Abstract
Background Orbital blowout fractures are peculiar injuries causing disruption of both ocular function and symmetry. We present our experience with the use of a precontoured titanium mesh in orbital blowout fractures.
Methods A retrospective study of patients undergoing correction of orbital blowout fractures with a precontoured titanium mesh was done at a tertiary care center in Mumbai. Data regarding demographics and pre- and postoperative clinical and radiological attributes were retrieved and compared.
Results A total of 21 patients (19 males and 2 females) underwent correction of blowout fractures with a precontoured titanium mesh. The follow-up period ranged from 6 to 10 months. Road traffic accident (76%) was the most common etiology. Twenty (95%) patients had impure blowout fractures and 1 (5%) patient had a pure blowout. The orbital floor was most commonly fractured (16 [76%]). Associated fractures of the zygomaticomaxillary complex were found in 71% of patients. All patients were operated on within 3 weeks of trauma. A comparison of the operated and uninjured sides on coronal views of computed tomography (CT) scan in nine patients by Photopea application revealed a correction of the increased cross-sectional area in all cases. Enophthalmos was completely corrected in 94% patients, while 92% patients had complete correction of diplopia. One patient with a comminuted zygomatic fracture had persistent diplopia and mild enophthalmos. Infraorbital paresthesia persisted in 58% patients at 6 months of follow-up. No significant postoperative complications were noted.
Conclusion The precontoured titanium mesh restores orbital wall anatomy and is safe, quick, fairly easy, and reproducible with a shorter learning curve. With proper patient selection and execution, prefabricated titanium mesh can serve as an excellent reconstructive option in blowout fractures of the orbit.
Key-Words: blowout fracture, titanium mesh, precontoured titanium mesh, enophthalmos, orbital floor
Introduction
Fractures of the bony orbit are fairly common, constituting 4 to 16% of facial fractures alone and 30 to 55% in combination with other maxillofacial fractures. 1
Although fractures of the orbit with resultant enophthalmos were described as early as 1889 by Lang, the term “blowout”—alluding to the safety valve mechanism of the injury—was first used by Smith and Regan. 2 3 4 They are further categorized as pure and impure.
The bony orbits house and protect the eyeballs and related soft-tissue structures. Naturally, the sequalae of blowout fractures relate to these structures and include diplopia, enophthalmos, infraorbital paresthesia, and visual disturbances. It is well established that the only way to correct early enophthalmos and avoid late deformity is by early surgical correction of the increased orbital volume by reconstructing the defects in the orbital walls. 5 There is still no consensus regarding the ideal biomaterial for such reconstruction—both autologous and alloplastic materials have been used. We present our experience with the use of a precontoured titanium mesh for orbital reconstruction in blowout fractures.
Materials and Methods
This is a retrospective study of orbital blowout fractures undergoing reconstruction with a precontoured titanium mesh between June 2017 and June 2021 at a tertiary health care center in Mumbai. The records of all patients presenting with blowout fractures in this period were retrieved.
Inclusion Criteria
The including criteria are the following:
Age > 18 years.
Surgical correction with a precontoured titanium mesh.
Follow-up of at least 6 months.
Patients with bilateral blowout fractures and posttraumatic blurring/vision loss were excluded.
Indications for Surgical Intervention
Enophthalmos.
Diplopia and restricted extraocular movements with positive forced duction test.
Computed tomography (CT) findings: muscle incarceration and orbital floor defect >50%. 6
For all patients fulfilling the inclusion criteria, the following data were collected: demographics, details of trauma, symptoms at presentation and just before surgery, examination findings including detailed ophthalmological evaluation before and after surgery and at last follow-up, surgical indications, pre- and postoperative CT scan, postoperative complications, and any revision surgeries.
The relevant clinical findings were graded as follows:
Enophthalmos:
Significant = –1.
Minimal = 0.
Absent = 1.
Extraocular movements:
Significant restriction with diplopia or other visual disturbance = –1.
Mild restriction without ocular symptoms = 0.
Normal = 1.
