Abstract
Since the emergence of COVID-19, several different medicines including antimicrobials have been administered to patients to treat COVID-19. This is despite limited evidence of the effectiveness of many of these, fueled by misinformation. These utilization patterns have resulted in concerns for patients’ safety and a rise in antimicrobial resistance (AMR). Healthcare workers (HCWs) were required to serve in high-risk areas throughout the pandemic. Consequently, they may be inclined towards self-medication. However, they have a responsibility to ensure any medicines recommended or prescribed for the management of patients with COVID-19 are evidence-based. However, this is not always the case. A descriptive cross-sectional study was conducted among HCWs in six districts of the Punjab to assess their knowledge, attitude and practices of self-medication during the ongoing pandemic. This included HCWs working a range of public sector hospitals in the Punjab Province. A total of 1173 HCWs were included in the final analysis. The majority of HCWs possessed good knowledge regarding self-medication and good attitudes. However, 60% were practicing self-medication amid the COVID-19 pandemic. The most frequent medicines consumed by the HCWs under self-medication were antipyretics (100%), antibiotics (80.4%) and vitamins (59.9%). Azithromycin was the most commonly purchase antibiotic (35.1%). In conclusion, HCWs possess good knowledge of, and attitude regarding, medicines they purchased. However, there are concerns that high rates of purchasing antibiotics, especially “Watch” antibiotics, for self-medication may enhance AMR. This needs addressing.
Keywords: hospitals, healthcare workers, COVID-19, self-medication, antibiotics, Pakistan, antimicrobial resistance, AWaRe classification
1. Introduction
Since the emergence of the coronavirus disease of 2019 (COVID-19) in China, Pakistan has been at considerable risk of the virus due to border sharing, trade and travel ties with China through land, sea and air [1,2,3]. After reporting the first positive case of COVID-19 in Pakistan on 26 February 2020, comprehensive measures were introduced by the government to reduce its spread, similar to other countries [1,4,5,6,7,8]. These measures included a country wide lockdown, which resulted in the closure of markets, educational/religious institutes and marriage/banquet halls, as well as the cancellation of religious congregations and ceremonies and public and private sport festivals [4,8,9]. However, despite these initiatives, cases of COVID-19 continued to rise in Pakistan, with a substantial number of positive cases reported in different waves of the pandemic. This rise was exacerbated by concerns with poverty and unemployment in Pakistan with continued lockdown measures as well as social distancing and other measures not being strictly followed [4,8,10].
Alongside lockdown and other measures, there were designated COVID-19 wards among secondary and tertiary care hospitals throughout Pakistan providing care to patients hospitalized with COVID-19 [4]. Up to 25 January 2023, more than 1.5 million people had the virus in Pakistan, with over 30,000 deaths out of a population of over 200 million [11].
Healthcare workers (HCWs) including physicians, nurses and pharmacists are regarded as first-line employees in the fight against COVID-19. Consequently, they are more likely to contract severe COVID-19 than the overall population [12,13,14,15,16]. HCWs typically treat COVID-19 patients admitted to hospitals in emergency units, general and isolation wards, intensive care units (ICUs) and critical care units (CCUs) [17,18,19,20]. By mid-May 2021, more than 115,000 HCWs had lost their lives globally after being infected with COVID-19 [21]. Local media reports in Pakistan revealed that 14,627 HCWs had been infected throughout Pakistan by 22 March 2021, with 143 deaths [22]. Not surprisingly, the increased chance of infection, coupled with the pressures placed on HCWs by the pandemic including working in high-risk environments and longer hours, adversely impacted on the mental and physical health of HCWs across countries [23,24,25,26]. A similar situation was seen in Pakistan [27,28].
With the progression of pandemic, many antimicrobials including hydroxychloroquine, ivermectin, remdesivir and azithromycin along with vitamins and other supplements to boost the immune system had been proposed to prevent or treat COVID-19 [29,30]. However, the vast majority of re-purposed medicines had little or no clinical benefit for patients, whilst increasing morbidity, mortality and costs [31,32,33,34,35,36,37,38,39,40]. The exception was dexamethasone among ventilated patients in hospital with COVID-19 [41]. The prescribing of antimicrobials including hydroxychloroquine as well as ivermectin was fueled by social media, often without input from healthcare professionals, negatively impacting on the health of patients [42,43,44,45]. This called for a greater cognizance of evidence-based medicine, as well as greater scrutiny regarding clinical trial design, when different approaches have been suggested for the treatment of patients with COVID-19, endorsed by the approaches taken in the WHO Solidarity Trial and the UK Recovery Trials [31,34,35,46]. The same situation was seen with respect to the appreciable prescribing and dispensing of antimicrobials, including antibiotics, across sectors to treat patients with COVID-19 despite limited evidence of bacterial or fungal secondary or co-infections [4,29,47,48,49,50,51,52,53,54]. This included self-medication with antimicrobials across countries, especially among low- and middle-income countries (LMICs) [39,40,54,55]. This includes Pakistan, with extensive self-purchasing of antimicrobials and currently limited measures in place to reduce this [56,57,58]. Such practices are a concern as this will increase antimicrobial resistance (AMR) rates unless addressed, increasing morbidity, mortality and costs [59,60,61,62,63].
The threat of COVID-19 itself may well lead to increased self-medication among HCWs in view of the pressures on them [64,65]. This is a challenge if unnecessary consumption of medicines results in increased costs and morbidities due to adverse drug reactions (ADRs) and increased drug–drug interactions alongside the masking of certain symptoms and delays in seeking professional help [29,66,67]. Systematic reviews and other studies have suggested that vitamins, including Vitamins C and D, can play a role in the prevention and management of patients with COVID-19; however, there can be concerns with the level of evidence [68,69,70,71,72,73].
Within Pakistan, rising AMR rates are a concern, including both the multi-drug resistant (MDR) and extensively drug resistant (XDR) bacteria, acknowledged in the recent National Action Plan to reduce AMR [74,75,76,77]. Self-medication with antibiotics among the general population, as well as among HCWs, is one of the contributing factors to rising AMR rates including within Pakistan [56,58,78,79,80,81,82,83,84]. Published studies have highlighted that self-medication with antibiotics is common among the general population in Pakistan for a number of reasons. These include a lack of time to visit doctors, the poor socioeconomic status of patients, the convenience of community pharmacies/drugs stores, previous successful experiences with antibiotics and antibiotics freely available at pharmacies/drugs store without a prescription [56,58,85,86,87]. A key concern is the extent of dispensing of “Watch” and “Reserve” antibiotics with their increasing potential for resistance [56,88,89]. This is in addition to the extensive prescribing of antibiotics among hospitalized patients in Pakistan before and during the pandemic enhancing AMR rates [4,50,90,91,92,93].
To date, numerous studies have been conducted among the general population [94,95,96], university students [97], and medical students [98], to determine their self-medication knowledge, behaviors and rationale. To the best of our knowledge, however, no study evaluating HCW self-medication habits during the COVID-19 pandemic has been published. Since HCWs including community pharmacists play a crucial role in the prevention and management of COVID-19, including enhancing vaccination uptake [65,99,100,101,102], it is imperative to assess their knowledge and attitudes towards self-medication. This includes the purchasing of antibiotics without a prescription. In this context, we conducted a multi-center, cross-sectional study with the primary objective of evaluating the awareness and practices of self-medication, including antibiotics, among HCWs in the Punjab Province in Pakistan amid the current COVID-19 pandemic.
2. Results
The investigators reached out to 1450 HCWs in an attempt to recruit them for the study. Overall, 1173 HCWs subsequently agreed to participate in the study, which gave a response rate of 80.9%. As far as the category of HCWs are concerned, the principal categories were physicians (31.9%), nurses (28.0%), health technicians (17.3%) and pharmacists (11.8%). The characteristics of the study sample are documented in Table 1. There was a preponderance of HCWs <40 years old (72.4%) and females (51.7%). Overall, 9.5% of participants had obtained a post-graduation or specialization in their field, with the highest number of the study HCWs providing services in secondary care institutions (48.6%).
Table 1.
Demographic details of the sample.
| Variables | N (%) |
|---|---|
| Age | |
| <30 years | 486 (41.4) |
| 31–40 years | 364 (31.0) |
| 41–50 years | 183 (15.6) |
| 51–60 years | 140 (11.9) |
| Gender | |
| Male | 567 (48.3) |
| Female | 606 (51.7) |
| Residence | |
| Urban | 816 (69.6) |
| Rural | 357 (30.4) |
| Marital status | |
| Single/Divorced/Widow | 697 (59.4) |
| Married | 476 (40.6) |
| Occupation | |
| Medical doctor | 374 (31.9) |
| Pharmacist | 139 (11.8) |
| Nurse | 329 (28.0) |
| Lab technician | 84 (7.2) |
| Physiotherapist | 18 (1.5) |
| Health technician | 203 (17.3) |
| Others | 26 (2.2) |
| Education | |
| Diploma | 549 (46.8) |
| Bachelor’s degree | 512 (43.6) |
| Post-graduation/specialization | 112 (9.5) |
| Hospital | |
| Tertiary | 150 (12.8) |
| Secondary | 570 (48.6) |
| Primary | 453 (38.6) |
| Experience | |
| 1–3 years | 355 (30.3) |
| 4–7 years | 431 (36.7) |
| 8–12 years | 242 (20.6) |
| >12 years | 145 (12.4) |
NB: N = 1173.
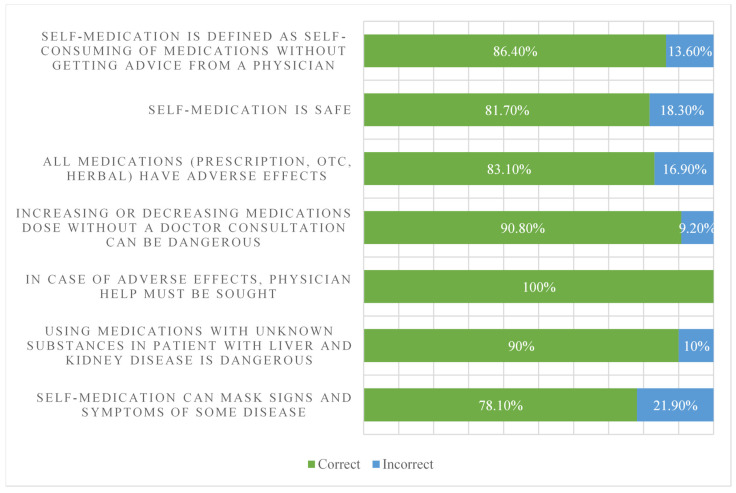
Figure 1 depicts the participants’ responses to all the knowledge items regarding self-medication. Overall, 86.4% were aware of what self-medication was and 81.7% gave correct responses to the question assessing the safety of self-medication. Overall, 83.1% agreed that all medicines (herbal, over-the-counter agents, prescription medicines) have adverse effects, and all the study participants knew that a physician’s help must be sought in case of any adverse effects from self-medication rather than managing these effects on their own. Taken together, the study participants appeared to have a good understanding of self-medication and the associated risks (correct rate 78.1% to 100% for all items; Figure 1).
