Abstract
Despite the obvious morphological differences in the visual system, zebrafish share a similar architecture and components of the same embryonic origin as humans. The zebrafish retina has the same layered structure and cell types with similar metabolic and phototransduction support as humans, and is functional 72 h after fertilization, allowing tests of visual function to be performed. The zebrafish genomic database supports genetic mapping studies as well as gene editing, both of which are useful in the ophthalmological field. It is possible to model ocular disorders in zebrafish, as well as inherited retinal diseases or congenital or acquired malformations. Several approaches allow the evaluation of local pathological processes derived from systemic disorders, such as chemical exposure to produce retinal hypoxia or glucose exposure to produce hyperglycemia, mimicking retinopathy of prematurity or diabetic retinopathy, respectively. The pathogenesis of ocular infections, autoimmune diseases, or aging can also be assessed in zebrafish larvae, and the preserved cellular and molecular immune mechanisms can be assessed. Finally, the zebrafish model for the study of the pathologies of the visual system complements certain deficiencies in experimental models of mammals since the regeneration of the zebrafish retina is a valuable tool for the study of degenerative processes and the discovery of new drugs and therapies.
Keywords: zebrafish, larvae model, retina, visual impairment, diabetic retinopathy, regeneration, ocular infections
1. Introduction
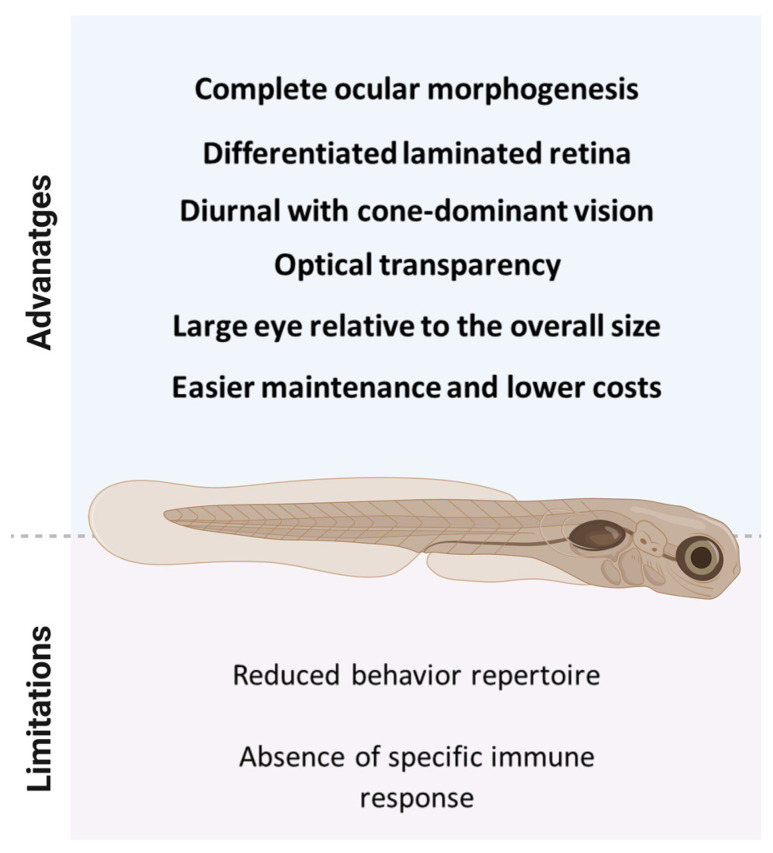
Zebrafish (Danio rerio) present development of the brain, nervous system, and visual system that is similar to that of other vertebrates, which makes it a valuable model for the study of visual neuroscience. The anatomical, physiological, genetic, and behavioral components of zebrafish visual processing were studied in adults and during the embryo-larval period (Figure 1), providing an opportunity for the study of disorders related to defects in the developmental process, hereditary diseases, or provoked by environmental stressors (light, chemicals, or trauma), infections and [1,2].
Figure 1.
Experimental advantages and limitations of 72 h post-fertilization zebrafish larvae.
Here, we revisit important insights into zebrafish visual system morphogenesis, and summarize established zebrafish models of ocular pathologies, from inherited retinal diseases to congenital or acquired malformations and ocular infections. We discuss important features of photoreceptor degenerations, as well as anterior and posterior eye diseases, along with pathophysiological mechanisms and their relation to human diseases. We also discuss the contribution of zebrafish to regenerative research and highlight the understanding of zebrafish retina regeneration, reinforcing future directions to explore ophthalmological research with zebrafish.
For this review, we searched the PubMed database and cited recent articles, most of which were published in the last 5 years. Articles previous to 2018 that are cited refer to proof-of-concept articles or consolidated concepts about anatomical features, physiological hallmarks, or pathophysiological mechanisms.
2. Zebrafish Ocular Development and Physiology
Eye development begins with the specification of the eye field within the anterior neural plate, which is established by the overlapping expression of several eye field transcription factors. The structures of the anterior eye include the cornea, lens, iris, ciliary body, hyaloid vasculature, and specialized structures at the iridocorneal angle, and the structures of the posterior eye include the neural retina, retinal pigment epithelium (RPE), and choroid.
The morphogenesis of the visual system in zebrafish presents similarities with humans since it is also based on the same three embryonic tissues: neuroectoderm, superficial ectoderm, and mesenchyme. The optic vesicle, a structure that derives from the forebrain, appears at approximately 12 hpf (hours post fertilization) and at 20 hpf it forms a structure composed of an internal neural ectoderm, which will give rise to the retina and external neural ectoderm, which give rise to the RPE, forming the posterior segment of the eye [3].
The retina is a structure of particular interest as it is responsible for sensory detection and damage to the retina results in loss of vision. Zebrafish retinal neurogenesis begins with the differentiation of ganglion cells at around 28 hpf in the ventronasal retina, followed by amacrine, horizontal and Müller glia cells at around 50 hpf. The exit of the axons to the optic tectum occurs around 40 hpf. Most of the lamination process of the retina occurs by 48 hpf. Between 50 and 55 hpf, the expression of opsin and rod cells begins and four different cone photoreceptor subtypes (UV-, S-, M-, and L-cones) become apparent. Synaptic structures indicative of functional maturation (ribbon triads) arises within photoreceptor synaptic terminals at around 65 hpf, followed by bipolar cell ribbon synapses at approximately 70 hpf. The signal transmission from photoreceptors to second-order neurons starts around 84 hpf and becomes fully functional at 5 dpf [4]
Structurally, the mature zebrafish retina is composed of three nuclear layers separated by the outer and inner plexiform layers (OPL and IPL, respectively). Photoreceptor cell bodies (rods and cones glutamate releasing-cells) reside in the outer nuclear layer (ONL), amacrine (local dopaminergic interneurons that provide modulation pre- and/or post-synaptically), bipolar (glutamatergic neurons that transmit light signals into the next processing layer), and horizontal (inhibitory interneurons that locally modulate photoreceptor synaptic output) occupy the inner nuclear layer (INL), and ganglion cell bodies (glutamatergic spiking neurons) are contained in the ganglion cell layer (GCL). Synapses between these nuclear layers and retinal neurons occur in the plexiform layers [1,4,5].
From GCL, ganglion cell axons emerge and form the optic nerve, which transmits information to the optic centers in the brain. Additionally, the retina contains microglia (resident immune cells located primarily in the synaptic layers) and two types of true glial cells: Müller cells (a type of radial glia) and astrocytes (associated with axons of retinal ganglion cells—RGCs) [4].
Photoreceptors (PRs) are specialized cells that compose the layered structure of the retina and promote and maintain the phototransduction process. These neuron cells comprise the inner segment (IS), where most of the organelles required for metabolic functions are found, and the outer segment (OS), which is rich in mitochondria, generating the necessary amount of energy for phototransduction. UV-cones are short single cones that express sws1, an opsin with maximum sensitivity in the ultraviolet range. The S-cones are long single and express sws2, with sensitivity to short wavelengths in blue. M-cones express rh2 class opsins, detecting medium wavelengths in red. L-cones express an lws-class opsin gene, with sensitivity to longer wavelengths in green. In rod and cone photoreceptors, light triggers opsin activation followed by phototransduction and synaptic signaling [6].
The photoreceptors also closely associate with the RPE cells, which provide structural, trophic, and metabolic support and are directly involved in the recycling of opsins [6]. Damage in PRs can be caused by several cellular dysfunctions, such as non-functional ion channels and enzymes and altered phototransduction cascade components or cellular structures. Melanin in the RPE is believed to play an important role in protecting photoreceptors from light-induced damage by absorbing stray light, which would otherwise degrade retinal image quality [6]. Thus, RPE dysfunctions negatively affect the photoreceptors, ultimately leading to cell death.
The process of intraocular vascularization is initiated at 29 hpf by a population of mesodermal and neural crest cells that have migrated around the optic cup to enter the eye through the choroid fissure to form the periocular mesenchyme (POM). This mesenchyme gives rise to the first hyaloid vessels. Rapidly, the vessels organize in a hemispherical basket at the back of the lens forming the hyaloid vasculature, which is composed entirely of arterial vessels. This embryonic hyaloid vasculature is eventually replaced by the mature retinal vasculature that is tightly associated with the RGC layer [7]. The final step in the development of a functional vasculature is the formation of the blood–retinal barrier (BRB) by vascular endothelial cells lining the retinal vessels and an epithelial component formed by the RPE [8].
The zebrafish cornea is a laminated avascular structure and quite similar to that of a human, presenting the epithelium, Bowman’s layer, stroma, Descemet’s membrane, and a single layer of junctionally connected and polygonal endothelium cells. However, the zebrafish cornea has a thinner stroma and does not show corneal nerve fibers [9]. In the same way, the iridocorneal angle in zebrafish and humans is responsible for maintaining the intraocular pressure (IOP) by producing and draining aqueous humor.
Although the zebrafish lens is more spherical than a human’s and made of an outer epithelial layer, its morphological structure is remarkably similar to that of humans [7]. The lens is contained within a semi-elastic capsule and grows by depositing concentric layers of fibrous cells over existing tissue. Epithelial cells proliferate, differentiate, and elongate into lens fiber cells at the equator of the capsule. Fiber cells contain high concentrations of crystalline proteins that range from periphery to center, creating a gradient of concentration and refraction. The zebrafish lens delaminates from the overlying surface ectoderm as a solid mass of cells rather than invaginating to form a hollow vesicle [10].
Zebrafish show a high degree of binocular coordination; most of the time, the eyes are moved in a conjugate fashion with the notable exception of convergence during prey capture and spontaneous monocular saccades [11]. Recently, the oculomotor system studies were expanded by Brysch, Leyden, & Arrenberg (2019) [12], which presented evidence for a mixed mono-/binocular code in the hindbrain.
The oculomotor system for horizontal movement participates in maintaining the stability of eye positions, as well as eye movements during saccades, optokinetic, and vestibulo-ocular reflexes (OKR and VOR, respectively) and other behaviors.
Quick eye movements are important components of visual behavior, improving individual visual ability. Schoonheim, Arrenberg, Del Bene & Baier (2010) [13] described the brain region responsible for saccade movement in a larval zebrafish model, besides describing the neuron circuitry, suggesting certain homology to mammal circuits. The comprehension of complex eye movements is essential for a better understanding of ocular disorders, providing different perspectives for novel treatments.
3. Zebrafish as a Model for Ocular Pathologies
Zebrafish is a suitable model for the recapitulation of eye and vision diseases since it allows the sub-localization of the injury process from the visualization of the eye and its structures through the transparent larva. In this way, the underlying cellular and molecular mechanisms of pathology can be understood. Phenotype-based screening, including the assessment of the behavioral repertoire pattern of zebrafish larvae, has been applied to assess visual-neural circuits and has revolutionized the scientific environment of the pharmaceutical industry, allowing the simultaneous screening of numerous new molecules, the repositioning of already approved drugs, as well as the investigation of alternative therapies [14,15,16].
Several groups have been using mutagenesis (large-scale mutant or targeted genetic screens) or gene editing approaches to create mutants and morphants of zebrafish in order to obtain models for the study of human congenital eye diseases. More recently, the use of CRISPR-mediated gene editing technology associated with the use of morpholinos in zebrafish fluorescent reporter lines can track potentially pathogenic genetic variants as well as understand the intricate molecular signaling cascade underlying diseases provoked by environmental stressors (light, chemicals, or trauma), infections, altered metabolisms, and aging reviewed by [17,18]. With these approaches in zebrafish, congenital malformations generated from disruptions in genes important for the morphogenesis of both anterior and posterior structures of the eye during the early stages of embryonic development have been mapped.
