Abstract
Background
Neck pain is a common problem in the general population and second only to low back pain in musculoskeletal problems. The aim of this study is to compare three different types of exercise training in patients with chronic neck pain.
Methods
This study was conducted on 45 patients with neck pain. Patients were divided into 3 groups Group 1 (conventional treatment), Group 2 (conventional treatment plus deep cervical flexor training), and Group 3 (conventional treatment plus stabilization of the neck and core region). The exercise programs were applied for four weeks, three days a week. The demographic data, pain intensity (verbal numeric pain scale), posture (Reedco’s posture scale), cervical range of motion ([ROM] goniometer), and disability (Neck Disability Index [NDI]) were evaluated.
Results
In all groups, a significant improvement was found in terms of pain, posture, ROM, and NDI values in all groups (P < 0.001). Between the groups, analyses showed that the pain and posture improved more in Group 3, while the ROM and NDI improved more in Group 2.
Conclusions
In addition to conventional treatment, applying core stabilization exercises or deep cervical flexor muscle training to patients with neck pain may be more effective in reducing pain and disability and increasing ROM than conventional treatment alone.
Keywords: Cervical Vertebrae; Exercise; Muscle, Skeletal; Neck Pain; Pain Measurement; Posture; Proprioception; Range of Motion, Articular
INTRODUCTION
Neck pain is a frequently observed problem in the broad population and is the second most frequently seen musculoskeletal problem [1]. Symptoms of chronic neck pain occur on palpation of that area and a feeling of hyperalgesia against muscles and ligaments during active or passive movement. If there is no specific pathology and the intensity of pain can be increased with provocative stimuli, it can be called mechanical neck pain [2]. Chronic neck pain has the potential to change the cervical region biomechanics by adversely affecting the muscle imbalance and head-neck posture [3,4]. Forward head posture problems are commonly seen in persons with neck pain [4,5]. According to previous studies, it has been proven that an average of 60% of patients with neck pain have a forward head posture [3]. Previous studies have indicated that patients suffering from neck pain have decreased endurance in their deep cervical flexor muscles such as the longus colli and longus capitis. The deep cervical flexor muscles provide postural endurance support, and it is known that activation of these muscles is impaired in people with neck pain. Moreover, it has been observed that performance of the clinical cranio-cervical flexion test reduces the symptoms of patients with neck pain. Since training the deep cervical flexor muscles increases deep cervical flexor muscles activation, it can improve the ability of the cervical spine to maintain its neutral posture [6]. The deep cervical flexor muscles support the cervical lordosis and are an important stabilizer of the head and neck posture. In individuals with mechanical neck pain, there is a decrease in muscle activation of the deep cervical stabilizer muscles. This causes superficial muscles such as the trapezius muscle to undertake postural functions and increase the load on these muscles. When the performance of these muscles’ decreases, it means that the balance between the stabilizing muscles in posterior of the neck is disturbed. The deep cervical flexor muscles can deteriorate and cause a loss of proper posture, contributing to cervical impairment. Therefore, deep cervical flexor training is suggested to increase the endurance of these postural muscles, and this results in a reduction in symptoms of neck pain. Research shows that motor control training of the deep cervical flexor muscles before strengthening the global cervical muscles is more efficient in neck pain rehabilitation [7].
The aim of this research was to compare conventional therapy, the cervical stabilization exercise approach, and core stabilization exercise in addition to the cervical stabilization in patients suffering from chronic neck pain.
MATERIALS AND METHODS
1. Study design
In order to conduct this study, approval was received from the Research Ethics Committee of Yeditepe University (Number: 11.07.2019-1071). An informed written consent form was obtained from the volunteers before any participation in the experiment. This study was registered in ClinicalTrials.gov (CT number: NCT05488756), and the study was conducted in accordance with the Helsinki Declaration.
We calculated the sample size with the G*power software version 3.1.9.6 (Heinrich-Heine-Universität). The authors chose F tests and “ANOVA: repeated measures, within factors” with assuming a 0.25 effect size (f), 90% power, and 0.05 significance level. Forty-five participants were found, for total minimal sample (15 for every group). An additional participant was added to each group as a safeguard against the possibility of drop out. So, finally, a total of 48 participants were included in the study.
