Abstract
There is a rising incidence of coronary artery diseases and myocardial infarction (MI). Mortality associated with acute MI (AMI) is directly linked to the time to receive treatment and missed diagnoses. Although health professionals are aware of typical AMI presentation, atypical MI is difficult to diagnose, which on the other hand, is likely to have an impact on morbidity and mortality. Therefore, it is prudent to know such atypical presentations, especially for emergency and primary care physicians. We aimed to systematically evaluate the clinical presentations of atypical MI and analyze them to characterize the common clinical presentations of atypical MI. We researched the PubMed database, did citation tracking, and performed Google Scholar advanced search to find the cases reported on the atypical presentation of MI published from January 2000 to September 2022. Articles of all languages were included; Google Translate was used to translate articles published in languages other than English. A total of 496 (56 PubMed articles, 340 citations from included PubMed articles, and 100 articles from Google Scholar advanced search) were screened; 52 case reports were evaluated, and their data were analyzed. Atypical presentations of myocardial infarction are vast; patients may have chest pain without typical characteristics of angina pain or may not have chest pain. No typical characterization could be done. Most patients were in their fifth decade or above of their life and commonly presented with pain and discomfort in the abdomen, head, and neck regions. Prodromal symptoms were consistent findings, and many patients had two to three comorbidities out of four common comorbidities, i.e., diabetes, hypertension, dyslipidemia, and substance abuse. A patient who is 50 years old or more, having comorbidities such as diabetes, hypertension, dyslipidemia, history of tobacco or marijuana usage, presenting with prodromal symptoms like shortness of breath, dizziness, fatigue, syncope, gastrointestinal discomfort or head/neck pain should be suspected for atypical MI.
Keywords: emergency medical service, primary care medicine, acute ischemic heart disease, acute myocardial infarction, clinical features of myocardial ischemia, atypical presentation of myocardial ischemia, acute coronary syndrome
Introduction and background
Acute coronary syndrome (ACS) leading to myocardial infarction (MI) is the leading cause of mortality around the globe [1]. Acute MI (AMI) frequently leads to cardiogenic shock. Morbidity and mortality associated with MI are proportionate to the time taken to receive treatment from the onset of symptoms. Studies indicate chest pain as the most common presenting symptom (prevalence nearly 92%) in patients with suspected ACS [2,3]. This chest pain is often described with a few characteristics; retrosternal chest pain of squeezing/tightness/heaviness nature, which gets provoked by exertion or stress and relieved by rest or nitroglycerin. Pain may radiate to the left jaw and shoulder/arm. However, atypical clinical features, including but not limited to neck pain, pain in the back, throat pain, ear discomfort, and hiccups, are not uncommon [4,5]. Craniofacial pain can be the sole symptom in up to 6% of patients with AMI [6]. Women need special mention as they often present with atypical symptoms, and a high index of suspicion is required [7]. It can lead to delayed diagnosis, suboptimal treatment, and detrimental outcomes [8].
Moreover, around 5% of patients with AMI may develop cardiogenic shock with a mortality of 40-50% [9]. To avoid such mishaps, accurate and timely interpretation of atypical clinical symptomatology of AMI has a vital bearing on patient triage, treatment, and subsequent management. For example, improved survival has been demonstrated by the timely implementation of suitable reperfusion therapy [10]. With this background, we conducted a literature search and review related to atypical presentations of MI so that patients with such presentations can be suspected easily. Further, we also aimed to characterize the common atypical presentation, if possible.
Review
Study design and selection
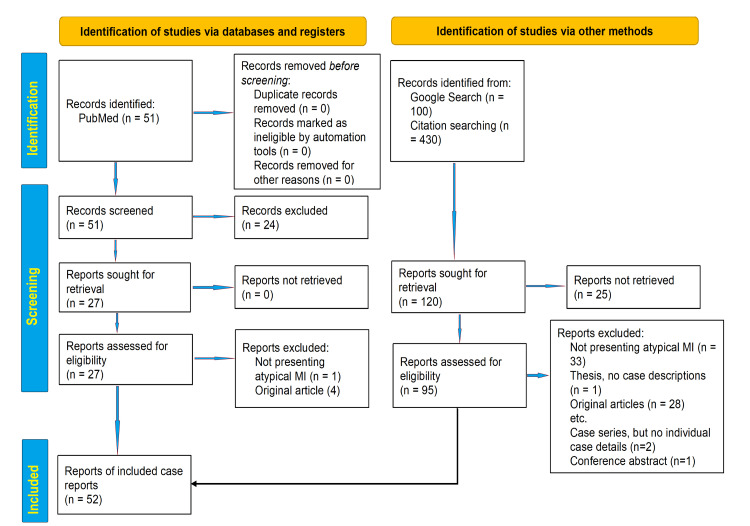
The present unregistered systematic review was conducted by searching the medical database in PubMed using PubMed advanced search engine and Medical Subject Heading (MeSH) index term combination of ("myocardial infarction"[Title/Abstract]) AND ("atypical presentation"[Title/Abstract]) to find the relevant articles published between 01/01/2000 and 30/09/2022. Further, we did a citation tracking of the included articles from the PubMed search process to collect and synthesize different atypical presentations of myocardial ischemia mentioned in recent literature. Furthermore, Google Scholar advanced search in the article's title with the words "myocardial infarction" (with all the words) and "atypical" (with at least one of the words) fields of the search engine was done. The period for the Google Scholar search was also limited to the same period as for PubMed. The article was searched by two researchers (Habib Md R. Karim [HK] and Ghazal Ahmed [GA]). Although our study does not require meta-analysis, the search methodology and result reporting are done as per the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines for the applicable segments.
