Abstract
Introduction
Trauma patients are twice as likely to be uninsured as the general population, which can lead to limited access to postinjury resources and higher mortality. The Hospital Presumptive Eligibility (HPE) program offers emergency Medicaid for eligible patients at presentation. The HPE program underwent several changes during the COVID-19 pandemic; we quantify the program's success during this time and seek to understand features associated with HPE approval.
Methods
A mixed methods study at a Level I trauma center using explanatory sequential design, including: 1) a retrospective cohort analysis (2015-2021) comparing HPE approval before and after COVID-19 policy changes; and 2) semistructured interviews with key stakeholders.
Results
589 patients listed as self-pay or Medicaid presented after March 16, 2020, when COVID-19 policies were first implemented. Of these, 409 (69%) patients were already enrolled in Medicaid at hospitalization. Among those uninsured at arrival, 160 (89%) were screened and 98 (61%) were approved for HPE. This marks a significant improvement in the prepandemic HPE approval rate (48%). In adjusted logistic regression analyses, the COVID-19 period was associated with an increased likelihood of HPE approval (versus prepandemic: aOR, 1.64; P = 0.005). Qualitative interviews suggest that mechanisms include state-based expansion in HPE eligibility and improvements in remote approval such as telephone/video conferencing.
Conclusions
The HPE program experienced an overall increased approval rate and adapted to policy changes during the pandemic, enabling more patients’ access to health insurance. Ensuring that these beneficial changes remain a part of our health policy is an important aspect of improving access to health insurance for our patients.
Keywords: Access, Disparities, Health policy, Medicaid, Trauma
Introduction
Trauma patients are twice as likely to lack healthcare insurance when seeking care than the general population (13% versus 6.8%).1 The consequences of their lack of insurance have been well-described in the literature, including higher mortality rates and more limited access to postinjury care, such as mental health services and rehabilitation.2 Not only do uninsured patients endure significant damage to their health, but they also face significant financial sequelae, with 90% accruing catastrophic health expenditures.3 The Congressional Budget Office estimated the number of uninsured individuals was 31-32 million at the end of 2020.4 In addition, from February to July 2020, the COVID-19 pandemic left an estimated 12 million individuals without employer-sponsored health insurance coverage due to job losses.5 Medicaid is likely the primary alternative source of coverage for those who have lost their employer-sponsored health insurance coverage during the pandemic.
Hospital Presumptive Eligibility (HPE) through the Affordable Care Act grants eligible uninsured patients temporary Medicaid coverage for up to 60 days, who must then apply separately to obtain long-term Medicaid insurance coverage.6 , 7 The HPE program underwent several policy changes due to the COVID-19 pandemic. The Department of Healthcare Services and the State of California approved immediate changes to HPE approval policies, including the expansion of two periods of presumptive eligibility within 12 months and a move to semiremote work, including a “COVID-19 protocol,” enabling telephone approvals for patients no longer at the hospital.8 , 9 However, there is a lack of formal data related to patient and hospital factors influencing HPE eligibility and participation during the COVID-19 pandemic.
We sought to evaluate the changes in the HPE program during the COVID-19 pandemic and assessed whether the policy changes implemented over this period were associated with improvements in the HPE approval rate compared to the pre-COVID-19 period.
Materials and Methods
Data source and study population
We conducted an explanatory mixed methods study which included a chart review and quantitative analysis of our single-center trauma registry, as well as qualitative semistructured interviews of key stakeholders involved with the HPE process at our institution.10
We identified patients between the ages 18-64 who presented with Medicaid coverage or no insurance (self-pay) to our Level I trauma center between 2015 and 2021. 2015 was the first year when financial counselors documented HPE application information within the electronic medical record chart. We excluded patients who died in hospital, had burn injuries, or had additional non-Medicaid payment (e.g., worker's compensation). For patients with multiple trauma visits during the relevant period, we selected only their first visit. We analyzed two distinct periods, before and during the COVID-19 pandemic, defined as beginning on March 16, 2020, in conjunction with our county-based COVID-19 mitigation policies.8 , 9
Electronic health record review
Two raters (T.J.H., A.C.B.) reviewed financial counselor and social worker notes in patients' electronic medical records to determine insurance status at arrival, as insurance status in the registry is captured at discharge. Financial counselors’ free-text notes within the medical record were reviewed to abstract screenings for insurance coverage, receipt of inhospital HPE insurance, referral for follow-up Medicaid coverage services, and reasons for coverage denial. A subset of the charts (n = 60) was scored independently by two raters to determine interrater reliability. Following four rounds of review, scoring discrepancies were discussed to ensure the continuity of scoring the remaining charts. In the first round, raters achieved 88% agreement with a kappa = 0.76, in the second round, 92% agreement and kappa = 0.69, in the third round, 92% agreement and kappa = 0.72, in the final round, the raters achieved 98% agreement and improved kappa = 0.94. Overall, raters independently achieved strong agreement (93%, kappa = 0.75).
