Abstract
Carpal tunnel syndrome (CTS) is the most common peripheral entrapment, and recently, ultrasound-guided perineural injection (UPIT) and percutaneous flexor retinaculum release (UPCTR) have been utilized to treat CTS. However, no systematic review or meta-analysis has included both intervention types of ultrasound-guided interventions for CTS. Therefore, we performed this review using four databases (i.e., PubMed, EMBASE, Scopus, and Cochrane) to evaluate the quality of evidence, effectiveness, and safety of the published studies on ultrasound-guided interventions in CTS. Among sixty studies selected for systemic review, 20 randomized treatment comparison or controlled studies were included in six meta-analyses. Steroid UPIT with ultrasound guidance outperformed that with landmark guidance. UPIT with higher-dose steroids outperformed that with lower-dose steroids. UPIT with 5% dextrose in water (D5W) outperformed control injection and hydrodissection with high-volume D5W was superior to that with low-volume D5W. UPIT with platelet-rich plasma outperformed various control treatments. UPCTR outperformed open surgery in terms of symptom improvement but not functional improvement. No serious adverse events were reported in the studies reviewed. The findings suggest that both UPIT and UPCTR may provide clinically important benefits and appear safe. Further treatment comparison studies are required to determine comparative therapeutic efficacy.
Keywords: carpal tunnel syndrome, ultrasound-guided, intervention, injection, release
1. Introduction
Carpal tunnel syndrome (CTS) is the most commonly diagnosed (90%) peripheral entrapment neuropathy [1]. The worldwide incidence of CTS ranges from 3% to 4%, and its typical symptoms and signs include numbness, tingling, pain or burning sensation, and nocturnal paresthesia in the regions innervated by the median nerve (MN). Weakness with thenar muscle atrophy may occur in severe cases or in later stages in mild-to-moderate cases [2,3]. Although the pathophysiology of CTS remains unclear, it is generally acknowledged to involve MN compression by increased pressure within the carpal tunnel caused by swollen flexor retinaculum (FR), flexor tenosynovium, or subsynovial connective tissue (SSCT), or a combination thereof. Increased intracarpal pressure contributes to interruption of nerve microcirculation, ischemia, impaired nerve conduction, decreased MN dynamics with adhesion, increased MN vascular permeability, and interruption of the axoplasmic flow, with subsequent nerve swelling proximal and distal to the compression site [4,5,6]. The “hourglass” configuration distortion of the MN could further decrease the MN excursion, thereby exacerbating traction neuropathy [7].
The treatment of CTS includes non-surgical and surgical management depending on symptom severity [4,8]. Generally, non-surgical treatments (such as splints, medications with nonsteroidal anti-inflammatory drugs, and physical therapy) are recommended for mild-to-moderate CTS. However, non-surgical treatments have a limited therapeutic effect with a short duration [9]. A recent systemic review revealed that 57–66% of patients underwent surgery after receiving non-surgical treatments for 1–3 years [1]. An excellent outcome after CTS surgery was reported in 75% of patients, with symptom escalation in 8% of patients, and revision surgeries in 12% of patients [10]. However, revision surgery is associated with a dramatic increase in the failure rate [10,11,12]. The percentage of unfavorable surgical outcomes primarily due to an incomplete release of the FR or scar formation with resultant grasp weakness or pillar pain has been reported to be consistent since 1988 [12]. Conventionally, carpal tunnel release (CTR) is performed using open CTR (OCTR), endoscopic CTR (ECTR), or mini-open CTR (mini-OCTR) approaches. Overall, OCTR and ECTR have similar percentages of successful surgical outcomes and associated complications [13,14]. OCTR has the advantage of enabling clear visualization of the essential anatomic structures; however, it typically requires a 2–7 cm palmar skin incision [15]. The time to return to work for OCTR is typically 3 to 4 weeks [13,16]. ECTR requires one or two portals of entry, each via a smaller (1.5–2 cm) incision than that required by OCTR, leading to fewer scar-related complications and a shorter duration of work loss (2–3 weeks). However, ECTR is associated with a higher rate of transient nerve injury [15]. Moreover, mini-OCTR also aims to minimize surgical trauma and has shown positive results, but a portion of the surgery is performed blindly [17,18].
High-resolution ultrasound has been increasingly used to administer nerve blocks because the direct visualization of nerves enables more precise, effective, and safe anesthetic infiltration while limiting the potential for neural trauma [19,20]. Recently, ultrasound-guided perineural injection and percutaneous FR release have been utilized to treat CTS, with reported clinically and statistically significant benefits [21,22]. Although a review in 2022 mentioned several potential injectates for use in the perineural injection therapy (PIT) of CTS [23], the only systematic collection of outcomes of all injectate types used for PIT was reported by Buntragulpoontawee et al., with a literature review through August 2020 [24]. To date, a systematic review pertaining to both ultrasound-guided PIT (UPIT) and ultrasound-guided percutaneous CTR (UPCTR) has not been reported. Therefore, we performed this systematic review based on published studies to examine the quality of evidence, effectiveness, and safety of UPIT and UPCTR in CTS. We hypothesized that both ultrasound-guided interventions are safe and effective for CTS.
2. Materials and Methods
This review conforms to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [25]. The protocol was registered at PROSPERO 2022 CRD42022384170 (available from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022384170; accessed on 29 December 2022).
2.1. Data Sources and Search Strategy
Four databases (i.e., PubMed, EMBASE, Scopus, and Cochrane) were systematically searched for the relevant literature from inception up to 30 June 2022. The search strategy included a combination of the following search terms together using logical Boolean operators “AND” and “OR”: “ultrasound-guided,“ “hydrodissection,“ “intervention,“ “injection,“ “surgery,“ “release,“ “complication,“ “adverse effect,“ and “CTS.“ The references of the articles were manually searched to identify additional relevant publications.
2.2. Inclusion and Exclusion Criteria
Inclusion criteria were as follows: (1) English language clinical trials, retrospective studies, or case series in humans assessing the efficacy and safety of either UPIT or UPCTR for CTS; (2) studies with outcome measures including changes in pain intensity, other clinical symptoms, function, electrophysiological measures, day of return to work, or the cross-sectional area (CSA) of the MN; and (3) UPCTR studies requiring the release of the entire FR width. There were no limitations on the therapy provided to the control groups for included studies. Exclusion criteria were as follows: (1) studies using a mixed injectate for UPIT, and (2) studies with components of open surgery or endoscopic release for UPCTR.
2.3. Data Extraction
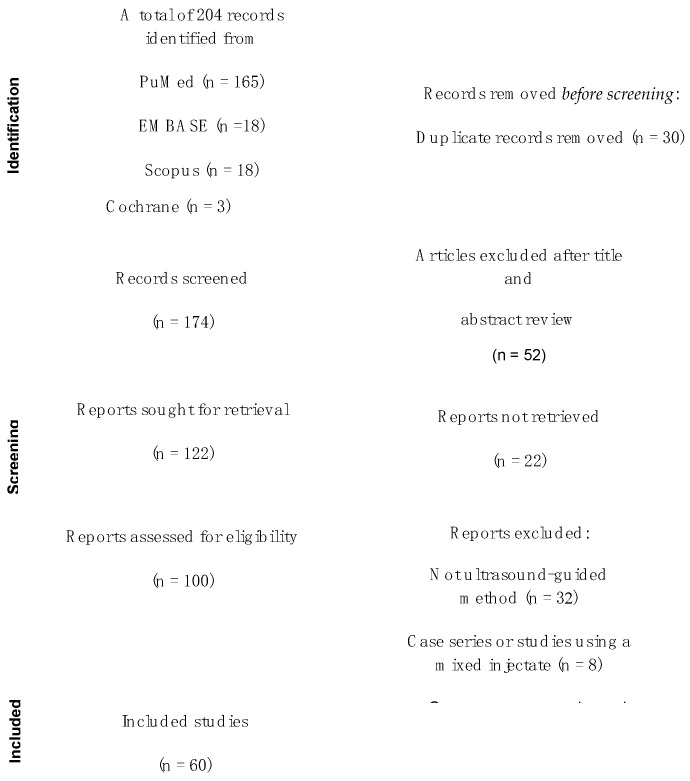
Two reviewers (KHSL and YTW), each with more than seven years of research experience, independently performed full-text reviews to extract data for analysis. The collected data included study the design, inclusion criteria, ultrasound-guided (UG) intervention and treatment allocation, participants’ characteristics, CTS severity, outcome measurements, follow-up period, and safety outcomes (Figure 1). Discrepancies in study selection were resolved by a third reviewer (KDR).
Figure 1.
PRISMA flow diagram showing the selection of studies.
2.4. Outcome Measures for Meta-Analysis
The primary outcomes of interest for meta-analysis were changes in symptom severity, measured using a visual analogue scale (VAS), numerical rating scale (NRS), or the Boston Carpal Tunnel Questionnaire symptom scale (BCTQ-SS) and function scale (BCTQ-FS) [26]. VAS or NRS values were converted to a 0–10 format for analysis, and BCTQ values were converted to a standard 0–5 format for symptom and function scale analyses.
2.5. Bias Assessment
Bias risks and the critical appraisal of the manuscripts were independently assessed using the Cochrane risk-of-bias tool for randomized trials, version 2 (RoB 2) [27] and the Joanna Biggs Institute (JBI) Critical Appraisal Checklist for Case Series [28] and Cohort Studies [29]. Using the RoB 2 tool, an overall risk of bias for a specific outcome was judged as “low risk ” only when all individual domains were scored as low risk, “some concerns” if any one category was scored as “some concern,” and “high risk” if any one category was scored as “high risk” or with more than one category scored as “some concern” [27]. The overall bias risk for case series or cohort studies was scored as “low” if more than 7 of 10 items or 8 of 11 items on the JBI Critical Appraisal Checklist for Cases Series [28] or Cohort Studies [29], respectively, were scored as low risk. The risk of bias was assessed by two independent reviewers (KHSL and AEA), with discrepancies resolved by a third reviewer (KDR).
2.6. Analysis
All meta-analyses were conducted using Revman version 5.4.1 [30]. A random effects model was used to pool study results. Changed scores for continuous outcome measures (VAS, BCTQ-SS, or BTCT-SS) were pooled as standardized mean differences with a confidence interval of 95% and a weighted mean difference was calculated. Potential clinical importance was interpreted according to minimal clinically important differences for VAS and BCTQ [31,32]. Heterogeneity between studies was reported as an I2 value and an overall effect was reported as a Z score with a corresponding p value.
3. Results
3.1. Study Selection and Characteristics
Selection (Figure 1)
After our primary search, 84 potentially relevant studies on UPIT were identified, of which 36 publications met the inclusion criteria. Among them, 18 studies reported outcomes of UPIT with corticosteroid injection, six with 5% dextrose in water (D5W), seven with platelet-rich plasma (PRP), two with hyaluronidase, one with hyaluronic acid (HA), one with insulin, and one with ozone. The publication types included 31 randomized controlled trials (RCTs), three retrospective studies, and one pilot study. Regarding UPCTR, 90 potentially relevant papers were identified, of which 24 met the inclusion criteria, including four RCTs, four cohort studies, and 16 case series.
3.2. Bias Analysis of UPIT and UPCTR Studies
3.2.1. Bias Analysis of RCTs (Table 1)
Table 1.
Bias table for RCTs of UPIT and UPCTR.
| Author | Domain 1 | Domain 2 | Domain 3 | Domain 4 | Domain 5 | Overall Bias |
|---|---|---|---|---|---|---|
| Bias table for RCTs of UPIT using Steroids | ||||||
| Ustun (2013) [33] |

|

|

|

|

|

|
| Lee (2014) [34] |

|

|

|

|

|

|
| Makhlouf (2014) [35] |

|

|

|

|

|

|
| Eslamian (2017) [36] |

|

|

|

|

|

|
| Karaahmet (2017) [37] |

|

|

|

|

|

|
| Wang (2017) [38] |

|

|

|

|

|

|
| Chen (2018) [39] |

|

|

|

|

|

|
| Ba-baei-Ghazani (2018) [40] |

|

|

|

|

|

|
| Roghani (2018) [41] |

|

|

|

|

|

|
| Roh (2019) [42] |

|

|

|

|

|

|
| Rayegani (2019) [43] |

|

|

|

|

|

|
| Hsu (2020) [44] |

|

|

|

|

|

|
| Ba-baei-Ghazani (2020) [45] |

|

|

|

|

|

|
| Mezian (2021) [46] |

|

|

|

|

|

|
| Wang (2021) [47] |

|

|

|

|

|

|
| Mathew (2022) [48] |

|

|

|

|

|

|
| Bias table for RCTs of UPIT using 5% Dextrose | ||||||
| Wu (2017) [49] |

|

|

|

|

|

|
| Wu (2018) [50] |

|

|

|

|

|

|
| Lin (2020) [51] |

|

|

|

|

|

|
| Lin (2021) [52] |

|

|

|

|

|

|
| Bias table for RCTs of UPIT using Platelet-Rich Plasma | ||||||
| Wu et al. (2017) [53] |

|

|

|

|

|

|
| Malahias et al. (2018) [54] |

|

|

|

|

|

|
| Senna et al. (2019) [55] |

|

|

|

|

|

|
| Shen 2019 [56] |

|

|

|

|

|

|
| Chen et al. (2021) [57] |

|

|

|

|

|

|
| Bias table for RCTs of UPIT using other Injectates | ||||||
| Su et al. (2021) [58] |

