ABSTRACT
A field study was conducted to examine the vulnerability of military divers to non-freezing cold injury (NFCI) during Arctic ice-diving operations. Participants were instrumented with temperature sensors on the back of their hands and on the bottom of their big toe for each dive to measure cooling of their extremities. While NFCI was not diagnosed in any of the participants during this field study, the data indicate that the feet were particularly vulnerable during the dives given that they were mostly in a temperature zone that could cause pain and performance decrements. The data also show that for short term dives, the dry and wet suits with wet gloves in both configurations were thermally more comfortable for the hands than the dry suit with dry glove configuration; however, the latter would be more protective against potential NFCI during longer dives. Features such as hydrostatic pressure and repetitive diving that are unique to diving but not previously considered as risk factors for NFCI are examined herein and warrant deeper investigation given that symptoms of NFCI might be mistaken as decompression sickness.
KEYWORDS: Arctic, diving, cold, non-freezing cold injury, military
Introduction
The Government of Canada has a continued interest in maintaining an operational military presence in the Arctic, made increasingly complex by melting ice coverage and permafrost due to climate change. Canada’s constant presence in the north requires a capability to operate effectively and to respond proficiently to threats and emergencies in various extreme cold weather conditions in both land and sea environments [1]. As part of its on-going efforts to maintain readiness, the Canadian Armed Forces (CAF) train and conduct exercises year-round through a series of operations called Op NANOOK-NUNALIVUT (Op NA-NU). These operations are often “joint” and coalition, including the CAF Army, Royal Canadian Air Force (RCAF), and the Royal Canadian Navy (RCN) in addition to international military participation from nations such as the United States, France, Norway, Finland, and Sweden. The goal of OP NA-NU is to reinforce national defence and security, develop unique skill sets for Arctic operations, and train for a variety of emergency scenarios such as search and rescue missions.1
A primary health and operational threat to functioning in the Arctic is the occurrence of cold weather incidents involving freezing and non-freezing cold injuries (NFCI). Significant whole-body heat loss leading to possible hypothermia can impede both physical performance (strength and dexterity [2]; and cognitive performance [3]. Recent research conducted by DRDC (Defence Research and Development Canada) found that CAF members experienced a high occurrence of freezing cold injuries and human impairments during land operations in the Arctic [4,5]. However, little is known about the risk of NFCI for RCN personnel operating in the water even though ice diving is a routine component of RCN training. The purpose of the 2019 field study examined herein was to collect medical event data to investigate possible deficiencies in equipment and protocol that might exacerbate vulnerability to NFCI as well as undermine the performance of RCN divers during Arctic operations.
Military divers can be exposed to extreme cold temperatures as low as −2°C (e.g. Arctic sea water) and endure heat loss at rates about 25 times faster in water than if exposed to cold air at the same temperature.2 Considerable research has been conducted to help improve military diver performance in the cold [6–9]. Yet, while the testing of various wet and dry suits has often proven sufficient to provide adequate protection for preventing decreases in core temperature, the maintenance of tissue temperature in the extremities is particularly challenging [10]. Cold water diving enhances the possibility of reduced peripheral blood flow to the extremities that can cause a lack of dexterity, reduced skin temperatures, and potentially lead to NFCI [11,12].
DRDC Toronto conducted a field study to investigate the extent to which RCN divers were at risk for NFCI by directly measuring the cooling of the divers’ hands and feet when submersed in ice-cold water during OP NA-NU 2019. This paper summarises the data collected and analysed from the event, which took place in Tuktoyaktuk, Northwest Territories, Canada, in March 2019.
Materials and methods
The study and data collected were approved by the Defence Research and Development Canada Human Research Ethics Committee. Participants (all male) consisted of 24 clearance and combat divers from the RCN, and 8 international divers from France, Norway, Finland, and Sweden.
Participants dressed in either a dry suit3 with dry gloves (DD), a dry suit3 with wet gloves and dry feet (DW), or a wet suit3 with wet gloves (WW) configuration. The entire body was fully covered including face masks. Hand and foot temperatures were measured with iButtons4 taped on the back of both hands between the thumb and forefinger, and on the bottom of both big toes with KT tape®. All divers stood on grass type mats that were often wet/icy during the preparation time lasting approximately 30 min, which took place in a heated tent that ranged from 10 to 14°C.