Figure 1.
Participants’ knowledge related to self-medication. NB: N = 1173.
There was a significant difference in the knowledge score among both occupation and education categories (Table 2). The findings of a post hoc analysis of knowledge scores between the different HCW occupational and education categories are shown in Table 3. There was no significant difference in the knowledge score between medical doctors and pharmacists; however, both had better knowledge scores than nurses and physiotherapists. Participants with a bachelor’s degree or specialization had significantly better knowledge scores than HCWs with only a diploma.
Table 2.
Comparison of self-medication-related knowledge and attitude scores among selected demographics.
| Variables | Subgroups | Mean Rank | Self-Medication Practice N (%) |
||
|---|---|---|---|---|---|
| Knowledge Score | Attitude Score | Yes | No | ||
| Age | <30 years | 605.69 | 593.70 | 324 (41.9%) | 162 (40.6) |
| 31–40 years | 583.30 | 579.92 | 241 (31.1) | 123 (30.8) | |
| 41–50 years | 547.69 | 592.00 | 115 (14.9) | 68 (17.0) | |
| 51–60 years | 583.13 | 575.63 | 94 (12.1) | 46 (11.5) | |
| p-value | 0.199 | 0.908 | 0.802 | ||
| Gender | Male | 591.37 | 592.43 | 372 (48.1) | 195 (48.9) |
| Female | 582.92 | 581.92 | 402 (51.9) | 204 (51.1) | |
| p-value | 0.645 | 0.594 | 0.805 * | ||
| Residence | Urban | 582.10 | 586.29 | 552 (71.3) | 264 (66.2) |
| Rural | 598.20 | 588.62 | 222 (28.7) | 135 (33.8) | |
| p-value | 0.419 | 0.914 | 0.071 * | ||
| Occupation | Medical doctor | 776.84 | 570.93 | 239 (30.9) | 135 (33.8) |
| Pharmacist | 731.27 | 601.06 | 80 (10.3) | 59 (14.8) | |
| Nurse | 572.62 | 599.87 | 220 (28.4) | 109 (27.3) | |
| Lab technician | 461.83 | 534.34 | 65 (8.4) | 19 (4.8) | |
| Physiotherapist | 508.11 | 622.50 | 15 (1.9) | 3 (0.8) | |
| Health technician | 264.81 | 618.18 | 137 (17.7) | 66 (16.5) | |
| Others | 241.42 | 482.27 | 18 (2.3) | 8 (2.0) | |
| p-value | <0.001 | 0.236 | 0.046 | ||
| Education | Diploma | 456.53 | 594.79 | 376 (48.6) | 173 (43.4) |
| Bachelor’s degree | 694.19 | 583.51 | 327 (42.2) | 185 (46.4) | |
| Post-graduation/specialization | 736.53 | 564.75 | 71 (9.2) | 41 (10.3) | |
| p-value | <0.001 | 0.660 | 0.236 | ||
| Hospital | Tertiary | 575.62 | 609.43 | 98 (12.7) | 52 (13.0) |
| Secondary | 606.91 | 588.08 | 377 (48.7) | 193 (48.4) | |
| Primary | 565.71 | 578.21 | 299 (38.6) | 4154 (38.6) | |
| p-value | 0.102 | 0.615 | 0.983 | ||
| Experience | 1–3 years | 601.99 | 582.00 | 241 (31.1) | 114 (28.6) |
| 4–7 years | 600.69 | 596.65 | 279 (36.0) | 152 (38.1) | |
| 8–12 years | 545.58 | 585.99 | 152 (19.6) | 90 (22.6) | |
| >12 years | 578.72 | 572.23 | 102 (13.2) | 43 (10.8) | |
| p-value | 0.115 | 0.871 | 0.364 | ||
NB * Fischer’s Exact test; Bold = statistically significant.
Table 3.
Pairwise comparisons of knowledge scores in occupation and education variables.
| Sample 1–Sample 2 | Test Statistic | Std. Error | Std. Test Statistic | Sig. |
|---|---|---|---|---|
| Pairwise comparisons of occupation | ||||
| Others—Health technicians | 23.387 | 65.434 | 0.357 | 0.721 |
| Others—Laboratory personnel | 220.410 | 70.500 | 3.126 | 0.002 |
| Others—Physiotherapist | 266.688 | 96.322 | 2.769 | 0.006 |
| Others—Nurses | 331.197 | 63.996 | 5.175 | 0.000 |
| Others—Pharmacist | 489.843 | 67.123 | 7.298 | 0.000 |
| Others—Doctors | 535.421 | 63.713 | 8.404 | 0.000 |
| Health technicians—Laboratory personnel | 197.023 | 40.754 | 4.834 | 0.000 |
| Health technicians—Physiotherapist | 243.301 | 77.256 | 3.149 | 0.002 |
| Health technicians—Nurses | 307.810 | 28.037 | 10.979 | 0.000 |
| Health technicians—Pharmacist | 466.456 | 34.584 | 13.488 | 0.000 |
| Health technicians—Doctors | 512.033 | 27.386 | 18.697 | 0.000 |
| Laboratory personnel—Physiotherapist | −46.278 | 81.591 | −0.567 | 0.571 |
| Laboratory personnel—Nurses | 110.787 | 38.402 | 2.885 | 0.004 |
| Laboratory personnel—Pharmacist | 269.433 | 43.414 | 6.206 | 0.000 |
| Laboratory personnel—Doctors | 315.010 | 37.930 | 8.305 | 0.000 |
| Physiotherapist—Nurses | 64.509 | 76.042 | 0.848 | 0.396 |
| Physiotherapist—Pharmacist | 223.155 | 78.691 | 2.836 | 0.005 |
| Physiotherapist—Doctors | 268.732 | 75.804 | 3.545 | 0.000 |
| Nurses—Pharmacist | 158.646 | 31.779 | 4.992 | 0.000 |
| Nurses—Doctors | 204.224 | 23.745 | 8.601 | 0.000 |
| Pharmacist—Doctors | 45.577 | 31.206 | 1.461 | 0.144 |
| Pairwise comparisons of education categories | ||||
| Diploma—Bachelor | −237.665 | 19.300 | −12.314 | 0.000 |
| Diploma—Post-grad/Specialization | −279.999 | 32.571 | −8.597 | 0.000 |
| Bachelor—Post-grad/Specialization | −42.334 | 32.769 | −1.292 | 0.196 |
NB: Each row tests the null hypothesis that the Sample 1 and Sample 2 distributions are the same. Asymptotic significances (2-sided tests) are displayed. The significance level is 0.05.
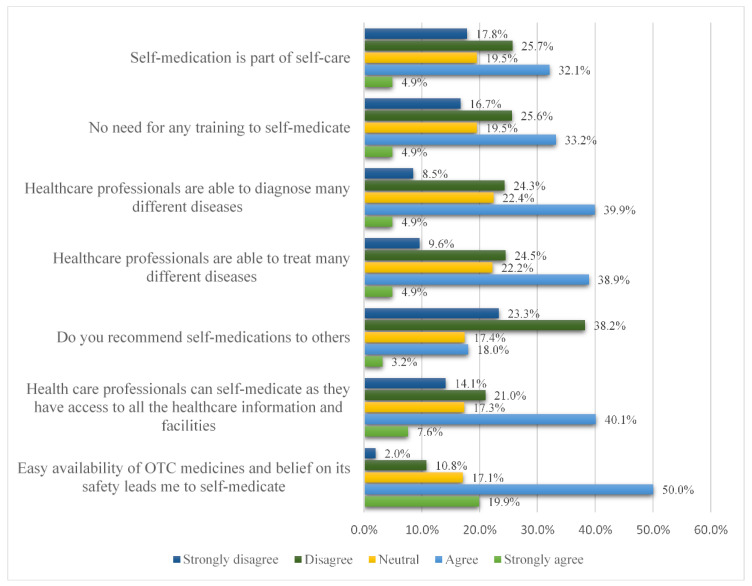
Figure 2 illustrates HCW’s attitudes towards self-medication. Approximately 37% considered self-medication as a part of self-care, and many HCWs were of the opinion that they can diagnose and manage many different diseases by themselves and did not require any advice from a medical specialist. Approximately 62% reported that they do not recommend self-medication to others. Furthermore, an appreciable proportion (strongly agreed 7.6%, agreed 40.1% and neutral 17.3%) of our sample believed they can successfully self-medicate as they had access to all the healthcare information. As shown in Table 2, there was no significant difference in the attitude scores among the different demographic variables.
Figure 2.
Healthcare workers’ attitudes towards self-medication. NB: N = 1173.
Overall, 774 HCWs (60%) reported they were self-medicated during the COVID-19 pandemic. The reasons for self-medication are shown in Table 4. Approximately 42% were taking medication in order to prevent them from catching the virus, whereas 20.7% self-medicated because they suspected they had COVID-19 symptoms. Nearly 28% self-medicated to treat their colds and influenza.
Table 4.
Respondents’ practices related to self-medication amid the COVID pandemic.
| N (%) | |
|---|---|
| Self-medication during COVID-19 * | |
| Yes | 774 (66.0) |
| No | 399 (34.0) |
| Reason for self-medication? ** | |
| Cold or flu | 216 (27.9) |
| COVID-19 prevention | 324 (41.9) |
| Suspected COVID symptoms | 160 (20.7) |
| COVID-19 positive | 36 (4.7) |
| Consuming regularly | 19 (2.5) |
| Miscellaneous | 19 (2.5) |
| Symptom improvement ** | |
| All symptoms improved | 40 (5.1) |
| Many symptoms improved | 326 (42.0) |
| Some symptoms improved | 295 (38.0) |
| One symptom improved | 89 (11.4) |
| No improvement | 28 (3.6) |
NB: * N = 1173; ** N = 774.