2. Participants
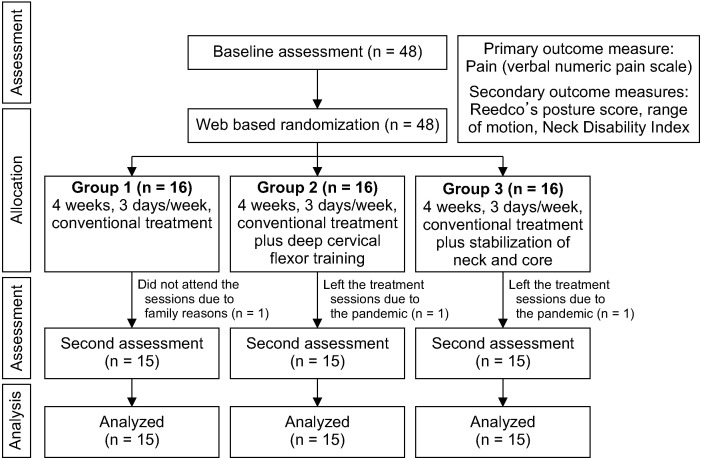
Volunteer participants who had been diagnosed with mechanical neck pain were referred to the physical therapy and rehabilitation clinic of the university by a specialist at Pendik Regional Hospital. The inclusion criteria were as follows: (1) having chronic neck pain more than 3 months; (2) ages between 25 and 60 years; and (3) being medically stable. The exclusion criteria were as follows: (1) patients with benign or tumors in the cervical region; (2) having active, localized osseous and discal infection in the spine (spondylodiscitis) and a history of spinal fractures; (3) having a congenital anomaly; (4) patients with neck surgery and spinal instability; and (5) patients receiving injections or other interventions in last year for his/her neck. At baseline, 48 eligible cases were evaluated, and then divided into 3 groups by randomization: Group 1 (conventional treatment), Group 2 (conventional treatment plus deep cervical flexor training), and Group 3 (conventional treatment plus stabilization of the neck and core region). After three dropouts, 45 subjects completed the study. The participants were re-evaluated at the end of the 4-week treatment period (Fig. 1). The treatment programs of the patients were applied under the supervision of an experienced physiotherapist for four weeks, three days a week.
Fig. 1.
Flow diagram for study subjects.
3. Outcome measures
Assessments were done twice. One was at baseline, a day before the first treatment session, and the second was a day after the last day of the 4-week treatment program. Evaluations and appointments for treatment sessions were given according to the patients' availability.
1) Demographic characteristics of participants
Gender, age, and body mass index (BMI) of the participants were recorded on a form prepared by researchers. BMI was calculated twice, before and after the 4-week treatment.
2) Primary outcome measure: pain intensity assessment
Pain intensity was measured via an 11-point verbal numeric pain scale (VNPS) (0–10; 0 means no pain; 10 means worst pain). VNPS is a reliable and valid measure for subjective pain measurement. Participants were asked to report the pain severity at that moment on a scale from 0 to 10 [8,9].
3) Secondary outcome measures
(1) Posture evaluation
Reedco’s posture score (REEDCO, 1974) was assessed visually on 10 postural traits. The value of 0 equals signifies poor posture or severe deviation, a value of 5 showed fair posture or minimal to moderate deviation, and a value of 10 showed good posture or normal alignment.
While 100 points claimed good posture and a score of 59% or less is showed as postural dysfunction [10].
(2) Evaluation of cervical range of motion (ROM)
Cervical ROM was evaluated using a goniometer while the patient was sitting on a chair with both feet on the ground. After the goniometer was brought to the neutral position, the patient was asked to perform the desired movement with the head: flexion, extension, right and left lateral flexion, and right and left rotation. A degree was recorded for each neck motion and used in the average analysis [11].
(3) Disability evaluation
The Neck Disability Index (NDI) was used to assess the disability due to neck pain during daily activities. The form contains 10 questions related to pain, lifting, and different activities. The score of each question is 0–5 according to the options and the total score is recorded by adding the scores of all the answers. The lower the total score, the less the effect of pain on the performance of daily activities. The higher the score, the greater the performance of daily activities is affected [12].
4. Treatment programs
A standardized therapy as conventional treatment was given in all groups. The group that received conventional treatment alone, was accepted as a control group. The patients were treated under the supervision of an experienced physiotherapist, three times a week for four weeks. Each exercise program lasted an average of 30 minutes. Although questions were asked about possible side effects by the physiotherapist during each therapy session, no side effects of exercises were reported by the subjects.
5. Conventional treatment
The conventional treatment included electrotherapy agents (transcutaneous electrical nerve stimulation [TENS], ultrasound, and hot packs) and isometric exercise training. TENS was applied for 20 minutes with an intensity of 10–30 mA and a frequency of 80 Hz with a TENS device (Sonopuls 492, Enraf-Nonius). A couple of surface electrodes were placed over the painful area in the neck. The intensity of the TENS was adjusted according to the sensory threshold of the patient so that it would not be disturbed by the tingling sensation. After TENS, continuous ultrasound was applied to the neck area to produce thermal effects at a density of 1.5 W/cm2 for 5 minutes. At least, a hot pack applied the neck area for 10 minutes. Isometric exercises were done for flexors, extensors, rotators, and lateral flexors of the neck. The patient was asked to isometrically contract his working muscle for 5 seconds against his own hand, which was placed in compliance with the working muscles, with a total of 10 repetitions. All patients in each group were given conventional treatment.