Once readied, the DW and WW divers entered the water through a hole in the ice within the sheltered space. Three international divers in the DD configuration dove through a hole outside a few metres away from the tent where the air temperature ranged from −9 to −18°C. Diving through an outside hole was conducted to maintain consistency with the diving practices in the international divers’ countries. Most of the dives took place within 6 m of the surface while a few took place about 24 m from the surface. Temperature monitoring began approximately 15–30 min prior to a dive and lasted approximately 5–10 min after the diver exited from the water. The temperature sample rate was every 15 s, but differed between participants during the pre- and post-dive periods to keep pace with the training exercise without interruption. Water temperature was recorded and varied between 0°C5 and 2°C.
A total of 83 dives among the 32 divers were recorded over the course of 4 days with dive times ranging from about 5 to 37 minutes. The divers were also asked to rate their overall thermal comfort based on the McGinnis Thermal Scale (MTS [13]; ranging from 1 (So cold I am helpless) to 13 (So hot I am sick and nauseated) just prior to diving and shortly after diving. Separate ratings for the thermal comfort of the hands and feet were obtained from only four divers. Divers were not queried about pain nor were any performance measures taken.
An initial review of the data revealed a number of dives where measurements were either missing or suspect,6 which reduced the number of dives to 69 among 28 participants suitable for further analysis. Where divers participated in additional dives under different configurations (e.g. DD, DW, and/or WW), the configuration chosen for analysis was based on the dive of longest duration (five occurrences). This constraint further reduced the number of suitable dives for analysis to 64 involving totals of 3 participants under the DD configuration, 17 under the DW configuration, and 8 under the WW configuration. All but three of the 28 participants dove more than once. Hence, hand and foot temperatures at the start and end of a dive, and dive times from repeated dives were averaged to represent a single data set for each diver for a total of 28 data sets. Finally, hand and foot temperatures are presented as averages from their corresponding right and left sides. A single-factor 3-way (DD x DW x WW configurations) ANOVA was applied to compare pre- and post-dive measurements with post-hoc testing for significance (p < 0.05), and a single-factor 2-way (pre x post temperatures) ANOVA was applied to compare measurements within a configuration.
Results
Figure 1 shows the scatter of all averaged temperatures of the hands and feet at the end of the dives plotted against dive times, which varied from 11 to 26 min. Striking is the number of cases where foot temperatures ended below 15°C (79%) in contrast to that of the hands (11%). Further, hands that ended with average temperatures below 15°C were confined to two cases under the DD configuration and a single case under the DW configuration. Average foot temperatures ended below 15°C in all three divers under the DD configuration, in 12 out of 17 divers under the DW configuration, and in 7 out of 8 divers under the WW configuration. Surprisingly, no correspondence between the time spent in the water and the end-point extremity temperature is evident for either the hands or feet.
Figure 1.
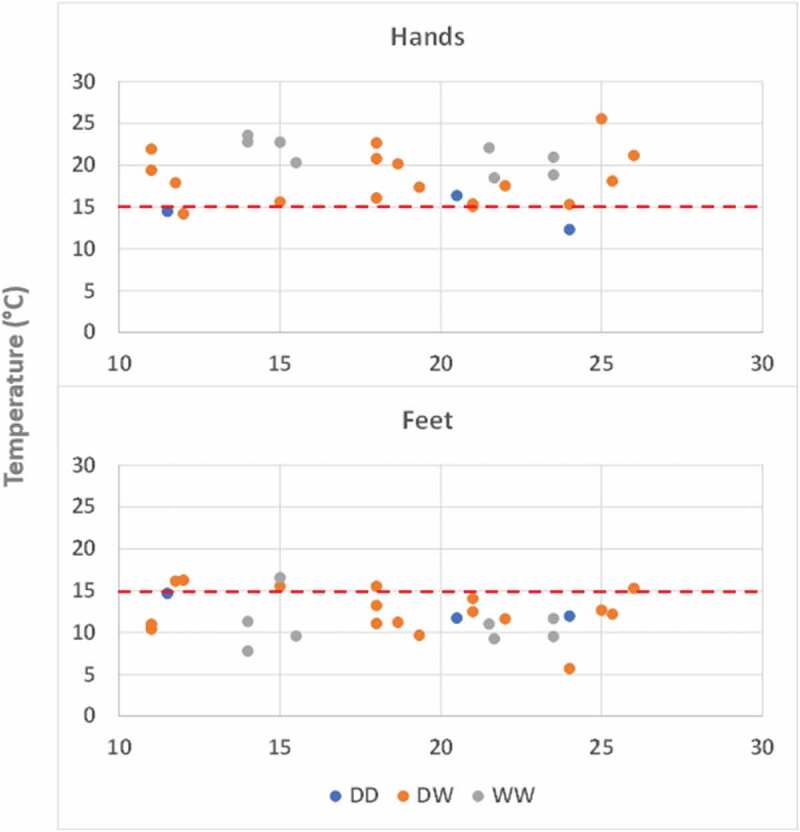
Temperatures (°C) of the hands and feet plotted against dive time (min) for the DD (dry-dry), DW (dry-wet), and WW (wet-wet) configurations.
