Abstract
For almost nearly a century, memory functions have been attributed only to acquired immune cells. Lately, this paradigm has been challenged by an increasing number of studies revealing that innate immune cells are capable of exhibiting memory-like features resulting in increased responsiveness to subsequent challenges, a process known as trained immunity (known also as innate memory). In contrast, the refractory state of endotoxin tolerance has been defined as an immunosuppressive state of myeloid cells portrayed by a significant reduction in the inflammatory capacity. Both training as well tolerance as adaptive features are reported to be accompanied by epigenetic and metabolic alterations occurring in cells. While training conveys proper protection against secondary infections, the induction of endotoxin tolerance promotes repairing mechanisms in the cells. Consequently, the inappropriate induction of these adaptive cues may trigger maladaptive effects, promoting an increased susceptibility to secondary infections—tolerance, or contribute to the progression of the inflammatory disorder—trained immunity. This review aims at the discussion of these opposing manners of innate immune and non-immune cells, describing the molecular, metabolic and epigenetic mechanisms involved and interpreting the clinical implications in various inflammatory pathologies.
Keywords: trained immunity, tolerance, inflammatory, dose, PAMPs, DAMPs, epigenetic, metabolic, signaling, diseases
1. Introduction
In the early 20th century, the Nobel laureate Paul Ehrlich, in a spectacular lecture, introduced the concept of specific antigen–antibody interaction, which established the fundamental basis of the adaptive arm of immune responses. Later, several reports clarified major questions related to adaptive (acquired) immunity, which relies mainly on two different types of lymphocytes, T and B cells, able to recognize pathogen-specific antigens and develop immunologic memory against them whilst promoting the long-term specific elimination of the pathogen after a subsequent encounter [1,2].
Different from the acquired immune system, innate immune cells were considered as evolutionary archaic due to the lack of memory responses, characterized particularly by a rapid cell recruitment to the site of infection, producing various inflammatory mediators (i.e., cytokines and chemokines), and by engulfing the pathogen, thus eliminating the infectious invader [3,4]. The overall impression that immunological memory was an exclusive hallmark of the adaptive immune response was challenged by several studies in plants and invertebrates, indicating a greater protection against reinfection [5,6,7]. Interestingly, since the last universal common ancestor of all cells (LUCA) evolved into diverse phylogenic groups where the majority (>95%) of the living organisms relies on the protection responses driven mainly by the innate immune system, the acquisition of adaptive-like immune memory for innate immune cells may be considered as an evolutionary success [7,8,9,10]. Initial observations about memory effects arising from the innate immune system were reported in 1934 by a Swedish scientist Naeslund, then followed by a report of Mackaness (in 1968) and later from Garly et al. (in 2003), showing that mammals vaccinated by Bacillus Calmette–Guerin (BCG) improved survival rates with effects exceeding the burden of tuberculosis, affording appropriate non-specific protection against various infectious diseases [11,12,13,14]. Similar findings about the non-specific protective effects of BCG as well as measles were reported by other groups [15,16,17,18,19].
Netea and colleagues, in a seminal report in 2011, suggested the concept of trained immunity, defining it as a non-specific property of innate immune cells as well as tissue-resident stem cells to act against secondary infectious challenges [20,21]. Trained immunity, known also as innate memory or trained innate memory (abbr. TRIM), describes a long-term functional reprogramming evoked by various endogenous danger signals (damage-associated molecular patterns, DAMPs) released upon cellular stress or tissue injury, or exogenous pathogenic conserved molecules (pathogen-associated molecular patterns, PAMPs) [21,22,23,24]. Notably, recent studies have demonstrated also the capability of hormones to support the induction of trained immunity, especially by sex-related (i.e., β-estradiol) hormones or aldosterone as a mineralocorticoid that regulates electrolyte homeostasis and affects many cardiovascular inflammatory events [25,26].
Trained cells adopt a prolonged activated phenotype characterized by enhanced levels of pro-inflammatory mediators ( such as IL-1β, TNF-α, IL-6 and reactive oxygen species (ROS)) and increased antimicrobial and antitumoral activities, a process regulated mainly by epigenetic changes with resulting changes in metabolism and their functional reprogramming [27,28]. In contrast to trained immunity, endotoxin tolerance (ET) as an opposing feature is well known and represents a transient unresponsive state of immune cells against further challenges characterized by decreased pro-inflammatory signatures and an increased anti-inflammatory mode [29,30]. Chromatin modifications and gene reprogramming supported by metabolic changes have been demonstrated as crucial developments supporting ET [30,31,32,33,34,35,36,37]. Innate immune cells sense different PAMPs and DAMPs by germline-encoded pattern recognition receptors (PRRs), resulting in downstream signaling events culminating in the release of various inflammatory mediators [38,39,40]. To date, training as well as tolerance reactions are mainly imposed by alterations occurring in different classes of PRRs, such as Toll-like receptors (TLRs), nucleotide oligomerization domain (NOD)-like receptors (NLRs), retinoic acid-inducible gene-I (RIG-I)-like receptors (RLRs) and C-type lectin receptors (CLRs) instructing local and systemic inflammatory responses in the living organisms [40,41,42,43]. Altogether, the activation of these signaling pathways contributes to the evolvement of inflammatory diseases. To date, an increasing number of studies has shown the clinical importance of trained immunity as well as tolerance implicated in numerous inflammatory diseases [21,23,44,45,46,47,48].
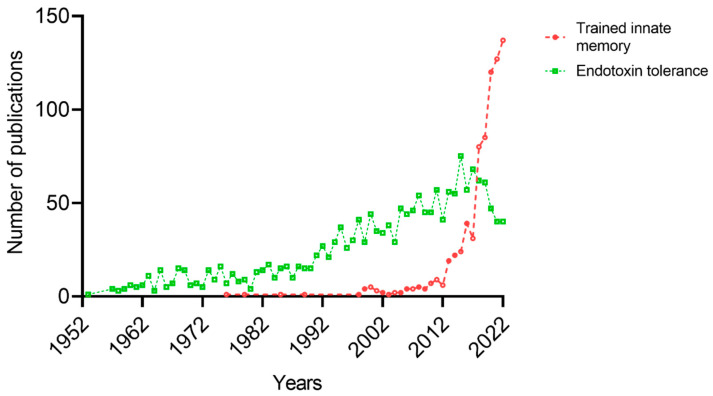
Trained innate immunity as well as the topic of endotoxin tolerance have gained considerable interest through the years (Figure 1). In the present review, we discuss in depth the different characteristic properties of trained immunity and endotoxin tolerance and their role in various inflammatory diseases.
Figure 1.
Number of publications related to trained innate memory and endotoxin tolerance as adaptive manners (PubMed, January 2023).
2. Trained Immunity
Trained immunity represents a functional state of the innate immune cells and tissue-resident stem cells adjusting their response to subsequent insults, characterized particularly by a prolonged activation after a resting period, orchestrated mainly by epigenetic reprogramming and the metabolic rewiring of cells [24]. It describes a property of innate immune system to mount memory-like responses against past microbial and non-microbial challenges [20,21,24]. To date, studies have shown that trained immunity can be maintained in innate immune cells for months up to decades, a process occurring in the bone marrow progenitor cells–central trained immunity, or for days up to a week in circulating innate immune cells–peripheral training [21,49,50,51,52].
Emerging investigations have revealed two distinct hypotheses about the induction of trained immunity and tolerance in innate immune cells: first, the stressor-dependent hypothesis, where priming by specific PAMPs/DAMPs (i.e., β-glucan, BCG, oxidized low-density lipoprotein (oxLDL) and heme) triggers the induction of training, whereas the Gram-negative endotoxin (i.e., lipopolysaccharide (LPS)) promotes only tolerant reactions; and the dose-dependent hypothesis, which demonstrates a biphasic dose–response where low-dose priming results in a trained phenotype, whereas high-dose exposure triggers an immune-suppressive phenotype (tolerance) after a secondary insult [20,21,53,54]. Moreover, other reports elaborated also the role of corticosteroid hormones, dietary restriction and maturation state supporting the induction of these adaptive cues in innate immune cells.
2.1. Stressor-Dependent Induction of Trained Innate Memory
Innate immune cells as gatekeepers recognize various pathogens, mounting immediate immune resistance reactions aimed at eliminating the microbial intruder [53]. In the early 20th century, Shwartzman described long-term adaptation reactions occurring by continuous intravenous injections of the same filtrate promoting hemorrhagic necrosis at the site of injection in the skin [55]. This phenomenon, where cells sense the initial injection supporting resistance mechanisms against a secondary challenge, is known as Shwartzman reaction.
Later, Netea and colleagues proposed the concept of stressor-dependent induction of trained immunity in innate immune system [20]. They principally showed that the pre-exposure of monocytes to the fungal-cell-wall-constituent β-glucan (C. albicans) triggers an exaggerated burst of inflammatory responses upon secondary infectious stimuli (i.e., LPS), a process called trained immunity [56,57]. Further in vitro and in vivo studies demonstrated comparable effects when innate immune cells (monocytes, macrophages, microglia, neutrophils, mast cells and dendritic cells) as well as hematopoietic stem cells, primed by β-glucan or Candida albicans infections, promote protective reactions against various infections (such as Mycobacterium tuberculosis, Leishmania braziliensis and influenza) or support anti-tumoral effects in a ROS- or CCR2-dependent manner [52,58,59,60,61,62,63,64]. C. albicans as well as β-glucan induce a functional reprogramming of innate immune cells, resulting in enhanced release of pro-inflammatory mediators (i.e., IL-1β, TNF-α, IL-6, IL-32 and ROS) mediated by an IL-1-dependent signaling [58,59,62]. Similarly, LPS guides the induction of training or tolerance depending on the type of secondary stimulus [65].
Extensive studies from different research groups have led to the identification of other inducers of trained immunity. Muramyl dipeptide (MDPs) and tripeptide (MTPs), as bacterial wall peptidoglycans recognized by NOD2 receptors, were reported to induce trained immunity and inhibit cancer growth by sensitizing melanoma cells to inhibitory checkpoint therapy [66,67]. Likewise, Pseudomonas aeruginosa serves as an important pathogen-associated microbial component, causing acute and chronic lung infections [68,69]. Bigot et al., in a proof-of-concept study, demonstrated the ability of human respiratory epithelial cells to memorize former exposures to P. aeruginosa and provide protective reactions against a wide spectrum of pathogens, a process relying on epigenetic regulation [70]. Similarly, in another investigation, where mice were trained by a wide range of infections such as S. aureus, L. monocytogenes, E. coli, C. rodentium and P. aeruginosa to mimic systemic infections, peritonitis, enteritis and pneumonia, the ability of mice to exhibit wide-range protective effects from heterologous infections at distant anatomic sites from the training site, particularly regulated by IL-1 pathway, was revealed [71,72]. The data presented by these studies may be of crucial importance since they provide a double-edge property of trained immunity: first, providing antimicrobial responses against heterologous infections, and second, serving as a therapeutic tool to control inflammatory exacerbations during multi-microbial infections. However, these findings should be considered with caution since P. aeruginosa, during pulmonary infections, might utilize the host defense system to its advantage by redirecting the host metabolism toward itaconate production, promoting biofilm formation resulting in human tissue colonization [73]. Extensive studies are required to further determine all the detrimental factors (i.e., epigenetic regulation, metabolic rewiring and former exposures) that can promote trained immunity and further elucidate the clinical relevance.
To date, it is well-known that BCG vaccination is associated with decreased mortality rates, driven mainly by its non-specific protective actions against other infections in addition to the targeted pathogens [14,74,75,76]. Furthermore, it has been hypothesized that these non-specific protective effects of certain vaccines, such as BCG, measles and polio, are driven by the innate immune system. Kleinnijenhuis and colleagues provided firm evidence that BCG promotes the non-specific long-term boosting of innate immune system, trained immunity, mediated by a NOD2-dependent regulation of epigenetic marks such as histone H3 at lysine 4 (H3K4) trimethylation [77,78]. γδ T cells, as a unique T-cell subpopulation featuring functions of both immune systems, innate and adaptive, not restricted to the major histocompatibility complex (MHC) of signaling, represent a key role for the innate immune system of responses to various microbial infections [79,80]. A growing body of evidence demonstrated that γδ T cells are early responders sensing different viruses by their PRRs, natural killer type receptors (NKRs) or via T-cell receptors (TCRs) exerting their protective function by a rapid and effective resolution of the viral infection [80,81,82,83,84,85]. In a recent work, Röring et al., elaborated on the role of the measles, mumps and rubella (MMR) vaccine, affording a broader protection against heterologous infections, and found that MMR triggers profound long-term functional changes (trained immunity) in γδ T cells characterized by increased levels of TNF-α and IFN-γ as well as an enhanced reliance on mitochondrial metabolism [86]. Moreover, several studies have reported the analogous contribution of BCG vaccination to γδ T cells expressing a typical heterologous effect observed in trained immunity [87,88,89,90].
In a recent report, Debisarun et al., demonstrated that the quadrivalent inactivated influenza vaccine triggers the transcriptional reprogramming of innate immune cells, training effects, resulting in fine-tuned anti-SARS-CoV-2 responses supporting enhanced protective reactions against COVID-19 [91]. Moreover, a study indicates that a single dose of the ChAdOx1 nCoV-19 vaccine (AZD1222), which uses an adenoviral vector, displayed a prolonged effective protection by myeloid cells characterized by heightened levels of pro- and anti-inflammatory cytokines (i.e., IL-1β, IL-6, CXCL1 and IL-10) in response to subsequent unrelated stimuli, featuring innate memory cues [92]. Other attempts included the investigation of viral components promoting innate memory. Comparable effects have been shown also by murine infections with cytomegalovirus (CMV) displaying a T/B-cell-independent and natural killer cell (NK)-dependent protective mechanism against re-infections [93,94]. In addition, earlier studies related to NK cells revealed a unique property of this type of cells expressing memory-like features driven by previous encounters to CMV infection or mediated by a cocktail of inflammatory cytokines (IL-12, IL-15 and IL-18) [95,96,97,98]. Both, murine and human CMV promoted the antigen-specific induction of memory NKs [93,98,99,100]. Nevertheless, cytokine-mediated memory NKs expressed non-specific adaptive manners with enhanced proliferative capacity, elevated interferon-γ (IFN-γ) and prolonged persistence [98,101,102,103]. Because of these adaptive cues, NK cells can be considered as an evolutionary bridge between acquired and innate immune system.
Different ventures of existing vaccines or viral components to induce trained immunity seek to improve conventional vaccines toward the new formulations of the so-called trained immunity-based vaccines (TIbV), aimed at stimulating broader responses beyond their specific antigens, an approach that could make it possible to afford proper resistance against viral outbreaks [104,105,106,107]. However, this might not be the case for allergen vaccines. In a recent study Benito-Villalvilla et al., it was demonstrated that allergoid–mannan conjugates, which serve as next-generation vaccines for allergen-specific immunotherapy (AIT), contribute to allergen tolerance by the differentiation of monocytes into tolerogenic dendritic cells (DCs), but lack the capacity to induce any trained immunity effects [107,108]. Similarly, the innate counterparts of T cells—innate lymphoid cells (ILCs)—primed by IL-33 or allergic inflammation mount enduring memory-like responses against other allergens, which can serve as double-edged sword, on the one side affording proper protection against infectious diseases and, on the other side, by contributing to pathology or disease progression [109,110,111]. Altogether, these data indicate that further research is necessary to clarify the role of different vaccines, allergens or cytokines promoting training or tolerant reactions.
The multifold interplay between microbiota and the immune system during homeostasis or diseases represents a crucial factor orchestrating continuously the development of host’s immune responses whilst maintaining its microbiota composition [54,112,113]. The probiotic gut commensal Limosilactobacillus reuteri recalls enhanced responses with mixed secondary responses in human monocyte-derived DCs upon subsequent exposure, accompanied with enriched histone modifications and portrayed particularly by an increased IL-1β and IL-6 phenotype, but diminished TNF-α, IL-23 and IL-27 [114]. However, blood DCs primed by L. reuteri exclusively resembled a tolerant phenotype upon a second challenge. Furthermore, our group demonstrated that gut microbiota cell-derived nano-sized biovesicles, known as extracellular vesicles (EVs), drive the induction of innate memory in murine bone-marrow neutrophils in a TLR2-dependent manner in vitro [115]. Similarly, the role of extracellular vesicles from HIV-infected humans maintaining persistent chronic inflammatory responses (phenomenon of trained immunity) of myeloid cells, associated with increased morbidities against secondary infections, has been described by Dubrovsky et al. [116]. Although there are still many issues to be clarified, these studies nonetheless shed some encouraging light to the role of microbiota or bilipid-enclosed envelopes, such as EVs, encouraging trained effects in innate immune cells.
In addition to the aforementioned PAMPs, DAMPs, such as oxLDL, heme, urate, vimentin and high-mobility group box 1 (HMGB1), recognized mainly by TLR4, can be targeted for trained immunity modulation [24,117,118]. Pre-exposure to specific DAMPs as non-microbial triggers can induce the functional reprogramming of innate immune cells triggering an altered immune response toward a subsequent challenge [117]. DAMPs released during tissue injury from cell death or after organ transplantation allow innate immune cells to elicit long-term epigenetic changes at the promoters of inflammatory genes and cause metabolic rewiring [24,119]. Vimentin and HMGB1 represent inflammatory mediators upregulated during organ transplantation, responsible for acute and chronic transplant rejection [120,121]. A study by Braza et al., demonstrated that vimentin and HMGB1 drive the trained immunity-associated cytokine production of infiltrating macrophages during allograft rejection [23]. Moreover, a large number of infiltrating innate immune cells, especially macrophages and neutrophils during transplant rejection, present a significantly higher phagocytic activity if exposed to HMGB1 [122,123,124]. Another well-described consequence of oxidative stress, oxLDL, is associated with an increased probability of graft rejection [125,126,127,128]. Patients with chronic kidney disease (CKD) display higher serum levels of oxLDL, characterized by an hyperinflammatory phenotype of monocytes accompanied by an increased production of pro-inflammatory cytokines (i.e., TNF-α, IL-1β and IL-6) [128,129,130,131]. Priming by oxLDL, upon secondary exposure to TLR2 and TLR4 agonists, resulted in a training phenotype of macrophages characterized by increased production of inflammatory cytokines, monocyte chemoattractant protein 1 (MCP-1) and matrix metalloproteinase 2 (MMP2) and 9 (MMP9) [117,132]. Likewise, human non-immune cells from the vascular wall primed by oxLDL exhibit pro-inflammatory features regulated presumably by trained immunity effects [133]. Although it is well-known that oxLDL induces trained immunity in myeloid cells by shifting the metabolism toward glycolysis, there are still no data about the role of training in CKD or dialysis patients [24].
Hyperuricemia represents one of the main factors linked to gouty arthritis, caused by elevated levels of uric acid (urate) [134,135,136]. Existing evidence demonstrated that urate induces transcriptional and epigenetic modifications in circulating monocytes resulting in enhanced responsiveness marked by increased levels of IL-1β, indicating a crucial role of trained immunity [136,137,138]. Moreover, heme is another DAMP involved in multiple biological processes that regulate trained responses of innate immune cells by increasing the frequency of myeloid-biased multipotent progenitors, associated with increased monocyte and neutrophil infiltration in the murine peritoneum [139,140].
Mechanistically trained immunity is reported to be supported by different alterations occurring on the PRRs, driving the activation of the mechanistic target of rapamycin (mTOR) through phosphoinositide 3-kinases (PI3Ks) triggering downstream signaling events promoting the activation of nuclear factor-κB (NF-κB), resulting in the production of several inflammatory mediators [21,59,117,141]. Cheng et al., identified a canonical hypoxia sensing system required for the induction of memory-like responses in monocytes, where dectin-1-dependent activation of mTOR by β-glucan provokes increased expression of hypoxia-inducible factor 1α (HIF-1α) [142]. Ongoing studies showed that the downstream activation of intermediate proteins, such as protein kinase B (Akt), by PI3Ks, encouraged by TLR4 activation serves as crucial factor for the induction of innate memory in murine microglial cells [46,143]. Similarly, a recent work elaborated the role of trained immunity driving the pathological inflammation in a murine model of Duchenne muscular dystrophy (DMD), a genetic disease affecting more commonly males than females, revealing TLR4-dependent activation of bone-marrow-derived macrophages as the central cause for the DMD pathogenesis [144]. Furthermore, the activation of PRRs, notably dectin-1 by β-glucan or TLR4 by LPS, triggered the activation of mitogen-activated protein kinase (MAPK)-mediated pro-inflammatory pathway, exclusively extracellular signal-regulated kinase (ERK) 1/2, p38 and Jun N-terminal protein kinase (JNK) supporting the production of pro-inflammatory mediators [56,59,143]. Comparable mechanistic events have been shown also by neutrophils and macrophages primed by lipoteichoic acid (LTA) from the Gram-positive Staphylococcus aureus as a TLR2-activator [145,146,147,148].
Epigenetic reprogramming at the promoters of inflammatory genes with resulting changes in cell metabolism have been identified to orchestrate memory-like features in innate immune cells [21,24,28,149]. Epigenetic signatures triggering trained immunity are driven by histone modifications, such as histone methylation and acetylation, resulting in chromatin reconfiguration, rendering a more accessible form of chromatin facilitating the transcription of pro-inflammatory genes [28,117,150]. Current data determined the specific epigenetic hallmarks of trained immunity, including monomethylation or trimethylation of histone 3 lysine 4 (H3K4me1 or H3K4me3) at the promoters of stimulated genes, and the acetylation of histone 3 lysine 27 (H3K27ac) at distal enhancers [21,59,117,151]. MicroRNAs (miRNAs) as small non-coding regulatory RNAs are known epigenetic modulators that can alter the levels of target mRNAs, regulating also the induction of innate memory in innate immune cells [21,152]. Several studies identified miR-155, miR-146a-5p and miR-9-5p to be critical regulators of trained immunity supporting the hyperactivation of myeloid cells [153,154,155,156]. These may likely be a conjoint result of the decreased activity of phosphatases (i.e., SHIP1) by miRNAs [157]. A specific set of long non-coding RNAs (lncRNAs), known as immune gene-priming lncRNAs (IPLs), alters histone modifications, especially H3K4me3 on promoters of pro-inflammatory cytokines supporting trained immunity in macrophages [158]. Moreover, a study suggested that changes occurring in the DNA methylation pattern may discriminate between ‘responders’ and ‘non-responders’, identifying several genes that can be used as predictors of training effects [21,159].