Scar:
Puckered/ectropion/sinuses/hypertrophic = –1.
Well-settled yet visible = 0.
Imperceptible = 1.
Based on the scores, a scoring system was designed to categorize the results ( Table 1 ).
Table 1. Scoring system.
| Scoring criteria | Score | Result | |
|---|---|---|---|
| 1 | Enophthalmos | –1, 0,1 | Excellent score: 3 Good score: 2 Fair score: 0,1 Poor score: –1, –2, –3 |
| 2 | Diplopia/extraocular muscle movement (EOM) | –1, 0, 1 | |
| 3 | Scar | –1, 0, 1 | |
| Total score | –3 to 3 |
For comparison, the coronal images of postoperative CT scans were imported into Photopea R photo editor application and enlarged to 100% on the computer screen. Using the lasso tool, the cursor was used to outline the contour of the internal orbit on both the reconstructed and the opposite uninjured side at two levels closest to the equator of the globe. The number of pixels within the outlined orbits (as a measure of cross-sectional area of the orbit) was tabulated and compared ( Fig. 1 ).
Fig. 1.
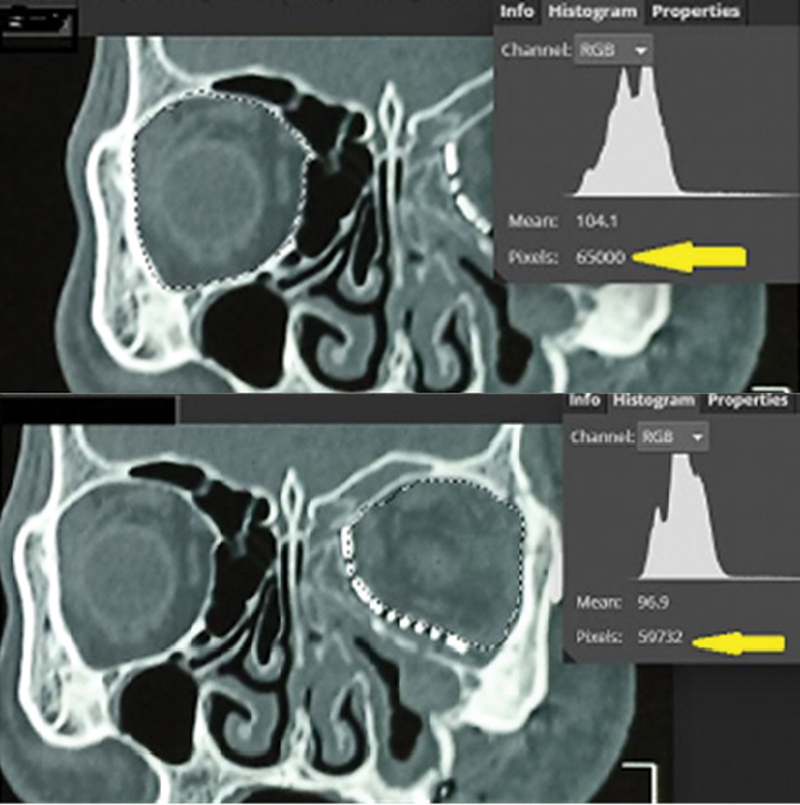
Method of comparing cross-sectional area of normal and reconstructed orbits in Photopea. The number of pixels contained within the outlined area ( dashed line ) is calculated using histogram function.
All data were tabulated in a master chart and analyzed.
Surgical Technique
All the patients were operated on under general anesthesia. Forced duction test was performed at the beginning. The pupillary response was checked at frequent intervals. Other associated fractures were reduced prior to orbital floor exploration. In case of impure blowout, the primary step was fixation of the zygomatic fracture.
The orbital floor was approached by a transconjunctival, infraorbital rim incision or via preexisting lacerations. The floor was exposed by a subperiosteal dissection and the herniated orbital contents were reduced. The posterior ledge and margins of the fracture were delineated and both globes were compared. A precontoured titanium mesh was placed to achieve minimal overcorrection of the globe position.