|

|

|

|

|

|
| Alsaeid et al. (2019) [59] |

|

|

|

|

|

|
| Elawa-my et al. (2020) [60] |

|

|

|

|

|

|
| Kamel et al. (2021) [61] |

|

|

|

|

|

|
| Forogh et al. (2021) [62] |

|

|

|

|

|

|
| Bias table for RCTs of UPCTR | ||||||
| Capa Grasa (2014) [63] |

|

|

|

|

|

|
| Rojo-Manaute (2016) [64] |

|

|

|

|

|

|
| Zhang (2019) [65] |

|

|

|

|

|

|
| Fuente (2021) [66] |

|

|

|

|

|

|
Domain 1, bias arising from the randomization process; Domain 2, bias due to deviations from intended interventions; Domain 3, bias due to missing outcome data; Domain 4, bias in the measurement of the outcome; and Domain 5, bias in the selection of the reported result. Red color dots signifie high bias, orange color dots point to some concerns on bias analysis, and green color dots denote low bias.
The bias assessments for all the RCTs are listed in Table 1. Of 30 RCTs of UPIT, 17 showed a high overall bias risk, mainly due to high bias owing to deviations from intended interventions because the study participants could not be blinded; four showed some concerns in overall bias risk; and nine had a low overall risk of bias.
3.2.2. Bias Analysis of Cohort Studies
The critical appraisals for cohort studies are summarized in Table 2. Only one cohort study showed a high bias risk.
Table 2.
JBI Critical Appraisal Checklist for Cohort Studies.
| Criteria and Corresponding Scores | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | #1 | #2 | #3 | #4 | #5 | #6 | #7 | #8 | #9 | #10 | #11 | Total | % | Bias Risk |
| Bias table for case cohort of UPIT using Steroids | ||||||||||||||
| Hsu (2018) [67] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 1 | 8 | 72.7 | Low |
| Yeom (2021) [68] | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 6 | 54.5 | High |
| Bias table for case cohort of UPIT using Platelet-Rich Plasma | ||||||||||||||
| Guven et al. (2019) [69] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | N | 1 | 8 | 80 | Low |
| Bias table for case cohort of UPCTR | ||||||||||||||
| Nakamichi et al. (2010) [17] | 1 | 1 | 1 | U | U | 1 | 1 | 1 | 1 | U | 1 | 8 | 72.7 | Low |
| Guo et al. (2018) [70] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | U | U | 1 | 8 | 72.7 | Low |
| Burnham et al. (2021) [71] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 11 | 100 | Low |
| Asserson 2022 [72] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | U | 1 | 10 | 90.0 | Low |
| Quality measures of cohort studies based on the following listed criteria: | ||||||||||||||
| #1. Were the two groups similar and recruited from the same population? | ||||||||||||||
| #2. Were the exposures measured similarly to assign people to both exposed and unexposed groups? | ||||||||||||||
| #3. Was the exposure measured in a valid and reliable way? | ||||||||||||||
| #4. Were confounding factors identified? | ||||||||||||||
| #5. Were strategies to deal with confounding factors stated? | ||||||||||||||
| #6. Were the groups/participants free of the outcome at the start of the study (or at the moment of exposure)? | ||||||||||||||
| #7. Were the outcomes measured in a valid and reliable way? | ||||||||||||||
| #8. Was the follow-up time reported and sufficient to be long enough for outcomes to occur? | ||||||||||||||
| #9. Was follow-up completed, and if not, were the reasons for the loss of follow-up described and explored? | ||||||||||||||
| #10. Were strategies to address incomplete follow-up utilized? | ||||||||||||||
| #11. Was appropriate statistical analysis used? | ||||||||||||||
NB: 1 indicates the article does fulfill the specified criteria; 0 indicates the article does not fulfill the stated criteria; U indicates the article is unclear about the criteria; N indicates the criteria are not applicable to the article. Red color front signifies high bias, and green color words denote low bias.
3.2.3. Bias Analysis of Case Series (Table 3)
Table 3.
JBI Critical Appraisal Checklist for Case Series.
| Criteria and Corresponding Scores | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author | #1 | #2 | #3 | #4 | #5 | #6 | #7 | #8 | #9 | #10 | Total | % | Bias Risk |
| Bias table for case series of UPIT using Dextrose | |||||||||||||
| Li et al. (2021) [73] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | 100 | Low |
| Chao et al. (2022) [74] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 10 | 100 | Low |
| Bias table for case series of UPIT using Platelet-Rich Plasma | |||||||||||||
| Malahias et al. (2015) [75] | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 9 | 90 | Low |
| Bias table for case series for UPCTR | |||||||||||||
| Chern et al. (2015) [76] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | U | 8 | 80 | Low |
| Guo et al. (2015) [77] | U | 1 | 1 | U | U | 1 | 0 | 1 | 0 | U | 4 | 40 | High |
| Guo et al. (2017) [78] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 | 90 | Low |
| Petrover et al. (2017) [79] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 8 | 80 | Low |
| Henning et al. (2018) [80] | 1 | 1 | 1 | U | U | 1 | 0 | 1 | 0 | 1 | 6 | 60 | High |
| Luanchumroen et al. (2019) [81] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 8 | 80 | Low |
| Wang et al. (2019) [82] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 | 90 | Low |
| Chappell et al. (2020) [83] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | U | 8 | 80 | Low |
| Hebbard et al. (2020) [84] | 0 | U | U | U | U | 1 | 0 | 1 | 0 | 1 | 3 | 30 | High |
| Joseph et al. (2020) [85] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 | 90 | Low |
| Kamel et al. (2020) [86] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 | 90 | Low |
| Wang et al. (2021) [87] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | U | 7 | 70 | High |
| Leiby et al. (2021) [88] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 9 | 90 | Low |
| Loizides (2021) [89] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | U | 8 | 80 | Low |
| Lee (2022) [90] | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 8 | 80 | Low |
| Fowler (2022) [91] | 1 | 1 | 1 | 0 | U | 1 | 1 | 1 | 0 | 1 | 7 | 70 | High |
| Quality measures of case series studies based on the following listed criteria: | |||||||||||||
| #1. Were there clear criteria for inclusion in the case series? | |||||||||||||
| #2. Was the condition measured in a standard, reliable way for all participants included in the case series? | |||||||||||||
| #3. Were valid methods used for identification of the condition for all participants included in the case series? | |||||||||||||
| #4. Did the case series have consecutive inclusion of participants? | |||||||||||||
| #5. Did the case series have complete inclusion of participants? | |||||||||||||
| #6. Was there clear reporting of the demographics of the participants in the study? | |||||||||||||
| #7. Was there clear reporting of clinical information of the participants? | |||||||||||||
| #8. Were the outcomes or follow-up results of cases clearly reported? | |||||||||||||
| #9. Was there clear reporting of the demographic information of the presenting site(s)/clinic(s)? | |||||||||||||
| #10. Was statistical analysis appropriate? | |||||||||||||
NB: 1 indicates the article does fulfill the specified criteria; 0 indicates the article does not fulfill the stated criteria; U indicates the article is unclear about the criteria; Red color front signifies high bias, and green color words denote low bias.
The critical appraisals for case series studies are presented in Table 3. The case series for the UPIT had a low-risk bias; however, five of 16 case series studies for UPCTR had a high-risk bias and the rest of the studies had a low-risk bias.
3.3. UPIT Study Characteristics
3.3.1. UPIT Using Corticosteroids
Among the 18 studies on the outcomes of UPIT with corticosteroid injection (Table 4), eight compared the efficacy of ultrasound-guided injections vs. that of blind landmark-guided injections [33,34,35,36,37,39,42,43]. Several recent UPIT studies investigated the efficacy of different concentrations of the same steroid (four UPIT studies [37,39,41,44,47]), use of different steroids (one study [48]), hydrodissection superficial vs. deep to the MN (one study [40]), effects of short vs. long-axis UPIT (one study [43]), intra- vs. extraepineurial UPIT (one study [67]), ulnar vs. radial approaches for UPIT (one study [45]), and perineural vs. peritendinous approaches (one study [46]).
Table 4.
Intervention details of included studies using ultrasound-guided corticosteroid injections for treating carpal tunnel syndrome.
| Author, Year | Study Design | Inclusion Criteria |
UG Intervention and Treatment Allocation |
Participant Characteristics | CTS Severity |
Outcome Measurements |
Follow-Up | Safety Outcome (n) |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size (Wrists) Cases/Controls | Mean Age (Years) Cases/Controls |
Female (%) Cases/Controls |
Symptom Duration (Months) Cases/Controls |
||||||||
| Üstün (2013) [33] | Single-blind RCT | Clinical + EDS |
UG (Ulnar S–O below MN) vs. Blind (Ulnar to PL) 40 mg methylprednisolone |
23/23 | 45.96/42.71 | 82.6/95.7 | 16.78/10.19 | Moderate | BCTQ | 3 months | Procedural pain UG group (4) Blind group (8) |
| Lee et al. (2014) [34] |
Single–blind RCT | Clinical + EDS |
UG (Ulnar S–I below and above MN)) vs. UG (Ulnar S–O below MN) vs. Blind (Ulnar to PL) 1 mL triamcinolone (40 mg/mL) + 1 mL 1% lidocaine |
24/26/25 | 52.6/55.2/50.3 | 100/93.3/86.7 | 9.4/8.9/7.6 | Mild to moderate | BCTQ EDS CSA of MN |
3 months | Nerve insult Ulnar S–I (1) Ulnar S–O (6) Blind (5) Vessel insult Ulnar S–I (0) Ulnar S–O (0) Blind (2) Skin lesion Ulnar S–I (3) Ulnar S–O (1) Blind (8) |
| Makhlouf et al. (2014) [35] | Single-blind RCT | Clinical | UG (Ulnar S–I above and below MN) vs. Blind (Ulnar to PL) 3 mL 80 mg triamcinolone + 3 mL 1 % lidocaine |
37/40 | 45.7/52.2 | 94.6/80 | NR | Mild to moderate | VAS Duration of therapeutic effect time to next procedure, procedural costs |
6 months | No AE reported |
| Eslamian et al. (2017) [36] | Single-blind RCT | Clinical + EDS |
UG (Ulnar S–I below MN) vs. Blind (ulnar to PL) 40 mg methylprednisolone |
30/30 | 54.52/49.33 | 86.2/100 | NR | Moderate | BCTQ EDS, |
3 months | 1 wrist flexor tendonitis in blind group |
| Karaahmet al. (2017) [37] |
Single-blind RCT | Clinical + EDS |
UG (Ulnar S–I, NR about above or below MN) vs. Blind (Ulnar to PL) 1 mL betamethasone (2.63 mg)/betamethasone (6.43 mg) |
21/19 | 59.4/61.5 | 86.7/93.8 | 28.5/38.5 | Severe | BCTQ EDS |
4 weeks | No AE reported |
| Wang et al. (2017) [38] | Single-blind RCT | Clinical + EDS |
Splint + UG (Ulnar S–I above and below MN) vs. UG (Ulnar S–I above and below MN) 1 mL 10 mg (10 mg/mL) triamcinolone + 1 mL 2% lidocaine |
24/24 | 54.34/55.76 | 83.3/87.5 | 6/5 (3 to 6 months) 6/7 (6 to 12 months) 6/5 (1 to 2 years) 8/9 (>2 years) |
NR | VAS BCTQ EDS Global assessment of treatment results |
12 weeks | No AE reported |
| Chen et al. (2018) [39] | Double-blind RCT | Clinical + EDS |
UG (Ulnar S–O below MN) vs. Blind (Ulnar to PL) 1 mL betamethasone (betamethasone dipropionate 5 mg and betamethasone disodium phosphate 2 mg) |
22/17 | 51.09/51.12 | 76.5/71.4 | 70.55/65.12 | Mild to moderate | Physical findings BCTQ EDS |
6 months | UG group Numbness (1) Swelling (4) Pain (10) Weakness (0) Blind group Numbness (4) Swelling (6) Pain (10) Weakness (3) |
| Babaei-Ghazani et al. (2018) [40] |
Double-blind RCT | Clinical + EDS |
UG (Ulnar S–I above MN) vs. UG (Ulnar S–I below MN) 1 mL triamcinolone (40 mg/mL) |
22/22 | 56.63/51.09 | 91/91 | NR | Mild to moderate | VAS BCTQ EDS CSA of MN |
3 months | No AE reported |
| Roghani et al. (2018) [41] | Triple-blind RCT | Clinical + EDS |
UG (Long-axis from distal to proximal, above MN) 80 mg triamcinolone (2 mL) + 1 mL 2% lidocaine vs. 40 mg triamcinolone (1 mL) + 1 mL 2% lidocaine + 1 mL NS vs. 1 mL 2% lidocaine + 2 mL NS |
32/32/30 | 66.1/66/63.4 | 68.8/87.5/90 | NR | Moderate | VAS BCTQ EDS CSA of MN |
6 months | No AE reported |
| Hsu et al. (2018) [67] | Case cohort | Clinical + EDS + US |
UG (Ulnar S–I above MN) Intraepineurium vs. Extraepineurium 3 mL 10 mg triamcinolone + 3 mL 1% lidocaine |
39/62 | 53/56 | 74.4/75.8 | 33.2/33.5 | NR | BCTQ CSA of MN Satisfaction scale of treatment results |
6 months | MN injury Intraepineurium (2) Extraepineurium (4) |
| Roh et al. (2019) [42] |
Single-blind RCT | Clinical + EDS |
UG (Ulnar S–I above MN) vs. Blind (Ulnar to PL) 1 mL triamcinolone (20 mg/mL) + 1 mL lidocaine (10 mg/mL) |
51/51 | 54/55 | 76.5/80.4 | 15/14 | Mild to extremely severe CTS | BCTQ grip strength |
6 months | UG group Finger numbness or weakness (1) Skin discoloration or subcutaneous fat atrophy (1) Steroid flare (2) Blind group Finger numbness or weakness (7) Skin discoloration or subcutaneous fat atrophy (3) Steroid flare (3) |
| Rayegani et al. (2019) [43] |
Single-blind RCT | Clinical + EDS |
UG (Ulnar S–I below MN) vs. UG (Long-axis from proximal to distal, above MN) vs. Blind 1 mL triamcinolone (40 mg) + 1 mL 2% lidocaine |
26/27/23 | 54.39/54.56/54.04 | 73.1/81.5/78.3 | NR | Mild to moderate | VAS BCTQ grip strength CSA of MN EDS |
10 weeks | No AE reported |
| Hsu et al. (2020) [44] |
Double-blind RCT | Clinical + EDS |
UG (Ulnar S–I, NR about above or below MN) 40 mg triamcinolone (40 mg/mL) + 1 mL 2% lidocaine vs. 10 mg triamcinolone (10 mg/mL) +1 mL 2% lidocaine |
28/28 | 57.1/54.5 | 75/78.6 | 42.3/27.5 | Mild to moderate | VAS BCTQ EDS |
3 months | No AE reported |
| Babaei-Ghazani et al. (2020) [45] |
Double-blind RCT | Clinical + EDS |
UG (Ulnar S–I, below MN) vs. UG (Radial S–I, below MN) 1 cc triamcinolone (40 mg/mL) |
30/30 | 51.7/52.67 | NR | NR | Mild to moderate | VAS BCTQ EDS CSA of MN |
3 months | No AE reported |
| Mezian et al. (2021) [46] | Double-blind RCT | Clinical + EDS + US |
UG (Ulnar S–I, below MN) Perineural vs. Peritendinous 1 mL methylprednisolone (40 mg/mL) + 1 mL trimecaine hydrochloride |
23/23 | 50/54.3 | 78.3/82.6 | 5.9/5.9 | At least mild CTS | VAS BCTQ, Physical findings Grip strength EDS CSA of MN |
3 months | No AE reported |
| Yeom et al. (2021) [68] | Retrospective study | Clinical + EDS + US |
UG (Radial S–I, below MN) 1 mL triamcinolone (40 mg/mL) + 1 mL of 1% lidocaine |
40 | 59.6 | 77.5 | 15.8 | NR | BCTQ Q-DASH, percentage of treatment failure |
Mean 16 months (range 7 to 43 months) | No AE reported |
| Wang (2021) [47] | Single-blind RCT | Clinical + EDS |
UG (Ulnar S–I, above and below MN) 1 mL triamcinolone (10 mg/mL) + 1 mL 2% lidocaine + 8 mL NS vs. 1 mL triamcinolone (10 mg/mL) + 1 mL 2% lidocaine |
32/32 | 52.87/53.28 | 75/87.5 | 22.93/24.31 | Mild to moderate | BCTQ EDS |
12 weeks | 2 patients in the hydrodissection group reported minor post-injection pain on the first day after the intervention that resolved spontaneously |
| Mathew et al. (2022) [48] | Open-label parallel RCT (non-blind) |
Clinical + EDS |
UG (Ulnar S–I, around MN) Dexamethasone 8 mg (2 mL) + 2 mL 0.5% bupivacaine) vs. Triamcinolone 40 mg/mL (1 mL) + 2 mL 0.5% bupivacaine + 1 mL NS |
33/36 | 42.64/45.22 | 80.6/87.1 | NR | Mild to moderate | VAS BCTQ EDS Phalen’s test |
4 months | No AE reported |
CTS: carpal tunnel syndrome; RCT: randomized controlled trial; UG: ultrasound-guided; NS: normal saline; VAS: visual analog scale; NR: not reported; AE: adverse effect; BCTQ: Boston Carpal Tunnel Syndrome Questionnaire; EDS: electrodiagnostic study; CSA: cross-sectional area; MN: median nerve; 2PD: two-point discrimination; Ulnar S–O: ulnar short-axis out-of-plane; Ulnar S–I: ulnar short-axis in-plane; Ulnar S–O: ulnar short-axis out-of-plane; Radial S–I: radial short-axis in-plane; PL: palmaris longus tendon; US: ultrasound; DASH: Disabilities of the Arm, Shoulder and Hand.
3.3.2. UPIT with D5W