The interplay of numerous intracellular metabolic pathways, such as glycolysis, oxidative phosphorylation (OXPHOS), accumulation of metabolites from the tricarboxylic acid cycle (TCA) and cholesterol biosynthesis, serve as fundamental immune-metabolic circuits endorsing the effects of trained immunity [160,161,162]. The activation of the dectin-1- mTOR- HIF-1α pathway resulted in a shift of metabolism toward aerobic glycolysis with increased glucose consumption, higher levels of L-lactate and elevated levels of its reduced form of nicotinamide adenine dinucleotide (NADH) [142]. The overall notion of glycolysis-induced trained immunity has been challenged by several reports, showing that oxLDL-, LPS-, β-glucan or BCG-trained macrophages adopt OXPHOS as an immunometabolic mechanism to express increased hyperresponsiveness [163,164,165,166]. The accumulation of intermediary metabolites of the TCA cycle, such as fumarate, as a result of glutamine replenishment (glutaminolysis), altogether with cholesterol synthesis contributes to the induction of innate immune memory in myeloid cells, downregulating the activity of KDM5 histone demethylases [167,168]. Moreover, mevalonate as an upstream metabolite of cholesterol synthesis triggers the training of monocytes by an insulin-like growth factor 1 receptor (IGF1-R) and mTOR-dependent signaling pathway, a mechanism that may further explain the hyperactivated phenotype of hyper-immunoglobulin D syndrome (HIDS) pathology [21,169]. Since training effects have been portrayed by enhanced levels of ROS, Ferreira et al., investigated the role of its intracellular molecule scavenger- glutathione, showing a close association of glutathione with the increased production of pro-inflammatory mediators upon trained immunity in human monocytes [170]. Other attempts to understand the role of the pentose phosphate pathway (PPP) in trained immunity responses by the pharmacological blockage of this metabolic event demonstrated this pathway as a dispensable occasion [161,167,171]. Even though, to date, there have been several papers indicating the crucial role of several metabolic pathways supporting the induction of training effects in innate immune cells, individual metabolic variations (i.e., glycolytic variability in diabetes patients) of the organisms should be taken into consideration since they significantly alter this resistance reaction [172].
Neutrophils, monocytes, macrophages, dendritic cells as well as microglial cells as a part of innate immune system are well known to be active phagocytes, producing a variety of antimicrobial substances (i.e., degrading enzymes, antimicrobial peptides and ROS) eliminating invaders [173,174,175]. To date, it has been shown that trained cells display greater antimicrobial efficacy characterized with increased phagocytic activity [50,62,176,177,178]. However, opposing findings were reported for the murine resident macrophages of the central nervous system, microglia, where the enhanced phagocytic capacity was featured exclusively by tolerant microglial cells resulting in decreased accumulation of β-amyloid plaques [46,179,180]. Anti-tumoral effects resulting from trained immunity-induced myelopoiesis caused by epigenetic and transcriptomic rewiring was reported in β-glucan-treated mice manifesting reduced tumor burden in a ROS-dependent manner [61,63]. The increased production of MCP-1 by trained cells triggers altered immune-regulatory properties, specifically elevated cell recruitment and the migration of myeloid cells, maintaining proper immune responses in health and diseases [92,176,181].
Contradictory data have arisen about the intergenerational inheritance of trained immunity providing heterologous resistance against infections in offspring [182,183]. Katzmarski et al., showed that sublethal infections o C. albicans or zymosan drive immune-resistance reactions to the progeny against heterologous infections caused by LPS or E. coli and L. monocytogenes infections [182]. Opposing findings were reported by Kaufmann et al., where the pre-exposure of parental mice to BCG, β-glucan or C. albicans did not exhibit any protective responses against viral, bacterial or fungal infections in the offspring [183]. A plausible explanation for this discrepancy of data likely involves several housing or dietary factors, the composition of the microbiome, environmental conditions as well as previous expositions to any infectious stressors [184].
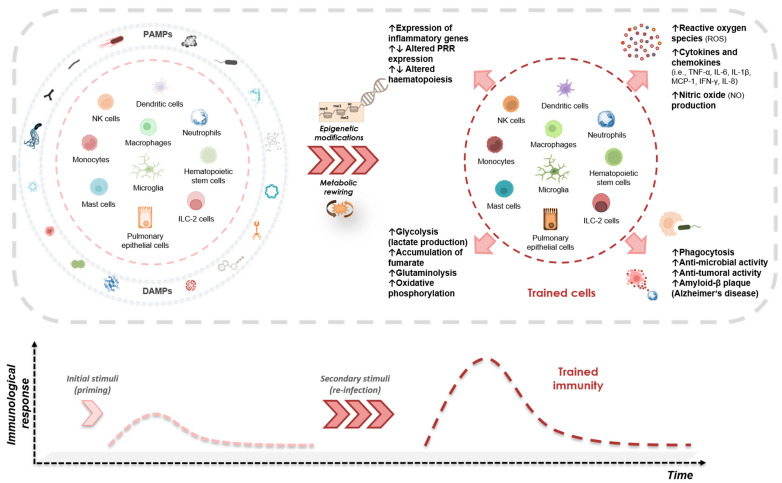
To date, an increasing number of studies has investigated the role of different PRRs, epigenetic marks as well as metabolic changes involved in the induction of training effects, yet many aspects remain obscure. An illustrative demonstration of all the above-mentioned stressor-dependent inducers of trained immunity and their characteristics is presented in Figure 2.
Figure 2.
Stressor-dependent induction of trained immunity. Innate immune cells as well as non-immune cells primed by specific exogenous (i.e., PAMPs) and endogenous (i.e., DAMPs) signals evoke long-term non-specific functional modifications mediated by epigenetic and metabolic rewiring toward a secondary insult. Trained cells express a multi-level entity of features characterized by the increased production of inflammatory mediators and altered epigenetic and metabolic marks, and reflected functionally by changes occurring in several cellular activities.
2.2. Dose-Dependent Induction of Trained Innate Memory and Immune Tolerance
“The dose makes the poison” (lat. dosis sola facit venenum) was one of quotes credited to Paracelsus underlining the importance of dose exhibiting beneficial or toxic events in organisms. Ongoing studies showed that cells strive to demonstrate hormetic or biphasic dose responses if exposed to a stimuli (intrinsic or extrinsic), where low doses promote stimulatory effects and high doses trigger inhibitory responses [185,186,187]. A similar concept has been proposed for the adaptive responses introduced by innate immune cells upon a secondary insult, where low-dose priming can trigger resistance (training) responses and high-dose priming results in tolerance reactions [53,54,188].
Actually, the role of low-dose priming enhancing the capacity of myeloid cells to subsequent challenges by bacterial infectious constituents was reported in the late 1980s, where the priming of monocytes and macrophages by endogenous IFN-γ upon a secondary stimulus by LPS triggered heightened immune responses [189,190,191], a process regulated particularly by the transcription factor NF-κB [192]. A suitable explanation for this hypothesis may serve the mechanistic interplay of mTOR and AMP-activated protein kinase (AMPK) as central regulators of cell metabolism [193,194,195]. AMPK is known to inhibit mTOR activity, orchestrating a cellular adaptive response promoting catabolic pathways and thus modulating the resistance mechanism toward an immune-suppressed phenotype [196,197]. In contrast, mTOR is well-known to support resistance mechanisms in innate immune cells and promote the memory-like cues of innate immune cells [142,198]. Interestingly, the activation of these signaling pathways depends also on the dose of stressors, where super-low doses promote resistance by a mTOR-dependent mechanism, and tolerant responses are promoted by high-stressor loads mediated by AMPK [53,196,199,200].
A growing body of evidence demonstrated comparable dose-dependent features being responsible for the induction of training and tolerance responses in myeloid cells. The application of low doses of LPS prior to any septic insults resulted in the increased mortality of mice characterized with heightened levels of inflammatory mediators, distinct from high-dose LPS pre-conditioning, which triggered an immune-suppressed phenotype portrayed by diminished levels of TNF-α and reduced sepsis mortality [201]. Furthermore, other in vitro studies revealed similar adaptive dose-dependent responses for LPS in murine monocytes and macrophages, where an increased expression of pro-inflammatory mediators by a low-dose LPS is preferentially dependent on the removal of negative modulators such as B-lymphocyte-induced maturation protein-1 (Blimp-1), different from tolerized cells induced by high doses of LPS supporting an anti-inflammatory phenotype [202,203,204,205]. Likewise, murine bone-marrow neutrophils primed with low doses of Gram-negative (i.e., LPS) or Gram-positive (i.e., LTA) constituents or gut microbiota-derived bacterial EVs upon a secondary stimulus by endotoxin exhibit an increased production of pro-inflammatory cytokines by a TLR4- and TLR-2-dependent manner activation of NF-κB by intermediate signaling of PI3Ks/MAPKs [115,145,206]. In contrast, high-dose priming promoted immune-suppressed anti-inflammatory characteristics with a decreased production of pro-inflammatory cytokines and increased IL-10 [115,145,206]. Mechanistically, the crucial role of NF-κB mediating adaptive manners has been reported for various myeloid cells [143,169,202,204,206]. In humans, a study showed that the increased immune response by monocytic cells relies on the production of IL-6 and IL-12 [207].
Accumulating reports showed that murine microglial cells can express both types of immunological imprinting, training and tolerance, which may impact the pathological hallmarks of neurological diseases [46,143,180,208]. The application of low/single doses of LPS resulted in higher inflammatory responses (trained microglia), exacerbating cerebral β-amyloidosis in a murine model of Alzheimer’s disease [46,143,180]. On the contrary, high/repeated doses of LPS exhibited a tolerant phenotype of microglia supporting neuroprotective effects [46,143,208]. The capability of microglia to retain long-term memory features relies mainly on epigenetic modifications, enrichment (training) or loss (tolerance) of epigenetic marks at enhancer regions [46,143,209,210].
Contradictory findings arise about the role of endotoxin tolerance on the antimicrobial efficacy. While Grondman and colleagues demonstrated that human immunotolerant monocytes display decreased antimicrobial activities ex vivo, other studies revealed contrasting effects, where tolerant myeloid cells are capable to express an elevated antimicrobial capacity characterized by increased phagocytosis [211,212,213,214]. Similar divergent findings have been reported in high-dose primed cells, where murine tolerant microglia expressed increased phagocytic activity in vivo and in vitro, whereas bone-marrow-tolerant neutrophils exhibited diminished phagocytosis in vitro [143,179,206]. This issue needs further investigation in order to clarify under which circumstances immunotolerant cells express increased or decreased killing activities.
As mentioned previously, trained cells express anti-tumoral features, different from immunosuppressive tolerant cells that mimic the M2 phenotype expressing pro-tumoral activities while promoting angiogenesis and tissue repair [215,216,217,218].
A respective illustration of the dose-dependent induction of trained immunity and tolerance response is shown in Figure 3. Since the topic of pathogen dose supporting the induction of opposing adaptive responses is growing, we hypothesize that similar findings will be reported for other PAMPs and DAMPs in several innate immune and non-immune cells.
Figure 3.
Dose-dependent induction of opposing adaptive inflammatory cues in innate immune system and non-immune cells. Innate immune cells primed by low/single dose PAMPs/DAMPs trigger a trained phenotype after subsequent encounter to a heterologous challenge, whereas high/repeated doses of PAMPs/DAMPs result in an immunotolerant phenotype. Both memory-like manners are mediated by epigenetic modifications with resulting effects on metabolism, altering various functional properties of the cells. This figure serves only for illustrative explanation of the hypothesis, since there are still missing data for such dose–response behaviors for certain types of cells.
2.3. Ageing, Hormones and Dietary Restrictions as Decisive Modifiers of Innate Memory
The biological mechanism of aging exposes the organism to a high susceptibility to infectious diseases due to an immune-compromised system that is incapable of mounting proper immune reactions [219,220,221,222]. Recent findings have revealed that aging relies on immune responses driven by the innate immune cells characterized by a chronic state of activation, inflammaging, which hampers T-cell recall responses to infections resulting in diminished responses of the acquired immune system [223,224]. To date, the role of innate immune memory by the innate immune compartment during ageing has only been slightly elaborated.
The investigation of human monocytes trained by β-glucan showed that trained cells from aged healthy volunteers exhibit an increased production of the pro-inflammatory TNF-α compared to young healthy individuals [225]. IL-6 was not significantly altered between the groups, while the heightened levels of cell surface markers and TNF-α were associated with an increased acetylation of H3K27 as well as enhanced metabolic capacity [225]. Additionally, as mentioned above, murine microglia as resident innate immune cells in the CNS also mount memory-like responses depending on the pathogen dose [46,143,208]. Different from the human monocytes trained by β-glucan, the trained phenotype of aged microglia induced by low doses of LPS lost the ability to express training effects in vitro [180]. This study demonstrated the pronounced plasticity of newborn microglia to introduce training effects by LPS upon a secondary stimulus. These data may be of relevance to explain the increased neuro-inflammatory susceptibility of the immature brain [180]. Moreover, it is well known that microglia during aging express a so-called “sensitized/primed” state mirrored by a heightened inflammatory profile [221]. High-dose LPS-induced immune tolerance was further significantly pronounced in aged microglial cells in vitro, which can be the result of cells attenuating excessive damage after any recurrent systemic inflammation [180]. This conclusion is also supported by other studies where tolerant microglia promotes neuroprotective reactions in the murine brain [46,208]. However, since the topic of innate memory is quite recent, there are still many aspects of aging that remain unclear and need further investigation.
Aldosterone as a mineralocorticoid hormone is essential for blood pressure and electrolyte homeostasis [226,227]. High levels of aldosterone are associated to plaque formation by monocyte-derived macrophages during atherosclerosis [228,229]. The role of aldosterone promoting training effects has been elaborated lately and the data showed that brief exposure to high amounts of aldosterone in human monocytes upon a secondary challenge by TLR2 and TLR4 ligands in vitro, resulted in enduring memory features with increased levels of pro-inflammatory mediators (TNF-α, IL-6 and ROS) regulated by H3K4me3 modifications occurring at promoters of genes important for the fatty acid synthesis pathway [26]. Therefore, the identification of such relation between supranormal levels of aldosterone and atherosclerosis may be of profound interest to understand the molecular mechanism and for the development of new therapeutic strategies to control the risk of cardiovascular diseases [26,227]. Similarly, sex hormones, such as estradiol (E2), regulates β-glucan-induced trained immunity responses in females, as shown in a septic mouse model via the non-canonical NF-κB pathway inhibiting the nuclear translocation of RelB [25]. These findings serve as a good basis to perceive the common understanding of males being more vulnerable to septic reactions than females and further offer a possible explanation about the sexual dimorphism existing in a variety of immune processes, such as individual responses to vaccines and pathogens, a process linked particularly to epigenetic changes occurring in the immune system [25,230,231]. On the contrary, an in vitro study by D’Avila et al., demonstrated that BCG training with increased production of pro-inflammatory cytokines can be suppressed by sex hormones [231,232]. However, the role of sex hormones altering the inflammatory state of innate immune cells remains controversial and needs further investigation.
Dietary mode serves as another important element that can govern the induction of trained immunity in innate immune cells [233]. Caloric restriction is known to improve health outcomes and longevity, hindering systemic inflammation driven by excessive energy intake and adiposity [233,234,235,236]. To date, reports have shown that the Western diet or the ketogenic diet, exclusively enriched in saturated fatty acids (SFAs), confers heightened responsiveness in myeloid cells upon a secondary challenge by endotoxins [237,238]. A NLRP3-dependent long-term functional reprogramming of precursor cells was reported as the main mechanistic event promoting trained immunity by dietary constituents [237]. Similarly, dietary components, such as bovine milk and milk-derived immunoglobulin G (IgG), drive the training effects on human monocytes in vitro upon a secondary insult by TLR ligands [239]. Altogether, these studies highlight the plasticity of innate immune cells to be reprogrammed by dietary supplementation types, resulting in the effective clearance of an infection or further potentially contributing to the severity of inflammatory diseases.
3. Endotoxin Tolerance
In contrast to the above-mentioned Schwartzman reaction, Beeson observed a progressive diminution of immune responses, Immune tolerance, in rabbits treated continuously by bacterial filtrates [53,240]. The phenomenon of ET was described as a key mechanistic development in myeloid cells regulating uncontrolled extensive inflammatory events, preventing harmful pathologies (i.e., sepsis) [30]. During ET, the cells enter into a temporary unresponsive state characterized by a decreased release of pro-inflammatory elements, such as TNF-α, IL-1 family of pro-inflammatory cytokines and IL-6 due to an impaired NF-κB translocation, as well as increased levels of the anti-inflammatory mediators, such as IL-10, TGF-β and arginase-1 (Arg-1) [29,30]. Inducible nitric oxide synthase (iNOS), as one of the main bacterial killing pathways, is also attenuated during ET [241]. A close competitive interplay of Arg-1 and iNOS regulating ET was reported since both enzymes share the common substrate L-arginine [242,243,244]. To date, numerous studies proclaim that, in addition to myeloid cells (i.e., monocytes, macrophages, dendritic cells, microglia and neutrophils), the development of ET also occurs in lymphoid cells, such as T cells, and non-immune cells (i.e., endothelial cells) [245,246,247,248,249,250,251,252].
The phenomenon of ET is a non-specific event, which is not limited to a specific receptor or element as the main reason for the cell anergy, since many cytokines, pathogens, fever or endogenous glucocorticoids can mimic the effects of endotoxin and LPS [253].
The activation of TLR4 by LPS recruits two distinct signaling routes, the MyD88-dependent and -independent (TRIF) pathways [254]. Both signaling events trigger the activation of NF-κB in a TRAF6 or TBK1-dependent manner, respectively [254]. However, during ET, most LPS-induced signaling events are impaired, but not entirely shut down since several anti-inflammatory mediators (i.e., IL-10) are upregulated—a process driven particularly by the delayed signaling of the MyD88-independent pathway [254,255]. TREM-1, as an orphan immunoreceptor, drives the inhibition of MMPs, also resulting in a diminished cytokine production thus contributing to the control of ET [47,256,257]. To date, researchers identified many negative regulators (SHIP, IRAK-M, SOCS1 and A20) that are implicated in the development of ET and innate immune homeostasis [254,258,259,260]. Furthermore, ongoing studies have demonstrated that the elevated release of IL-10 counteracts pro-inflammatory responses by sustaining the phosphorylation of Stat3 proteins [261]. AMPK serves as another well-known sensor and mediator of energy expenditure exerting the regulatory features of ET by suppressing LPS-induced TNF-α release and supporting anti-inflammatory reactions [196,197,262].
The transcriptomic and epigenetic analysis of myeloid cells undergoing ET have shown that this mechanistic process is accompanied by epigenetic modifications occurring on histones and regulated mainly by miRNAs. Histone modifications, especially deacetylation or methylation, cause gene silencing and are associated directly with the development of ET [30,263]. Tolerant human leukocytes display defective p65 activation on the promoter of IL-1β driven by the repressor transcription factor RelB via histone H3K9 dimethylation (H3K9me2) [35]. Comparable findings have been reported for human leukocytes, where the transcription silencing of acute pro-inflammatory genes (repression phase) during the severe systemic inflammation (SSI) is linked to chromatin remodeling, specifically to H3K9 histone methylation and RelB binding [264]. Likewise, both types of positive histone modifications, such as H3K4me3 and H4 acetylation, are selectively lost on the promoters of some pro-inflammatory genes, such as IL-6, during ET [34]. Further investigations have shown that gene-specific silencing by RelB is linked to the recruitment of histone H3 lysine 9 methyltransferase G9a and HP1 [35,36].
MiRNAs, as small non-coding RNAs (~22 nucleotides), were also described to be involved in the post-transcriptional regulation of inflammatory reactions during ET. Numerous studies described several miRNAs as being involved in the development of ET, such as miR-98, miR-125b, miR-132, miR-146a, miR-155, miR-221, miR-222, miR-579 and let-7 family [47,265,266]. For instance, miR-146, miR-155 and let-7 family target TLR4, attenuating signaling through the regulation of TRAF6 or IKKε, triggering downregulation inflammatory responses [267,268,269,270,271,272]. Diminished levels of TNF-α, as a result of subsequent challenge by LPS, were reported by the activation of miR-125b, targeting the 3′-untranslated regions of TNF-α transcripts [269]. MiR-132 has been shown to weaken inflammation in the brain, whereas miR-212 serves as a well-known tumor suppressor [273,274]. Both are known to be induced by TLR2 activation and being involved in cross tolerance responses through IRAK-4 modulation [275]. Lately, Seeley and colleagues identified miR-221 and miR-222 as critical regulators of macrophage reprogramming during LPS-tolerization, particularly associated with immunoparalysis and organ damage [276]. Moreover, miR-579 is also reported to reduce inflammatory reactions by inhibiting the translation of TNF-α in macrophages [249,277]. On the contrary, miR-98 targets the 3′-untranslated regions of IL-10 transcripts as a key cytokine for the development of ET; thus, the decreased activation of miR-98 in macrophages is accompanied with reduced levels of IL-10 [249,278]. However, the role of other miRNAs in the induction of endotoxin tolerance remains elusive and needs to be clarified. Furthermore, it would be of profound interest to determine whether the dysregulation of miRNAs may significantly affect the development and progression of inflammatory diseases [265].
Earlier studies disclosed weakened metabolic changes, especially affecting glucose metabolism during ET [279]. Changes in bioenergetics occurring during ET have been reported to be linked to several intermediate signaling proteins, such as Akt-1 or sirtuin-1 (SIRT1) [280,281]. A proper induction of ET by LPS requires the involvement of diverse intermediate proteins, such as Akt1 or SIRT1, anticipating the diminished levels of pro-inflammatory cytokines (i.e., TNF-α, IL-6 and IL-12p40) in mammals [282,283]. An increasing number of studies have suggested a close interplay between metabolism and inflammatory responses [284,285,286]. Impaired glycolysis is likely to be associated with declined inflammatory responses [287]. Supporting evidence has shown that decreased levels of lactate as an end product of glycolysis triggers reduced pro-inflammatory features and supports an anti-inflammatory phenotype in immune cells, especially on myeloid cells [288,289,290,291]. To date, reports postulated that LPS-tolerant innate immune cells are associated with reduced glycolysis as well as dysregulated cellular respiration, a process that alters the production of adenosine triphosphate (ATP) [166,211,292,293]. Recent work from Chen et al. demonstrated that the prominent gene immune-responsive gene 1 (IRG1) of activated myeloid lineage cells is responsible for encoding mitochondrial enzymes that drive the synthesis of itaconate, supporting anti-inflammatory responses mainly by modifying crucial glycolytic enzymes (impaired glycolysis) in LPS-stimulated cells [294,295]. At a mechanistic level, the attenuated inflammation by endogenous itaconate is attributed to the inhibitory effects on TET-family DNA dioxygenases, especially TET2 as a major target, thus suppressing the activation of NF-κB and STAT signaling routes [294,296]. Comparable findings for itaconate expressing anti-inflammatory properties were also highlighted in an earlier investigation by Lampropoulou et al., where they demonstrated that itaconate modulates the cell metabolism by suppressing the oxidation of succinate as a key regulator of the IL-1β–HIF-1α axis by succinate dehydrogenase [297].