Figure 2 shows a comparison of extremity temperatures between the start and end of the dives. The mean dive times among the DD, DW, and WW configurations were not different (18.7, 18.7, and 18.6 min, respectively). Mean temperatures ± SE of the participants’ hands differed at the start (19.7 ± 2.4, 24.2 ± 0.8, and 28.0 ± 0.7°C) and at the end (14.4 ± 1.2, 18.5 ± 0.8, and 21.2 ± 0.7°C) of the dives among all three configurations (DD, DW, and WW), respectively. The hands also ended significantly colder at the end of the dives for the DW and WW configurations. Mean temperatures ± SE of the participants’ feet were not different at the start (16.6 ± 1.8, 16.7 ± 1.0, and 13.3 ± 1.0°C) nor at the end (12.8 ± 1.0, 12.6 ± 0.7, and 10.8 ± 0.9°C) of the dives for all three configurations (DD, DW, and WW), respectively. However, the feet ended significantly colder at the end of the dives for the DW configuration.
Figure 2.
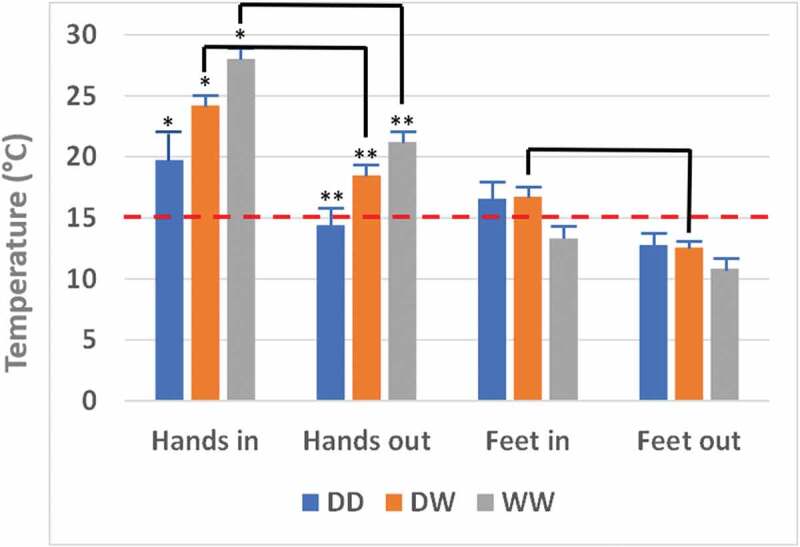
Mean ± SE temperatures (°C) of the hands and feet at the start and end of dives for the DD (dry-dry), DW (dry-wet), and WW (wet-wet) conditions. * indicates significant differences in the starting hand temperatures between the DD, DW, and WW conditions and ** indicates significant differences in the end-point hand temperatures between the respective conditions. The elbowed lines indicate significant temperature differences between the start and end times (e.g. Hands in vs Hands out for both DW and WW conditions).