6. Deep cervical flexor muscle training
Cranio-cervical flexor muscle training focuses on the deep flexor muscles such as longus capitis and longus colli muscles, which flex the neck, not the head. Also, these low-load exercises train the deep cervical flexors more specifically, rather than all the neck flexors involved in the head-lifting exercise. Exercises were performed with an air-filled pressure stabilizer (StabilizerTM; Chattanooga Stabilizer Group Inc.) placed in the sub-occipital region to monitor the flattening of the cervical lordosis caused by the contraction of the longus colli muscle [6]. Group 2 was given deep cervical flexor muscle training in addition to the conventional treatment. Cervical stabilization exercises were started by teaching the patient to contract the deep cervical flexors. After activation of these muscles, the patient was asked to continue this movement in each exercise and in every activity to achieve automatic stabilization. The patients were hospitalized in the supine hook position (without a pillow) to ensure the neutral position of the neck. For cranio-cervical flexion and mild axial extension, each patient was individually treated with a slow, controlled head and upper cervical area flexion by bringing the chin closer to the chest ("yes" movement). StabilizerTM was inflated to 20 mmHg. Gradual training was given to increase the pressure value between 20 and 30 mmHg by 2 mmHg. It was kept for 10 seconds at each pressure value (22, 24, 26, 28 mmHg) and operated 10 times. Then, while providing motor control with the pressurized stabilizer device, the arm is flexed 90 degrees. After training with visual feedback, the patient is asked to slowly move his chin closer to his chest (chin-tuck). In this exercise, the neck makes posterior tilt without head flexion. After the motor control of the cervical stabilization was achieved, training was continued gradually with prone, crawling, and limb movements while crawling followed by overhead ball lifting movements and scapular correction exercises (scapular mobilization and shoulder rolls). These exercises were performed for 10 repetitions with 10 seconds of contraction and 5 seconds of relaxation.
7. Core stabilization training
While core stabilization training control head position, arms, and trunk segment related to the body’s base of support, provide to stabilize the lumbopelvic region. All the subjects in the third group had undergone 4 weeks core stability training which comprises of exercises aimed at increasing spinal stability. The Group 3 was given neck and core stabilization exercises in addition to the conventional treatment.
Core stabilization exercises were started by teaching the patient the basic exercises with an air-inflated pressure sensor StabilizerTM. While the patient is in the supine position with the knees at a 90° flexion, the pressure cuff was placed under the lumbar spine and inflated to 40 mmHg. Exercises were started with a stabilizer to activate the main muscles. The level at which the patient can keep the pressure constant (stable pelvis) was determined while doing the exercises. The subjects were first taught the "abdominal hollowing" (pulling the belly up and in) exercise, which provides transversus abdominis and multifidus co-contraction. After motor control of the core stabilization, basic training was continued progressively in the supine, prone, crawling and sitting positions on the ball (straight leg raising, abdominal crunch exercise, bridge exercises, swimming exercises, exercises in a crawling position and limb movements in sitting position and while sitting on the ball). These exercises were performed for 10 repetitions with 10 seconds of contraction and 5 seconds of relaxation.
8. Statistical analysis
SPSS 24.0 program (IBM Co.) was used for the statistical analysis, and P < 0.05 was accepted as significant in all analyzes. Whether the data were convenient for normal distribution was determined by the Kolmogorov–Smirnov test. According to analysis of the results of this test, non-parametric tests were used in the analysis. In the statistical analysis of the study, the variables considered were defined with mean (min–max), standard deviation, minimum, and maximum values.
The baseline variables of all three groups were compared with the chi-squared (categorical variables) and Kruskal–Wallis (continuous variables) tests. The Mann–Whitney U-test was used to analyze the difference of the continuous variables between groups. The pre- and post-treatment values of the groups were compared with the Wilcoxon test. The effect sizes were calculated for the intragroup changes with a formula as follows: Effect size = the difference of the pre-post assessments / standard deviation of the first assessment. An effect size of 0.2–0.5 was interpreted as “small”, 0.51–0.80 as “medium”, and 0.81 and above as “large” [13]. Effect sizes were calculated for significant variables. Also, pre- to post-treatment changes were compared between groups with the Kruskal–Wallis test, and significant values were analyzed with the Mann–Whitney U-test for pair group comparison.
RESULTS
The baseline demographic characteristics (age, gender, BMI) and assessment results (VNPS, ROM, and NDI) of the groups are shown in Table 1. There was no statistical difference between the groups for baseline assessments.
Table 1.
Pre-treatment value of pain, posture, joint ROM and NDI measurements of the groups
| Parameters | Group 1 (n = 15) | Group 2 (n = 15) | Group 3 (n = 15) | P value |
|---|---|---|---|---|
| Age (yr) | 38.73 (26–59) ± 12.3 | 42.27 (27–60) ± 10.64 | 42.07(26–59) ± 10.86 | 0.461 |
| Gender | ||||
| Female | 10 (66.7) | 8 (53.3) | 9 (60.0) | 0.762 |
| Male | 5 (33.3) | 7 (46.7) | 6 (40.0) | |
| BMI (kg/m2) | 23.4 (19.05–27.04) ± 2.4 | 24.35 (19.47–28.58) ± 2.66 | 24.76 (20.80–29.32) ± 2.72 | 0.284 |
| Pain (VNPS) | 6.40 (5–8) ± 1.056 | 6.80 (5–8) ± 1.01 | 6.67 (5–8) ± 0.97 | 0.562 |
| Posture | 76.33 (65–90) ± 6.93 | 76.00 (65–85) ± 5.07 | 74.00 (65–80) ± 5.07 | 0.496 |
| ROM (degrees) | ||||
| Flexion | 40.67 (35–50) ± 4.60 | 39.73 (35–45) ± 3.36 | 39.73 (35–45) ± 3.49 | 0.874 |
| Extension | 45.00 (40–50) ± 3.46 | 42.27 (35–55) ± 5.67 | 42.33 (40–50) ± 2.94 | 0.072 |
| R Lat. flexion | 34.67 (30–45) ± 4.10 | 31.13 (27–35) ± 2.94 | 32.47 (27–37) ± 3.18 | 0.054 |
| L Lat. flexion | 35.33 (30–40) ± 3.59 | 32.00 (27–37) ± 3.29 | 33.13 (27–40) ± 3.70 | 0.081 |
| R rotation | 48.07 (40–55) ±4.54 | 45.07 (35–56) ± 5.16 | 45.13 (35–51) ± 4.74 | 0.135 |
| L rotation | 48.60 (38–55) ± 4.99 | 45.13 (37–56) ± 4.96 | 46.13 (37–52) ± 4.43 | 0.090 |
| NDI | 27.27 (16–34) ± 5.36 | 30.00 (23–34) ± 3.60 | 28.67 (23–34) ± 3.47 | 0.312 |
Values are presented as mean (min–max) ± standard deviation or number (%).
