. Melatonin secretion and the incidence of type 2 diabetes. JAMA. 2013;309:1388–1396. doi: 10.1001/jama.2013.2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Minich DM, Henning M, Darley C, Fahoum M, Schuler CB, Frame J. Is melatonin the "next vitamin D"? A review of emerging science, clinical uses, safety, and dietary supplements. Nutrients. 2022;14(19):3934. doi: 10.3390/nu14193934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Mohammed A. Should All patients having planned procedures or surgeries be tested for COVID-19. Am J Surg Clin Case Rep. 2020;2(2):1–3. [Google Scholar]
- 105.Monteleone P, Maj M. The circadian basis of mood disorders: recent developments and treatment implications. Eur Neuropsychopharmacol. 2008;18(10):701–711. doi: 10.1016/j.euroneuro.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 106.Monteleone P, Martiadis V, Maj M. Circadian rhythms and treatment implications in depression. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:1569–1574. doi: 10.1016/j.pnpbp.2010.07.028. [DOI] [PubMed] [Google Scholar]
- 107.Mortezaee K, Potes Y, Mirtavoos-Mahyari H, Motevaseli E, Shabeeb D, Musa AE, et al. Boosting immune system against cancer by melatonin: A mechanistic viewpoint. Life Sci. 2019;238:116960. doi: 10.1016/j.lfs.2019.116960. [DOI] [PubMed] [Google Scholar]
- 108.Munk-Jørgensen P. Manipulating melatonin in managing mood. Acta Psychiatr Scand. 2013;128(Suppl 444):16-23. Corrigendum: Acta Psychiatr Scand. 2014;130:240. doi: 10.1111/acps.12175. [DOI] [PubMed] [Google Scholar]
- 109.Nelson AG, Kokkonen J, Mickenberg M. Acute short-term dim light exposure can lower muscle strength endurance. J Sport Health Sci. 2015;4:270–274. [Google Scholar]
- 110.Ochoa JJ, Díaz‐Castro J, Kajarabille N, García C, Guisado IM, De Teresa C, et al. Melatonin supplementation ameliorates oxidative stress and inflammatory signaling induced by strenuous exercise in adult human males. J Pineal Res. 2011;51:373–380. doi: 10.1111/j.1600-079X.2011.00899.x. [DOI] [PubMed] [Google Scholar]
- 111.Pandi-Perumal S, Zisapel N, Srinivasan V, Cardinali D. Melatonin and sleep in aging population. Exp Gerontol. 2005;40:911–925. doi: 10.1016/j.exger.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 112.Pandi-Perumal SR, BaHammam AS, Ojike NI, Akinseye OA, Kendzerska T, Buttoo K, et al. Melatonin and human cardiovascular disease. J Cardiovasc Pharmacol Ther. 2016;22:122–132. doi: 10.1177/1074248416660622. [DOI] [PubMed] [Google Scholar]
- 113.Paulis L, Šimko F. Blood pressure modulation and cardiovascular protection by melatonin: potential mechanisms behind. Physiol Res. 2007;56:671–684. doi: 10.33549/physiolres.931236. [DOI] [PubMed] [Google Scholar]
- 114.Peck JS, LeGoff DB, Ahmed I, Goebert D. Cognitive effects of exogenous melatonin administration in elderly persons: a pilot study. Am J Geriatr Psychiatry. 2004;12:432–436. doi: 10.1176/appi.ajgp.12.4.432. [DOI] [PubMed] [Google Scholar]
- 115.Peuhkuri K, Sihvola N, Korpela R. Dietary factors and fluctuating levels of melatonin. Food Nutr Res. 2012;56:17252. doi: 10.3402/fnr.v56i0.17252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Pickel L, Sung H-K. Feeding rhythms and the circadian regulation of metabolism. Front Nutr. 2020;7:39. doi: 10.3389/fnut.2020.00039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Pierpaoli W, Regelson W, Colman C. The melatonin miracle: Nature's age-reversing, disease-fighting, sex-enhancing hormone. New York, NY: Simon & Schuster; 1995. [Google Scholar]
- 118.Quera Salva MA, Hartley S. Mood disorders, circadian rhythms, melatonin and melatonin agonists. J Cent Nerv Syst Dis. 2012;4:15–26. doi: 10.4137/jcnsd.s4103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Rajpoot K. Nanotechnology-based targeting of neurodegenerative disorders: a promising tool for efficient delivery of neuromedicines. Curr Drug Targets. 2020;21:819–836. doi: 10.2174/1389450121666200106105633. [DOI] [PubMed] [Google Scholar]