Studies from several groups demonstrate the requirement of some genes in malformations of the anterior structures of the eye in zebrafish, recapitulating diseases such as microphthalmia (M), anophthalmia (A), and synophthlamia/cyclopia. According to Yin et al. (2014) [19], transcription factors such as retinal homeobox (Rx) are vital for the correct development of the eye, and zebrafish with mutated genes encoding these factors demonstrated that eye morphogenesis is dependent on a signaling network to regulate these factors. Besides genetic mutations, the modulation of transcription factors can be assessed with chemical exposure. Santos-Ledo et al. (2013) [20] exposed zebrafish embryos to ethanol treatment and observed that ethanol exposure disrupts the correct eye morphogenesis.
Coloboma (C) resulted from the failure of the optic fissure to close properly, and Pillai-Kastoori et al. (2014) [21] showed that the transcription factor Sox11 is required to maintain specific levels of Hedgehog signaling during ocular development; once Sox11 has mutated, zebrafish present abnormal ocular formation. Likewise, hyaloid vasculature formation is crucial for optic fissure fusion, and the action of transcription factor pax2a facilitates the remodeling process [22].
Aniridia (complete absence of the iris), corneal opacities, iris hypoplasia, aphakia (absence of the lens), and corneal dystrophies are anterior eye abnormalities, and were reproduced in zebrafish [23,24]. Shi et al. (2005) [25] described a zebrafish model of Peter’s anomaly (persistent adhesion between the cornea and lens), identifying a gene encoding a protein similar to humans, the Pitx3 protein. Microphthalmia and aphakia were modeled in mab21l2−/− mutant zebrafish [26]. Besides, Axenfeld–Rieger syndrome (combinations of anterior segment malformations with dental anomalies) and human congenital nystagmus (HCN)/infantile nystagmus syndrome (INS) [27,28,29] have also been recapitulated in zebrafish.
Finally, cataracts (congenital or age-related), defined as a clouding or loss of transparency in the lens, have been recapitulated in zebrafish that possess gene orthologs expressed exclusively in the lens (reviewed by [30]—Table 1).
Table 1.
Defects of the Anterior Eye.
| Ocular Disease | Reference | Model | Zebrafish Features * | Human Features * |
|---|---|---|---|---|
| Cataracts (congenital or age-related) | Morris, 2011 [30] | Extensive review | ||
| Li et al., 2012 [31] | Mutation of crygc | Embrionic lens defects | Congenital cataract phenotype | |
| Wu, Zou, Mishr & Mchaourab, 2018 [32] | Mutation of cryga and crygb | |||
| Mishra et al., 2018 [33] | Mutation of crygb | |||
| Vorontsova, Gehring, Hall, & Schilling, 2018 [34] | Mutation of aqp0a and aqp0b | |||
| Zhang et al., 2020 [35] | dnase1l1l knockout | Lens denucleation defect and cataract | Not described | |
| Anophthalmia (A) | Yin et al., 2014 [19] | Mutation of rx3 | Anophthalmia and expanded forebrain | Microphthalmia and anophthalmia |
| Synophthlamia/cyclopia | Santos-Ledo et al., 2013 [20] | six3a, rx3 and rx1 disruption | Cyclopia | Holoprosencephaly and cyclopia |
| Swartz et al., 2013 [36] | vangl2, plk1, hinfp, mars, and foxi1 disruption | Synophthalmia and narrowing of the palatal skeleton | Not described | |
| Coloboma (C) | Pillai-Kastoori et al., 2014 [21] | Mutation of sox11 | Delayed and abnormal lens formation, coloboma, and reduction in rod photoreceptors | Coloboma phenotype |
| Weaver, Piedade, Meshram, & Famulski, 2018 [22] | pax2a depletion | Optic fissure (OP) failure | Not described | |
| Ouyang et al., 2022 [37] | Loss-of-funtion of hnrnph1 | Coloboma | High myopia | |
| Corneal opacities | Reis et al., 2019 [38] | Mutation of wdr37 | Cataract, microphthalmia, glaucoma, corneal clouding | Corneal opacity, coloboma, microcornea |
| Iris hypoplasia | Chawla, Swain, Williams, & Bohnsack, 2018 [23] | Increase/decrease in retinoic acid modulating myoc and pitx2 | Changes in the ventral iridocorneal angle and decreased aqueous outflow | Corneal, iris, and trabecular meshwork abnormalities |
| Aniridia | Seese et al., 2021 [24] | Loss-of-function of mab21l1 | Congenital glaucoma aphakia, malformed retina, and abnormally thick cornea, severe microphthalmia, disorganized retinal lamination, abnormal anterior structures | Microphthalmia, variable aniridia, coloboma, microcornea, lens defects (microspherophakia, cataracts) and nystagmus |
| Peter’s anomaly | Shi et al., 2005 [25] | Mutation of pitx3 | Lens or other anterior segment defects | Anterior segment dysgenesis, Peter’s anomaly, and cataracts. |
| Axenfeld–Rieger syndrome | Reviewed by French, 2021 [39] | Extensive review | ||
| Microphthalmia (M) | Casey et al., 2011 [40] | Mutation of stra6 | Congenital eye malformations | Non-syndromic anophthalmia |
| Aphakia | Gath & Gross, 2019 [26] | Loss-of-function of mab21l2 | Lens and retina defects, coloboma | Defects of lens development |
| Corneal dystrophies | Oliver et al., 2015 [41] | Mutation of col17a1a | Not described | Epithelial recurrent erosion dystrophy (ERED) |
| Human congenital nystagmus (HCN)/infantile nystagmus syndrome (INS) | Huang et al., 2006 [27] | Defective retinotectal projections | Strong spontaneous eye oscillations | Congenital nystagmus |
| Maurer, Huang, & Neuhauss, 2011 [28] | ||||
| Huber-Reggi et al., 2011 [29] | ||||
* Features specifically related to eye disorders.
The effect of gene knockdown or knockout on eye development has been used to investigate the crucial role of numerous genes in the development of the posterior eye that lead to several ocular dysfunctions, vision impairment, and blindness. Retinal degeneration (RD) forms a group of diseases resulting from a primary dysfunction in the RPE that are classified into three types: (i) diseases primarily affecting rods; (ii) diseases primarily affecting cones; and (iii) diseases where both photoreceptors (PRs) are affected.
Photoreceptor dystrophies are characterized by photoreceptor loss on the retina, and the disbalance of the retinal pigmented epithelium (RPE) leading to RD. In zebrafish, cones rely on RPE-expressed Cralbpa protein for chromophore regeneration and retinal function, and Schlegel et al. (2019) [42] reported that rlbp1a impairment disturbed the photoreceptor morphology, ultimately leading to cellular degeneration. Other factors such as growth differentiation factor 6a (gdf6a) are important to photoreceptor maintenance; Nadolski et al. (2020) [43] reported that mutated gdf6a in zebrafish led to photoreceptor aberrant growth and morphology.
RD encompasses several inherited retinal dystrophies such as retinitis pigmentosa (RP, an inherited heterogeneous disease), age-related macular degeneration (AMD), diabetic retinopathy (DR), achromatopsia, cone–rod dystrophy, and congenital stationary night blindness. Jia et al. (2014) [44] demonstrated that proper synaptic ribbon formation is essential for photoreceptor function. To assess this matter, the author used mutant zebrafish expressing human Cacna1f as a model system.
Night vision impairment is a key feature of congenital stationary night blindness (CSNB), representing a non-progressive disease caused by defective synapsis between photoreceptors and ON-bipolar cells. Bahadori et al. (2006) [45] explored the activity of nyctalopin protein on photoreceptor metabolism as a model for CSNB. Some other RD are characterized by hypopigmentation/albinism, such as Chediak–Higashi syndrome, and Hermansky–Pudlak syndrome, a disease characterized by oculocutaneous albinism, and were successfully modeled in zebrafish by Bahadori et al. (2006) [46].
Furthermore, zebrafish have greatly improved the understanding of diseases of posterior structures of the eye related to several syndromes, such as Leber’s congenital amaurosis (LCA), modeled by Minegishi, Nakaya, & Tomarev (2018) [47] through a cct2 mutant zebrafish line, whereas Stiebel-Kalish et al. (2012) [48] studied the same disease with a Gucy2f zebrafish knockdown line; Stargardt’s disease, Bardet–Biedl syndrome (BBS), Usher syndrome, Joubert syndrome, Meckel-Gruber syndrome, and Senior-Loken syndrome (Table 2).
Table 2.
Defects of the Posterior Eye.
| Ocular Disease | Reference | Model | Zebrafish Features * | Human Features * |
|---|---|---|---|---|
| Age-related macular degeneration (AMD) | Noel et al., 2020 [49] | Mutation of rp1l1 | Photoreceptor degeneration | Photoreceptor diseases |
| Rastoin, Pagès, & Dufies, 2020 [50] | Extensive review | |||
| Xia et al., 2020 [51] | Knockdown of ube3d | Neovascular AMD | Oxidative damage in retinal pigment epithelium (hRPE) (in vitro) | |
| Cheng et al., 2021 [52] | Blue light-induced retinal damage | Retinal degeneration | Not described | |
| Noel, Allison, MacDonald, & Hocking, 2022 [53] | Extensive review | |||
| Diabetic retinopathy | Jung, Kim, Lee, & Kim, 2016 [54] | Glucose exposure | Neovascularization, dilation of hyaloid-retinal vessels | Diabetic retinopathy |
| Lee & Yang, 2021 [55] | ||||
| Singh et al., 2019 [56] | Neovascularization, dilation of hyaloid-retinal vessels, and microvascular alterations | |||
| Reichenbach et al., 2007 [57] | Extensive review | |||
| Li et al., 2019 [58] | Methylglyoxal exposure | Neovascularization, dilation of hyaloid-retinal vessels | Diabetic retinopathy | |
| Glaucoma | Skarie & Link, 2009 [59] | Knockdown of foxc1 | Disruption of vascular endothelial tissue | Glaucoma |
| Iglesias et al., 2014 [60] | Knockdown of six6b | Small eye phenotype | Not described | |
| Williams, Eason, Chawla, & Bohnsack, 2017 [61] | Manipulation of cyp1b1 | Regulation of ocular fissure closure | Mutation on cyp1b1 is related to primary infantile-onset glaucoma | |
| Giannaccini et al., 2018 [62] | Exposure to H2O2 | Oxidative stress-induced damage | Not described | |
| Cavodeassi & Wilson, 2019 [18] | Extensive review | |||
| Morales-Cámara et al., 2020 [63] | Knockout of guca1c | Retinal ganglion cell apoptosis | Not described | |
| Retinitis pigmentosa (RP) | Zelinka, Sotolongo-Lopez, & Fadool, 2018 [64] | Mutations of rh1–1 | Rod degeneration | Autosomal dominant retinitis pigmentosa |
| Ganzen et al., 2021 [65] | rho:NTR zebrafish line | Rod ablation | Not described | |
| Santhanam et al., 2020 [66] | Mutation of p23h | Rod degeneration | Not described | |
| Campochiaro & Mir, 2018 [67] | Extensive review | |||
| Crouzier et al., 2021 [68] | Mutation of pde6a | Photoreceptor degeneration | Retinitis pigmentosa | |
| Kawase et al., 2016 [69] | Ligh-induced retinopathy | Not described | ||
| Lu et al., 2019 [70] | Mutation of prom1 | Retinitis pigmentosa, macular degeneration, and cone–rod dystrophy | ||
| Noel et al., 2020 [49] | Mutation of rp1l1 | Photorecepetor disease | ||
| Schlegel, Ramkumar, von Lintig, & Neuhauss, 2021 [42] | Mutation of rlbp1 | |||
| Zhang et al., 2021 [71] | rho:NTR zebrafish line | Rod ablation | Not described | |
| Achromatopsia | Kennedy et al., 2007 [72] | No optokinetic response of mutant (nof) | Achromatopic blindness | Not described |
| Stearns, Evangelista, Fadool, & Brockerhoff, 2007 [73] | Mutation of pde6c | Blindness (degeneration of cone photoreceptors) | Achromatopsia | |
| Viringipurampeer et al., 2014 [74] | ||||
| Huang et al., 2018 [75] | Mutation of per2 | Reduced vision behavior | Not described | |
| Cone–rod dystrophy | Iribarne et al., 2017 [76] | Zebrafish Gold Rush mutant (aipl1 mutant) | Cone-specific degeneration | Leber congenital amaurosis 4 (LCA4) |
| Daly et al., 2017 [77] | Zebrafish dying on edge (dye) mutant | Defective visual behavior, altered retina morphology, photoreceptor degeneration | Visual impairment | |
| Schlegel et al., 2019 [78] | Knockout of cacna2d4b | Electroretinogram impaired response (defective phototransduction) | Retinal dysfunction (impaired cone vision) | |
| Nadolski et al., 2020 [43] | Mutation of gdf6a | Microphthalmia, photoreceptor degeneration | Not described | |
| Congenital stationary night blindness | Bahadori et al., 2006 [46] | Zebrafish fade out (fad) mutant | Retina structural defects, photoreceptor degeneration | Hermansky–Pudlak syndrome (HPS) |
| Jia et al., 2014 [44] | Zebrafish wait until dark (wud) mutant | Electroretinogram impaired response (defective phototransduction) | Congenital stationary night blindness type 2 (CSNB2) | |
| Leber’s congenital amaurosis (LCA) | Stiebel-Kalish et al., 2012 [48] | Knockdown of gucy2df | Shortening of cone and rod outer segments. | Leber congenital amaurosis-1 (LCA1). |
| Minegishi, Nakaya, & Tomarev, 2018 [47] | Mutation of cct2 | Microphthalmia | ||
| Bardet–Biedl syndrome (BBS) | Castro-Sánchez et al., 2019 [79] | Mutation of bbs | Microphthalmia | Ciliopathy |
| Song et al., 2020 [80] | Photoreceptor degeneration | |||
| Usher syndrome | Gopal et al., 2015 [81] | Knockout of clrn1 | Ciliopathy | Ciliopathy |
| Miles, Blair, Emili, & Tropepe, 2021 [82] | Mutation of pcdh15b | Loss of photoreceptor integrity | Blindness associated with Usher syndrome type 1 (USH1) | |
| Joubert syndrome | Song & Perkins, 2018 [83] | Mutation of arl13a | Slow progressive photoreceptor degeneration | Joubert syndrome phenotype |
| Liu, Cao, Yu, & Hu, 2020 [84] | Knockout of tmem216 | Photoreceptor degeneration | ||
| Rusterholz, Hofmann, & Bachmann-Gagescu, 2022 [85] | Extensive review | |||
| Meckel-Gruber syndrome | Lessieur et al., 2019 [86] | Zebrafish cep290fh297/fh297 mutant | Slow progressive photoreceptor degeneration | Meckel-Gruber syndrome phenotype |
| Hermansky-Pudlak syndrome | Bahadori et al., 2006 [46] | Zebrafish fade out (fad) mutant | Retina structural defects, photoreceptor degeneration | Hermansky–Pudlak syndrome (HPS) |
* Features specifically related to eye disorders.