Another metabolite that facilitates ET serves α-ketoglutarate (αKG). αKG is an end product of glutamine metabolism (glutaminolysis) that exerts anti-inflammatory properties of myeloid cells by modulating the NF-κB and Jmjd3 signaling pathways [298,299]. In addition to αKG, the engagement of fatty acid oxidation (FAO) has been shown as a crucial metabolic event contributing to the development of ET by AMPK-dependent activation [166,298,300,301,302,303]. Altogether, based on these characteristic features, we may conclude that ET, specifically cross-tolerance as a non-specific feature mainly attributed to innate immune cells, can serve as an antagonistic reaction to trained immunity.
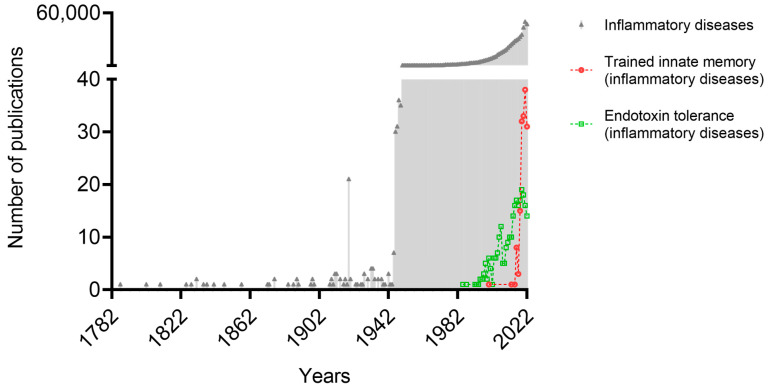
4. Role of Trained Immunity and Endotoxin Tolerance in Inflammatory Diseases
Training as well as tolerance represent memory-like (adaptive) manners of the innate immune cells. Both opposing adaptive reactions of the innate immune system are of fundamental interest since they may represent a double-edged sword counteracting each other driving, this protecting or supporting the pathogenesis of a variety of inflammatory diseases. To date, the number of studies suggesting the involvement of training or tolerance in inflammatory diseases is continuously rising (Figure 4). In this review, we briefly discuss the role of these adaptive cues in several inflammation-related disorders.
Figure 4.
A timeline of the increasing number of publications related to the induction of trained immunity and endotoxin tolerance in various inflammatory disorders. Both adaptive inflammatory processes appear to exhibit a crucial role on the suppression or progression of several inflammatory diseases (PubMed, January 2023).
To date, trained immunity has been described as a non-specific defense mechanism where innate immune cells primed by different microbial or endogenous molecular ligands confer protection against a broad spectrum of lethal pathologic infections [21,24,72]. On the contrary, the maladaptive activation of trained immunity triggers deleterious effects due to uncontrolled hyperactivation contributing to the severity of inflammatory pathologies [28,304]. Atherosclerosis, as an inflammatory disease, represents one of the main causes of coronary heart diseases, which is mainly driven by innate immune cells, especially monocytes and macrophages [305,306,307]. Recently, it was shown that trained monocytes and macrophages by oxLDL, aldosterone or hyperglycemia can contribute to the pathophysiology of atherosclerosis [26,163,308,309,310]. A similar correlation between BCG vaccination and increased aortic atherosclerosis in rabbits has been reported in the late 20th century [311].
Periodontitis, as a local inflammatory disease of oral mucosa, is associated with increased risk of certain systemic inflammatory diseases [312,313]. A recent work by Li et al., demonstrated that periodontitis-induced trained immunity in bone marrow exhibited increased severity when subjected to inflammatory comorbidities, such as rheumatic arthritis [304]. Furthermore, it is well-known that the pathogenesis of rheumatic arthritis as a chronic inflammatory disease affecting predominantly the joints is driven by several innate immune cells (i.e., monocytes, macrophages and dendritic cells) [314,315,316,317]. A close interplay between trained innate immune cells and the progression of rheumatic arthritis has been postulated, where the augmented inflammatory response by myeloid cells is controlled by epigenetic and metabolic changes mediated by the mTOR/STAT3 pathway [318,319,320,321]. Likewise, BCG-trained murine macrophages, characterized by an elevated cytokine production, can modulate fibroblast transformation involving T/B cells affecting the severity of systemic sclerosis (SSc) and inflammatory fibrotic disorders [322].
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease, where monocytes, macrophages and neutrophils play a prominent role in the disease progression [323,324,325,326]. An increasing number of studies has shown that, in SLE patients, myeloid cells manifest a dominant pro-inflammatory phenotype [327,328,329,330]. Neutrophil extracellular trap (NET) formation has been shown to participate in the pathogenesis of SLE [331]. Interestingly, C. albicans-injected mice demonstrated an increased production of NETs linked to exacerbated disease progression, a memory response attributed presumably to trained neutrophils [332,333].
A growing body of evidence has shown that β-glucan-trained myeloid cells, especially monocytes, macrophages and neutrophils, promote anti-tumoral activities controlling tumor progression, a process associated with transcriptomic, epigenetic and metabolic reprograming [61]. The appropriate rewiring of myelopoiesis by β-glucan or nanobiologic compounds, such as MTP10-HDL, results in the increased ability of innate immune cells to penetrate the tumoral environment, exhibiting suppressive effects on tumor growth [63,66]. The combination of trained immunity activities with the current immune therapy by checkpoint inhibitors represents a more efficient way of cancer immune therapy. However, it is well-known that prolonged inflammation fuels the progression of neoplastic transformation, supporting tumor growth into highly aggressive entities [334,335,336].
Nonetheless, a close association of training effects by innate immune cells supporting the pathogenesis of other inflammatory/metabolic diseases, such as diabetes mellitus type 2, obesity and chronic obstructive pulmonary diseases (COPD), has been suggested [308,337,338,339,340,341,342,343].
The process of neuroinflammation is linked to the development of neurodegenerative diseases, such as Alzheimer’s disease, Parkinson’s disease and amyotrophic lateral sclerosis [344,345,346]. An exaggerated immune response, training, by microglia contributes to the pathological hallmarks of neurodegenerative disease in mouse models [46,208,347,348]. On the contrary, the development of immune tolerance in microglial cell by continuous challenge by LPS could be a mitigating factor for neuroprotective effects in the brain [46,208,349].
The tolerant phenotype of innate immune cells, especially monocytes and macrophages, is primarily linked to the progression of cancer and sepsis, and has been observed in other diseases, such as hepatic ischemia, cystic fibrosis, pancreatitis and acute coronary syndrome [30,47]. Cytokines and chemokines released by tumor-associated macrophages (TAMs) and tumor-associated neutrophils (TANs) express pro-tumoral properties by promoting the angiogenesis, invasion and metastasis, while suppressing the immune system [350,351,352]. In vitro, tumor cells trigger the deactivation of monocytes by IRAK-M-dependent upregulation marked by declined levels of pro-inflammatory cytokines, a characteristic of tolerance development against neoplasms that can justify the increased risk of infections in leukemia patients [353,354,355,356,357]. Moreover, considering it from the phenotypic aspect, it is important to mention that TAMs exhibit comparable features to tolerant macrophages in vivo [358,359,360].
Sepsis is a life-threating organ dysfunction caused by a dysregulated host response to infections [361]. It represents a highly inflammatory disorder mediated by the uncontrolled activation of the immune system [362,363,364]. The early phase of sepsis is characterized by a hyper-inflammatory state where the induction of ET is likely to contribute to protective effects supporting decreased inflammation and repairing mechanisms [365,366]. The development of ET during the late phases of sepsis is associated with increased mortality due to suppressed immune functions and organ failure [47,366,367,368]. These findings indicate a far more complex role of ET during sepsis.
Hepatic ischemic-reperfusion (I/R) injury is a pathophysiological process of liver surgery accompanied by oxidative stress triggering cell damage and inflammation [369,370,371]. The local inflammatory reaction is driven by the innate immune cells [372]. In a rat model, it was shown that endotoxin preconditioning results in diminished hepatic I/R injury probably via the IRAK-4-dependent downregulation of intra-organ TNF-α expression [373,374]. Similar findings were reported earlier by other groups for I/R injury of the heart and hemorrhagic shock [375,376].
Other disease development which is linked to inflammatory responses of myeloid cells includes the cardiovascular disorder of acute coronary syndrome (ACS) [47,377]. This represents a good example of the hetero-tolerance where several internal factors, DAMPs (i.e., HMGB1, hyaluronic acid or heat-shock proteins), during ACS prime circulating monocytes toward a tolerant phenotype, failing to respond to subsequent challenges by external pathogenic agonists, such as LPS ex vivo [47,377]. As a result, ACS patients can be more vulnerable to secondary infections due to this phenomenon.
Finally, one of the most critical avenues is the investigation of the impact of trained immunity and endotoxin tolerance on different diseases, particularly how these adaptive features contribute to the pathogenesis of various diseases and how these reactions can be approached as preventive or therapeutic targets. As mentioned above, great emphasis has been placed on the development of trained immunity-based vaccines to increase the immunogenicity of current anti-infectious vaccines to stimulate broader responses [104]. Other relevant areas where the modulation of trained immunity may be of crucial relevance include: sepsis, cancer, allergy, neurodegenerative diseases and other immune-mediated pathologies [21,378]. Similarly, endotoxin tolerance was initially considered as a relevant mechanism to counteract hyper-inflammation-mediated diseases. As discussed previously, the immuno-suppressive state of endotoxin tolerance is involved in numerous pathologies, such as sepsis, hepatic and renal ischemia, cystic fibrosis, acute pulmonary syndrome and cancer [30]. Initial attempts of the modulation of these adaptive manners included designing proper small-molecule agonists/antagonist that may act in different PRRs; however, since some receptors (i.e., TLR4) may trigger the development of both opposing reactions, this attempt may not be of ideal use. Promising data are expected to appear in the coming years involving epigenomic and transcriptomic modulations as crucial regulators of trained immunity and tolerance.
Taken together, both opposing memory-like inflammatory reactions (training and tolerance) may play a crucial role in the progression or suppression of various inflammatory diseases. To date, the role of both adaptive cues of innate immune system in other diseases remains elusive and needs to be clarified.
5. Conclusions
The identification of these antagonistic inflammatory cues, trained immunity and endotoxin tolerance, has greatly challenged overall considerations accumulated through the years regarding the “primitivity” of the innate immune cells. While trained immunity aims at pathogen elimination, it may contribute also to the progression of inflammatory diseases. On the contrary, tolerance may promote repairing/protective mechanisms against some inflammatory pathologies, but on the other hand, its incidence correlates with an increased risk to secondary infections. Both opposing reactions of the innate immune system represent a highly complex, multi-level number of events notably regulated by diverse alterations occurring on signaling pathways, chromatin modulations as well as metabolic rewiring. However, we hope that future investigations in regard to the role of training and tolerance in various diseases will pave the way for the development of novel strategies for preventive and therapeutic purposes.
Author Contributions
Conceptualization, T.L., N.K.-G., H.H. and C.G.; methodology, T.L.; validation, T.L., N.K.-G., R.B., S.G.Z., E.L., V.A., S.D., S.A.K., J.R., A.D., J.H., M.B., D.F., H.H. and C.G.; formal analysis, T.L., N.K.-G., R.B., S.G.Z., E.L., V.A., S.D., S.A.K., J.R., A.D., J.H., M.B., D.F., H.H. and C.G.; data curation, T.L. and C.G.; writing—original draft preparation, T.L., H.H. and C.G.; writing—review and editing, N.K.-G., R.B., S.G.Z., M.B. and D.F.; visualization, T.L. and E.L.; supervision, H.H. and C.G.; funding acquisition, N.K.-G., D.F., M.B., H.H. and C.G. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The PubMed data presented in this paper are accessible online for any reader (Link: https://pubmed.ncbi.nlm.nih.gov/ (accessed on 10 January 2023)).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
This research was funded by Bundesministerium für Bildung und Forschung (BMBF, Germany), Project PRIMAL with grant numbers 01GL1746E (D.F. and H.H.) and 01GL1745F (N.K.-G. and C.G.). M.B. was funded by the Olympia Morata Fellowship from Heidelberg University and acknowledges Baden-Württemberg Stiftung for the financial support by the Eliteprogramme for Postdocs.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Marshall J.S., Warrington R., Watson W., Kim H.L. An Introduction to Immunology and Immunopathology. Allergy Asthma Clin. Immunol. 2018;14((Suppl. 2)):49. doi: 10.1186/s13223-018-0278-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bonilla F.A., Oettgen H.C. Adaptive Immunity. J. Allergy Clin. Immunol. 2010;125:S33–S40. doi: 10.1016/j.jaci.2009.09.017. [DOI] [PubMed] [Google Scholar]
- 3.Turvey S.E., Broide D.H. Innate Immunity. J. Allergy Clin. Immunol. 2010;125:S24–S32. doi: 10.1016/j.jaci.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Medzhitov R. Toll-like Receptors and Innate Immunity. Nat. Rev. Immunol. 2001;1:135–145. doi: 10.1038/35100529. [DOI] [PubMed] [Google Scholar]
- 5.Kurtz J. Specific Memory within Innate Immune Systems. Trends Immunol. 2005;26:186–192. doi: 10.1016/j.it.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 6.Wenig M., Ghirardo A., Sales J.H., Pabst E.S., Breitenbach H.H., Antritter F., Weber B., Lange B., Lenk M., Cameron R.K., et al. Systemic Acquired Resistance Networks Amplify Airborne Defense Cues. Nat. Commun. 2019;10:3813. doi: 10.1038/s41467-019-11798-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gourbal B., Pinaud S., Beckers G.J.M., Van Der Meer J.W.M., Conrath U., Netea M.G. Innate Immune Memory: An Evolutionary Perspective. Immunol. Rev. 2018;283:21–40. doi: 10.1111/imr.12647. [DOI] [PubMed] [Google Scholar]
- 8.Weiss M.C., Sousa F.L., Mrnjavac N., Neukirchen S., Roettger M., Nelson-Sathi S., Martin W.F. The Physiology and Habitat of the Last Universal Common Ancestor. Nat. Microbiol. 2016;1:16116. doi: 10.1038/nmicrobiol.2016.116. [DOI] [PubMed] [Google Scholar]
- 9.Purvis A., Hector A. Getting the Measure of Biodiversity. Nature. 2000;405:212–219. doi: 10.1038/35012221. [DOI] [PubMed] [Google Scholar]
- 10.Titley M.A., Snaddon J.L., Turner E.C. Scientific Research on Animal Biodiversity Is Systematically Biased towards Vertebrates and Temperate Regions. PLoS ONE. 2017;12:e0189577. doi: 10.1371/journal.pone.0189577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naeslund C. Expérience de Vaccination Par Le BCG Dans La Province Du Norrbotten (Suède) Rev. Tuberc. 1931;12:617–636. [Google Scholar]
- 12.Mackaness G.B. The Immunology of Antituberculous Immunity. Am. Rev. Respir. Dis. 1968;97:337–344. doi: 10.1164/arrd.1968.97.3.337. [DOI] [PubMed] [Google Scholar]
- 13.Blanden R.V., Lefford M.J., Mackaness G.B. The Host Response to Calmette-Guérin Bacillus Infection in Mice. J. Exp. Med. 1969;129:1079–1107. doi: 10.1084/jem.129.5.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garly M.L., Martins C.L., Balé C., Baldé M.A., Hedegaard K.L., Gustafson P., Lisse I.M., Whittle H.C., Aaby P. BCG Scar and Positive Tuberculin Reaction Associated with Reduced Child Mortality in West Africa: A Non-Specific Beneficial Effect of BCG? Vaccine. 2003;21:2782–2790. doi: 10.1016/S0264-410X(03)00181-6. [DOI] [PubMed] [Google Scholar]
- 15.Aaby P., Roth A., Ravn H., Napirna B.M., Rodrigues A., Lisse I.M., Stensballe L., Diness B.R., Lausch K.R., Lund N., et al. Randomized Trial of BCG Vaccination at Birth to Low-Birth-Weight Children: Beneficial Nonspecific Effects in the Neonatal Period? J. Infect. Dis. 2011;204:245–252. doi: 10.1093/infdis/jir240. [DOI] [PubMed] [Google Scholar]
- 16.Aaby P., Martins C.L., Garly M.-L., Balé C., Andersen A., Rodrigues A., Ravn H., Lisse I.M., Benn C.S., Whittle H.C. Non-Specific Effects of Standard Measles Vaccine at 4.5 and 9 Months of Age on Childhood Mortality: Randomised Controlled Trial. BMJ. 2010;341:c6495. doi: 10.1136/bmj.c6495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Biering-Sørensen S., Jensen K.J., Monterio I., Ravn H., Aaby P., Benn C.S. Rapid Protective Effects of Early BCG on Neonatal Mortality Among Low Birth Weight Boys: Observations From Randomized Trials. J. Infect. Dis. 2018;217:759–766. doi: 10.1093/infdis/jix612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Escobar L.E., Molina-Cruz A., Barillas-Mury C. BCG Vaccine Protection from Severe Coronavirus Disease 2019 (COVID-19) Proc. Natl. Acad. Sci. USA. 2020;117:17720–17726. doi: 10.1073/pnas.2008410117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prentice S., Nassanga B., Webb E.L., Akello F., Kiwudhu F., Akurut H., Elliott A.M., Arts R.J.W., Netea M.G., Dockrell H.M., et al. BCG-Induced Non-Specific Effects on Heterologous Infectious Disease in Ugandan Neonates: An Investigator-Blind Randomised Controlled Trial. Lancet. Infect. Dis. 2021;21:993–1003. doi: 10.1016/S1473-3099(20)30653-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Netea M.G., Quintin J., van der Meer J.W.M. Trained Immunity: A Memory for Innate Host Defense. Cell Host Microbe. 2011;9:355–361. doi: 10.1016/j.chom.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 21.Netea M.G., Domínguez-Andrés J., Barreiro L.B., Chavakis T., Divangahi M., Fuchs E., Joosten L.A.B., van der Meer J.W.M., Mhlanga M.M., Mulder W.J.M., et al. Defining Trained Immunity and Its Role in Health and Disease. Nat. Rev. Immunol. 2020;20:375–388. doi: 10.1038/s41577-020-0285-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ochando J., Fayad Z.A., Madsen J.C., Netea M.G., Mulder W.J.M. Trained Immunity in Organ Transplantation. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2020;20:10–18. doi: 10.1111/ajt.15620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Braza M.S., van Leent M.M.T., Lameijer M., Sanchez-Gaytan B.L., Arts R.J.W., Pérez-Medina C., Conde P., Garcia M.R., Gonzalez-Perez M., Brahmachary M., et al. Inhibiting Inflammation with Myeloid Cell-Specific Nanobiologics Promotes Organ Transplant Acceptance. Immunity. 2018;49:819–828.e6. doi: 10.1016/j.immuni.2018.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ochando J., Mulder W.J.M., Madsen J.C., Netea M.G., Duivenvoorden R. Trained Immunity - Basic Concepts and Contributions to Immunopathology. Nat. Rev. Nephrol. 2023;19:23–37. doi: 10.1038/s41581-022-00633-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun Z., Pan Y., Qu J., Xu Y., Dou H., Hou Y. 17β-Estradiol Promotes Trained Immunity in Females Against Sepsis via Regulating Nucleus Translocation of RelB. Front. Immunol. 2020;11:1591. doi: 10.3389/fimmu.2020.01591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van der Heijden C.D.C.C., Keating S.T., Groh L., Joosten L.A.B., Netea M.G., Riksen N.P. Aldosterone Induces Trained Immunity: The Role of Fatty Acid Synthesis. Cardiovasc. Res. 2020;116:317–328. doi: 10.1093/cvr/cvz137. [DOI] [PubMed] [Google Scholar]