Eligibility criteria
We included all case reports, letters, and commentary, with case details for atypical myocardial infarction. If case series reported individual cases, it was included, otherwise excluded. All other types of articles were excluded. If any article was available other than in the English language, we used Google Translate online to read the abstract and determine the suitability of inclusion. We did not include any grey material in the analysis. It was followed by a screening of the article by two researchers (Imran A. Khan [IK] and Chinmaya K. Panda [CP]) who were not involved in the respective database search. Tabulation of the included articles was done jointly by HK and IK, and Swatishree Nayak [SN] and CP did verification.
Statistical analysis
The characteristics (ages, gender, comorbidities, symptomatologies) of the case-based reports were further used to generate a master chart in Excell and analyzed to find the common characteristics of atypical presentation of MI. As no randomized study is feasible according to our study hypothesis and no original article has been analyzed, we have not reported any risk for bias.
Results
Our PubMed search yielded 51 articles - 26 were related to atypical MI, and 22 were case reports. There were 430 citations in these 26 related articles that were also used for citation tracking, and ten case reports were found eligible for inclusion. Furthermore, the Google Scholar search resulted in 100 articles after filtering the citations, which were screened and analyzed, and another 20 articles were included. The flow diagram depicting the search, screening, and inclusion is presented per the PRISMA 2020 flow diagram in Figure 1 [11].
Figure 1. PRISMA 2020 flow diagram .
MI - myocardial infarction; PRISMA - Preferred Reporting Items for Systematic Reviews and Meta-Analyses
The characteristics of the included case report-based articles are presented in Table 1.
Table 1. Brief description of included articles.
AF - atrial fibrillation; CAD - coronary artery disease; CRF - chronic renal failure; CVA - cerebrovascular accidents; DM - diabetes mellitus; ESRD - end-stage renal disease; F - female; HTN - hypertension; IHD - ischemic heart disease; M - male, PCI - percutaneous coronary intervention; RBBB - right bundle branch block; TIA - transient ischemic attack; TKR - total knee replacement; TTP - thrombotic thrombocytopenic purpura
| No. | Authors (year) [Reference] | N (sex/age in years) | Atypical symptoms | Comorbidities |
| 1 | Madias et al. (2002) [12] | Two (M/75, M/62) | Fatigue and lightheadedness, intermittent epigastric discomfort without nausea or vomiting | HTN, RBBB, DM, ESRD, hyperlipemia |
| 2 | Timurkaynak et al. (2002) [13] | One (F/28) | Severe, sudden onset of localized back pain and tachypnoea | Smoking, oral contraceptive use, thyrotoxicosis |
| 3 | Wittlesey (2002) [14] | One (M/54) | Pleuritic chest pain, worsening with movement and deep breathing, weakness, and fatigue | DM, HTN, Reiter's syndrome |
| 4 | Dwyer (2003) [15] | One (F/64) | Mid-back pain, dizziness, persistent cough | Chronic renal infection, RBBB, atrial premature contractions |
| 5 | Ivanović et al. (2005) [16] | One (M/44) | Atypical chest pain during exercise | None |
| 6 | Zeina et al. (2006) [17] | One (M/23) | Intermittent left-sided atypical chest pain | Hyperlipidemia |
| 7 | Wei et al. (2008) [18] | Two (M/36, F/85) | Intolerable and refractory headache, eyeball pain, atypical chest pain | CVA |
| 8 | Lin et al. (2009) [19] | One (M/83) | Severe and diffuse bone pain | DM |
| 9 | Siau K. (2009) [20] | One (M/61) | Pain along the medial aspect of his left thigh | Recurrent reflux oesophagitis |
| 10 | Kohli et al. (2010) [21] | One (F/66) | Sudden onset of slurred speech preceded by dizziness and vomiting | None |
| 11 | Amirhaeri et al. (2010) [22] | One (F/53) | Earache and sore throat | Smoker, dyslipidemia, DM, post-PCI |
| 12 | Davenport et al. (2012) [23] | One (M/68) | Intractable hiccups causing insomnia | DM, HTN, tobacco use |
| 13 | Her et al. (2012) [24] | One (F/54) | Atypical chest pain | Papillary fibroelastoma of the aortic valve |
| 14 | Holm et al. (2012) [25] | One (M/48) | Leg pain due to arterial occlusion | Smoking |
| 15 | Khoroshikh (2013) [26] | One (M/57) | Atypical hand pain, shortness of breath while walking | HTN, hypercholesterolemia, smoking |
| 16 | Abdalla et al. (2014) [27] | One (M/65) | Progressive dyspnoea, presyncope | Morbid obesity, post gastric bypass, depression, alcohol dependence |
| 17 | Basic-Jukic et al. (2014) [28] | One (M/55) | Otalgia on post-op renal transplant day three | DM, coronary stent, post-renal transplant |
| 18 | Dundar et al. (2014) [29] | One (F/87) | Otalgia with sweating on head and neck | DM |