Finally, the development of methods to measure intraocular pressure (IOP) in zebrafish mutants has enhanced the offer of models for the study of the complex genetics and molecular mechanisms of congenital or age-related glaucoma. Glaucoma characterized by ganglion cell death and damage to the optic nerve can be divided into primary open-angle glaucoma, in which the iridocorneal angle is not blocked, primary closed-angle glaucoma, in which the iridocorneal angle is blocked, and secondary glaucoma, in which the glaucoma arises due to a prior insult to the eye (reviewed by [18]. Table 2).
The World Report on Vision [87] by WHO estimates that the leading causes of vision impairment and blindness are cataract (17.8 million and the second leading cause of moderate or severe vision impairment, with 83.2 million), glaucoma (3.6 million and the fourth leading cause of moderate or severe vision impairment, with 4.1 million), age-related macular degeneration (AMD, 1.9 million and the third leading cause of moderate or severe vision impairment, with 6.2 million), and diabetic retinopathy (DR, 1.1 million and the fifth leading cause of moderate or severe vision impairment, with 3.8 million people). The report estimates that a person can have more than one cause of vision impairment; however, epidemiological studies tend to report only the primary cause.
In this review, we will detail the research carried out in a zebrafish model that aims to elucidate the genetic and cellular mechanisms of the diseases that most affect the world population: cataract, glaucoma, age-related macular degeneration (AMD), and diabetic retinopathy (DR). Finally, we will also address the progress made in this model organism of retinitis pigmentosa (RP) and the regeneration process.
3.1. Cataract
Cataract is a disease characterized by visual impairment due to lens opacity. This disorder is considered the primary cause of vision loss, and is therefore a major public health issue [88]. According to disease origins, cataract can be classified as congenital, when caused by genetic mutation and consequent misfolding of the lens proteins. Physiologically, the lens is formed by laminar structures of fiber cells derived from epithelial cells. In the fiber cells that form the lens, crystallin is a key protein to maintain the optical properties and its expression represents a complete differentiated state of fiber cells [89,90].
The crystallin protein family represents about 90% of soluble proteins in the human lens, including α-, β-, and γ-crystallins [91]. According to data reviewed by Hong & Luo (2021) [15], mutated genes encoding the crystallin proteins lead to the misfolding of proteins, resulting in degraded and unfunctional proteins and, consequently, lens abnormality, resulting in visual impairment. Thus, the generation of models with mutated lens proteins represents a valuable tool to study cataract phenotypes [92,93,94].
Li et al. (2012) [31] injected mutant crystallin gamma C (crygc) mRNA into zebrafish embryos, producing a mutated crystallin protein, which resulted in a cataract phenotype. In the same way, Wu, Zou, Mishra, & Mchaourab (2018) [32] used transgenic strains of zebrafish with crystallin protein mutations, which produced lens abnormalities, similar to the findings of Mishra et al. (2018) [33], who developed a zebrafish line with the loss of function of αB-crystallin and reported that a greater part of the embryo presented lens abnormalities, suggesting that this protein is essential to lens development.
Besides crystallin, other protein types also contribute to lens formation. As reviewed by Zhang et al. (2020) [35], for the correct lens development process, an organelle-free zone is crucial in order for fiber cells to appear optically transparent. In this process, the cells’ nuclei must be removed through degradation by nuclease enzymes. In the same work, the author produced a mutant zebrafish line induced by the CRISPR-Cas9 system with silenced DNase1l1l, an essential enzyme for the lens fiber cell denucleation process. The work resulted in the successful induction of a cataract phenotype in zebrafish.
The membrane-bound organelles of fiber cells in the lens undergo degradation during terminal differentiation. Organelle degradation by PLAAT (phospholipase A/acyltransferase, also known as HRASLS)-family phospholipases is essential for achieving optimal transparency and refractive function of the lens. Morishita et al. (2021) [95] reported that Hrasls phospholipases of the Plaat1 family in zebrafish are essential for the degradation of lens organelles such as mitochondria, the endoplasmic reticulum, and lysosomes.
In the developing lens, the RNA-binding protein Rbm24 binds to a wide spectrum of lens-specific mRNAs through the RNA recognition motif and interacts with the cytoplasmic polyadenylation element-binding protein (Cpeb1b) and cytoplasmic poly(A)-binding protein (Pabpc1l) through the C-terminal region. Shao et al. (2020) [96] demonstrated in zebrafish embryos that the expression of the rbm24 gene is restricted in differentiating lens fiber cells, and its loss of function severely compromises the accumulation of crystallin proteins in the developing lens. Moreover, Rbm24 binds to a wide spectrum of lens-specific mRNAs and interacts with key components of the cytoplasmic polyadenylation complex.
Aquaporins are proteins with water permeability regulation activities, and are, according to Vorontsova, Gehring, Hall & Schilling (2018) [34], essential to lens transparency. These authors used mutant zebrafish to assess the role of these proteins on lens development and reported that Aquaporin 0a and Aquaporin 0b knocked out zebrafish present fiber lens cell disruption and lens opacity, similar to the cataract phenotype.
During the differentiation of epithelial to fiber cells, most organelles are lost, turning into quiescent cells and are thus more vulnerable to exogen damage. Thus, cataract can also be classified as acquired, generally when derived from primary conditions. High levels of glucose (diabetic cataract), ionizing radiation (radiation cataract), and alteration in intraocular pression (glaucoma) are common triggers of cataract, besides aging (age-related cataract) (Lu et al., 2022) [97]. These primary disorders produce high levels of reactive oxygen species (ROS), which are counterbalanced by the protective antioxidant system.
GJA8 is a major gap junction protein in the vertebrate lens, and mutations in the gja8 gene cause cataracts in humans. The well-known cataractogenesis mechanism is that mutated GJA8 leads to abnormal assembly of gap junctions, resulting in defects in intercellular communication between lens cells. In the study of Ping et al. (2021) [98], they demonstrated that the ablation of Gja8b (a homolog of mammalian gja8) in zebrafish led to severe defects in organelle degradation, an important cause of cataractogenesis in the developing lens.
The nuclear factor-erythroid-2-related factor 2 (Nrf2), a transcriptional factor for cell cytoprotection, is known as the master regulator of redox homeostasis. Nrf2 regulates a wide range of genes involved in cellular protection against contributing factors of oxidative stress, including aging, disease, and inflammation. Nrf2 was reported to disrupt the oxidative stress that activates nuclear factor-κB (NFκB) and pro-inflammatory mediators. One representative example is the matrix metalloproteinase 9 (MMP-9), which may decompose the extracellular matrix (ECM) of lens epithelial cells (LECs) [99].
In both primary conditions and aging, the balance between ROS production and antioxidant system failure leads to oxidative stress, causing DNA damage and lipid oxidation in fiber cells, leading to cellular protein degradation, resulting in lens opacity (reviewed by [100].
3.2. Glaucoma
Under physiological conditions, aqueous humor is drained in order to preserve intraocular pressure, and this drainage system is composed of a structured outflow channel consisting of the trabecular meshwork, Schlemm’s channel, and the uveoscleral channel. The elevated intraocular pressure caused by an undeveloped drainage system leads to retinal ganglion cells death, culminating with optic nerve degeneration and consequent irreversible blindness, characterizing glaucoma [101]. As reviewed by Gross & Perkins (2008) [102], zebrafish are an ideal model system to study genetic mutations and multigenic interactions that lead to glaucoma.
Skarie & Link (2009) [59] reported that a mutant zebrafish line with silenced forkhead box C1 (foxc1) presented altered hyaloid vasculature and arteriovenous defects, as well as ocular hemorrhages and increased vascular permeability, indicative of the disruption of basement membrane integrity, which is related to the glaucoma development process. The most striking feature of Axenfeld–Rieger Syndrome (ARS) is developmental abnormalities in the anterior segment of the eye, leading to an increased risk of early-onset glaucoma. With loss-of-function techniques in zebrafish (CRISPR and morpholino), several zebrafish models have been reported to recapitulate the phenotypes of patients with ARS attributable to the foxc1 gene mutations (reviewed by [39]. Morales-Cámara et al. (2021) [63] studied the involvement of guanylate cyclase activator 1C (guca1c) in the pathophysiology of primary congenital glaucoma through the generation of a guca1c knocked out zebrafish, which presented cell apoptosis and gliosis, with the Müller cells intensifying the expression of glial fibrillary acidic protein. The biochemical events led to retinal damage similar to cataract.
In zebrafish, which have all four cone subtypes, rh2 opsin gene expression depends on homeobox transcription factors such as sine oculis homeobox 7 (six). Using a morpholino strategy, Iglesias et al. (2014) [60] produced a knockdown zebrafish with loss-of-function of (six6b), which resulted in underdeveloped eyes in individuals, which is the result of an altered proliferative pattern of retinal cells, suggesting an involvement of this gene with primary open-angle glaucoma. However, the six7 gene is found only in the ray-finned fish lineage, suggesting the existence of another evolutionarily conserved transcriptional factor(s) controlling rh2 opsin expression in vertebrates. Ogawa et al. (2019) [103] found that the reduced rh2 expression caused by six7 deficiency in zebrafish by the TALEN-induced mutation method was rescued by forced expression of six6b, which is a six7-related transcription factor conserved widely among vertebrates.
Through genetic and pharmacologic modulation of yp1b1 and retinoic acid, it is possible to investigate the CYP1B1 gene function, and Williams, Eason, Chawla, & Bohnsack (2017) [61] described that both under- and overexpression of cyp1b1 affects the permeability of the ocular fissure, implying an ocular pressure disbalance, similar to glaucoma. To test the efficacy of neurotrophins on glaucoma treatment, Giannaccini et al. (2018) [62] exposed zebrafish larvae to an oxidative stress protocol induced by ocular injection of H2O2. The oxidative damage depleted the retinal ganglionar cells, a propitious condition to develop glaucoma.
3.3. Age-Related Macular Degeneration (AMD)
Cone photoreceptors are equally affected by degenerative disorders. Age-related macular degeneration (AMD) affects cone photoreceptors leading to progressive central vision loss, visual acuity impairment, and color vision defects. The degeneration impacts macular cone photoreceptors, and occurs in two forms: atrophic, also called dry AMD, where the RPE, photoreceptor and choroid go through an atrophy process, and neovascular, also called wet AMD, characterized by fluid accumulation from fragile and unfunctional new blood vessels in choroid.
RP1L1 is a component of the photoreceptor axoneme, the backbone structure of the photoreceptor’s light-sensing outer segment. Noel et al. (2020) [49] generated a rp1l1 zebrafish mutant using CRISPR/Cas9 genome editing and found that mutant fish had progressive photoreceptor functional defects, determined by electrophysiological assessment, indicating that mutations in rp1l1 lead to photoreceptor degenerations.