Statistical analysis
Our primary outcome was HPE approval. We evaluated unadjusted differences between uninsured and HPE-approved patients at discharge using χ2 or Fisher's exact tests for categorical variables and Wilcoxon rank-sum tests for continuous variables. We developed a multivariate logistic regression model to assess predictors of HPE approval before and during COVID-19. Preselected model variables were based on the previously published literature.11 These included demographic variables (age, sex, race, and ethnicity), markers of clinical severity (e.g., Injury Severity Score [ISS], Glasgow Coma Scale [GCS], and whether a surgical procedure was required), temporal dynamics of case presentation (day of presentation: i.e., weekday or weekend; and time: i.e., day [7 AM-7 PM] or night [7 PM-7 AM]), and a COVID-19 time period indicator. To ensure the validity of our findings, we conducted a sensitivity analysis with a reduced logistic regression model with fewer dichotomized covariates to decrease the degrees of freedom. We assessed the trend in HPE approval rates for patients eligible for HPE across study years, both visually and quantitatively, using a chi-squared test for trend in proportion. Statistical significance was assessed at the level of α = 0.05 (two-tailed test). All statistical analyses were performed using R.12 Retrospective data were de-identified, and thus informed consent was waived. Informed consent was obtained from all interview participants. The Stanford University Institutional Review Board approved this research study (protocol number IRB-54789).
Stakeholder interviews
We conducted seven in-depth semistructured key stakeholder interviews with staff (financial counselors, social workers, and contractors) who were involved with the coverage determination, screening, approval, and sustainment of HPE at our institution. These were designed to explain and provide context for the initial quantitative results, in particular, to elicit which elements of policy implemented due to the COVID-19 pandemic affected HPE approval.13
Interviews were conducted via videoconference by two of the authors (A.C.B., T.J.H.). The interviews were conducted by both interviewers: one led the conversation while the other took thematic notes and asked clarifying questions. Immediately after each interview, the interviewers met to discuss first impressions and major themes, and then each interviewer separately wrote memos summarizing their observations. Each interview was transcribed through Zoom automatic transcriptions and then cross-checked by our research analyst to ensure that the automatic transcriptions matched the voice-recorded interviews accurately. Transcripts were examined for underlying thematic mechanisms which may explain differences in policy before and after the beginning of the COVID-19 period. Information revealed from the interviews with financial counselors provided context for COVID-19 policy changes.
Qualitative analysis
All interviews were audio recorded, transcribed verbatim, and de-identified. We performed a thematic analysis of transcripts concurrent with data collection.14 We used an inductive approach to create the codebook. Two investigators independently identified preliminary codes from three interviews, and then the whole research team met to discuss, revise, and confirm codes to be entered into a codebook with agreed-upon definitions. In any event that coders could not reach an agreement, coding was adjudicated by the Principal Investigator. Then, we conducted two full cycles of coding.15 During the first cycle of coding, two raters separately applied the finalized codebook to all interviews. During the second cycle of coding, the raters together went through each individual transcript and discussed all codes to reach an agreement on the best code applications. The whole research team frequently met to discuss the refinement of codes and themes. We used NVivo software (QSR International) to assist with qualitative data analysis and interpretation. We validated findings from coding and analysis through triangulation, member-checking, and search for disconfirming evidence.16 We considered thematic saturation to be achieved when we had interviewed stakeholders from all parts of the HPE approval process, and when no new themes were identified from three sequential interviews.