- 27.Netea M.G., Joosten L.A.B. Trained Immunity and Local Innate Immune Memory in the Lung. Cell. 2018;175:1463–1465. doi: 10.1016/j.cell.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 28.Netea M.G., Joosten L.A.B., Latz E., Mills K.H.G., Natoli G., Stunnenberg H.G., ONeill L.A.J., Xavier R.J. Trained Immunity: A Program of Innate Immune Memory in Health and Disease. Science. 2016;352:aaf1098. doi: 10.1126/science.aaf1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.West M.A., Heagy W. Endotoxin Tolerance: A Review. Crit. Care Med. 2002;30:S64–S73. doi: 10.1097/00003246-200201001-00009. [DOI] [PubMed] [Google Scholar]
- 30.Biswas S.K., Lopez-Collazo E. Endotoxin Tolerance: New Mechanisms, Molecules and Clinical Significance. Trends Immunol. 2009;30:475–487. doi: 10.1016/j.it.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 31.Chen J., Ivashkiv L.B. IFN-γ Abrogates Endotoxin Tolerance by Facilitating Toll-like Receptor-Induced Chromatin Remodeling. Proc. Natl. Acad. Sci. USA. 2010;107:19438–19443. doi: 10.1073/pnas.1007816107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ip W.K.E., Hoshi N., Shouval D.S., Snapper S., Medzhitov R. Anti-Inflammatory Effect of IL-10 Mediated by Metabolic Reprogramming of Macrophages. Science. 2017;356:513–519. doi: 10.1126/science.aal3535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jentho E., Lajqi T., Yang K., Winkler R., Stojiljkovic M., Wetzker R., Bauer M. Pathogen-Induced Hormetic Responses. In: Rattan S.I.S., Kyriazis M., editors. The Science of Hormesis in Health and Longevity. Elsevier; Amsterdam, The Netherlands: 2019. pp. 161–170. [Google Scholar]
- 34.Foster S.L., Hargreaves D.C., Medzhitov R. Gene-Specific Control of Inflammation by TLR-Induced Chromatin Modifications. Nature. 2007;447:972–978. doi: 10.1038/nature05836. [DOI] [PubMed] [Google Scholar]
- 35.Chan C., Li L., McCall C.E., Yoza B.K. Endotoxin Tolerance Disrupts Chromatin Remodeling and NF-ΚB Transactivation at the IL-1β Promoter. J. Immunol. 2005;175:461–468. doi: 10.4049/jimmunol.175.1.461. [DOI] [PubMed] [Google Scholar]
- 36.Chen X., El Gazzar M., Yoza B.K., McCall C.E. The NF-KB Factor RelB and Histone H3 Lysine Methyltransferase G9a Directly Interact to Generate Epigenetic Silencing in Endotoxin Tolerance. J. Biol. Chem. 2009;284:27857–27865. doi: 10.1074/jbc.M109.000950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Domínguez-Andrés J., Novakovic B., Li Y., Scicluna B.P., Gresnigt M.S., Arts R.J.W., Oosting M., Moorlag S.J.C.F.M., Groh L.A., Zwaag J., et al. The Itaconate Pathway Is a Central Regulatory Node Linking Innate Immune Tolerance and Trained Immunity. Cell Metab. 2019;29:211–220.e5. doi: 10.1016/j.cmet.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 38.Mogensen T.H. Pathogen Recognition and Inflammatory Signaling in Innate Immune Defenses. Clin. Microbiol. Rev. 2009;22:240–273. doi: 10.1128/CMR.00046-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kieser K.J., Kagan J.C. Multi-Receptor Detection of Individual Bacterial Products by the Innate Immune System. Nat. Rev. Immunol. 2017;17:376–390. doi: 10.1038/nri.2017.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Takeuchi O., Akira S. Pattern Recognition Receptors and Inflammation. Cell. 2010;140:805–820. doi: 10.1016/j.cell.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 41.Li D., Wu M. Pattern Recognition Receptors in Health and Diseases. Signal Transduct. Target. Ther. 2021;6:291. doi: 10.1038/s41392-021-00687-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Agier J., Pastwińska J., Brzezińska-Błaszczyk E. An Overview of Mast Cell Pattern Recognition Receptors. Inflamm. Res. Off. J. Eur. Histamine Res. Soc. 2018;67:737–746. doi: 10.1007/s00011-018-1164-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kawai T., Akira S. The Role of Pattern-Recognition Receptors in Innate Immunity: Update on Toll-like Receptors. Nat. Immunol. 2010;11:373–384. doi: 10.1038/ni.1863. [DOI] [PubMed] [Google Scholar]
- 44.Leentjens J., Bekkering S., Joosten L.A.B., Netea M.G., Burgner D.P., Riksen N.P. Trained Innate Immunity as a Novel Mechanism Linking Infection and the Development of Atherosclerosis. Circ. Res. 2018;122:664–669. doi: 10.1161/CIRCRESAHA.117.312465. [DOI] [PubMed] [Google Scholar]
- 45.Bekkering S., Stiekema L.C.A., Bernelot Moens S., Verweij S.L., Novakovic B., Prange K., Versloot M., Roeters van Lennep J.E., Stunnenberg H., de Winther M., et al. Treatment with Statins Does Not Revert Trained Immunity in Patients with Familial Hypercholesterolemia. Cell Metab. 2019;30:1–2. doi: 10.1016/j.cmet.2019.05.014. [DOI] [PubMed] [Google Scholar]
- 46.Wendeln A.-C., Degenhardt K., Kaurani L., Gertig M., Ulas T., Jain G., Wagner J., Häsler L.M., Wild K., Skodras A., et al. Innate Immune Memory in the Brain Shapes Neurological Disease Hallmarks. Nature. 2018;556:332–338. doi: 10.1038/s41586-018-0023-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.López-Collazo E., del Fresno C. Pathophysiology of Endotoxin Tolerance: Mechanisms and Clinical Consequences. Crit. Care. 2013;17:242. doi: 10.1186/cc13110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Morris M.C., Gilliam E.A., Li L. Innate Immune Programing by Endotoxin and Its Pathological Consequences. Front. Immunol. 2015;6:1–8. doi: 10.3389/fimmu.2014.00680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rieckmann A., Villumsen M., Sørup S., Haugaard L.K., Ravn H., Roth A., Baker J.L., Benn C.S., Aaby P. Vaccinations against Smallpox and Tuberculosis Are Associated with Better Long-Term Survival: A Danish Case-Cohort Study 1971-2010. Int. J. Epidemiol. 2017;46:695–705. doi: 10.1093/ije/dyw120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kaufmann E., Sanz J., Dunn J.L., Khan N., Mendonça L.E., Pacis A., Tzelepis F., Pernet E., Dumaine A., Grenier J.-C., et al. BCG Educates Hematopoietic Stem Cells to Generate Protective Innate Immunity against Tuberculosis. Cell. 2018;172:176–190.e19. doi: 10.1016/j.cell.2017.12.031. [DOI] [PubMed] [Google Scholar]
- 51.Chavakis T., Mitroulis I., Hajishengallis G. Hematopoietic Progenitor Cells as Integrative Hubs for Adaptation to and Fine-Tuning of Inflammation. Nat. Immunol. 2019;20:802–811. doi: 10.1038/s41590-019-0402-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mitroulis I., Ruppova K., Wang B., Chen L.-S., Grzybek M., Grinenko T., Eugster A., Troullinaki M., Palladini A., Kourtzelis I., et al. Modulation of Myelopoiesis Progenitors Is an Integral Component of Trained Immunity. Cell. 2018;172:147–161.e12. doi: 10.1016/j.cell.2017.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bauer M., Weis S., Netea M.G., Wetzker R. Remembering Pathogen Dose: Long-Term Adaptation in Innate Immunity. Trends Immunol. 2018;39:438–445. doi: 10.1016/j.it.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 54.Lajqi T., Pöschl J., Frommhold D., Hudalla H. The Role of Microbiota in Neutrophil Regulation and Adaptation in Newborns. Front. Immunol. 2020;11:568685. doi: 10.3389/fimmu.2020.568685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shwartzman G. Concerning the Specificity and Nature of the Phenomenon of Local Skin Reactivity to Various Bacterial Filtrates. J. Exp. Med. 1930;51:571–583. doi: 10.1084/jem.51.4.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ifrim D.C., Quintin J., Joosten L.A.B., Jacobs C., Jansen T., Jacobs L., Gow N.A.R., Williams D.L., van der Meer J.W.M., Netea M.G. Trained Immunity or Tolerance: Opposing Functional Programs Induced in Human Monocytes after Engagement of Various Pattern Recognition Receptors. Clin. Vaccine Immunol. 2014;21:534–545. doi: 10.1128/CVI.00688-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Netea M.G., van der Meer J.W.M. Trained Immunity: An Ancient Way of Remembering. Cell Host Microbe. 2017;21:297–300. doi: 10.1016/j.chom.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 58.Moorlag S.J.C.F.M., Khan N., Novakovic B., Kaufmann E., Jansen T., van Crevel R., Divangahi M., Netea M.G. β-Glucan Induces Protective Trained Immunity against Mycobacterium Tuberculosis Infection: A Key Role for IL-1. Cell Rep. 2020;31:107634. doi: 10.1016/j.celrep.2020.107634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Quintin J., Saeed S., Martens J.H.A.A., Giamarellos-Bourboulis E.J., Ifrim D.C., Logie C., Jacobs L., Jansen T., Kullberg B.J., Wijmenga C., et al. Candida Albicans Infection Affords Protection against Reinfection via Functional Reprogramming of Monocytes. Cell Host Microbe. 2012;12:223–232. doi: 10.1016/j.chom.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moerings B.G.J., de Graaff P., Furber M., Witkamp R.F., Debets R., Mes J.J., van Bergenhenegouwen J., Govers C. Continuous Exposure to Non-Soluble β-Glucans Induces Trained Immunity in M-CSF-Differentiated Macrophages. Front. Immunol. 2021;12:672796. doi: 10.3389/fimmu.2021.672796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kalafati L., Kourtzelis I., Schulte-Schrepping J., Li X., Hatzioannou A., Grinenko T., Hagag E., Sinha A., Has C., Dietz S., et al. Innate Immune Training of Granulopoiesis Promotes Anti-Tumor Activity. Cell. 2020;183:771–785. doi: 10.1016/j.cell.2020.09.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.dos Santos J.C., Barroso de Figueiredo A.M., Teodoro Silva M.V., Cirovic B., de Bree L.C.J., Damen M.S.M.A., Moorlag S.J.C.F.M., Gomes R.S., Helsen M.M., Oosting M., et al. β-Glucan-Induced Trained Immunity Protects against Leishmania Braziliensis Infection: A Crucial Role for IL-32. Cell Rep. 2019;28:2659–2672.e6. doi: 10.1016/j.celrep.2019.08.004. [DOI] [PubMed] [Google Scholar]
- 63.Geller A.E., Shrestha R., Woeste M.R., Guo H., Hu X., Ding C., Andreeva K., Chariker J.H., Zhou M., Tieri D., et al. The Induction of Peripheral Trained Immunity in the Pancreas Incites Anti-Tumor Activity to Control Pancreatic Cancer Progression. Nat. Commun. 2022;13:759. doi: 10.1038/s41467-022-28407-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vetvicka V., Vetvickova J. Glucan Supplementation Enhances the Immune Response against an Influenza Challenge in Mice. Ann. Transl. Med. 2015;3:22. doi: 10.3978/j.issn.2305-5839.2015.01.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.De Zuani M., Dal Secco C., Tonon S., Arzese A., Pucillo C.E.M., Frossi B. LPS Guides Distinct Patterns of Training and Tolerance in Mast Cells. Front. Immunol. 2022;13:835348. doi: 10.3389/fimmu.2022.835348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Priem B., van Leent M.M.T., Teunissen A.J.P., Sofias A.M., Mourits V.P., Willemsen L., Klein E.D., Oosterwijk R.S., Meerwaldt A.E., Munitz J., et al. Trained Immunity-Promoting Nanobiologic Therapy Suppresses Tumor Growth and Potentiates Checkpoint Inhibition. Cell. 2020;183:786–801.e19. doi: 10.1016/j.cell.2020.09.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mourits V.P., Koeken V.A.C.M., de Bree L.C.J., Moorlag S.J.C.F.M., Chu W.C., Xu X., Dijkstra H., Lemmers H., Joosten L.A.B., Wang Y., et al. BCG-Induced Trained Immunity in Healthy Individuals: The Effect of Plasma Muramyl Dipeptide Concentrations. J. Immunol. Res. 2020;2020:5812743. doi: 10.1155/2020/5812743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Riquelme S.A., Prince A. Airway Immunometabolites Fuel Pseudomonas Aeruginosa Infection. Respir. Res. 2020;21:326. doi: 10.1186/s12931-020-01591-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Qin S., Xiao W., Zhou C., Pu Q., Deng X., Lan L., Liang H., Song X., Wu M. Pseudomonas Aeruginosa: Pathogenesis, Virulence Factors, Antibiotic Resistance, Interaction with Host, Technology Advances and Emerging Therapeutics. Signal Transduct. Target. Ther. 2022;7:199. doi: 10.1038/s41392-022-01056-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bigot J., Guillot L., Guitard J., Ruffin M., Corvol H., Chignard M., Hennequin C., Balloy V. Respiratory Epithelial Cells Can Remember Infection: A Proof-of-Concept Study. J. Infect. Dis. 2020;221:1000–1005. doi: 10.1093/infdis/jiz569. [DOI] [PubMed] [Google Scholar]
- 71.Ciarlo E., Heinonen T., Théroude C., Asgari F., Le Roy D., Netea M.G., Roger T. Trained Immunity Confers Broad-Spectrum Protection Against Bacterial Infections. J. Infect. Dis. 2020;222:1869–1881. doi: 10.1093/infdis/jiz692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Théroude C., Reverte M., Heinonen T., Ciarlo E., Schrijver I.T., Antonakos N., Maillard N., Pralong F., Le Roy D., Roger T. Trained Immunity Confers Prolonged Protection From Listeriosis. Front. Immunol. 2021;12:723393. doi: 10.3389/fimmu.2021.723393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Riquelme S.A., Liimatta K., Wong Fok Lung T., Fields B., Ahn D., Chen D., Lozano C., Sáenz Y., Uhlemann A.-C., Kahl B.C., et al. Pseudomonas Aeruginosa Utilizes Host-Derived Itaconate to Redirect Its Metabolism to Promote Biofilm Formation. Cell Metab. 2020;31:1091–1106.e6. doi: 10.1016/j.cmet.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Quinn M.K., Edmond K.M., Fawzi W.W., Hurt L., Kirkwood B.R., Masanja H., Muhihi A.J., Newton S., Noor R.A., Williams P.L., et al. Non-Specific Effects of BCG and DTP Vaccination on Infant Mortality: An Analysis of Birth Cohorts in Ghana and Tanzania. Vaccine. 2022;40:3737–3745. doi: 10.1016/j.vaccine.2022.04.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wilkie M., Tanner R., Wright D., Lopez Ramon R., Beglov J., Riste M., Marshall J.L., Harris S.A., Bettencourt P.J.G., Hamidi A., et al. Functional In-Vitro Evaluation of the Non-Specific Effects of BCG Vaccination in a Randomised Controlled Clinical Study. Sci. Rep. 2022;12:7808. doi: 10.1038/s41598-022-11748-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Aaby P., Benn C.S., Flanagan K.L., Klein S.L., Kollmann T.R., Lynn D.J., Shann F. The Non-Specific and Sex-Differential Effects of Vaccines. Nat. Rev. Immunol. 2020;20:464–470. doi: 10.1038/s41577-020-0338-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kleinnijenhuis J., Quintin J., Preijers F., Joosten L.A.B., Ifrim D.C., Saeed S., Jacobs C., van Loenhout J., de Jong D., Stunnenberg H.G., et al. Bacille Calmette-Guerin Induces NOD2-Dependent Nonspecific Protection from Reinfection via Epigenetic Reprogramming of Monocytes. Proc. Natl. Acad. Sci. USA. 2012;109:17537–17542. doi: 10.1073/pnas.1202870109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kleinnijenhuis J., Quintin J., Preijers F., Benn C.S., Joosten L.A.B., Jacobs C., Van Loenhout J., Xavier R.J., Aaby P., Van Der Meer J.W.M., et al. Long-Lasting Effects of Bcg Vaccination on Both Heterologous Th1/Th17 Responses and Innate Trained Immunity. J. Innate Immun. 2014;6:152–158. doi: 10.1159/000355628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bonneville M., O’Brien R.L., Born W.K. Gammadelta T Cell Effector Functions: A Blend of Innate Programming and Acquired Plasticity. Nat. Rev. Immunol. 2010;10:467–478. doi: 10.1038/nri2781. [DOI] [PubMed] [Google Scholar]
- 80.Caron J., Ridgley L.A., Bodman-Smith M. How to Train Your Dragon: Harnessing Gamma Delta T Cells Antiviral Functions and Trained Immunity in a Pandemic Era. Front. Immunol. 2021;12:666983. doi: 10.3389/fimmu.2021.666983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Deetz C.O., Hebbeler A.M., Propp N.A., Cairo C., Tikhonov I., Pauza C.D. Gamma Interferon Secretion by Human Vgamma2Vdelta2 T Cells after Stimulation with Antibody against the T-Cell Receptor plus the Toll-Like Receptor 2 Agonist Pam3Cys. Infect. Immun. 2006;74:4505–4511. doi: 10.1128/IAI.00088-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lester S.N., Li K. Toll-like Receptors in Antiviral Innate Immunity. J. Mol. Biol. 2014;426:1246–1264. doi: 10.1016/j.jmb.2013.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wesch D., Beetz S., Oberg H.-H., Marget M., Krengel K., Kabelitz D. Direct Costimulatory Effect of TLR3 Ligand Poly(I:C) on Human Gamma Delta T Lymphocytes. J. Immunol. 2006;176:1348–1354. doi: 10.4049/jimmunol.176.3.1348. [DOI] [PubMed] [Google Scholar]
- 84.González S., López-Soto A., Suarez-Alvarez B., López-Vázquez A., López-Larrea C. NKG2D Ligands: Key Targets of the Immune Response. Trends Immunol. 2008;29:397–403. doi: 10.1016/j.it.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 85.Spada F.M., Grant E.P., Peters P.J., Sugita M., Melián A., Leslie D.S., Lee H.K., van Donselaar E., Hanson D.A., Krensky A.M., et al. Self-Recognition of CD1 by Gamma/Delta T Cells: Implications for Innate Immunity. J. Exp. Med. 2000;191:937–948. doi: 10.1084/jem.191.6.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Röring R.J., Debisarun P.A., Botey-Bataller J., Suen T.K., Bulut Ö., Kilic G., Koeken V.A.C.M., Sarlea A., Bahrar H., Dijkstra H., et al. MMR Vaccination Induces a Trained Immunity Program Characterized by Functional and Metabolic Reprogramming of Γδ T Cells. bioRxiv. 2022 doi: 10.1101/2022.11.24.516894. (Preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mazzola T.N., Da Silva M.T.N., Moreno Y.M.F., Lima S.C.B.S., Carniel E.F., Morcillo A.M., Antonio M.A.R.G.M., Zanolli M.L., Netto A.A., Blotta M.H., et al. Robust Gammadelta+ T Cell Expansion in Infants Immunized at Birth with BCG Vaccine. Vaccine. 2007;25:6313–6320. doi: 10.1016/j.vaccine.2007.06.039. [DOI] [PubMed] [Google Scholar]
- 88.Zufferey C., Germano S., Dutta B., Ritz N., Curtis N. The Contribution of Non-Conventional T Cells and NK Cells in the Mycobacterial-Specific IFNγ Response in Bacille Calmette-Guérin (BCG)-Immunized Infants. PLoS ONE. 2013;8:e77334. doi: 10.1371/journal.pone.0077334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Taştan Y., Arvas A., Demir G., Alikaşifoğlu M., Gür E., Kiray E. Influence of Bacillus Calmette-Guèrin Vaccination at Birth and 2 Months Old Age on the Peripheral Blood T-Cell Subpopulations [Gamma/Delta and Alpha-Beta T Cell] Pediatr. allergy Immunol. Off. Publ. Eur. Soc. Pediatr. Allergy Immunol. 2005;16:624–629. doi: 10.1111/j.1399-3038.2005.00329.x. [DOI] [PubMed] [Google Scholar]
- 90.Bukowski J.F., Morita C.T., Brenner M.B. Recognition and Destruction of Virus-Infected Cells by Human Gamma Delta CTL. J. Immunol. 1994;153:5133–5140. doi: 10.4049/jimmunol.153.11.5133. [DOI] [PubMed] [Google Scholar]
- 91.Debisarun P.A., Gössling K.L., Bulut O., Kilic G., Zoodsma M., Liu Z., Oldenburg M., Rüchel N., Zhang B., Xu C.-J., et al. Induction of Trained Immunity by Influenza Vaccination - Impact on COVID-19. PLoS Pathog. 2021;17:e1009928. doi: 10.1371/journal.ppat.1009928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Murphy D.M., Cox D.J., Connolly S.A., Breen E.P., Brugman A.A., Phelan J.J., Keane J., Basdeo S.A. Trained Immunity Is Induced in Humans after Immunization with an Adenoviral Vector COVID-19 Vaccine. J. Clin. Investig. 2023;133:e162581. doi: 10.1172/JCI162581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sun J.C., Beilke J.N., Lanier L.L. Adaptive Immune Features of Natural Killer Cells. Nature. 2009;457:557–561. doi: 10.1038/nature07665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.O’Leary J.G., Goodarzi M., Drayton D.L., von Andrian U.H. T Cell- and B Cell-Independent Adaptive Immunity Mediated by Natural Killer Cells. Nat. Immunol. 2006;7:507–516. doi: 10.1038/ni1332. [DOI] [PubMed] [Google Scholar]