Ubiquitin protein ligase E3D (UBE3D) gene missense has been proven to be associated with neovascular AMD in the East Asian population. The ube3d gene was knocked down in zebrafish by Xia et al. (2020) [51], and increased angiogenesis was observed in ube3d morphants.
It was demonstrated by Ashikawa et al. (2017) [104] in zebrafish that the deletion of fatty acid desaturase (fads2), which encodes a protein that functions as both Fads1 and Fads2 in other species, enhanced apoptosis in the retina upon exposure to intense light. Similarly, pharmacological inhibition of Srebf1 enhanced apoptosis and reduced fads2 expression in zebrafish exposed to intense light.
Mutations in human prominin 1 (prom1), encoding a transmembrane glycoprotein localized mainly to plasma membrane protrusions, have been reported to cause retinitis pigmentosa, macular degeneration, and cone-rod dystrophy. Lu et al. (2019) [70] utilized a zebrafish model to investigate prom1a and prom1b’s role in the retina and found that prom1b, rather than prom1a, plays an important role in zebrafish photoreceptors. The loss of prom1b disrupted outer-segment (OS) morphogenesis, with cones degenerating at an early age, whereas rods remained viable but with an abnormal OS, even at 9 months post fertilization.
The pathogenesis of AMD using zebrafish von Hippel-Lindau (vhl) mutants demonstrated the development of key aspects of the human AMD disease condition, including activation of the hypoxia-inducible factor (HIF) signaling pathway, polycythemia, excessive neovascularization, macular edema, and pronephric abnormalities [105].
The disruption of RPE is also involved in the pathophysiology of AMD, once the atrophic AMD results in photoreceptor degeneration derived from RPE loss. As demonstrated by Lu, Leach, & Gross (2022) [106] using rpe65a:nfsB-eGFP transgenic zebrafish and metronidazole (MTZ)-mediated cell ablation, the mTOR activation is involved in the repair response to the retinal damage initiated by Müller glia.
Rastoin, Pagès & Dufies (2020) [50] compiled data about neovascular AMD, as well as its pathophysiology and treatment. Furthermore, the authors explored the zebrafish as a model system, connecting important factors related to novel angiogenesis and the rise of AMD.
By concept, AMD is derived from photoreceptor degeneration. Thus, different assaults can trigger the degenerative process. Cheng et al. (2021) [52] exposed zebrafish to light-induced retinal damage, and reported light-induced apoptosis, oxidative stress, DNA damage and autophagy on retinal cells, suggesting the production of a zebrafish model to AMD.
3.4. Diabetic Retinopathy (DR)
Diabetic retinopathy (DR) associated with several diabetes-induced dysfunctions include the apoptosis of endothelial cells (ECs) and pericytes, a chronic low-grade inflammatory response with leukocyte adhesion to the retinal vasculature, increased vascular permeability, breakdown of the blood–retinal barrier (BRB), and the presence of acellular capillaries and microaneurysms. The pathogenesis of DR is multi-faceted and includes oxidative stress, pro-inflammatory changes, and advanced glycation end products (reviewed by [107]. The prevalence of DR from the year 2015–2019 has been described [108] as 27% of non-proliferative diabetic retinopathy (NPDR) covering almost up to a quarter, followed by diabetic macula oedema (DMO) at 4.6% and proliferative diabetic retinopathy (PDR) at 1.4%.
The induction of a hyperglycemic status is a valuable approach to study the pathologic alterations in zebrafish retina derived from diabetic retinopathy. Jung, Kim, Lee, & Kim (2016) [54] exposed 3 days post-fertilization (dpf) zebrafish larvae to an embryo medium with several concentrations of glucose and defined the treatment as high-glucose condition. The study demonstrated that 72 h of exposure to a concentration of 130 mM of glucose was able to provoke morphological alterations in hyaloid-retinal vessels (augmented vessel diameter), increased levels of VEGF mRNA, and irregular staining of the zonula ocludens-1 protein (ZO-1), indicating endothelial tissue disruption.
In the same way, Lee & Yang (2021) [55] exposed 3 dpf zebrafish larvae to determined concentrations of glucose for 72 h. The authors found increased retinal vessel diameter and VEGF and diminished expression of ZO-1. They also measured the retina layer thickness through histology, and despite no alterations, the TUNEL (terminal deoxynucleotidyl transferase dUTP nick end labeling) assay revealed increased apoptotic cells following glucose exposure. Hyperglycemia during embryogenesis of the retina also leads to pathological alterations in the retina vasculature.
Singh et al. (2019) [56] used different concentrations of glucose (4 and 5%) to induce hyperglycemia during embryonic development in zebrafish. The work consisted of 3 hpf embryos exposed to glucose in a fluctuating way, alternating the different concentrations of glucose every 24 h with vehicle until 120 hpf. They evidenced an alteration in the retinal vasculature, with exposure to 4% and 5% of glucose increasing the retinal blood sprouts and provoking microvascular damage, evidenced by extravasation of the hemoglobin in retinal blood vessels. Additionally, the histologic analysis showed increasing INL thickness, suggestive of Müller glial cell hypertrophy. According to Reichenbach et al. (2007), the hypertrophy and loss of metabolic function of Müller glia cells lead to progressive neuronal loss and consequent visual impairment.
Advanced glycation end products (AGEs) seem to be related to DR; the glucose metabolite methylglyoxal (MG) and its derived hydroimidazolone were found in elevated levels in the blood of patients with PDR [109]. Thus, Li, Zhao, Sang, & Leung (2019) [58] exposed 10 hpf zebrafish to different concentrations of MG until 96 hpf, in combination with glucose or not to mimic diabetes hyperglycemia. As a positive control to angiogenesis, they used GS4012 as an angiogenesis inducer. The authors reported that treatments with a higher concentration of MG (1000 µM) and MG plus glucose caused an increase in retinal blood vessel diameter and vascular density, similar to the group exposed to VEGF inducer, indicating intense angiogenesis following MG treatment.
3.5. Retinitis Pigmentosa (RP)
Both rods and cones PR can be affected by developmental diseases. As reviewed by Noel, Allison, MacDonald, & Hocking (2022) [53], defective cellular processes such as inefficient cell adhesion and impaired vesicle trafficking, along with ciliopathies, can drive PR diseases and degeneration, and can generally be modeled by producing mutants expressing failed visual function and ocular architecture genes.
RP is a genetically heterogeneous disease in which one of a large number of mutations causes the death of rod photoreceptors, and it is a common nomenclature for rod photoreceptor diseases and degeneration. Photoreceptor loss provokes a disruption of retina homeostasis due to an alteration of the metabolic processes, and consequently leads to retina dysfunction. Inflammatory events and the activation of glial cells (gliosis) damage the blood–retina barrier and the retinal vascular unit, causing pathological retina remodeling [110,111].
Night blindness and progressive peripheral vision impairment are signals of rod photoreceptor loss, a primary event of RP. After the complete degeneration of rod cells, visual function is maintained by cone photoreceptors, where macular cones ensure central vision. Nevertheless, secondary to RP, cone photoreceptor degeneration generally occurs, provoking total blindness disorders. Neurodegeneration caused by inherited retinal dystrophies (IRDs) leads to visual impairment and even blindness [112].
Zelinka, Sotolongo-Lopez & Fadool (2018) [64] produced a transgenic zebrafish with a specific mutation in the gene encoding the visual pigment rhodopsin (RHO), which is a common cause of retinitis pigmentosa (RP). Transgenic zebrafish expressing mutant human rhodopsin—Tg(rho:Hsa.RH1_Q344X)—was used by Ganzen et al. (2021) [65] as a RP model. The Q344X larvae intrinsically presented significant rod degeneration circa 120 hpf.
In the same way, Santhanam et al. (2020) [66] generated a RP model through a transgenic line of zebrafish expressing a mutation that results in a misfolded rhodopsin, which activates the unfolded protein response followed by proteasomal degradation, leading to rod cell death. Furthermore, it has been demonstrated that the death of rods reduces oxygen consumption, resulting in residual excess oxygen in the outer retina and the consequent production of superoxide radicals. High levels of superoxide radicals overload the antioxidant defense system and generate more reactive species, including peroxynitrite. This results in progressive oxidative damage to the cones, which contributes to their death and loss of function (reviewed by [67].
Cyclic nucleotide phosphodiesterase (PDEs) is an enzyme family that catalyzes nucleotide hydrolysis, and PDE6a plays a key role in the phototransduction process. In humans, mutated pde6a leads to RP. The crucial role of PDE6a was demonstrated in a zebrafish transgenic strain with a mutated PDE6a protein in retinal rods, which presented degeneration of rods and consequent vision impairment [68].
Kawase et al. (2016) [69] used light-induced retinal damage (LIRD) in 72 hpf zebrafish larvae, aiming to compare and identify deregulated genes in several models of LIRD. To perform the test, zebrafish larvae were held in the absence of light from 72 to 120 hpf, and then exposed to intense light (13,000 lux) for 24 h. The zebrafish larvae remained in the presence or absence of the histone acetyltransferase (HAT) EP300 inhibitor C646. The treatment was able to produce increasing apoptosis, photoreceptor degeneration, and Müller cell proliferation. They found that EP300 protects the retina against light-induced damage, acting as an anti-apoptotic agent.
In order to evaluate whether the cellular retinaldehyde-binding protein (CRALBP) is involved in pigment regeneration in the visual system, Schlegel, Ramkumar, von Lintig, & Neuhauss (2021) [42] produced a knockout (KO) zebrafish line for rlbp1a and rlbp1b, genes that encode for CRALBP in retinal pigmented epithelium (RPE) cells and Müller glia cells (MGCs), respectively. To assess the effect of CRALBP on retinoid metabolism, the larvae were exposed to a LIRD protocol consisting of different light exposures (30 min or 1 h exposure to 20,000 lux, with adaptation to the dark or not). They found that in rlbp1a-KO, accumulation of subretinal lipid deposits and dimorphic outer segments (OS) occurred, indicating the abnormal development or death of photoreceptors in 120 hpf larvae. Thus, the protocol of LIRD was able to produce retinal damage similar to that found in genetic disorders such as retinitis pigmentosa.
Thus, Zhang et al. (2021) [71] executed a large-scale drug screening with a zebrafish larvae model of RP using a transgenic line (rho:YFP-NTR) that express a yellow fluorescent protein (YFP) and a bacterial nitroreductase (NTR) enzyme in rod photoreceptors. This inducible model of RP was effective to implicate Poly (ADP-ribose) polymerase (PARP) as a key mediator of NTR/Mtz-mediated rod cell ablation.
4. Ocular Infections
While chronic eye diseases such as cataract, glaucoma, age-related macular degeneration, and diabetic retinopathy now account for a greater proportion of blindness and vision impairment globally and have their cellular and molecular mechanisms investigated in at least one zebrafish model, other treatable conditions equally important in inducing vision disturbances and blindness are still waiting to be recapitulated in the zebrafish model. Among the common eye conditions causing vision impairment, corneal injury can increase the risk of infections and keratitis.
Some of the most common pathogens that are associated with bacterial keratitis particularly when the corneal epithelial barrier is compromised or injured include Gram-positive organisms, such as coagulase-negative Staphylococcus, (e.g., Staphylococcus epidermidis), and the common Gram-negative strain Pseudomonas, Chlamydia trachomatis, Onchocerca volvulus (transmitted by the blackfly Simulium damnosum), virus (herpes simplex), filamentous fungi such as Fusarium spp. and Aspergillus spp., protozoa such as acanthamoeba, tuberculosis, and Toxoplasma gondii.
However, it is worth mentioning that infectious causes such as trachoma and onchocerciasis have declined in the last 30 years in the world [113] while Zika virus (ZIKV), a positive-sense, single-stranded, enveloped RNA virus belonging to the Flaviviridae family, has provided a large number of cases of congenital Zika syndrome due to vertical transmission characterized by severe microcephaly and ocular abnormalities, including chorioretinal atrophy with a hyperpigmented border and focal pigment at the macula, optic nerve abnormalities, and lens dislocation [114].
Recently, we recapitulated for the first time ZIKV infection using zebrafish embryos and larvae, especially the ability of ZIKV to infect head and eye structures during embryonic development, leading to developmental changes characterized by a reduction in head size and increased thickness of the retinal cell layers with consequent impairment of neurological and visual functions [115]. Toxoplasma gondii tachyzoites were demonstrated to infect cardiac myocytes, liver, spleen, brain, ovaries, pancreas, kidney and skeletal muscles, gills, and eyes of adult zebrafish; clinical signs presented in these fish included bilateral exopthalmia [116].