There were no differences in the participants’ pre- and post-diving thermal comfort for the DD (mean ± SE change in MTS from 6.6 ± 0.3 to 6.2 ± 0.6) and WW (7.5 ± 0.3 to 7.5 ± 0.3) configurations, despite a significant decrease in the temperature of the hands in the WW configuration (Figure 2). The overall thermal comfort of the DW divers dropped marginally, but significantly by the end of the dives (mean ± SE change in MTS from 7.6 ± 0.6 to 6.1 ± 0.6), which is consistent with the significant cooling of both the hands and feet in the DW configuration (Figure 2). MTS values of 6 and 7 refer to “Cool but fairly comfortable” and “Comfortable”, respectively. The four divers that were additionally asked about their hands and feet rated their values from 3 “Very cold” to 5 “Uncomfortably cool”.
Figure 3 shows a comparison of the mean rates of temperature change (°C/min) of the extremities during the dives. Mean ± SE rates of change were not different between the DD, DW, and WW configurations for either the hands (0.25 ± 0.12, 0.35 ± 0.04, and 0.37 ± 0.05°C/min) or feet (0.18 ± 0.8, 0.21 ± 0.3, and 0.15 ± 0.3°C/min), respectively. However, the mean rates of temperature change were significantly higher for the hands compared to the feet for the DW and WW configurations.
Figure 3.
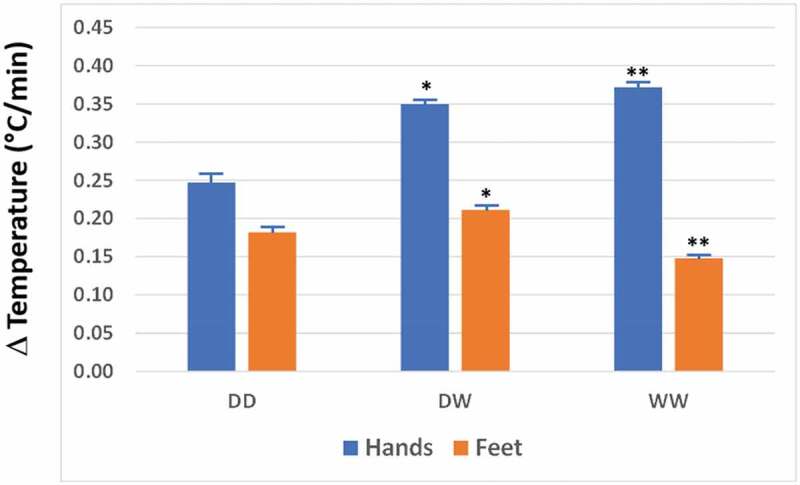
Mean ± SE rates of change (Δ) of temperatures (°C/min) of the hands and feet for the DD (dry-dry), DW (dry-wet), and WW (wet-wet) conditions. * and ** indicate significant differences between the hands and feet for the DW and WW conditions, respectively.
At this point, we return to the raw data of the 64 dives and investigate the lowest extremity temperatures recorded. Figure 4 shows the scatter of the lowest hand and foot temperatures of all 28 subjects at the end of their dives plotted against dive times, which varied from 16 to 26 min. As with the averaged data presented above, no discernible pattern between the time spent in the water and the end-point extremity temperature is evident. Minimum hand temperatures were 8.8, 8.8, and 13.3°C, under the DD, DW, and WW conditions, respectively, and 8.5, 4.5, and 6.8°C for the feet. Interestingly, all three DD subjects ended a dive with at least one extremity below 15°C. All DW and WW subjects ended dives with at least one foot below 15°C. And about 2/3 of DW and 3/8 of WW subjects ended dives with at least one hand below 15°C. Yet, despite the occurrences of sub-15°C skin temperatures of the extremities, no incidence of NFCI was reported.
Figure 4.