Among the six studies of UPIT using D5W (Table 5), four were double-blind RCTs [49,50,51,52], one investigated UPIT with D5W vs. normal saline [49], one evaluated UPIT with D5W vs. corticosteroids [50], and two compared different volumes of D5W in UPIT [51,52]. Of the two retrospective case series [73,74], one reported the long-term outcomes of UPIT with D5W [73] and another evaluated the effectiveness of UPIT with D5W in the post-surgical persistence and recurrence of CTS [74].
Table 5.
Intervention details of included studies using ultrasound-guided D5W injection for treating carpal tunnel syndrome.
| Author, Year | Study Design | Inclusion Criteria |
UG Intervention and Treatment Allocation |
Participant Characteristics | CTS Severity | Outcome Measurements |
Follow-Up | Safety Outcome (n) |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size (Wrists) Cases/Controls | Mean Age (Years) Cases/Controls |
Female (%) Cases/Controls |
Symptom Duration (Months) Cases/Controls |
||||||||
| Wu et al. (2017) [49] | Double-blind RCT | Clinical + EDS |
UG (Ulnar S–I below and above MN) 5 mL D5W vs. 5 mL NS |
30/30 | 58.4/58.1 | 86.7/80 | 44.5/44.4 | Mild to moderate | VAS BCTQ EDS CSA of MN Global assessment of treatment results |
6 months | No AE reported |
| Wu et al. (2018) [50] | Double-blind RCT | Clinical + EDS |
UG (Ulnar S–I below and above MN) 5 mL D5W vs. 3 mL triamcinolone (10 mg/mL) + 2 mL NS |
27/27 | 58.6/54.3 | 81.4/77.7 | 46.8/45.6 | Mild to moderate | VAS BCTQ EDS CSA of MN Global assessment of treatment results |
6 months | No AE reported |
| Lin et al. (2020) [51] | Randomized, double-blind, three-arm trial | Clinical + EDS |
UG (Radial S–I below and above MN) 4 mL D5W vs. 2 mL D5W vs. 1 mL D5W |
21/21/21 | 58.4/55.2/60.3 | 95.2/81/81 | 54.4/20.6/49.8 | NR | VAS BCTQ Q-DASH EDS CSA of MN |
6 months | No AE reported |
| Lin et al. (2021) [52] | Randomized, double-blind, three-arm trial | Clinical + EDS |
UG (Radial S–I below and above MN) 4 mL D5W vs. 2 mL D5W vs. 1 mL D5W |
17/14/14 | 56.9/52.9/59.2 | 94.1/85.7/85.7 | 66/21.9/58.4 | NR | Mobility, shear wave elastography CSA of MN VAS BCTQ |
6 months | NR |
| Li et al. (2021) [73] |
Retrospective study | Clinical + EDS |
Mean 2.2 UG injections with 10 mL D5W (Ulnar S–I below and above MN + L–I from proximal to distal) | 185 | 55.4 | 65.4 | 30.8 | All grades | VAS Surgical rate |
At least 1 year (1–3 years) post-injection (mean 15.8 months) | No AE reported |
| Chao et al. (2022) [74] |
Retrospective study | Clinical + EDS |
Mean 3.1 UG injections with 10 mL D5W (Ulnar S–I below and above MN + L–I from proximal to distal) | 36 | 59.2 | 77.8 | 15.1 | Persistent or recurrent CTS after surgery | VAS | At least 6 months (6–67 months) post-injection (mean 33 months) | No AE reported |
CTS: carpal tunnel syndrome; RCT: randomized controlled trial; VAS: visual analog scale; NR: not reported; AE: adverse effect; BCTQ: Boston Carpal Tunnel Syndrome Questionnaire; NS: normal saline; EDS: electrodiagnostic study; CSA: cross-sectional area; MN: median nerve; Q-DASH: Quick Disabilities of the Arm, Shoulder and Hand score; Ulnar S–I: ulnar short-axis in-plane; Radial S–I: radial short-axis in-plane; D5W: 5% dextrose in water.
3.3.3. UPIT with PRP
Seven studies evaluated the effectiveness UPIT with PRP [53,54,55,56,57,69,75] (Table 6). Of these studies, one RCT and one case study compared PRP with splint use [53,69], two RCTs compared PRP with normal saline [54,57], one RCT compared PRP with steroids [55], and one RCT compared PRP with D5W [56].
Table 6.
Intervention details of included studies using ultrasound-guided PRP injection for treating carpal tunnel syndrome.
| Author, Year | Study Design |
Inclusion Criteria |
UG intervention and Treatment Allocation |
Participant Characteristics | CTS Severity |
Outcome Measurements |
Follow-Up | Safety Outcome (n) |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size (Wrists) Cases/Controls | Mean Age (Years) Cases/Controls |
Female (%) Cases/Controls |
Symptom Duration (Months) Cases/Controls |
||||||||
| Malahias et al. (2015) [75] | Pilot study (Case series) |
NR | UG (Ulnar S–I below MN) 1–2 mL PRP |
14/0 | 61.5 | 92% | NR (Minimum of 3-month duration of symptoms) |
Mild to moderate |
Q-DASH VAS |
3 months | No AE reported |
| Wu et al. (2017) [53] |
Single-blind RCT | Clinical + EDS |
UG (Ulnar S–I below and above MN) 3 mL PRP vs. Splint |
30/30 | 57.87/54.27 | 90%/8 3.3% | 34.43/30.7 | Mild to moderate |
VAS BCTQ EDS CSA of MN Finger pinch strength |
6 months | No AE reported |
| Malahias et al. (2018) [54] | Double-blind RCT | Clinical | UG (Ulnar S–I below MN) 2 mL PRP vs. NS |
26/24 | 60.4/57.1 | NR | NR (Minimum of 3-month duration of symptoms) |
Mild to moderate |
VAS Q-DASH Delta- CSA of MN |
3 months | No AE reported |
| Guven et al. (2019) [69] | Prospective quasi-experimental | Clinical + EDS |
UG (above MN, no mentioned approach side) 1 mL PRP + splint vs. Splint |
20/20 | 47.5/50 | 94.4/91.6 | 72/60 | Mild to moderate |
BCTQ EDS CSA of MN Monofilament testing score Static 2PD testing score Dynamic 2PD testing score |
4 weeks | No AE reported |
| Senna et al. (2019) [55] | Single-blind RCT | Clinical + EDS |
UG (Ulnar S–I above MN) 2 mL PRP vs. Corticosteroid |
43/42 | 38.3/40.7 | 81.4/85.7 | NR | Mild to moderate | VAS BCTQ EDS CSA of MN Paresthesia Phalen’s maneuver Tinel’s sign |
3 months | No AE reported |
| Shen et al. (2019) [56] | Single-blind RCT | Clinical + EDS |
UG (Ulnar S–I below and above MN) 3 mL PRP vs. 3 mL D5W |
26/26 | 56.8/58.5 | 96.2/84.6 | 58.3/37.5 | Moderate | BCTQ EDS CSA of MN |
6 months | No AE reported |
| Chen et al. (2021) [57] | Double-blind RCT | Clinical + EDS |
UG (Ulnar S–I below and above MN) 3.5 mL PRP vs. NS |
24/24 | 53/53 | 87.5/87.5 | 35.3/36.2 | Moderate to severe | BCTQ EDS CSA of MN |
1 year | No AE reported |
CTS: carpal tunnel syndrome; RCT: randomized controlled trial; Q-DASH: Quick Disabilities of the Arm, Shoulder and Hand score; VAS: visual analog scale; NR: not reported; AE: adverse effect; BCTQ: Boston Carpal Tunnel Syndrome Questionnaire; VAS: visual analog scale; PRP: platelet-rich plasma; D5W: 5% dextrose in water; EDS: electrodiagnostic study; CSA: cross-sectional area; MN: median nerve; 2PD: two-point discrimination; Delta-CSA: cross-sectional area of the median nerve at the tunnel’s inlet, minus the median nerve, proximal to the tunnel and overpronator quadratus.
3.3.4. UPT with Other Injectates
Of the five other RCTs of UPIT using other injectates [58,59,60,61,62] (Table 7), one compared HA with normal saline [58]; one evaluated hyaluronidase vs. steroids [59]; one investigated hyaluronidase vs. normal saline [60]; one compared insulin alone vs. steroids alone, steroids alone, and steroids followed by insulin [61]; and one evaluated ozone vs. steroids [62].
Table 7.
Intervention details of included studies using ultrasound-guided hyaluronic acid, hyaluronidase, insulin, and ozone injection for treating carpal tunnel syndrome.
| Author, Year | Study Design |
Inclusion Criteria |
UG Intervention and Treatment Allocation |
Participant Characteristics | CTS Severity |
Outcome Measurements |
Follow-Up | Safety Outcome (n) |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size (Wrists) Cases/Controls | Mean Age (Years) Cases/Controls |
Female (%) Cases/Controls |
Symptom Duration (Months) Cases/Controls |
||||||||
| Su et al. (2021) [58] | Double-blind RCT | Clinical + EDS |
UG (Long-axis from proximal to distal, above MN) 2.5 mL HA vs. 2.5 mL NS |
17/15 | 50.9/58.9 | 76.5/80 | 35.6/28.6 | Mild to moderate | NRS BCTQ EDS CSA of MN |
6 months | No AE reported |
| Alsaeid et al. (2019) [59] | Double-blind RCT | Clinical + EDS + US |
UG (Ulnar S–I above and below MN) 300 units IU hyaluronidase in 2 mL NS + 3 mL 0.5% plain bupivacaine vs. 2 mL (8 mg) dexamethasone) + 3 mL 0.5% plain bupivacaine |
20/20 | 40.18/42.76 | 55/50 | NR | Mild to moderate | BCTQ EDS CSA of MN Echogenicity score + mobility score + vascularity score of MN |
6 months | NR |
| Elawamy et al. (2020) [60] |
Double-blind RCT | Clinical + EDS |
UG (Ulnar S–I above MN) 1500 IU hyalase in 10 mL NS vs. 10 mL NS |
30/30 | 40.7/38.3 | 56.7/56.7 | 8.5/8.5 | Mild to moderate | VAS Modified BCTQ EDS CSA Power Doppler of MN |
6 months | No AE reported |
| Kamel et al. (2019) [61] | Single-blind RCT | Clinical + EDS |
UG (Ulnar S–I above MN) 10 IU insulin * 2 times (2 weeks interval) vs. 40 mg methylprednisolone vs. 40 mg methylprednisolone + 10 IU insulin * 2 times after 2 and 4 weeks |
20/20/20 | 40.7/44.7/38.3 | 85/90/90 | 8.5/8.1/7.5 | Mild to moderate | Modified BCTQ EDS Physical finding CSA Power Doppler of MN |
10 weeks | NR |
| Forogh et al. (2021) [62] |
Double-blind RCT | Clinical + EDS |
UG (Ulnar S–I above MN) 3 mL ozone (O2–O3) (10 μg/mL) + 1 mL lidocaine vs. 40 mg triamcinolone + 1 mL lidocaine |
20/20 | 54.7/53.65 | NR | 9.1/10.85 | Mild to moderate | VAS BCTQ EDS Circumference and CSA of MN |
3 months | NR |
CTS: carpal tunnel syndrome; RCT: randomized controlled trial; NRS: numeric rating scale; VAS: visual analog scale; NR: not reported; US: ultrasound; AE: adverse effect; BCTQ: Boston Carpal Tunnel Syndrome Questionnaire; NS: normal saline; UG: ultrasound-guided; EDS: electrodiagnostic study; CSA: cross-sectional area; MN: median nerve; Ulnar S–I: ulnar short-axis in-plane; HA: hyaluronic acid.
3.4. UPCTR Study Characteristics
Of the 24 included studies for UPCTR, (Table 8) there were four RCTs [63,64,65,66]: two investigated UPCTR using a hook knife vs. mini-OCTR [63,64]; one compared miniscalpel needles plus steroid injection with corticosteroid injection only [65]; and one evaluated a U-shaped probe/trough plus 5 mm Dovetail blades vs. OCTR [66]. There were four case-cohort UPCTR studies [17,70,71,72]: one compared UPCTR with mini-OCTR [17]; one investigated UPCTR vs. OCTR [72]; one evaluated UPCTR using a 22 G hypodermic needle vs. UPCTR plus corticosteroid injection [70]; and the last case-cohort study compared the use of a UPCTR of an uncoated multifilament stainless steel wire looped thread with no interventions [71]. Among 16 case series [76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91], six investigated the effects of different hook knives [76,79,81,82,87,89], five evaluated the use of microknives [80,83,85,86,88], two analyzed loop threads [77,78], one assessed a microblade [84], and one investigated an 18 G needle with a tip bent in the opposite direction to the needle bevel [90].
Table 8.
Summary of the intervention details in the included studies using ultrasound-guided percutaneous carpal tunnel release.
| Author, Year | Study Design | Inclusion Criteria |
UG Intervention (Device) and Treatment Allocation |
Participant Characteristics | CTS Severity | Outcome Measurements |
Follow-Up | Safety Outcome | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size (Wrists) Cases/Controls | Mean Age (Years) Cases/Controls |
Female (%) Cases/Controls |
Symptom Duration (Months) Cases/Controls |
||||||||
| Nakamichi et al. (2010) [17] |
Controlled trial | Clinical + EDS |
UPCTR (NR device) vs. Mini-OCTR |
25/39 | 58 (all patients) |
100 (all patients) |
NR | NR | EDS Sensibility (static 2-point discrimination, monofilament) Grip and key pinch strength Pain Scar sensitivity |
24 months | No AE reported |
| Capa-Grasa et al. (2014) [63] |
RCT | Clinical + EDS |
UPCTR (Acufex 3.0 mm hook knife) vs. Mini-OCTR |
20/20 | 63/58 | 90/85 | 37/38 | NR | Q-DASH Grip strength, time to stopping oral analgesics, complete wrist flexion and extension, relieving paresthesia, and returning to normal daily activities |
3 months |
No AE reported |
| Chern et al. (2015) [76] |
Case series | Clinical | UPCTR (custom-made hook knife) |
91 | 58 | 77.5 | 48 | NR | BCTQ Sensibility (2-point discrimination, monofilament) Grip, key pinch, and three-jaw chuck pinch strength |
12 months | No AE reported |
| Guo et al. (2015) [77] |
Case series | Clinical | UPCTR (GuoPercutaneousWire™ looped thread) |
34 | 52 | 60 | >12 months | NR | BCTQ | 3 months |
Self-limited wrist swelling 3 weeks after the procedure (1) |
| Rojo-Manaute et al. (2016) [64] |
RCT | Clinical + EDS |
UPCTR (Acufex 3.0 mm hook knife) vs. Mini-OCTR |
46/46 | 58/59 | 58.7/63 | 36/36 | NR | Q-DASH Grip strength, pain scores, time to stopping oral analgesics, complete wrist flexion and extension, 2-point discrimination, relieving paresthesia, and returning to normal activities |
12 months | UPCTR group No AE reported Mini-OCTR Group CRPS (2) Superficial infection (1) |
| Guo et al. (2017) [78] |
Case series | Clinical + EDS + US |
UPCTR (loop and shear looped thread) |
159 | 54.83 | 66.3 | Most >1 year | NR (either failed conservative treatment or requested a surgical release) |
BCTQ | 12 months | Infection (2) Self-limited pillar pain at 2–6 weeks (8) |
| Petrover et al. (2017) [79] |
Prospective, open-label study | Clinical + EDS |
UPCTR (Acufex 3.0 mm hook knife) |
129 | 61.5 | 69.7 | >6 months | NR (failed on conservative treatment) |
BCTQ | 6 months | No AE reported |
| Guo et al. (2018) [70] |
Controlled trial | Clinical + EDS + US |
UPCTR (22 G hypodermic needle) vs. UPCTR + CSI |
25/25 | 50.52/48.64 | 79.1/68 | 20.92/19.32 | Early to middle stage | Global assessment of treatment results CSA of MN EDS |
3 months | No AE reported |
| Henning et al. (2018) [80] |
Case series | Clinical + EDS |
UPCTR (SX-One MicroKnife) |
22 | 64 | NR | NR | NR | BCTQ Q-DASH |
3 months | No AE reported |
| Luanchumroen (2019) [81] |
Case series | Clinical + EDS |
UPCTR (Acufex 3.0 mm hook knife) |
20 | 55 | 87.5 | >6 months | Moderate to severe | BCTQ CSA of MN EDS |
6 months | Transient paresthesia for 1–2 weeks (5) |
| Wang et al. (2019) [82] |
Case series | Clinical + EDS |
UPCTR (hook knife) |
113 | 61 | 66.6 | 24 | Hemodialysis patient who had failed on conservative treatment >3 months |
BCTQ Sensibility (2-point discrimination, monofilament) Grip and pinch strength |
2 years | No AE reported |
| Zhang et al. (2019) [65] |
RCT | Clinical + EDS |
UPCTR (Hanzhang miniscalpel needle) + CSI vs. CSI |
23/23 | 48.7/53.1 | 78.2/73.9 | 10.2/11.1 | NR | BCTQ EDS CSA of MN |
12 weeks | No AE reported |
| Chappell et al. (2020) [83] |
Case series | Clinical | UPCTR (SX-One MicroKnife) |
37 | 62 | 30.4 | 26% <1 year 39% 1 to 5 years 31% >5 years 4% NR |
Severe or failed on conservative treatment | BCTQ CSA of MN |
10 weeks | No AE reported |
| Hebbard et al. (2020) [84] |
Case series | Clinical + EDS |
UPCTR (MICROi-Blade) |
166 | 57 | 46.3 | NR | NR | BCTQ Days of return to work |
6 months | Self-limited post-operative numbness for 1–3 weeks (several) Post-operative swelling resolved with CSI (2) |
| Joseph et al. (2020) [85] |
Case series | Clinical + US |
UPCTR (SX-One MicroKnife) |
35 | 60 | 59.1 | NR | NR (Failed on conservative treatment >6 months) |
BCTQ Q-DASH |
3 months | No AE reported |
| Burnham et al. 2021 [71] | Controlled trial | Clinical + EDS + US |
UPCTR (sterile uncoated multifilament stainless steel wire looped thread) vs. No intervention |
40/20 | NR | 55 | >3 months | Moderate to severe | BCTQ CSA of MN EDS Sensibility (Semmes–Weinstein monofilaments) Grip and pinch strength) |
6 months | No AE reported |
| Kamel et al. (2021) [86] | Case series | Clinical + US |
UPCTR (SX-One MicroKnife) |
61 | 61 | 54.3 | NR | NR (Failed on conservative treatment >6 months) |
BCTQ Q-DASH |
>1 year (median: 20 months) | Infection after a fall on open wound on post-op day 8 (1) Post-traumatic compartment syndrome on post-op day 10 after wrist injury (1) |
| Wang et al. (2021) [87] |
Case series | Clinical + EDS |
UPCTR (ECTRA or E-Z knife hook knife) |
641 | 60 | 64.1 | 29 | NR (Failed on conservative treatment >3 months or thenar muscle atrophy or weakness) |
BCTQ Sensibility (2-point discrimination) Grip strength |
24 months | Transient nerve palsy for 6 week (1) |
| Leiby et al. (2021) [88] | Case series | Clinical + US |
UPCTR (SX-One MicroKnife) |
76 | 58 | 57.4 | NR | NR | BCTQ Q-DASH |
12 months | No AE reported |
| Fuente et al. (2021) [66] | Open RCT | Clinical + EDS |
UPCTR (U-shaped probe/ trough + 5 mm dovetail blades) vs. OCTR |