Takaki, Ramakrishnan, & Basu (2018) [117] developed a model for ocular tuberculosis by artificial infection with Mycobacterium marinum (M. marinun), by injecting the pathogen into the caudal vein of 48 and 72 hpf zebrafish larvae. The M. marinum is a classical pathogen to study tuberculosis in zebrafish, leading to ocular granulomas in zebrafish similar to that in humans. Additionally, they verified that the pathogen is able to infect the eyes even with an intact blood–retina barrier (BRB). Li & Hu (2012) [118] studied the pathophysiology of Staphylococcus aureus (S. aureus) infection in a multi-site infection approach, inoculating the pathogen in distinguished locations of 36 hpf zebrafish. The microinjection of S. aureus in the eye led to the local growth of bacteria with intense migration of neutrophils followed by macrophages, and the eye was also affected by yolk circulation valley injection.
Although Chlamydia [119], Onchocerca volvulus [120], and HSV-1 virus [121] research were conducted in the zebrafish model and recapitulated the infection and the concomitant immune and anti-viral responses, ocular abnormalities were not mimicked in this model.
Detailed analyzes have shown that many of the developmental features of eye formation are conserved between zebrafish and humans. However, there are notable differences in both the development and the ability of infectious agents to infect zebrafish. But still research has shown that embryos, larvae, or adult zebrafish are useful models for studying eye diseases that cause blindness or impairment of vision.
5. Zebrafish Larvae as a Model for Retina Regeneration
The zebrafish ability to regenerate the retina after an injury represents an advantage in studies of retina degeneration associated with inherited retinal dystrophies (IRDs) and traumatic optic neuropathy, as well as glaucoma and diabetic retinopathy, enabling the application of zebrafish larvae on drug-screenings for IRD treatments (reviewed by [122]).
The mature adult zebrafish retina never stops developing and has a remarkable regenerative capacity. All types of retinal cells are constantly generated in the circumferential germinal zone or ciliary marginal zone (CMZ), and rod photoreceptors originating from rod precursor cells of the inner retina are added throughout life. In addition to the essential role in the maintenance of ionic homeostasis, metabolic support of neurons, uptake and recycling of neurotransmitters from synapses, Müller glia cells of the inner nuclear layer are capable of asymmetric division to generate committed progenitors of all types of retinal cells in response to injury [123].
Pioneering work demonstrated that Müller glia expressing α1T, a neuron-specific microtubule protein induced in the developing and regenerating central nervous system (CNS), can de-differentiate and become multipotent in the injured zebrafish retina [124]. Then, Bernardos et al. (2007) found that Müller glia also express the multipotent progenitor marker Pax6 (paired box gene 6), and Müller glia-derived progenitors expressing Crx (cone-rod homeobox) have a low level of proliferation in the uninjured retina, and remain competent to regenerate missing retinal neurons. Photoreceptor degeneration and other retinal cellular damage provoke a disruption in Notch signaling and cell communication, producing a series of chemical cues that interact with Müller glia, and signalize to alter several gene expression patterns and activate the cell, in a process known as gliosis.
Asymmetric, self-renewal divisions of injury-induced Müller glia and N-cadherin-mediated adhesion are required in the regeneration of neurons, as found by Nagashima, Barthel, & Raymond (2013) [125]. Dying neurons release signaling factors such as tumor necrosis factor alpha (TNFα), that up-regulate the Müller glia reprogramming genes ascl1a and stat3 [126]. Likewise, TNFα can also activate microglia, and Munzel, Becker, Becker, & Williams (2014) [127] demonstrated that inflammatory cytokines produced by activated microglia, such as interleukin 6 (IL-6) and IL-11, are related to Müller glia reprogramming.
The pancreatic transcription factor mutant pdx1−/− zebrafish, described to show a diabetic phenotype, exhibits functional deficits including a significant reduction in the b-wave amplitude accompanied by retinal vascular abnormalities and the degeneration of rods and cones [128].
Molecular pathways such as ciliary neurotrophic factor [129], TGF- [130], and fibroblast growth factor (Fgf) [131], as well as the β-catenin/Wnt signaling [132] and the transcription factor Ascl1a [133], are associated with the regeneration of the zebrafish retina.
Using light-induced photoreceptor damage in larval zebrafish, Craig et al. (2010) [134] showed that light-induced photoreceptor death increased secreted β-galactoside binding protein, Galectin 1-like 2 (Drgal1-L2) from microglia and proliferating Müller glia, as well as mitotic progeny. Drgal1-L2 was demonstrated to be involved in rod regeneration, since morpholino knockdown of Drgal1-L2 resulted in reduced regeneration of rods, but not cones.
6. Conclusions
The unique features of the teleost eye include continued retinal growth and plasticity during post-embryonic changes and development. Zebrafish represent a useful model for recapitulation of hereditary genetic ocular abnormalities and diseases of posterior and anterior structures that significantly compromise vision and negatively affect the quality of life.
Despite all the research on neurodegenerative diseases and regeneration using the zebrafish as a model, a complete picture of all molecular factors involved in the pathophysiology of ocular diseases has not yet been achieved. However, utilizing recent advances in genome sequencing that have provided access to the complete zebrafish genome and the ability to edit genes of interest have served to expand our ability to understand, at a mechanistic level, the triggering factors as well as their interrelation with other associated endocrine factors such as metabolic disorders (obesity and diabetes).
Interestingly, different aspects of myopia, the most common human eye disease worldwide with increasing incidence, and ocular surface diseases have been established using the zebrafish model, bugeye/lrp2 mutants [135]. It was demonstrated that lrpap1 deficiency could lead to myopia through TGF-β-induced apoptosis signaling [136].
Nevertheless, eye diseases including dry eye disease and pterygium, as well as injuries and trauma, which can even result in blindness, remain a major challenge in ophthalmological studies, including modeling in zebrafish.
It is expected that, based on experimental experiences with zebrafish, the results achieved will allow future translational research and indicate the direction we should follow to overcome the limitations of using this model organism.
Acknowledgments
We thank the São Paulo Research Foundation (FAPESP) for the support—notably through the Center for Toxins, Immune Response and Cell Signaling (CeTICS).
Author Contributions
Conceptualization, C.L., M.L.-F. and J.G.S.R.; methodology, J.G.S.R.; data curation, C.L., J.G.S.R. and M.L.-F.; writing—original draft preparation, C.L., J.G.S.R. and M.L.-F.; writing—review and editing, C.L. and M.L.-F.; supervision, C.L. and M.L.-F.; project administration, C.L. and M.L.-F.; funding acquisition, C.L. and M.L.-F. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by the São Paulo Research Foundation—FAPESP (#2013/07467-1 and #2021/08891-8) and the National Council for Scientific and Technological Development—CNPq (#305414/2019-4). The funders had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Bibliowicz J., Tittle R.K., Gross J.M. Toward a Better Understanding of Human Eye Disease: Insights from the zebrafish, Danio rerio. Prog. Mol. Biol. Transl. Sci. 2011;100:287–330. doi: 10.1016/B978-0-12-384878-9.00007-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Richardson R., Tracey-White D., Webster A., Moosajee M. The Zebrafish Eye—A Paradigm for Investigating Human Ocular Genetics. Eye. 2017;31:68–86. doi: 10.1038/eye.2016.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cassar S., Adatto I., Freeman J.L., Gamse J.T., Iturria I., Lawrence C., Muriana A., Peterson R.T., Van Cruchten S., Zon L.I. Use of Zebrafish in Drug Discovery Toxicology. Chem. Res. Toxicol. 2020;33:95–118. doi: 10.1021/acs.chemrestox.9b00335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmitt E.A., Dowling J.E. Early Retinal Development in the Zebrafish, Danio rerio: Light and Electron Microscopic Analyses. J. Comp. Neurol. 1999;404:515–536. doi: 10.1002/(SICI)1096-9861(19990222)404:4<515::AID-CNE8>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 5.Zhao X.C., Yee R.W., Norcom E., Burgess H., Avanesov A.S., Barrish J.P., Malicki J. The Zebrafish Cornea: Structure and Development. Investig. Ophthalmol. Vis. Sci. 2006;47:4341. doi: 10.1167/iovs.05-1611. [DOI] [PubMed] [Google Scholar]
- 6.Jaroszynska N., Harding P., Moosajee M. Metabolism in the Zebrafish Retina. J. Dev. Biol. 2021;9:10. doi: 10.3390/jdb9010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Greiling T.M.S., Aose M., Clark J.I. Cell Fate and Differentiation of the Developing Ocular Lens. Investig. Ophthalmol. Vis. Sci. 2010;51:1540. doi: 10.1167/iovs.09-4388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hyoung Kim J., Suk Yu Y., Kim K.-W., Hun Kim J. Investigation of Barrier Characteristics in the Hyaloid-Retinal Vessel of Zebrafish. J. Neurosci. Res. 2011;89:921–928. doi: 10.1002/jnr.22607. [DOI] [PubMed] [Google Scholar]
- 9.Greiling T.M.S., Clark J.I. The Transparent Lens and Cornea in the Mouse and Zebra Fish Eye. Semin. Cell Dev. Biol. 2008;19:94–99. doi: 10.1016/j.semcdb.2007.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang K., Vorontsova I., Hoshino M., Uesugi K., Yagi N., Hall J.E., Schilling T.F., Pierscionek B.K. Optical Development in the Zebrafish Eye Lens. FASEB J. 2020;34:5552–5562. doi: 10.1096/fj.201902607R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bianco I.H., Kampff A.R., Engert F. Prey Capture Behavior Evoked by Simple Visual Stimuli in Larval Zebrafish. Front. Syst. Neurosci. 2011;5:101. doi: 10.3389/fnsys.2011.00101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brysch C., Leyden C., Arrenberg A.B. Functional Architecture Underlying Binocular Coordination of Eye Position and Velocity in the Larval Zebrafish Hindbrain. BMC Biol. 2019;17:110. doi: 10.1186/s12915-019-0720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schoonheim P.J., Arrenberg A.B., Del Bene F., Baier H. Optogenetic Localization and Genetic Perturbation of Saccade-Generating Neurons in Zebrafish. J. Neurosci. 2010;30:7111–7120. doi: 10.1523/JNEUROSCI.5193-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ohnesorge N., Sasore T., Hillary D., Alvarez Y., Carey M., Kennedy B.N. Orthogonal Drug Pooling Enhances Phenotype-Based Discovery of Ocular Antiangiogenic Drugs in Zebrafish Larvae. Front. Pharmacol. 2019;10:508. doi: 10.3389/fphar.2019.00508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hong Y., Luo Y. Zebrafish Model in Ophthalmology to Study Disease Mechanism and Drug Discovery. Pharmaceuticals. 