Min: minimum, Max: maximum, BMI: body mass index, VNPS: verbal numeric pain scale, ROM: range of motion, R: right, L: left, Lat: lateral, NDI: Neck Disability Index, Group 1: conventional treatment, Group 2: conventional treatment plus deep cervical flexor training, Group 3: conventional treatment plus stabilization of the neck and core region.
The comparison of pain, posture, ROM, and NDI values of the patients within the groups are shown in Table 2. In all groups, a significant improvement was found in pain, posture, ROM, and NDI values for the in-group evaluation results (P < 0.001).
Table 2.
Comparison of within–group pain, posture, ROM, and NDI values
| Parameters | Groups | Pre–treatment | Post–4 week treatment | P value |
|---|---|---|---|---|
| Pain (VNPS) | Group 1 | 6.40 (5–8) ± 1.05 | 3.47 (2–5) ± 1.06 | < 0.001 |
| Group 2 | 6.80 (8–5) ± 1.01 | 2.87 (2–4) ± 0.74 | < 0.001 | |
| Group 3 | 6.67 (5–8) ± 0.97 | 2.53 (1–4) ± 0.74 | < 0.001 | |
| Posture | Group 1 | 76.33 (65–90) ± 6.93 | 80.00 (70–90) ± 5.35 | < 0.001 |
| Group 2 | 76.00 (65–85) ± 5.07 | 84.33 (80–90) ± 2.58 | < 0.001 | |
| Group 3 | 74.00 (65–80) ± 5.07 | 84.00 (80–90) ± 2.80 | < 0.001 | |
| ROM (degrees) | ||||
| Flexion | Group 1 | 40.67 (35–50) ± 4.60 | 43.93 (38–50) ± 4.60 | < 0.001 |
| Group 2 | 39.73 (35–45) ± 3.36 | 46.20 (42–50) ± 2.88 | < 0.001 | |
| Group 3 | 39.73 (35–45) ± 3.49 | 44.93 (40–50) ± 3.26 | < 0.001 | |
| Extension | Group 1 | 45.00 (40–50) ± 3.46 | 48.20 (45–57) ± 3.82 | < 0.001 |
| Group 2 | 42.27 (35–55) ± 5.67 | 48.93 (42–57) ± 4.41 | < 0.001 | |
| Group 3 | 42.33 (40–50) ± 2.94 | 47.73 (45–57) ± 3.51 | < 0.001 | |
| R Lat. flexion | Group 1 | 34.67 (30–45) ± 4.10 | 37.40 (35–45) ± 3.15 | < 0.001 |
| Group 2 | 31.13 (27–35) ± 2.94 | 36.73 (35–42) ± 2.43 | < 0.001 | |
| Group 3 | 32.47 (27–37) ± 3.18 | 37.27 (35–42) ± 2.52 | < 0.001 | |
| L Lat. flexion | Group 1 | 35.33 (30–40) ± 3.59 | 37.93 (35–45) ± 3.15 | < 0.001 |
| Group 2 | 32.00 (27–37) ± 3.29 | 37.00 (33–42) ± 2.67 | < 0.001 | |
| Group 3 | 33.13 (27–40) ± 3.70 | 37.67 (34–42) ± 2.71 | < 0.001 | |
| R rotation | Group 1 | 48.07 (40–55) ± 4.54 | 51.33 (40–57) ± 4.90 | < 0.001 |
| Group 2 | 45.07 (35–56) ± 5.16 | 50.47 (45–60) ± 4.10 | < 0.001 | |
| Group 3 | 45.13 (35–51) ± 4.74 | 50.27 (45–55) ± 3.73 | < 0.001 | |
| L rotation | Group 1 | 48.60 (38–55) ± 4.99 | 51.13 (40–57) ± 4.77 | < 0.001 |
| Group 2 | 45.13 (37–56) ± 4.96 | 51.27 (44–61) ± 4.38 | < 0.001 | |
| Group 3 | 46.13 (37–52) ± 4.43 | 51.07 (44–57) ± 4.25 | < 0.001 | |
| NDI | Group 1 | 27.27 (16–34) ± 5.36 | 18.27 (10–26) ± 4.69 | < 0.001 |
| Group 2 | 30.00 (23–34) ± 3.60 | 14.53 (11–24) ± 3.15 | < 0.001 | |
| Group 3 | 28.67 (23–34) ± 3.47 | 13.40 (10–18) ± 2.26 | < 0.001 | |
Values are presented as mean (min–max) ± standard deviation.