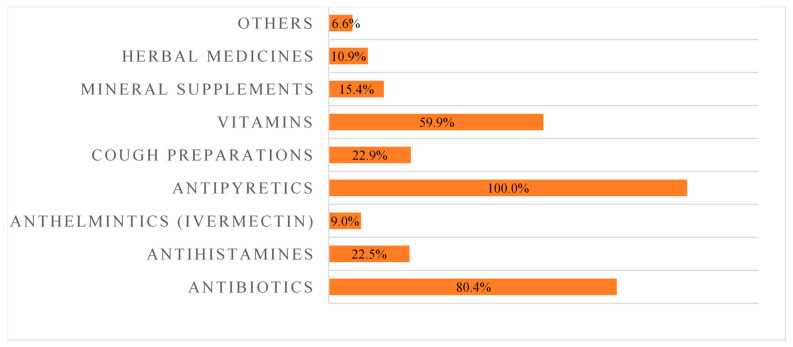
The details of the different types of medicines used for self-medication are shown in Figure 3. The top three most commonly purchased medicines were antipyretics (100%), antibiotics (80.4%) and vitamins (59.9%).
Figure 3.
Pharmacological agents used for self-medication. NB: N = 774.
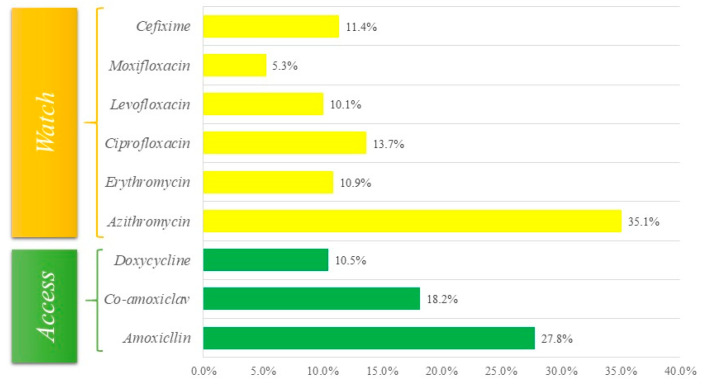
Further details of individual medicines used for self-medication are given in Table 5. A total of nine antibiotics were used for self-medication, with azithromycin being the most commonly purchased antibiotic followed by amoxicillin and co-amoxiclav. A concern is that an appreciable number of purchased antibiotics were “Watch” antibiotics (Figure 4).
Table 5.
Medications self-administered to treat suspected COVID-19.
| Pharmacological Class | Individual Medicine | Overall N (%) |
|---|---|---|
| Antibiotics | Amoxicillin (J01CA04) | 215 (27.8) |
| Co-amoxiclav (J01CR02) | 141 (18.2) | |
| Azithromycin (J01FA10) | 272 (35.1) | |
| Ciprofloxacin (J01MA02) | 106 (13.7) | |
| Levofloxacin (J01MA12) | 78 (10.1) | |
| Moxifloxacin (J01MA14) | 41 (5.3) | |
| Cefixime (J01DD08) | 88 (11.4) | |
| Erythromycin (J01FA01) | 84 (10.9) | |
| Doxycycline (J01AA02) | 81 (10.5) | |
| Antihistamines | Ebastine (R06AX22) | 49 (6.3) |
| Fexofenadine (R06AX26) | 56 (7.2) | |
| Cetirizine (R06AE07) | 85 (11.0) | |
| Anthelmintics | Ivermectin (P02CF01) | 70 (9.0) |
| Vitamins | Multivitamins | 254 (32.8) |
| Vitamin C + Calcium | 314 (40.6) | |
| Mineral supplements | Zinc supplement | 118 (15.2) |
| Antipyretics | Paracetamol | 774 (100.0) |
| Cough preparations | Cough preparations | 177 (22.8) |
| Herbal medicines | -- | 84 (10.9) |
| Others | -- | 51 (6.6) |
NB: N = 774.
Figure 4.
Details of antibiotics purchased by AWaRe classification. NB: “access” and “watch” antibiotics taken from the WHO AWaRe list, see Methods.
A number (9%) of the study participants also reported consuming ivermectin. Out of the 568 HCWs who reported using vitamins, the majority were taking a Vitamin C and calcium combination to boost their immunity. Herbal supplements use was observed in 9% of the study population.
3. Discussion
We believe this is the first study conducted in Pakistan to ascertain the extent of self-medication among HCWs during the recent COVID-19 pandemic. Encouragingly, the response rate was high at 80.9%, and the majority of participating HCWs had good knowledge regarding self-medication. Most participants knew that herbal, over the counter (OTC) and prescription medicines have adverse effects and that consultation among physicians is necessary when adverse events occur. More than one-third of HCWs considered self-medication as a part of self-care and they felt they could diagnose different diseases by themselves. These findings are similar to a study from Saudi Arabia among medical and pharmacy students where most participants had good knowledge of self-medication [103]. However, physicians and pharmacists had better knowledge of self-medication in our study compared with nurses and other HCWs. This is similar to the findings of Akande-Sholabi et al. (2021) in Nigeria, where pharmacy students possessed good knowledge of self-medication versus nursing students [104]. This may be due to the fact that pharmacists generally have good knowledge of medicines, and they are considered to be custodians of medicines. This is reflected by the fact that community pharmacists are often the first healthcare professionals (HCPs) that patients consult with in the community before seeing a physician, further endorsed by the recent COVID-19 pandemic [105,106,107,108,109].
Pharmacists should typically have good knowledge of the adverse effects of medicines and the importance of their appropriate use. Moreover, HCWs having graduate or master degrees had better knowledge compared with diploma holders in our study.
Our study showed that 60% of the HCWs surveyed practiced self-medication during the COVID-19 pandemic, with common reasons for self-medication being the prevention of an infection followed by cold/flu symptoms and suspecting they have COVID-19 infections. These findings are in line with a previous study among medical students from Pakistan, Medical and Pharmacy students in Iran [98,110], as well as among the general population in Peru during the COVID-19 pandemic and globally in pooled studies [55,111]. In addition, this was also the case among HCWs in Nigeria (54.6–89.3%) [104,112]. However, this is in contrast to another study in Nigeria, where only one third of HCWs surveyed practiced self-medication during the COVID-19 pandemic [64], and in Ethiopia (22.7%) [113], with similar findings among pooled studies of HCWs across multiple countries (32.5%) [111].
Paracetamol was consumed by all HCW participants in our study along with variable use of Vitamin C plus calcium (40.6% of HCWs) and multivitamins (32.8%). The high use of paracetamol reflects the typical symptoms of patients, with the variable use of vitamins probably reflecting some of the controversies surrounding their use, including concerns with the evidence base [68,69,70,71,72,73]. However, this needs further investigating before any definitive conclusions can be drawn.
Of concern was the appreciable number of HCWs (80.4%) stating that they were self-medicating with antibiotics despite very limited bacterial co-infections or bacterial secondary infections seen even among patients hospitalized with COVID-19 [4,50,52,53]. In addition, there was appreciable purchasing of “Watch” versus “Access” antibiotics despite regulations limiting such activities. This behavior may relate to the overall stress of potentially contracting COVID-19 and/or concerns with its consequences [114]. These findings are similar to a study among HCWs in Nigeria (71.2%) [112], and also among the general population with COVID-19 in Iran as well as among Medical and Pharmacy students in Iran and Sudan during the pandemic [110,115,116]. However, this is different to HCWs in Togo, where there was only limited self-purchasing of azithromycin (1.4%) to manage their COVID-19 symptoms [117]. This is a concern, as their overuse, particularly of “Watch” antibiotics, will increase AMR rates, and the associated impact on morbidity, which is already a key issue in Pakistan [59,76,77,80,118,119,120]. There are also concerns with self-medication with ivermectin in view of its lack of effectiveness in these patients coupled with concerns with side-effects [42,121,122,123].
Potential ways forward among HCWs, especially in LMICs, include ensuring appropriate knowledge among healthcare students during their studies in order that they are fully conversant regarding antibiotics and antimicrobial stewardship (AMS), as well as helping to undertake antimicrobial stewardship programs (ASPs) on graduation. This includes knowledge of the AWaRe classification of antibiotics, suggested antibiotics for treating a range of infections in both ambulatory and hospital care with the emphasis on “Access” antibiotics, and the implications for excessive prescribing of “Watch” and “Reserve” antibiotics [88,89,124]. This is because there have been concerns with the level of knowledge of these key issues among students and healthcare professionals in LMICs [125,126,127,128,129,130,131,132,133].
In view of these findings, there is a need to ensure that the curricula for new HCWs, including those on diploma courses, adequately covers all key aspects of antibiotics, AMS and ASPs. In this way, helping to ensure that HCWs are fully conversant with these key issues on graduation, which can be built upon post-qualification [80,134]. This includes all the key issues surrounding self-purchasing of antibiotics as the activities of HCWs do influence patient behavior. This is because we do know that trained community pharmacists in LMICs, combined with appropriate guidelines, do recommend alternative approaches to antibiotics for the management of self-limiting viral infections, providing direction for the future [102,105,135,136,137]. This is important going forward, with HCWs necessarily playing a key role in addressing the considerable misinformation surrounding the prevention and treatment of patients with COVID-19 as well as future pandemics [42,101].
We are aware of a number of limitations with this study. Firstly, we only conducted this study in one province in Pakistan. However, Punjab is the most populated province in Pakistan. Secondly, we only conducted the research among public institutions. This was deliberate as they treat the most patients, especially those that are most likely to purchase medicines from pharmacists and drug stores in Pakistan in view of co-payment issues. Thirdly, we generated our own questionnaire. However, this was based on multiple publications together with the experience of the co-authors. In addition, the questionnaire was piloted. Fourthly, there may be over-representation of certain HCW groups as a result of our sampling approach. In addition, there may be under-representation of others if the responders felt that giving wrong answers reflects badly on their group. Overall, despite these limitations, we are confident of our findings in view of the methodology used and the number of HCWs taking part. As a result, we believe our findings will provide direction to the authorities in Pakistan as they move forward with the NAP to reduce AMR rates in Pakistan.
4. Materials and Methods
4.1. Study Design
A cross-sectional study design was employed in this study, and data was collected from HCWs over a four-month period from May–August 2022 using a convenient sampling technique. All HCWs included in the study worked in the public sector among primary, secondary and tertiary healthcare institutions in six districts (Pakpattan, Sahiwal, Faisalabad, Bahawalpur, Okara and Chakwal) of Punjab Province. We chose Punjab Province for this study in view of its population size within Pakistan, i.e., accounting for more than half of the population of Pakistan. Furthermore, similar research has been conducted in this province, with this research following on from existing research studies undertaken by the co-authors [4,50,125,133,138].
4.2. Data Collection Tool and Data Procedure
The data collection tool used in our survey was developed from previous studies combined with the considerable experience of the co-authors as well as observing local practices [55,103,110,113,114,139]. We have used this method before when developing context-specific data collection forms [101,131,140,141,142].
A pilot study was conducted among twenty-five HCWs across a range of different occupations in the districts Pakpattan and Sahiwal to assess the reliability and validity of the study instrument. The overall value of the study instrument fell within the acceptable range of internal consistency.