- 120.Ramos E, López-Muñoz F, Gil-Martín E, Egea J, Álvarez-Merz I, Painuli S, et al. The Coronavirus Disease 2019 (COVID-19): key emphasis on melatonin safety and therapeutic efficacy. Antioxidants (Basel) 2021;10(7):1152. doi: 10.3390/antiox10071152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Reiter RJ, Ma Q, Sharma R. Melatonin in mitochondria: mitigating clear and present dangers. Physiology. 2020;35:86–95. doi: 10.1152/physiol.00034.2019. [DOI] [PubMed] [Google Scholar]
- 122.Reiter RJ, Ma Q, Sharma R. Treatment of Ebola and other infectious diseases: melatonin “goes viral”. Melatonin Res. 2020;3:43–57. [Google Scholar]
- 123.Reiter RJ, Tan D-X, Paredes SD, Fuentes-Broto L. Beneficial effects of melatonin in cardiovascular disease. Ann Med. 2010;42:276–285. doi: 10.3109/07853890903485748. [DOI] [PubMed] [Google Scholar]
- 124.Robillard R, Carpenter JS, Feilds KL, Hermens DF, White D, Naismith SL, et al. Parallel changes in mood and melatonin rhythm following an adjunctive multimodal chronobiological intervention with agomelatine in people with depression: a proof of concept open label study. Front Psychiatry. 2018;9:624. doi: 10.3389/fpsyt.2018.00624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Romdhani M, Ammar A, Trabelsi K, Chtourou H, Vitale J, Masmoudi L, et al. Ramadan observance exacerbated the negative effects of COVID-19 lockdown on sleep and training behaviors: an international survey on 1,681 Muslim athletes. Front Nutr. 2022;9:925092. doi: 10.3389/fnut.2022.925092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Romdhani M, Fullagar H, Vitale J, Nedelec M, Rae D, Ammar A, et al. Lockdown duration and training intensity affect sleep behavior in an international sample of 1,454 elite athletes. Front Physiol. 2022;13:904778. doi: 10.3389/fphys.2022.904778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Romdhani M, Hammouda O, Chaabouni Y, Mahdouani K, Driss T, Chamari K, et al. Sleep deprivation affects post-lunch dip performances, biomarkers of muscle damage and antioxidant status. Biol Sport. 2019;36:55–65. doi: 10.5114/biolsport.2018.78907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Romdhani M, Rae D, Nedelec M, Ammar A, Chtourou H, Al-horani R, et al. COVID-19 lockdowns: a worldwide survey of circadian rhythms and sleep quality in 3911 athletes from 49 countries, with data-driven recommendations. Sports Med. 2022;52:1433–1448. doi: 10.1007/s40279-021-01601-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Rong B, Wu Q, Sun C. Melatonin: A novel strategy for prevention of obesity and fat accumulation in peripheral organs through the improvements of circadian rhythms and antioxidative capacity. Melatonin Res. 2020;3:58–76. [Google Scholar]
- 130.Ronkainen H, Vakkuri O, Kauppila A. Effects of physical exercise on the serum concentration of melatonin in female runners. Acta Obstet Gynecol Scand. 1986;65:827–829. doi: 10.3109/00016348609157031. [DOI] [PubMed] [Google Scholar]
- 131.Sánchez-Barceló E, Mediavilla M, Tan D, Reiter R. Clinical uses of melatonin: evaluation of human trials. Curr Med Chem. 2010;17:2070–2095. doi: 10.2174/092986710791233689. [DOI] [PubMed] [Google Scholar]
- 132.Sang Y, Gu X, Pan L, Zhang C, Rong X, Wu T, et al. Melatonin ameliorates coxsackievirus B3-induced myocarditis by regulating apoptosis and autophagy. Front Pharmacol. 2018;9:1384. doi: 10.3389/fphar.2018.01384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Sayed RK, Fernández-Ortiz M, Diaz-Casado ME, Rusanova I, Rahim I, Escames G, et al. The protective effect of melatonin against age-associated, sarcopenia-dependent tubular aggregate formation, lactate depletion, and mitochondrial changes. J Gerontol A Biol Sci Med Sci. 2018;73:1330–1338. doi: 10.1093/gerona/gly059. [DOI] [PubMed] [Google Scholar]