Results
Quantitative findings
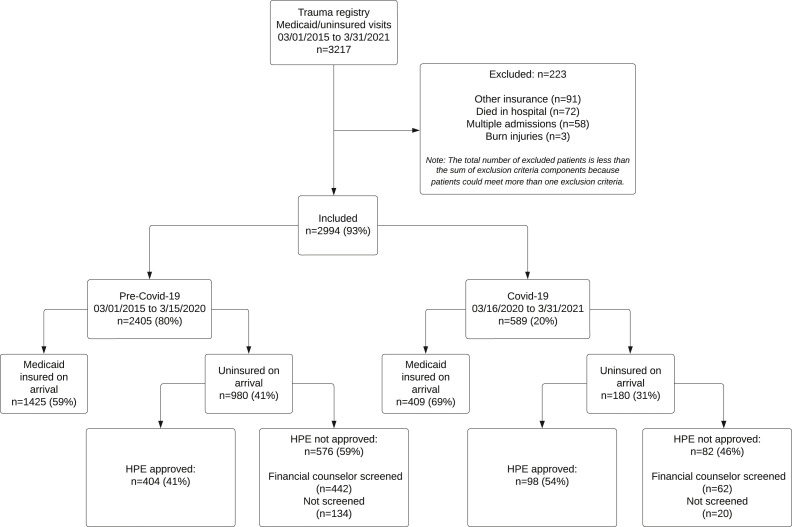
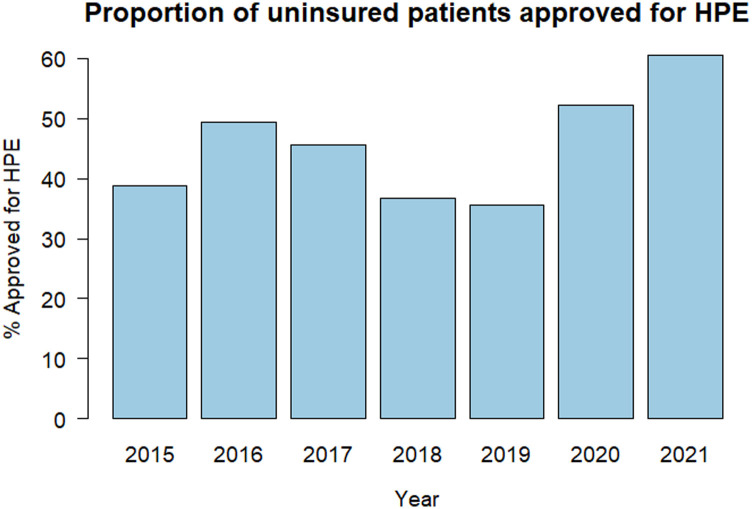
Between 2015 and 2021, there were 3217 uninsured or Medicaid visits documented in the trauma registry. A total of 223 visits were excluded, and 2994 visits met the inclusion criteria. During the COVID-19 period (March 16, 2020, to March 31, 2021), a total of 589 trauma patients with Medicaid or uninsured status at presentation were included in the trauma registry. Of the 589 patients who met the inclusion criteria, 409 (69%) had Medicaid at the time of hospitalization and 180 (31%) were uninsured. Among uninsured patients, 160 (89%) were screened for HPE and 98 (61%) were approved for HPE, compared to 846 (86%) screened and 404 (48%) approved among 980 uninsured patients during the pre-COVID-19 period (Fig. 1 ). Among all uninsured patients, screened or not, 41% were approved for HPE during the pre-COVID-19 period and 54% were approved during the COVID-19 period, representing a 13-point improvement in HPE approval. HPE approval rates across the study years are shown in Figure 2 . There was no statistically significant trend in proportion over time (P = 0.28).
Fig. 1.
Study participant flow diagram for Medicaid status and HPE approval.
Fig. 2.
HPE approval rates year to year.
Using unadjusted analyses, we compared the characteristics of uninsured patients who were either HPE approved or unapproved for the two time periods (pre-COVID-19 and COVID-19) (Table 1 ). Patient characteristics (age, sex, race, and ethnicity) and temporal characteristics of the Emergency Room presentation (day and time) were similar between the two time periods for both HPE-approved and nonapproved patients. Among the examined clinical characteristics, GCS, ISS, and mechanism of injury were not statistically different between pre-COVID-19 and COVID-19 patients for either HPE-approved or nonapproved patients. Among the HPE approved, pre-COVID-19 patients had more blunt injuries than those in the COVID-19 period (90.3% versus 82.7% P = 0.046), while injury types among the nonapproved were not statistically different across the time periods.
Table 1.