Following the suggested recommendations from the participants in the pilot study, the final version of the study instrument (Table S1—Supplementary Material) incorporated the following five sections:
Section I: Comprised nine questions relating to the demographic details of the study population. This included their age, gender, residence, marital status, designation, level of education, working department in the hospital, institution type and working experience.
Section II: Consisted of seven questions relating to their knowledge of self-medication. Each questions had three options: “yes”, “no” and “don’t know”, designed to assess the extent of their knowledge about the appropriate use of antibiotics.
Section III: Consisted of seven questions to extract information about the attitude of self-education among HCWs. Study participants were requested to select one option in a 5-item Likert scale, with the 5 items ranging from strongly agree to strongly disagree, which is typically seen in such scales [143,144,145].
Section IV: Consisted of three questions to assess the prevalence of self-medication among the HCWs taking part, their reasons for self-medication and any subsequent improvement in any of their symptoms as a result of self-medication
Section V: Enlisted commonly used types of medicines for self-medication in viral diseases such as COVID-19. These included antibiotics, antiallergic, antipyretics and supplements potentially purchased by the HCWs. Potential choices of antibiotics were based on the experience of the co-authors supplemented with observing local practices. Hydroxychloroquine was not included with high-profile studies, showing no benefit and potential harm [31,37,146].
The data collection team comprised physicians, hospital pharmacists, and pharmacy/laboratory technicians. They subsequently visited the various public health facilities during the study period to enlist support for completing the questionnaire. The study instrument was distributed among the HCWs of these hospitals and they were requested to provide their responses. Completion was entirely voluntary, and informed consent was given before the questionnaires were distributed. The completed study questionnaires were subsequently collected by the investigators, with each questionnaire anonymous to help reduce any misinformation and potential bias in their replies.
4.3. Inclusion and Exclusion Criteria
Our survey included HCWs currently working in public sector primary, secondary and tertiary healthcare facilities in six districts in Punjab Province during the study period (May–August 2022).
Our survey excluded HCWs who were working in other cities in Punjab Province or in the private sector in these six districts during this period. HCWs that did not have enough time to participate in the study were also excluded from our survey.
4.4. Data Analysis Including Statistical Analysis
We entered and analyzed the data in the SPSS® version 22 for Microsoft Windows. Continuous variables were expressed as median and interquartile range, whereas categorical variables were expressed as numbers and percentages. Non-parametric inferential statistical techniques were used to compare knowledge and attitude scores between demographic variables (Mann–Whitney U test and Kruskal–Wallis Test). Chi-Square test was used to determine the difference of self-medication practices between demographic variables. Statistical significance was taken as an alpha value of less than 0.05.
Purchased antibiotics were analyzed in accordance with the WHO AWaRe classification. The “access” group of antibiotics are typically considered as first- or second-line antibiotics for a range of infectious diseases. They generally have a narrow spectrum and low resistance potential. The “watch” group of antibiotics have a higher resistance potential as well as a greater side-effect profile, with the “reserve” group recommended only as a last resort and typically prioritized for any ASPs alongside agreed quality indicators [88,89]. As a result, the WHO is developing quality indicators to reduce the utilization of “Watch” and “Reserve” antibiotics in favor of greater utilization of “Access” antibiotics [147]. In addition, antimicrobials and antihistamines dispensed were classified by their ATC classification [148].
5. Conclusions
In conclusion, the majority of HCWs serving in public sector health facilities of different hospitals in Pakistan did possess appropriate knowledge regarding self-medication. However, there were appreciable levels of self-purchasing of antibiotics, especially those from the “Watch” category. This is a concern that needs to be urgently addressed in Pakistan to reduce rising levels of AMR, especially given the influence of HCWs in Pakistan and beyond in preventing and treating COVID-19.
Key future activities start in the universities to ensure adequate coverage of antibiotics, the AWaRe classification and book containing suggested first and second line treatments for multiple infections and their importance, as well as AMS and ASPs. Coverage of ASPs includes providing adequate input to key tasks to ensure HCWs are confident about implementing them post-qualification. Such educational activities need to be continued post-qualification to help improve the appropriateness of future antimicrobial use as well as address misinformation regarding infectious diseases and their treatment, which has been especially prevalent during the current pandemic.
Community pharmacists have a key role to play in Pakistan in the future to reduce AMR, especially given the existing high levels of self-purchasing of antibiotics among the general population. We have observed that trained pharmacists in some LMICs are directing patients with self-limiting infectious diseases towards alternative treatments that do not include antibiotics, and this should be encouraged in Pakistan. We will be exploring these activities further in future studies.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics12030481/s1, Table S1: Study Questionnaire.
Author Contributions
Z.U.M., S.I., H.R.A., M.S., S.J., T.H.M., Y.H.K. and B.G. were involved with the conceptualization of the study and the methodology. Z.U.M., T.M.S., N.S., J.C.M. and B.G. provided the background for the study assisting with the methodology, Z.U.M., S.I., H.R.A., M.S., S.J., T.H.M. and Y.H.K. were involved with data collection, its analysis and validation. Z.U.M., S.I., H.R.A., M.S., S.J., T.H.M., Y.H.K., N.S., J.C.M. and B.G. assisted with the analysis and interpretation of the data. Z.U.M., T.M.S., N.S., J.C.M. and B.G. assisted with drafting the first paper with all authors contributing to reviewing subsequent drafts before submission. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was approved by the Research Ethics Committee of the Department of Pharmacy Practice, Faculty of Pharmacy, The University of Lahore (Ref. No. REC/DPP/FOP/UOL/67).
Informed Consent Statement
The data collection team obtained informed consent from every study participant before their recruitment into the study. No personal information was collected from the participants, and all subsequent participants were guaranteed confidentiality of their data.
Data Availability Statement
Further data are available upon reasonable request from the co-authors.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Salman M., Mustafa Z.U., Khan T.M., Shehzadi N., Hussain K. How Prepared Was Pakistan for the COVID-19 Outbreak? Disaster Med. Public Health Prep. 2020;14:e44–e45. doi: 10.1017/dmp.2020.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abid K., Bari Y.A., Younas M., Tahir Javaid S., Imran A. Progress of COVID-19 Epidemic in Pakistan. Asia Pac. J. Public Health. 2020;32:154–156. doi: 10.1177/1010539520927259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramzan K., Shafiq S., Raees I., Mustafa Z.U., Salman M., Khan A.H., Meyer J.C., Godman B. Co-Infections, Secondary Infections, and Antimicrobial Use in Patients Hospitalized with COVID-19 during the First Five Waves of the Pandemic in Pakistan; Findings and Implications. Antibiotics. 2022;11:789. doi: 10.3390/antibiotics11060789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ayouni I., Maatoug J., Dhouib W., Zammit N., Fredj S.B., Ghammam R., Ghannem H. Effective public health measures to mitigate the spread of COVID-19: A systematic review. BMC Public Health. 2021;21:1015. doi: 10.1186/s12889-021-11111-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Talic S., Shah S., Wild H., Gasevic D., Maharaj A., Ademi Z., Li X., Xu W., Mesa-Eguiagaray I., Rostron J., et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: Systematic review and meta-analysis. BMJ. 2021;375:e068302. doi: 10.1136/bmj-2021-068302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogunleye O.O., Basu D., Mueller D., Sneddon J., Seaton R.A., Yinka-Ogunleye A.F., Wamboga J., Miljkovi’c N., Mwita J.C., Rwegerera G.M., et al. Response to the Novel Corona Virus (COVID-19) Pandemic Across Africa: Successes, Challenges, and Implications for the Future. Front. Pharmacol. 2020;11:1205. doi: 10.3389/fphar.2020.01205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iqbal M., Zahidie A. Pakistan’s Health System Against COVID-19: Where Do Things Stand? J. Coll. Physicians Surg. Pak. 2020;30:3–8. doi: 10.29271/jcpsp.2020.Supp1.S3. [DOI] [PubMed] [Google Scholar]
- 9.Bilawal Khaskheli M., Wang S., Hussain R.Y., Jahanzeb Butt M., Yan X., Majid S. Global law, policy, and governance for effective prevention and control of COVID-19: A comparative analysis of the law and policy of Pakistan, China, and Russia. Front. Public Health. 2022;10:1035536. doi: 10.3389/fpubh.2022.1035536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zakar R., Yousaf F., Zakar M.Z., Fischer F. Sociocultural Challenges in the Implementation of COVID-19 Public Health Measures: Results From a Qualitative Study in Punjab, Pakistan. Front. Public Health. 2021;9:703825. doi: 10.3389/fpubh.2021.703825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO WHO Coronavirus (COVID-19) Dashboard. 2023. [(accessed on 26 January 2023)]. Available online: https://covid19.who.int/
- 12.Vargese S.S., Dev S.S., Soman A.S., Kurian N., Varghese V.A., Mathew E. Exposure risk and COVID-19 infection among frontline health-care workers: A single tertiary care centre experience. Clin. Epidemiol. Glob. Health. 2022;13:100933. doi: 10.1016/j.cegh.2021.100933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haq F.U., Rahman S.U., Imran M., Romman M., Shah A., Aslam Z., Ullah F., Madadi S., Steinmetz C.D., Cuschieri S., et al. COVID-19 among health care workers and their impact on the health care system in a teaching hospital in Pakistan: A cross sectional observational study. Health Sci. Rep. 2023;6:e975. doi: 10.1002/hsr2.975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Razu S.R., Yasmin T., Arif T.B., Islam M.S., Islam S.M.S., Gesesew H.A., Ward P. Challenges Faced by Healthcare Professionals During the COVID-19 Pandemic: A Qualitative Inquiry From Bangladesh. Front. Public Health. 2021;9:647315. doi: 10.3389/fpubh.2021.647315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muiry R., Parsons V., Madan I. Risks posed by COVID-19 to healthcare workers. Occup. Med. 2021;71:56–58. doi: 10.1093/occmed/kqaa191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen L.H., Drew D.A., Graham M.S., Joshi A.D., Guo C.G., Ma W., Mehta R.S., Warner E.T., Sikavi D.R., Lo C.-H., et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health. 2020;5:e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deressa W., Worku A., Abebe W., Gizaw M., Amogne W. Risk perceptions and preventive practices of COVID-19 among healthcare professionals in public hospitals in Addis Ababa, Ethiopia. PLoS ONE. 2021;16:e0242471. doi: 10.1371/journal.pone.0242471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Almohammed O.A., Aldwihi L.A., Alragas A.M., Almoteer A.I., Gopalakrishnan S., Alqahtani N.M. Knowledge, Attitude, and Practices Associated With COVID-19 Among Healthcare Workers in Hospitals: A Cross-Sectional Study in Saudi Arabia. Front. Public Health. 2021;9:643053. doi: 10.3389/fpubh.2021.643053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chou R., Dana T., Buckley D.I., Selph S., Fu R., Totten A.M. Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers: A Living Rapid Review. Ann. Intern. Med. 2020;173:120–136. doi: 10.7326/M20-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang J.Y., Parkins M.D., Canakis A., Aroniadis O.C., Yadav D., Dixon R.E., Joseph Elmunzer B., Forbes N., DMC-19 Study Group and the North American Alliance for the Study of Digestive Manifestations of COVID-19 Outcomes of COVID-19 Among Hospitalized Health Care Workers in North America. JAMA Netw. Open. 2021;4:e2035699. doi: 10.1001/jamanetworkopen.2020.35699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO Director-General’s Opening Remarks at the World Health Assembly—24 May 2021. [(accessed on 30 January 2023)]. Available online: https://www.who.int/director-general/speeches/detail/director-general-s-opening-remarks-at-the-world-health-assembly.