The final angulation between the anterior portion of the mesh used for fixation and the “intraorbital” portion of the mesh supporting the globe was closely tailored to achieve a slight overcorrection of the globe position. The mesh was fixed with one or two titanium screws at the inferior orbital rim.
Forced duction test was repeated to confirm the absence of soft-tissue incarceration. Incision was closed in layers.
Results
In the study period, a total of 24 patients with orbital blowout fractures underwent reconstruction with precontoured titanium mesh; of these 1 had bilateral injuries and 2 had insufficient postoperative follow-up data, and were excluded. Thus, 21 subjects were included in the study comprising 19 males (91%) and 2 females (9%). The average age was 27.1 years (range: 17–55 years). Road traffic accident (16/21 [76%]) was the most common mode of injury, followed by assault (3/21 [14.29%]), railway accident (1/21 [4.76%]), and fall from height (1/21 [4.76%]).
The follow-up period ranged from 6 to 10 months.
The preoperative findings were as under Table 2 .
Table 2. Clinical findings and associated fractures.
| Clinical finding | Incidence | Associated fractures | Incidence |
|---|---|---|---|
| Enophthalmos | 18 (85%) | Zygomaticomaxillary complex (ZMC) including Le Fort | 15 (71.4%) |
| Diplopia | 12 (57%) | Nasoethmoid complex | 5 (23.8%) |
| Restricted range of motion | 7 (33%) | ||
| Infraorbital paresthesia | 12 (57%) |
All cases were operated on within 3 weeks of trauma, 52% within the first week and 48% between 1 and 3 weeks posttrauma.
Twenty patients had impure blowout fractures (95%), while only 1 (5%) had a pure blowout; the orbital floor was most commonly fractured (16 [76%]), followed by the floor and the medial wall combined (5 [24%]). There were no isolated medial wall fractures.
The orbital floor was accessed by an infraorbital rim incision in 13 (62%) patients, transconjunctival in 5 (24%) patients, and through the preexisting lacerations in 3 (14%) patients.
Postoperative CT scans were done in the later 9 patients of the series. The analysis of coronal views by the Photopea R application comparing the operated and normal orbits at two levels revealed a correction of the increased cross-sectional area in all cases ( Table 3 ).
Table 3. Comparison of cross-sectional areas.
| Sl. no. | Ratio of cross-sectional area (pixels) of normal to reconstructed orbit at level I | Ratio of cross-sectional area (pixels) of normal to reconstructed orbit at level II |
|---|---|---|
| 1 | 1/0.98 | 1/1.05 |
| 2 | 1/0.92 | 1/0.98 |
| 3 | 1/0.92 | 1/0.91 |
| 4 | 1/0.91 | 1/0.93 |
| 5 | 1/0.97 | 1/0.98 |
| 6 | 1/0.99 | 1/1 |
| 7 | 1/0.97 | 1/0.98 |
| 8 | 1/0.99 | 1/1 |
| 9 | 1/0.99 | 1/0.99 |
Enophthalmos was completely corrected in 17/18 patients, while 11/12 patients had complete correction of diplopia ( Figs. 2 3 ). One patient with a comminuted zygomatic fracture with severe loss of floor, medial walls, and late presentation (>2 weeks) had persistent diplopia and mild enophthalmos. Infraorbital paresthesia persisted in 7/12 patients at 6 months of follow-up. All scars healed uneventfully and were well settled ( Figs. 2 , 3 , 4 ).
Fig. 2.
