Abstract
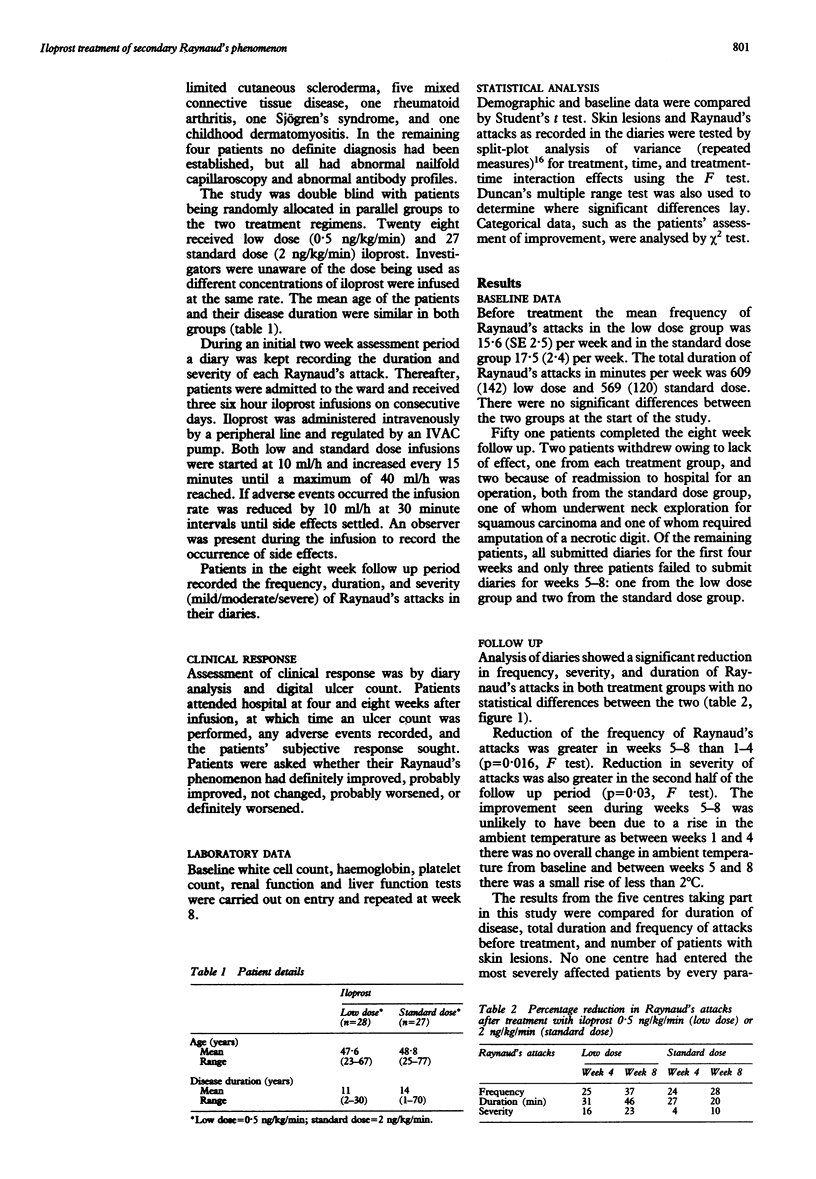
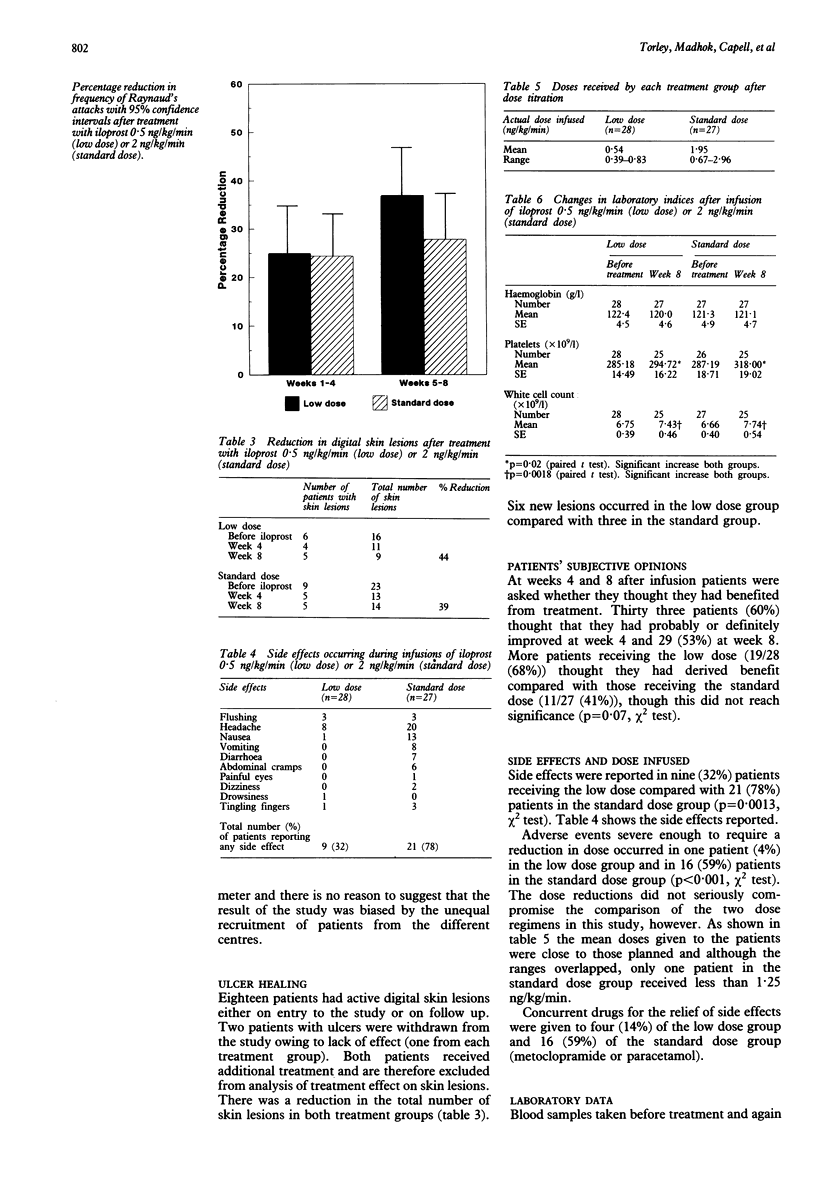
OBJECTIVE--To compare low (0.5 ng/kg/min) and standard dose (2 ng/kg/min) iloprost (a stable carbacyclin analogue of prostacyclin) in patients with Raynaud's phenomenon secondary to connective tissue disorders. DESIGN--Double blind, random allocation, three six hour infusions on consecutive days. Follow up period eight weeks. SETTING--Rheumatology units, five teaching hospitals. PATIENTS--55 Patients with Raynaud's phenomenon (greater than seven attacks per week), 32 secondary to well documented classical progressive systemic sclerosis (American Rheumatism Association criteria), 11 CREST syndrome, 5 mixed connective tissue disease, 1 rheumatoid arthritis, 1 Sjögren's syndrome, 1 childhood dermatomyositis, and 4 abnormal nailfold capillaroscopy and antibody profiles but no definite diagnosis. INTERVENTIONS--All other treatment for Raynaud's phenomenon was discontinued two weeks before entry. 28 Patients were randomly allocated to receive the low dose, 27 the standard dose. Differing dilutions allowed infusion rates to be started at 10 ml/h with increments of 10 ml/h every 15 minutes until infusion rates reached 0.5 ng/kg/min and 2 ng/kg/min respectively. MAIN OUTCOME MEASURE(s)--Reduction in frequency, duration, and severity of attacks of Raynaud's phenomenon. Assessment of ulcer and ischaemic lesion healing. RESULTS--Both dosage regimens were equally effective in reducing severity, frequency, and duration of Raynaud's attacks. Ulcer healing occurred to similar degree in both treatment groups (standard dose 44%, low dose 39%). Low dose was associated with significantly fewer side effects. CONCLUSIONS--Both dosage regimens reduce severity of Raynaud's phenomenon and encourage ulcer healing. Low dose was associated with fewer side effects and was better tolerated by the patients.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Belch J. J., Drury J., McLaughlin K., O'Dowd A., Anderson J., Sturrock R. D., Forbes C. D. Abnormal biochemical and cellular parameters in the blood of patients with Raynauds phenomenon. Scott Med J. 1987 Feb;32(1):12–14. doi: 10.1177/003693308703200106. [DOI] [PubMed] [Google Scholar]