2021;14:716. doi: 10.3390/ph14080716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosa J.G.S., Lima C., Lopes-Ferreira M. Zebrafish Larvae Behavior Models as a Tool for Drug Screenings and Pre-Clinical Trials: A Review. Int. J. Mol. Sci. 2022;23:6647. doi: 10.3390/ijms23126647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ganzen L., Venkatraman P., Pang C., Leung Y., Zhang M. Utilizing Zebrafish Visual Behaviors in Drug Screening for Retinal Degeneration. Int. J. Mol. Sci. 2017;18:1185. doi: 10.3390/ijms18061185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cavodeassi F., Wilson S.W. Looking to the Future of Zebrafish as a Model to Understand the Genetic Basis of Eye Disease. Hum. Genet. 2019;138:993–1000. doi: 10.1007/s00439-019-02055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yin J., Morrissey M.E., Shine L., Kennedy C., Higgins D.G., Kennedy B.N. Genes and Signaling Networks Regulated during Zebrafish Optic Vesicle Morphogenesis. BMC Genom. 2014;15:825. doi: 10.1186/1471-2164-15-825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santos-Ledo A., Cavodeassi F., Carreño H., Aijón J., Arévalo R. Ethanol Alters Gene Expression and Cell Organization during Optic Vesicle Evagination. Neuroscience. 2013;250:493–506. doi: 10.1016/j.neuroscience.2013.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pillai-Kastoori L., Wen W., Wilson S.G., Strachan E., Lo-Castro A., Fichera M., Musumeci S.A., Lehmann O.J., Morris A.C. Sox11 Is Required to Maintain Proper Levels of Hedgehog Signaling during Vertebrate Ocular Morphogenesis. PLoS Genet. 2014;10:e1004491. doi: 10.1371/journal.pgen.1004491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weaver M.L., Piedade W.P., Meshram N.N., Famulski J.K. Hyaloid Vasculature and Mmp2 Activity Play a Role during Optic Fissure Fusion in Zebrafish. Sci. Rep. 2020;10:10136. doi: 10.1038/s41598-020-66451-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chawla B., Swain W., Williams A.L., Bohnsack B.L. Retinoic Acid Maintains Function of Neural Crest–Derived Ocular and Craniofacial Structures in Adult Zebrafish. Investig. Ophthalmol. Vis. Sci. 2018;59:1924. doi: 10.1167/iovs.17-22845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seese S.E., Reis L.M., Deml B., Griffith C., Reich A., Jamieson R.V., Semina E.V. Identification of Missense MAB21L1 Variants in Microphthalmia and Aniridia. Hum. Mutat. 2021;42:877–890. doi: 10.1002/humu.24218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shi X., Bosenko D.V., Zinkevich N.S., Foley S., Hyde D.R., Semina E.V., Vihtelic T.S. Zebrafish Pitx3 Is Necessary for Normal Lens and Retinal Development. Mech. Dev. 2005;122:513–527. doi: 10.1016/j.mod.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 26.Gath N., Gross J.M. Zebrafish Mab21l2 Mutants Possess Severe Defects in Optic Cup Morphogenesis, Lens and Cornea Development. Dev. Dyn. 2019;248:514–529. doi: 10.1002/dvdy.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang Y.-Y., Rinner O., Hedinger P., Liu S.-C., Neuhauss S.C.F. Oculomotor Instabilities in Zebrafish Mutant Belladonna: A Behavioral Model for Congenital Nystagmus Caused by Axonal Misrouting. J. Neurosci. 2006;26:9873–9880. doi: 10.1523/JNEUROSCI.2886-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maurer C.M., Huang Y.-Y., Neuhauss S.C.F. Application of Zebrafish Oculomotor Behavior to Model Human Disorders. Rev. Neurosci. 2011;22:5–16. doi: 10.1515/rns.2011.003. [DOI] [PubMed] [Google Scholar]
- 29.Huber-Reggi S.P., Chen C.-C., Grimm L., Straumann D., Neuhauss S.C.F., Huang M.Y.-Y. Severity of Infantile Nystagmus Syndrome-Like Ocular Motor Phenotype Is Linked to the Extent of the Underlying Optic Nerve Projection Defect in Zebrafish Belladonna Mutant. J. Neurosci. 2012;32:18079–18086. doi: 10.1523/JNEUROSCI.4378-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morris A.C. The Genetics of Ocular Disorders: Insights from the Zebrafish. Birth Defects Res. Part C Embryo Today Rev. 2011;93:215–228. doi: 10.1002/bdrc.20211. [DOI] [PubMed] [Google Scholar]
- 31.Li X.-Q., Cai H.-C., Zhou S.-Y., Yang J.-H., Xi Y.-B., Gao X.-B., Zhao W.-J., Li P., Zhao G.-Y., Tong Y., et al. A Novel Mutation Impairing the Tertiary Structure and Stability of ΓC-Crystallin (CRYGC) Leads to Cataract Formation in Humans and Zebrafish Lens. Hum. Mutat. 2012;33:391–401. doi: 10.1002/humu.21648. [DOI] [PubMed] [Google Scholar]
- 32.Wu S.-Y., Zou P., Mishra S., Mchaourab H.S. Transgenic Zebrafish Models Reveal Distinct Molecular Mechanisms for Cataract-Linked AA-Crystallin Mutants. PLoS ONE. 2018;13:e0207540. doi: 10.1371/journal.pone.0207540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mishra S., Wu S.-Y., Fuller A.W., Wang Z., Rose K.L., Schey K.L., Mchaourab H.S. Loss of AB-Crystallin Function in Zebrafish Reveals Critical Roles in the Development of the Lens and Stress Resistance of the Heart. J. Biol. Chem. 2018;293:740–753. doi: 10.1074/jbc.M117.808634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vorontsova I., Gehring I., Hall J.E., Schilling T.F. Aqp0a Regulates Suture Stability in the Zebrafish Lens. Investig. Ophthalmol. Vis. Sci. 2018;59:2869–2879. doi: 10.1167/iovs.18-24044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang J., Cui W., Du C., Huang Y., Pi X., Guo W., Wang J., Huang W., Chen D., Li J., et al. Knockout of DNase1l1l Abrogates Lens Denucleation Process and Causes Cataract in Zebrafish. Biochim. Biophys. Acta Mol. Basis Dis. 2020;1866:165724. doi: 10.1016/j.bbadis.2020.165724. [DOI] [PubMed] [Google Scholar]
- 36.Swartz M.E., Wells M.B., Griffin M., McCarthy N., Lovely C.B., McGurk P., Rozacky J., Eberhart J.K. A Screen of Zebrafish Mutants Identifies Ethanol-Sensitive Genetic Loci. Alcohol. Clin. Exp. Res. 2014;38:694–703. doi: 10.1111/acer.12286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ouyang J., Li S., Sun W., Xiao X., Wang Y., Jiang Y., Zhang Q. Variants in HNRNPH1 Are Associated with High Myopia in Humans and Ocular Coloboma in Zebrafish. Clin. Genet. 2022;102:424–433. doi: 10.1111/cge.14213. [DOI] [PubMed] [Google Scholar]
- 38.Reis L.M., Sorokina E.A., Thompson S., Muheisen S., Velinov M., Zamora C., Aylsworth A.S., Semina E.V. De Novo Missense Variants in WDR37 Cause a Severe Multisystemic Syndrome. Am. J. Hum. Genet. 2019;105:425–433. doi: 10.1016/j.ajhg.2019.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.French C.R. Mechanistic Insights into Axenfeld–Rieger Syndrome from Zebrafish Foxc1 and Pitx2 Mutants. Int. J. Mol. Sci. 2021;22:10001. doi: 10.3390/ijms221810001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Casey J., Kawaguchi R., Morrissey M., Sun H., McGettigan P., Nielsen J.E., Conroy J., Regan R., Kenny E., Cormican P., et al. First Implication of STRA6 Mutations in Isolated Anophthalmia, Microphthalmia, and Coloboma: A New Dimension to the STRA6 Phenotype. Hum. Mutat. 2011;32:1417–1426. doi: 10.1002/humu.21590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oliver V.F., van Bysterveldt K.A., Cadzow M., Steger B., Romano V., Markie D., Hewitt A.W., Mackey D.A., Willoughby C.E., Sherwin T., et al. A COL17A1 Splice-Altering Mutation Is Prevalent in Inherited Recurrent Corneal Erosions. Ophthalmology. 2016;123:709–722. doi: 10.1016/j.ophtha.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 42.Schlegel D.K., Ramkumar S., von Lintig J., Neuhauss S.C. Disturbed Retinoid Metabolism upon Loss of Rlbp1a Impairs Cone Function and Leads to Subretinal Lipid Deposits and Photoreceptor Degeneration in the Zebrafish Retina. eLife. 2021;10:e71473. doi: 10.7554/eLife.71473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nadolski N.J., Balay S.D., Wong C.X.L., Waskiewicz A.J., Hocking J.C. Abnormal Cone and Rod Photoreceptor Morphogenesis in Gdf6a Mutant Zebrafish. Investig. Ophthalmol. Vis. Sci. 2020;61:9. doi: 10.1167/iovs.61.4.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jia S., Muto A., Orisme W., Henson H.E., Parupalli C., Ju B., Baier H., Taylor M.R. Zebrafish Cacna1fa Is Required for Cone Photoreceptor Function and Synaptic Ribbon Formation. Hum. Mol. Genet. 2014;23:2981–2994. doi: 10.1093/hmg/ddu009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bahadori R., Biehlmaier O., Zeitz C., Labhart T., Makhankov Y.V., Forster U., Gesemann M., Berger W., Neuhauss S.C.F. Nyctalopin Is Essential for Synaptic Transmission in the Cone Dominated Zebrafish Retina. Eur. J. Neurosci. 2006;24:1664–1674. doi: 10.1111/j.1460-9568.2006.05053.x. [DOI] [PubMed] [Google Scholar]
- 46.Bahadori R., Rinner O., Schonthaler H.B., Biehlmaier O., Makhankov Y.V., Rao P., Jagadeeswaran P., Neuhauss S.C.F. The Zebrafish Fade out Mutant: A Novel Genetic Model for Hermansky–Pudlak Syndrome. Investig. Ophthalmol. Vis. Sci. 2006;47:4523. doi: 10.1167/iovs.05-1596. [DOI] [PubMed] [Google Scholar]
- 47.Minegishi Y., Nakaya N., Tomarev S.I. Mutation in the Zebrafish Cct2 Gene Leads to Abnormalities of Cell Cycle and Cell Death in the Retina: A Model of CCT2-Related Leber Congenital Amaurosis. Investig. Ophthalmol. Vis. Sci. 2018;59:995–1004. doi: 10.1167/iovs.17-22919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stiebel-Kalish H., Reich E., Rainy N., Vatine G., Nisgav Y., Tovar A., Gothilf Y., Bach M. Gucy2f Zebrafish Knockdown--a Model for Gucy2d-Related Leber Congenital Amaurosis. Eur. J. Hum. Genet. 2012;20:884–889. doi: 10.1038/ejhg.2012.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Noel N.C.L., Nadolski N.J., Hocking J.C., MacDonald I.M., Allison W.T. Progressive Photoreceptor Dysfunction and Age-Related Macular Degeneration-Like Features in Rp1l1 Mutant Zebrafish. Cells. 2020;9:2214. doi: 10.3390/cells9102214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rastoin O., Pagès G., Dufies M. Experimental Models in Neovascular Age Related Macular Degeneration. Int. J. Mol. Sci. 2020;21:4627. doi: 10.3390/ijms21134627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xia H., Zhang Q., Shen Y., Bai Y., Ma X., Zhang B., Qi Y., Zhang J., Hu Q., Du W., et al. Ube3d, a New Gene Associated with Age-Related Macular Degeneration, Induces Functional Changes in Both In Vivo and In Vitro Studies. Mol. Ther. Nucleic Acids. 2020;20:217–230. doi: 10.1016/j.omtn.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cheng K.-C., Hsu Y.-T., Liu W., Huang H.-L., Chen L.-Y., He C.-X., Sheu S.-J., Chen K.-J., Lee P.-Y., Lin Y.-H., et al. The Role of Oxidative Stress and Autophagy in Blue-Light-Induced Damage to the Retinal Pigment Epithelium in Zebrafish In Vitro and In Vivo. Int. J. Mol. Sci. 2021;22:1338. doi: 10.3390/ijms22031338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Noel N.C.L., Allison W.T., MacDonald I.M., Hocking J.C. Zebrafish and Inherited Photoreceptor Disease: Models and Insights. Prog. Retin. Eye Res. 2022;91:101096. doi: 10.1016/j.preteyeres.2022.101096. [DOI] [PubMed] [Google Scholar]
- 54.Jung S.-H., Kim Y.S., Lee Y.-R., Kim J.S. High Glucose-Induced Changes in Hyaloid-Retinal Vessels during Early Ocular Development of Zebrafish: A Short-Term Animal Model of Diabetic Retinopathy. Br. J. Pharmacol. 2016;173:15–26. doi: 10.1111/bph.13279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lee Y., Yang J. Development of a Zebrafish Screening Model for Diabetic Retinopathy Induced by Hyperglycemia: Reproducibility Verification in Animal Model. Biomed. Pharmacother. 2021;135:111201. doi: 10.1016/j.biopha.2020.111201. [DOI] [PubMed] [Google Scholar]