47/42 | 46.7/49.1 | 51.1/57.1 | NR | NR | BCTQ Sensibility (2-point discrimination) Grip strength |
12 months | UPCTR group epineural fibrosis (1) OCTR group CRPS (1) |
| Loizides et al. (2021) [89] | Case series | Clinical + EDS |
UPCTR (button tip cannula + hook knife) |
104 | 60.6 | 64.4 | NR | NR | US of FR Simplified BCTQ |
2 weeks | Sparse hematoma at the incision site |
| Lee et al. (2021) [90] | Prospective case series | Clinical | UPCTR (18 G needle tip bent in the opposite direction to the needle bevel) |
188 | 54.7 | 71 | 50.3 weeks | NR (Failed on conservative treatment) |
NRS | 6 months | No AE reported |
| Fowler (2022) [91] |
Multicenter observational study | Clinical + EDS |
UPCTR (UltraGuideCTR device) |
427 | 55 | 71 | 11.6% ≤6 months 21.6% >6 months to 1 year 15.1% >1 year to 2 years 51.7% >2 years |
NR | Q-DASH BCTQ Time to return to normal activities |
6 months | Incomplete release (1) |
| Asserson et al. 2022 [72] |
Retrospective study | Clinical + EDS |
UPCTR (NR device) vs. OCTR |
18/17 | 52.1/47.3 | 72.2/88.2 | NR | NR | Day of return the work | 52 weeks | No AE reported |
CTS: carpal tunnel syndrome; RCT: randomized controlled trial; NRS: numeric rating scale; VAS: visual analog scale; NR: not reported; US: ultrasound; AE: adverse effect; BCTQ: Boston Carpal Tunnel Syndrome Questionnaire; NS: normal saline; UG: ultrasound-guided; EDS: electrodiagnostic study; CSA: cross-sectional area; MN: median nerve; Q-DASH: Quick Disabilities of the Arm, Shoulder and Hand score; UPCTR: ultrasound-guided percutaneous carpal tunnel release; FR: flexor retinaculum; OCTR: open carpal tunnel release; CSI: corticosteroid injection.
3.5. Meta-Analysis Results
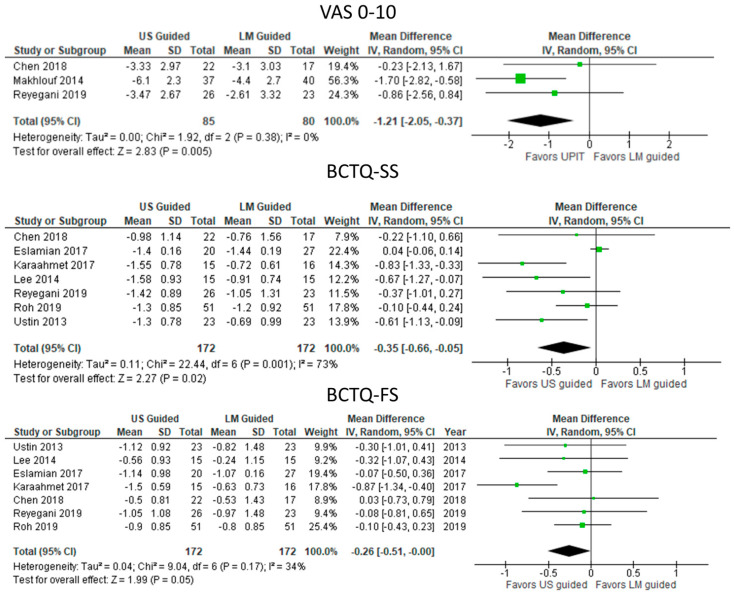
3.5.1. UPIT with Steroids vs. Landmark-Guided Steroid Injection (Figure 2)
Figure 2.
Meta—analysis of UPIT with steroids vs. landmark-guided steroid injection. US, ultrasound; LM, landmark; VAS, visual analogue scale; BCTQ—SS, Boston Carpal Tunnel Questionnaire—symptom scale; BCTQ—FS, Boston Carpal Tunnel Questionnaire—functional scale. The green squares represent the differences between the means of each of the two groups compared, i.e., the mean differences. The size of the green square represents how much that individual study affects the overall outcome of the meta—analysis, i.e., the weight of the studies on the meta—analysis. The precision of the study depends on the 95% confidence interval for that mean difference, i.e., the length of the straight lines, the shorter the lines, the more precise the mean differences. The black trapezoid is the pooled mean difference of all the studies combined in consideration of the weight of each study, with its confidence interval extending from the left tip to the right tip.
Steroid injection by ultrasound guidance reduced symptoms significantly more than landmark guidance in the pooled results with variable heterogeneity, as indicated by improvement in VAS0-10 (MD: −1.21 [95% CI: −2.05 to −0.37]; p = 0.005) and BCTQ-SS (MD: −0.35 [95% CI: −0.66 to −0.05]; p = 0.02). Functional improvement (BCTQ-SF) was significantly greater after ultrasound-guided steroid injection (MD: −0.26 [95% CI: −0.51 to −0.00] p = 0.05) with low heterogeneity (I2 = 34%).
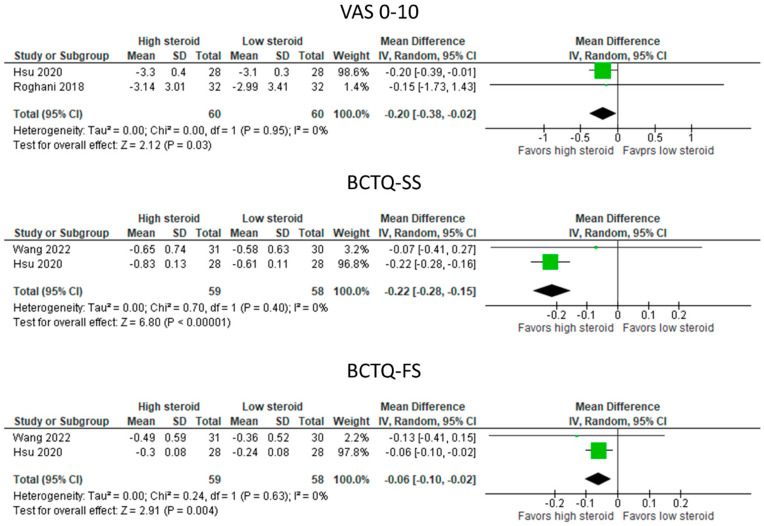
3.5.2. UPIT with High-Dose vs. Low-Dose Steroids (Figure 3)
Figure 3.
Meta—analysis of UPIT with high—dose vs. low—dose steroids. VAS, visual analogue scale; BCTQ—SS, Boston Carpal Tunnel Questionnaire—symptom scale; BCTQ—FS, Boston Carpal Tunnel Questionnaire—functional scale. The green squares represent the differences between the means of each of the two groups compared, i.e., the mean differences. The size of the green square represents how much that individual study affects the overall outcome of the meta—analysis, i.e., the weight of the studies on the meta—analysis. The precision of the study depends on the 95% confidence interval for that mean difference, i.e., the length of the straight lines, the shorter the lines, the more precise the mean differences. The black trapezoid is the pooled mean difference of all the studies combined in consideration of the weight of each study, with its confidence interval extending from the left tip to the right tip.
Higher doses of steroid injection by ultrasound guidance reduced symptoms significantly more than lower doses of steroids in the pooled results with low heterogeneity (I2 = 0%), as indicated by improvement in VAS0-10 (MD: −0.020 [95% CI: −0.38 to −0.02]; p = 0.03) and BCTQ-SS (MD: −0.22 [95% CI: −0.28 to −0.15]; p < 0.00001). Functional improvement (BCTQ-SF) was significantly greater after ultrasound guidance (MD: −0.06 [95% CI: −0.10 to −0.02] p = 0.004).
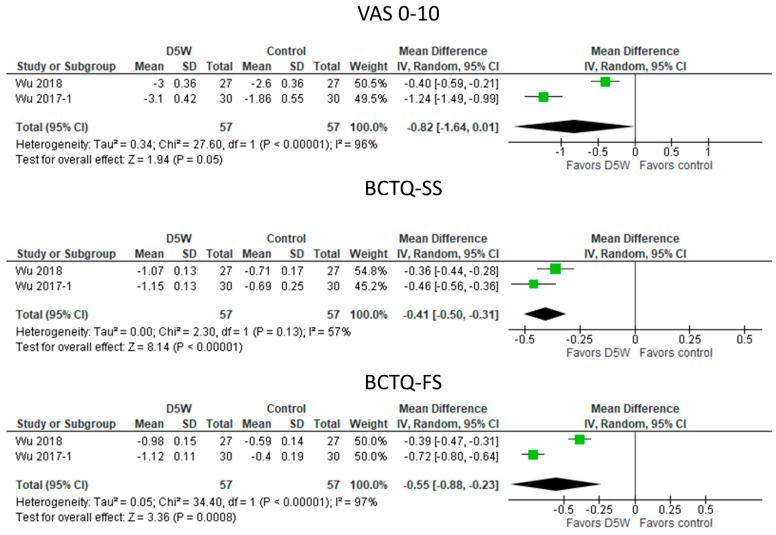
3.5.3. UPIT with D5W vs. Control Injections (Figure 4)
Figure 4.
Meta—analysis of UPIT with D5W vs. control injections. VAS, visual analogue scale; BCTQ—SS, Boston Carpal Tunnel Questionnaire—symptom scale; BCTQ—FS, Boston Carpal Tunnel Questionnaire—functional scale. The green squares represent the differences between the means of each of the two groups compared, i.e., the mean differences. The size of the green square represents how much that individual study affects the overall outcome of the meta—analysis, i.e., the weight of the studies on the meta—analysis. The precision of the study depends on the 95% confidence interval for that mean difference, i.e., the length of the straight lines, the shorter the lines, the more precise the mean differences. The black trapezoid is the pooled mean difference of all the studies combined in consideration of the weight of each study, with its confidence interval extending from the left tip to the right tip.
UPIT with D5W reduced symptoms significantly more than UPIT with either triamcinolone (Wu, 2018) or saline (Wu, 2017-1) in the pooled results with moderate to high heterogeneity, as indicated by improvement in VAS0-10 (MD: −0.82 [95% CI: −1.64 to 0.01]; p = 0.05) and BCTS-SS (MD: −0.41 [95% CI: −0.50 to −0.31]; p < 0.00001). Functional improvements were significantly greater with UPIT using D5W as the injectate (MD: −0.55 [95% CI: −0.88 to −0.33]; p = 0.0008), with high study heterogeneity (I2 = 97%).
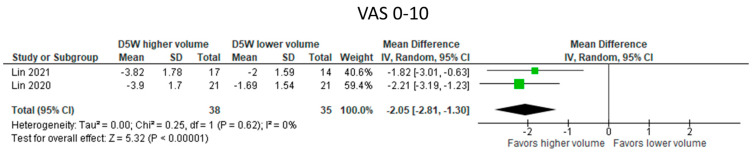
3.5.4. UPIT with Higher Volumes of D5W vs. Lower Volumes of D5W (Figure 5)
Figure 5.
Meta—analysis of UPIT with higher volumes of D5W vs. lower volumes of D5W. VAS, visual analogue scale. The green squares represent the differences between the means of each of the two groups compared, i.e., the mean differences. The size of the green square represents how much that individual study affects the overall outcome of the meta—analysis, i.e., the weight of the studies on the meta—analysis. The precision of the study depends on the 95% confidence interval for that mean difference, i.e., the length of the straight lines, the shorter the lines, the more precise the mean differences. The black trapezoid is the pooled mean difference of all the studies combined in consideration of the weight of each study, with its confidence interval extending from the left tip to the right tip.
Data for BCTS subscales were unavailable. Symptom improvements, however, were significantly greater with higher volumes of D5W than with lower volumes of D5W (4 mL vs. 1 mL D5W; MD: −2.21 [95% CI: −3.19 to −1.23]; p < 0.00001).
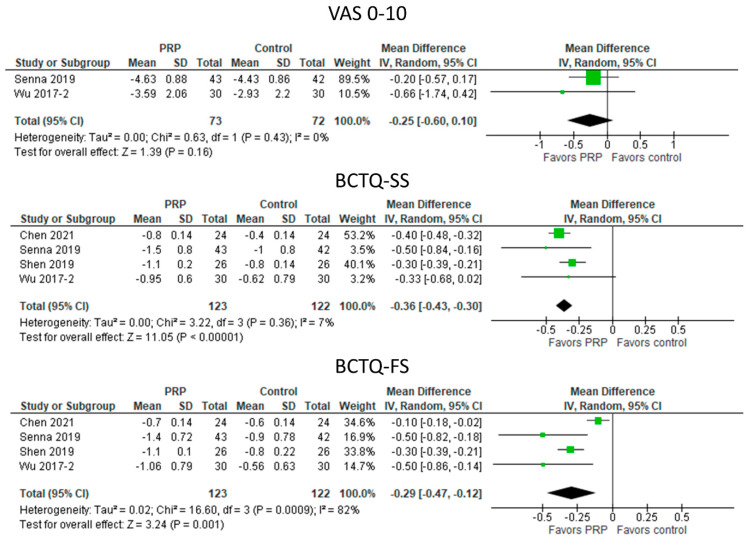
3.5.5. UPIT with PRP vs. Control Treatments (Figure 6)
Figure 6.
Meta—analysis of UPIT with PRP vs. control treatments. VAS, visual analogue scale; BCTQ—SS, Boston Carpal Tunnel Questionnaire—symptom scale; BCTQ—FS, Boston Carpal Tunnel Questionnaire—functional scale. The green squares represent the differences between the means of each of the two groups compared, i.e., the mean differences. The size of the green square represents how much that individual study affects the overall outcome of the meta—analysis, i.e., the weight of the studies on the meta—analysis. The precision of the study depends on the 95% confidence interval for that mean difference, i.e., the length of the straight lines, the shorter the lines, the more precise the mean differences. The black trapezoid is the pooled mean difference of all the studies combined in consideration of the weight of each study, with its confidence interval extending from the left tip to the right tip.
UPIT with PRP did not significantly reduce VAS0-10 compared with the control treatment. However, the reduction in symptoms, as measured by BCTQ-SS, was significantly greater after UPIT with PRP (MD: −0.36 [95% CI −0.43 to −0.30]; p < 0.00001). In addition, functional improvement also favored treatment with PRP injection (MD: −0.29 [95% CI: −0.47 to −0.12]; p = 0.001).
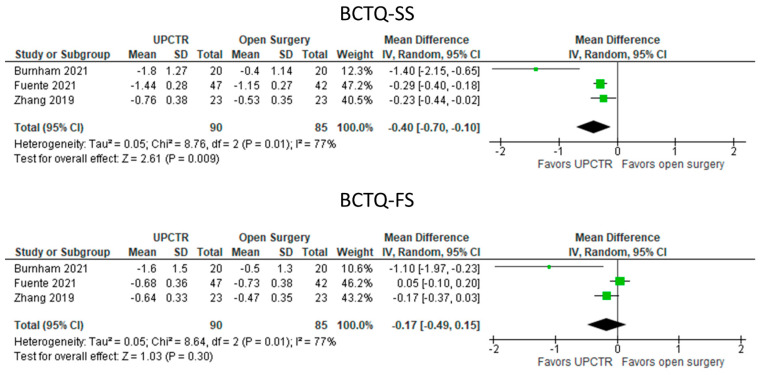
3.5.6. UPCTR Vs. Surgery (Figure 7)
Figure 7.
Meta—analysis of UPCTR vs. surgery. BCTQ—SS, The Boston Carpal Tunnel Questionnaire—symptom scale; BCTQ—FS, The Boston Carpal Tunnel Questionnaire—functional scale. The green squares represent the differences between the means of each of the two groups compared, i.e., the mean differences. The size of the green square represents how much that individual study affects the overall outcome of the meta—analysis, i.e., the weight of the studies on the meta—analysis. The precision of the study depends on the 95% confidence interval for that mean difference, i.e., the length of the straight lines, the shorter the lines, the more precise the mean differences. The black trapezoid is the pooled mean difference of all the studies combined in consideration of the weight of each study, with its confidence interval extending from the left tip to the right tip.
Comparative VAS0-10 data were unavailable. UPCTR outperformed open surgery in terms of symptom improvement (MD: −0.40 [95% CI: −0.70 to −0.10]; p = 0.009), but functional improvements were not significantly different between UPCTR and open surgery.
4. Discussion
4.1. Meta-Analysis Findings
We found that UPIT with steroids significantly improved symptoms and function in carpal tunnel syndrome compared with landmark guidance and UPIT with high-dose steroids was superior to that with low-dose steroids. Meta-analyses on UPIT with D5W or PRP showed that these treatments outperformed their corresponding controls, including steroid injections. Further investigations are needed to determine the relative cost-effectiveness of D5W vs. PRP injections for CTS. Meta-analyses of the effects of UPCTR vs. open surgery revealed that UPCTR was at least as efficacious as open surgery and performed better in terms of symptom reduction, but not functional improvement.
4.2. Literature Review of UPIT
The mechanisms of UPIT for CTS can be either mechanical (hydrodissection) or pharmacological effects.
4.2.1. Mechanical Effect (Hydrodissection)
Hydrodissection can extricate the entrapped MN from the surrounding adhesive/compressive tissue by exerting a non-specific effect of fluid-under-force to further increase the blood flow and alleviate nerve compression injury [92,93,94,95]. Extrication with an associated restoration of MN kinematics breaks the vicious cycle of compression, inflammation, SSCT fibrosis, and nerve ischemia and could contribute to subsequent nerve regeneration [49,53,92,95]. Evers et al. [96] reported that hydrodissection with normal saline (NS) reduces MN gliding resistance within the carpal tunnel in the cadaveric wrist. This effect cannot be explained based on the fluid lubrication effect, as it persists without degradation over 1000 repetitions. Wu et al. [93] confirmed the clinical benefits of hydrodissection with NS for mild-to-moderate CTS. A single injection of 5 mL NS resulted in medium-term (6-month) symptom reduction and decreased MN CSA. In addition, a study comparing three different injectate volumes (1, 2, or 4 mL) showed that hydrodissection with a higher volume of injectate yielded better nerve mobility and decreased MN CSA [52]. Simultaneous hydrodissection above and below the MN was more effective than only hydrodissection between the FR and MN [97]. The minimum volume requirement for an optimum mechanical effect and whether this effect includes a beneficial effect from the NS require further investigations.
4.2.2. UPIT Results by Injectate
Corticosteroids (Table 1)
In recent decades, corticosteroids have been the most frequently used ultrasound-guided injectate for CTS. The proposed primary mechanism of corticosteroid injection benefit in CTS is a reduction in intracarpal pressure via exertion of an anti-inflammatory effect, decompressing the nervi nervorum, rather than a direct pharmacological effect on the MN [98]. Various ultrasound-guided techniques for CTS treatment by corticosteroid injection have been reported, with inconclusive results for comparative effectiveness but intriguing preliminary findings. No significant differences were reported in the subjective and objective measurements between perineural and peritendinous (between carpal bone) corticosteroid injections through 12 weeks of follow-up [46]. Babaei-Ghazani et al. [40] concluded that ultrasound-guided corticosteroid injection above or below the MN was equally effective in symptom reduction, functional improvement, and electrophysiologic and sonographic findings. Hsu et al. [67] reported that intraepineurial corticosteroid injections outperformed extraepineurial injections in improving patient satisfaction, symptom relief, and MN CSA. Lee et al. [34] showed that a short-axis in-plane approach below and above the MN improved the symptoms, function, CSA, and electrophysiological parameters more than a short-axis out-of-plane approach below the MN. Rayegani et al. [43] demonstrated that a long-axis in-plane approach above the MN tended to decrease CSA more than did a short-axis in-plane approach below the MN; however, the between-group difference did not reach significance. Babaei-Ghazani et al. [45] revealed no differences between ultrasound-guided short-axis ulnar and radial injection direction approaches for CTS. Wang et al. [47] showed that ultrasound-guided hydrodissection using triamcinolone or corticosteroid perineural injection alone resulted in clinical and electrophysiological improvement in patients with CTS, but hydrodissection did not offer additional benefits. However, the hydrodissection techniques in Wang et al.’s study have been considered imperfect [99], and the volume and concentration of steroids used for hydrodissection and perineural injection were different, which might be interventional confounding variables [99]. Although a few studies showed similar efficacy between landmark-based and ultrasound-guided injection approaches [36,42], most studies demonstrated that ultrasound-guided injection resulted in significantly greater clinical improvements [33,35,37,39].
The pharmacological effects of corticosteroids may outweigh those of injection techniques, partially explaining the diversity of findings in the studies mentioned above [100]. Moreover, the hydrodissection effects might have been less notable in corticosteroid injection studies as most injection methods used only 1–3 mL of corticosteroids, which might not have been sufficient for an adequate hydrodissection effect. However, Wang et al. [47] conducted a single-blind trial in which the participants were randomly assigned hydrodissection with a mixture of 1 mL of triamcinolone acetonide (10 mg/mL), 1 mL of 2% lidocaine, and 8 mL of NS or perineural injection with 1 mL of triamcinolone acetonide (10 mg/mL) and 1 mL of 2% lidocaine. They reported no additional benefit from the corticosteroid injection of a 10 mL volume compared with that from the injection of a 2 mL volume with the same corticosteroid dosage. This finding suggests that the anti-inflammatory effect of corticosteroids is more important than the hydrodissection effect. However, this conclusion is weakened by a potential bias from a difference in corticosteroid concentration through dilution and the limitation in their techniques of hydrodissection which may have affected the outcome [99].