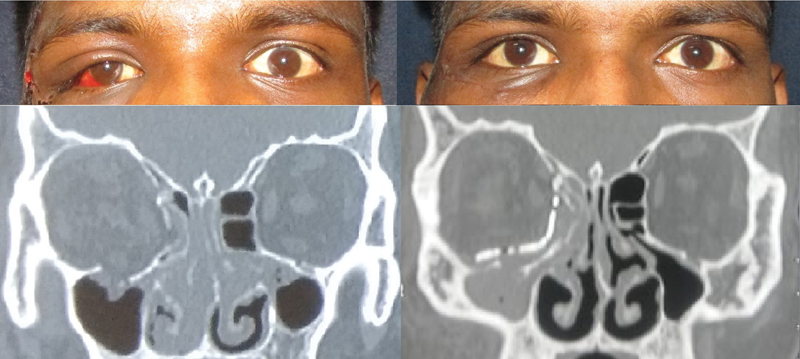
(Above) Pre- and postoperative photographs of a 20-year-old student with right-sided impure blowout fracture; correction of enophthalmos following open reduction and internal fixation (ORIF) of the zygoma and prefabricated titanium mesh for the blowout. (Below) Pre- and postoperative computed tomography (CT) scan showing restoration of the floor and medial wall anatomy with prefabricated titanium mesh.
Fig. 3.

A 32-year-old housewife with right-sided impure blowout fracture following an accident with enophthalmos and restricted upward gaze. (Above) Pre- and postoperative photographs showing correction of enophthalmos. (Below) Pre- and postoperative photographs showing correction of restricted upward gaze.
Fig. 4.
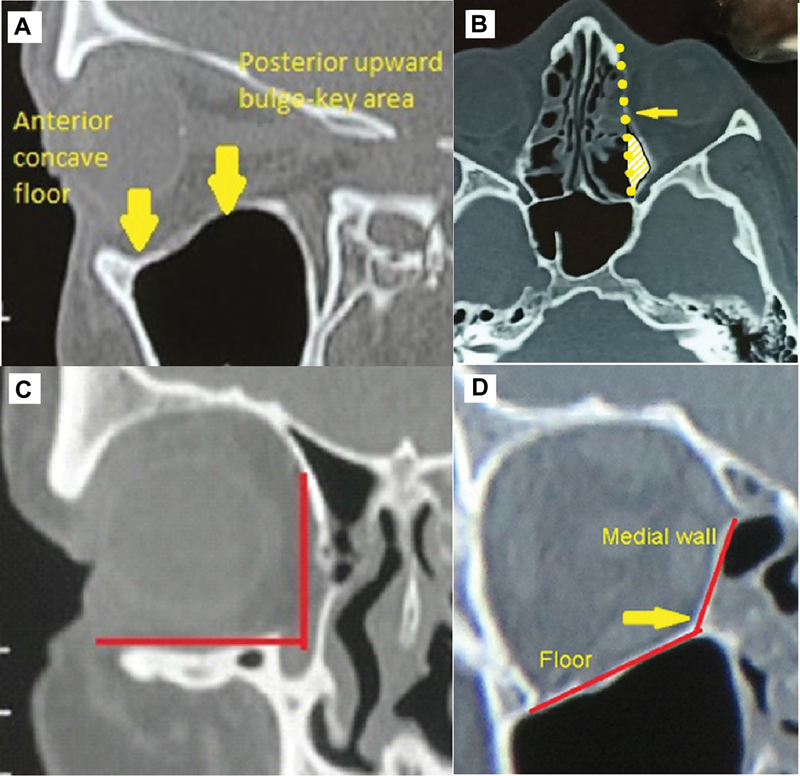
Features relevant to blowout fractures are portrayed in this figure.
According to the scoring system, 17 patients had excellent results, 3 patients had good results, and 1 patient had a fair result.
There was no case of implant infection, extrusion or migration, ectropion of the lower eyelid, or scar hypertrophy.
Discussion
Anatomic Peculiarities of the Orbital Walls
The anatomy of the bony orbit is well described. 7 8 Features relevant to blowout fractures are ( Fig. 4 ):
The medial wall and floor are the thinnest and almost exclusively involved; they meet at an angle at the superomedial buttress of the maxillary sinus. In combined fractures of the floor and medial wall, this region needs to be accurately reconstructed ( Fig. 4C and 4D ).
Both the floor and the medial wall demonstrate a bulge into the orbital cavity just behind the globe. This retrobulbar bulge contributes to supporting the globe in its correct anteroposterior position ( Fig. 4A and 4B ).