Min: minimum, Max: maximum, VNPS: verbal numeric pain scale, ROM: range of motion, R: right, L: left, Lat: lateral, NDI: Neck Disability Index, Group 1: conventional treatment, Group 2: conventional treatment plus deep cervical flexor training, Group 3: conventional treatment plus stabilization of the neck and core region.
There was significant improvement for the differences of pain, NYPS, ROM, and NDI parameters between the groups. The comparison of changes is shown in Table 3. When the source of the difference between the groups was analyzed, statistical significance was recorded between Group 1 and Group 2 in all parameters, between Groups 1 and Group 3 in all parameters except cervical extension and lateral flexion ROM, but no significance was recorded between Groups 2 and Group 3. The P values of the pair group analysis for the significant values are also shown in Table 3.
Table 3.
Comparison of group differences in pre– and post–4–week treatment change scores for pain, posture, ROM, and NDI
| Parameters | Group 1 Δ | Group 2 Δ | Group 3 Δ | P valuea | Groups | P valueb |
|---|---|---|---|---|---|---|
| Pain (VNPS) | –2.93 ± 0.46 | –3.93 ± 0.79 | –4.13 ± 0.83 | < 0.001*** | 1–2 1–3 2–3 |
< 0.001*** < 0.001*** 0.567 |
| Posture | 3.66 ± 4.41 | 8.33 ± 4.87 | 10.33 ± 4.80 | < 0.001*** | 1–2 1–3 2–3 |
0.019* 0.002* 0.389 |
| ROM (degrees) | ||||||
| Flexion | 3.26 ± 1.83 | 6.46 ± 1.50 | 5.20±2.14 | < 0.001*** | 1–2 1–3 2–3 |
< 0.001*** 0.013* 0.081 |
| Extension | 3.20 ± 2.42 | 6.66 ± 2.76 | 5.40±2.69 | < 0.001*** | 1–2 1–3 2–3 |
0.002* 0.056 0.174 |
| R Lat. flexion | 2.73 ± 1.70 | 5.60 ± 1.50 | 4.80±1.89 | < 0.001*** | 1–2 1–3 2–3 |
< 0.001*** 0.011* 0.267 |
| L Lat. flexion | 2.60 ± 2.35 | 5.00 ± 2.03 | 4.53±2.38 | 0.048* | 1–2 1–3 2–3 |
0.023* 0.067 0.775 |
| R rotation | 3.26 ± 2.05 | 5.40 ± 1.95 | 5.13±2.26 | 0.035* | 1–2 1–3 2–3 |
0.021* 0.037* 0.935 |
| L rotation | 2.53 ± 1.99 | 6.13 ± 1.35 | 4.93±2.46 | < 0.001*** | 1–2 1–3 2–3 |
< 0.001*** 0.007* 0.217 |
| NDI | –9.00 ± 2.61 | –15.46 ± 3.44 | –15.26 ± 3.10 | < 0.001*** | 1–2 1–3 2–3 |
< 0.001*** < 0.001*** 0.935 |
Values are presented as mean ± standard deviation.
VNPS: verbal numeric pain scale, ROM: range of motion, R: right, L: left, Lat: lateral, NDI: Neck Disability Index, Δ: difference between assessments, Group 1: conventional treatment, Group 2: conventional treatment plus deep cervical flexor training, Group 3: conventional treatment plus stabilization of the neck and core region.
aKruskal–Wallis test, bMann–Whitney U-test.
*P < 0.05, ***P < 0.001.
DISCUSSION
The aim of this research was to compare the three different treatment programs including conventional therapy, deep cervical flexor muscle training, and cervical-core stabilization exercises in the patients suffering from chronic neck pain. A significant improvement was found in pain, posture, ROM, and NDI variables in all groups. The change after 4 weeks of treatment was higher in Group 2 and Group 3 compared to Group 1. However, there was no significant difference between Group 1 and Group 3 in terms of extension and lateral flexion.
The demographic characteristics of the groups (age, gender, BMI) were recorded. There was no significant difference between the groups in terms of demographic characteristics. McLean et al. [14] stated in their study that there was a higher incidence of neck pain is in women. It was thought that this may have been due to the lower neck muscle strength and endurance in women compared to men. It was shown that the prevalence of neck pain is greater in those over 40 [14]. The average age of the individuals participating in the present study was between 38 in Group 1 and 42 in Group 2 and Group 3. The findings in this study are consistent with the literature in terms of age range. It was observed that more female patients participated (27 female, 18 male).
In a study conducted by Gupta et al. [15] of 30 dentists with chronic neck pain, deep neck flexor training was given to one group, while isometric exercises were given to the other group. At the end of 4 weeks, the NDI for pain and digital photography for the anterior head position were evaluated. Although pain and functionality decreased in both groups, posture improved only in the deep neck flexor group. As a result, deep neck flexor training gives more effective results in people with anterior head position [15]. In the present study, deep neck flexor muscle training was more likely to reduce pain compared to the isometric exercise group. However, in the other group, additionally applied core stabilization exercises were found to be more influential in decreasing pain.