The follow-up periods of the corticosteroid injection studies varied, with therapeutic benefits reported for 3 months by Lee et al. [34], Üstün et al. [33], and Wang et al. [38] and 6 months and 16 months by Makhlouf et al. [35] and Yeom et al. [68], respectively. Notably, recent trials demonstrated no dose-dependent effect of ultrasound-guided corticosteroid injections [41,44]. Although no difference in clinical outcomes between particulate (triamcinolone acetonide) and non-particulate (dexamethasone sodium phosphate) corticosteroid injections for CTS was observed, the particulate group showed significantly longer post-injection pain duration [48].
The efficacy of ultrasound-guided corticosteroid injection for CTS is uncertain because of the absence of a well-designed control group. The published research only compared different guided methods, i.e., the ultrasound-guided method vs. blind injection or different ultrasound-guided techniques. These published studies might have overestimated the therapeutic effect owing to the absence of a well-controlled placebo group. A Cochrane review concluded that the beneficial effect of corticosteroid injections using a blind technique has only a short-term benefit compared with that of a placebo injection (about one month) [101]. This finding suggests that the medium- and long-term clinical benefits reported represent, in part, a placebo effect. The possible adverse effects of corticosteroids include widespread axonal and myelin degeneration, skin thinning, tendon rupture, soft tissue atrophy, steroid flare, crystal-induced synovitis, and hot flushes [102,103]. Additional randomized, double-blind, controlled trials with well-designed control groups with limited therapeutic activity, such as those administered NS, or active non-steroid treatment comparison groups, are needed to confirm the clinical benefit of ultrasound-guided corticosteroid injection and its comparative risk/benefit ratios.
Five Percent Dextrose in Water (Table 2)
In 2017, Wu et al. [49] first proved that a single hydrodissection with 5 mL D5W, compared with NS hydrodissection, could significantly improve the symptoms, electrophysiological measures, and MN CSA for CTS. Wu et al. [50] subsequently reported the waning benefits of single corticosteroid hydrodissection from 3–6 months in contrast with cumulative improvement in the subjective symptoms and disability associated with single hydrodissection with 5 mL D5W. Lin et al. [51] showed that increasing the volume of D5W showed better efficacy in reducing CTS-related symptoms and disability in a 24-week post-injection follow-up. A higher injectate volume also increased nerve mobility and reduced nerve swelling [52].
Li et al. [73] administered UPIT using D5W with multiple injection sections (mean 2.2 injections with 10 mL D5W), with 1.7 to 3 injections, to achieve an effective outcome over a mean of 15.8 months follow-up, and they found that only 1% (2/185) of the patients ultimately underwent surgery [73]. Given the early level A evidence that hydrodissection with D5W for CTS is likely to outperform or supplement the current conservative treatment approaches and significantly reduce the probability of surgery, this injection is listed as one of the treatment options by UpToDate [104]. In addition, the 20th edition of Harrison’s Principles of Internal Medicine also officially lists this method as an alternative treatment for CTS [105]. Recently, a retrospective study by Chao et al. [74] suggested that UPIT with D5W is clinically important with a durable effect in patients with failure of CTS surgery. They retrospectively followed 36 patients with persistent or recurrent symptoms after CTS surgery for a mean post-injection follow-up of 33 months and symptom relief of more than 50% was reported by 22 patients (61%) after a mean of 3.1 injections of UPIT with 10 mL D5W.
The pharmacological effects of D5W for CTS are still unclear. Theoretically, they include stabilization effects on neural activity, normalization of glucose metabolism, and a decrease in neurogenic inflammation, reducing neuropathic pain via multifactorial mechanisms. Glucose has been speculated to indirectly inhibit capsaicin-sensitive receptors (e.g., transient receptor potential vanilloid receptor-1) and block the secretion of substance P and calcitonin gene-related peptides, which are pro-nociceptive substances involved in neurogenic inflammation [95,106,107,108,109,110,111]. Wu et al. [112] observed that high glucose concentrations could mitigate TNF-α-induced NF-κB activation, upregulation of pro-inflammatory cytokines, and metabolic dysfunction in nerve cells; the in vitro findings support the hypothesized mechanism that glucose may reduce neurogenic inflammation. Moreover, pre-treatment with TNF-α also promotes energy uptake, leading to glucose deprivation [113,114,115,116,117], and glucose exposure could restore impaired glucose metabolism. Additional studies are needed to further explore the apparent ameliorative pharmacological mechanisms of D5W in CTS and its optimal dosage and frequency for CTS injection.
PRP (Table 3)
PRP is rich in various growth factors that can help neural repair and regeneration, as shown by animal and in vitro studies, but PRP must be used at patients’ own expense [118]. Additionally, PRP can reduce the levels of pro-inflammatory cytokines, local inflammation, and intracarpal pressure to normalize the pressure on MN [119]. Since 2015, clinical studies have investigated the efficacy of UPIT with PRP for CTS [53,54,55,57,69,75]. Wu et al. [53] showed that ultrasound-guided PRP injection was more effective for symptom relief and CSA of MN than using a wrist splint for six months. Malahias et al. [54] performed the first double-blind placebo-controlled PRP vs. NS injection trial and found significant between-group differences favoring PRP at the 3-month follow-up. Senna et al. [55] conducted a randomized, single-blind controlled trial and reported that PRP was more effective in reducing the symptoms and improving electrophysiologic measures at three months of post-injection than corticosteroid injection. A non-blind trial with a short-term follow-up (4 weeks) reported no additional benefit from the addition of 1 mL of PRP to the use of a wrist splint for CTS compared with the use of a splint alone. However, that trial had a very short follow-up and the volume used was not expected to produce a hydrodissection effect [69]. Shen et al. [56] compared PRP to D5W administration with a single injection only for moderate CTS. They found more benefits from PRP injection in functional improvement, electrophysiologic measures, and CSA of MN.
In 2021, Chen et al. [57] first demonstrated and compared the long-term efficacy (1-year follow-up) of a single PRP injection vs. NS in terms of symptom relief, functional scores, and MN CSA in a randomized, double-blind, controlled trial. Recently, Lai et al. [120] retrospectively followed up on 81 patients at least two years after a single PRP injection; after a mean of 43.8 months (24–60 months) post-injection follow-up, 70% of patients reported symptom relief >50%. Considering the biological properties of PRP, it is possibly the most effective injectate at present, especially for more severe-grade presurgical CTS. However, further studies with larger sample sizes and comparing PRP with other active injectates for CTS, considering differences in dosage needs and cost efficacy, are needed.
HA, Hyaluronidase, Insulin, or Ozone (Table 4)
Single studies with a small sample size have reported results from the ultrasound-guided injection of HA, hyaluronidase, insulin, or ozone for mild-to-moderate CTS. Studies with larger sample sizes and more extended follow-up periods are needed in the future to evaluate their efficacy or comparative efficacy.
HA
HA, which has anti-adhesion effects, has clinical applications for post-surgical adhesion [121,122]. Su et al. [58] reported that compared with an NS injection, a single ultrasound-guided HA injection had significant efficacy for symptom and functional improvement at two weeks post-injection. Retention of the majority of the HA injectate was still visualizable by ultrasound one hour after injection, while NS was almost completely absorbed. Prolonged HA retention surrounding MN and its anti-adhesion effect may contribute to early symptom relief through lubrication, MN mobility improvement, and decreased pressure within the carpal tunnel [123,124,125].
Hyaluronidase
Hyaluronidase, an enzyme catalyzing the hydrolysis of HA, can reduce viscoelasticity, increase tissue permeability, and allow the local anesthetic to diffuse through the surrounding tissue [126]. Several studies have revealed significant but brief pain reduction from the perineural injection of hyaluronidase in a local anesthetic solution vs. local anesthetic only in symptomatic CTS [126,127,128]. A randomized control trial with mid-term follow-up was conducted to compare hydrodissection under the ultrasound guidance of hyaluronidase vs. dexamethasone for mild-to-moderate CTS [59]; this trial demonstrated significantly greater improvements in the symptoms, function, electrophysiological findings, and CSA of MN in a 6-month follow-up in the hyaluronidase group compared with those in the dexamethasone group [59]. In addition, in 2020, Elawamy et al. [60] reported that ultrasound-guided injection with hyaluronidase combined with NS, compared with NS alone, resulted in significantly more improvements in the pain, function, electrophysiological parameters, and CSA of MN in a 6-month follow-up for mild-to-moderate CTS. The possible mechanism may be that HA accumulates around demyelinated nerves, inhibiting oligodendrocyte precursor cell maturation and remyelination, and injected hyaluronidases can stimulate remyelination via hydrolysis of local HA [60,129].
Insulin
Kamel et al. [61] reported that ultrasound-guided injection with corticosteroids plus insulin, compared with corticosteroids alone, significantly decreased the CSA of MN. However, symptoms and functional outcomes did not differ between the groups. Further research on the use of insulin for injection is anticipated based on the potential role of insulin (e.g., acting like a growth factor) to determine its therapeutic efficacy in compression-related nerve dysfunction [130].
Ozone
Ozone exerts anti-inflammatory and analgesic properties by inhibiting pro-inflammatory mediators [131]. Forogh et al. [62] compared ultrasound-guided injection with ozone vs. corticosteroid for mild-to-moderate CTS in a randomized trial; ozone was non-inferior to corticosteroid injection with respect to pain reduction and functional improvement at the 12-week follow-up, although improvement in electrophysiological parameters and MN CSA was observed only among patients after corticosteroid injection.
4.3. Ultrasound-Guided Percutaneous Carpal Tunnel Release (Table 5)
Studies have confirmed that UPCTR is feasible and it is receiving increasing attention in the literature [21,64]. Compared with the standard-of-care OCTR, UPCTR has the following advantages:
(1) smaller incision size, typically 0.1–0.3 cm only;
(2) better safety due to full-time continuous visualization and monitoring of the neurovascular structures and the instruments while releasing the FR [21];
(3) significantly faster wound healing and resumption of daily activities and work [21], with five studies reporting a return to work as early as the first week post-UPCTR [64,77,78,84];
(4) faster improvement in the short-term functional scores, grip strength, and paresthesia disappearance [21]; and
(5) non-inferior median and long-term outcomes when compared with those of the current standard-of-care OCTR.
Due to the surgery’s minimally invasive nature and much faster healing, five of the included 24 studies reported simultaneous bilateral UPCTR [63,83,84,85,88], which is not feasible when performing mini-OCTR. Early studies have suggested that UPCTR is an effective, relatively safe treatment option for patients with CTS who have failed to respond to conservative treatments.
Ultrasonography helps doctors identify the FR and the structures at risk, e.g., the MN, the recurrent motor branch of MN, third common palmar digital nerve and any unusual distal branches, the superficial palmar arch, and the ulnar artery. For safe and effective transection of FR, a transverse safe zone between the hook of the hamate or ulnar vessels and the MN and another longitudinal safe zone between the superficial palmar arch and the distal FR should be identified by ultrasound. The FR, nerves, blood vessels, other at-risk structures, and safe zones could be identified using ultrasound in all the included studies. To enhance the safety of the transection, in addition to ultrasound visualization of the structures at risk of being damaged by the transection, e.g., the palmar cutaneous branch of the MN and the Berrettini communication between the third and fourth common palmar digital nerves, many studies adopted other measures to enlarge the safe zone. Five clinical trials utilized the ZX-One MicroKnife (Sonex Health, Eagen, MN, USA), which has inflatable balloon buffers [80,83,85,86,88]. Three other studies employed K-wires [63,64,81], two with a Penfill curved elevator [85,88], one with a uterine dilator [86], one with a U-shaped trough/probe [66], and one with a button tip cannula with hydrodissection to enlarge the safe zone [89].
4.3.1. Methods of Ultrasound-Guided Percutaneous Carpal Tunnel Release
The approaches for UPCTR also differ in terms of the direction of entry of the instruments and transection devices and the number of passes required for complete transection. Nineteen studies utilized a proximal to distal instrument entry/incision site and three used a distal entry site in the palm proximal to the superficial palmar arch, usually just distal to the distal end of FR [17,71,78]. Thirteen studies used a hook knife as the transection instrument, which is a retrograde blade; in addition, three, three, and three used a needle, a looped thread, and anterograde blades, respectively. Two main approaches have been employed in the studies using a hook knife. In 10 studies from eight groups, the hook knife was positioned deep at the FR and transected the FR with the blade pointing upward [63,64,79,80,81,83,85,86,88,89]. Three clinical studies by the same group placed the hook knife superficial to the FR, with the blade directed downward [76,82,87]. Regarding passes using a hooked knife, one pass of the blade is generally adequate for the complete transection of the FR (85% or more) [85,88]. Kamel et al. [86] reported that nearly 39% of patients needed two passes for a complete transection in the presence of a markedly thickened FR. Among the studies using anterograde blades, Fuente et al. and Nakamichi et al. employed a single passage to divide the FR [17,66], whereas Hebbard et al. [84] used two to three passes to completely transect the FR. The studies using multiple fenestrations with a needle reported requiring 10–15 fenestrations for a complete UPCTR [65]. The studies using a looped thread typically employed a forward and backward sawing motion to transect the FR [71,77,78]. Only one study by Lee et al. [90] used an 18 G needle with the tip bent to release the FR under ultrasound guidance and by repeated cutting. However, no study has directly compared any two different approaches of UPCTR or any two different devices in the literature. Further studies are needed to evaluate their comparative efficacy.
4.3.2. Potential Cost Benefits of UPCTR