The cross-sectional area reduces drastically posterior to the equator of the globe; dissection in this posterior third with protruding edematous fat and soft tissue to delineate the bony ledge can be difficult.
Blowout fractures are peculiar injuries adversely affecting both ocular function and aesthetics. Enophthalmos is caused by an increase in intraorbital volume and the only way to correct it is by restoring the volume, while persistent diplopia is due to extraocular muscle entrapment/incarceration and needs release of muscle and bridging the defect.
Reconstruction of three-dimensional anatomy of the orbital floor/medial wall with a retrobulbar bulge to support the globe position is critical for success. Depending on the defect location and size, various reconstructive materials have been recommended.
While autologous grafts are the gold standard in craniofacial reconstruction, the rigidity of bone/cartilage grafts makes precise reconstruction of the contour of the orbital floor difficult; isolated medial wall and combined medial wall/floor defects present challenges. Further disadvantages include donor site morbidity, additional operative time, and problems with fixation.
Titanium has good biocompatibility, strength, and osteointegration properties. It is radio-opaque and has been successfully used for craniomaxillofacial osteosynthesis for several decades. A precontoured titanium mesh is precut and contoured to mimic the native orbital anatomy based on normative data and adult skull models. 9 It can be easily trimmed to the required size and permits easy and quick contouring while maintaining its shape once contoured. It also provides plenty of options for fixation depending upon individual fracture patterns. This allows precise volume restoration, saves operative time, and eliminates donor site morbidity.
Pure blowout fractures have normally positioned orbital rims. Thus, replacing a correctly contoured missing floor and/or medial wall may suffice. In case of impure blowouts, however, a lot depends on the accuracy of reduction of the rim fracture. Even a minor discrepancy in craniocaudal positioning of the infraorbital rim can render any attempted reconstruction imprecise by adding to the effective intraorbital volume ( Fig. 5 ).
Fig. 5.
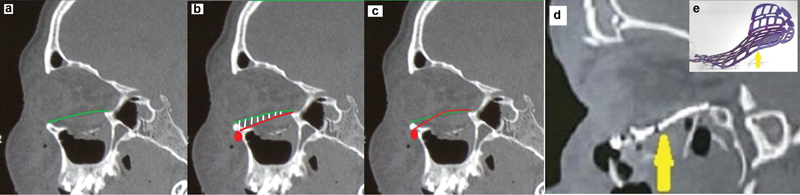
Influence of infraorbital rim position on orbital volume restoration. (a) Pure blowout; rim in normal position, reconstruction adequate. (b) Rim fixed caudally ( red indicator ); any material from this position to the posterior ledge will correct orbital volume incompletely ( shaded area ) causing residual enophthalmos. (c) Rim fixed caudally; the titanium mesh with retrobulbar bulge allows further contouring to compensate for the excessive volume, thus restoring the globe position. (d) The precontoured mesh mirroring the retrobulbar bulge of the floor on sagittal view. (e) Profile view of the precontoured titanium mesh.
A precontoured mesh has the advantage of providing a bulge in the floor and medial wall where it is most needed to support the globe. Also, in the cases with incompletely corrected rims, it permits tailoring/accentuating the retrobulbar bulge based on the desired globe position and maintains the contour once achieved.
In a study of 405 blowout fractures treated with either polyethylene or hydroxyapatite, Nam et al 10 reported that impure blowouts were more likely to have persistent enophthalmos and diplopia (11.9%) as compared with isolated orbital fractures (2.7%). They concluded that this is not caused by the implant itself but by the severity and extension of the fracture, which causes undercorrection of the orbital rim. As discussed earlier, a precontoured mesh can overcome this shortcoming.
In a study of 58 patients with pure blowout fractures treated with cranial bone graft (26) or titanium mesh (32), Ellis and Tan 11 concluded that the orbits reconstructed with titanium mesh were architecturally more accurate than those with bone grafts. However, they only analyzed postoperative CT scans and accepted that a clinical analysis of ocular motility/function, enophthalmos, and surgical complications was needed for more comprehensive results.