| 19 | Petrović et al. (2014) [30] | One (M/63) | TIA without chest pain, sinus tachycardia | HTN, smoking |
| 20 | Parekh et al. (2014) [31] | One (M/55) | Unexplained lethargy and anxiety | CAD, post-stent, and on dual antiplatelet |
| 21 | Wang et al. (2014) [32] | One (M/79) | Abdominal pain and fever | Gastric villous adenoma, TTP |
| 22 | Ajayi et al. (2015) [33] | One (M/58) | Shortness of breathing, aphasia, with hypoxia | Prostate cancer, HTN, hyperlipidemia, peripheral vascular disease, alcoholism, and past-smoker |
| 23 | Taylor (2015) [34] | One (M/44) | Recurrent short-duration atypical chest pain with no radiation and no associated symptoms | Smoking |
| 24 | Bharvin et al. (2016) [35] | One (M/34) | Abdominal discomfort, pain, vomiting, and mild breathlessness | Alcohol use |
| 25 | Chaturvedi et al. (2016) [36] | One (M/77) | Syncope | HTN, DM |
| 26 | Ebrahem et al. (2016) [37] | One (F/39) | Syncopal episodes | Post splenectomy |
| 27 | Castillo et al. (2016) [38] | One (F/61) | Right sides arm and scalp numbness | None |
| 28 | Ahmed et al. (2017) [39] | One (M/43) | Right otalgia associated with mild dyspnoea and fatigability | DM, dyslipidemia, heavy smoker, family history of HTN and, IHD |
| 29 | Anzai et al. (2017) [40] | Three (F/72, M/84, F/89) | Pharyngeal pain/sore throat | Patient 1 - none; patient 2 - CRF, TIA, DM, aortic aneurysm; patient 3 - unstable angina |
| 30 | Zhang et al. (2017) [4] | One (M/51) | Intractable hiccups and fever without chest pain | HTN, DM, asthma, and gastritis, marijuana addiction |
| 31 | Kyaw et al. (2018) [41] | One (F/74) | Isolated throat pain and Wellens' pattern in the initial EGG | DM, HTN, dyslipidemia, hypothyroidism |
| 32 | Ugalde et al. (2018) [42] | One (M/47) | Bilateral otalgia | HTN and CAD |
| 33 | Bouthillet et al. (2019) [43] | One (F/75) | Tiredness, nausea, dizziness | HTN, DM, hyperlipidemia, and obesity |
| 34 | Broughton et al. (2019) [44] | One (M/59) | Bout of hiccups during hospital admission for septic arthritis | DM |
| 35 | Gao et al. (2019) [45] | One (M/46) | Recurrent abdominal pain, constipation, persistent hiccups | Smoker, CVA, cholecystitis |
| 36 | Ghazzay et al. (2019) [46] | One (M/55) | Diarrhea, mild lower abdominal pain, and nausea | DM, dyslipidemia, smoking |
| 37 | Mehmood et al. (2019) [47] | One (F/25) | Atypical chest pain relieved by deep sternal massage, anxiety | DM |
| 38 | Rigueira et al. (2019) [48] | One (F/66) | Atypical chest pain, nausea, and hypersudorese, followed by syncope | Rheumatoid arthritis, HTN, and dyslipidemia |
| 39 | Zakaria et al. (2019) [49] | One (F/31) | Epigastric pain, belatedness, and nausea | Post-COVID-19 |
| 40 | Alahmad et al. (2020) [50] | One (M/35) | Palpitation with De Winter ECG pattern | Palpitation, AF |
| 41 | Harikrishnan et al. (2020) [51] | One (M/65) | Fever, cough, shortness of breath | COVID-19 |
| 42 | Mandal s et al. (2020) [52] | One (F/36) | Back pain in the thoracic region | Polycystic ovarian syndrome |
| 43 | Pickard et al. (2020) [53] | One (M/56) | Shortness of breath in the recovery ward after TKR | Follow-up case of TKR |
| 44 | Faridi et al. (2021) [54] | One (M/39) | Pain abdomen, palpitation, episodic headache, and shortness of breath | Pheochromocytoma with secondary cardiomyopathy |
| 45 | Hovey et al. (2021) [5] | One (M/62) | Persistent hiccups | HTN, DM, CVA |
| 46 | Khan et al. (2021) [7] | One (48/F) | Atypical chest pain | None |
| 47 | Mayfield et al. (2021) [55] | One (63/F) | Left shoulder pain, tender to touch | Smoking |
| 48 | Santana et al. (2021) [56] | One (M/36) | Agitation, auditory hallucination | None |
| 49 | Atere et al. (2022) [57] | One (M/58) | Abdominal pain | Myeloproliferative neoplasm |
| 50 | Benjanuwattra et al. (2022) [58] | One (M/53) | Haemoptysis | HTN, dyslipidemia |
| 51 | Cheema et al. (2022) [59] | One (M/28) | Retrosternal atypical chest pain | Marfan syndrome, post aortic root and arch replacement |
| 52 | Kirchner (2022) [60] | One (F/47) | Stressed, jaw pain | None |
The included 52 case-based articles presented data from 56 patients; most reported cases were male, i.e., 36 (64.29%). The median, interquartile range of age of the pooled cases was 55.5 (44-65.75) years. The three most common atypical presentations were gastrointestinal discomfort, chest pain without having typical characteristics of angina pectoris, syncope, and cough and breathlessness, while the three most common comorbidities were diabetes, hypertension, and dyslipidemia (Table 2). Prodromal symptoms like dizziness, weakness, and fatiguability were frequently noted in such patients despite not having typical chest pain of acute coronary syndrome (Table 2).