The literature has shown that pressurized biofeedback is effective in treating neck pain. Karthi et al. [16] concluded that endurance exercises with pressure feedback for deep cervical flexor muscles in mechanical neck pain was significantly effective in reducing pain compared to deep cervical flexor exercises with visual biofeedback. Lwin et al. [17] conducted a study of 60 people having neck pain randomly divided into 2 groups, experimental and control. While the experimental group received pressure-biofeedback guided cranio-cervical flexion exercise four times per week for four weeks, the control group received electrotherapy agents (TENS and radiant heat). Visual analogue scale (VAS) and NDI were included. The demographics and outcome measurements, as initial assessments, were not significantly different between the two groups. A more significant reduction in VAS scores was found in the experimental group in comparison with the control group at week 2 and week 4. There was a more significant reduction in the NDI scores in the experimental group than the control group at week 4. The pressure-biofeedback guided cranio-cervical flexion exercise found useful for improving pain and functional disability on neck pain [17]. In the present study, the group in which the exercises were performed with a stabilizer was found to have better results than the conventional group.
Kim and Kwag [18] reported that 28 people with chronic neck pain were studied in the general strengthening exercise group and the deep cervical flexor muscle activation group. NDI and numeric rating scale (NRS) scores were determined and radiological assessment of neck and shoulder postures, neck flexion angle, and forward shoulder angle were evaluated before treatment. Exercises using deep cervical flexor muscle activation were effective to decrease pain, improve neck functions, and maintain correction of head position in patients having neck pain. The deep cervical flexor muscle activation exercises significantly decreased the NRS scores after exercise according to the general strengthening exercise group [18]. In the present study, the pain was significantly reduced after neck stabilization exercises with core stabilization after deep cervical flexor muscle exercises.
Shah et al. [19] studied 30 patients with chronic cases of non-specific neck pain between the ages of 18 and 40 years. Patients were randomly divided into 2 groups. Group A (conventional therapy + core stability exercises group) included 15 patients and Group B (conventional therapy group) included 15 patients. Exercise therapy was applied for 1 month. Results showed that there was a significant difference in VAS scores and deep neck flexor strength between Group A and Group B. Stability exercises applied in addition to conventional physiotherapy was found to be more effective in patients with chronic non-specific neck pain [19]. In the present study, the improvement in the group with core stabilization exercises was the highest, indicating that it showed similar characteristics with this study.
Iqbal et al. [7] divided the patients into two groups in their study with 30 teachers aged 25 to 45 years. The experimental group received deep cervical flexor muscles training with pressure biofeedback and conventional exercises (stretching and strengthening exercises). The control group received deep cervical flexor muscles training with only conventional exercises. Pain status was assessed using an NRS and functional disability was assessed using the NDI. In this 4-week study, there was significant improvement in NRS and NDI scores in both the groups and the results were better in the deep cervical flexor group. The addition of pressure biofeedback for deep cervical flexor muscles training gave a better result than conventional exercises alone [7].
The superiority of deep neck flexor exercise in pain outcomes compared to isometric, stretching, and scapulothoracic exercises was established in another randomized clinical trial [20]. In the present study, there was a significant improvement in the group doing deep cervical flexor training with biofeedback compared to those who did isometric exercises. However, there is no significant difference between the core exercise group and the deep cervical flexor training group.
Kim et al. [21] studied 25 students who had forward head postures that was caused by excessive use of smartphones. They were divided into a deep neck flexor training group and an extension-based Mackenzie exercise group for four weeks. Their study examined NDI scores, changes in the degree of respiratory function with the device evaluating pulmonary volumes and ventilation, and the test of deep cervical flexors with a biofeedback unit after the treatment. Evaluation of forward vital capacity and the degree of breathing in expiratory volumes resulted in no statistically significant changes in the pressure biofeedback unit-based deep cervical flexor training exercise group and the McKenzie cervical exercise group. However, it revealed statistically significant changes in NDI scores in both groups [21]. In the present study, the cervical stabilization exercise group proved more effective in improving the NDI scores compared to the conventional treatment group. However, there is no significant difference between the additional core stabilization exercise group with cervical stabilization and the cervical stabilization group.
In a study conducted by Kang [22], cervical ROM was evaluated in 20 students after deep cervical flexor muscle training with a pressure biofeedback device and conventional deep cervical flexor training for six weeks. Cervical ROM increased significantly in a group receiving deep cervical flexor training compared to another group that performed chin tucks, stretching, and ROM exercises. So, deep cervical flexor training with a pressure biofeedback device is an effective method for increasing neck movement and muscular endurance in people with forward head posture [22].
Lee and Shin [23] evaluated 44 patients suffering neck pain divided into three groups: a neuromuscular control exercise group (upper limb pattern rolling exercises), a self-stretch group, and a neck stabilization exercise with the pressure biofeedback device group. In comparison, the neuromuscular control exercise group showed a significant reduction in pain in comparison to the results of the other two groups. However, there was no significant difference in ROM values of the groups after treatment [23]. In the present study, ROM increased in all groups. While there was a significant difference in all values between Group 1 and Group 2, a significant difference was found between Group 1 and Group 3 in all values except neck extension and neck left lateral flexion. In the comparison of these values, there was no significant difference between Group 2 and Group 3 in all parameters. According to these results, adding cervical stabilization exercises to classical neck pain treatment is important for the development of ROM. However, the application of core stabilization exercises did not affect the neck ROM.