- 95.Sun J.C., Madera S., Bezman N.A., Beilke J.N., Kaplan M.H., Lanier L.L. Proinflammatory Cytokine Signaling Required for the Generation of Natural Killer Cell Memory. J. Exp. Med. 2012;209:947–954. doi: 10.1084/jem.20111760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Björkström N.K., Lindgren T., Stoltz M., Fauriat C., Braun M., Evander M., Michaëlsson J., Malmberg K.-J., Klingström J., Ahlm C., et al. Rapid Expansion and Long-Term Persistence of Elevated NK Cell Numbers in Humans Infected with Hantavirus. J. Exp. Med. 2011;208:13–21. doi: 10.1084/jem.20100762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Della Chiesa M., Falco M., Podestà M., Locatelli F., Moretta L., Frassoni F., Moretta A. Phenotypic and Functional Heterogeneity of Human NK Cells Developing after Umbilical Cord Blood Transplantation: A Role for Human Cytomegalovirus? Blood. 2012;119:399–410. doi: 10.1182/blood-2011-08-372003. [DOI] [PubMed] [Google Scholar]
- 98.Tarannum M., Romee R. Cytokine-Induced Memory-like Natural Killer Cells for Cancer Immunotherapy. Stem Cell Res. Ther. 2021;12:592. doi: 10.1186/s13287-021-02655-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Luetke-Eversloh M., Hammer Q., Durek P., Nordström K., Gasparoni G., Pink M., Hamann A., Walter J., Chang H.-D., Dong J., et al. Human Cytomegalovirus Drives Epigenetic Imprinting of the IFNG Locus in NKG2Chi Natural Killer Cells. PLoS Pathog. 2014;10:e1004441. doi: 10.1371/journal.ppat.1004441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Brown M.G., Dokun A.O., Heusel J.W., Smith H.R., Beckman D.L., Blattenberger E.A., Dubbelde C.E., Stone L.R., Scalzo A.A., Yokoyama W.M. Vital Involvement of a Natural Killer Cell Activation Receptor in Resistance to Viral Infection. Science. 2001;292:934–937. doi: 10.1126/science.1060042. [DOI] [PubMed] [Google Scholar]
- 101.Karo J.M., Schatz D.G., Sun J.C. The RAG Recombinase Dictates Functional Heterogeneity and Cellular Fitness in Natural Killer Cells. Cell. 2014;159:94–107. doi: 10.1016/j.cell.2014.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cooper M.A., Elliott J.M., Keyel P.A., Yang L., Carrero J.A., Yokoyama W.M. Cytokine-Induced Memory-like Natural Killer Cells. Proc. Natl. Acad. Sci. USA. 2009;106:1915–1919. doi: 10.1073/pnas.0813192106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Romee R., Schneider S.E., Leong J.W., Chase J.M., Keppel C.R., Sullivan R.P., Cooper M.A., Fehniger T.A. Cytokine Activation Induces Human Memory-like NK Cells. Blood. 2012;120:4751–4760. doi: 10.1182/blood-2012-04-419283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sánchez-Ramón S., Conejero L., Netea M.G., Sancho D., Palomares Ó., Subiza J.L. Trained Immunity-Based Vaccines: A New Paradigm for the Development of Broad-Spectrum Anti-Infectious Formulations. Front. Immunol. 2018;9:2936. doi: 10.3389/fimmu.2018.02936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Conejero L., Saz-Leal P., Subiza J.L. Trained Immunity-Based Vaccines: A Ready-to-Act Strategy to Tackle Viral Outbreaks. In: Claborn D., editor. Current Perspectives on Viral Disease Outbreaks. IntechOpen; Rijeka, Croatia: 2021. [Google Scholar]
- 106.O’Neill L.A.J., Netea M.G. BCG-Induced Trained Immunity: Can It Offer Protection against COVID-19? Nat. Rev. Immunol. 2020;20:335–337. doi: 10.1038/s41577-020-0337-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Martín-Cruz L., Sevilla-Ortega C., Angelina A., Domínguez-Andrés J., Netea M.G., Subiza J.L., Palomares O. From Trained Immunity in Allergy to Trained Immunity-Based Allergen Vaccines. Clin. Exp. Allergy J. Br. Soc. Allergy Clin. Immunol. 2022;53:145–155. doi: 10.1111/cea.14261. [DOI] [PubMed] [Google Scholar]
- 108.Benito-Villalvilla C., Pérez-Diego M., Angelina A., Kisand K., Rebane A., Subiza J.L., Palomares O. Allergoid-Mannan Conjugates Reprogram Monocytes into Tolerogenic Dendritic Cells via Epigenetic and Metabolic Rewiring. J. Allergy Clin. Immunol. 2022;149:212–222.e9. doi: 10.1016/j.jaci.2021.06.012. [DOI] [PubMed] [Google Scholar]
- 109.Hartung F., Esser-von Bieren J. Trained Immunity in Type 2 Immune Responses. Mucosal Immunol. 2022;15:1158–1169. doi: 10.1038/s41385-022-00557-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ebihara T., Tatematsu M., Fuchimukai A., Yamada T., Yamagata K., Takasuga S., Yamada T. Trained Innate Lymphoid Cells in Allergic Diseases. Allergol. Int. Off. J. Japanese Soc. Allergol. 2021;70:174–180. doi: 10.1016/j.alit.2020.11.007. [DOI] [PubMed] [Google Scholar]
- 111.Eljaszewicz A., Ruchti F., Radzikowska U., Globinska A., Boonpiyathad T., Gschwend A., Morita H., Helbling A., Arasi S., Kahlert H., et al. Trained Immunity and Tolerance in Innate Lymphoid Cells, Monocytes, and Dendritic Cells during Allergen-Specific Immunotherapy. J. Allergy Clin. Immunol. 2021;147:1865–1877. doi: 10.1016/j.jaci.2020.08.042. [DOI] [PubMed] [Google Scholar]
- 112.Zheng D., Liwinski T., Elinav E. Interaction between Microbiota and Immunity in Health and Disease. Cell Res. 2020;30:492–506. doi: 10.1038/s41422-020-0332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Belkaid Y., Hand T.W. Role of the Microbiota in Immunity and Inflammation. Cell. 2014;157:121–141. doi: 10.1016/j.cell.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lasaviciute G., Barz M., van der Heiden M., Arasa C., Tariq K., Quin J., Östlund Farrants A.-K., Sverremark-Ekström E. Gut Commensal Limosilactobacillus Reuteri Induces Atypical Memory-like Phenotype in Human Dendritic Cells in Vitro. Gut Microbes. 2022;14:2045046. doi: 10.1080/19490976.2022.2045046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lajqi T., Köstlin-Gille N., Hillmer S., Braun M., Kranig S.A., Dietz S., Krause C., Rühle J., Frommhold D., Pöschl J., et al. Gut Microbiota-Derived Small Extracellular Vesicles Endorse Memory-like Inflammatory Responses in Murine Neutrophils. Biomedicines. 2022;10:442. doi: 10.3390/biomedicines10020442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dubrovsky L., Brichacek B., Prashant N.M., Pushkarsky T., Mukhamedova N., Fleetwood A.J., Xu Y., Dragoljevic D., Fitzgerald M., Horvath A., et al. Extracellular Vesicles Carrying HIV-1 Nef Induce Long-Term Hyperreactivity of Myeloid Cells. Cell Rep. 2022;41:111674. doi: 10.1016/j.celrep.2022.111674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.van Leent M.M.T., Priem B., Schrijver D.P., de Dreu A., Hofstraat S.R.J., Zwolsman R., Beldman T.J., Netea M.G., Mulder W.J.M. Regulating Trained Immunity with Nanomedicine. Nat. Rev. Mater. 2022;7:465–481. doi: 10.1038/s41578-021-00413-w. [DOI] [Google Scholar]
- 118.Kalafati L., Hatzioannou A., Hajishengallis G., Chavakis T. The Role of Neutrophils in Trained Immunity. Immunol. Rev. 2022 doi: 10.1111/imr.13142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bindu S., Dandapat S., Manikandan R., Dinesh M., Subbaiyan A., Mani P., Dhawan M., Tiwari R., Bilal M., Bin Emran T., et al. Prophylactic and Therapeutic Insights into Trained Immunity: A Renewed Concept of Innate Immune Memory. Hum. Vaccin. Immunother. 2022;18:2040238. doi: 10.1080/21645515.2022.2040238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Azimzadeh A.M., Pfeiffer S., Wu G.S., Schröder C., Zhou H., Zorn G.L., 3rd, Kehry M., Miller G.G., Rose M.L., Pierson R.N. 3rd. Humoral Immunity to Vimentin Is Associated with Cardiac Allograft Injury in Nonhuman Primates. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2005;5:2349–2359. doi: 10.1111/j.1600-6143.2005.01022.x. [DOI] [PubMed] [Google Scholar]
- 121.Huang Y., Yin H., Han J., Huang B., Xu J., Zheng F., Tan Z., Fang M., Rui L., Chen D., et al. Extracellular Hmgb1 Functions as an Innate Immune-Mediator Implicated in Murine Cardiac Allograft Acute Rejection. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2007;7:799–808. doi: 10.1111/j.1600-6143.2007.01734.x. [DOI] [PubMed] [Google Scholar]
- 122.Uhl B., Vadlau Y., Zuchtriegel G., Nekolla K., Sharaf K., Gaertner F., Massberg S., Krombach F., Reichel C.A. Aged Neutrophils Contribute to the First Line of Defense in the Acute Inflammatory Response. Blood. 2016;128:2327–2337. doi: 10.1182/blood-2016-05-718999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Christen T., Nahrendorf M., Wildgruber M., Swirski F.K., Aikawa E., Waterman P., Shimizu K., Weissleder R., Libby P. Molecular Imaging of Innate Immune Cell Function in Transplant Rejection. Circulation. 2009;119:1925–1932. doi: 10.1161/CIRCULATIONAHA.108.796888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Scozzi D., Ibrahim M., Menna C., Krupnick A.S., Kreisel D., Gelman A.E. The Role of Neutrophils in Transplanted Organs. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2017;17:328–335. doi: 10.1111/ajt.13940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bosmans J.L., Holvoet P., Dauwe S.E., Ysebaert D.K., Chapelle T., Jürgens A., Kovacic V., Van Marck E.A., De Broe M.E., Verpooten G.A. Oxidative Modification of Low-Density Lipoproteins and the Outcome of Renal Allografts at 1 1/2 Years. Kidney Int. 2001;59:2346–2356. doi: 10.1046/j.1523-1755.2001.00752.x. [DOI] [PubMed] [Google Scholar]
- 126.Agarwal A., Prasad G.V.R. Post-Transplant Dyslipidemia: Mechanisms, Diagnosis and Management. World J. Transplant. 2016;6:125–134. doi: 10.5500/wjt.v6.i1.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Regnström J., Nilsson J., Tornvall P., Landou C., Hamsten A. Susceptibility to Low-Density Lipoprotein Oxidation and Coronary Atherosclerosis in Man. Lancet. 1992;339:1183–1186. doi: 10.1016/0140-6736(92)91129-V. [DOI] [PubMed] [Google Scholar]
- 128.Samouilidou E.C., Karpouza A.P., Kostopoulos V., Bakirtzi T., Pantelias K., Petras D., Tzanatou-Exarchou H., Grapsa E.J. Lipid Abnormalities and Oxidized LDL in Chronic Kidney Disease Patients on Hemodialysis and Peritoneal Dialysis. Ren. Fail. 2012;34:160–164. doi: 10.3109/0886022X.2011.641515. [DOI] [PubMed] [Google Scholar]
- 129.Diepeveen S.H.A., Verhoeven G.H.W.E., van der Palen J., Dikkeschei B.L.D., van Tits L.J., Kolsters G., Offerman J.J.G., Bilo H.J.G., Stalenhoef A.F.H. Oxidative Stress in Patients with End-Stage Renal Disease Prior to the Start of Renal Replacement Therapy. Nephron. Clin. Pract. 2004;98:c3–c7. doi: 10.1159/000079921. [DOI] [PubMed] [Google Scholar]
- 130.Rogacev K.S., Seiler S., Zawada A.M., Reichart B., Herath E., Roth D., Ulrich C., Fliser D., Heine G.H. CD14++CD16+ Monocytes and Cardiovascular Outcome in Patients with Chronic Kidney Disease. Eur. Heart J. 2011;32:84–92. doi: 10.1093/eurheartj/ehq371. [DOI] [PubMed] [Google Scholar]
- 131.Pertosa G., Grandaliano G., Gesualdo L., Schena F.P. Clinical Relevance of Cytokine Production in Hemodialysis. Kidney Int. Suppl. 2000;76:S104–S111. doi: 10.1046/j.1523-1755.2000.07613.x. [DOI] [PubMed] [Google Scholar]
- 132.Bekkering S., Quintin J., Joosten L.A.B., Van Der Meer J.W.M., Netea M.G., Riksen N.P. Oxidized Low-Density Lipoprotein Induces Long-Term Proinflammatory Cytokine Production and Foam Cell Formation via Epigenetic Reprogramming of Monocytes. Arterioscler. Thromb. Vasc. Biol. 2014;34:1731–1738. doi: 10.1161/ATVBAHA.114.303887. [DOI] [PubMed] [Google Scholar]
- 133.Schnack L., Sohrabi Y., Lagache S.M.M., Kahles F., Bruemmer D., Waltenberger J., Findeisen H.M. Mechanisms of Trained Innate Immunity in OxLDL Primed Human Coronary Smooth Muscle Cells. Front. Immunol. 2019;10:13. doi: 10.3389/fimmu.2019.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kuo C.-F., Grainge M.J., Zhang W., Doherty M. Global Epidemiology of Gout: Prevalence, Incidence and Risk Factors. Nat. Rev. Rheumatol. 2015;11:649–662. doi: 10.1038/nrrheum.2015.91. [DOI] [PubMed] [Google Scholar]
- 135.Stamp L.K., Dalbeth N. Critical Appraisal of Serum Urate Targets in the Management of Gout. Nat. Rev. Rheumatol. 2022;18:603–609. doi: 10.1038/s41584-022-00816-1. [DOI] [PubMed] [Google Scholar]
- 136.Cabău G., Crișan T.O., Klück V., Popp R.A., Joosten L.A.B. Urate-Induced Immune Programming: Consequences for Gouty Arthritis and Hyperuricemia. Immunol. Rev. 2020;294:92–105. doi: 10.1111/imr.12833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Crișan T.O., Cleophas M.C.P., Oosting M., Lemmers H., Toenhake-Dijkstra H., Netea M.G., Jansen T.L., Joosten L.A.B. Soluble Uric Acid Primes TLR-Induced Proinflammatory Cytokine Production by Human Primary Cells via Inhibition of IL-1Ra. Ann. Rheum. Dis. 2016;75:755–762. doi: 10.1136/annrheumdis-2014-206564. [DOI] [PubMed] [Google Scholar]
- 138.Crişan T.O., Cleophas M.C.P., Novakovic B., Erler K., van de Veerdonk F.L., Stunnenberg H.G., Netea M.G., Dinarello C.A., Joosten L.A.B. Uric Acid Priming in Human Monocytes Is Driven by the AKT-PRAS40 Autophagy Pathway. Proc. Natl. Acad. Sci. USA. 2017;114:5485–5490. doi: 10.1073/pnas.1620910114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Chiabrando D., Vinchi F., Fiorito V., Mercurio S., Tolosano E. Heme in Pathophysiology: A Matter of Scavenging, Metabolism and Trafficking across Cell Membranes. Front. Pharmacol. 2014;5:61. doi: 10.3389/fphar.2014.00061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Jentho E., Ruiz-Moreno C., Novakovic B., Kourtzelis I., Megchelenbrink W.L., Martins R., Chavakis T., Soares M.P., Kalafati L., Guerra J., et al. Trained Innate Immunity, Long-Lasting Epigenetic Modulation, and Skewed Myelopoiesis by Heme. Proc. Natl. Acad. Sci. USA. 2021;118:e2102698118. doi: 10.1073/pnas.2102698118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Schlegel C., Liu K., Spring B., Dietz S., Poets C.F., Hudalla H., Lajqi T., Köstlin-Gille N., Gille C. Decreased Expression of Hypoxia-Inducible Factor 1α (HIF-1α) in Cord Blood Monocytes under Anoxia. Pediatr. Res. 2022;2022:1–8. doi: 10.1038/s41390-022-02193-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Cheng S.C., Quintin J., Cramer R.A., Shepardson K.M., Saeed S., Kumar V., Giamarellos-Bourboulis E.J., Martens J.H.A., Rao N.A., Aghajanirefah A., et al. MTOR- and HIF-1α-Mediated Aerobic Glycolysis as Metabolic Basis for Trained Immunity. Science. 2014;345:1250684. doi: 10.1126/science.1250684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Lajqi T., Lang G.-P., Haas F., Williams D.L., Hudalla H., Bauer M., Groth M., Wetzker R., Bauer R. Memory-Like Inflammatory Responses of Microglia to Rising Doses of LPS: Key Role of PI3Kγ. Front. Immunol. 2019;10:2492. doi: 10.3389/fimmu.2019.02492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Bhattarai S., Li Q., Ding J., Liang F., Gusev E., Lapohos O., Fonseca G.J., Kaufmann E., Divangahi M., Petrof B.J. TLR4 Is a Regulator of Trained Immunity in a Murine Model of Duchenne Muscular Dystrophy. Nat. Commun. 2022;13:879. doi: 10.1038/s41467-022-28531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lajqi T., Frommhold D., Braun M., Alexander Kranig S., Pöschl J., Hudalla H. Gram-Positive Staphylococcus Aureus LTA Promotes Distinct Memory-like Effects in Murine Bone Marrow Neutrophils. Cell. Immunol. 2022;376:104535. doi: 10.1016/j.cellimm.2022.104535. [DOI] [PubMed] [Google Scholar]
- 146.Feuerstein R., Forde A.J., Lohrmann F., Kolter J., Ramirez N.J., Zimmermann J., Gomez de Agüero M., Henneke P. Resident Macrophages Acquire Innate Immune Memory in Staphylococcal Skin Infection. Elife. 2020;9:e55602. doi: 10.7554/eLife.55602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Chan L.C., Rossetti M., Miller L.S., Filler S.G., Johnson C.W., Lee H.K., Wang H., Gjertson D., Fowler V.G.J., Reed E.F., et al. Protective Immunity in Recurrent Staphylococcus Aureus Infection Reflects Localized Immune Signatures and Macrophage-Conferred Memory. Proc. Natl. Acad. Sci. USA. 2018;115:E11111–E11119. doi: 10.1073/pnas.1808353115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Horn C.M., Kielian T. Crosstalk Between Staphylococcus Aureus and Innate Immunity: Focus on Immunometabolism. Front. Immunol. 2020;11:621750. doi: 10.3389/fimmu.2020.621750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Saeed S., Quintin J., Kerstens H.H.D., Rao N.A., Aghajanirefah A., Matarese F., Cheng S.-C., Ratter J., Berentsen K., van der Ent M.A., et al. Epigenetic Programming of Monocyte-to-Macrophage Differentiation and Trained Innate Immunity. Science. 2014;345:1251086. doi: 10.1126/science.1251086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mantovani A., Netea M.G. Trained Innate Immunity, Epigenetics, and Covid-19. N. Engl. J. Med. 2020;383:1078–1080. doi: 10.1056/NEJMcibr2011679. [DOI] [PubMed] [Google Scholar]
- 151.Rasid O., Chevalier C., Camarasa T.M.-N., Fitting C., Cavaillon J.-M., Hamon M.A. H3K4me1 Supports Memory-like NK Cells Induced by Systemic Inflammation. Cell Rep. 2019;29:3933–3945.e3. doi: 10.1016/j.celrep.2019.11.043. [DOI] [PubMed] [Google Scholar]
- 152.Yao Q., Chen Y., Zhou X. The Roles of MicroRNAs in Epigenetic Regulation. Curr. Opin. Chem. Biol. 2019;51:11–17. doi: 10.1016/j.cbpa.2019.01.024. [DOI] [PubMed] [Google Scholar]
- 153.Zawislak C.L., Beaulieu A.M., Loeb G.B., Karo J., Canner D., Bezman N.A., Lanier L.L., Rudensky A.Y., Sun J.C. Stage-Specific Regulation of Natural Killer Cell Homeostasis and Response against Viral Infection by MicroRNA-155. Proc. Natl. Acad. Sci. USA. 2013;110:6967–6972. doi: 10.1073/pnas.1304410110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zou L., He J., Gu L., Shahror R.A., Li Y., Cao T., Wang S., Zhu J., Huang H., Chen F., et al. Brain Innate Immune Response via MiRNA-TLR7 Sensing in Polymicrobial Sepsis. Brain. Behav. Immun. 2022;100:10–24. doi: 10.1016/j.bbi.2021.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Curtale G., Rubino M., Locati M. MicroRNAs as Molecular Switches in Macrophage Activation. Front. Immunol. 2019;10:799. doi: 10.3389/fimmu.2019.00799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Su H., Liang Z., Weng S., Sun C., Huang J., Zhang T., Wang X., Wu S., Zhang Z., Zhang Y., et al. MiR-9-5p Regulates Immunometabolic and Epigenetic Pathways in β-Glucan-Trained Immunity via IDH3α. JCI Insight. 2021;6:e144260. doi: 10.1172/jci.insight.144260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Saz-Leal P., Del Fresno C., Brandi P., Martínez-Cano S., Dungan O.M., Chisholm J.D., Kerr W.G., Sancho D. Targeting SHIP-1 in Myeloid Cells Enhances Trained Immunity and Boosts Response to Infection. Cell Rep. 2018;25:1118–1126. doi: 10.1016/j.celrep.2018.09.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Fanucchi S., Fok E.T., Dalla E., Shibayama Y., Börner K., Chang E.Y., Stoychev S., Imakaev M., Grimm D., Wang K.C., et al. Immune Genes Are Primed for Robust Transcription by Proximal Long Noncoding RNAs Located in Nuclear Compartments. Nat. Genet. 2019;51:138–150. doi: 10.1038/s41588-018-0298-2. [DOI] [PubMed] [Google Scholar]