One of the potentially significant benefits of UPCTR is the shortened procedural duration, which may lead to a shorter duration of time in the operation theater or the use of alternate settings, both potentially cost-saving. Only five of the 24 included studies described the average duration of the procedure, which ranged from 5.8 to 16.8 min [77,79,84,86,88]. Eleven studies described the procedural setting, with four performed in the operation theater [76,80,85,88], six in an ambulatory clinic procedure room [63,64,80,81,83,132], and one in an interventional radiology procedure room [79]. The timing of return to work was assessed in five studies. Two reported a return to work time of a combined mean of 4 to 5 days in the UPCTR groups compared with 26 days in the mini-OCTR groups [63,64]. Hebbard et al. [84] reported a mean return to work time of 7 days [84]. Guo et al. [78] reported a mean of 17.7 days in their first case series, but in their second case series, the time to return to work was two weeks for manual workers and one day for office workers. Asserson et al. [72] found that the average time of return to work was 12 days in the UPCTR group and 33 days in the OCTR group. Joseph and Leiby et al. suggested that patients with occupations requiring repetitive or heavy use of hands could return to light duties one week after UPCTR [85,88]. Henning et al. [80] reported that three patients using a crutch or wheelchair could ambulate immediately after UPCTR. Chappell et al. [83] advised patients to avoid strenuous activities for four days, whereas Guo et al. [70] immobilized the treated wrists for three days. Asserson et al. [72] showed that participants in the UPCTR group had an average of 12 days to return to work without restriction, whereas those in the OCTR group had an average of 33 days to return to work. A multicenter case series of UPCTR by Fowler et al. [91], including 373 patients (427 hands), reported a rapid median time to return to normal activities (3 days) or work (5 days), in addition to clinically meaningful improvements in symptoms and function.
4.3.3. Other Observations across All Studies Pertaining to Primary Measures and Other Measures Not Utilized for the Meta-Analyses
Boston Carpal Tunnel Questionnaire (BCTQ)
Seventeen of the included studies used the BCTQ [133] for pre- and post-procedural assessment of the severity of the symptoms [65,66,71,76,77,78,79,80,81,82,83,84,85,86,87,88,89]. Significant improvements in the BCTQ symptom severity scale and functional status scale were reported as early as one week after UPCTR [78,85,88], and the statistical significance was maintained for up to 2 years [82,87]. The remaining studies showed statistically significantly improved scores from the BCTQ compared with pre-procedural scores. Although significant improvements occurred, as measured by the BCTQ in these studies, the clinical magnitude of improvement may be limited, in that only six of the 17 studies [66,80,83,85,86,88] reported improvements exceeding the reported minimal clinically important difference of 1.14 points for BCTQ-SS and 0.74 points for BCTQ-FS [31,32].
Sensory Examination and Grip or Pinch Strength
Among the eight included studies that used sensory examination changes via two-point discrimination or monofilament testing [17,63,64,66,71,76,82,87], seven showed statistically significant improvement from the baseline [17,63,64,66,71,82,87]. The sensory outcomes were statistically similar between the UPCTR and mini-OCTR groups [17,63,64,66]. Seven studies [17,63,64,66,76,82,87] showed long-term statistically significant improvement in hand grip and pinch strength from the pre-procedural state, whereas two studies found no improvement [71,132]. UPCTR outperformed mini-OCTR in terms of hand grip or pinch strength changes for up to 6 weeks post-procedure in two studies [17,64]. However, no long-term differences were detected between the groups in three RCTs [63,64,66].
Electrodiagnostic Outcomes
Electrodiagnostic outcomes were evaluated in six studies. Distal motor latencies (DMLs) of MN improved significantly in all six studies [17,65,66,70,71,81] and sensory conduction velocities (SCV) improved significantly in the five studies in which it was measured [17,65,66,70,71]. In the two RCTs comparing UPCTR and mini-CTR for electrodiagnostic outcomes, no differences were found between the UPCTR and mini-CTR groups at long-term follow-up for DML or SCV [17,66]. Guo et al. [70] evaluated UPCTR with or without additional post-procedural corticosteroid injection and showed significantly more DML and SCV improvement in the group receiving post-procedural corticosteroid injection.
CSA of the MN
Seven studies employed interval CSA ultrasound measurement of the MN. Pre-treatment MN CSA ranged from 13 to 19 mm2 and post-procedure MN CSA ranged from 10 to 15 mm2 [65,70,71,81,83,132] across the studies. A statistically significant decrease in MN CSA was reported in five of the seven studies [65,70,81,83,132], in one study CSA changes did not reach statistical significance [71], and one study did not report the statistics of MN CSA changes [83]. Two of them showed an increased diameter of MN at the carpal tunnel exit in the post-procedure follow-up [81,132].
Quick Disabilities of the Arm, Shoulder and Hand (Q-DASH)
Six studies [63,64,80,85,86,88] adopted Q-DASH [134] for outcome assessment and five of them reported statistically significant improvement in Q-DASH scores from 1 week [63,64,85] up to 1 year [86,88]. Four of these six studies reported exceeding the MCID for Q-DASH [80,85,86,88] of 15 points post-operatively [135].
4.3.4. Safety and Complications
No significant safety issue and complications were reported in UPIT. Lam et al. has stressed how to prevent damaging the MN during ultrasound-guided nerve hydrodissection [95,99,136,137]. A total of 33 complications were reported among the 2547 wrists that received UPCTR: 13 out of 213 with the loop thread approach, 10 out of 1400 with the hook knife (retrograde blade) method, and 10 out of 148 with anterograde blade use. Kamel et al. [86] defined major complications of UPCTR as nerve, tendon, or vessel injury that required operative management, and by that definition, no major complications were reported. One patient required surgery for acute compartment syndrome post-UPCTR using a hook knife release [86]. However, he reportedly played racquetball on day 10 post-procedure. Of the five patients that required revision surgeries after UPCTR, two patients had persistent symptoms after dovetail blade use, two had persistent symptoms related to incomplete FR transection using the loop thread approach, and one developed recurrent symptoms two years following hook knife UPCTR [66,71,76]. Other mild complications included self-limited pain or swelling in nine patients following looped thread and in two patients following blade UPCTR [77,78,84]. One patient complained of persistent moderate wrist pain without sensory symptoms at one-year post-UPCTR with the hook knife approach [76]. Six patients complained of transient paresthesia after UPCTR with a hook knife, resolving in 1–6 weeks [81,87]. Infections were observed in four patients after UPCTR. Infection occurred in two patients following the inclusion of a corticosteroid in the hydrodissection fluid for looped thread UPCTR [78], in one patient who suffered a fall eight days post-hook knife UPCTR [86], and in another patient following UPCTR with a blade [66].
4.4. Limitations and Future Perspectives
The current study has some limitations. First, all six studies of UPIT with D5W were from a single country, and four were from the same research group, which limited the generalization of results. Second, only a few studies had a follow-up period of more than six months which risks underreporting long-term complications or recurrence and limits the evaluation of the comparative regenerative effects post-injection or surgery. Third, the varying injected volume among the studies may have affected clinical outcomes as a larger volume would be expected to provide greater mechanical hydrodissection. In addition to the shortcomings mentioned above, the current research did not consider all aspects of UPIT and UPCTR. Future studies should clarify other questions regarding UPIT and UPCTR, such as the optimal dosage and frequency of UPIT with different injectates, direct comparisons of effects and efficacy of different devices in UPCTR, and their effect for subgroup patients who have a higher risk of developing CTS, e.g., those with uremia, diabetes mellitus, or rheumatoid arthritis.
5. Conclusions
This is the first systematic meta-analysis pertaining to both UPIT and UPCTR. Despite a broad spectrum of bias risks and heterogeneities across the included studies, these results suggest that UPIT with D5W or PRP outperforms the corresponding controls for the treatment of CTS and that UPCTR is at least as effective as open surgery. Both UPIT and UPCTR appear to have safety advantages compared to open surgery. Further studies are needed to determine the relative cost efficacy of these treatment approaches.
Acknowledgments
Due to their equal and extensive contribution, Y.-T.W. and K.H.S.L. are listed as the co-first author.
Author Contributions
Conceptualization, Y.-T.W. and K.H.S.L.; methodology, Y.-T.W., K.H.S.L., K.D.R. and P.W.H.P.; investigation, Y.-T.W. and K.H.S.L.; resources, Y.-T.W. and K.H.S.L.; data curation, Y.-T.W. and K.H.S.L.; writing—original draft preparation, Y.-T.W. and K.H.S.L.; writing—review and editing, Y.-T.W., K.H.S.L., K.D.R., F.G., A.E.-S.A. and P.W.H.P.; supervision, Y.-T.W. and K.H.S.L. All authors have read and agreed to the published version of the manuscript. Y.-T.W. and K.H.S.L. contributed equally to this manuscript and are listed as the co-first author.
Institutional Review Board Statement
This systemic review did not require Institutional Review Board Approval.
Informed Consent Statement
Patient consent was waived because this is a review article on the available literature.
Data Availability Statement
Data are available within the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Burton C.L., Chesterton L.S., Chen Y., van der Windt D.A. Clinical Course and Prognostic Factors in Conservatively Managed Carpal Tunnel Syndrome: A Systematic Review. Arch. Phys. Med. Rehabil. 2016;97:836–852.e831. doi: 10.1016/j.apmr.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 2.Atroshi I., Gummesson C., Johnsson R., Ornstein E., Ranstam J., Rosen I. Prevalence for clinically proved carpal tunnel syndrome is 4 percent. Lakartidningen. 2000;97:1668–1670. [PubMed] [Google Scholar]
- 3.Werner R.A., Andary M. Carpal tunnel syndrome: Pathophysiology and clinical neurophysiology. Clin. Neurophysiol. 2002;113:1373–1381. doi: 10.1016/S1388-2457(02)00169-4. [DOI] [PubMed] [Google Scholar]
- 4.Padua L., Coraci D., Erra C., Pazzaglia C., Paolasso I., Loreti C., Caliandro P., Hobson-Webb L.D. Carpal tunnel syndrome: Clinical features, diagnosis, and management. Lancet Neurol. 2016;15:1273–1284. doi: 10.1016/S1474-4422(16)30231-9. [DOI] [PubMed] [Google Scholar]
- 5.Uchiyama S., Itsubo T., Nakamura K., Kato H., Yasutomi T., Momose T. Current concepts of carpal tunnel syndrome: Pathophysiology, treatment, and evaluation. J. Orthop. Sci. 2010;15:1–13. doi: 10.1007/s00776-009-1416-x. [DOI] [PubMed] [Google Scholar]
- 6.Chang K.V., Wu W.T., Ozcakar L. Ultrasound imaging and guidance in peripheral nerve entrapment: Hydrodissection highlighted. Pain. Manag. 2020;10:97–106. doi: 10.2217/pmt-2019-0056. [DOI] [PubMed] [Google Scholar]
- 7.Bland J.D.P. Hydrodissection for treatment of carpal tunnel syndrome. Muscle Nerve. 2017;57:4–5. doi: 10.1002/mus.25759. [DOI] [PubMed] [Google Scholar]
- 8.Wu Y.T., Ke M.J., Chou Y.C., Chang C.Y., Lin C.Y., Li T.Y., Shih F.M., Chen L.C. Effect of radial shock wave therapy for carpal tunnel syndrome: A prospective randomized, double-blind, placebo-controlled trial. J. Orthop. Res. 2016;34:977–984. doi: 10.1002/jor.23113. [DOI] [PubMed] [Google Scholar]
- 9.O’Connor D., Marshall S., Massy-Westropp N. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst. Rev. 2003;2003:CD003219. doi: 10.1002/14651858.CD003219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bland J.D. Treatment of carpal tunnel syndrome. Muscle Nerve. 2007;36:167–171. doi: 10.1002/mus.20802. [DOI] [PubMed] [Google Scholar]
- 11.Lauder A., Mithani S., Leversedge F.J. Management of Recalcitrant Carpal Tunnel Syndrome. J. Am. Acad. Orthop. Surg. 2019;27:551–562. doi: 10.5435/JAAOS-D-18-00004. [DOI] [PubMed] [Google Scholar]
- 12.Hoogendam L., Bakx J.A.C., Souer J.S., Slijper H.P., Andrinopoulou E.R., Selles R.W., Hand Wrist Study G. Predicting Clinically Relevant Patient-Reported Symptom Improvement After Carpal Tunnel Release: A Machine Learning Approach. Neurosurgery. 2022;90:106–113. doi: 10.1227/NEU.0000000000001749. [DOI] [PubMed] [Google Scholar]
- 13.Brown R.A., Gelberman R.H., Seiler J.G., 3rd, Abrahamsson S.O., Weiland A.J., Urbaniak J.R., Schoenfeld D.A., Furcolo D. Carpal tunnel release. A prospective, randomized assessment of open and endoscopic methods. J. Bone Jt. Surg. Am. Vol. 1993;75:1265–1275. doi: 10.2106/00004623-199309000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Agee J.M., Peimer C.A., Pyrek J.D., Walsh W.E. Endoscopic carpal tunnel release: A prospective study of complications and surgical experience. J. Hand Surg. 1995;20:165–171; discussion 172. doi: 10.1016/S0363-5023(05)80001-2. [DOI] [PubMed] [Google Scholar]
- 15.Li Y., Luo W., Wu G., Cui S., Zhang Z., Gu X. Open versus endoscopic carpal tunnel release: A systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet Disord. 2020;21:272. doi: 10.1186/s12891-020-03306-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sayegh E.T., Strauch R.J. Open versus endoscopic carpal tunnel release: A meta-analysis of randomized controlled trials. Clin. Orthop. Relat. Res. 2015;473:1120–1132. doi: 10.1007/s11999-014-3835-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakamichi K., Tachibana S., Yamamoto S., Ida M. Percutaneous carpal tunnel release compared with mini-open release using Ultrasonographic guidance for both techniques. J. Hand Surg. 2010;35:437–445. doi: 10.1016/j.jhsa.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 18.Ohuchi H., Hattori S., Shinga K., Ichikawa K., Yamada S. Ultrasound-Assisted Endoscopic Carpal Tunnel Release. Arthrosc. Technol. 2016;5:e483–e487. doi: 10.1016/j.eats.2016.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evers S., Bryan A.J., Sanders T.L., Selles R.W., Gelfman R., Amadio P.C. Effectiveness of Ultrasound-Guided Compared to Blind Steroid Injections in the Treatment of Carpal Tunnel Syndrome. Arthritis Care Res. 2017;69:1060–1065. doi: 10.1002/acr.23108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sites B.D., Brull R. Ultrasound guidance in peripheral regional anesthesia: Philosophy, evidence-based medicine, and techniques. Curr. Opin. Anaesthesiol. 2006;19:630–639. doi: 10.1097/ACO.0b013e3280101423. [DOI] [PubMed] [Google Scholar]
- 21.Petrover D., Hakime A., Silvera J., Richette P., Nizard R. Ultrasound-Guided Surgery for Carpal Tunnel Syndrome: A New Interventional Procedure. Semin. Interv. Radiol. 2018;35:248–254. doi: 10.1055/s-0038-1673360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rowe N.M., Michaels J.t., Soltanian H., Dobryansky M., Peimer C.A., Gurtner G.C. Sonographically guided percutaneous carpal tunnel release: An anatomic and cadaveric study. Ann. Plast Surg. 2005;55:52–56; discussion 56. doi: 10.1097/01.sap.0000168281.77528.02. [DOI] [PubMed] [Google Scholar]