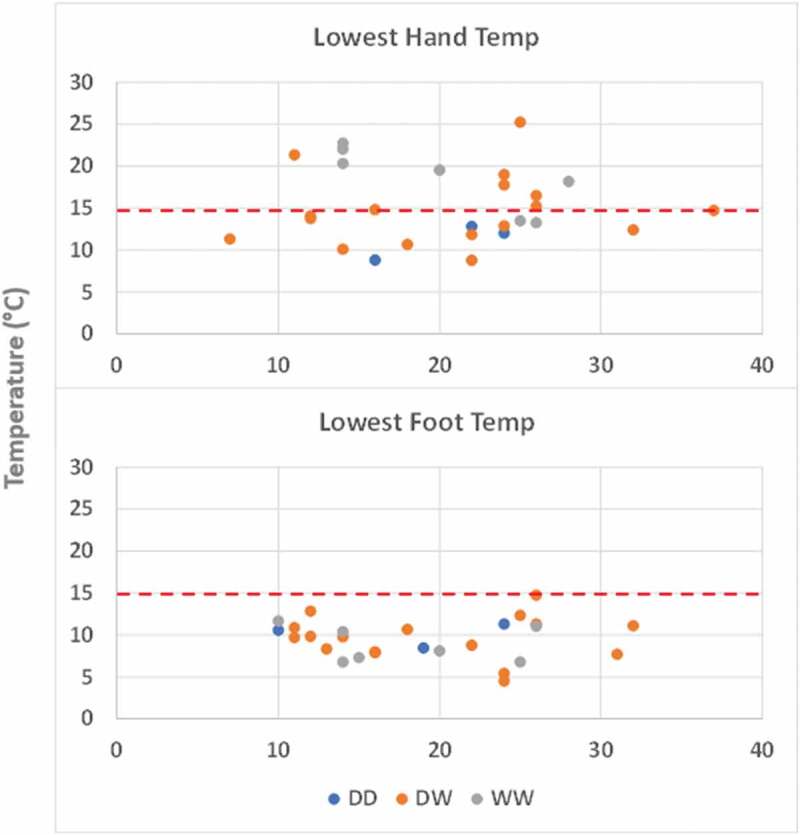
Lowest recorded temperatures (°C) of the hands and feet plotted against dive time (min) for all 28 subjects across 64 dives under the DD (dry-dry), DW (dry-wet), and WW (wet-wet) conditions.
Discussion
A key inquiry of this study was to assess whether military divers were at risk of NFCI during Arctic training. The divers were adequately protected by their clothing and procedures against freezing cold injury at all times. Although no incidence of NFCI was reported post dives, much is still unknown about the potential risk of NFCI during diving [14].
What is known is that NFCI is generally caused by a prolonged decrease in blood flow leading to microvascular damage and possible peripheral nerve damage most frequently affecting the hands and feet when exposed to non-freezing cold temperatures [15,16,17]. Specifically, skin temperatures below 15°C initiate the prerequisite maximum vasoconstriction in the extremities that impedes blood flow and induces numbness [18,19]. Also, as noted by Imray et al. [16], the duration of the cold exposure and the extent of skin cooling determines the likelihood and severity of NFCI in a somewhat reciprocal relationship (i.e. the colder the skin temperature, the shorter the exposure time required for the onset of NFCI).
Further, wetness increases the risk markedly. According to Zafren [19], wetness is a requirement for the onset of NFCI, although others have reported that dry cold cannot be dismissed as a possible risk, however low [15]. The incidence of NFCI typically occurs after several hours of exposure to a wet cold condition (e.g. 10°C for 10 h; Shaw and Levy, [20] in concurrence with the detailed report on the incidence and pathology of trench foot and immersion hand by Ungley et al. [21]. Marsh [22] and Tek [23] also reported trench foot incident rates of 11 to 14% in military personnel following 2–3 days exposures to mean temperatures of 7 and 0°C, respectively, under wet conditions. The three primary factors that determine the risk of NFCI can be summarised as cold skin (0 to 15°C), duration of exposure, and wetness. Other factors pertinent to diving such as hydrostatic pressure, restricted movement, and frequency of diving that might also add to the risk of NFCI are explored further below.
Despite the hands having cooled faster than the feet (Figure 3), they did not end up colder (Figure 2), which can be explained by the much higher starting hand temperatures that created a higher gradient for heat loss than for the feet.7 The participants’ feet started at a colder temperature than their hands (mean participant-weighted values of 15.7 and 24.8°C, respectively, for all three clothing configurations) as a consequence of standing on icy-wet mats for about 30 min prior to diving. According to an extremity cooling study by van der Struijs et al. [24], bare toes cooled more than the fingers for both cold air exposure (−18°C) and cold water immersion (5°C). Mean toe and finger temperatures during the last 20 min of the 30 min of the reported cold air trial were 20.9°C and 25.6°C, respectively. Mean respective temperatures in the cold water trial of the same study were considerably cooler at 7.1°C and 9.3°C. Therefore, it also appears natural for toes to cool more than the fingers when exposed unprotected to cold. Hence, the finding of colder feet than hands (mean participant-weighted difference of 7.7°C by the end of the dives for all three clothing configurations) in the current field study is not surprising.