- 22.GeoNews 143 Health Workers Have Lost Life to Coronavirus in Pakistan so Far. [(accessed on 30 January 2023)]. Available online: https://www.geo.tv/latest/340998-143-health-workers-have-lost-life-to-coronavirus-in-pakistan-so-far.
- 23.Galanis P., Vraka I., Fragkou D., Bilali A., Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J. Adv. Nurs. 2021;77:3286–3302. doi: 10.1111/jan.14839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aldhamin R.A., Al Saif A.Z. The mental health of healthcare workers in GCC countries during the COVID-19 pandemic: A systematic review and meta-analysis. J. Taibah Univ. Med. Sci. 2023;18:45–60. doi: 10.1016/j.jtumed.2022.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saragih I.D., Tonapa S.I., Saragih I.S., Advani S., Batubara S.O., Suarilah I., Lin C.-J. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2021;121:104002. doi: 10.1016/j.ijnurstu.2021.104002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aymerich C., Pedruzo B., Pérez J.L., Laborda M., Herrero J., Blanco J., Mancebo G., Andrés L., Estévez O., Fernandez M., et al. COVID-19 pandemic effects on health worker’s mental health: Systematic review and meta-analysis. Eur. Psychiatry. 2022;65:e10. doi: 10.1192/j.eurpsy.2022.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Salman M., Mustafa Z.U., Raza M.H., Khan T.M., Asif N., Tahir H., Shehzadi N., Mallhi T.H., Khan Y.H., Sultana K., et al. Psychological Effects of COVID-19 Among Health Care Workers, and How They Are Coping: A Web-Based, Cross-Sectional Study During the First Wave of COVID-19 in Pakistan. Disaster Med. Public Health Prep. 2022;17:1–6. doi: 10.1017/dmp.2022.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khan T.M., Tahir H., Salman M., Ul Mustafa Z., Raza M.H., Asif N., Shehzadi N., Hussain K., Al-Worafi Y.M., Baig M.R. General Anxiety Predictors among Frontline Warriors of COVID: Cross-Sectional Study among Nursing Staff in Punjab, Pakistan. Arch. Pharm. Pract. 2021;12:40–44. doi: 10.51847/A0j3y5qmHp. [DOI] [Google Scholar]
- 29.Quincho-Lopez A., Benites-Ibarra C.A., Hilario-Gomez M.M., Quijano-Escate R., Taype-Rondan A. Self-medication practices to prevent or manage COVID-19: A systematic review. PLoS ONE. 2021;16:e0259317. doi: 10.1371/journal.pone.0259317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Siemieniuk R.A., Bartoszko J.J., Ge L., Zeraatkar D., Izcovich A., Kum E., Izcovich A., Lamontagne F., Han M.A., Agarwal A., et al. Drug Treatments For Covid-19: Living Systematic Review and Network Meta-Analysis. BMJ. 2020;370:M2980. doi: 10.1136/bmj.m2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Horby P., Mafham M., Linsell L., Bell J.L., Staplin N., Emberson J.R., Wiselka M., Ustianowski A., Elmahi E., Prudon B., et al. Effect of Hydroxychloroquine in Hospitalized Patients with Covid-19. N. Engl. J. Med. 2020;383:2030–2040. doi: 10.1056/NEJMoa2022926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dyer O. COVID-19: Remdesivir has little or no impact on survival, WHO trial shows. BMJ. 2020;371:m4057. doi: 10.1136/bmj.m4057. [DOI] [PubMed] [Google Scholar]
- 33.Charan J., Kaur R.J., Bhardwaj P., Haque M., Sharma P., Misra S., Godman B. Rapid review of suspected adverse drug events due to remdesivir in the WHO database; findings and implications. Expert Rev. Clin. Pharmacol. 2021;14:95–103. doi: 10.1080/17512433.2021.1856655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lopinavir-ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet. 2020;396:1345–1352. doi: 10.1016/S0140-6736(20)32013-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.WHO Solidarity Trail Consortium. Pan H., Peto R., Henao-Restrepo A.M., Preziosi M.P., Sathiyamoorthy V., Abdool Karim Q., Alejandria M.M., García C.H., Kieny M.-P., et al. Repurposed Antiviral Drugs for Covid-19—Interim WHO Solidarity Trial Results. N. Engl. J. Med. 2021;384:497–511. doi: 10.1056/NEJMoa2023184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.WHO WHO Discontinues Hydroxychloroquine and Lopinavir/Ritonavir Treatment Arms for COVID-19. 2020. [(accessed on 23 January 2023)]. Available online: https://www.who.int/news/item/04-07-2020-who-discontinues-hydroxychloroquine-and-lopinavir-ritonavir-treatment-arms-for-covid-19.
- 37.Abena P.M., Decloedt E.H., Bottieau E., Suleman F., Adejumo P., Sam-Agudu N.A., Muyembe TamFum J.-J., Seydi M., Eholie S.P., Mills E.J., et al. Chloroquine and Hydroxychloroquine for the Prevention or Treatment of COVID-19 in Africa: Caution for Inappropriate Off-label Use in Healthcare Settings. Am. J. Trop. Med. Hyg. 2020;102:1184–1188. doi: 10.4269/ajtmh.20-0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ferner R.E., Aronson J.K. Chloroquine and hydroxychloroquine in covid-19. BMJ. 2020;369:m1432. doi: 10.1136/bmj.m1432. [DOI] [PubMed] [Google Scholar]
- 39.ReportLinker Hydroxychloroquine Global Market Report 2021: COVID-19 Implications and Growth to 2030. 2021. [(accessed on 20 February 2023)]. Available online: https://finance.yahoo.com/news/hydroxychloroquine-global-market-report-2021-110000367.html?fr=sycsrp_catchall.
- 40.Sefah I.A., Ogunleye O.O., Essah D.O., Opanga S.A., Butt N., Wamaitha A., Guantai A.N., Chikowe I., Khuluza F., Kibuule D., et al. Rapid Assessment of the Potential Paucity and Price Increases for Suggested Medicines and Protection Equipment for COVID-19 Across Developing Countries With a Particular Focus on Africa and the Implications. Front. Pharmacol. 2020;11:588106. doi: 10.3389/fphar.2020.588106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.RECOVERY Collaborative Group. Horby P., Lim W.S., Emberson J.R., Mafham M., Bell J.L., Linsell L., Staplin N., Brightling C., Ustianowski A., et al. Dexamethasone in Hospitalized Patients with Covid-19. N. Engl. J. Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schellack N., Strydom M., Pepper M.S., Herd C.L., Hendricks C.L., Bronkhorst E., Meyer J.C., Padayachee N., Bangalee V., Truter I., et al. Social Media and COVID-19—Perceptions and Public Deceptions of Ivermectin, Colchicine and Hydroxychloroquine: Lessons for Future Pandemics. Antibiotics. 2022;11:445. doi: 10.3390/antibiotics11040445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rocha Y.M., de Moura G.A., Desidério G.A., de Oliveira C.H., Lourenço F.D., de Figueiredo Nicolete L.D. The impact of fake news on social media and its influence on health during the COVID-19 pandemic: A systematic review. Z Gesundh Wiss. 2021:1–10. doi: 10.1007/s10389-021-01658-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stewart R., Madonsela A., Tshabalala N., Etale L., Theunissen N. The importance of social media users’ responses in tackling digital COVID-19 misinformation in Africa. Digit Health. 2022;8:20552076221085070. doi: 10.1177/20552076221085070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Joseph A.M., Fernandez V., Kritzman S., Eaddy I., Cook O.M., Lambros S., Jara Silva C.E., Arguelles D., Abraham C., Dorgham N., et al. COVID-19 Misinformation on Social Media: A Scoping Review. Cureus. 2022;14:e24601. doi: 10.7759/cureus.24601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.ISAC/Elsevier Statement Joint ISAC and Elsevier Statement on Gautret et al. paper [PMID 32205204] 2020. [(accessed on 20 February 2023)]. Available online: https://www.isac.world/news-and-publications/isac-elsevier-statement.