Patient and clinical utilization characteristics of uninsured trauma patients who were approved or not approved for the hospital presumptive eligibility (HPE) program.
| Patient and clinical utilization characteristics | HPE approved, n (%) |
HPE not approved, n (%) |
||
|---|---|---|---|---|
| Pre-COVID-19 |
COVID-19 |
Pre-COVID-19 |
COVID-19 |
|
| n = 404 (80) | n = 98 (20) | n = 576 (87) | n = 82 (13) | |
| Patient characteristics | ||||
| Age, median (IQR) | 33 (18) | 34.5 (17) | 30 (19) | 30 (16) |
| Age category | ||||
| 18-24 | 78 (19.3) | 20 (20.4) | 147 (25.5) | 17 (20.7) |
| 25-44 | 230 (56.9) | 54 (55.1) | 294 (51.0) | 51 (62.2) |
| 45-64 | 96 (23.8) | 24 (24.5) | 135 (23.4) | 14 (17.1) |
| Gender | ||||
| Female | 76 (18.8) | 12 (12.2) | 121 (21.0) | 17 (20.7) |
| Male | 328 (81.2) | 86 (87.8) | 455 (79.0) | 65 (79.3) |
| Race | ||||
| Asian | 16 (4.0) | <10 (<10.2) | 36 (6.3) | <10 (<12.2) |
| African American/Black | 23 (5.7) | <10 (<10.2) | 24 (4.2) | <10 (<12.2) |
| White | 121 (30.0) | 24 (24.5) | 139 (24.1) | 18 (22.0) |
| Other | >234 (>57.9) | 66 (67.3) | >367 (>63.7) | 52 (63.4) |
| Unknown | <10 (<2.5) | <10 (<10.2) | <10 (<1.7) | <10 (<12.2) |
| Ethnicity | ||||
| Hispanic or Latino | >227 (>56.2) | >51 (>52.0) | >311(>54.0) | >34 (>41.5) |
| Non-Hispanic or Latino | 167 (41.3) | 38 (38.8) | 255 (44.3) | 38 (46.3) |
| Unknown | <10 (<2.5) | <10 (<10.2) | <10 (<1.7) | <10 (<12.2) |
| Clinical characteristics | ||||
| GCS on arrival | ||||
| Severe (<8) | 21 (5.2) | <10 (<10.2) | 10 (1.7) | <10 (<12.2) |
| Moderate (9-12) | 12 (3.0) | <10 (<10.2) | 25 (4.3) | <10 (<12.2) |
| Mild (13-15) | 354 (87.6) | 88 (89.8) | 527 (91.5) | 75 (91.5) |
| Unknown | 17 (4.2) | <10 (<10.2) | 14 (2.4) | <10 (<12.2) |
| ISS category | ||||
| Minor (0-8) | 230 (56.9) | 51 (52.0) | >398 (>69.1) | 57 (69.5) |
| Moderate (9-15) | 88 (21.8) | 22 (22.5) | 69 (12.0) | 12 (14.6) |
| Major (16-25) | 37 (9.2) | 12 (12.3) | 28 (4.9) | <10 (<12.2) |
| Severe (>25) | 23 (5.7) | <10 (<10.2) | <10 (<1.7) | <10 (<12.2) |
| Unknown | 26 (6.4) | <10 (<10.2) | 71 (12.3) | <10 (<12.2) |
| Injury type | ||||
| Blunt | 365 (90.3) | 81 (82.7) | 526 (91.3) | >72 (>87.8) |
| Penetrating | 39 (9.7) | 17 (17.3) | 50 (8.7) | <10 (<12.2) |
| Mechanism of injury | ||||
| Assault | 35 (8.7) | 16 (16.3) | 43 (7.5) | 11 (13.4) |
| Bicycle/pedestrian | 60 (14.9) | 12 (12.2) | 66 (11.5) | <10 (<12.2) |
| Fall | 67 (16.6) | 21 (21.4) | 80 (13.9) | <10 (<12.2) |
| Gunshot/stabbing | 29 (7.2) | <10 (<10.2) | 33 (5.7) | <10 (<12.2) |
| Motorcycle crash/motor vehicle crash | 188 (46.5) | 34 (34.7) | 313 (54.3) | 44 (53.7) |
| Other/unknown | 25 (6.2) | <10 (<10.2) | 41 (7.1) | <10 (<12.2) |
| Temporal characteristics of ER presentation | ||||
| Day | ||||
| Weekend (Saturday-Sunday) | 148 (36.6) | 45 (45.9) | 199 (34.5) | 25 (30.5) |
| Weekday (Monday-Friday) | 256 (63.4) | 53 (54.1) | 377 (65.5) | 57 (69.5) |
| Time | ||||
| Day (7AM to 7PM) | 210 (52.0) | 56 (57.1) | 274 (47.6) | 38 (46.3) |
| Night (7PM to 7AM) | 194 (48.0) | 42 (42.9) | 302 (52.4) | 44 (53.7) |
GCS = Glasgow Coma Scale; ISS = Injury Severity Score; IQR = interquartile range; ER = emergency room.