The results also indicate that the hands ended colder under a dry (DD) vs wet (DW and WW) configuration. However, the hands under the DD configuration were also colder prior to diving (Figure 2), which might have been due to the colder outdoor air exposure (recall that the three DD divers were outside the tent) before entering the water. Yet, this difference in starting hand temperatures between the divers outside vs inside the tent was not replicated for the feet possibly because standing on an icy surface presented a similar cold challenge to the feet irrespective of the air temperature.
In contrast to the hands, the divers’ feet mostly ended below 15°C placing them in a zone of pain and impaired performance irrespective of the clothing configuration. Indeed, the DW divers perceived a significant drop in overall thermal comfort during the dive and a few rated their hands and feet as cold or uncomfortably cool. Yet, were the divers at risk of NFCI? The reported times to NFCI due to wet cold conditions (typically several hours [18,25]) are considerably greater than the submersion times analysed herein. However, the divers were under hydrostatic stress (i.e. increased ambient pressure), which would have reduced the insulation of the WW neoprene suits, thus exacerbating the cold-induced vasoconstriction that potentially could have hastened the onset of NFCI had the dives continued longer.
In other words, the onset of NFCI during diving might occur sooner than a land-based exposure under similar environmental wet cold conditions. And such an occurrence might be mistaken for decompression sickness. For example, Leitch and Pearson [26] described the likelihood that cold exposure vs decompression sickness was the cause of immersion hand injury following dives in 1.7°C water at a depth of 7 m for 13 min in one case and in 16°C water at a depth of 75 m for 25 min followed by 15 min of in-water decompression in the second case.8 That NFCI may have occurred in just 16°C water implicates hydrostatic pressure as a potentially important risk factor of NFCI. Another interesting case study reported NFCI of a diver’s hand (numbness and paraesthesia) following a dive in 6°C water to a depth of 90 m with prescribed decompression for a total in-water duration of 90 min [11]. Hence, while it appears that NFCI is unlikely for short wet cold exposures on land, it would be prudent to further investigate the risk of NFCI during wet cold dives characterised by an elevated hydrostatic pressure.
Another possible factor that might hasten the onset of NFCI is the restriction of movement under a wet cold condition as noted by Smith et al. [27] and Zafren [19]. Smith et al. pointed out that voluntary movements to promote blood circulation in the trenches and dug-outs of WWI were severely limited and likely contributed to the incidence of trench foot. Tight protective clothing (especially wet suits) coupled with hydrostatic pressure creating a greater squeeze will amplify the restriction of movement and possibly increase the risk of NFCI in divers.
Given the varying circumstances of military operations, it is conceivable that a diver could be submersed for longer than the actual planned time. Along similar lines, the frequency of diving (i.e. repetitive dives) might generate a cumulative strain that also increases the risk of NFCI, a consideration that has not been fully investigated. In the first case study of diving NFCI examined by Leitch and Pearson (1978), the individual had swum in 1.7°C water with some water leakage into his wet suit causing pre-cooling prior to the diving excursion, which added to the overall cold stress. It is important to recognise that the diagnosis of diving injury is complicated by an overlap of symptoms between decompression sickness and NFCI [11]. specifically advise that “For any diver presenting with a painful extremity following long dive times in cold water, NFCI should be a considered differential diagnosis”.
Conclusion & recommendations
Despite the limited resources and limitations inherent in field work, the data reported here yielded useful information and opened new lines of inquiry regarding extremity cooling during ice cold water diving. The data indicate that the feet (under both the dry and wet suit configurations) reached the threshold temperature for the possible onset of pain and performance decrements much sooner than the hands. That the extremities might be at risk of NFCI is noteworthy given that the divers’ perception of overall thermal comfort fell between “Cool but fairly comfortable” and “Comfortable” suggesting that the dive suits adequately protected the core of the body, but not the extremities according to the temperatures measured.