- 47.Al-Hadidi S.H., Alhussain H., Abdel Hadi H., Johar A., Yassine H.M., Al Thani A.A., Eltai N.O. The Spectrum of Antibiotic Prescribing During COVID-19 Pandemic: A Systematic Literature Review. Microb. Drug Resist. 2021;27:1705–1725. doi: 10.1089/mdr.2020.0619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mondal U.K., Haque T., Biswas M., Satter S.M., Islam M.S., Alam Z., Shojon M., Debnath S., Islam M., Murshid H.B., et al. Antibiotic Prescribing Practices for Treating COVID-19 Patients in Bangladesh. Antibiotics. 2022;11:1350. doi: 10.3390/antibiotics11101350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kamara I.F., Kumar A.M.V., Maruta A., Fofanah B.D., Njuguna C.K., Shongwe S., Moses F., Tengbe S.M., Kanu J.S., Lakoh S., et al. Antibiotic Use in Suspected and Confirmed COVID-19 Patients Admitted to Health Facilities in Sierra Leone in 2020-2021: Practice Does Not Follow Policy. Int. J. Environ. Res. Public Health. 2022;19:4005. doi: 10.3390/ijerph19074005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mustafa Z.U., Saleem M.S., Ikram M.N., Salman M., Butt S.A., Khan S., Godman B., Seaton R.S. Co-infections and antimicrobial use among hospitalized COVID-19 patients in Punjab, Pakistan: Findings from a multicenter, point prevalence survey. Pathog. Glob. Health. 2022;116:421–427. doi: 10.1080/20477724.2021.1999716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Langford B.J., So M., Raybardhan S., Leung V., Soucy J.R., Westwood D., Daneman N., MacFadden D.R. Antibiotic prescribing in patients with COVID-19: Rapid review and meta-analysis. Clin. Microbiol. Infect. 2021;27:520–531. doi: 10.1016/j.cmi.2020.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Langford B.J., So M., Raybardhan S., Leung V., Westwood D., MacFadden D.R., Soucy J.-P.R., Daneman N. Bacterial co-infection and secondary infection in patients with COVID-19: A living rapid review and meta-analysis. Clin. Microbiol. Infect. 2020;26:1622–1629. doi: 10.1016/j.cmi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lansbury L., Lim B., Baskaran V., Lim W.S. Co-infections in people with COVID-19: A systematic review and meta-analysis. J. Infect. 2020;81:266–275. doi: 10.1016/j.jinf.2020.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sulis G., Batomen B., Kotwani A., Pai M., Gandra S. Sales of antibiotics and hydroxychloroquine in India during the COVID-19 epidemic: An interrupted time series analysis. PLoS Med. 2021;18:e1003682. doi: 10.1371/journal.pmed.1003682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Quispe-Cañari J.F., Fidel-Rosales E., Manrique D., Mascaró-Zan J., Huamán-Castillón K.M., Chamorro-Espinoza S.E., Garayar-Peceros H., Ponce-López V.L., Sifuentes-Rosales I., Alvarez-Risco A., et al. Self-medication practices during the COVID-19 pandemic among the adult population in Peru: A cross-sectional survey. Saudi Pharm. J. 2021;29:1–11. doi: 10.1016/j.jsps.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Saleem Z., Hassali M.A., Godman B., Fatima M., Ahmad Z., Sajid A., Rehman I.U., Nadeem M.U., Javaid Z., Malik M., et al. Sale of WHO AWaRe groups antibiotics without a prescription in Pakistan: A simulated client study. J. Pharm. Policy Pract. 2020;13:26. doi: 10.1186/s40545-020-00233-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ahmad T., Khan F.U., Ali S., Rahman A.U., Ali Khan S. Assessment of without prescription antibiotic dispensing at community pharmacies in Hazara Division, Pakistan: A simulated client’s study. PLoS ONE. 2022;17:e0263756. doi: 10.1371/journal.pone.0263756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Saleem Z., Hassali M.A., Hashmi F.K., Godman B., Saleem F. Antimicrobial dispensing practices and determinants of antimicrobial resistance: A qualitative study among community pharmacists in Pakistan. Fam. Med. Community Health. 2019;7:e000138. doi: 10.1136/fmch-2019-000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Antimicrobial Resistance Collaborators Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet. 2022;399:629–655. doi: 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Founou R.C., Blocker A.J., Noubom M., Tsayem C., Choukem S.P., Dongen M.V., Founou L.L. The COVID-19 pandemic: A threat to antimicrobial resistance containment. Future Sci. OA. 2021;7:Fso736. doi: 10.2144/fsoa-2021-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hsu J. How covid-19 is accelerating the threat of antimicrobial resistance. BMJ. 2020;369:m1983. doi: 10.1136/bmj.m1983. [DOI] [PubMed] [Google Scholar]
- 62.Hofer U. The cost of antimicrobial resistance. Nat. Rev. Microbiol. 2019;17:3. doi: 10.1038/s41579-018-0125-x. [DOI] [PubMed] [Google Scholar]
- 63.OECD Health Policy Studies Stemming the Superbug Tide. 2018. [(accessed on 28 January 2023)]. Available online: https://www.oecd-ilibrary.org/sites/9789264307599-en/index.html?itemId=/content/publication/9789264307599-en&mimeType=text/html.
- 64.Okoye O.C., Adejumo O.A., Opadeyi A.O., Madubuko C.R., Ntaji M., Okonkwo K.C., Edeki I.R., Agboje U.O., Alli O.E., Ohaju-Obodo J.O., et al. Self medication practices and its determinants in health care professionals during the coronavirus disease-2019 pandemic: Cross-sectional study. Int. J. Clin. Pharm. 2022;44:507–516. doi: 10.1007/s11096-021-01374-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Onchonga D., Omwoyo J., Nyamamba D. Assessing the prevalence of self-medication among healthcare workers before and during the 2019 SARS-CoV-2 (COVID-19) pandemic in Kenya. Saudi Pharm. J. 2020;28:1149–1154. doi: 10.1016/j.jsps.2020.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sachdev C., Anjankar A., Agrawal J. Self-Medication With Antibiotics: An Element Increasing Resistance. Cureus. 2022;14:e30844. doi: 10.7759/cureus.30844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Elayeh E., Akour A., Haddadin R.N. Prevalence and predictors of self-medication drugs to prevent or treat COVID-19: Experience from a Middle Eastern country. Int. J. Clin. Pract. 2021;75:e14860. doi: 10.1111/ijcp.14860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pal R., Banerjee M., Bhadada S.K., Shetty A.J., Singh B., Vyas A. Vitamin D supplementation and clinical outcomes in COVID-19: A systematic review and meta-analysis. J. Endocrinol. Investig. 2022;45:53–68. doi: 10.1007/s40618-021-01614-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Petrelli F., Luciani A., Perego G., Dognini G., Colombelli P.L., Ghidini A. Therapeutic and prognostic role of vitamin D for COVID-19 infection: A systematic review and meta-analysis of 43 observational studies. J. Steroid Biochem. Mol. Biol. 2021;211:105883. doi: 10.1016/j.jsbmb.2021.105883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Szarpak L., Filipiak K.J., Gasecka A., Gawel W., Koziel D., Jaguszewski M.J., Chmielewski J., Gozhenko A., Bielski K., Wroblewski P., et al. Vitamin D supplementation to treat SARS-CoV-2 positive patients. Evidence from meta-analysis. Cardiol. J. 2022;29:188–196. doi: 10.5603/CJ.a2021.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chiscano-Camón L., Ruiz-Rodriguez J.C., Ruiz-Sanmartin A., Roca O., Ferrer R. Vitamin C levels in patients with SARS-CoV-2-associated acute respiratory distress syndrome. Crit. Care. 2020;24:522. doi: 10.1186/s13054-020-03249-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Carr A.C., Rowe S. The Emerging Role of Vitamin C in the Prevention and Treatment of COVID-19. Nutrients. 2020;12:3286. doi: 10.3390/nu12113286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mehta N., Pokharna P., Shetty S.R. Unwinding the potentials of vitamin C in COVID-19 and other diseases: An updated review. Nutr. Health. 2022:2601060221139628. doi: 10.1177/02601060221139628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tasneem U., Majid M., Mehmood K., Redaina Rehman F.U., Andleeb S., Jamal M. Co-occurrence of antibiotic resistance and virulence Genes in Methicillin Resistant Staphylococcus aureus (MRSA) Isolates from Pakistan. Afr. Health Sci. 2022;22:486–495. doi: 10.4314/ahs.v22i1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Arshad F., Saleem S., Tahir R., Ghazal A., Khawaja A., Jahan S. Four year trend of antimicrobial susceptibility of methicillin-resistant Staphylococcus aureus in a tertiary care hospital, Lahore. J. Pak. Med. Assoc. 2022;72:296–299. doi: 10.47391/JPMA.20-509. [DOI] [PubMed] [Google Scholar]
- 76.Bilal H., Khan M.N., Rehman T., Hameed M.F., Yang X. Antibiotic resistance in Pakistan: A systematic review of past decade. BMC Infect. Dis. 2021;21:244. doi: 10.1186/s12879-021-05906-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Saleem Z., Hassali M.A., Hashmi F.K. Pakistan’s national action plan for antimicrobial resistance: Translating ideas into reality. Lancet Infect. Dis. 2018;18:1066–1067. doi: 10.1016/S1473-3099(18)30516-4. [DOI] [PubMed] [Google Scholar]
- 78.Auta A., Hadi M.A., Oga E., Adewuyi E.O., Abdu-Aguye S.N., Adeloye D., Strickland-Hodge B., Morgan D.J. Global access to antibiotics without prescription in community pharmacies: A systematic review and meta-analysis. J. Infect. 2019;78:8–18. doi: 10.1016/j.jinf.2018.07.001. [DOI] [PubMed] [Google Scholar]
- 79.Nepal G., Bhatta S. Self-medication with Antibiotics in WHO Southeast Asian Region: A Systematic Review. Cureus. 2018;10:e2428. doi: 10.7759/cureus.2428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Godman B., Egwuenu A., Haque M., Malande O.O., Schellack N., Kumar S., Saleem Z., Sneddon J., Hoxha I., Islam S., et al. Strategies to Improve Antimicrobial Utilization with a Special Focus on Developing Countries. Life. 2021;11:528. doi: 10.3390/life11060528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Torres N.F., Chibi B., Kuupiel D., Solomon V.P., Mashamba-Thompson T.P., Middleton L.E. The use of non-prescribed antibiotics; prevalence estimates in low-and-middle-income countries. A systematic review and meta-analysis. Arch. Public Health. 2021;79:2. doi: 10.1186/s13690-020-00517-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Afari-Asiedu S., Abdulai M.A., Tostmann A., Boamah-Kaali E., Asante K.P., Wertheim H.F.L., Hulscher M. Interventions to improve dispensing of antibiotics at the community level in low and middle income countries: A systematic review. J. Glob. Antimicrob. Resist. 2022;29:259–274. doi: 10.1016/j.jgar.2022.03.009. [DOI] [PubMed] [Google Scholar]
- 83.Do N.T.T., Vu H.T.L., Nguyen C.T.K., Punpuing S., Khan W.A., Gyapong M., Asante K.P., Munguambe K., Xavier Gómez-Olivé F., John-Langba J., et al. Community-based antibiotic access and use in six low-income and middle-income countries: A mixed-method approach. Lancet Glob. Health. 2021;9:e610–e619. doi: 10.1016/S2214-109X(21)00024-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rather I.A., Kim B.C., Bajpai V.K., Park Y.H. Self-medication and antibiotic resistance: Crisis, current challenges, and prevention. Saudi J. Biol. Sci. 2017;24:808–812. doi: 10.1016/j.sjbs.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Aslam A., Zin C.S., Jamshed S., Rahman N.S.A., Ahmed S.I., Pallós P., Gajdács M. Self-Medication with Antibiotics: Prevalence, Practices and Related Factors among the Pakistani Public. Antibiotics. 2022;11:795. doi: 10.3390/antibiotics11060795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Nazir S., Azim M. Assessment of antibiotic self-medication practice among public in the northwestern region of Pakistan. Eur. J. Hosp. Pharm. 2017;24:200–203. doi: 10.1136/ejhpharm-2015-000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Shah S.J., Ahmad H., Rehan R.B., Najeeb S., Mumtaz M., Jilani M.H., Rabbani M.S., Alam M.Z., Farooq S., Kadir M., et al. Self-medication with antibiotics among non-medical university students of Karachi: A cross-sectional study. BMC Pharmacol. Toxicol. 2014;15:74. doi: 10.1186/2050-6511-15-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sharland M., Gandra S., Huttner B., Moja L., Pulcini C., Zeng M., Mendelson M., Cappello B., Cooke G., Magrini N., et al. Encouraging AWaRe-ness and discouraging inappropriate antibiotic use-the new 2019 Essential Medicines List becomes a global antibiotic stewardship tool. Lancet Infect. Dis. 2019;19:1278–1280. doi: 10.1016/S1473-3099(19)30532-8. [DOI] [PubMed] [Google Scholar]