- 134.Shneider A, Kudriavtsev A, Vakhrusheva A. Can melatonin reduce the severity of COVID-19 pandemic? Int Rev Immunol. 2020;39:153–162. doi: 10.1080/08830185.2020.1756284. [DOI] [PubMed] [Google Scholar]
- 135.Slominski RM, Reiter RJ, Schlabritz-Loutsevitch N, Ostrom RS, Slominski AT. Melatonin membrane receptors in peripheral tissues: distribution and functions. Mol Cell Endocrinol. 2012;351:152–166. doi: 10.1016/j.mce.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Souissi A, Ben Maaouia G, Dergaa I, Ghram A, Ben Saad H. The fat burning ability of melatonin during submaximal exercise. Biol Rhythm Res. 2022;epub ahead of print [Google Scholar]
- 137.Souissi A, Dergaa I, Chtourou H, Ben Saad H. The effect of daytime ingestion of melatonin on thyroid hormones responses to acute submaximal exercise in healthy active males: a pilot study. Am J Men's Health. 2022;16(1):15579883211070383. doi: 10.1177/15579883211070383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Souissi A, Farjallah M, Chortane OG, Dergaa I, Mejri M, Gaamouri N, et al. The effects of daytime melatonin ingestion on arousal and vigilance vanish after sub-maximal exercise: a pilot study. Eur Rev Med Pharmacol Sci. 2022;26:6065–6072. doi: 10.26355/eurrev_202209_29622. [DOI] [PubMed] [Google Scholar]
- 139.Souissi A, Haddad M, Dergaa I, Saad HB, Chamari K. A new perspective on cardiovascular drift during prolonged exercise. Life Sci. 2021;287:120109. doi: 10.1016/j.lfs.2021.120109. [DOI] [PubMed] [Google Scholar]
- 140.Souissi A, Yousfi N, Dabboubi R, Aloui G, Haddad M, Souissi N. Effect of acute melatonin administration on physiological response to prolonged exercise. Biol Rhythm Res. 2020;51:980–987. [Google Scholar]
- 141.Soysal P, Arik F, Smith L, Jackson SE, Isik AT. Inflammation, frailty and cardiovascular disease. Adv Exp Med Biol. 2020;1216:55–64. doi: 10.1007/978-3-030-33330-0_7. [DOI] [PubMed] [Google Scholar]
- 142.St Louis EK, Boeve BF. REM Sleep behavior disorder: diagnosis, clinical implications, and future directions. Mayo Clinic Proc. 2017;92:1723–1736. doi: 10.1016/j.mayocp.2017.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Strassman RJ, Appenzeller O, Lewy AJ, Qualls CR, Peake GT. Increase in plasma melatonin, β-endorphin, and cortisol after a 28.5-mile mountain race: relationship to performance and lack of effect of naltrexone. J Clin Endocrinol Metab. 1989;69:540–545. doi: 10.1210/jcem-69-3-540. [DOI] [PubMed] [Google Scholar]
- 144.Su WL, Wu CC, Wu SV, Lee MC, Liao MT, Lu KC, et al. A review of the potential effects of melatonin in compromised mitochondrial redox activities in elderly patients with COVID-19. Front Nutr. 2022;9:865321. doi: 10.3389/fnut.2022.865321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sun H, Gusdon AM, Qu S. Effects of melatonin on cardiovascular diseases: progress in the past year. Curr Opin Lipidol. 2016;27:408–413. doi: 10.1097/MOL.0000000000000314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Sundberg I, Ramklint M, Stridsberg M, Papadopoulos FC, Ekselius L, Cunningham JL. Salivary melatonin in relation to depressive symptom severity in young adults. PloS One. 2016;11(4):e0152814. doi: 10.1371/journal.pone.0152814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Tan D-X, Reiter RJ. Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality. Life Sci. 2022;294:120368. doi: 10.1016/j.lfs.2022.120368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Theron J, Oosthuizen, JMC, Rautenbach M. Effect of physical exercise on plasma melatonin levels in normal volunteers. S Afr Med J. 1984;66:838–841. [PubMed] [Google Scholar]