- Belch J. J., Madhok R., Shaw B., Leiberman P., Sturrock R. D., Forbes C. D. Double-blind trial of CL115,347, a transdermally absorbed prostaglandin E2 analogue, in treatment of Raynaud's phenomenon. Lancet. 1985 May 25;1(8439):1180–1183. doi: 10.1016/s0140-6736(85)92862-4. [DOI] [PubMed] [Google Scholar]
- Belch J. J., McLaren M., Anderson J., Lowe G. D., Sturrock R. D., Capell H. A., Forbes C. D. Increased prostacyclin metabolites and decreased red cell deformability in patients with systemic sclerosis and Raynauds syndrome. Prostaglandins Leukot Med. 1985 Jan;17(1):1–9. doi: 10.1016/0262-1746(85)90029-0. [DOI] [PubMed] [Google Scholar]
- Belch J. J., Newman P., Drury J. K., Capell H., Leiberman P., James W. B., Forbes C. D., Prentice C. R. Successful treatment of Raynaud's Syndrome with prostacyclin. Thromb Haemost. 1981 Jun 30;45(3):255–256. [PubMed] [Google Scholar]
- Belch J. J., Newman P., Drury J. K., McKenzie F., Capell H., Leiberman P., Forbes C. D., Prentice C. R. Intermittent epoprostenol (prostacyclin) infusion in patients with Raynaud's syndrome. A double-blind controlled trial. Lancet. 1983 Feb 12;1(8320):313–315. doi: 10.1016/s0140-6736(83)91624-0. [DOI] [PubMed] [Google Scholar]
- Bertelé V., Mussoni L., del Rosso G., Pintucci G., Carriero M. R., Merati M. G., Libretti A., de Gaetano G. Defective fibrinolytic response in atherosclerotic patients--effect of iloprost and its possible mechanism of action. Thromb Haemost. 1988 Oct 31;60(2):141–144. [PubMed] [Google Scholar]
- Boxer L. A., Allen J. M., Schmidt M., Yoder M., Baehner R. L. Inhibition of polymorphonuclear leukocyte adherence by prostacyclin. J Lab Clin Med. 1980 May;95(5):672–678. [PubMed] [Google Scholar]