- 159.Das J., Verma D., Gustafsson M., Lerm M. Identification of DNA Methylation Patterns Predisposing for an Efficient Response to BCG Vaccination in Healthy BCG-Naïve Subjects. Epigenetics. 2019;14:589–601. doi: 10.1080/15592294.2019.1603963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Ferreira A.V., Domiguéz-Andrés J., Netea M.G. The Role of Cell Metabolism in Innate Immune Memory. J. Innate Immun. 2021;13:194. doi: 10.1159/000512280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Riksen N.P., Netea M.G. Immunometabolic Control of Trained Immunity. Mol. Aspects Med. 2021;77:100897. doi: 10.1016/j.mam.2020.100897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Arts R.J.W., Joosten L.A.B., Netea M.G. Immunometabolic Circuits in Trained Immunity. Semin. Immunol. 2016;28:425–430. doi: 10.1016/j.smim.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 163.Groh L.A., Ferreira A.V., Helder L., van der Heijden C.D.C.C., Novakovic B., van de Westerlo E., Matzaraki V., Moorlag S.J.C.F.M., de Bree L.C., Koeken V.A.C.M., et al. OxLDL-Induced Trained Immunity Is Dependent on Mitochondrial Metabolic Reprogramming. Immunometabolism. 2021;3:e210025. doi: 10.20900/immunometab20210025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Keating S.T., Groh L., van der Heijden C.D.C.C., Rodriguez H., Dos Santos J.C., Fanucchi S., Okabe J., Kaipananickal H., van Puffelen J.H., Helder L., et al. The Set7 Lysine Methyltransferase Regulates Plasticity in Oxidative Phosphorylation Necessary for Trained Immunity Induced by β-Glucan. Cell Rep. 2020;31:107548. doi: 10.1016/j.celrep.2020.107548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Koeken V.A.C.M., Qi C., Mourits V.P., de Bree L.C.J., Moorlag S.J.C.F.M., Sonawane V., Lemmers H., Dijkstra H., Joosten L.A.B., van Laarhoven A., et al. Plasma Metabolome Predicts Trained Immunity Responses after Antituberculosis BCG Vaccination. PLoS Biol. 2022;20:e3001765. doi: 10.1371/journal.pbio.3001765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Lajqi T., Marx C., Hudalla H., Haas F., Große S., Wang Z.Q., Heller R., Bauer M., Wetzker R., Bauer R. The Role of the Pathogen Dose and PI3Kγ in Immunometabolic Reprogramming of Microglia for Innate Immune Memory. Int. J. Mol. Sci. 2021;22:2578. doi: 10.3390/ijms22052578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Arts R.J.W., Novakovic B., ter Horst R., Carvalho A., Bekkering S., Lachmandas E., Rodrigues F., Silvestre R., Cheng S.C., Wang S.Y., et al. Glutaminolysis and Fumarate Accumulation Integrate Immunometabolic and Epigenetic Programs in Trained Immunity. Cell Metab. 2016;24:807–819. doi: 10.1016/j.cmet.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Pérez-Hernández C.A., Kern C.C., Butkeviciute E., McCarthy E., Dockrell H.M., Moreno-Altamirano M.M.B., Aguilar-López B.A., Bhosale G., Wang H., Gems D., et al. Mitochondrial Signature in Human Monocytes and Resistance to Infection in C. Elegans During Fumarate-Induced Innate Immune Training. Front. Immunol. 2020;11:1715. doi: 10.3389/fimmu.2020.01715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Bekkering S., Arts R.J.W., Novakovic B., Kourtzelis I., van der Heijden C.D.C.C., Li Y., Popa C.D., ter Horst R., van Tuijl J., Netea-Maier R.T., et al. Metabolic Induction of Trained Immunity through the Mevalonate Pathway. Cell. 2018;172:135–146.e9. doi: 10.1016/j.cell.2017.11.025. [DOI] [PubMed] [Google Scholar]
- 170.Ferreira A.V., Koeken V.A.C.M., Matzaraki V., Kostidis S., Alarcon-Barrera J.C., de Bree L.C.J., Moorlag S.J.C.F.M., Mourits V.P., Novakovic B., Giera M.A., et al. Glutathione Metabolism Contributes to the Induction of Trained Immunity. Cells. 2021;10:971. doi: 10.3390/cells10050971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Arts R.J.W., Carvalho A., La Rocca C., Palma C., Rodrigues F., Silvestre R., Kleinnijenhuis J., Lachmandas E., Gonçalves L.G., Belinha A., et al. Immunometabolic Pathways in BCG-Induced Trained Immunity. Cell Rep. 2016;17:2562–2571. doi: 10.1016/j.celrep.2016.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Vrieling F., van Dierendonck X.A.M.H., Jaeger M., Janssen A.W.M., Hijmans A., Netea M.G., Tack C.J., Stienstra R. Glycolytic Activity in Human Immune Cells: Inter-Individual Variation and Functional Implications during Health and Diabetes. Immunometabolism. 2022;4:e00008. doi: 10.1097/IN9.0000000000000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Soehnlein O., Lindbom L. Phagocyte Partnership during the Onset and Resolution of Inflammation. Nat. Rev. Immunol. 2010;10:427–439. doi: 10.1038/nri2779. [DOI] [PubMed] [Google Scholar]
- 174.Gordon S. Phagocytosis: An Immunobiologic Process. Immunity. 2016;44:463–475. doi: 10.1016/j.immuni.2016.02.026. [DOI] [PubMed] [Google Scholar]
- 175.Fu R., Shen Q., Xu P., Luo J.J., Tang Y. Phagocytosis of Microglia in the Central Nervous System Diseases. Mol. Neurobiol. 2014;49:1422–1434. doi: 10.1007/s12035-013-8620-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Domínguez-Andrés J., Dos Santos J.C., Bekkering S., Mulder W.J.M., van der Meer J.W.M., Riksen N.P., Joosten L.A.B., Netea M.G. Trained Immunity: Adaptation within Innate Immune Mechanisms. Physiol. Rev. 2023;103:313–346. doi: 10.1152/physrev.00031.2021. [DOI] [PubMed] [Google Scholar]
- 177.Moorlag S.J.C.F.M., Rodriguez-Rosales Y.A., Gillard J., Fanucchi S., Theunissen K., Novakovic B., de Bont C.M., Negishi Y., Fok E.T., Kalafati L., et al. BCG Vaccination Induces Long-Term Functional Reprogramming of Human Neutrophils. Cell Rep. 2020;33:108387. doi: 10.1016/j.celrep.2020.108387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Bickett T.E., McLean J., Creissen E., Izzo L., Hagan C., Izzo A.J., Silva Angulo F., Izzo A.A. Characterizing the BCG Induced Macrophage and Neutrophil Mechanisms for Defense Against Mycobacterium Tuberculosis. Front. Immunol. 2020;11:1202. doi: 10.3389/fimmu.2020.01202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Schaafsma W., Zhang X., van Zomeren K.C., Jacobs S., Georgieva P.B., Wolf S.A., Kettenmann H., Janova H., Saiepour N., Hanisch U.K., et al. Long-Lasting pro-Inflammatory Suppression of Microglia by LPS-Preconditioning Is Mediated by RelB-Dependent Epigenetic Silencing. Brain. Behav. Immun. 2015;48:205–221. doi: 10.1016/j.bbi.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 180.Lajqi T., Stojiljkovic M., Williams D.L., Hudalla H., Bauer M., Witte O.W., Wetzker R., Bauer R., Schmeer C. Memory-Like Responses of Brain Microglia Are Controlled by Developmental State and Pathogen Dose. Front. Immunol. 2020;11:546415. doi: 10.3389/fimmu.2020.546415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Funes S.C., Rios M., Fernández-Fierro A., Di Genaro M.S., Kalergis A.M. Trained Immunity Contribution to Autoimmune and Inflammatory Disorders. Front. Immunol. 2022;13:868343. doi: 10.3389/fimmu.2022.868343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Katzmarski N., Domínguez-Andrés J., Cirovic B., Renieris G., Ciarlo E., Le Roy D., Lepikhov K., Kattler K., Gasparoni G., Händler K., et al. Transmission of Trained Immunity and Heterologous Resistance to Infections across Generations. Nat. Immunol. 2021;22:1382–1390. doi: 10.1038/s41590-021-01052-7. [DOI] [PubMed] [Google Scholar]
- 183.Kaufmann E., Landekic M., Downey J., Chronopoulos J., Teimouri Nezhad S., Tran K., Vinh D.C., Barreiro L.B., Divangahi M. Lack of Evidence for Intergenerational Inheritance of Immune Resistance to Infections. Nat. Immunol. 2022;23:203–207. doi: 10.1038/s41590-021-01102-0. [DOI] [PubMed] [Google Scholar]
- 184.Katzmarski N., Domínguez-Andrés J., Cirovic B., Renieris G., Ciarlo E., Le Roy D., Lepikhov K., Kattler K., Gasparoni G., Händler K., et al. Reply to: “Lack of Evidence for Intergenerational Inheritance of Immune Resistance to Infections”. Nat. Immunol. 2022;23:208–209. doi: 10.1038/s41590-021-01103-z. [DOI] [PubMed] [Google Scholar]
- 185.Calabrese E.J., Baldwin L.A. Defining Hormesis. Hum. Exp. Toxicol. 2002;21:91–97. doi: 10.1191/0960327102ht217oa. [DOI] [PubMed] [Google Scholar]
- 186.Calabrese E.J., Mattson M.P. How Does Hormesis Impact Biology, Toxicology, and Medicine? NPJ Aging Mech. Dis. 2017;3:13. doi: 10.1038/s41514-017-0013-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Lajqi T., Stojiljkovic M., Wetzker R. Toxin-Induced Hormesis May Restrain Aging. Biogerontology. 2019;20:571–581. doi: 10.1007/s10522-019-09806-5. [DOI] [PubMed] [Google Scholar]
- 188.Leak R.K., Calabrese E.J., Kozumbo W.J., Gidday J.M., Johnson T.E., Mitchell J.R., Ozaki C.K., Wetzker R., Bast A., Belz R.G., et al. Enhancing and Extending Biological Performance and Resilience. Dose Response. 2018;16:1559325818784501. doi: 10.1177/1559325818784501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Gifford G.E., Lohmann-Matthes M.L. Gamma Interferon Priming of Mouse and Human Macrophages for Induction of Tumor Necrosis Factor Production by Bacterial Lipopolysaccharide. J. Natl. Cancer Inst. 1987;78:121–124. doi: 10.1093/jnci/78.1.121. [DOI] [PubMed] [Google Scholar]
- 190.Koerner T.J., Adams D.O., Hamilton T.A. Regulation of Tumor Necrosis Factor (TNF) Expression: Interferon-Gamma Enhances the Accumulation of MRNA for TNF Induced by Lipopolysaccharide in Murine Peritoneal Macrophages. Cell. Immunol. 1987;109:437–443. doi: 10.1016/0008-8749(87)90326-1. [DOI] [PubMed] [Google Scholar]
- 191.Hayes M.P., Zoon K.C. Priming of Human Monocytes for Enhanced Lipopolysaccharide Responses: Expression of Alpha Interferon, Interferon Regulatory Factors, and Tumor Necrosis Factor. Infect. Immun. 1993;61:3222–3227. doi: 10.1128/iai.61.8.3222-3227.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Hayes M.P., Freeman S.L., Donnelly R.P. IFN-Gamma Priming of Monocytes Enhances LPS-Induced TNF Production by Augmenting Both Transcription and MRNA Stability. Cytokine. 1995;7:427–435. doi: 10.1006/cyto.1995.0058. [DOI] [PubMed] [Google Scholar]
- 193.Garza-Lombó C., Schroder A., Reyes-Reyes E.M., Franco R. MTOR/AMPK Signaling in the Brain: Cell Metabolism, Proteostasis and Survival. Curr. Opin. Toxicol. 2018;8:102–110. doi: 10.1016/j.cotox.2018.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.González A., Hall M.N., Lin S.-C., Hardie D.G. AMPK and TOR: The Yin and Yang of Cellular Nutrient Sensing and Growth Control. Cell Metab. 2020;31:472–492. doi: 10.1016/j.cmet.2020.01.015. [DOI] [PubMed] [Google Scholar]
- 195.Herzig S., Shaw R.J. AMPK: Guardian of Metabolism and Mitochondrial Homeostasis. Nat. Rev. Mol. Cell Biol. 2018;19:121–135. doi: 10.1038/nrm.2017.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Soares M.P., Gozzelino R., Weis S. Tissue Damage Control in Disease Tolerance. Trends Immunol. 2014;35:483–494. doi: 10.1016/j.it.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 197.Kim J., Kwak H.J., Cha J.Y., Jeong Y.S., Rhee S.D., Kim K.R., Cheon H.G. Metformin Suppresses Lipopolysaccharide (LPS)-Induced Inflammatory Response in Murine Macrophages via Activating Transcription Factor-3 (ATF-3) Induction. J. Biol. Chem. 2014;289:23246–23255. doi: 10.1074/jbc.M114.577908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Weichhart T., Hengstschlager M., Linke M. Regulation of Innate Immune Cell Function by MTOR. Nat. Rev. Immunol. 2015;15:599–614. doi: 10.1038/nri3901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Reiling J.H., Sabatini D.M. Stress and MTORture Signaling. Oncogene. 2006;25:6373–6383. doi: 10.1038/sj.onc.1209889. [DOI] [PubMed] [Google Scholar]
- 200.Jeon S.-M.M. Regulation and Function of AMPK in Physiology and Diseases. Exp. Mol. Med. 2016;48:e245. doi: 10.1038/emm.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Chen K., Geng S., Yuan R., Diao N., Upchurch Z., Li L. Super-Low Dose Endotoxin Pre-Conditioning Exacerbates Sepsis Mortality. EBioMedicine. 2015;2:324–333. doi: 10.1016/j.ebiom.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Yuan R., Geng S., Li L. Molecular Mechanisms That Underlie the Dynamic Adaptation of Innate Monocyte Memory to Varying Stimulant Strength of TLR Ligands. Front. Immunol. 2016;7:497. doi: 10.3389/fimmu.2016.00497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Rahtes A., Li L. Polarization of Low-Grade Inflammatory Monocytes Through TRAM-Mediated Up-Regulation of Keap1 by Super-Low Dose Endotoxin. Front. Immunol. 2020;11:1478. doi: 10.3389/fimmu.2020.01478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Deng H., Maitra U., Morris M., Li L. Molecular Mechanism Responsible for the Priming of Macrophage Activation. J. Biol. Chem. 2013;288:3897–3906. doi: 10.1074/jbc.M112.424390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Maitra U., Deng H., Glaros T., Baker B., Capelluto D.G.S., Li Z., Li L. Molecular Mechanisms Responsible for the Selective and Low-Grade Induction of Proinflammatory Mediators in Murine Macrophages by Lipopolysaccharide. J. Immunol. 2012;189:1014–1023. doi: 10.4049/jimmunol.1200857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Lajqi T., Braun M., Kranig S.A., Frommhold D., Johannes P., Hudalla H. LPS Induces Opposing Memory-like Inflammatory Responses in Mouse Bone Marrow Neutrophils. Int. J. Mol. Sci. 2021;22:9803. doi: 10.3390/ijms22189803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Morris M.C., Gilliam E.A., Button J., Li L. Dynamic Modulation of Innate Immune Response by Varying Dosages of Lipopolysaccharide (LPS) in Human Monocytic Cells. J. Biol. Chem. 2014;289:21584–21590. doi: 10.1074/jbc.M114.583518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Zhou X.Y., Gao R., Hu J., Gao D.P., Liao Y.L., Yang J.J. Trained Innate Immunity by Repeated Low-Dose Lipopolysaccharide Injections Displays Long-Term Neuroprotective Effects. Mediat. Inflamm. 2020;2020:8191079. doi: 10.1155/2020/8191079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Heng Y., Zhang X., Borggrewe M., van Weering H.R.J., Brummer M.L., Nijboer T.W., Joosten L.A.B., Netea M.G., Boddeke E.W.G.M., Laman J.D., et al. Systemic Administration of β-Glucan Induces Immune Training in Microglia. J. Neuroinflammation. 2021;18:57. doi: 10.1186/s12974-021-02103-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Zhang X., Kracht L., Lerario A.M., Dubbelaar M.L., Brouwer N., Wesseling E.M., Boddeke E.W.G.M., Eggen B.J.L., Kooistra S.M. Epigenetic Regulation of Innate Immune Memory in Microglia. J. Neuroinflammation. 2022;19:111. doi: 10.1186/s12974-022-02463-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Grondman I., Arts R.J.W., Koch R.M., Leijte G.P., Gerretsen J., Bruse N., Kempkes R.W.M., Ter Horst R., Kox M., Pickkers P., et al. Frontline Science: Endotoxin-Induced Immunotolerance Is Associated with Loss of Monocyte Metabolic Plasticity and Reduction of Oxidative Burst. J. Leukoc. Biol. 2019;106:11–25. doi: 10.1002/JLB.5HI0119-018R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Hill A.W., Shears A.L., Hibbitt K.G. Increased Antibacterial Activity against Escherichia Coli in Bovine Serum after the Induction of Endotoxin Tolerance. Infect. Immun. 1976;14:257–265. doi: 10.1128/iai.14.1.257-265.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Wheeler D.S., Lahni P.M., Denenberg A.G., Poynter S.E., Wong H.R., Cook J.A., Zingarelli B. Induction of Endotoxin Tolerance Enhances Bacterial Clearance and Survival in Murine Polymicrobial Sepsis. Shock. 2008;30:267–273. doi: 10.1097/SHK.0b013e318162c190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Lehner M.D., Ittner J., Bundschuh D.S., Van Rooijen N., Wendel A., Hartung T. Improved Innate Immunity of Endotoxin-Tolerant Mice Increases Resistance to Salmonella Enterica Serovar Typhimurium Infection despite Attenuated Cytokine Response Improved Innate Immunity of Endotoxin-Tolerant Mice Increases Resistance to Salmonella Enter. Infect. Immun. 2001;69:463–471. doi: 10.1128/IAI.69.1.463-471.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Kim H.-D., Kim S.Y., Kim J., Kim J.E., Hong Y.S., Han B., Tak E., Ryu Y.-M., Kim S.-Y., Kim T.W. Dynamic Increase of M2 Macrophages Is Associated with Disease Progression of Colorectal Cancers Following Cetuximab-Based Treatment. Sci. Rep. 2022;12:1678. doi: 10.1038/s41598-022-05694-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Duan Z., Luo Y. Targeting Macrophages in Cancer Immunotherapy. Signal Transduct. Target. Ther. 2021;6:127. doi: 10.1038/s41392-021-00506-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Mantovani A., Allavena P., Marchesi F., Garlanda C. Macrophages as Tools and Targets in Cancer Therapy. Nat. Rev. Drug Discov. 2022;21:799–820. doi: 10.1038/s41573-022-00520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Genard G., Lucas S., Michiels C. Reprogramming of Tumor-Associated Macrophages with Anticancer Therapies: Radiotherapy versus Chemo- and Immunotherapies. Front. Immunol. 2017;8:828. doi: 10.3389/fimmu.2017.00828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Montecino-Rodriguez E., Berent-Maoz B., Dorshkind K. Causes, Consequences, and Reversal of Immune System Aging. J. Clin. Investig. 2013;123:958–965. doi: 10.1172/JCI64096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Mogilenko D.A., Shchukina I., Artyomov M.N. Immune Ageing at Single-Cell Resolution. Nat. Rev. Immunol. 2022;22:484–498. doi: 10.1038/s41577-021-00646-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Niraula A., Sheridan J.F., Godbout J.P. Microglia Priming with Aging and Stress. Neuropsychopharmacology. 2017;42:318–333. doi: 10.1038/npp.2016.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Bulut O., Kilic G., Domínguez-Andrés J. Immune Memory in Aging: A Wide Perspective Covering Microbiota, Brain, Metabolism, and Epigenetics. Clin. Rev. Allergy Immunol. 2022;63:499–529. doi: 10.1007/s12016-021-08905-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Chambers E.S., Vukmanovic-Stejic M., Shih B.B., Trahair H., Subramanian P., Devine O.P., Glanville J., Gilroy D., Rustin M.H.A., Freeman T.C., et al. Recruitment of Inflammatory Monocytes by Senescent Fibroblasts Inhibits Antigen-Specific Tissue Immunity during Human Aging. Nat. Aging. 2021;1:101–113. doi: 10.1038/s43587-020-00010-6. [DOI] [PubMed] [Google Scholar]
- 224.Kasler H., Verdin E. How Inflammaging Diminishes Adaptive Immunity. Nat. Aging. 2021;1:24–25. doi: 10.1038/s43587-020-00021-3. [DOI] [PubMed] [Google Scholar]
- 225.Gill P.S., Ozment T.R., Lewis N.H., Sherwood E.R., Williams D.L. Trained Immunity Enhances Human Monocyte Function in Aging and Sepsis. Front. Immunol. 2022;13:872652. doi: 10.3389/fimmu.2022.872652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Funder J.W. Mineralocorticoid Receptors: Distribution and Activation. Heart Fail. Rev. 2005;10:15–22. doi: 10.1007/s10741-005-2344-2. [DOI] [PubMed] [Google Scholar]
- 227.Zhong C., Yang X., Feng Y., Yu J. Trained Immunity: An Underlying Driver of Inflammatory Atherosclerosis. Front. Immunol. 2020;11:284. doi: 10.3389/fimmu.2020.00284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Moore K.J., Tabas I. Macrophages in the Pathogenesis of Atherosclerosis. Cell. 2011;145:341–355. doi: 10.1016/j.cell.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Barrett T.J. Macrophages in Atherosclerosis Regression. Arterioscler. Thromb. Vasc. Biol. 2020;40:20–33. doi: 10.1161/ATVBAHA.119.312802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Shepherd R., Cheung A.S., Pang K., Saffery R., Novakovic B. Sexual Dimorphism in Innate Immunity: The Role of Sex Hormones and Epigenetics. Front. Immunol. 2020;11:604000. doi: 10.3389/fimmu.2020.604000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Acevedo O.A., Berrios R.V., Rodríguez-Guilarte L., Lillo-Dapremont B., Kalergis A.M. Molecular and Cellular Mechanisms Modulating Trained Immunity by Various Cell Types in Response to Pathogen Encounter. Front. Immunol. 2021;12:745332. doi: 10.3389/fimmu.2021.745332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.D’Avila H., Roque N.R., Cardoso R.M., Castro-Faria-Neto H.C., Melo R.C.N., Bozza P.T. Neutrophils Recruited to the Site of Mycobacterium Bovis BCG Infection Undergo Apoptosis and Modulate Lipid Body Biogenesis and Prostaglandin E Production by Macrophages. Cell. Microbiol. 2008;10:2589–2604. doi: 10.1111/j.1462-5822.2008.01233.x. [DOI] [PubMed] [Google Scholar]
- 233.Christ A., Lauterbach M., Latz E. Western Diet and the Immune System: An Inflammatory Connection. Immunity. 2019;51:794–811. doi: 10.1016/j.immuni.2019.09.020. [DOI] [PubMed] [Google Scholar]