Tang et al used rapid prototyping and titanium mesh reconstruction to achieve orbital volumes within 2% of uninjured side; however, 16/41 (34%) subjects still had persistent enophthalmos. 12
In a study of blowout fractures treated with high-density porous polyethylene (HDPE) MEDPOR composite titanium mesh, Han et al 13 reported that 15 of 19 patients (78.94%) with enophthalmos showed complete correction. Similarly, diplopia resolved in 12 of 14 patients (85.71%). Although postoperative CT scans were obtained, no formal volumetric or cross-sectional area analysis was done.
In a systematic review of 55 articles studying biomaterials for repair of blowout fractures, Gunarajah et al 14 found the incidence of persistent enophthalmos to be 29.8% (134/449) across all types of biomaterials, 23.3% (18/77) for autologous bone grafts, 50.9% (28/55) for titanium mesh, and 24.78% (28/113) for porous polyethylene implants.
In our study, enophthalmos was corrected in 94% (17/18) patients, while diplopia correction was achieved in 92% (11/12) patients, which compares favorably with the above studies. Since the final outcome measure is clinical, that is, enophthalmos, the decision regarding positioning the reconstructing material must be based on intraoperative assessment of the globe position rather than just statistical restoration of the orbital volume. We recommend minimal overcorrection of the globe position expecting some postoperative edema resolution.
In a review of alloplasts for orbital fracture reconstruction, Seen et al 16 concluded that prefabricated titanium meshes were used more significantly for complex fractures due to its mechanical strength, biocompatibility, and long-lasting stability. Also, titanium meshes are at lower risk of postoperative orbital compartment syndrome due to the openings compared with solid implants such as HDPE (MEDPOR).
The adequacy of these corrections can most precisely be assessed by CT volumetric studies. However, our cases did not use this technology and we applied cross-sectional areas to compare volume (since volume of a pyramid is dependent on the area of the base) in nine cases, which revealed correction of increased volume in all cases.
There are more sophisticated techniques for reconstruction of orbital anatomy including intraoperative CT scans and navigation. 15 16 17 18 19 However, till these become more widely accessible, clinical assessment of implant placement continues to be the norm.
Conclusion
Orbital blowout fractures are one of the most challenging injuries in the management of maxillofacial trauma. Despite significant advances in our understanding of these injuries, a universal “ideal” reconstructive material remains elusive. We have attempted to elaborate our experience with precontoured mesh, which restores orbital wall anatomy, is safe, quick, and fairly easy and reproducible with a shorter learning curve. With proper patient selection and execution, precontoured titanium mesh can serve as an excellent reconstructive option in blowout fractures of the orbit.
Footnotes
Conflict of Interest None declared.