- 56.Singh A., Castillo H.A., Brown J., Kaslin J., Dwyer K.M., Gibert Y. High Glucose Levels Affect Retinal Patterning during Zebrafish Embryogenesis. Sci. Rep. 2019;9:4121. doi: 10.1038/s41598-019-41009-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Reichenbach A., Wurm A., Pannicke T., Iandiev I., Wiedemann P., Bringmann A. Müller Cells as Players in Retinal Degeneration and Edema. Graefe’s Arch. Clin. Exp. Ophthalmol. 2007;245:627–636. doi: 10.1007/s00417-006-0516-y. [DOI] [PubMed] [Google Scholar]
- 58.Li Y., Zhao Y., Sang S., Leung T. Methylglyoxal-Induced Retinal Angiogenesis in Zebrafish Embryo: A Potential Animal Model of Neovascular Retinopathy. J. Ophthalmol. 2019;2019:1–8. doi: 10.1155/2019/2746735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Skarie J.M., Link B.A. FoxC1 Is Essential for Vascular Basement Membrane Integrity and Hyaloid Vessel Morphogenesis. Investig. Ophthalmol. Vis. Sci. 2009;50:5026. doi: 10.1167/iovs.09-3447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Iglesias A.I., Springelkamp H., van der Linde H., Severijnen L.-A., Amin N., Oostra B., Kockx C.E.M., van den Hout M.C.G.N., van IJcken W.F.J., Hofman A., et al. Exome Sequencing and Functional Analyses Suggest That SIX6 Is a Gene Involved in an Altered Proliferation–Differentiation Balance Early in Life and Optic Nerve Degeneration at Old Age. Hum. Mol. Genet. 2014;23:1320–1332. doi: 10.1093/hmg/ddt522. [DOI] [PubMed] [Google Scholar]
- 61.Williams A.L., Eason J., Chawla B., Bohnsack B.L. Cyp1b1 Regulates Ocular Fissure Closure Through a Retinoic Acid–Independent Pathway. Investig. Ophthalmol. Vis. Sci. 2017;58:1084. doi: 10.1167/iovs.16-20235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Giannaccini M., Usai A., Chiellini F., Guadagni V., Andreazzoli M., Ori M., Pasqualetti M., Dente L., Raffa V. Neurotrophin-Conjugated Nanoparticles Prevent Retina Damage Induced by Oxidative Stress. Cell. Mol. Life Sci. 2018;75:1255–1267. doi: 10.1007/s00018-017-2691-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Morales-Cámara S., Alexandre-Moreno S., Bonet-Fernández J.-M., Atienzar-Aroca R., Aroca-Aguilar J.-D., Ferre-Fernández J.-J., Méndez C.-D., Morales L., Fernández-Sánchez L., Cuenca N., et al. Role of GUCA1C in Primary Congenital Glaucoma and in the Retina: Functional Evaluation in Zebrafish. Genes. 2020;11:550. doi: 10.3390/genes11050550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zelinka C.P., Sotolongo-Lopez M., Fadool J.M. Targeted Disruption of the Endogenous Zebrafish Rhodopsin Locus as Models of Rapid Rod Photoreceptor Degeneration. Mol. Vis. 2018;24:587–602. [PMC free article] [PubMed] [Google Scholar]
- 65.Ganzen L., Ko M.J., Zhang M., Xie R., Chen Y., Zhang L., James R., Mumm J., van Rijn R.M., Zhong W., et al. Drug Screening with Zebrafish Visual Behavior Identifies Carvedilol as a Potential Treatment for an Autosomal Dominant Form of Retinitis Pigmentosa. Sci. Rep. 2021;11:11432. doi: 10.1038/s41598-021-89482-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Santhanam A., Shihabeddin E., Atkinson J.A., Nguyen D., Lin Y.-P., O’Brien J. A Zebrafish Model of Retinitis Pigmentosa Shows Continuous Degeneration and Regeneration of Rod Photoreceptors. Cells. 2020;9:2242. doi: 10.3390/cells9102242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Campochiaro P.A., Mir T.A. The Mechanism of Cone Cell Death in Retinitis Pigmentosa. Prog. Retin. Eye Res. 2018;62:24–37. doi: 10.1016/j.preteyeres.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 68.Crouzier L., Diez C., Richard E.M., Cubedo N., Barbereau C., Rossel M., Delaunay T., Maurice T., Delprat B. Loss of Pde6a Induces Rod Outer Segment Shrinkage and Visual Alterations in Pde6aQ70X Mutant Zebrafish, a Relevant Model of Retinal Dystrophy. Front. Cell Dev. Biol. 2021;9:675517. doi: 10.3389/fcell.2021.675517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kawase R., Nishimura Y., Ashikawa Y., Sasagawa S., Murakami S., Yuge M., Okabe S., Kawaguchi K., Yamamoto H., Moriyuki K., et al. EP300 Protects from Light-Induced Retinopathy in Zebrafish. Front. Pharmacol. 2016;7:126. doi: 10.3389/fphar.2016.00126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lu Z., Hu X., Reilly J., Jia D., Liu F., Yu S., Liu X., Xie S., Qu Z., Qin Y., et al. Deletion of the Transmembrane Protein Prom1b in Zebrafish Disrupts Outer-Segment Morphogenesis and Causes Photoreceptor Degeneration. J. Biol. Chem. 2019;294:13953–13963. doi: 10.1074/jbc.RA119.008618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang L., Chen C., Fu J., Lilley B., Berlinicke C., Hansen B., Ding D., Wang G., Wang T., Shou D., et al. Large-Scale Phenotypic Drug Screen Identifies Neuroprotectants in Zebrafish and Mouse Models of Retinitis Pigmentosa. eLife. 2021;10:e57245. doi: 10.7554/eLife.57245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kennedy B.N., Alvarez Y., Brockerhoff S.E., Stearns G.W., Sapetto-Rebow B., Taylor M.R., Hurley J.B. Identification of a Zebrafish Cone Photoreceptor–Specific Promoter and Genetic Rescue of Achromatopsia in the Nof Mutant. Investig. Ophthalmol. Vis. Sci. 2007;48:522. doi: 10.1167/iovs.06-0975. [DOI] [PubMed] [Google Scholar]
- 73.Stearns G., Evangelista M., Fadool J.M., Brockerhoff S.E. A Mutation in the Cone-Specific Pde6 Gene Causes Rapid Cone Photoreceptor Degeneration in Zebrafish. J. Neurosci. 2007;27:13866–13874. doi: 10.1523/JNEUROSCI.3136-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Viringipurampeer I.A., Shan X., Gregory-Evans K., Zhang J.P., Mohammadi Z., Gregory-Evans C.Y. Rip3 Knockdown Rescues Photoreceptor Cell Death in Blind Pde6c Zebrafish. Cell Death Differ. 2014;21:665–675. doi: 10.1038/cdd.2013.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Huang D., Wang M., Yin W., Ma Y., Wang H., Xue T., Ren D., Hu B. Zebrafish Lacking Circadian Gene Per2 Exhibit Visual Function Deficiency. Front. Behav. Neurosci. 2018;12:53. doi: 10.3389/fnbeh.2018.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Iribarne M., Nishiwaki Y., Nakamura S., Araragi M., Oguri E., Masai I. Aipl1 Is Required for Cone Photoreceptor Function and Survival through the Stability of Pde6c and Gc3 in Zebrafish. Sci. Rep. 2017;7:45962. doi: 10.1038/srep45962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Daly C., Shine L., Heffernan T., Deeti S., Reynolds A.L., O’Connor J.J., Dillon E.T., Duffy D.J., Kolch W., Cagney G., et al. A Brain-Derived Neurotrophic Factor Mimetic Is Sufficient to Restore Cone Photoreceptor Visual Function in an Inherited Blindness Model. Sci. Rep. 2017;7:11320. doi: 10.1038/s41598-017-11513-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Schlegel D.K., Glasauer S.M.K., Mateos J.M., Barmettler G., Ziegler U., Neuhauss S.C.F. A New Zebrafish Model for CACNA2D4-Dysfunction. Investig. Ophthalmol. Vis. Sci. 2019;60:5124. doi: 10.1167/iovs.19-26759. [DOI] [PubMed] [Google Scholar]
- 79.Castro-Sánchez S., Suarez-Bregua P., Novas R., Álvarez-Satta M., Badano J.L., Rotllant J., Valverde D. Functional Analysis of New Human Bardet-Biedl Syndrome Loci Specific Variants in the Zebrafish Model. Sci. Rep. 2019;9:12936. doi: 10.1038/s41598-019-49217-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Song P., Fogerty J., Cianciolo L.T., Stupay R., Perkins B.D. Cone Photoreceptor Degeneration and Neuroinflammation in the Zebrafish Bardet-Biedl Syndrome 2 (Bbs2) Mutant Does Not Lead to Retinal Regeneration. Front. Cell Dev. Biol. 2020;8:578528. doi: 10.3389/fcell.2020.578528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gopal S.R., Chen D.H.-C., Chou S.-W., Zang J., Neuhauss S.C.F., Stepanyan R., McDermott B.M., Alagramam K.N. Zebrafish Models for the Mechanosensory Hair Cell Dysfunction in Usher Syndrome 3 Reveal That Clarin-1 Is an Essential Hair Bundle Protein. J. Neurosci. 2015;35:10188–10201. doi: 10.1523/JNEUROSCI.1096-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Miles A., Blair C., Emili A., Tropepe V. Usher Syndrome Type 1-Associated Gene, Pcdh15b, Is Required for Photoreceptor Structural Integrity in Zebrafish. Dis. Model. Mech. 2021;14:48965. doi: 10.1242/dmm.048965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Song P., Perkins B.D. Developmental Expression of the Zebrafish Arf-like Small GTPase Paralogs Arl13a and Arl13b. Gene Expr. Patterns. 2018;29:82–87. doi: 10.1016/j.gep.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Liu Y., Cao S., Yu M., Hu H. TMEM216 Deletion Causes Mislocalization of Cone Opsin and Rhodopsin and Photoreceptor Degeneration in Zebrafish. Investig. Ophthalmol. Vis. Sci. 2020;61:24. doi: 10.1167/iovs.61.8.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rusterholz T.D.S., Hofmann C., Bachmann-Gagescu R. Insights Gained From Zebrafish Models for the Ciliopathy Joubert Syndrome. Front. Genet. 2022;13:939527. doi: 10.3389/fgene.2022.939527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lessieur E.M., Song P., Nivar G.C., Piccillo E.M., Fogerty J., Rozic R., Perkins B.D. Ciliary Genes Arl13b, Ahi1 and Cc2d2a Differentially Modify Expression of Visual Acuity Phenotypes but Do Not Enhance Retinal Degeneration Due to Mutation of Cep290 in Zebrafish. PLoS ONE. 2019;14:e0213960. doi: 10.1371/journal.pone.0213960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Burton M.J., Ramke J., Marques A.P., Bourne R.R.A., Congdon N., Jones I., Ah Tong B.A.M., Arunga S., Bachani D., Bascaran C., et al. The Lancet Global Health Commission on Global Eye Health: Vision beyond 2020. Lancet Glob. Health. 2021;9:e489–e551. doi: 10.1016/S2214-109X(20)30488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.WHO . World Health Organization Blindness and Vision Impairment. WHO; Geneva, Switzerland: 2022. [Google Scholar]
- 89.Cvekl A., Piatigorsky J. Lens Development and Crystallin Gene Expression: Many Roles for Pax-6. BioEssays. 1996;18:621–630. doi: 10.1002/bies.950180805. [DOI] [PubMed] [Google Scholar]
- 90.Bloemendal H., de Jong W., Jaenicke R., Lubsen N.H., Slingsby C., Tardieu A. Ageing and Vision: Structure, Stability and Function of Lens Crystallins. Prog. Biophys. Mol. Biol. 2004;86:407–485. doi: 10.1016/j.pbiomolbio.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 91.Andley U.P. Crystallins in the Eye: Function and Pathology. Prog. Retin. Eye Res. 2007;26:78–98. doi: 10.1016/j.preteyeres.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 92.Goishi K., Shimizu A., Najarro G., Watanabe S., Rogers R., Zon L.I., Klagsbrun M. AA-Crystallin Expression Prevents γ-Crystallin Insolubility and Cataract Formation in the Zebrafish Cloche Mutant Lens. Development. 2006;133:2585–2593. doi: 10.1242/dev.02424. [DOI] [PubMed] [Google Scholar]
- 93.Prior H.M., Letwin K., Tuininga A., Nguyen M. A Simple Method of Cataract Induction in Adult Zebrafish. Zebrafish. 2018;15:211–212. doi: 10.1089/zeb.2017.1533. [DOI] [PubMed] [Google Scholar]
- 94.Zhang M., Luo J., Chen X., Chen Y., Li P., Zhang G., Guan H., Lu P. Identification and Integrated Analysis of the MiRNA-MRNA Regulatory Network in Lens from an H2O2-Induced Zebrafish Cataract Model. Curr. Eye Res. 2022;47:854–865. doi: 10.1080/02713683.2022.2050263. [DOI] [PubMed] [Google Scholar]
- 95.Morishita H., Eguchi T., Tsukamoto S., Sakamaki Y., Takahashi S., Saito C., Koyama-Honda I., Mizushima N. Organelle Degradation in the Lens by PLAAT Phospholipases. Nature. 2021;592:634–638. doi: 10.1038/s41586-021-03439-w. [DOI] [PubMed] [Google Scholar]