- 23.Tumpaj T., Potocnik Tumpaj V., Albano D., Snoj Z. Ultrasound-guided carpal tunnel injections. Radiol. Oncol. 2022;56:14–22. doi: 10.2478/raon-2022-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buntragulpoontawee M., Chang K.V., Vitoonpong T., Pornjaksawan S., Kitisak K., Saokaew S., Kanchanasurakit S. The Effectiveness and Safety of Commonly Used Injectates for Ultrasound-Guided Hydrodissection Treatment of Peripheral Nerve Entrapment Syndromes: A Systematic Review. Front. Pharmacol. 2020;11:621150. doi: 10.3389/fphar.2020.621150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leite J.C., Jerosch-Herold C., Song F. A systematic review of the psychometric properties of the Boston Carpal Tunnel Questionnaire. BMC Musculoskelet Disord. 2006;7:78. doi: 10.1186/1471-2474-7-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Higgins S.J., Page M.J., Elbers R.G., Sterne J.A.C., editors. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane, Wiley; West Sussex, UK: 2022. Chapter 8: Assessing risk of bias in a randomized trial. Version 6.3. [Google Scholar]
- 28.Munn Z., Barker T.H., Moola S., Tufanaru C., Stern C., McArthur A., Stephenson M., Aromataris E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid. Synth. 2020;18:2127–2133. doi: 10.11124/JBISRIR-D-19-00099. [DOI] [PubMed] [Google Scholar]
- 29.Moola S., Munn Z., Tufanaru C., Aromataris E., Sears K., Sfetcu R., Currie M., Qureshi R., Mattis P., Lisy K., et al. JBI Manual for Evidence Synthesis. Wolters Kluwer Health; Philadelphia, PA, USA: 2020. Chapter 7: Systematic reviews of etiology and risk. [Google Scholar]
- 30.ReviewManager (RevMan) is Cochrane’s Bespoke Software for Writing Cochrane Reviews. [(accessed on 2 January 2023)]. Available online: https://training.cochrane.org/online-learning/core-software/revman.
- 31.De Kleermaeker F., Boogaarts H.D., Meulstee J., Verhagen W.I.M. Minimal clinically important difference for the Boston Carpal Tunnel Questionnaire: New insights and review of literature. J. Hand Surg. Eur. Vol. 2019;44:283–289. doi: 10.1177/1753193418812616. [DOI] [PubMed] [Google Scholar]
- 32.Kim J.K., Jeon S.H. Minimal clinically important differences in the Carpal Tunnel Questionnaire after carpal tunnel release. J. Hand Surg. Eur. Vol. 2013;38:75–79. doi: 10.1177/1753193412442137. [DOI] [PubMed] [Google Scholar]
- 33.Ustun N., Tok F., Yagz A.E., Kizil N., Korkmaz I., Karazincir S., Okuyucu E., Turhanoglu A.D. Ultrasound-guided vs. blind steroid injections in carpal tunnel syndrome: A single-blind randomized prospective study. Am. J. Phys. Med. Rehabil. 2013;92:999–1004. doi: 10.1097/PHM.0b013e31829b4d72. [DOI] [PubMed] [Google Scholar]
- 34.Lee J.Y., Park Y., Park K.D., Lee J.K., Lim O.K. Effectiveness of ultrasound-guided carpal tunnel injection using in-plane ulnar approach: A prospective, randomized, single-blinded study. Medicine. 2014;93:e350. doi: 10.1097/MD.0000000000000350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Makhlouf T., Emil N.S., Sibbitt W.L., Jr., Fields R.A., Bankhurst A.D. Outcomes and cost-effectiveness of carpal tunnel injections using sonographic needle guidance. Clin. Rheumatol. 2014;33:849–858. doi: 10.1007/s10067-013-2438-5. [DOI] [PubMed] [Google Scholar]
- 36.Eslamian F., Eftekharsadat B., Babaei-Ghazani A., Jahanjoo F., Zeinali M. A Randomized Prospective Comparison of Ultrasound-Guided and Landmark-Guided Steroid Injections for Carpal Tunnel Syndrome. J. Clin. Neurophysiol. 2017;34:107–113. doi: 10.1097/WNP.0000000000000342. [DOI] [PubMed] [Google Scholar]
- 37.Karaahmet Ö.Z., Gürçay E., Kara M., Serçe A., Kıraç Ünal Z., Çakcı A. Comparing the effectiveness of ultrasound-guided versus blind steroid injection in the treatment of severe carpal tunnel syndrome. Turk. J. Med. Sci. 2017;47:1785–1790. doi: 10.3906/sag-1704-97. [DOI] [PubMed] [Google Scholar]
- 38.Wang J.C., Liao K.K., Lin K.P., Chou C.L., Yang T.F., Huang Y.F., Wang K.A., Chiu J.W. Efficacy of Combined Ultrasound-Guided Steroid Injection and Splinting in Patients With Carpal Tunnel Syndrome: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2017;98:947–956. doi: 10.1016/j.apmr.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 39.Chen P.C., Wang L.Y., Pong Y.P., Hsin Y.J., Liaw M.Y., Chiang C.W. Effectiveness of ultrasound-guided vs. direct approach corticosteroid injections for carpal tunnel syndrome: A double-blind randomized controlled trial. J. Rehabil. Med. 2018;50:200–208. doi: 10.2340/16501977-2308. [DOI] [PubMed] [Google Scholar]
- 40.Babaei-Ghazani A., Nikbakht N., Forogh B., Raissi G.R., Ahadi T., Ebadi S., Roomizadeh P., Fadavi H.R., Raeissadat S.A., Eftekharsadat B. Comparison Between Effectiveness of Ultrasound-Guided Corticosteroid Injection Above Versus Below the Median Nerve in Mild to Moderate Carpal Tunnel Syndrome: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2018;97:407–413. doi: 10.1097/PHM.0000000000000877. [DOI] [PubMed] [Google Scholar]
- 41.Salman Roghani R., Holisaz M.T., Tarkashvand M., Delbari A., Gohari F., Boon A.J., Lokk J. Different doses of steroid injection in elderly patients with carpal tunnel syndrome: A triple-blind, randomized, controlled trial. Clin. Interv. Aging. 2018;13:117–124. doi: 10.2147/CIA.S151290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roh Y.H., Hwangbo K., Gong H.S., Baek G.H. Comparison of Ultrasound-Guided Versus Landmark-Based Corticosteroid Injection for Carpal Tunnel Syndrome: A Prospective Randomized Trial. J. Hand Surg. 2019;44:304–310. doi: 10.1016/j.jhsa.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 43.Rayegani S.M., Raeissadat S.A., Ahmadi-Dastgerdi M., Bavaghar N., Rahimi-Dehgolan S. Comparing The Efficacy Of Local Triamcinolone Injection In Carpal Tunnel Syndrome Using Three Different Approaches with or without Ultrasound Guidance. J. Pain Res. 2019;12:2951–2958. doi: 10.2147/JPR.S212948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hsu P.C., Liao K.K., Lin K.P., Chiu J.W., Wu P.Y., Chou C.L., Wang N.Y., Wang J.C. Comparison of Corticosteroid Injection Dosages in Mild to Moderate Idiopathic Carpal Tunnel Syndrome: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2020;101:1857–1864. doi: 10.1016/j.apmr.2020.06.018. [DOI] [PubMed] [Google Scholar]
- 45.Babaei-Ghazani A., Forogh B., Raissi G.R., Ahadi T., Eftekharsadat B., Yousefi N., Rahimi-Dehgolan S., Moradi K. Ultrasound-Guided Corticosteroid Injection in Carpal Tunnel Syndrome: Comparison Between Radial and Ulnar Approaches. J. Pain Res. 2020;13:1569–1578. doi: 10.2147/JPR.S248600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang J.C., Hsu P.C., Wang K.A., Chang K.V. Ultrasound-Guided Triamcinolone Acetonide Hydrodissection for Carpal Tunnel Syndrome: A Randomized Controlled Trial. Front. Med. 2021;8:742724. doi: 10.3389/fmed.2021.742724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mathew M.M., Gaur R., Gonnade N., Asthana S.S., Ghuleliya R. Efficacy of Ultrasound-Guided Particulate Versus Nonparticulate Steroid Injection in Carpal Tunnel Syndrome: An Open-Label Randomized Control Trial. Cureus. 2022;14:e21591. doi: 10.7759/cureus.21591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mezian K., SobotovÁ K., Kuliha M., Chang K.V., CeÉ J., AngerovÁ Y., ÖzÇakar L. Ultrasound-guided perineural vs. peritendinous corticosteroid injections in carpal tunnel syndrome: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2021;57:775–782. doi: 10.23736/S1973-9087.21.06682-X. [DOI] [PubMed] [Google Scholar]
- 49.Wu Y.T., Ho T.Y., Chou Y.C., Ke M.J., Li T.Y., Tsai C.K., Chen L.C. Six-month Efficacy of Perineural Dextrose for Carpal Tunnel Syndrome: A Prospective, Randomized, Double-Blind, Controlled Trial. Mayo Clin. Proc. 2017;92:1179–1189. doi: 10.1016/j.mayocp.2017.05.025. [DOI] [PubMed] [Google Scholar]
- 50.Wu Y.T., Ke M.J., Ho T.Y., Li T.Y., Shen Y.P., Chen L.C. Randomized double-blinded clinical trial of 5% dextrose versus triamcinolone injection for carpal tunnel syndrome patients. Ann. Neurol. 2018;84:601–610. doi: 10.1002/ana.25332. [DOI] [PubMed] [Google Scholar]
- 51.Lin M.T., Liao C.L., Hsiao M.Y., Hsueh H.W., Chao C.C., Wu C.H. Volume Matters in Ultrasound-Guided Perineural Dextrose Injection for Carpal Tunnel Syndrome: A Randomized, Double-Blinded, Three-Arm Trial. Front. Pharmacol. 2020;11:625830. doi: 10.3389/fphar.2020.625830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lin M.-T., Liu I.-C., Syu W.-T., Kuo P.-L., Wu C.-H. Effect of Perineural Injection with Different Dextrose Volumes on Median Nerve Size, Elasticity and Mobility in Hands with Carpal Tunnel Syndrome. Diagnostics. 2021;11:849. doi: 10.3390/diagnostics11050849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu Y.T., Ho T.Y., Chou Y.C., Ke M.J., Li T.Y., Huang G.S., Chen L.C. Six-month efficacy of platelet-rich plasma for carpal tunnel syndrome: A prospective randomized, single-blind controlled trial. Sci. Rep. 2017;7:94. doi: 10.1038/s41598-017-00224-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Malahias M.A., Nikolaou V.S., Johnson E.O., Kaseta M.K., Kazas S.T., Babis G.C. Platelet-rich plasma ultrasound-guided injection in the treatment of carpal tunnel syndrome: A placebo-controlled clinical study. J. Tissue Eng. Regen. Med. 2018;12:e1480–e1488. doi: 10.1002/term.2566. [DOI] [PubMed] [Google Scholar]
- 55.Senna M.K., Shaat R.M., Ali A.A.A. Platelet-rich plasma in treatment of patients with idiopathic carpal tunnel syndrome. Clin. Rheumatol. 2019;38:3643–3654. doi: 10.1007/s10067-019-04719-7. [DOI] [PubMed] [Google Scholar]
- 56.Shen Y.P., Li T.Y., Chou Y.C., Ho T.Y., Ke M.J., Chen L.C., Wu Y.T. Comparison of perineural platelet-rich plasma and dextrose injections for moderate carpal tunnel syndrome: A prospective randomized, single-blind, head-to-head comparative trial. J. Tissue Eng. Regen. Med. 2019;13:2009–2017. doi: 10.1002/term.2950. [DOI] [PubMed] [Google Scholar]
- 57.Chen S.R., Shen Y.P., Ho T.Y., Li T.Y., Su Y.C., Chou Y.C., Chen L.C., Wu Y.T. One-Year Efficacy of Platelet-Rich Plasma for Moderate-to-Severe Carpal Tunnel Syndrome: A Prospective, Randomized, Double-Blind, Controlled Trial. Arch. Phys. Med. Rehabil. 2021;102:951–958. doi: 10.1016/j.apmr.2020.12.025. [DOI] [PubMed] [Google Scholar]
- 58.Su Y.C., Li T.Y., Ho T.Y., Chen L.C., Wu Y.T. The efficacy of hyaluronic acid for carpal tunnel syndrome: A randomized double-blind trial. Pain Med. 2021;22:2676–2685. doi: 10.1093/pm/pnab109. [DOI] [PubMed] [Google Scholar]
- 59.Alsaeid M.A. Dexamethasone versus Hyaluronidase as an Adjuvant to Local Anesthetics in the Ultrasound-guided Hydrodissection of the Median Nerve for the Treatment of Carpal Tunnel Syndrome Patients. Anesth. Essays Res. 2019;13:417–422. doi: 10.4103/aer.AER_104_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Elawamy A., Hassanien M., Hamed A., Roushdy A.S.I., Abass N.A., Mohammed G., Hasan M., Kamel E.Z. Efficacy of Hyalase Hydrodissection in the Treatment of Carpal Tunnel Syndrome: A Randomized, Double-Blind, Controlled, Clinical Trial. Pain Physician. 2020;23:E175–E183. [PubMed] [Google Scholar]
- 61.Kamel S.R., Sadek H.A., Hamed A., Sayed O.A., Mahmud M.H., Mohamed F.A., El Sagher G.M., Aly L.H. Ultrasound-guided insulin injection for carpal tunnel syndrome in type 2 diabetes mellitus patients. Clin. Rheumatol. 2019;38:2933–2940. doi: 10.1007/s10067-019-04638-7. [DOI] [PubMed] [Google Scholar]
- 62.Forogh B., Mohamadi H., Fadavi H.R., Madani S.P., Aflakian N., Ghazaie F., Babaei-Ghazani A. Comparison of Ultrasound-Guided Local Ozone (O2-O3) Injection Versus Corticosteroid Injection in Patients With Mild to Moderate Carpal Tunnel Syndrome. Am. J. Phys. Med. Rehabil. 2021;100:168–172. doi: 10.1097/PHM.0000000000001546. [DOI] [PubMed] [Google Scholar]
- 63.Capa-Grasa A., Rojo-Manaute J.M., Rodriguez F.C., Martin J.V. Ultra minimally invasive sonographically guided carpal tunnel release: An external pilot study. Orthop. Traumatol. Surg. Res. 2014;100:287–292. doi: 10.1016/j.otsr.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 64.Rojo-Manaute J.M., Capa-Grasa A., Chana-Rodriguez F., Perez-Mananes R., Rodriguez-Maruri G., Sanz-Ruiz P., Munoz-Ledesma J., Aburto-Bernardo M., Esparragoza-Cabrera L., Cerro-Gutierrez M.D., et al. Ultra-Minimally Invasive Ultrasound-Guided Carpal Tunnel Release: A Randomized Clinical Trial. J. Ultrasound Med. 2016;35:1149–1157. doi: 10.7863/ultra.15.07001. [DOI] [PubMed] [Google Scholar]
- 65.Zhang S., Wang F., Ke S., Lin C., Liu C., Xin W., Wu S., Ma C. The Effectiveness of Ultrasound-Guided Steroid Injection Combined with Miniscalpel-Needle Release in the Treatment of Carpal Tunnel Syndrome vs. Steroid Injection Alone: A Randomized Controlled Study. BioMed Res. Int. 2019;2019:9498656. doi: 10.1155/2019/9498656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.de la Fuente J., Aramendi J.F., Ibanez J.M., Blasi M., Vazquez A., Aurrekoetxea J.J., Davila F. Minimally invasive ultrasound-guided vs. open release for carpal tunnel syndrome in working population: A randomized controlled trial. J. Clin. Ultrasound. 2021;49:693–703. doi: 10.1002/jcu.23019. [DOI] [PubMed] [Google Scholar]
- 67.Hsu Y.C., Yang F.C., Hsu H.H., Huang G.S. Ultrasound-Guided Corticosteroid Injection in Patients with Carpal Tunnel Syndrome: Efficacy of Intra-Epineurial Injection. Ultraschall Med. 2018;39:334–342. doi: 10.1055/s-0043-120109. [DOI] [PubMed] [Google Scholar]
- 68.Yeom J.W., Cho J.H., Kim S.J., Lee H.I. Cross-Sectional Area of the Median Nerve as a Prognostic Indicator in Carpal Tunnel Syndrome Treated With Local Steroid Injection. J. Hand Surg. 2021;48:85.e1–85.e10. doi: 10.1016/j.jhsa.2021.09.022. [DOI] [PubMed] [Google Scholar]
- 69.Guven S.C., Ozcakar L., Kaymak B., Kara M., Akinci A. Short-term effectiveness of platelet-rich plasma in carpal tunnel syndrome: A controlled study. J. Tissue Eng. 2019;13:709–714. doi: 10.1002/term.2815. [DOI] [PubMed] [Google Scholar]
- 70.Guo X.Y., Xiong M.X., Lu M., Cheng X.Q., Wu Y.Y., Chen S.Y., Chen K., Zhou Q.D., Wang L., Tan L., et al. Ultrasound-guided needle release of the transverse carpal ligament with and without corticosteroid injection for the treatment of carpal tunnel syndrome. J. Orthop. Surg. Res. 2018;13:69. doi: 10.1186/s13018-018-0771-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Burnham R.S., Loh E.Y., Rambaransingh B., Roberts S.L., Agur A.M., Playfair L.D. A Controlled Trial Evaluating the Safety and Effectiveness of Ultrasound-Guided Looped Thread Carpal Tunnel Release. Hand. 2021;16:73–80. doi: 10.1177/1558944719842199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Asserson D.B., North T.J., Rhee P.C., Bishop A.T., Brault J.S., Shin A.Y. Return to work following ultrasound guided thread carpal tunnel release versus open carpal tunnel release: A comparative study. J. Hand Surg. Eur. Vol. 2022;47:359–363. doi: 10.1177/17531934211051276. [DOI] [PubMed] [Google Scholar]
- 73.Li T.Y., Chen S.R., Shen Y.P., Chang C.Y., Su Y.C., Chen L.C., Wu Y.T. Long-Term Outcome after Perineural Injection with 5% Dextrose for Carpal Tunnel Syndrome: A Retrospective Follow-Up Study. Rheumatology. 2021;60:881–887. doi: 10.1093/rheumatology/keaa361. [DOI] [PubMed] [Google Scholar]
- 74.Chao T.C., Reeves K.D., Lam K.H.S., Li T.Y., Wu Y.T. The Effectiveness of Hydrodissection with 5% Dextrose for Persistent and Recurrent Carpal Tunnel Syndrome: A Retrospective Study. J. Clin. Med. 2022;11:3705. doi: 10.3390/jcm11133705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Malahias M.A., Johnson E.O., Babis G.C., Nikolaou V.S. Single injection of platelet-rich plasma as a novel treatment of carpal tunnel syndrome. Neural Regen. Res. 2015;10:1856–1859. doi: 10.4103/1673-5374.165322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chern T.C., Kuo L.C., Shao C.J., Wu T.T., Wu K.C., Jou I.M. Ultrasonographically Guided Percutaneous Carpal Tunnel Release: Early Clinical Experiences and Outcomes. Arthroscopy. 2015;31:2400–2410. doi: 10.1016/j.arthro.2015.06.023. [DOI] [PubMed] [Google Scholar]