Table 2. The derived data and results of common atypical symptoms and comorbidities.
| Parameters | Values | ||
| Age (in years) | Mean | Standard deviation | |
| 55.14 | 16.69 | ||
| Parameters (n=56) | Number | Percentage | |
| Gender | Male | 36 | 64.29 |
| Female | 20 | 35.61 | |
| Common atypical symptoms | Gastri-intestinal discomfort | 12 | 21.43 |
| Atypical chest pain | 10 | 17.86 | |
| Syncope | 7 | 12.5 | |
| Cough/breathlessness | 7 | 12.5 | |
| Sore throat/throat pain | 6 | 10.71 | |
| Otalgia | 5 | 8.92 | |
| Fatigue | 5 | 8.92 | |
| Dizziness | 4 | 7.14 | |
| Hiccups | 4 | 7.14 | |
| Anxiety | 4 | 7.14 | |
| Fever | 4 | 7.14 | |
| Palpitation | 3 | 5.35 | |
| Mid-back pain | 2 | 3.57 | |
| Headache | 2 | 3.57 | |
| Common comorbidities | Diabetes mellitus | 17 | 30.35 |
| Hypertension | 14 | 25.0 | |
| Dyslipidemia | 12 | 21.43 | |
| Smoking | 10 | 17.87 | |
| Coronary artery disease | 7 | 12.5 | |
| Chronic kidney disease | 4 | 7.14 | |
| Alcohol | 3 | 5.35 | |
| Obesity | 2 | 3.57 | |
| Thyroid abnormality | 2 | 3.57 | |
| COVID-19 | 2 | 3.57 | |
Discussion
The present analysis indicates that the atypical presentation of myocardial infarction is wide. We intended to know the atypical presentation as these bear critical value for physicians and the public as patients with AMI having atypical symptoms often delay in care seeking and suspecting or diagnosing by the treating physician resulting in poor prognosis [61]. The prevalence of atypical presentations is high, epidemiological studies indicate that 26% of MI patients can present without typical chest pain [62], and the atypical presentation of MI is nearly 34% [63]. Prodromal symptoms constitute a significant portion of the atypical presentations. Khan et al. [64] analyzed the prodromal symptoms and their gender differences in 1245 patients aged less than or equal to 55 years and found that women had a higher prevalence of prodromal symptoms than men. However, the prodromal symptoms were the same among both gender, i.e., unusual fatigue, sleep disturbances, arm ache/tingling, heart racing (palpitation), frequent indigestion, increased frequency/intensity of headache, etc. Although our analysis of the pooled cases can not indicate the prevalence data, the symptoms, including the prodromal, were similar to those found in the epidemiological studies [62-64]. ACS is a common and potentially life-threatening condition encountered in emergency departments (ED). Clinical symptoms are usually the first step for risk stratification of ED patients presenting with suspected ACS. Despite its dreaded nature, 33% of ACS may mislead clinicians with atypical presentations [65]. The atypical symptoms tend to occur more commonly among older, female, diabetic (possibly due to autonomic neuropathy), hypertensive, and with prior heart failure. They were reported in 5.7% and 12.3% of patients with unstable angina and non-ST elevation myocardial infarction (NSTEMI), respectively [66]. A delay in the diagnosis of ACS has been associated with poor clinical outcomes and increased mortality. Moreover, women have shown increased mortality than men, and increased atypical symptom presentations associated with myocardial infarction in women are thought to contribute to delayed presentation, lower diagnosis and treatment rates might be leading to worse outcomes [67]. International guidelines reinforce the view that atypical symptoms, such as epigastric pain, dyspepsia, or breathlessness, are more likely to present in women [68]. Although our analysis of the reported cases showed a more significant number of cases in males, it cannot refute the female preponderance as it is not an epidemiological study but rather an analysis of the published atypical cases, which represents the tip of the iceberg only.