- Dowd P. M., Martin M. F., Cooke E. D., Bowcock S. A., Jones R., Dieppe P. A., Kirby J. D. Treatment of Raynaud's phenomenon by intravenous infusion of prostacyclin (PGI2). Br J Dermatol. 1982 Jan;106(1):81–89. doi: 10.1111/j.1365-2133.1982.tb00905.x. [DOI] [PubMed] [Google Scholar]
- Evans S. J. Uses and abuses of analysis of variance. Br J Clin Pharmacol. 1983 Jun;15(6):629–648. doi: 10.1111/j.1365-2125.1983.tb01544.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher C. A., Kappa J. R., Sinha A. K., Cottrell E. D., Reiser H. J., Addonizio V. P. Comparison of equimolar concentrations of iloprost, prostacyclin, and prostaglandin E1 on human platelet function. J Lab Clin Med. 1987 Feb;109(2):184–190. [PubMed] [Google Scholar]
- Jarrett P. E., Morland M., Browse N. L. Treatment of Raynaud's phenomenon by fibrinolytic enhancement. Br Med J. 1978 Aug 19;2(6136):523–525. doi: 10.1136/bmj.2.6136.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahan A., Weber S., Amor B., Saporta L., Hodara M., Degeorges M. Nifedipine and Raynaud's phenomenon. Ann Intern Med. 1981 Apr;94(4 Pt 1):546–546. doi: 10.7326/0003-4819-94-4-546_1. [DOI] [PubMed] [Google Scholar]
- Kyle V., Parr G., Salisbury R., Thomas P. P., Hazleman B. Prostaglandin E1 vasospastic disease and thermography. Ann Rheum Dis. 1985 Feb;44(2):73–78. doi: 10.1136/ard.44.2.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh N. J., Csuka M., Watson H., Belcher G., Amadi A., Ring E. F., Black C. M., Maddison P. J. Infusion of iloprost, a prostacyclin analogue, for treatment of Raynaud's phenomenon in systemic sclerosis. Ann Rheum Dis. 1988 Jan;47(1):43–47. doi: 10.1136/ard.47.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musiał J., Wilczyńska M., Sładek K., Cierniewski C. S., Nizankowski R., Szczeklik A. Fibrinolytic activity of prostacyclin and iloprost in patients with peripheral arterial disease. Prostaglandins. 1986 Jan;31(1):61–70. doi: 10.1016/0090-6980(86)90225-x. [DOI] [PubMed] [Google Scholar]