- 234.Spadaro O., Youm Y., Shchukina I., Ryu S., Sidorov S., Ravussin A., Nguyen K., Aladyeva E., Predeus A.N., Smith S.R., et al. Caloric Restriction in Humans Reveals Immunometabolic Regulators of Health Span. Science. 2022;375:671–677. doi: 10.1126/science.abg7292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Meydani S.N., Das S.K., Pieper C.F., Lewis M.R., Klein S., Dixit V.D., Gupta A.K., Villareal D.T., Bhapkar M., Huang M., et al. Long-Term Moderate Calorie Restriction Inhibits Inflammation without Impairing Cell-Mediated Immunity: A Randomized Controlled Trial in Non-Obese Humans. Aging. 2016;8:1416–1431. doi: 10.18632/aging.100994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Ma S., Sun S., Geng L., Song M., Wang W., Ye Y., Ji Q., Zou Z., Wang S., He X., et al. Caloric Restriction Reprograms the Single-Cell Transcriptional Landscape of Rattus Norvegicus Aging. Cell. 2020;180:984–1001.e22. doi: 10.1016/j.cell.2020.02.008. [DOI] [PubMed] [Google Scholar]
- 237.Christ A., Günther P., Lauterbach M.A.R., Duewell P., Biswas D., Pelka K., Scholz C.J., Oosting M., Haendler K., Baßler K., et al. Western Diet Triggers NLRP3-Dependent Innate Immune Reprogramming. Cell. 2018;172:162–175.e14. doi: 10.1016/j.cell.2017.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Seufert A.L., Hickman J.W., Traxler S.K., Peterson R.M., Waugh T.A., Lashley S.J., Shulzhenko N., Napier R.J., Napier B.A. Enriched Dietary Saturated Fatty Acids Induce Trained Immunity via Ceramide Production That Enhances Severity of Endotoxemia and Clearance of Infection. Elife. 2022;11:e76744. doi: 10.7554/eLife.76744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.van Splunter M., van Osch T.L.J., Brugman S., Savelkoul H.F.J., Joosten L.A.B., Netea M.G., van Neerven R.J.J. Induction of Trained Innate Immunity in Human Monocytes by Bovine Milk and Milk-Derived Immunoglobulin G. Nutrients. 2018;10:1378. doi: 10.3390/nu10101378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Beeson P.B. Tolerance to Bacterial Pyrogens: I. Factors Influencing Its Development. J. Exp. Med. 1947;86:29–38. doi: 10.1084/jem.86.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Szabó C., Thiemermann C., Wu C.C., Perretti M., Vane J.R. Attenuation of the Induction of Nitric Oxide Synthase by Endogenous Glucocorticoids Accounts for Endotoxin Tolerance in Vivo. Proc. Natl. Acad. Sci. USA. 1994;91:271–275. doi: 10.1073/pnas.91.1.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Hesse M., Modolell M., La Flamme A.C., Schito M., Fuentes J.M., Cheever A.W., Pearce E.J., Wynn T.A. Differential Regulation of Nitric Oxide Synthase-2 and Arginase-1 by Type 1/Type 2 Cytokines in Vivo: Granulomatous Pathology Is Shaped by the Pattern of L-Arginine Metabolism. J. Immunol. 2001;167:6533–6544. doi: 10.4049/jimmunol.167.11.6533. [DOI] [PubMed] [Google Scholar]
- 243.Suwanpradid J., Shih M., Pontius L., Yang B., Birukova A., Guttman-Yassky E., Corcoran D.L., Que L.G., Tighe R.M., MacLeod A.S. Arginase1 Deficiency in Monocytes/Macrophages Upregulates Inducible Nitric Oxide Synthase To Promote Cutaneous Contact Hypersensitivity. J. Immunol. 2017;199:1827–1834. doi: 10.4049/jimmunol.1700739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Xu H., Chen J., Si X., Chen M., Pei F., Qiu C., Wu J., Guan X. PKR Inhibition Mediates Endotoxin Tolerance in Macrophages through Inactivation of PI3K/AKT Signaling. Mol. Med. Rep. 2018;17:8548–8556. doi: 10.3892/mmr.2018.8869. [DOI] [PubMed] [Google Scholar]
- 245.Beutler B. SHIP, TGF-Beta, and Endotoxin Tolerance. Immunity. 2004;21:134–135. doi: 10.1016/j.immuni.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 246.Biswas S.K., Bist P., Dhillon M.K., Kajiji T., Del Fresno C., Yamamoto M., Lopez-Collazo E., Akira S., Tergaonkar V. Role for MyD88-Independent, TRIF Pathway in Lipid A/TLR4-Induced Endotoxin Tolerance. J. Immunol. 2007;179:4083–4092. doi: 10.4049/jimmunol.179.6.4083. [DOI] [PubMed] [Google Scholar]
- 247.Biswas S.K., Tergaonkar V. Myeloid Differentiation Factor 88-Independent Toll-like Receptor Pathway: Sustaining Inflammation or Promoting Tolerance? Int. J. Biochem. Cell Biol. 2007;39:1582–1592. doi: 10.1016/j.biocel.2007.04.021. [DOI] [PubMed] [Google Scholar]
- 248.Medvedev A.E., Kopydlowski K.M., Vogel S.N. Inhibition of Lipopolysaccharide-Induced Signal Transduction in Endotoxin-Tolerized Mouse Macrophages: Dysregulation of Cytokine, Chemokine, and Toll-like Receptor 2 and 4 Gene Expression. J. Immunol. 2000;164:5564–5574. doi: 10.4049/jimmunol.164.11.5564. [DOI] [PubMed] [Google Scholar]
- 249.Vergadi E., Vaporidi K., Tsatsanis C. Regulation of Endotoxin Tolerance and Compensatory Anti-Inflammatory Response Syndrome by Non-Coding RNAs. Front. Immunol. 2018;9:2705. doi: 10.3389/fimmu.2018.02705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Chu C.-H., Wang S., Li C.-L., Chen S.-H., Hu C.-F., Chung Y.-L., Chen S.-L., Wang Q., Lu R.-B., Gao H.-M., et al. Neurons and Astroglia Govern Microglial Endotoxin Tolerance through Macrophage Colony-Stimulating Factor Receptor-Mediated ERK1/2 Signals. Brain. Behav. Immun. 2016;55:260–272. doi: 10.1016/j.bbi.2016.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Andrade M.M.C., Ariga S.S.K., Barbeiro D.F., Barbeiro H.V., Pimentel R.N., Petroni R.C., Soriano F.G. Endotoxin Tolerance Modulates TREG and TH17 Lymphocytes Protecting Septic Mice. Oncotarget. 2019;10:3451–3461. doi: 10.18632/oncotarget.26919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Ogawa H., Rafiee P., Heidemann J., Fisher P.J., Johnson N.A., Otterson M.F., Kalyanaraman B., Pritchard K.A.J., Binion D.G. Mechanisms of Endotoxin Tolerance in Human Intestinal Microvascular Endothelial Cells. J. Immunol. 2003;170:5956–5964. doi: 10.4049/jimmunol.170.12.5956. [DOI] [PubMed] [Google Scholar]
- 253.Cavaillon J.M. The Nonspecific Nature of Endotoxin Tolerance. Trends Microbiol. 1995;3:320–324. doi: 10.1016/S0966-842X(00)88963-5. [DOI] [PubMed] [Google Scholar]
- 254.Sly L.M., Rauh M.J., Kalesnikoff J., Song C.H., Krystal G. LPS-Induced Upregulation of SHIP Is Essential for Endotoxin Tolerance. Immunity. 2004;21:227–239. doi: 10.1016/j.immuni.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 255.Chang J., Kunkel S.L., Chang C.-H. Negative Regulation of MyD88-Dependent Signaling by IL-10 in Dendritic Cells. Proc. Natl. Acad. Sci. USA. 2009;106:18327–18332. doi: 10.1073/pnas.0905815106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Gómez-Piña V., Martínez E., Fernández-Ruíz I., Del Fresno C., Soares-Schanoski A., Jurado T., Siliceo M., Toledano V., Fernández-Palomares R., García-Rio F., et al. Role of MMPs in Orchestrating Inflammatory Response in Human Monocytes via a TREM-1-PI3K-NF-ΚB Pathway. J. Leukoc. Biol. 2012;91:933–945. doi: 10.1189/jlb.0711340. [DOI] [PubMed] [Google Scholar]
- 257.Arts R.J.W., Joosten L.A.B., van der Meer J.W.M., Netea M.G. TREM-1: Intracellular Signaling Pathways and Interaction with Pattern Recognition Receptors. J. Leukoc. Biol. 2013;93:209–215. doi: 10.1189/jlb.0312145. [DOI] [PubMed] [Google Scholar]
- 258.Kobayashi K., Hernandez L.D., Galán J.E., Janeway C.A.J., Medzhitov R., Flavell R.A. IRAK-M Is a Negative Regulator of Toll-like Receptor Signaling. Cell. 2002;110:191–202. doi: 10.1016/S0092-8674(02)00827-9. [DOI] [PubMed] [Google Scholar]
- 259.Kinjyo I., Hanada T., Inagaki-Ohara K., Mori H., Aki D., Ohishi M., Yoshida H., Kubo M., Yoshimura A. SOCS1/JAB Is a Negative Regulator of LPS-Induced Macrophage Activation. Immunity. 2002;17:583–591. doi: 10.1016/S1074-7613(02)00446-6. [DOI] [PubMed] [Google Scholar]
- 260.Xiong Y., Medvedev A.E. Induction of Endotoxin Tolerance in Vivo Inhibits Activation of IRAK4 and Increases Negative Regulators IRAK-M, SHIP-1, and A20. J. Leukoc. Biol. 2011;90:1141–1148. doi: 10.1189/jlb.0611273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Chang E.Y., Guo B., Doyle S.E., Cheng G. Cutting Edge: Involvement of the Type I IFN Production and Signaling Pathway in Lipopolysaccharide-Induced IL-10 Production. J. Immunol. 2007;178:6705–6709. doi: 10.4049/jimmunol.178.11.6705. [DOI] [PubMed] [Google Scholar]
- 262.O’Neill L.A.J., Hardie D.G. Metabolism of Inflammation Limited by AMPK and Pseudo-Starvation. Nature. 2013;493:346–355. doi: 10.1038/nature11862. [DOI] [PubMed] [Google Scholar]
- 263.Wilson A.G. Epigenetic Regulation of Gene Expression in the Inflammatory Response and Relevance to Common Diseases. J. Periodontol. 2008;79:1514–1519. doi: 10.1902/jop.2008.080172. [DOI] [PubMed] [Google Scholar]
- 264.El Gazzar M., Yoza B.K., Chen X., Garcia B.A., Young N.L., McCall C.E. Chromatin-Specific Remodeling by HMGB1 and Linker Histone H1 Silences Proinflammatory Genes during Endotoxin Tolerance. Mol. Cell. Biol. 2009;29:1959–1971. doi: 10.1128/MCB.01862-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Nahid M.A., Satoh M., Chan E.K. MicroRNA in TLR Signaling and Endotoxin Tolerance. Cell. Mol. Immunol. 2011;8:388–403. doi: 10.1038/cmi.2011.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Quinn E.M., Wang J., Redmond H.P. The Emerging Role of MicroRNA in Regulation of Endotoxin Tolerance. J. Leukoc. Biol. 2012;91:721–727. doi: 10.1189/jlb.1111571. [DOI] [PubMed] [Google Scholar]
- 267.Baltimore D., Boldin M.P., O’Connell R.M., Rao D.S., Taganov K.D. MicroRNAs: New Regulators of Immune Cell Development and Function. Nat. Immunol. 2008;9:839–845. doi: 10.1038/ni.f.209. [DOI] [PubMed] [Google Scholar]
- 268.Taganov K.D., Boldin M.P., Chang K.-J., Baltimore D. NF-KappaB-Dependent Induction of MicroRNA MiR-146, an Inhibitor Targeted to Signaling Proteins of Innate Immune Responses. Proc. Natl. Acad. Sci. USA. 2006;103:12481–12486. doi: 10.1073/pnas.0605298103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Tili E., Michaille J.-J., Cimino A., Costinean S., Dumitru C.D., Adair B., Fabbri M., Alder H., Liu C.G., Calin G.A., et al. Modulation of MiR-155 and MiR-125b Levels Following Lipopolysaccharide/TNF-Alpha Stimulation and Their Possible Roles in Regulating the Response to Endotoxin Shock. J. Immunol. 2007;179:5082–5089. doi: 10.4049/jimmunol.179.8.5082. [DOI] [PubMed] [Google Scholar]
- 270.Chen X.-M., Splinter P.L., O’Hara S.P., LaRusso N.F. A Cellular Micro-RNA, Let-7i, Regulates Toll-like Receptor 4 Expression and Contributes to Cholangiocyte Immune Responses against Cryptosporidium Parvum Infection. J. Biol. Chem. 2007;282:28929–28938. doi: 10.1074/jbc.M702633200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Nahid M.A., Pauley K.M., Satoh M., Chan E.K.L. MiR-146a Is Critical for Endotoxin-Induced Tolerance: Implication in Innate Immunity. J. Biol. Chem. 2009;284:34590–34599. doi: 10.1074/jbc.M109.056317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Chassin C., Kocur M., Pott J., Duerr C.U., Gütle D., Lotz M., Hornef M.W. MiR-146a Mediates Protective Innate Immune Tolerance in the Neonate Intestine. Cell Host Microbe. 2010;8:358–368. doi: 10.1016/j.chom.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 273.Shaked I., Meerson A., Wolf Y., Avni R., Greenberg D., Gilboa-Geffen A., Soreq H. MicroRNA-132 Potentiates Cholinergic Anti-Inflammatory Signaling by Targeting Acetylcholinesterase. Immunity. 2009;31:965–973. doi: 10.1016/j.immuni.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 274.Incoronato M., Garofalo M., Urso L., Romano G., Quintavalle C., Zanca C., Iaboni M., Nuovo G., Croce C.M., Condorelli G. MiR-212 Increases Tumor Necrosis Factor-Related Apoptosis-Inducing Ligand Sensitivity in Non-Small Cell Lung Cancer by Targeting the Antiapoptotic Protein PED. Cancer Res. 2010;70:3638–3646. doi: 10.1158/0008-5472.CAN-09-3341. [DOI] [PubMed] [Google Scholar]
- 275.Nahid M.A., Yao B., Dominguez-Gutierrez P.R., Kesavalu L., Satoh M., Chan E.K.L. Regulation of TLR2-Mediated Tolerance and Cross-Tolerance through IRAK4 Modulation by MiR-132 and MiR-212. J. Immunol. 2013;190:1250–1263. doi: 10.4049/jimmunol.1103060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Seeley J.J., Baker R.G., Mohamed G., Bruns T., Hayden M.S., Deshmukh S.D., Freedberg D.E., Ghosh S. Induction of Innate Immune Memory via MicroRNA Targeting of Chromatin Remodelling Factors. Nature. 2018;559:114–119. doi: 10.1038/s41586-018-0253-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.El Gazzar M., McCall C.E. MicroRNAs Distinguish Translational from Transcriptional Silencing during Endotoxin Tolerance. J. Biol. Chem. 2010;285:20940–20951. doi: 10.1074/jbc.M110.115063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Liu Y., Chen Q., Song Y., Lai L., Wang J., Yu H., Cao X., Wang Q. MicroRNA-98 Negatively Regulates IL-10 Production and Endotoxin Tolerance in Macrophages after LPS Stimulation. FEBS Lett. 2011;585:1963–1968. doi: 10.1016/j.febslet.2011.05.029. [DOI] [PubMed] [Google Scholar]
- 279.Lang C.H., Spitzer J.A. Glucose Kinetics and Development of Endotoxin Tolerance during Long-Term Continuous Endotoxin Infusion. Metabolism. 1987;36:469–474. doi: 10.1016/0026-0495(87)90045-X. [DOI] [PubMed] [Google Scholar]
- 280.Androulidaki A., Iliopoulos D., Arranz A., Doxaki C., Schworer S., Zacharioudaki V., Margioris A.N., Tsichlis P.N., Tsatsanis C. The Kinase Akt1 Controls Macrophage Response to Lipopolysaccharide by Regulating MicroRNAs. Immunity. 2009;31:220–231. doi: 10.1016/j.immuni.2009.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Liu T.F., Yoza B.K., El Gazzar M., Vachharajani V.T., McCall C.E. NAD+-Dependent SIRT1 Deacetylase Participates in Epigenetic Reprogramming during Endotoxin Tolerance. J. Biol. Chem. 2011;286:9856–9864. doi: 10.1074/jbc.M110.196790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Yang H., Zhang W., Pan H., Feldser H.G., Lainez E., Miller C., Leung S., Zhong Z., Zhao H., Sweitzer S., et al. SIRT1 Activators Suppress Inflammatory Responses through Promotion of P65 Deacetylation and Inhibition of NF-ΚB Activity. PLoS ONE. 2012;7:e46364. doi: 10.1371/journal.pone.0046364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.van der Meer A.J., Scicluna B.P., Moerland P.D., Lin J., Jacobson E.W., Vlasuk G.P., van der Poll T. The Selective Sirtuin 1 Activator SRT2104 Reduces Endotoxin-Induced Cytokine Release and Coagulation Activation in Humans. Crit. Care Med. 2015;43:e199–e202. doi: 10.1097/CCM.0000000000000949. [DOI] [PubMed] [Google Scholar]
- 284.Gaber T., Strehl C., Buttgereit F. Metabolic Regulation of Inflammation. Nat. Rev. Rheumatol. 2017;13:267–279. doi: 10.1038/nrrheum.2017.37. [DOI] [PubMed] [Google Scholar]
- 285.Kominsky D.J., Campbell E.L., Colgan S.P. Metabolic Shifts in Immunity and Inflammation. J. Immunol. 2010;184:4062–4068. doi: 10.4049/jimmunol.0903002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Pålsson-McDermott E.M., O’Neill L.A.J. Targeting Immunometabolism as an Anti-Inflammatory Strategy. Cell Res. 2020;30:300–314. doi: 10.1038/s41422-020-0291-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Xu J., Gao C., He Y., Fang X., Sun D., Peng Z., Xiao H., Sun M., Zhang P., Zhou T., et al. NLRC3 Expression in Macrophage Impairs Glycolysis and Host Immune Defense by Modulating the NF-ΚB-NFAT5 Complex during Septic Immunosuppression. Mol. Ther. 2023;31:154–173. doi: 10.1016/j.ymthe.2022.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Ratter J.M., Rooijackers H.M.M., Hooiveld G.J., Hijmans A.G.M., de Galan B.E., Tack C.J., Stienstra R. In Vitro and in Vivo Effects of Lactate on Metabolism and Cytokine Production of Human Primary PBMCs and Monocytes. Front. Immunol. 2018;9:2564. doi: 10.3389/fimmu.2018.02564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Caslin H.L., Abebayehu D., Abdul Qayum A., Haque T.T., Taruselli M.T., Paez P.A., Pondicherry N., Barnstein B.O., Hoeferlin L.A., Chalfant C.E., et al. Lactic Acid Inhibits Lipopolysaccharide-Induced Mast Cell Function by Limiting Glycolysis and ATP Availability. J. Immunol. 2019;203:453–464. doi: 10.4049/jimmunol.1801005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Abebayehu D., Spence A.J., Qayum A.A., Taruselli M.T., McLeod J.J.A., Caslin H.L., Chumanevich A.P., Kolawole E.M., Paranjape A., Baker B., et al. Lactic Acid Suppresses IL-33-Mediated Mast Cell Inflammatory Responses via Hypoxia-Inducible Factor-1α-Dependent MiR-155 Suppression. J. Immunol. 2016;197:2909–2917. doi: 10.4049/jimmunol.1600651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Yang K., Xu J., Fan M., Tu F., Wang X., Ha T., Williams D.L., Li C. Lactate Suppresses Macrophage Pro-Inflammatory Response to LPS Stimulation by Inhibition of YAP and NF-ΚB Activation via GPR81-Mediated Signaling. Front. Immunol. 2020;11:587913. doi: 10.3389/fimmu.2020.587913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Cheng S.-C., Scicluna B.P., Arts R.J.W., Gresnigt M.S., Lachmandas E., Giamarellos-Bourboulis E.J., Kox M., Manjeri G.R., Wagenaars J.A.L., Cremer O.L., et al. Broad Defects in the Energy Metabolism of Leukocytes Underlie Immunoparalysis in Sepsis. Nat. Immunol. 2016;17:406–413. doi: 10.1038/ni.3398. [DOI] [PubMed] [Google Scholar]
- 293.Gillen J., Ondee T., Gurusamy D., Issara-Amphorn J., Manes N.P., Yoon S.H., Leelahavanichkul A., Nita-Lazar A. LPS Tolerance Inhibits Cellular Respiration and Induces Global Changes in the Macrophage Secretome. Biomolecules. 2021;11:164. doi: 10.3390/biom11020164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Chen L.-L., Morcelle C., Cheng Z.-L., Chen X., Xu Y., Gao Y., Song J., Li Z., Smith M.D., Shi M., et al. Itaconate Inhibits TET DNA Dioxygenases to Dampen Inflammatory Responses. Nat. Cell Biol. 2022;24:353–363. doi: 10.1038/s41556-022-00853-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Qin W., Qin K., Zhang Y., Jia W., Chen Y., Cheng B., Peng L., Chen N., Liu Y., Zhou W., et al. S-Glycosylation-Based Cysteine Profiling Reveals Regulation of Glycolysis by Itaconate. Nat. Chem. Biol. 2019;15:983–991. doi: 10.1038/s41589-019-0323-5. [DOI] [PubMed] [Google Scholar]
- 296.Zasłona Z., O’Neill L.A.J. Cytokine-like Roles for Metabolites in Immunity. Mol. Cell. 2020;78:814–823. doi: 10.1016/j.molcel.2020.04.002. [DOI] [PubMed] [Google Scholar]
- 297.Lampropoulou V., Sergushichev A., Bambouskova M., Nair S., Vincent E.E., Loginicheva E., Cervantes-Barragan L., Ma X., Huang S.C.-C., Griss T., et al. Itaconate Links Inhibition of Succinate Dehydrogenase with Macrophage Metabolic Remodeling and Regulation of Inflammation. Cell Metab. 2016;24:158–166. doi: 10.1016/j.cmet.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Liu P.-S., Wang H., Li X., Chao T., Teav T., Christen S., Di Conza G., Cheng W.-C., Chou C.-H., Vavakova M., et al. α-Ketoglutarate Orchestrates Macrophage Activation through Metabolic and Epigenetic Reprogramming. Nat. Immunol. 2017;18:985–994. doi: 10.1038/ni.3796. [DOI] [PubMed] [Google Scholar]