Somatic referred pain is felt at a distant site other than the noxious stimulus-affected area, often described as dull with poor localization. The pain may radiate to corresponding dermatomes such as the epigastrium, shoulders, arms, back (interscapular region), lower jaw, and neck [69]. There are usually no neurological symptoms or weakness because there is no compression or direct injury of the spinal nerves. The pathophysiology is thought to be related to the neuroanatomy of the nerves innervating the heart and dermatome. Convergence-projection theory has been postulated as a cause of this referred pain. This occurs due to the incapability of the central nervous system to differentiate between stimuli that converge on common sensory pathways [70]. Our analysis showed that myocardial infarction could present with atypical chest pain or, most of the time, without chest pain. Although the common symptoms are gastrointestinal, cough, throat pain, and otalgia were also found in nearly 10% of cases, a few patients even presented with eyeball pain, pain along the medial aspect of their left thigh, left shoulder pain, agitation, auditory hallucination, hemoptysis, severe and diffuse bone pain, leg pain, atypical hand pain, jaw pain, right sides arm, and scalp numbness. All these vast types of pain, which are not even related to the dermatomes of the heart and chest, made it difficult to find a link between them. The same was also noted for associated comorbidities. While hypertension (HTN), diabetes mellitus (DM), dyslipidemia, and smoking have been linked in the epidemiological studies as risk factors [71], several other comorbidities were noted in our pooled cohort, i.e., recurrent reflux oesophagitis, gastric villous adenoma, thrombotic thrombocytopenic purpura, depression, post-surgery, asthma, polycystic ovarian syndrome, Reiter's syndrome, prostate cancer, myeloproliferative neoplasm, rheumatoid arthritis. However, our study can not ascertain their association with atypical presentation owing to the non-epidemiological nature of the methodology and the smaller pooled sample. Although some patients did not have proven risk factors for coronary artery disease (CAD), they had some other cardiac or vascular pathologies like pheochromocytoma with secondary cardiomyopathy, Marfan syndrome, post aortic root and arch replacement, cerebral infarction, peripheral vascular disease, papillary fibroelastoma of the aortic valve. Some patients also had a family history of HTN and ischemic heart disease (IHD) or had personal habits like tobacco chewing and marijuana addiction. Notably, 86% of the patients had comorbidities, and the majority had more than one. Interestingly two out of 57 patients also had post-COVID-19 status without any other comorbidities. While diabetes, HTN, dyslipidemia, and substance abuse are expected comorbidities, the intriguing finding was that nine (15.8%) patients had three, and another eight (14%) patients had two out of these comorbidities.
Our systematic review has only case reports, which, as such, have a low level of evidence. Although attrition, allocation, selection, blinding, and statistical analysis-related biases are unlikely in our selected articles, selective reporting of the symptoms and publication can still be possible. Further, not all cases are reported in the literature; instead, it is usually noted that unusual or unique cases are only published, so the impact of publication bias is very much feasible. The other limitation of our review is that we have not searched Embase or Web of Sciences as these were not freely accessible, which also have vast data. Although Google Scholar search and citation tracking are likely to cover up the limitation, there is still a possibility that a few cases might have been left out. We also limited our data research, including articles from the year 2000 and afterward. It was done with the intention to keep the data relevant to recent times as the definition of MI, their management, and even reporting of the cases in academic journals have undergone significant changes over the last few decades.
Conclusions
This review highlights the atypical presentations of myocardial infarctions. The analysis findings indicate that a primary care or ED physician should suspect atypical presentation of myocardial infarction even in patients who do not have chest pain or have chest pain but not having typical characteristics of angina pain. A patient is in the fifth decade of life or above, having comorbidities like DM, HTN, dyslipidemia, or having a habit of tobacco or marijuana use, significantly if associated with prodromal symptoms like feeling breathlessness, dizziness, fatiguability, or syncope, is likely to present with atypical presentation. As early diagnosis and intervention can save a life in AMI, such patients can be investigated to rule out AMI.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
Footnotes
The authors have declared that no competing interests exist.
References
- 1.Epidemiology of coronary heart disease and acute coronary syndrome. Sanchis-Gomar F, Perez-Quilis C, Leischik R, Lucia A. Ann Transl Med. 2016;4:256. doi: 10.21037/atm.2016.06.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Presenting symptoms in men and women diagnosed with myocardial infarction using sex-specific criteria. Ferry AV, Anand A, Strachan FE, et al. J Am Heart Assoc. 2019;8:0. doi: 10.1161/JAHA.119.012307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Development of a clinical prediction rule for 30-day cardiac events in emergency department patients with chest pain and possible acute coronary syndrome. Hess EP, Brison RJ, Perry JJ, et al. Ann Emerg Med. 2012;59:115–125. doi: 10.1016/j.annemergmed.2011.07.026. [DOI] [PubMed] [Google Scholar]