References
- 1.Jatania H.Spectrum of Ocular Changes after Zygomatico-Maxillary-Complex and Orbital Fractures [dissertation]. Bengaluru, India: Rajiv Gandhi University of Health Science; 2012:1–4, 30–54
- 2.Pfeiffer R L. Traumatic enophthalmos. Trans Am Ophthalmol Soc. 1943;41:293–306. [PMC free article] [PubMed] [Google Scholar]
- 3.Phalen J J, Baumel J J, Kaplan P A. Orbital floor fractures: a reassessment of pathogenesis. Nebr Med J. 1990;75(05):100–103. [PubMed] [Google Scholar]
- 4.Smith B, Regan W F., Jr Blow-out fracture of the orbit; mechanism and correction of internal orbital fracture. Am J Ophthalmol. 1957;44(06):733–739. doi: 10.1016/0002-9394(76)90774-1. [DOI] [PubMed] [Google Scholar]
- 5.Hawes M J, Dortzbach R K. Surgery on orbital floor fractures. Influence of time of repair and fracture size. Ophthalmology. 1983;90(09):1066–1070. doi: 10.1016/s0161-6420(83)80049-9. [DOI] [PubMed] [Google Scholar]
- 6.Wevers M, Strabbing E M, Engin O, Gardeniers M, Koudstaal M J. CT parameters in pure orbital wall fractures and their relevance in the choice of treatment and patient outcome: a systematic review. Int J Oral Maxillofac Surg. 2022;51(06):782–789. doi: 10.1016/j.ijom.2021.10.001. [DOI] [PubMed] [Google Scholar]
- 7.Douglas R H, Lawrenson J G. Orbit and accessory apparatus. In: Gray's Anatomy: The Anatomical Basis of Clinical Practice. 41st ed. London: Elsevier; 2016:666–685 [Google Scholar]
- 8.Manson P N, Clifford C M, Su C T, Iliff N T, Morgan R. Mechanisms of global support and posttraumatic enophthalmos: I. The anatomy of the ligament sling and its relation to intramuscular cone orbital fat. Plast Reconstr Surg. 1986;77(02):193–202. [PubMed] [Google Scholar]
- 9.Cornelius C, Gellrich N. Choice of implants. AO Surgery Reference. Available at:https://surgeryreference.aofoundation.org/cmf/trauma/midface/further-reading/choice-of-implants#orbital-plates
- 10.Nam S-B, Bae Y-C, Moon J-S, Kang Y-S. Analysis of the postoperative outcome in 405 cases of orbital fracture using 2 synthetic orbital implants. Ann Plast Surg. 2006;56(03):263–267. doi: 10.1097/01.sap.0000199173.73610.bc. [DOI] [PubMed] [Google Scholar]
- 11.Ellis E, III, Tan Y. Assessment of internal orbital reconstructions for pure blowout fractures: cranial bone grafts versus titanium mesh. J Oral Maxillofac Surg. 2003;61(04):442–453. doi: 10.1053/joms.2003.50085. [DOI] [PubMed] [Google Scholar]
- 12.Tang W, Guo L, Long J. Individual design and rapid prototyping in reconstruction of orbital wall defects. J Oral Maxillofac Surg. 2010;68(03):562–570. doi: 10.1016/j.joms.2009.04.042. [DOI] [PubMed] [Google Scholar]
- 13.Han X, Yang S, Dong Z, Feng W. Reconstruction of orbital blowout fractures using MEDPOR titanium mesh implants. Int J Clin Exp Med. 2016;9(06):12411–12415. [Google Scholar]
- 14.Gunarajah D R, Samman N. Biomaterials for repair of orbital floor blowout fractures: a systematic review. J Oral Maxillofac Surg. 2013;71(03):550–570. doi: 10.1016/j.joms.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 15.Potter J K, Malmquist M, Ellis E., III Biomaterials for reconstruction of the internal orbit. Oral Maxillofac Surg Clin North Am. 2012;24(04):609–627. doi: 10.1016/j.coms.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Seen S, Young S, Lang S S, Lim T C, Amrith S, Sundar G. Orbital implants in orbital fracture reconstruction: a ten-year series. Craniomaxillofac Trauma Reconstr. 2021;14(01):56–63. doi: 10.1177/1943387520939032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Metzger M C, Schön R, Schulze D, Carvalho C, Gutwald R, Schmelzeisen R. Individual preformed titanium meshes for orbital fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(04):442–447. doi: 10.1016/j.tripleo.2006.02.031. [DOI] [PubMed] [Google Scholar]
- 18.Metzger M C, Schön R, Weyer N. Anatomical 3-dimensional pre-bent titanium implant for orbital floor fractures. Ophthalmology. 2006;113(10):1863–1868. doi: 10.1016/j.ophtha.2006.03.062. [DOI] [PubMed] [Google Scholar]
- 19.Lim C G, Campbell D I, Cook N, Erasmus J. A case series of rapid prototyping and intraoperative imaging in orbital reconstruction. Craniomaxillofac Trauma Reconstr. 2015;8(02):105–110. doi: 10.1055/s-0034-1395384. [DOI] [PMC free article] [PubMed] [Google Scholar]