Unlike the authors’ study, Raju et al. [24] divided seventy patients with a diagnosis of chronic neck pain into two groups. Deep neck flexor muscle training was performed on a group with a pressurized biofeedback device. The neck stabilization exercise group performed chin tucks for deep cervical flexor muscles, cervical extensions, shoulder shrugs, and shoulder rolls exercises to relieve muscle tension. As a result of the 4-week study, VAS, NDI, and muscle test scores were improved effectively in both groups [24]. In the present study, the group was given a combination of deep neck flexor muscle group exercises and neck stabilization exercises. Compared to the conventional exercise group, this approach is more significant in all parameters of the treatment.
Since neck pain is a chronic condition, it is important that treatment methods applied to patients improve long-term pain and disability. In the present study, long-term follow-up evaluations could not be made due to the education, work life, as well as socio-cultural and economic conditions of the patients. Therefore, in addition to these exercises, it is beneficial to conduct future studies to investigate and compare the long-term effects of neck stabilization exercises and core stabilization exercises, and to determine effective treatment approaches in physiotherapy and rehabilitation science.
A long-term exercise program should be given to see the effectiveness of exercise therapy. In this study, the treatment program was applied to patients for 4 weeks, 3 days a week, for a total of 12 sessions. Significant improvements were observed in the patients during this period as well.
The assessment of the patients had to be measured by the specific head posture rather than assessing the general posture with Reedco’s posture scale. This can be evaluated with objective neck posture-specific methods. If this assessment could be made, the effect of stabilization exercises on the region could be better demonstrated, especially due to the relationship between the forward head posture and decreased deep cervical muscle strength. In the present study, the postural changes which were evaluated were limited, and the cervical region muscle strength was not evaluated.
The effectiveness of the three treatment programs was not compared with a control group that received no treatment. A non-treatment group could not be created because the patients who came to the clinic had pain.
Implementation of three different exercise programs is one of the strengths of this study. In this way, the effectiveness of different exercise approaches were evaluated with each other.Another strength of this study is that significant improvements were also observed in the patients, although patients went through a total of 12 sessions: 4 weeks, 3 days a week.
It can be concluded that both deep cervical flexion muscle training and cervical-core stabilization exercises combined with conventional treatment may be more effective for pain, posture, ROM and disability than the conventional therapy alone.
The authors suggest that the combined use of both deep flexor muscle trainings and stabilization exercises clinically may provide good long-term results in patients with neck pain. The effects of both treatment methods, which were observed to have similar effects in this study, can be better demonstrated in future studies with long-term follow-up.
Funding Statement
FUNDING No funding to declare.
Footnotes
DATA AVAILABILITY
All data produced in the present study are available upon reasonable request to the authors. The data are not publicly available due to the restriction of the Ethics Committee, because it contains information that could compromise the privacy of research participants.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Besta Hazal Gumuscu: Conception, data interpretation, methodology, draft and revision, final approval of the work; Eylul Pinar Kisa: Methodology, data interpretation, draft and revision, final approval of the work; Begum Kara Kaya: Data interpretation, draft and revision, final approval of the work; Rasmi Muammer: Draft and revision, final approval of the work.
REFERENCES
- 1.Cox LG, Kidgell DJ, Iles RA. Neck-specific strengthening exercises and cognitive therapy for chronic neck pain: a systematic review. Phys Ther Rev. 2019;24:335–45. doi: 10.1080/10833196.2019.1664081. [DOI] [Google Scholar]
- 2.Cunha AC, Burke TN, França FJ, Marques AP. Effect of global posture reeducation and of static stretching on pain, range of motion, and quality of life in women with chronic neck pain: a randomized clinical trial. Clinics (Sao Paulo) 2008;63:763–70. doi: 10.1590/S1807-59322008000600010.4c0e916b5a19421ea05a4f2e39a976c7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Im B, Kim Y, Chung Y, Hwang S. Effects of scapular stabilization exercise on neck posture and muscle activation in individuals with neck pain and forward head posture. J Phys Ther Sci. 2016;28:951–5. doi: 10.1589/jpts.28.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mustafaoglu R, Yasaci Z, Zirek E, Griffiths MD, Ozdincler AR. The relationship between smartphone addiction and musculoskeletal pain prevalence among young population: a cross-sectional study. Korean J Pain. 2021;34:72–81. doi: 10.3344/kjp.2021.34.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yip CH, Chiu TT, Poon AT. The relationship between head posture and severity and disability of patients with neck pain. Man Ther. 2008;13:148–54. doi: 10.1016/j.math.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Falla D, Jull G, Russell T, Vicenzino B, Hodges P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther. 2007;87:408–17. doi: 10.2522/ptj.20060009. [DOI] [PubMed] [Google Scholar]