- 4.ST-segment elevation myocardial infarction with acute stent thrombosis presenting as intractable hiccups: an unusual case. Zhang F, Tongo ND, Hastings V, Kanzali P, Zhu Z, Chadow H, Rafii SE. Am J Case Rep. 2017;18:467–471. doi: 10.12659/AJCR.903345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Acute coronary syndrome presenting with hiccups. Hovey J, Perwez T, Regula P, Chaucer B, Nagalapuram V. Cureus. 2021;13:0. doi: 10.7759/cureus.16244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Craniofacial pain as the sole symptom of cardiac ischemia: a prospective multicenter study. Kreiner M, Okeson JP, Michelis V, Lujambio M, Isberg A. J Am Dent Assoc. 2007;138:74–79. doi: 10.14219/jada.archive.2007.0024. [DOI] [PubMed] [Google Scholar]
- 7.The Yentl syndrome: a case report. Khan B, Basnet AK. JNMA J Nepal Med Assoc. 2021;59:910–912. doi: 10.31729/jnma.7004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The relationship between off-hours admissions for primary percutaneous coronary intervention, door-to-balloon time and mortality for patients with ST-elevation myocardial infarction in England: a registry-based prospective national cohort study. Jayawardana S, Salas-Vega S, Cornehl F, Krumholz HM, Mossialos E. https://qualitysafety.bmj.com/content/29/7/541. BMJ Qual Safety. 2020;29:541–549. doi: 10.1136/bmjqs-2019-010067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Management of cardiogenic shock complicating myocardial infarction: an update 2019. Thiele H, Ohman EM, de Waha-Thiele S, Zeymer U, Desch S. Eur Heart J. 2019;40:2671–2683. doi: 10.1093/eurheartj/ehz363. [DOI] [PubMed] [Google Scholar]
- 10.Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Devereaux PJ, Xavier D, Pogue J, et al. Ann Intern Med. 2011;154:523–528. doi: 10.7326/0003-4819-154-8-201104190-00003. [DOI] [PubMed] [Google Scholar]
- 11.The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Page MJ, McKenzie JE, Bossuyt PM, et al. BMJ. 2021;372:0. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Posterior myocardial infarction and complete right bundle- branch block. Madias JE, Bravidis D, Attari M. Chest. 2002;122:1860–1864. doi: 10.1378/chest.122.5.1860. [DOI] [PubMed] [Google Scholar]
- 13.Acute myocardial infarction secondary to thyrotoxicosis. Timurkaynak T, Aydogdu G, Cengel A. Acta Cardiol. 2002;57:439–442. doi: 10.2143/AC.57.6.2005470. [DOI] [PubMed] [Google Scholar]
- 14.Case study: atypical myocardial infarction in a man with type 2 diabetes. Wittlesey CD. Clin Diabetes. 2002;20:101–102. [Google Scholar]
- 15.Atypical presentation of myocardial infarction in the outpatient setting, a lapse in clinical knowledge and inadequate data transfer constitute a potentially fatal error. Dwyer K. Int J Qual Health Care. 2003;15:179. doi: 10.1093/intqhc/mzg027. [DOI] [PubMed] [Google Scholar]
- 16.Atypical presentation of right coronary artery occlusion. Ivanović V, Jelkić N, Srdić S, Bikicki M, Canji T, Srdanović I. Med Pregl. 2005;58:498–502. doi: 10.2298/mpns0510498i. [DOI] [PubMed] [Google Scholar]
- 17.Atypical presentation of acute myocardial infarction in a young man diagnosed by multidetector computed tomography. Zeina AR, Orlov I, Blinder J, Hassan A, Rosenschein U, Barmeir E. https://www.ima.org.il/MedicineIMAJ/viewarticle.aspx?year=2006&month=01&page=69. Isr Med Assoc J. 2006;8:69–70. [PubMed] [Google Scholar]
- 18.Cardiac cephalalgia: case reports and review. Wei JH, Wang HF. Cephalalgia. 2008;28:892–896. doi: 10.1111/j.1468-2982.2008.01590.x. [DOI] [PubMed] [Google Scholar]
- 19.Bone pain as an atypical early manifestation of acute myocardial infarction. Lin GM, Han CL. Am J Emerg Med. 2009;27:894–895. doi: 10.1016/j.ajem.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 20.Thigh pain preceding myocardial infarction--is this merely coincidence? Siau K. Int J Cardiol. 2011;147:19–20. doi: 10.1016/j.ijcard.2009.06.035. [DOI] [PubMed] [Google Scholar]
- 21.An unusual presentation of acute coronary syndrome. Kohli SC, Parajuli M, Maskey A, Acharya CP. https://pubmed.ncbi.nlm.nih.gov/21876578/ J Nepal Health Res Counc. 2010;8:124–125. [PubMed] [Google Scholar]
- 22.Myocardial infarction with unusual presentation of otalgia: a case report. Amirhaeri S, Spencer D. Int J Emerg Med. 2010;3:459–460. doi: 10.1007/s12245-010-0222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hiccups as the only symptom of non-ST-segment elevation myocardial infarction. Davenport J, Duong M, Lanoix R. Am J Emerg Med. 2012;30:266–262. doi: 10.1016/j.ajem.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 24.Papillary fibroelastoma of the aortic valve with atypical chest pain: late presentation with acute myocardial infarction and cardiac arrest. Her AY, Kim YH, Heo JW, Yie K, Lee S. J Card Surg. 2012;27:327–330. doi: 10.1111/j.1540-8191.2011.01385.x. [DOI] [PubMed] [Google Scholar]
- 25.Atypical primary symptom in the form of peripheral syndromeion after painless myocardial infarction [in Danish] Holm J, Taskiran M, Nielsen T. https://ugeskriftet.dk/videnskab/atypisk-debutsymptom-i-form-af-perifer-emboli-efter-stumt-myokardieinfarkt. Ugeskr Laeger. 2012;174:2310–2311. [PubMed] [Google Scholar]