The adjusted logistic regression model indicated that trauma patients who visited the Emergency Room during COVID-19 had a higher likelihood of HPE approval compared to the pre-COVID-19 trauma patients (adjusted Odds Ratio [aOR] = 1.64, P = 0.005) (Table 2 ). Additionally, race and ethnicity affected odds of HPE approval. Compared to White trauma patients, those who classified their race as Asian were less likely to receive HPE approval (aOR = 0.49, P = 0.02) and those of Hispanic or Latino ethnicity had an increased odds of HPE approval than Non-Hispanic/Latino patients (aOR = 1.51, P = 0.01). Furthermore, trauma patients admitted at night (7 PM to 7 AM) compared to day (7 AM to 7 PM) were 0.77 times as likely to receive HPE approval (aOR = 0.77, P = 0.04). ISS was significantly associated with a progressive increased odds of HPE approval (reference: minor [ISS 0-8], moderate [ISS 9-15] aOR = 2.25, P < 0.001, major [16-25] aOR = 2.50, P < 0.001, and severe [>25] aOR = 4.72, P < 0.001). We also report how the percentage of patients who were screened for HPE varies by ISS (Table 3 ). The sensitivity analysis using the reduced model had quantitatively similar results (See Supplementary Table 1).
Table 2.
Logistic regression analysis of significant predictors of HPE success among uninsured trauma patients.
| HPE approval | Adjusted OR | 95% CI | P value |
|---|---|---|---|
| COVID-19 period | 1.64 | 1.16-2.33 | 0.005 |
| Male sex | 1.02 | 0.75-1.40 | 0.89 |
| Age, years | |||
| 18-24 | Ref | ||
| 25-44 | 1.28 | 0.94-1.75 | 0.12 |
| 45-64 | 1.23 | 0.84-1.79 | 0.29 |
| Race | |||
| White | Ref | ||
| Asian | 0.49 | 0.26-0.90 | 0.02 |
| African American/Black | 1.21 | 0.66-2.21 | 0.54 |
| Other | 0.71 | 0.50-1.01 | 0.05 |
| Unknown | 1.05 | 0.12-11.25 | 0.97 |
| Ethnicity | |||
| Non-Hispanic or Latino | Ref | ||
| Hispanic or Latino | 1.51 | 1.09-2.10 | 0.01 |
| Unknown | 1.50 | 0.19-10.35 | 0.67 |
| Night admission (7PM to 7AM) | 0.77 | 0.60-0.98 | 0.03 |
| Weekend admission (Saturday-Sunday) | 1.13 | 0.87-1.46 | 0.35 |
| ISS | |||
| Minor (0-8) | Ref | ||
| Moderate (9-15) | 2.25 | 1.61-3.16 | <0.001 |
| Major (16-25) | 2.50 | 1.53-4.13 | <0.001 |
| Severe (>25) | 4.72 | 2.18-11.13 | <0.001 |
| Unspecified | 0.69 | 0.43-1.06 | 0.10 |
| GCS | |||
| Mild (13-15) | Ref | ||
| Moderate (9-12) | 0.70 | 0.35-1.34 | 0.23 |
| Severe (≤8) | 1.57 | 0.75-3.35 | 0.29 |
| Unknown | 1.84 | 0.89-3.90 | 0.10 |
| Operating room procedure | 0.96 | 0.73-1.25 | 0.74 |
Table 3.