- 77.Guo D., Tang Y., Ji Y., Sun T., Guo J., Guo D. A non-scalpel technique for minimally invasive surgery: Percutaneously looped thread transection of the transverse carpal ligament. Hand. 2015;10:40–48. doi: 10.1007/s11552-014-9656-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Guo D., Guo D., Guo J., Schmidt S.C., Lytie R.M. A Clinical Study of the Modified Thread Carpal Tunnel Release. Hand. 2017;12:453–460. doi: 10.1177/1558944716668831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Petrover D., Silvera J., De Baere T., Vigan M., Hakime A. Percutaneous Ultrasound-Guided Carpal Tunnel Release: Study Upon Clinical Efficacy and Safety. Cardiovasc. Interv. Radiol. 2017;40:568–575. doi: 10.1007/s00270-016-1545-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Henning P.T., Yang L., Awan T., Lueders D., Pourcho A.M. Minimally Invasive Ultrasound-Guided Carpal Tunnel Release: Preliminary Clinical Results. J. Ultrasound Med. 2018;37:2699–2706. doi: 10.1002/jum.14618. [DOI] [PubMed] [Google Scholar]
- 81.Luanchumroen N. Ultrasound-guided percutaneous carpal tunnel release with hook blade. J. Med. Assoc. Thail. 2019;102:481–488. [Google Scholar]
- 82.Wang P.H., Li C.L., Shao C.J., Wu K.C., Chern T.C., Jou I.M. Ultrasound-guided percutaneous carpal tunnel release in patients on hemodialysis: Early experiences and clinical outcomes. Ther. Clin. Risk Manag. 2019;15:711–717. doi: 10.2147/TCRM.S206362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Chappell C.D., Beckman J.P., Baird B.C., Takke A.V. Ultrasound (US) Changes in the Median Nerve Cross-Sectional Area After Microinvasive US-Guided Carpal Tunnel Release. J. Ultrasound Med. 2020;39:693–702. doi: 10.1002/jum.15146. [DOI] [PubMed] [Google Scholar]
- 84.Hebbard P., Thomas P., Fransch S.V., Cichowitz A., Franzi S. Microinvasive Carpal Tunnel Release Using a Retractable Needle-Mounted Blade. J. Ultrasound Med. 2021;40:1451–1458. doi: 10.1002/jum.15509. [DOI] [PubMed] [Google Scholar]
- 85.Joseph A.E., Leiby B.M., Beckman J.P. Clinical Results of Ultrasound-Guided Carpal Tunnel Release Performed by a Primary Care Sports Medicine Physician. J. Ultrasound Med. 2020;39:441–452. doi: 10.1002/jum.15120. [DOI] [PubMed] [Google Scholar]
- 86.Kamel S.I., Freid B., Pomeranz C., Halpern E.J., Nazarian L.N. Minimally Invasive Ultrasound-Guided Carpal Tunnel Release Improves Long-Term Clinical Outcomes in Carpal Tunnel Syndrome. AJR Am. J. Roentgenol. 2021;217:460–468. doi: 10.2214/AJR.20.24383. [DOI] [PubMed] [Google Scholar]
- 87.Wang P.H., Wu P.T., Jou I.M. Ultrasound-guided percutaneous carpal tunnel release: 2-year follow-up of 641 hands. J. Hand Surg. Eur. Vol. 2021;46:305–307. doi: 10.1177/1753193420948824. [DOI] [PubMed] [Google Scholar]
- 88.Leiby B.M., Beckman J.P., Joseph A.E. Long-term Clinical Results of Carpal Tunnel Release Using Ultrasound Guidance. Hand. 2022;17:1074–1081. doi: 10.1177/1558944720988080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Loizides A., Honold S., Skalla-Oberherber E., Gruber L., Loscher W., Moriggl B., Konschake M., Gruber H. Ultrasound-Guided Minimal Invasive Carpal Tunnel Release: An Optimized Algorithm. Cardiovasc. Interv. Radiol. 2021;44:976–981. doi: 10.1007/s00270-021-02789-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lee S.H., Choi H.H., Chang M.C. Effect of Ultrasound-Guided Partial Release of the Transverse Carpal Ligament with a Needle in Patients with Refractory Carpal Tunnel Syndrome. Pain Physician. 2022;25:E141–E145. [PubMed] [Google Scholar]
- 91.Fowler J.R., Chung K.C., Miller L.E. Multicenter pragmatic study of carpal tunnel release with ultrasound guidance. Expert Rev. Med. Devices. 2022;19:273–280. doi: 10.1080/17434440.2022.2048816. [DOI] [PubMed] [Google Scholar]
- 92.Cass S.P. Ultrasound-Guided Nerve Hydrodissection: What is it? A Review of the Literature. Curr. Sport. Med. Rep. 2016;15:20–22. doi: 10.1249/JSR.0000000000000226. [DOI] [PubMed] [Google Scholar]
- 93.Wu Y.T., Chen S.R., Li T.Y., Ho T.Y., Shen Y.P., Tsai C.K., Chen L.C. Nerve hydrodissection for carpal tunnel syndrome: A prospective, randomized, double-blind, controlled trial. Muscle Nerve. 2019;59:174–180. doi: 10.1002/mus.26358. [DOI] [PubMed] [Google Scholar]
- 94.Lam S.K.H., Reeves K.D., Cheng A.L. Transition from Deep Regional Blocks toward Deep Nerve Hydrodissection in the Upper Body and Torso: Method Description and Results from a Retrospective Chart Review of the Analgesic Effect of 5% Dextrose Water as the Primary Hydrodissection Injectate to Enhance Safety. BioMed Res. Int. 2017;2017:7920438. doi: 10.1155/2017/7920438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lam K.H.S., Hung C.Y., Chiang Y.P., Onishi K., Su D.C.J., Clark T.B., Reeves K.D. Ultrasound-Guided Nerve Hydrodissection for Pain Management: Rationale, Methods, Current Literature, and Theoretical Mechanisms. J. Pain Res. 2020;13:1957–1968. doi: 10.2147/JPR.S247208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Evers S., Thoreson A.R., Smith J., Zhao C., Geske J.R., Amadio P.C. Ultrasound-guided hydrodissection decreases gliding resistance of the median nerve within the carpal tunnel. Muscle Nerve. 2018;57:25–32. doi: 10.1002/mus.25723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chen S.-R., Ho T.-Y., Shen Y.-P., Li T.-Y., Su Y.-C., Lam K.H.S., Chen L.-C., Wu Y.-T. Comparison of short- and long-axis nerve hydrodissection for carpal tunnel syndrome: A prospective randomized, single-blind trial. Int. J. Med. Sci. 2021;18:3488–3497. doi: 10.7150/ijms.63815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Huisstede B.M., Hoogvliet P., Randsdorp M.S., Glerum S., van Middelkoop M., Koes B.W. Carpal tunnel syndrome. Part I: Effectiveness of nonsurgical treatments–a systematic review. Arch. Phys. Med. Rehabil. 2010;91:981–1004. doi: 10.1016/j.apmr.2010.03.022. [DOI] [PubMed] [Google Scholar]
- 99.Lam K.H.S., Lai W.W., Ngai H.Y., Wu W.K.R., Wu Y.-T. Commentary: Ultrasound-Guided Triamcinolone Acetonide Hydrodissection for Carpal Tunnel Syndrome: A Randomized Controlled Trial. Front. Med. 2022;8:833862. doi: 10.3389/fmed.2021.833862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Stark H., Amirfeyz R. Cochrane corner: Local corticosteroid injection for carpal tunnel syndrome. J. Hand Surg. Eur. Vol. 2013;38:911–914. doi: 10.1177/1753193413490848. [DOI] [PubMed] [Google Scholar]
- 101.Marshall S., Tardif G., Ashworth N. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst. Rev. 2007;2007:CD001554. doi: 10.1002/14651858.CD001554.pub2. [DOI] [PubMed] [Google Scholar]
- 102.Wang P.H., Tsai C.L., Lee J.S., Wu K.C., Cheng K.I., Jou I.M. Effects of topical corticosteroids on the sciatic nerve: An experimental study to adduce the safety in treating carpal tunnel syndrome. J. Hand Surg. Eur. Vol. 2011;36:236–243. doi: 10.1177/1753193410390760. [DOI] [PubMed] [Google Scholar]
- 103.Peters-Veluthamaningal C., Winters J.C., Groenier K.H., Meyboom-de Jong B. Randomised controlled trial of local corticosteroid injections for carpal tunnel syndrome in general practice. BMC Fam. Pract. 2010;11:54. doi: 10.1186/1471-2296-11-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kothari M.J.J.U., Waltham M.A., Disponível E.M. Carpal Tunnel Syndrome: Treatment and Prognosis. 2019. [(accessed on 1 October 2022)]. Available online: https://www.uptodate.com/contents/carpal-tunnel-syndrome-treatment--and-prognosis.
- 105.Amato A.A., Barohn R.J. Peripheral Neuropathy. In: Jameson J.L., Fauci A.S., Kasper D.L., Hauser S.L., Longo D.L., Loscalzo J., editors. Harrison’s Principles of Internal Medicine, 20e. McGraw-Hill Education; New York, NY, USA: 2018. [Google Scholar]
- 106.Yelland M.J., Sweeting K.R., Lyftogt J.A., Ng S.K., Scuffham P.A., Evans K.A. Prolotherapy injections and eccentric loading exercises for painful Achilles tendinosis: A randomised trial. Br. J. Sport. Med. 2011;45:421–428. doi: 10.1136/bjsm.2009.057968. [DOI] [PubMed] [Google Scholar]
- 107.Rabago D., Patterson J.J., Mundt M., Kijowski R., Grettie J., Segal N.A., Zgierska A. Dextrose prolotherapy for knee osteoarthritis: A randomized controlled trial. Ann. Fam. Med. 2013;11:229–237. doi: 10.1370/afm.1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Bertrand H., Kyriazis M., Reeves K.D., Lyftogt J., Rabago D. Topical Mannitol Reduces Capsaicin-Induced Pain: Results of a Pilot-Level, Double-Blind, Randomized Controlled Trial. PM&R. 2015;7:1111–1117. doi: 10.1016/j.pmrj.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 109.Murakawa Y., Zhang W., Pierson C.R., Brismar T., Ostenson C.G., Efendic S., Sima A.A. Impaired glucose tolerance and insulinopenia in the GK-rat causes peripheral neuropathy. Diabetes Metab. Res. Rev. 2002;18:473–483. doi: 10.1002/dmrr.326. [DOI] [PubMed] [Google Scholar]
- 110.Zamami Y., Takatori S., Yamawaki K., Miyashita S., Mio M., Kitamura Y., Kawasaki H. Acute hyperglycemia and hyperinsulinemia enhance adrenergic vasoconstriction and decrease calcitonin gene-related peptide-containing nerve-mediated vasodilation in pithed rats. Hypertens Res. 2008;31:1033–1044. doi: 10.1291/hypres.31.1033. [DOI] [PubMed] [Google Scholar]
- 111.Wei Z., Wang L., Han J., Song J., Yao L., Shao L., Sun Z., Zheng L. Decreased expression of transient receptor potential vanilloid 1 impaires the postischemic recovery of diabetic mouse hearts. Circ. J. 2009;73:1127–1132. doi: 10.1253/circj.CJ-08-0945. [DOI] [PubMed] [Google Scholar]
- 112.Wu Y.T., Chen Y.P., Lam KH S., Reeves K.D., Lin J.A., Kuo C.Y. Mechanism of glucose water as a neural injection: A perspective on neuroinflammation. Life. 2022;12:832. doi: 10.3390/life12060832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Pamir N., McMillen T.S., Kaiyala K.J., Schwartz M.W., LeBoeuf R.C. Receptors for tumor necrosis factor-alpha play a protective role against obesity and alter adipose tissue macrophage status. Endocrinology. 2009;150:4124–4134. doi: 10.1210/en.2009-0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lew J.H., Naruishi K., Kajiura Y., Nishikawa Y., Ikuta T., Kido J.I., Nagata T. High Glucose-Mediated Cytokine Regulation in Gingival Fibroblasts and THP-1 Macrophage: A Possible Mechanism of Severe Periodontitis with Diabetes. Cell Physiol. Biochem. 2018;50:973–986. doi: 10.1159/000494481. [DOI] [PubMed] [Google Scholar]
- 115.Wieman H.L., Wofford J.A., Rathmell J.C. Cytokine stimulation promotes glucose uptake via phosphatidylinositol-3 kinase/Akt regulation of Glut1 activity and trafficking. Mol. Biol. Cell. 2007;18:1437–1446. doi: 10.1091/mbc.e06-07-0593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Shikhman A.R., Brinson D.C., Valbracht J., Lotz M.K. Cytokine regulation of facilitated glucose transport in human articular chondrocytes. J. Immunol. 2001;167:7001–7008. doi: 10.4049/jimmunol.167.12.7001. [DOI] [PubMed] [Google Scholar]
- 117.Ye J., Keller J.N. Regulation of energy metabolism by inflammation: A feedback response in obesity and calorie restriction. Aging. 2010;2:361–368. doi: 10.18632/aging.100155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bastami F., Vares P., Khojasteh A. Healing Effects of Platelet-Rich Plasma on Peripheral Nerve Injuries. J. Craniofacial Surg. 2017;28:e49–e57. doi: 10.1097/SCS.0000000000003198. [DOI] [PubMed] [Google Scholar]
- 119.Osterman C., McCarthy M.B.R., Cote M.P., Beitzel K., Bradley J., Polkowski G., Mazzocca A.D. Platelet-rich plasma increases anti-inflammatory markers in a human coculture model for osteoarthritis. Am. J. Sport. Med. 2015;43:1474–1484. doi: 10.1177/0363546515570463. [DOI] [PubMed] [Google Scholar]
- 120.Lai C.Y., Li T.Y., Lam K.H.S., Chou Y.C., Hueng D.Y., Chen L.C., Wu Y.T. The long-term analgesic effectiveness of platelet-rich plasma injection for carpal tunnel syndrome: A cross-sectional cohort study. Pain Med. 2022;23:1249–1258. doi: 10.1093/pm/pnac011. [DOI] [PubMed] [Google Scholar]
- 121.Acunzo G., Guida M., Pellicano M., Tommaselli G.A., Di Spiezio Sardo A., Bifulco G., Cirillo D., Taylor A., Nappi C. Effectiveness of auto-cross-linked hyaluronic acid gel in the prevention of intrauterine adhesions after hysteroscopic adhesiolysis: A prospective, randomized, controlled study. Hum. Reprod. 2003;18:1918–1921. doi: 10.1093/humrep/deg368. [DOI] [PubMed] [Google Scholar]
- 122.Belluco C., Meggiolaro F., Pressato D., Pavesio A., Bigon E., Dona M., Forlin M., Nitti D., Lise M. Prevention of postsurgical adhesions with an autocrosslinked hyaluronan derivative gel. J. Surg. Res. 2001;100:217–221. doi: 10.1006/jsre.2001.6248. [DOI] [PubMed] [Google Scholar]
- 123.Ikeda K., Yamauchi D., Osamura N., Hagiwara N., Tomita K. Hyaluronic acid prevents peripheral nerve adhesion. Br. J. Plast. Surg. 2003;56:342–347. doi: 10.1016/S0007-1226(03)00197-8. [DOI] [PubMed] [Google Scholar]
- 124.Pucciarelli S., Codello L., Rosato A., Del Bianco P., Vecchiato G., Lise M. Effect of antiadhesive agents on peritoneal carcinomatosis in an experimental model. Br. J. Surg. 2003;90:66–71. doi: 10.1002/bjs.4006. [DOI] [PubMed] [Google Scholar]
- 125.Smit X., van Neck J.W., Afoke A., Hovius S.E. Reduction of neural adhesions by biodegradable autocrosslinked hyaluronic acid gel after injury of peripheral nerves: An experimental study. J. Neurosurg. 2004;101:648–652. doi: 10.3171/jns.2004.101.4.0648. [DOI] [PubMed] [Google Scholar]
- 126.Dunn A.L., Heavner J.E., Racz G., Day M. Hyaluronidase: A review of approved formulations, indications and off-label use in chronic pain management. Expert Opin. Biol. Ther. 2010;10:127–131. doi: 10.1517/14712590903490382. [DOI] [PubMed] [Google Scholar]
- 127.Yeo G., Gupta A., Ding G., Skerman H., Khatun M., Melsom D. Pain Levels after Local Anaesthetic with or without Hyaluronidase in Carpal Tunnel Release: A Randomised Controlled Trial. Adv. Orthop. 2015;2015:784329. doi: 10.1155/2015/784329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Courtiss E.H., Ransil B.J., Russo J. The effects of hyaluronidase on local anesthesia: A prospective, randomized, controlled, double-blind study. Plast. Reconstr. Surg. 1995;95:876–883. doi: 10.1097/00006534-199504001-00017. [DOI] [PubMed] [Google Scholar]
- 129.Sloane J.A., Batt C., Ma Y., Harris Z.M., Trapp B., Vartanian T. Hyaluronan blocks oligodendrocyte progenitor maturation and remyelination through TLR2. Proc. Natl. Acad. Sci. USA. 2010;107:11555–11560. doi: 10.1073/pnas.1006496107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ibrahim S.E., Hussein A. New role for insulin injection in the treatment of idiopathic carpal tunnel syndrome. Egypt. Rheumatol. Rehabil. 2016;43:157–162. doi: 10.4103/1110-161X.192256. [DOI] [Google Scholar]
- 131.Ezeldin M., Leonardi M., Princiotta C., Dall’olio M., Tharwat M., Zaki M., Abdel-Wanis M.E., Cirillo L. Percutaneous ozone nucleolysis for lumbar disc herniation. Neuroradiology. 2018;60:1231–1241. doi: 10.1007/s00234-018-2083-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.McShane J.M., Slaff S., Gold J.E., Nazarian L.N. Sonographically guided percutaneous needle release of the carpal tunnel for treatment of carpal tunnel syndrome: Preliminary report. J. Ultrasound Med. 2012;31:1341–1349. doi: 10.7863/jum.2012.31.9.1341. [DOI] [PubMed] [Google Scholar]
- 133.Levine D.W., Simmons B.P., Koris M.J., Daltroy L.H., Hohl G.G., Fossel A.H., Katz J.N. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J. Bone Jt. Surg. Am. Vol. 1993;75:1585–1592. doi: 10.2106/00004623-199311000-00002. [DOI] [PubMed] [Google Scholar]
- 134.Beaton D.E., Wright J.G., Katz J.N., Upper Extremity Collaborative G. Development of the QuickDASH: Comparison of three item-reduction approaches. J. Bone Jt. Surg. Am. 2005;87:1038–1046. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 135.Franchignoni F., Vercelli S., Giordano A., Sartorio F., Bravini E., Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH) J. Orthop. Sport. Phys. Ther. 2014;44:30–39. doi: 10.2519/jospt.2014.4893. [DOI] [PubMed] [Google Scholar]
- 136.Lam K.H.S., Lai W.W., Ngai H.Y., Wu W.K.R., Wu Y.-T. Comment on the safety of the ultrasound-guided hydrodissection technique for carpal tunnel syndrome. J. Ultrasound. 2022 doi: 10.1007/s40477-022-00664-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Lam K.H.S., Lai W.W., Ngai H.Y., Wu W.K.R. Practical considerations for ultrasound-guided hydrodissection in Pronator Teres Syndrome. Pain Med. 2022;23:221–223. doi: 10.1093/pm/pnab277. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available within the manuscript.