- 89.Sulis G., Sayood S., Katukoori S., Bollam N., George I., Yaeger L.H., Chavez M.A., Tetteh E., Yarrabelli S., Pulcini C., et al. Exposure to World Health Organization’s AWaRe antibiotics and isolation of multidrug resistant bacteria: A systematic review and meta-analysis. Clin. Microbiol. Infect. 2022;28:1193–1202. doi: 10.1016/j.cmi.2022.03.014. [DOI] [PubMed] [Google Scholar]
- 90.Saleem Z., Hassali M.A., Versporten A., Godman B., Hashmi F.K., Goossens H., Saleem F. A multicenter point prevalence survey of antibiotic use in Punjab, Pakistan: Findings and implications. Expert Rev. Anti Infect Ther. 2019;17:285–293. doi: 10.1080/14787210.2019.1581063. [DOI] [PubMed] [Google Scholar]
- 91.Ali H., Zafar F., Alam S., Beg A.E., Bushra R., Manzoor A., Naqvi G.R., Yasmeen R., Shafiq Y., Tariq A., et al. Drug utilization and prescribing pattern of antibiotics in a tertiary care setups; trends and practices. Pak. J. Pharm. Sci. 2018;31:691–697. [PubMed] [Google Scholar]
- 92.Saleem Z., Haseeb A., Godman B., Batool N., Altaf U., Ahsan U., Khan F.U., Mustafa Z.U., Nadeem M.U., Farrukh M.J., et al. Point Prevalence Survey of Antimicrobial Use during the COVID-19 Pandemic among Different Hospitals in Pakistan: Findings and Implications. Antibiotics. 2023;12:70. doi: 10.3390/antibiotics12010070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mustafa Z.U., Salman M., Yasir M., Godman B., Majeed H.A., Kanwal M., Iqbal M., Riaz M.B., Hayat K., Hasan S.S. Antibiotic consumption among hospitalized neonates and children in Punjab province, Pakistan. Expert Rev. Anti Infect Ther. 2022;20:931–939. doi: 10.1080/14787210.2021.1986388. [DOI] [PubMed] [Google Scholar]
- 94.Raza S.Q., Waqar M.A., Ahmad S., Iqbal H.A., Saifullah A. Trends Toward Self-Medication Practices During COVID-19 in Gujranwala District. Pak. J. Health Sci. 2022;3:198–202. doi: 10.54393/pjhs.v3i06.259. [DOI] [Google Scholar]
- 95.Iqbal Arain M., Shahnaz S., Anwar R., Anwar K. Assessment of Self-medication Practices During COVID-19 Pandemic in Hyderabad and Karachi, Pakistan. Sudan J. Med. Sci. 2021;3:347–354. doi: 10.18502/sjms.v16i3.9696. [DOI] [Google Scholar]
- 96.Chaudhry B., Azhar S., Jamshed S., Ahmed J., Khan L.U., Saeed Z., Madléna M., Gajdács M., Rasheed A. Factors Associated with Self-Medication during the COVID-19 Pandemic: A Cross-Sectional Study in Pakistan. Trop. Med. Infect. Dis. 2022;7:330. doi: 10.3390/tropicalmed7110330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Saleem R.T.B.M., Ahmad A., Amin M., Amir A., Ahsan A., Fayyaz F., Saleem R., Riaz T., Waheed U., Zaman M. Practices and Attitude of Self-Medication during COVID-19 Pandemic in University Students with Interventional Role of Pharmacist: A Regional Analysis. [(accessed on 30 January 2022)];Lat. Am. J. Pharm. 2021 40:1946–1953. Available online: http://latamjpharm.org/resumenes/40/8/LAJOP_40_8_1_37.pdf. [Google Scholar]
- 98.Yasmin F., Asghar M.S., Naeem U., Najeeb H., Nauman H., Ahsan M.N., Khattak A.K. Self-Medication Practices in Medical Students During the COVID-19 Pandemic: A Cross-Sectional Analysis. Front. Public Health. 2022;10:803937. doi: 10.3389/fpubh.2022.803937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Biswas N., Mustapha T., Khubchandani J., Price J.H. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J. Community Health. 2021;46:1244–1251. doi: 10.1007/s10900-021-00984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ackah M., Ameyaw L., Gazali Salifu M., Afi Asubonteng D.P., Osei Yeboah C., Narkotey Annor E., Ankapong E.A.K., Boakye H. COVID-19 vaccine acceptance among health care workers in Africa: A systematic review and meta-analysis. PLoS ONE. 2022;17:e0268711. doi: 10.1371/journal.pone.0268711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ogunleye O.O., Godman B., Fadare J.O., Mudenda S., Adeoti A.O., Yinka-Ogunleye A.F., Ogundele S.O., Oyawole M.R., Schönfeldt M., Rashed W.M., et al. Coronavirus Disease 2019 (COVID-19) Pandemic across Africa: Current Status of Vaccinations and Implications for the Future. Vaccines. 2022;10:1553. doi: 10.3390/vaccines10091553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kibuule D., Nambahu L., Sefah I.A., Kurdi A., Phuong T.N.T., Kwon H.-Y., Godman B. Activities in Namibia to limit the prevalence and mortality from COVID-19 including community pharmacy activities and the implications. Sch. Acad. J. Pharm. 2021;5:82–92. doi: 10.36347/sajp.2021.v10i05.001. [DOI] [Google Scholar]
- 103.Alduraibi R.K., Altowayan W.M. A cross-sectional survey: Knowledge, attitudes, and practices of self-medication in medical and pharmacy students. BMC Health Serv. Res. 2022;22:352. doi: 10.1186/s12913-022-07704-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Akande-Sholabi W., Ajamu A.T., Adisa R. Prevalence, knowledge and perception of self-medication practice among undergraduate healthcare students. J. Pharm. Policy Pract. 2021;14:49. doi: 10.1186/s40545-021-00331-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Marković-Peković V., Grubiša N., Burger J., Bojanić L., Godman B. Initiatives to Reduce Nonprescription Sales and Dispensing of Antibiotics: Findings and Implications. J. Res. Pharm. Pract. 2017;6:120–125. doi: 10.4103/jrpp.JRPP_17_12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Agomo C.O. The role of community pharmacists in public health: A scoping review of the literature. J. Pharm. Health Serv. Res. 2012;3:25–33. doi: 10.1111/j.1759-8893.2011.00074.x. [DOI] [Google Scholar]
- 107.Rajiah K., Sivarasa S., Maharajan M.K. Impact of Pharmacists’ Interventions and Patients’ Decision on Health Outcomes in Terms of Medication Adherence and Quality Use of Medicines among Patients Attending Community Pharmacies: A Systematic Review. Int. J. Environ. Res. Public Health. 2021;18:4392. doi: 10.3390/ijerph18094392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cadogan C.A., Hughes C.M. On the frontline against COVID-19: Community pharmacists’ contribution during a public health crisis. Res. Soc. Adm. Pharm. 2021;17:2032–2035. doi: 10.1016/j.sapharm.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hedima E.W., Adeyemi M.S., Ikunaiye N.Y. Community Pharmacists: On the frontline of health service against COVID-19 in LMICs. Res. Soc. Adm. Pharm. 2021;17:1964–1966. doi: 10.1016/j.sapharm.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Hashemzaei M., Afshari M., Koohkan Z., Bazi A., Rezaee R., Tabrizian K. Knowledge, attitude, and practice of pharmacy and medical students regarding self-medication, a study in Zabol University of Medical Sciences; Sistan and Baluchestan province in south-east of Iran. BMC Med. Educ. 2021;21:49. doi: 10.1186/s12909-020-02374-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kazemioula G., Golestani S., Alavi S.M.A., Taheri F., Gheshlagh R.G., Lotfalizadeh M.H. Prevalence of self-medication during COVID-19 pandemic: A systematic review and meta-analysis. Front. Public Health. 2022;10:1041695. doi: 10.3389/fpubh.2022.1041695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Tobin E.A., Okonofua M.O., Adeke A.S., Obi A. Willingness to Accept a COVID-19 Vaccine in Nigeria: A Population-based Cross-sectional Study. Cent. Afr. J. Public Health. 2021;7:53–60. doi: 10.11648/j.cajph.20210702.12. [DOI] [Google Scholar]
- 113.Kassa T., Gedif T., Andualem T., Aferu T. Antibiotics self-medication practices among health care professionals in selected public hospitals of Addis Ababa, Ethiopia. Heliyon. 2022;8:e08825. doi: 10.1016/j.heliyon.2022.e08825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhang A., Hobman E.V., De Barro P., Young A., Carter D.J., Byrne M. Self-Medication with Antibiotics for Protection against COVID-19: The Role of Psychological Distress, Knowledge of, and Experiences with Antibiotics. Antibiotics. 2021;10:232. doi: 10.3390/antibiotics10030232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mahmoudi H. Assessment of knowledge, attitudes, and practice regarding antibiotic self-treatment use among COVID-19 patients. GMS Hyg. Infect. Control. 2022;17:Doc12. doi: 10.3205/dgkh000415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Elmahi O.K.O., Musa R.A.E., Shareef A.A.H., Omer M.E.A., Elmahi M.A.M., Altamih R.A.A., Mohamed R.I.H., Alsadig T.F.M. Perception and practice of self-medication with antibiotics among medical students in Sudanese universities: A cross-sectional study. PLoS ONE. 2022;17:e0263067. doi: 10.1371/journal.pone.0263067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Sadio A.J., Gbeasor-Komlanvi F.A., Konu R.Y., Bakoubayi A.W., Tchankoni M.K., Bitty-Anderson A.M., Gomez I.M., Denadou C.P., Anani J., Kouanfack H.R., et al. Assessment of self-medication practices in the context of the COVID-19 outbreak in Togo. BMC Public Health. 2021;21:58. doi: 10.1186/s12889-020-10145-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Saeed D.K., Farooqi J., Shakoor S., Hasan R. Antimicrobial resistance among GLASS priority pathogens from Pakistan: 2006–2018. BMC Infect. Dis. 2021;21:1231. doi: 10.1186/s12879-021-06795-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Llor C., Bjerrum L. Antimicrobial resistance: Risk associated with antibiotic overuse and initiatives to reduce the problem. Ther. Adv. Drug Saf. 2014;5:229–241. doi: 10.1177/2042098614554919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sunny T., Jacob R., Krishnakumar K., Varghese S. Self-medication: Is a serious challenge to control antibiotic resistance? Natl. J. Physiol. Pharm. Pharmacol. 2019;9:821–827. doi: 10.5455/njppp.2019.9.0620508062019. [DOI] [Google Scholar]
- 121.Parrish A.G., Blockman M., Cohen K., Dawood H., De Waal R., Gray A.L., Kredo T., Leong T.D., Nel J., Rees H., et al. Meta-analytic magic, ivermectin, and socially responsible reporting. S. Afr. Med. J. 2021;111:934–937. doi: 10.7196/SAMJ.2021.v111i10.16021. [DOI] [PubMed] [Google Scholar]
- 122.Garegnani L.I., Madrid E., Meza N. Misleading clinical evidence and systematic reviews on ivermectin for COVID-19. BMJ Evid. Based Med. 2021;23:156–158. doi: 10.1136/bmjebm-2021-111678. [DOI] [PubMed] [Google Scholar]
- 123.Deng J., Zhou F., Ali S., Heybati K., Hou W., Huang E., Wong C.Y. Efficacy and safety of ivermectin for the treatment of COVID-19: A systematic review and meta-analysis. QJM. 2021;114:721–732. doi: 10.1093/qjmed/hcab247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.WHO The WHO AWaRe (Access, Watch, Reserve) Antibiotic Book. 2022. [(accessed on 20 February 2023)]. Available online: https://www.who.int/publications/i/item/9789240062382.