Proportion of patients screened for HPE by injury severity score (ISS).
| ISS | Screened (%) | Not screened (%) |
|---|---|---|
| Minor injury (0-8) | 84% | 16% |
| Moderate injury (9-15) | 96% | 4% |
| Major injury (16-25) | 97% | 3% |
| Severe injury (>25) | 92% | 8% |
| Unspecified | 75% | 25% |
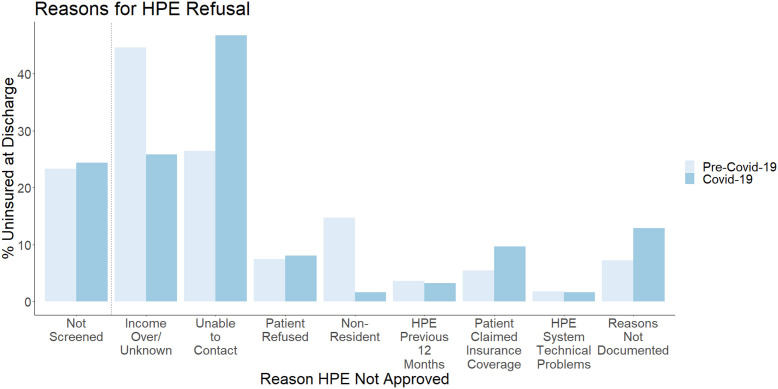
Various policy and personal reasons prevented uninsured patients from receiving HPE approval. Participants could identify more than one reason why HPE approval was denied, therefore, the sum of the following percentages and the percentages in Figure 3 exceed 100%. When examining the pre-COVID-19 uninsured patients, 576 did not receive HPE approval. 134 of the 980 uninsured patients (14%) were not screened for HPE. Among the 442 who were screened but not approved, 197 (45%) had an income that was either over the HPE limit or was unknown, 117 (27%) were unable to be contacted, and 33 (8%) cases where the patient refused HPE, 65 (15%) were nonresidents, 16 (4%) had already received HPE in the past year, 24 (5%) claimed other insurance coverage, 8 (2%) had HPE system technical issues, and 32 (7%) the reason for HPE refusal was not documented. Following the same structure, the COVID-19 group had 82 uninsured patients who did not receive HPE approval, 20 of the 180 uninsured patients (11%) were not screened for HPE. Among the 62 screened but not approved patients, 16 (26%) had an income that was either over the HPE limit or was unknown, 29 (47%) were unable to be contacted, 5 (8%) patients refused HPE, 1 (2%) was a nonresident, 2 (3%) had already received HPE in the past year, 6 (10%) claimed other insurance coverage, 1 (2%) had HPE system technical issues, and for 8 (12%) the reason for HPE refusal was not documented (Fig. 3).
Fig. 3.
Reasons for HPE denial for pre-COVID-19 and COVID-19 periods.
Qualitative findings—mechanisms of change
Stakeholder interviewees indicated two explanatory mechanisms for higher HPE approvals during COVID-19: an improvement in remote approval (via telephone/videoconferencing) and state-based expansion in HPE approval eligibility.
Before the COVID-19 era, patients were only eligible for HPE approval once in a 12-month period. During COVID-19, patients are now eligible for HPE approval up to twice within a 12-month period. The pandemic also sparked the launch of COVID-19-specific HPE coverage, which covers the costs of COVID-19-related medical expenses without restrictions based on maximum household income. Therefore, as highlighted by a financial counselor who participated in our study, anyone who “comes in for any COVID-19-related service or is diagnosed with COVID-19, is automatically eligible [to apply for HPE coverage], regardless of household income or age.” Those more inclusive eligibility criteria might have facilitated utilization of the HPE process because, according to the interviewed social worker, “[patients without] health insurance were probably waiting or did not go to the doctor and coming into the hospital when it was too late [and] they were already very sick. [Therefore], there's an uptick in patients who were screened or qualified for HPE.” In result, as one of the case managers stated, health plans were “inundated with referrals and applications,” in need of processing during the pandemic.
In addition to improved eligibility criteria, there were some logistical changes implemented as a result of the COVID-19 pandemic. Improvements in remote approvals were largely attributed to the use of telephone and videoconferencing, such as video meetings with families to complete discussions regarding eligibility criteria for HPE. The majority of applications were processed remotely in the COVID-19 period. As one of the contractors stated: “six out of ten patients [are processed for HPE] over the phone.” Reductions in time to physically reach patients and family members allowed for more time to process applications. Several stakeholders also identified ongoing challenges with the program, including remote communication issues. A case manager stated during an interview that “in-person communication is preferred when fostering a relationship of trust between insurance providers, healthcare workers, and patients.” There is a significant amount of personal information required for the application process, which can be difficult to elicit by phone or videoconference without in-person meetings. Additionally, there were patients and families who lacked access to email or telephones, resulting in more difficulties applying during the pandemic.