- 299.Liu S., Yang J., Wu Z. The Regulatory Role of α-Ketoglutarate Metabolism in Macrophages. Mediators Inflamm. 2021;2021:5577577. doi: 10.1155/2021/5577577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Nomura M., Liu J., Rovira I.I., Gonzalez-Hurtado E., Lee J., Wolfgang M.J., Finkel T. Fatty Acid Oxidation in Macrophage Polarization. Nature Immunol. 2016;17:216–217. doi: 10.1038/ni.3366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Vats D., Mukundan L., Odegaard J.I., Zhang L., Smith K.L., Morel C.R., Wagner R.A., Greaves D.R., Murray P.J., Chawla A. Oxidative Metabolism and PGC-1beta Attenuate Macrophage-Mediated Inflammation. Cell Metab. 2006;4:13–24. doi: 10.1016/j.cmet.2006.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Garcia D., Shaw R.J. AMPK: Mechanisms of Cellular Energy Sensing and Restoration of Metabolic Balance. Mol. Cell. 2017;66:789–800. doi: 10.1016/j.molcel.2017.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Jaroonwitchawan T., Visitchanakun P., Dang P.C., Ritprajak P., Palaga T., Leelahavanichkul A. Dysregulation of Lipid Metabolism in Macrophages Is Responsible for Severe Endotoxin Tolerance in FcgRIIB-Deficient Lupus Mice. Front. Immunol. 2020;11:959. doi: 10.3389/fimmu.2020.00959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Li X., Wang H., Yu X., Saha G., Kalafati L., Ioannidis C., Mitroulis I., Netea M.G., Chavakis T., Hajishengallis G. Maladaptive Innate Immune Training of Myelopoiesis Links Inflammatory Comorbidities. Cell. 2022;185:1709–1727.e18. doi: 10.1016/j.cell.2022.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Ross R. Atherosclerosis - an Inflammatory Disease. N. Engl. J. Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 306.Soehnlein O., Libby P. Targeting Inflammation in Atherosclerosis-from Experimental Insights to the Clinic. Nat. Rev. Drug Discov. 2021;20:589–610. doi: 10.1038/s41573-021-00198-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Wolf D., Ley K. Immunity and Inflammation in Atherosclerosis. Circ. Res. 2019;124:315–327. doi: 10.1161/CIRCRESAHA.118.313591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Edgar L., Akbar N., Braithwaite A.T., Krausgruber T., Gallart-Ayala H., Bailey J., Corbin A.L., Khoyratty T.E., Chai J.T., Alkhalil M., et al. Hyperglycemia Induces Trained Immunity in Macrophages and Their Precursors and Promotes Atherosclerosis. Circulation. 2021;144:961–982. doi: 10.1161/CIRCULATIONAHA.120.046464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Flores-Gomez D., Bekkering S., Netea M.G., Riksen N.P. Trained Immunity in Atherosclerotic Cardiovascular Disease. Arterioscler. Thromb. Vasc. Biol. 2021;41:62–69. doi: 10.1161/ATVBAHA.120.314216. [DOI] [PubMed] [Google Scholar]
- 310.Bekkering S., van den Munckhof I., Nielen T., Lamfers E., Dinarello C., Rutten J., de Graaf J., Joosten L.A.B., Netea M.G., Gomes M.E.R., et al. Innate Immune Cell Activation and Epigenetic Remodeling in Symptomatic and Asymptomatic Atherosclerosis in Humans in Vivo. Atherosclerosis. 2016;254:228–236. doi: 10.1016/j.atherosclerosis.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 311.Lamb D.J., Eales L.J., Ferns G.A. Immunization with Bacillus Calmette-Guerin Vaccine Increases Aortic Atherosclerosis in the Cholesterol-Fed Rabbit. Atherosclerosis. 1999;143:105–113. doi: 10.1016/S0021-9150(98)00284-6. [DOI] [PubMed] [Google Scholar]
- 312.Hajishengallis G., Chavakis T. Local and Systemic Mechanisms Linking Periodontal Disease and Inflammatory Comorbidities. Nat. Rev. Immunol. 2021;21:426–440. doi: 10.1038/s41577-020-00488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Holmstrup P., Damgaard C., Olsen I., Klinge B., Flyvbjerg A., Nielsen C.H., Hansen P.R. Comorbidity of Periodontal Disease: Two Sides of the Same Coin? An Introduction for the Clinician. J. Oral Microbiol. 2017;9:1332710. doi: 10.1080/20002297.2017.1332710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Edilova M.I., Akram A., Abdul-Sater A.A. Innate Immunity Drives Pathogenesis of Rheumatoid Arthritis. Biomed. J. 2021;44:172–182. doi: 10.1016/j.bj.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Gierut A., Perlman H., Pope R.M. Innate Immunity and Rheumatoid Arthritis. Rheum. Dis. Clin. North Am. 2010;36:271–296. doi: 10.1016/j.rdc.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Smolen J.S., Aletaha D., McInnes I.B. Rheumatoid Arthritis. Lancet (Lond. Engl.) 2016;388:2023–2038. doi: 10.1016/S0140-6736(16)30173-8. [DOI] [PubMed] [Google Scholar]
- 317.Guo Q., Wang Y., Xu D., Nossent J., Pavlos N.J., Xu J. Rheumatoid Arthritis: Pathological Mechanisms and Modern Pharmacologic Therapies. Bone Res. 2018;6:15. doi: 10.1038/s41413-018-0016-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.McGarry T., Hanlon M.M., Marzaioli V., Cunningham C.C., Krishna V., Murray K., Hurson C., Gallagher P., Nagpal S., Veale D.J., et al. Rheumatoid Arthritis CD14(+) Monocytes Display Metabolic and Inflammatory Dysfunction, a Phenotype That Precedes Clinical Manifestation of Disease. Clin. Transl. Immunol. 2021;10:e1237. doi: 10.1002/cti2.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Dai X., Dai X., Gong Z., Yang C., Zeng K., Gong F.-Y., Zhong Q., Gao X.-M. Disease-Specific Autoantibodies Induce Trained Immunity in RA Synovial Tissues and Its Gene Signature Correlates with the Response to Clinical Therapy. Mediat. Inflamm. 2020;2020:2109325. doi: 10.1155/2020/2109325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Messemaker T.C., Mikkers H.M.M., Huizinga T.W., Toes R.E.M., Van Der Helm-Van Mil A.H.M., Kurreeman F. Inflammatory Genes TNFα and IL6 Display No Signs of Increased H3K4me3 in Circulating Monocytes from Untreated Rheumatoid Arthritis Patients. Genes Immun. 2017;18:191–196. doi: 10.1038/gene.2017.20. [DOI] [PubMed] [Google Scholar]
- 321.Shao P., Ma L., Ren Y., Liu H. Modulation of the Immune Response in Rheumatoid Arthritis with Strategically Released Rapamycin. Mol. Med. Rep. 2017;16:5257–5262. doi: 10.3892/mmr.2017.7285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Jeljeli M., Riccio L.G.C., Doridot L., Chêne C., Nicco C., Chouzenoux S., Deletang Q., Allanore Y., Kavian N., Batteux F. Trained Immunity Modulates Inflammation-Induced Fibrosis. Nat. Commun. 2019;10:5670. doi: 10.1038/s41467-019-13636-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Pisetsky D.S. The Role of Innate Immunity in the Induction of Autoimmunity. Autoimmun. Rev. 2008;8:69–72. doi: 10.1016/j.autrev.2008.07.028. [DOI] [PubMed] [Google Scholar]
- 324.Liu L., Yin X., Wen L., Yang C., Sheng Y., Lin Y., Zhu Z., Shen C., Shi Y., Zheng Y., et al. Several Critical Cell Types, Tissues, and Pathways Are Implicated in Genome-Wide Association Studies for Systemic Lupus Erythematosus. G3 (Bethesda) 2016;6:1503–1511. doi: 10.1534/g3.116.027326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Li Y., Lee P.Y., Reeves W.H. Monocyte and Macrophage Abnormalities in Systemic Lupus Erythematosus. Arch. Immunol. Ther. Exp. 2010;58:355–364. doi: 10.1007/s00005-010-0093-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Herrada A.A., Escobedo N., Iruretagoyena M., Valenzuela R.A., Burgos P.I., Cuitino L., Llanos C. Innate Immune Cells’ Contribution to Systemic Lupus Erythematosus. Front. Immunol. 2019;10:772. doi: 10.3389/fimmu.2019.00772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Kavai M., Szegedi G. Immune Complex Clearance by Monocytes and Macrophages in Systemic Lupus Erythematosus. Autoimmun. Rev. 2007;6:497–502. doi: 10.1016/j.autrev.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 328.Steinbach F., Henke F., Krause B., Thiele B., Burmester G.R., Hiepe F. Monocytes from Systemic Lupus Erythematous Patients Are Severely Altered in Phenotype and Lineage Flexibility. Ann. Rheum. Dis. 2000;59:283–288. doi: 10.1136/ard.59.4.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Kaplan M.J. Neutrophils in the Pathogenesis and Manifestations of SLE. Nat. Rev. Rheumatol. 2011;7:691–699. doi: 10.1038/nrrheum.2011.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Zhu H., Hu F., Sun X., Zhang X., Zhu L., Liu X., Li X., Xu L., Shi L., Gan Y., et al. CD16(+) Monocyte Subset Was Enriched and Functionally Exacerbated in Driving T-Cell Activation and B-Cell Response in Systemic Lupus Erythematosus. Front. Immunol. 2016;7:512. doi: 10.3389/fimmu.2016.00512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Yu Y., Su K. Neutrophil Extracellular Traps and Systemic Lupus Erythematosus. J. Clin. Cell. Immunol. 2013;4 doi: 10.4172/2155-9899.1000139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Saithong S., Saisorn W., Visitchanakun P., Sae-Khow K., Chiewchengchol D., Leelahavanichkul A. A Synergy Between Endotoxin and (1→3)-Beta-D-Glucan Enhanced Neutrophil Extracellular Traps in Candida Administered Dextran Sulfate Solution Induced Colitis in FcGRIIB-/- Lupus Mice, an Impact of Intestinal Fungi in Lupus. J. Inflamm. Res. 2021;14:2333–2352. doi: 10.2147/JIR.S305225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Gao Y., Zhang J.-G., Liu Z.-Z., Ma K., Lin X.-Q., Zhang J.-B., Chen W., Yang Y.-J. Extracellular Trap Can Be Trained as a Memory Response. Virulence. 2022;13:471–482. doi: 10.1080/21505594.2022.2046950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Coussens L.M., Werb Z. Inflammation and Cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Galdiero M.R., Marone G., Mantovani A. Cancer Inflammation and Cytokines. Cold Spring Harb. Perspect. Biol. 2018;10 doi: 10.1101/cshperspect.a028662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Zhao H., Wu L., Yan G., Chen Y., Zhou M., Wu Y., Li Y. Inflammation and Tumor Progression: Signaling Pathways and Targeted Intervention. Signal Transduct. Target. Ther. 2021;6:263. doi: 10.1038/s41392-021-00658-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Donath M.Y., Shoelson S.E. Type 2 Diabetes as an Inflammatory Disease. Nat. Rev. Immunol. 2011;11:98–107. doi: 10.1038/nri2925. [DOI] [PubMed] [Google Scholar]
- 338.Das U.N. Is Obesity an Inflammatory Condition? Nutrition. 2001;17:953–966. doi: 10.1016/S0899-9007(01)00672-4. [DOI] [PubMed] [Google Scholar]
- 339.Choudhury R.P., Edgar L., Rydén M., Fisher E.A. Diabetes and Metabolic Drivers of Trained Immunity: New Therapeutic Targets Beyond Glucose. Arterioscler. Thromb. Vasc. Biol. 2021;41:1284–1290. doi: 10.1161/ATVBAHA.120.314211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Bekkering S., Saner C., Riksen N.P., Netea M.G., Sabin M.A., Saffery R., Stienstra R., Burgner D.P. Trained Immunity: Linking Obesity and Cardiovascular Disease across the Life-Course? Trends Endocrinol. Metab. 2020;31:378–389. doi: 10.1016/j.tem.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 341.Van Tuijl J., Vreeken D., Broeders W., Stienstra R., Joosten L.A.B., Netea M.G., Hazebroek E.J., Kiliaan A.J., Bekkering S., Riksen N.P. Adipose Tissue Induces Trained Innate Immunity in Patients with Obesity. Eur. Heart J. 2021;42 doi: 10.1093/eurheartj/ehab724.3438. [DOI] [Google Scholar]
- 342.Kotlyarov S. Involvement of the Innate Immune System in the Pathogenesis of Chronic Obstructive Pulmonary Disease. Int. J. Mol. Sci. 2022;23:985. doi: 10.3390/ijms23020985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.McGrath J.J.C., Stampfli M.R. The Immune System as a Victim and Aggressor in Chronic Obstructive Pulmonary Disease. J. Thorac. Dis. 2018;10:S2011–S2017. doi: 10.21037/jtd.2018.05.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Kwon H.S., Koh S.-H. Neuroinflammation in Neurodegenerative Disorders: The Roles of Microglia and Astrocytes. Transl. Neurodegener. 2020;9:42. doi: 10.1186/s40035-020-00221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Amor S., Puentes F., Baker D., Valk P. van der. Inflammation in Neurodegenerative Diseases. Immunology. 2010;129:154. doi: 10.1111/j.1365-2567.2009.03225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Ransohoff R.M. How Neuroinflammation Contributes to Neurodegeneration. Science. 2016;353:777–783. doi: 10.1126/science.aag2590. [DOI] [PubMed] [Google Scholar]
- 347.Perry V.H., Holmes C. Microglial Priming in Neurodegenerative Disease. Nat. Rev. Neurol. 2014;10:217–224. doi: 10.1038/nrneurol.2014.38. [DOI] [PubMed] [Google Scholar]
- 348.Neher J.J., Cunningham C. Priming Microglia for Innate Immune Memory in the Brain. Trends Immunol. 2019;40:358–374. doi: 10.1016/j.it.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 349.Sfera A., Gradini R., Cummings M., Diaz E., Price A.I., Osorio C. Rusty Microglia: Trainers of Innate Immunity in Alzheimer’s Disease. Front. Neurol. 2018;9:1062. doi: 10.3389/fneur.2018.01062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Noy R., Pollard J.W. Tumor-Associated Macrophages: From Mechanisms to Therapy. Immunity. 2014;41:49–61. doi: 10.1016/j.immuni.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Galdiero M.R., Garlanda C., Jaillon S., Marone G., Mantovani A. Tumor Associated Macrophages and Neutrophils in Tumor Progression. J. Cell. Physiol. 2013;228:1404–1412. doi: 10.1002/jcp.24260. [DOI] [PubMed] [Google Scholar]
- 352.Shaul M.E., Fridlender Z.G. Tumour-Associated Neutrophils in Patients with Cancer. Nat. Rev. Clin. Oncol. 2019;16:601–620. doi: 10.1038/s41571-019-0222-4. [DOI] [PubMed] [Google Scholar]
- 353.del Fresno C., Otero K., Gómez-García L., González-León M.C., Soler-Ranger L., Fuentes-Prior P., Escoll P., Baos R., Caveda L., García F., et al. Tumor Cells Deactivate Human Monocytes by Up-Regulating IL-1 Receptor Associated Kinase-M Expression via CD44 and TLR4. J. Immunol. 2005;174:3032–3040. doi: 10.4049/jimmunol.174.5.3032. [DOI] [PubMed] [Google Scholar]
- 354.Soares-Schanoski A., Jurado T., Córdoba R., Siliceo M., Del Fresno C., Gómez-Piña V., Toledano V., Vallejo-Cremades M.T., Alfonso-Iñiguez S., Carballo-Palos A., et al. Impaired Antigen Presentation and Potent Phagocytic Activity Identifying Tumor-Tolerant Human Monocytes. Biochem. Biophys. Res. Commun. 2012;423:331–337. doi: 10.1016/j.bbrc.2012.05.124. [DOI] [PubMed] [Google Scholar]
- 355.Nosari A. Infectious Complications in Chronic Lymphocytic Leukemia. Mediterr. J. Hematol. Infect. Dis. 2012;4:e2012070. doi: 10.4084/mjhid.2012.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Rolston K.V.I. Infections in Patients with Acute Leukemia. In: Maschmeyer G., Rolston K.V.I., editors. Infections in Hematology. Springer; Berlin/Heidelberg, Germany: 2015. pp. 3–23. [Google Scholar]
- 357.Logan C., Koura D., Taplitz R. Updates in Infection Risk and Management in Acute Leukemia. Hematol. Am. Soc. Hematol. Educ. Progr. 2020;2020:135–139. doi: 10.1182/hematology.2020000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Pena O.M., Pistolic J., Raj D., Fjell C.D., Hancock R.E.W. Endotoxin Tolerance Represents a Distinctive State of Alternative Polarization (M2) in Human Mononuclear Cells. J. Immunol. 2011;186:7243–7254. doi: 10.4049/jimmunol.1001952. [DOI] [PubMed] [Google Scholar]
- 359.Mantovani A., Sica A. Macrophages, Innate Immunity and Cancer: Balance, Tolerance, and Diversity. Curr. Opin. Immunol. 2010;22:231–237. doi: 10.1016/j.coi.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 360.Pan Y., Yu Y., Wang X., Zhang T. Tumor-Associated Macrophages in Tumor Immunity. Front. Immunol. 2020;11:583084. doi: 10.3389/fimmu.2020.583084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.van der Poll T., van de Veerdonk F.L., Scicluna B.P., Netea M.G. The Immunopathology of Sepsis and Potential Therapeutic Targets. Nat. Rev. Immunol. 2017;17:407–420. doi: 10.1038/nri.2017.36. [DOI] [PubMed] [Google Scholar]
- 362.Hotchkiss R.S., Moldawer L.L., Opal S.M., Reinhart K., Turnbull I.R., Vincent J.-L. Sepsis and Septic Shock. Nat. Rev. Dis. Prim. 2016;2:16045. doi: 10.1038/nrdp.2016.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Cao C., Yu M., Chai Y. Pathological Alteration and Therapeutic Implications of Sepsis-Induced Immune Cell Apoptosis. Cell Death Dis. 2019;10:782. doi: 10.1038/s41419-019-2015-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Gogos C., Kotsaki A., Pelekanou A., Giannikopoulos G., Vaki I., Maravitsa P., Adamis S., Alexiou Z., Andrianopoulos G., Antonopoulou A., et al. Early Alterations of the Innate and Adaptive Immune Statuses in Sepsis According to the Type of Underlying Infection. Crit. Care. 2010;14:R96. doi: 10.1186/cc9031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Cavaillon J.-M., Adrie C., Fitting C., Adib-Conquy M. Endotoxin Tolerance: Is There a Clinical Relevance? J. Endotoxin Res. 2003;9:101–107. doi: 10.1177/09680519030090020501. [DOI] [PubMed] [Google Scholar]
- 366.Hotchkiss R.S., Monneret G., Payen D. Immunosuppression in Sepsis: A Novel Understanding of the Disorder and a New Therapeutic Approach. Lancet. Infect. Dis. 2013;13:260–268. doi: 10.1016/S1473-3099(13)70001-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Pena O.M., Hancock D.G., Lyle N.H., Linder A., Russell J.A., Xia J., Fjell C.D., Boyd J.H., Hancock R.E.W. An Endotoxin Tolerance Signature Predicts Sepsis and Organ Dysfunction at Initial Clinical Presentation. EBioMedicine. 2014;1:64–71. doi: 10.1016/j.ebiom.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Hoogendijk A.J., Garcia-Laorden M.I., van Vught L.A., Wiewel M.A., Belkasim-Bohoudi H., Duitman J., Horn J., Schultz M.J., Scicluna B.P., van ’t Veer C., et al. Sepsis Patients Display a Reduced Capacity to Activate Nuclear Factor-ΚB in Multiple Cell Types. Crit. Care Med. 2017;45:e524–e531. doi: 10.1097/CCM.0000000000002294. [DOI] [PubMed] [Google Scholar]
- 369.Dar W.A., Sullivan E., Bynon J.S., Eltzschig H., Ju C. Ischaemia Reperfusion Injury in Liver Transplantation: Cellular and Molecular Mechanisms. Liver Int. Off. J. Int. Assoc. Study Liver. 2019;39:788–801. doi: 10.1111/liv.14091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Jaeschke H. Molecular Mechanisms of Hepatic Ischemia-Reperfusion Injury and Preconditioning. Am. J. Physiol. Gastrointest. Liver Physiol. 2003;284:G15–G26. doi: 10.1152/ajpgi.00342.2002. [DOI] [PubMed] [Google Scholar]
- 371.Peralta C., Jiménez-Castro M.B., Gracia-Sancho J. Hepatic Ischemia and Reperfusion Injury: Effects on the Liver Sinusoidal Milieu. J. Hepatol. 2013;59:1094–1106. doi: 10.1016/j.jhep.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 372.Hirao H., Nakamura K., Kupiec-Weglinski J.W. Liver Ischaemia-Reperfusion Injury: A New Understanding of the Role of Innate Immunity. Nat. Rev. Gastroenterol. Hepatol. 2022;19:239–256. doi: 10.1038/s41575-021-00549-8. [DOI] [PubMed] [Google Scholar]
- 373.Fernández E.D., Flohé S., Siemers F., Nau M., Ackermann M., Ruwe M., Schade F.U. Endotoxin Tolerance Protects against Local Hepatic Ischemia/Reperfusion Injury in the Rat. J. Endotoxin Res. 2000;6:321–328. doi: 10.1179/096805100101532216. [DOI] [PubMed] [Google Scholar]
- 374.Li J., Lai X., Chen Y., Niu B., Gong J. Endotoxin Tolerance Attenuates Liver Ischemia/Reperfusion Injury by down-Regulation of Interleukin-1 Receptor-Associated Kinase 4 in Kupffer Cells. Transplant. Proc. 2011;43:2531–2535. doi: 10.1016/j.transproceed.2011.05.045. [DOI] [PubMed] [Google Scholar]
- 375.Brown J.M., Grosso M.A., Terada L.S., Whitman G.J., Banerjee A., White C.W., Harken A.H., Repine J.E. Endotoxin Pretreatment Increases Endogenous Myocardial Catalase Activity and Decreases Ischemia-Reperfusion Injury of Isolated Rat Hearts. Proc. Natl. Acad. Sci. USA. 1989;86:2516–2520. doi: 10.1073/pnas.86.7.2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.DeMaria E.J., Pellicane J.V., Lee R.B. Hemorrhagic Shock in Endotoxin-Resistant Mice: Improved Survival Unrelated to Deficient Production of Tumor Necrosis Factor. J. Trauma. 1993;35:720–725. doi: 10.1097/00005373-199311000-00012. [DOI] [PubMed] [Google Scholar]
- 377.del Fresno C., Soler-Rangel L., Soares-Schanoski A., Gómez-Piña V., González-León M.C., Gómez-García L., Mendoza-Barberá E., Rodríguez-Rojas A., García F., Fuentes-Prior P., et al. Inflammatory Responses Associated with Acute Coronary Syndrome Up-Regulate IRAK-M and Induce Endotoxin Tolerance in Circulating Monocytes. J. Endotoxin Res. 2007;13:39–52. doi: 10.1177/0968051907078623. [DOI] [PubMed] [Google Scholar]
- 378.Nica V., Popp R.A., Crișan T.O., Joosten L.A.B. The Future Clinical Implications of Trained Immunity. Expert Rev. Clin. Immunol. 2022;18:1125–1134. doi: 10.1080/1744666X.2022.2120470. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The PubMed data presented in this paper are accessible online for any reader (Link: https://pubmed.ncbi.nlm.nih.gov/ (accessed on 10 January 2023)).