- 26.Atypical variants of myocardial infarction. case report of a rare form of acute coronary syndrome with peripheral equivalent of angina [in Russian] Khoroshikh OA. https://www.actabiomedica.ru/jour/article/view/1650 Acta Biomedica Scientifica. 2013;28:104–107. [Google Scholar]
- 27.'STEMI-like' acute pulmonary embolism, an unusual presentation. Abdalla A, Kelly F. BMJ Case Rep. 2014;2014:0. doi: 10.1136/bcr-2014-206517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pain in the left ear as the presenting symptom of acute myocardial infarction in a renal transplant recipient. Basic-Jukic N, Novosel D, Ivanac I, Danic-Hadzibegovic A, Kes P. Transplant Proc. 2014;46:284–285. doi: 10.1016/j.transproceed.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 29.Myocardial infarction as a rare cause of otalgia. Dundar R, Kulduk E, Kemal Soy F, Sengul E, Ertas F. Case Rep Otolaryngol. 2014;2014:106938. doi: 10.1155/2014/106938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Syncope as initial symptom of ostial lesion of the left main coronary artery with cardiogenic shock. Petrović M, Ivanov I, Vujin B, Ivanović V, Redzek A. Vojnosanit Pregl. 2014;71:1066–1071. doi: 10.2298/vsp1411066p. [DOI] [PubMed] [Google Scholar]
- 31.An atypical presentation of an extremely late stent thrombosis after more than 7 years (2634 days) of DES implantation in a patient without obvious risk factors on regular dual antiplatelet therapy. Parekh P, Agrawal N, Vasavada A, Vinchurkar M. BMJ Case Rep. 2014;2014:0. doi: 10.1136/bcr-2013-202454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Acute myocardial infarction caused by tumor-associated thrombotic thrombocytopenic purpura: case report. Wang J, Cai X, Cheng X, Song P, Jiang S, Gong J. Med Princ Pract. 2014;23:289–291. doi: 10.1159/000354096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Atypical presentation of acute myocardial infarction. [ Feb; 2023 ];Ajayi T, Nureddin A, Minhas J, Roberts D. https://www.consultant360.com/articles/atypical-presentation-acute-myocardial-infarction Consultant360. 2015 55 [Google Scholar]
- 34.Atypical myocardial infarction on a cruise ship. Taylor C. https://journals.viamedica.pl/international_maritime_health/article/view/IMH.2015.0006/28966. Int Marit Health. 2015;66:22–24. doi: 10.5603/IMH.2015.0006. [DOI] [PubMed] [Google Scholar]
- 35.A case of myocardial infarction with an atypical presentation. Bharvin AS, Devi RMR, Kumar SP. https://njp.org.in/images/pdf/2016-issue-1-amina.pdf Nat J Physiol. 2016;4:43–45. [Google Scholar]
- 36.Apical hypertrophic cardiomyopathy with hemodynamically unstable ventricular arrhythmia - atypical presentation. Chaturvedi H, Pandey RD, Sharma KK, Makkar JS, Sharma SK. Indian Heart J. 2016;68:0–6. doi: 10.1016/j.ihj.2015.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chronic myeloid leukemia: a case of extreme thrombocytosis causing syncope and myocardial infarction. Ebrahem R, Ahmed B, Kadhem S, Truong Q. Cureus. 2016;8:0. doi: 10.7759/cureus.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Atypical acute myocardial infarction and concomitant acute cerebral infarct. Castillo J. https://cdn.mdedge.com/files/s3fs-public/issues/articles/em048070305.pdf Emerg Med. 2016;48:305–308. [Google Scholar]
- 39.ST-elevation myocardial infarction due to left anterior descending artery occlusion presenting primarily with otalgia. Ahmed EK, Alkodaymi MS, Soliman MM, Shujaa AS. Am J Case Rep. 2017;18:1044–1047. doi: 10.12659/AJCR.905511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Unusual pharyngeal pain caused by acute coronary syndrome: a report of three cases. Anzai T, Hiroshige Y, Nakamura M, Iizuka T, Nakazato Y, Ikeda K. Clin Pract. 2017;7:904. doi: 10.4081/cp.2017.904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Atypical presentation of acute coronary syndrome and importance of Wellens' syndrome. Kyaw K, Latt H, Aung SS, Tun NM, Phoo WY, Yin HH. Am J Case Rep. 2018;19:199–202. doi: 10.12659/AJCR.907992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Myocardial infarction presenting as ear fullness and pain. Ugalde I, Anjum I, Lo Presti S, Tolentino A. J Investig Med High Impact Case Rep. 2018;6 doi: 10.1177/2324709618761753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Atypical presentation of myocardial infarction: quickly recognizing unusual symptoms can save lives. Bouthillet K. https://www.myamericannurse.com/atypical-presentation-of-myocardial-infarction/ American Nurse Today. 2019;14:13–14. [Google Scholar]
- 44.Acute myocardial ischemia associated with hiccups. Broughton J, Sharma A. CMAJ. 2019;191:0. doi: 10.1503/cmaj.181285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Acute proximal left anterior descending thrombosis manifested by persistent hiccups: a case report. Gao H, Zhang B, Song L, Yao S, Zhang Z, Bai M. Medicine. 2019;98:0. doi: 10.1097/MD.0000000000018096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Diarrhea as atypical symptom of acute myocardial infarction. Ghazzay H, Kamil A. https://www.iasj.net/iasj/article/172514 Al-Anbar Med J. 2019;15:48–50. [Google Scholar]
- 47.Atypical presentation of non-ST elevation myocardial infarction in a young Bengali women. Mehmood T, Munir I, Pena-Teotico M, et al. J Am Coll Cardiol. 2019;73:2913. [Google Scholar]
- 48.Atypical form of acute myocardial infarction with tamponade. Rigueira J, Rodrigues T, Aguiar-Ricardo I, Cunha N, Placido R, Pinto FJ, Almeida AG. Eur Heart J Cardiovasc Imaging. 2019;20:110. [Google Scholar]