- 7.Iqbal ZA, Rajan R, Khan SA, Alghadir AH. Effect of deep cervical flexor muscles training using pressure biofeedback on pain and disability of school teachers with neck pain. J Phys Ther Sci. 2013;25:657–61. doi: 10.1589/jpts.25.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marco CA, Marco AP, Plewa MC, Buderer N, Bowles J, Lee J. The verbal numeric pain scale: effects of patient education on self-reports of pain. Acad Emerg Med. 2006;13:853–9. doi: 10.1197/j.aem.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 9.Chiu TT, Lam TH, Hedley AJ. Correlation among physical impairments, pain, disability, and patient satisfaction in patients with chronic neck pain. Arch Phys Med Rehabil. 2005;86:534–40. doi: 10.1016/j.apmr.2004.02.030. [DOI] [PubMed] [Google Scholar]
- 10.Thawinchai N, Funprom K. Effect of carrying style on posture score in adolescents with musculoskeletal pain. Chiang Mai Univ J Nat Sci. 2019;18:553–61. doi: 10.12982/CMUJNS.2019.0036. [DOI] [Google Scholar]
- 11.Özer Kaya D, Toprak Çelenay Ş. Effectiveness of relaxation training in addition to stabilization exercises in chronic neck pain: a randomized clinical trial. Turk J Physiother Rehabil. 2019;30:145–53. doi: 10.21653/tjpr.665131. [DOI] [Google Scholar]
- 12.Shin YJ, Kim WH, Kim SG. Correlations among visual analogue scale, neck disability index, shoulder joint range of motion, and muscle strength in young women with forward head posture. J Exerc Rehabil. 2017;13:413–7. doi: 10.12965/jer.1734956.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sullivan GM, Feinn R. Using effect size-or why the P value is not enough. J Grad Med Educ. 2012;4:279–82. doi: 10.4300/JGME-D-12-00156.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McLean SM, May S, Klaber-Moffett J, Sharp DM, Gardiner E. Risk factors for the onset of non-specific neck pain: a systematic review. J Epidemiol Community Health. 2010;64:565–72. doi: 10.1136/jech.2009.090720. [DOI] [PubMed] [Google Scholar]
- 15.Gupta BD, Aggarwal S, Gupta B, Gupta M, Gupta N. Effect of deep cervical flexor training vs. conventional isometric training on forward head posture, pain, neck disability index in dentists suffering from chronic neck pain. J Clin Diagn Res. 2013;7:2261–4. doi: 10.7860/JCDR/2013/6072.3487.8cbc06c274a34b5497821acb3a7bf5a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karthi M, Gopalswami AD, Aseer AL. Efficacy of endurance training on deep cervical flexor muscles using pressure feedback in mechanical neck pain. Int J Physiother. 2019;6:95–101. doi: 10.15621/ijphy/2019/v6i3/183878.f249b6e11be245a199472bc5390240d5 [DOI] [Google Scholar]
- 17.Lwin NN, Myint T, Oo WM, San HH, Tun MT. Efficacy on pressure-biofeedback guided craniocervical flexion exercise in neck pain: a randomized controlled trial. J Musculoskelet Res. 2021:doi: 10.1142/S0218957721500135. doi: 10.1142/S0218957721500135. [DOI] [Google Scholar]
- 18.Kim JY, Kwag KI. Clinical effects of deep cervical flexor muscle activation in patients with chronic neck pain. J Phys Ther Sci. 2016;28:269–73. doi: 10.1589/jpts.28.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah N, Gill MA, Singal SK, Payla M. Effect of core stability exercise in patients with neckpain. Indian J Physiother Occup Ther. 2020;14:102–7. doi: 10.37506/ijpot.v14i4.11308. [DOI] [Google Scholar]
- 20.Abdel-aziem AA, Draz AH. Efficacy of deep neck flexor exercise for neck pain: a randomized controlled study. Turk J Phys Med Rehabil. 2016;62:107–15. doi: 10.5606/tftrd.2016.84565. [DOI] [Google Scholar]
- 21.Kim EY, Kim KJ, Park HR. Comparison of the effects of deep neck flexor strengthening exercises and Mackenzie neck exercises on head forward postures due to the use of smartphones. Indian J Sci Technol. 2015;8(Suppl 7):569–75. doi: 10.17485/ijst/2015/v8iS7/70462. [DOI] [Google Scholar]
- 22.Kang DY. Deep cervical flexor training with a pressure biofeedback unit is an effective method for maintaining neck mobility and muscular endurance in college students with forward head posture. J Phys Ther Sci. 2015;27:3207–10. doi: 10.1589/jpts.27.3207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee JD, Shin WS. Immediate effects of neuromuscular control exercise on neck pain, range of motion, and proprioception in persons with neck pain. Phys Ther Rehabil Sci. 2020;9:1–9. doi: 10.14474/ptrs.2020.9.1.1. [DOI] [Google Scholar]
- 24.Raju AS, Apparao P, Swamy G, Chaturvadi P, Mounika RG. A comparative study on deep cervical flexors training and neck stabilization exercises in subjects with chronic neck pain. Indian J Physiother Occup Ther. 2019;13:1–5. doi: 10.5958/0973-5674.2019.00035.2. [DOI] [Google Scholar]