Discussion
We found that the policies introduced during the COVID-19 pandemic were associated with an increase in the overall approval rate for patients eligible for HPE from 41% to 54%. These policy changes were associated with more people gaining access to health insurance in the 60 days following their injury. Further study is needed to investigate whether patients who received HPE went on to sustain coverage through Medicaid or other insurance postdischarge.
The HPE program underwent several policy changes due to the COVID-19 pandemic, with eligibility criteria changes and the implementation of remote work for financial counselors. The results of this eligibility expansion were reflected in our results, which showed that these changes were associated with a decrease in HPE denials in those who had received HPE in the past 12 months. This, along with adaptations to the monthly income limit for household size, is a possible mechanism for the increase in HPE approvals.
The policy changes to enable a move to semiremote work are associated with improved overall screening of patients for HPE eligibility. The interviews suggested that remote communication enabled applications to be completed faster, reducing the time from identifying an eligible patient to granting HPE coverage. Due to COVID-19 restrictions on physical contact, verbal consent was permitted in place of signed paperwork. According to the interviewed stakeholders, this step was also associated with faster processing. Providers may also obtain the required information to assist with HPE enrollment through an authorized representative of the patient. Similarly, patients were able to apply online using the state's online portal in order to secure ongoing Medicaid eligibility after their HPE period. However, ongoing challenges remain related to patient refusal and difficulty in making contact once they have left the hospital. Detailed qualitative interviews at the patient level are required to understand the reasons behind patient refusal and loss to follow-up. However, these issues suggest an opportunity for patient education surrounding the benefits of sustained insurance coverage as well as the potential for streamlining the HPE application process.
As in our previous work, we noted that patients who were HPE approved during the COVID-19 period had a higher ISS, likely reflecting a more complex clinical course and increasing the need for postacute services.11 These findings may reflect the fact that patients with higher injury severity are more likely to be admitted and have the opportunity to be screened. Within our sample of patients we found that as ISS increased from minor to major injuries, HPE screening increased (84%, 96%, 97%), though those with severe ISS had a slightly lower, yet still high chance of being screened (92%). Similarly, the reduced adjusted odds of HPE approval if patients were hospitalized overnight may reflect sparse staffing during off hours (7 PM-7 AM), leading to reductions in screening and subsequent approval. The COVID-19 HPE approval policy changes were associated with differential changes between racial and ethnic groups, most notably with a reduction in the chances of HPE approval in White patients (30.0% versus 24.4%), however, many of the groups were too small to determine statistical significance in this study.
Our study has several limitations. It is retrospective and limited to a single center, which may limit the generalizability of our findings. In addition, insurance screening, HPE coverage determination, and reasons for HPE nonapproval were determined from free-text notations in patients' electronic medical records. These notations taken by financial counselors were difficult to standardize. We did not have access to patient Medicaid claims records after discharge that would enable us to determine whether insurance coverage was sustained after the 60-day HPE period.
In summary, our findings can inform future directions and modifications in policies for the HPE program and Medicaid. The criteria implemented during the pandemic have the potential to expand access to health insurance for patients across California. HPE was enacted across all states in 2014, regardless of Medicaid expansion. Although each state has separate Medicaid programs and HPE eligibility criteria, lessons from the success of the local and state HPE programs could be adopted by other states to expand access to insurance for eligible patients. Future work should include a prospective assessment of expanded criteria for health insurance during the COVID-19 pandemic from multiple centers across the United States. Extending our evaluation to centers in different states would show variations in HPE approval and Medicaid sustainment, identifying existing patient and health system facilitators and barriers. Gathering these data will enable further discussion on the importance of expanding eligibility criteria and inform the most effective policies to expand coverage. In addition, greater standardization of the approval process documentation, particularly when patients are not screened or denied coverage, would benefit future analysis and enable iterative improvement.
Conclusions
The policy changes implemented in response to the COVID-19 pandemic were associated with higher levels of HPE approval. Expanded eligibility criteria and adaptations to the HPE screening and approval process have the potential to increase access to care and improve clinical and financial outcomes. Future research across states is needed to identify whether these improvements were experienced nationally. Our results can help guide policymakers to consider insurance eligibility criteria to increase access for our patients.
Supplementary Materials
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jss.2023.03.030.