- 125.Mustafa Z.U., Nazir M., Majeed H.K., Salman M., Hayat K., Khan A.H., Myer J.C., Godman B. Exploring Knowledge of Antibiotic Use, Resistance, and Stewardship Programs among Pharmacy Technicians Serving in Ambulatory Care Settings in Pakistan and the Implications. Antibiotics. 2022;11:921. doi: 10.3390/antibiotics11070921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hayat K., Fatima N., Umer M.F., Khan F.U., Khan F.U., Najeeb Z.U.R., Ghaffari M.A., Raza S.O., Liu W., Chen C., et al. Understanding of Future Prescribers About Antimicrobial Resistance and Their Preparedness Towards Antimicrobial Stewardship Activities in Pakistan: Findings and Implications. Front. Pharmacol. 2022;13:771083. doi: 10.3389/fphar.2022.771083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lubwama M., Onyuka J., Ayazika K.T., Ssetaba L.J., Siboko J., Daniel O., Mushi M.F. Knowledge, attitudes, and perceptions about antibiotic use and antimicrobial resistance among final year undergraduate medical and pharmacy students at three universities in East Africa. PLoS ONE. 2021;16:e0251301. doi: 10.1371/journal.pone.0251301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Augie B.M., van Zyl R.L., McInerney P.A., Miot J. Knowledge and perceptions about antibiotic resistance and prudent antibiotic prescribing among final year medical students in two African countries. Int. J. Pharm. Pract. 2021;29:508–514. doi: 10.1093/ijpp/riab044. [DOI] [PubMed] [Google Scholar]
- 129.Nogueira-Uzal N., Zapata-Cachafeiro M., Vázquez-Cancela O., López-Durán A., Herdeiro M.T., Figueiras A. Does the problem begin at the beginning? Medical students’ knowledge and beliefs regarding antibiotics and resistance: A systematic review. Antimicrob. Resist. Infect. Control. 2020;9:172. doi: 10.1186/s13756-020-00837-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhao A., Xiao S., Kandelaki K., Liu Y., Chen W., Ren R., Liu H., Wang Y. Knowledge, Perception, and Educational Status of Antimicrobial Resistance Among Chinese Medical Students. Microb. Drug Resist. 2019;25:1458–1464. doi: 10.1089/mdr.2018.0411. [DOI] [PubMed] [Google Scholar]
- 131.Hoxha I., Malaj A., Kraja B., Bino S., Oluka M., Marković-Peković V., Godman B. Are pharmacists’ good knowledge and awareness on antibiotics taken for granted? The situation in Albania and future implications across countries. J. Glob. Antimicrob. Resist. 2018;13:240–245. doi: 10.1016/j.jgar.2018.01.019. [DOI] [PubMed] [Google Scholar]
- 132.Kalungia A.C., Mwambula H., Munkombwe D., Marshall S., Schellack N., May C., Jones A.S.C., Godman B. Antimicrobial stewardship knowledge and perception among physicians and pharmacists at leading tertiary teaching hospitals in Zambia: Implications for future policy and practice. J. Chemother. 2019;31:378–387. doi: 10.1080/1120009X.2019.1622293. [DOI] [PubMed] [Google Scholar]
- 133.Mustafa Z.U.M.M., Shahid A., Salman M., Hayat K., Yasmin K., Baraka M.A., Mathew S., Kanwal M., Parveen S., Jamal I., et al. Nurses’ Perceptions, Involvement, Confidence and Perceived Barriers Towards Antimicrobial Stewardship Program in Pakistan: Findings from a Multi-Center, Cross-Sectional Study. J. Multidiscip. Healthc. 2022;15:2553–2562. doi: 10.2147/JMDH.S376664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Godman B., Egwuenu A., Wesangula E., Schellack N., Kalungia A.C., Tiroyakgosi C., Kgatlwane J., Mwita J.C., Patrick O., Niba L.L., et al. Tackling antimicrobial resistance across sub-Saharan Africa: Current challenges and implications for the future. Expert Opin. Drug Saf. 2022;21:1089–1111. doi: 10.1080/14740338.2022.2106368. [DOI] [PubMed] [Google Scholar]
- 135.Mukokinya M.M.A., Opanga S., Oluka M., Godman B. Dispensing of Antimicrobials in Kenya: A Cross-sectional Pilot Study and Its Implications. J. Res. Pharm. Pract. 2018;7:77–82. doi: 10.4103/jrpp.JRPP_17_88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Opanga S., Rizvi N., Wamaitha A., Abebrese Sefah I., Godman B.B. Availability of Medicines in Community Pharmacy to Manage Patients with COVID-19 in Kenya; Pilot Study and Implications. Sch. Acad. J. Pharm. 2021;3:36–42. doi: 10.36347/sajp.2021.v10i03.001. [DOI] [Google Scholar]
- 137.Sakeena M.H.F., Bennett A.A., McLachlan A.J. Enhancing pharmacists’ role in developing countries to overcome the challenge of antimicrobial resistance: A narrative review. Antimicrob. Resist. Infect. Control. 2018;7:63. doi: 10.1186/s13756-018-0351-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Mustafa Z.U., Tariq S., Iftikhar Z., Meyer J.C., Salman M., Mallhi T.H., Khan Y.H., Godman B., Seaton R.A. Predictors and Outcomes of Healthcare-Associated Infections among Patients with COVID-19 Admitted to Intensive Care Units in Punjab, Pakistan; Findings and Implications. Antibiotics. 2022;11:1806. doi: 10.3390/antibiotics11121806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Tobin E., Erhazele J., Okonofua M., Nnadi C., Nmema E., George O. Self-medication among health care workers in a tertiary hospital in Southern Nigeria: Knowledge, attitude, and practices. Med. J. Indones. 2020;29:403–409. doi: 10.13181/mji.oa.204223. [DOI] [Google Scholar]
- 140.Guma S.P., Godman B., Campbell S.M., Mahomed O. Determinants of the Empiric Use of Antibiotics by General practitioners in South Africa: Observational, Analytic, Cross-Sectional Study. Antibiotics. 2022;11:1423. doi: 10.3390/antibiotics11101423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Makwela A.B., Grootboom W.M., Abraham V., Witika B., Godman B., Skosana P.P. Antimicrobial Management of Skin and Soft Tissue Infections among Surgical Wards in South Africa: Findings and Implications. Antibiotics. 2023;12:275. doi: 10.3390/antibiotics12020275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Etando A., Amu A.A., Haque M., Schellack N., Kurdi A., Alrasheedy A.A., Timoney A., Mwita J.C., Rwegerera G.M., Tatrick O., et al. Challenges and Innovations Brought about by the COVID-19 Pandemic Regarding Medical and Pharmacy Education Especially in Africa and Implications for the Future. Healthcare. 2021;9:1722. doi: 10.3390/healthcare9121722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kandasamy G., Sivanandy P., Almaghaslah D., Khobrani M., Chinnadhurai M., Vasudevan R., Almeleebia T. Knowledge, attitude, perception and practice of antibiotics usage among the pharmacy students. Int. J. Clin. Pract. 2020;74:e13599. doi: 10.1111/ijcp.13599. [DOI] [PubMed] [Google Scholar]
- 144.Olaoye O., Tuck C., Khor W.P., McMenamin R., Hudson L., Northall M., Panford-Quainoo E., Asima D.M., Ashiru-Oredope D. Improving Access to Antimicrobial Prescribing Guidelines in 4 African Countries: Development and Pilot Implementation of an App and Cross-Sectional Assessment of Attitudes and Behaviour Survey of Healthcare Workers and Patients. Antibiotics. 2020;9:555. doi: 10.3390/antibiotics9090555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Gupta M.K., Vohra C., Raghav P. Assessment of knowledge, attitudes, and practices about antibiotic resistance among medical students in India. J. Fam. Med. Prim. Care. 2019;8:2864–2869. doi: 10.4103/jfmpc.jfmpc_504_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Manivannan E., Karthikeyan C., Moorthy N., Chaturvedi S.C. The Rise and Fall of Chloroquine/Hydroxychloroquine as Compassionate Therapy of COVID-19. Front. Pharmacol. 2021;12:584940. doi: 10.3389/fphar.2021.584940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Sharland M., Zanichelli V., Ombajo L.A., Bazira J., Cappello B., Chitatanga R., Chuki P., Gandra S., Getahun H., Harbarth S., et al. The WHO essential medicines list AWaRe book: From a list to a quality improvement system. Clin. Microbiol. Infect. 2022;28:1533–1535. doi: 10.1016/j.cmi.2022.08.009. [DOI] [PubMed] [Google Scholar]
- 148.WHO Anatomical Therapeutic Chemical (ATC) Classification. 2021. [(accessed on 2 December 2022)]. Available online: https://www.who.int/tools/atc-ddd-toolkit/atc-classification.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Further data are available upon reasonable request from the co-authors.