- 96.Shao M., Lu T., Zhang C., Zhang Y.-Z., Kong S.-H., Shi D.-L. Rbm24 Controls Poly(A) Tail Length and Translation Efficiency of Crystallin MRNAs in the Lens via Cytoplasmic Polyadenylation. Proc. Natl. Acad. Sci. USA. 2020;117:7245–7254. doi: 10.1073/pnas.1917922117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lu A., Duan P., Xie J., Gao H., Chen M., Gong Y., Li J., Xu H. Recent Progress and Research Trend of Anti-Cataract Pharmacology Therapy: A Bibliometric Analysis and Literature Review. Eur. J. Pharmacol. 2022;934:175299. doi: 10.1016/j.ejphar.2022.175299. [DOI] [PubMed] [Google Scholar]
- 98.Ping X., Liang J., Shi K., Bao J., Wu J., Yu X., Tang X., Zou J., Shentu X. Rapamycin Relieves the Cataract Caused by Ablation of Gja8b through Stimulating Autophagy in Zebrafish. Autophagy. 2021;17:3323–3337. doi: 10.1080/15548627.2021.1872188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chang P.Y., Bjornstad K.A., Rosen C.J., Lin S., Blakely E.A. Particle Radiation Alters Expression of Matrix Metalloproteases Resulting in ECM Remodeling in Human Lens Cells. Radiat. Environ. Biophys. 2007;46:187–194. doi: 10.1007/s00411-006-0087-7. [DOI] [PubMed] [Google Scholar]
- 100.Hilliard A., Mendonca P., Russell T.D., Soliman K.F.A. The Protective Effects of Flavonoids in Cataract Formation through the Activation of Nrf2 and the Inhibition of MMP-9. Nutrients. 2020;12:3651. doi: 10.3390/nu12123651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shinozaki Y., Saito K., Kashiwagi K., Koizumi S. Ocular P2 Receptors and Glaucoma. Neuropharmacology. 2023;222:109302. doi: 10.1016/j.neuropharm.2022.109302. [DOI] [PubMed] [Google Scholar]
- 102.Gross J.M., Perkins B.D. Zebrafish Mutants as Models for Congenital Ocular Disorders in Humans. Mol. Reprod. Dev. 2008;75:547–555. doi: 10.1002/mrd.20831. [DOI] [PubMed] [Google Scholar]
- 103.Ogawa Y., Shiraki T., Asano Y., Muto A., Kawakami K., Suzuki Y., Kojima D., Fukada Y. Six6 and Six7 Coordinately Regulate Expression of Middle-Wavelength Opsins in Zebrafish. Proc. Natl. Acad. Sci. USA. 2019;116:4651–4660. doi: 10.1073/pnas.1812884116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ashikawa Y., Nishimura Y., Okabe S., Sato Y., Yuge M., Tada T., Miyao H., Murakami S., Kawaguchi K., Sasagawa S., et al. Potential Protective Function of the Sterol Regulatory Element Binding Factor 1–Fatty Acid Desaturase 1/2 Axis in Early-Stage Age-Related Macular Degeneration. Heliyon. 2017;3:e00266. doi: 10.1016/j.heliyon.2017.e00266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.van Rooijen E., Voest E.E., Logister I., Korving J., Schwerte T., Schulte-Merker S., Giles R.H., van Eeden F.J. Zebrafish Mutants in the von Hippel-Lindau Tumor Suppressor Display a Hypoxic Response and Recapitulate Key Aspects of Chuvash Polycythemia. Blood. 2009;113:6449–6460. doi: 10.1182/blood-2008-07-167890. [DOI] [PubMed] [Google Scholar]
- 106.Lu F., Leach L.L., Gross J.M. MTOR Activity Is Essential for Retinal Pigment Epithelium Regeneration in Zebrafish. PLoS Genet. 2022;18:e1009628. doi: 10.1371/journal.pgen.1009628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sachdeva M.M. Retinal Neurodegeneration in Diabetes: An Emerging Concept in Diabetic Retinopathy. Curr. Diabetes Rep. 2021;21:65. doi: 10.1007/s11892-021-01428-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Thomas R.L., Halim S., Gurudas S., Sivaprasad S., Owens D.R. IDF Diabetes Atlas: A Review of Studies Utilising Retinal Photography on the Global Prevalence of Diabetes Related Retinopathy between 2015 and 2018. Diabetes Res. Clin. Pract. 2019;157:107840. doi: 10.1016/j.diabres.2019.107840. [DOI] [PubMed] [Google Scholar]
- 109.Fosmark D.S., Torjesen P.A., Kilhovd B.K., Berg T.J., Sandvik L., Hanssen K.F., Agardh C.-D., Agardh E. Increased Serum Levels of the Specific Advanced Glycation End Product Methylglyoxal-Derived Hydroimidazolone Are Associated with Retinopathy in Patients with Type 2 Diabetes Mellitus. Metabolism. 2006;55:232–236. doi: 10.1016/j.metabol.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 110.Corazza P., Cirafici P., Testa V., Orlans H.O., Berisso M., Traverso C.E., Vagge A., Nicolò M. Vascular Density and Retinal Function in Patients with Retinitis Pigmentosa Evaluated by Swept-Source OCT Angiography and Microperimetry. Ophthalmologica. 2021;244:27–33. doi: 10.1159/000507961. [DOI] [PubMed] [Google Scholar]
- 111.Cuenca N., Fernández-Sánchez L., Campello L., Maneu V., De la Villa P., Lax P., Pinilla I. Cellular Responses Following Retinal Injuries and Therapeutic Approaches for Neurodegenerative Diseases. Prog. Retin. Eye Res. 2014;43:17–75. doi: 10.1016/j.preteyeres.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 112.García Bohórquez B., Aller E., Rodríguez Muñoz A., Jaijo T., García García G., Millán J.M. Updating the Genetic Landscape of Inherited Retinal Dystrophies. Front. Cell Dev. Biol. 2021;9:645600. doi: 10.3389/fcell.2021.645600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Swenor B.K., Ehrlich J.R. Ageing and Vision Loss: Looking to the Future. Lancet Glob. Health. 2021;9:e385–e386. doi: 10.1016/S2214-109X(21)00031-0. [DOI] [PubMed] [Google Scholar]
- 114.Ventura C.V., Ventura Filho M.C., Ventura L.O. Ocular Manifestations and Visual Outcome in Children With Congenital Zika Syndrome. Top. Magn. Reson. Imaging. 2019;28:23–27. doi: 10.1097/RMR.0000000000000192. [DOI] [PubMed] [Google Scholar]
- 115.Maleski A.L.A., Rosa J.G.S., Bernardo J.T.G., Astray R.M., Walker C.I.B., Lopes-Ferreira M., Lima C. Recapitulation of Retinal Damage in Zebrafish Larvae Infected with Zika Virus. Cells. 2022;11:1457. doi: 10.3390/cells11091457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sanders J.L., Zhou Y., Moulton H.M., Moulton Z.X., McLeod R., Dubey J.P., Weiss L.M., Kent M.L. The Zebrafish, Danio rerio, as a Model for Toxoplasma Gondii: An Initial Description of Infection in Fish. J. Fish Dis. 2015;38:675–679. doi: 10.1111/jfd.12393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Takaki K., Ramakrishnan L., Basu S. A Zebrafish Model for Ocular Tuberculosis. PLoS ONE. 2018;13:e0194982. doi: 10.1371/journal.pone.0194982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Li Y., Hu B. Establishment of Multi-Site Infection Model in Zebrafish Larvae for Studying Staphylococcus Aureus Infectious Disease. J. Genet. Genom. 2012;39:521–534. doi: 10.1016/j.jgg.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 119.Fehr A.G.J., Ruetten M., Seth-Smith H.M.B., Nufer L., Voegtlin A., Lehner A., Greub G., Crosier P.S., Neuhauss S.C.F., Vaughan L. A Zebrafish Model for Chlamydia Infection with the Obligate Intracellular Pathogen Waddlia Chondrophila. Front. Microbiol. 2016;7:1829. doi: 10.3389/fmicb.2016.01829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hotterbeekx A., Raimon S., Abd-Elfarag G., Carter J.Y., Sebit W., Suliman A., Siewe Fodjo J.N., De Witte P., Logora M.Y., Colebunders R., et al. Onchocerca Volvulus Is Not Detected in the Cerebrospinal Fluid of Persons with Onchocerciasis-Associated Epilepsy. Int. J. Infect. Dis. 2020;91:119–123. doi: 10.1016/j.ijid.2019.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Burgos J.S., Ripoll-Gomez J., Alfaro J.M., Sastre I., Valdivieso F. Zebrafish as a New Model for Herpes Simplex Virus Type 1 Infection. Zebrafish. 2008;5:323–333. doi: 10.1089/zeb.2008.0552. [DOI] [PubMed] [Google Scholar]
- 122.Stella S.L., Geathers J.S., Weber S.R., Grillo M.A., Barber A.J., Sundstrom J.M., Grillo S.L. Neurodegeneration, Neuroprotection and Regeneration in the Zebrafish Retina. Cells. 2021;10:633. doi: 10.3390/cells10030633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lahne M., Nagashima M., Hyde D.R., Hitchcock P.F. Reprogramming Müller Glia to Regenerate Retinal Neurons. Annu. Rev. Vis. Sci. 2020;6:171–193. doi: 10.1146/annurev-vision-121219-081808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fausett B.V., Goldman D. A Role for 1 Tubulin-Expressing Muller Glia in Regeneration of the Injured Zebrafish Retina. J. Neurosci. 2006;26:6303–6313. doi: 10.1523/JNEUROSCI.0332-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Nagashima M., Barthel L.K., Raymond P.A. A Self-Renewing Division of Zebrafish Müller Glial Cells Generates Neuronal Progenitors That Require N-Cadherin to Regenerate Retinal Neurons. Development. 2013;140:4510–4521. doi: 10.1242/dev.090738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mitchell D.M., Lovel A.G., Stenkamp D.L. Dynamic Changes in Microglial and Macrophage Characteristics during Degeneration and Regeneration of the Zebrafish Retina. J. Neuroinflamm. 2018;15:163. doi: 10.1186/s12974-018-1185-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Münzel E.J., Becker C.G., Becker T., Williams A. Zebrafish Regenerate Full Thickness Optic Nerve Myelin after Demyelination, but This Fails with Increasing Age. Acta Neuropathol. Commun. 2014;2:77. doi: 10.1186/s40478-014-0077-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ali Z., Zang J., Lagali N., Schmitner N., Salvenmoser W., Mukwaya A., Neuhauss S.C.F., Jensen L.D., Kimmel R.A. Photoreceptor Degeneration Accompanies Vascular Changes in a Zebrafish Model of Diabetic Retinopathy. Investig. Ophthalmol. Vis. Sci. 2020;61:43. doi: 10.1167/iovs.61.2.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kassen S.C., Thummel R., Campochiaro L.A., Harding M.J., Bennett N.A., Hyde D.R. CNTF Induces Photoreceptor Neuroprotection and Müller Glial Cell Proliferation through Two Different Signaling Pathways in the Adult Zebrafish Retina. Exp. Eye Res. 2009;88:1051–1064. doi: 10.1016/j.exer.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 130.Lenkowski J.R., Qin Z., Sifuentes C.J., Thummel R., Soto C.M., Moens C.B., Raymond P.A. Retinal Regeneration in Adult Zebrafish Requires Regulation of TGFβ Signaling. Glia. 2013;61:1687–1697. doi: 10.1002/glia.22549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Qin Z., Kidd A.R., Thomas J.L., Poss K.D., Hyde D.R., Raymond P.A., Thummel R. FGF Signaling Regulates Rod Photoreceptor Cell Maintenance and Regeneration in Zebrafish. Exp. Eye Res. 2011;93:726–734. doi: 10.1016/j.exer.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Meyers J.R., Hu L., Moses A., Kaboli K., Papandrea A., Raymond P.A. β-Catenin/Wnt Signaling Controls Progenitor Fate in the Developing and Regenerating Zebrafish Retina. Neural Dev. 2012;7:30. doi: 10.1186/1749-8104-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tsuruma K., Saito Y., Okuyoshi H., Yamaguchi A., Shimazawa M., Goldman D., Hara H. Granulin 1 Promotes Retinal Regeneration in Zebrafish. Investig. Ophthalmol. Vis. Sci. 2018;59:6057. doi: 10.1167/iovs.18-24828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Craig S.E.L., Thummel R., Ahmed H., Vasta G.R., Hyde D.R., Hitchcock P.F. The Zebrafish Galectin Drgal1-L2 Is Expressed by Proliferating Müller Glia and Photoreceptor Progenitors and Regulates the Regeneration of Rod Photoreceptors. Investig. Ophthalmol. Vis. Sci. 2010;51:3244. doi: 10.1167/iovs.09-4879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Veth K.N., Willer J.R., Collery R.F., Gray M.P., Willer G.B., Wagner D.S., Mullins M.C., Udvadia A.J., Smith R.S., John S.W.M., et al. Mutations in Zebrafish Lrp2 Result in Adult-Onset Ocular Pathogenesis That Models Myopia and Other Risk Factors for Glaucoma. PLoS Genet. 2011;7:e1001310. doi: 10.1371/journal.pgen.1001310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Liu S., Chen T., Chen B., Liu Y., Lu X., Li J. Lrpap1 Deficiency Leads to Myopia through TGF-β-Induced Apoptosis in Zebrafish. Cell Commun. Signal. 2022;20:162. doi: 10.1186/s12964-022-00970-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.