- 149.Trabelsi K, Ammar A, Masmoudi L, Boukhris O, Chtourou H, Bouaziz B, et al. Globally altered sleep patterns and physical activity levels by confinement in 5056 individuals: ECLB COVID-19 international online survey. Biol Sport. 2021;38:495–506. doi: 10.5114/biolsport.2021.101605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Trefts E, Williams AS, Wasserman DH. Exercise and the regulation of hepatic metabolism. Prog Mol Biol Transl Sci. 2015;135:203–225. doi: 10.1016/bs.pmbts.2015.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Trionfante CP, Davis GR, Farney TM, Miskowiec RW, Nelson AG. A pre-exercise dose of melatonin can alter substrate use during exercise. Int J Exerc Sci. 2017;10:1029–1037. [PMC free article] [PubMed] [Google Scholar]
- 152.Van Someren EJ. Circadian rhythms and sleep in human aging. Chronobiol Int. 2000;17:233–243. doi: 10.1081/cbi-100101046. [DOI] [PubMed] [Google Scholar]
- 153.Varma A, Dergaa I, Ashkanani M, Musa S, Zidan M. Analysis of Qatar’s successful public health policy in dealing with the Covid-19 pandemic. Int J Med Rev Case Rep. 2021;5(2):6–11. [Google Scholar]
- 154.Videnovic A, Ju Y-ES, Arnulf I, Cochen-De Cock V, Högl B, Kunz D, et al. Clinical trials in REM sleep behavioural disorder: challenges and opportunities. J Neurol Neurosurg Psychiatry. 2020;91:740–749. doi: 10.1136/jnnp-2020-322875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Walsh NP, Halson SL, Sargent C, Roach GD, Nédélec M, Gupta L, et al. Sleep and the athlete: narrative review and 2021 expert consensus recommendations. Br J Sports Med. 2021;55:356–368. doi: 10.1136/bjsports-2020-102025. [DOI] [PubMed] [Google Scholar]
- 156.Warman GR, Pawley MD, Bolton C, Cheeseman JF, Fernando AT, III, Arendt J, et al. Circadian-related sleep disorders and sleep medication use in the New Zealand blind population: an observational prevalence survey. PloS One. 2011;6(7):e22073. doi: 10.1371/journal.pone.0022073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Wichniak A, Kania A, Siemiński M, Cubała WJ. Melatonin as a potential adjuvant treatment for COVID-19 beyond sleep disorders. Int J Mol Sci. 2021;22(16):8623. doi: 10.3390/ijms22168623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Wu X, Ji H, Wang Y, Gu C, Gu W, Hu L, et al. Melatonin alleviates radiation-induced lung injury via regulation of miR-30e/NLRP3 axis. Oxid Med Cell Longev. 2019;2019:4087298. doi: 10.1155/2019/4087298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Yip HK, Chang YC, Wallace CG, Chang LT, Tsai TH, Chen YL, et al. Melatonin treatment improves adipose‐derived mesenchymal stem cell therapy for acute lung ischemia–reperfusion injury. J Pineal Res. 2013;54:207–221. doi: 10.1111/jpi.12020. [DOI] [PubMed] [Google Scholar]
- 160.Zawilska JB, Lorenc A, Berezińska M, Vivien‐Roels B, Pévet P, Skene DJ. Daily oscillation in melatonin synthesis in the Turkey pineal gland and retina: diurnal and circadian rhythms. Chronobiol Int. 2006;23:341–350. doi: 10.1080/07420520500482082. [DOI] [PubMed] [Google Scholar]
- 161.Zhang B, Zhou X, Qiu Y, Song Y, Feng F, Feng J, et al. Clinical characteristics of 82 cases of death from COVID-19. PloS One. 2020;15(7):e0235458. doi: 10.1371/journal.pone.0235458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zhang R, Wang X, Ni L, Di X, Ma B, Niu S, et al. COVID-19: Melatonin as a potential adjuvant treatment. Life Sci. 2020;250:117583. doi: 10.1016/j.lfs.2020.117583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zhang W, Chen X-y, Su S-w, Jia Q-z, Ding T, Zhu Z-n, et al. Exogenous melatonin for sleep disorders in neurodegenerative diseases: a meta-analysis of randomized clinical trials. Neurol Sci. 2016;37:57–65. doi: 10.1007/s10072-015-2357-0. [DOI] [PubMed] [Google Scholar]
- 164.Zhao C-N, Wang P, Mao Y-M, Dan Y-L, Wu Q, Li X-M, et al. Potential role of melatonin in autoimmune diseases. Cytokine Growth Factor Rev. 2019;48:1–10. doi: 10.1016/j.cytogfr.2019.07.002. [DOI] [PubMed] [Google Scholar]