Author Contributions
Thomas J. Handley contributed in the study design, chart review, participant interviews, data analysis, and article preparation. Ana C. Boncompagni contributed in the study design, chart review, participant interviews, data analysis, and article preparation. Katherine Arnow contributed in the chart review, statistical analysis, and article revisions. Marzena Sasnal contributed in the study design, qualitative analysis, and article revisions. Heather S. Day contributed in the statistical analysis and article revisions. Amber W. Trickey contributed in the study design, statistical analysis, and article revisions. Arden M. Morris contributed in the study design, data interpretation, and article revisions. Lisa M. Knowlton contributed in the study design, chart review, data analysis, article preparation, and revisions.
Acknowledgments
We thank the work of Denise Greci Robinson, Michelle Woodfall, and our other trauma registrars for providing access to our institution's trauma registry data.
Disclosure
The authors declare no conflicts of interest.
Funding
L.M.K. is currently receiving a faculty research grant from the American Association for the Surgery of Trauma (Research and Education Faculty Scholarship) until 2021. T.J.H. is supported by a graduate fellowship award from Knight-Hennessy Scholars at Stanford University. The funding sources had no role in the study design, in the writing of the report, and in the decision to submit the paper for publication.
Supplementary Materials
References
- 1.Rajasingh C.M., Weiser T.G., Knowlton L.M., Tennakoon L., Spain D.A., Staudenmayer K.L. Trauma-induced insurance instability: variation in insurance coverage for patients who experience readmission after injury. J Trauma Acute Care Surg. 2018;84:876–884. doi: 10.1097/TA.0000000000001832. [DOI] [PubMed] [Google Scholar]
- 2.Haider A.H., Weygandt P.L., Bentley J.M., et al. Disparities in trauma care and outcomes in the United States: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2013;74:1195–1205. doi: 10.1097/TA.0b013e31828c331d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu C., Rahman A.S., Chao T.E. Catastrophic expenditures in California trauma patients after the affordable care act: reduced financial risk and racial disparities. Am J Surg. 2020;220:511–517. doi: 10.1016/j.amjsurg.2020.04.012. [DOI] [PubMed] [Google Scholar]
- 4.Finegold K., Conmy A., Chu R.C., Bosworth A., Sommers B.D. US Department of Health and Human Services; Washington, DC: 2021. Trends in the U.S. Uninsured population, 2010-2020. Office of the assistant secretary for planning and evaluation. Brief No. HP-2021-02):20. [Google Scholar]
- 5.Bivens J., Zipperer B. Health insurance and the COVID-19 shock: what we know so far about health insurance losses and what it means for policy. Economic Policy Institute. 2020. https://www.epi.org/publication/health-insurance-and-the-covid-19-shock/ Available at:
- 6.Brooks T. Hospital presumptive eligibility. The ACA expands the policy that allows key entities to temporarily enroll people in medicaid, creating a path to more stable coverage. Health Affairs. 2014. https://www.healthaffairs.org/do/10.1377/hpb20140109.508614/full/ Available at:
- 7.Center for Disease Control and Prevention Hospital presumptive eligibility. https://www.cdc.gov/phlp/docs/hospitalpe-brief.pdf Available at:
- 8.Public Health Orders - Emergency Operations Center - County of Santa Clara Santa clara county public health. https://covid19.sccgov.org/public-health-orders Available at:
- 9.Services D of HC Hospital presumptive eligibility program. https://www.dhcs.ca.gov/services/medi-cal/eligibility/Pages/HospitalPE.aspx Available at:
- 10.Creswell J. 1st ed. SAGE Publications; Thousand Oaks, CA: 2014. A concise introduction to mixed methods research. [Google Scholar]
- 11.Jaramillo J.D., Arnow K., Trickey A.W., et al. Acquisition of Medicaid at the time of injury: an opportunity for sustainable insurance coverage. J Trauma Acute Care Surg. 2021;91:249–259. doi: 10.1097/TA.0000000000003195. [DOI] [PubMed] [Google Scholar]
- 12.R: The R project for statistical computing. https://www.r-project.org/ Available at:
- 13.Edmonds W.A., Kennedy T.D. 2nd. SAGE Publications; Thousand Oaks, CA: 2022. An applied guide to research designs: quantitative, qualitative, and mixed methods. [Google Scholar]
- 14.Patton Q. 3rd ed. SAGE Publications; Thousand Oaks, CA: 2014. Qualitative research & evaluation methods. [Google Scholar]
- 15.Miles M.B., Huberman A.M., Saldana J. 3rd ed. SAGE Publications; Thousand Oaks, CA: 2014. Qualitative data analysis: a methods sourcebook. [Google Scholar]
- 16.Braun V., Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.