The possibility of colder hand temperatures under a dry vs wet condition introduces a critical trade-off. If the duration of the dive is sufficiently short, as in this study, the data suggest that a wet suit might be thermally more comfortable and thus enable higher operational performance than a dry suit. But if the dive duration is longer than reported herein, then the risk of NFCI in a neoprene wet suit increases, especially with increasing dive depth as compression of the suit lessens its insulation, in which case an incompressible dry suit with dry gloves might be more advantageous. Clearly, further investigation is required to ascertain the risks associated with NFCI and the benefits associated with the performance of wet vs dry suit diving with respect to extremity cooling and operational tolerances.
Wet vs dry suit options must be carefully considered when hydrostatic pressure, limited mobility, and the frequency of diving are added as potential vulnerability factors. Ultimately, with sufficient research and data, a predictive model of NFCI onset that takes into account the various risk factors outlined above would serve as a valuable decision aid whenever cold water diving is planned. And finally, to paraphrase Leitch and Pearson (1978), it would be prudent to provide sufficient thermal protection to the extremities to circumvent NFCI (i.e. ensuring dry skin preferably above 15°C) to avoid the high possibility of NFCI symptoms in common with decompression sickness, which would complicate choosing the correct therapeutic course of action.
Funding Statement
This work was funded by Defence Research and Development Canada Arctic Medicine project: People__21.
Footnotes
NATO up North: Operation Nanook-Nunalivut – NAOC (natoassociation.ca) Accessed July 20, 2022; Operation NANOOK – Canada.ca Accessed July 20, 2022.
Although there is no firm definition of what constitutes cold water, water is considered thermoneutral at approximately 35°C when resting naked, 25°C when exercising, and cold when below 15°C [24].
The Canadian divers wore either a trilaminate incompressible dry suit or a 7 mm neoprene wet suit.
iButtons consisted of a mixture of regular for dry use and silicone-covered for wet use.
Arctic sea water is typically −1.8°C during the winter (https://seatemperature.info/march/nunavut-water-temperature.html).
Extremity temperatures at the end of a dive that were widely apart (e.g. right vs. left hand) or higher than at the start, or dive times that were ambiguous (e.g. overlapping times between dives).
Assuming that the insulative values of the gloves and footwear are not too dissimilar, the loss of heat would then depend primarily on the temperature difference between the extremities and the water, in which case a higher temperature gradient would yield a higher rate of heat loss.
While decompression sickness cannot be ruled out in the second case, the authors considered this unlikely given that the response to rewarming closely followed the stages of immersion hand syndrome.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Lajeunesse A, Lakenbauer PW. editors. Canadian armed forces arctic operations, 1945-2015: historical and contemporary lessons learnedVol. xli. Frederiction: Gregg Centre for the Study of War and Society. 2017. p. 491. [Google Scholar]
- [2].Marrao C, Tikuisis P, Keefe AA, et al. Physical and cognitive performance during long-term cold weather operations. Aviat Space Environ Med. 2005;76(8):744–8. [PubMed] [Google Scholar]
- [3].Muller MD, Gunstad J, Alosco ML, et al. Acute cold exposure and cognitive function: evidence for sustained impairment. Ergonomics. 2012;55(7):792–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sullivan-Kwantes W, Dhillon P, Goodman L, et al. Medical encounters during a joint canadian/u.s. exercise in the high arctic (exercise arctic ram). Mil Med. 2017;182(9):e1764–8. [DOI] [PubMed] [Google Scholar]
- [5].Sullivan-Kwantes W, Moes K, Goodman L. Operating in the arctic: a qualitative report on understanding health risks and medical readiness challenges during canadian armed forces. Artic Operations (U). 2022. Protected A. DRDC-RDDC-2022-R022. [Google Scholar]