- Preliminary criteria for the classification of systemic sclerosis (scleroderma). Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum. 1980 May;23(5):581–590. doi: 10.1002/art.1780230510. [DOI] [PubMed] [Google Scholar]
- Rademaker M., Cooke E. D., Almond N. E., Beacham J. A., Smith R. E., Mant T. G., Kirby J. D. Comparison of intravenous infusions of iloprost and oral nifedipine in treatment of Raynaud's phenomenon in patients with systemic sclerosis: a double blind randomised study. BMJ. 1989 Mar 4;298(6673):561–564. doi: 10.1136/bmj.298.6673.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rademaker M., Thomas R. H., Provost G., Beacham J. A., Cooke E. D., Kirby J. D. Prolonged increase in digital blood flow following iloprost infusion in patients with systemic sclerosis. Postgrad Med J. 1987 Aug;63(742):617–620. doi: 10.1136/pgmj.63.742.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seibold J. R., Jageneau A. H. Treatment of Raynaud's phenomenon with ketanserin, a selective antagonist of the serotonin2 (5-HT2) receptor. Arthritis Rheum. 1984 Feb;27(2):139–146. doi: 10.1002/art.1780270204. [DOI] [PubMed] [Google Scholar]
- Smith C. D., McKendry R. J. Controlled trial of nifedipine in the treatment of Raynaud's phenomenon. Lancet. 1982 Dec 11;2(8311):1299–1301. doi: 10.1016/s0140-6736(82)91508-2. [DOI] [PubMed] [Google Scholar]
- Steen V. D., Ziegler G. L., Rodnan G. P., Medsger T. A., Jr Clinical and laboratory associations of anticentromere antibody in patients with progressive systemic sclerosis. Arthritis Rheum. 1984 Feb;27(2):125–131. doi: 10.1002/art.1780270202. [DOI] [PubMed] [Google Scholar]
- Yardumian D. A., Isenberg D. A., Rustin M., Belcher G., Snaith M. L., Dowd P. M., Machin S. J. Successful treatment of Raynaud's syndrome with Iloprost, a chemically stable prostacyclin analogue. Br J Rheumatol. 1988 Jun;27(3):220–226. doi: 10.1093/rheumatology/27.3.220. [DOI] [PubMed] [Google Scholar]