- 49.Thrombotic event post covid-19 infection: a case of myocardial infarction in COVID-19 survivor with atypical presentation. Zakaria MB, Razak ZR, Mustafa MS, Ahmad HB. https://www.m-jem.com/index.php/mjem/article/view/1216/698 M-JEM. 2021;5:126. [Google Scholar]
- 50.De Winter T-wave electrocardiogram pattern due to thromboembolic event: a rare phenomenon. Alahmad Y, Sardar S, Swehli H. Heart Views. 2020;21:40–44. doi: 10.4103/HEARTVIEWS.HEARTVIEWS_90_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Atypical presentations in COVID-19-lung abscess, pulmonary thromboembolism and ST-elevation myocardial infarction: diagnosis and management in a temporary COVID-19 hospital. Harikrishnan P, Mohakuda S, Pathak B, et al. J Mar Med Soc. 2020;22:128–132. [Google Scholar]
- 52.Atypical presentation of myocardial infarction in a young patient with polycystic ovarian syndrome. Mandal S, Pradhan RR, Mols Kowalczewski B. Cureus. 2020;12:0. doi: 10.7759/cureus.9494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.A post-operative masquerade: simulation-based scenario challenging clinical clerks to recognize an atypical presentation of myocardial infarction. Pickard V, O'Regan NB, Sheppard G, Dubrowski A. Cureus. 2020;12:0. doi: 10.7759/cureus.7510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bilateral pheochromocytoma: an atypical cause of myocardial infarction in a young male. Faridi SH, Harris SH, Afrose R, Siddiqui B, Ashraf H. World J Endoc Surg. 2021;13:64–67. [Google Scholar]
- 55.Sex-based differences in the presentation of myocardial infarction. Mayfield J, Gill M, Zhang HJ, Ganti L. Cureus. 2021;13:0. doi: 10.7759/cureus.16906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Spontaneous coronary artery dissection associated with incidental finding of left ventricular thrombus. Santana M, Guragai N, Patel B, et al. J Community Hosp Intern Med Perspect. 2021;11:249–252. doi: 10.1080/20009666.2021.1891689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Atypical myocardial infarction with apical thrombus and systemic embolism: a rare presentation of likely JAK2 V617F-positive myeloproliferative neoplasm. Atere M, Al-Zakhari R, Collins J, Rotatori F, Muzangwa L. Case Rep Oncol Med. 2020;2020:9654048. doi: 10.1155/2020/9654048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Massive haemoptysis following recurrent ST-elevation myocardial infarction due to undiagnosed granulomatosis with polyangiitis. Benjanuwattra J, Abdelnabi MH, Mekraksakit P, Ansari MM. BMJ Case Rep. 2022;15:0. doi: 10.1136/bcr-2021-246748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.A case report of Marfan syndrome presenting with atypical chest pain: a 28-year-old male with non-st-elevation myocardial infarction (NSTEMI) Cheema T, Balek M, Smith P, Hanan S. Cureus. 2022;14:0. doi: 10.7759/cureus.22040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Atypical myocardial infarction - clinical judgement led to swift action. Kirchner J. https://www.myamericannurse.com/atypical-myocardial-infarction-heart/ American Nurse. 2022;17 [Google Scholar]
- 61.Clinical impact of atypical chest pain and diabetes mellitus in patients with acute myocardial infarction from prospective KAMIR-NIH Registry. Lee JW, Moon JS, Kang DR, et al. J Clin Med. 2020;9:505. doi: 10.3390/jcm9020505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Characteristics and outcomes of MI patients with and without chest pain: a cohort study. Coventry LL, Bremner AP, Williams TA, Celenza A, Jacobs IG, Finn J. Heart Lung Circ. 2015;24:796–805. doi: 10.1016/j.hlc.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 63.Determinants of clinical presentation on outcomes in older patients with myocardial infarction. Breining A, Negers A, Mora L, et al. Geriatr Gerontol Int. 2018;18:1591–1596. doi: 10.1111/ggi.13530. [DOI] [PubMed] [Google Scholar]
- 64.Sex differences in prodromal symptoms in acute coronary syndrome in patients aged 55 years or younger. Khan NA, Daskalopoulou SS, Karp I, et al. Heart. 2017;103:863–869. doi: 10.1136/heartjnl-2016-309945. [DOI] [PubMed] [Google Scholar]
- 65.Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. Canto JG, Shlipak MG, Rogers WJ, et al. JAMA. 2000;283:3223–3229. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 66.Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Brieger D, Eagle KA, Goodman SG, Steg PG, Budaj A, White K, Montalescot G. Chest. 2004;126:461–469. doi: 10.1378/chest.126.2.461. [DOI] [PubMed] [Google Scholar]
- 67.Delayed care and mortality among women and men with myocardial infarction. Bugiardini R, Ricci B, Cenko E, et al. J Am Heart Assoc. 2017;6:0. doi: 10.1161/JAHA.117.005968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.CardioPulse: 'Ten Commandments' of 2015 European Society of Cardiology Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation (NSTE-ACS) Roffi M, Patrono C. https://europepmc.org/article/med/27471758. Eur Heart J. 2016;37:208. [PubMed] [Google Scholar]
- 69.On the definitions and physiology of back pain, referred pain, and radicular pain. Bogduk N. Pain. 2009;147:17–19. doi: 10.1016/j.pain.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 70.Visceral referred pain. Giamberardino MA, Affaitati G, Costantini R. J Musculoskelet Pain. 2010;18:403–410. [Google Scholar]
- 71.Risk factors for coronary artery disease: historical perspectives. Hajar R. Heart Views. 2017;18:109–114. doi: 10.4103/HEARTVIEWS.HEARTVIEWS_106_17. [DOI] [PMC free article] [PubMed] [Google Scholar]