- [6].Castellani JW, O’brien C, Stulz DA, et al. Physiological responses to cold exposure in men: a disabled submarine study. Undersea Hyperbaric Med. 2002;29(3):189–203. [PubMed] [Google Scholar]
- [7].Chapin AC, Arrington LJ, Bernards JR, et al. Thermoregulatory and metabolic demands of naval special warfare divers during a 6-h cold-water training dive. Front Physiol. 2021. Sep 29;12:674323. DOI: 10.3389/fphys.2021.674323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kelly KR, Arrington LJ, Bernards JR, et al. Prolonged extreme cold water diving and the acute stress response during military dive training. Front Physiol. 2022. Jul 8;13:842612. DOI: 10.3389/fphys.2022.842612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lundell RV, Räisänen-Sokolowski AK, Wuorimaa TK, et al. Diving in the arctic: cold water immersion’s effects on heart rate variability in navy divers. Front Physiol. 2019. Jan 31;10:1600. DOI: 10.3389/fphys.2019.01600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Valaik DJ, Hyde DE, Bowman K, et al. (1998). Thermal protection and diver performance in special operations forces combat swimmers (over-the-beach phase). Naval Medical Research Institute; Technical Report 98-11, Aug 1998. [Google Scholar]
- [11].Laden GD, Purdy G, O’rielly G. Cold injury to a diver’s hand after a 90-min dive in 6 degrees C water. Aviat Space Environ Med. 2007;78(5):523–525. [PubMed] [Google Scholar]
- [12].Jørum E, Opstad PK. A 4-year follow-up of non-freezing cold injury with cold allodynia and neuropathy in 26 naval soldiers. Scand J Pain. 2019. Jul 26;19(3):441–451. [DOI] [PubMed] [Google Scholar]
- [13].Norman R, Hollies S, Custer AG, et al. A human perception analysis approach to clothing comfort. Text Res J. 1979. Oct;49(10):557–564. [Google Scholar]
- [14].Haman F, Souza SCS, Castellani JW, et al. Human vulnerability and variability in the cold: establishing individual risks for cold weather injuries. Temperature. 2022;9(2):158–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Montgomery H. Experimental immersion foot, review of the physiopathology. Physiol Rev. 1954;34(1):127–137. DOI: 10.1152/physrev.1954.34.1.127. [DOI] [PubMed] [Google Scholar]
- [16].Imray CHE, Richards P, Greeves J, et al. Nonfreezing Cold-Induced Injuries. J R Army Med Corps. 2011;157(1):79–84. [DOI] [PubMed] [Google Scholar]
- [17].Melamed E, Glassberg E. Non-freezing cold injury in soldiers. Harefuah. 2002;141(12):1050–1054. [PubMed] [Google Scholar]
- [18].Francis TJ. Non freezing cold injury: a historical review. J R Nav Med Serv. 1984;70(3):134–139. [PubMed] [Google Scholar]
- [19].Zafren K. Nonfreezing cold injury (trench foot). Int J Environ Res Public Health. 2021;18(19):10482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Shaw J. Frostbite. Rosen P, Baker F, Barkin R, Braen, G, Dailey Rand Levy R, editors. Emergency Medicine. Concepts and Clinical practice. St Louis: Mosby. 1988:610. [Google Scholar]
- [21].Ungley CC, Channell CD, Richards RI. The immersion foot syndrome. Br J Surg. 1945;33(129):17–31. [Google Scholar]
- [22].Marsh AR. A short but distant war – the Falklands campaign. J. Roy. Soc. Med . 1983;76(Nov):972–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Tek D and Mackey S. Non-freezing cold injury in a marine infantry battalion. J. Wilderness Med . 1993;4:353–357. [Google Scholar]
- [24].van der Struijs Nr, van Es EM, Raymann RJ, et al. Finger and toe temperatures on exposure to cold water and cold air. Aviat Space Environ Med. 2008;79(10):941–946. DOI: 10.3357/asem.2258.2008. [DOI] [PubMed] [Google Scholar]
- [25].Tipton MJ, Collier N, Massey HC, et al. Cold water immersion: kill or cure? Exp Physiol. 2017;102(11):1335–1355. [DOI] [PubMed] [Google Scholar]
- [26].Leitch DR, Pearson RR. Decompression sickness or cold injury? Undersea Biomed Res . 1978. Dec;5(4):363–7. PMID: 734803. [PubMed] [Google Scholar]
- [27].Smith JL, Ritchie J, Dawson J. Clinical and experimental observations on the pathology of trench frostbite. J Pathology. 1915;20(1):159–190. [Google Scholar]


