Abstract
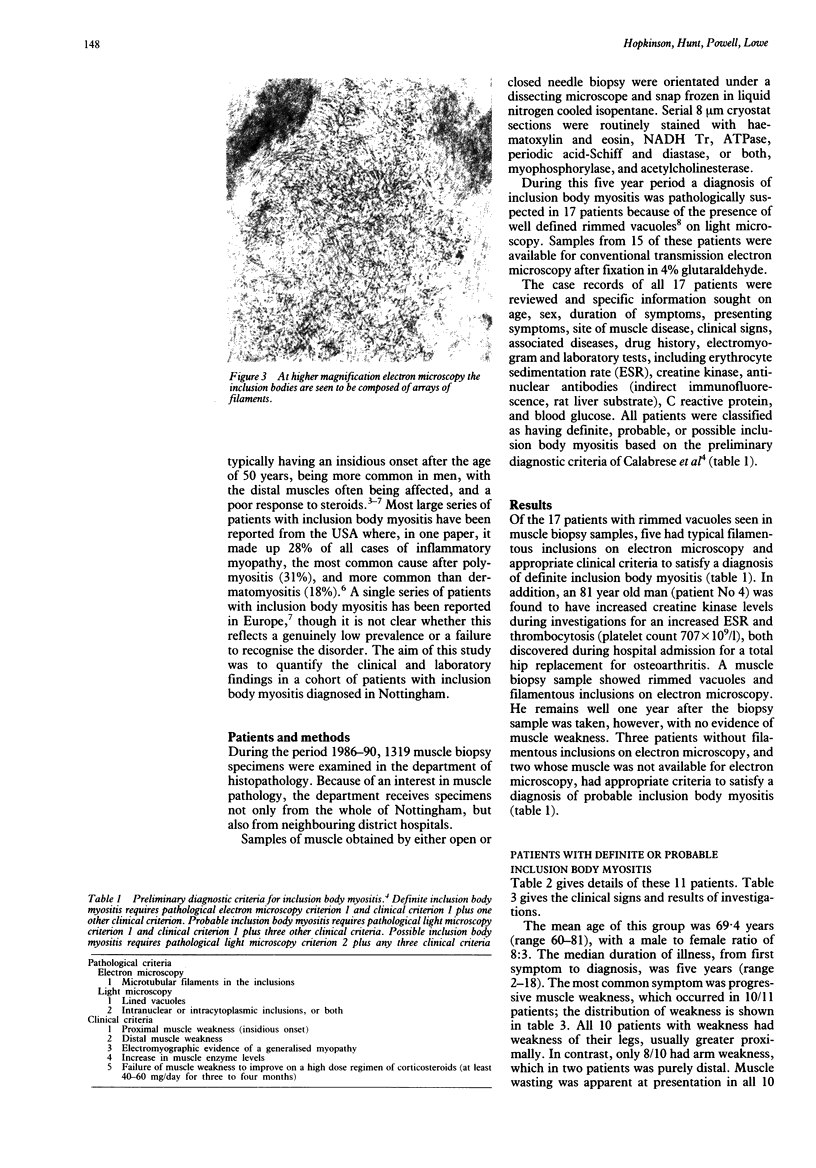
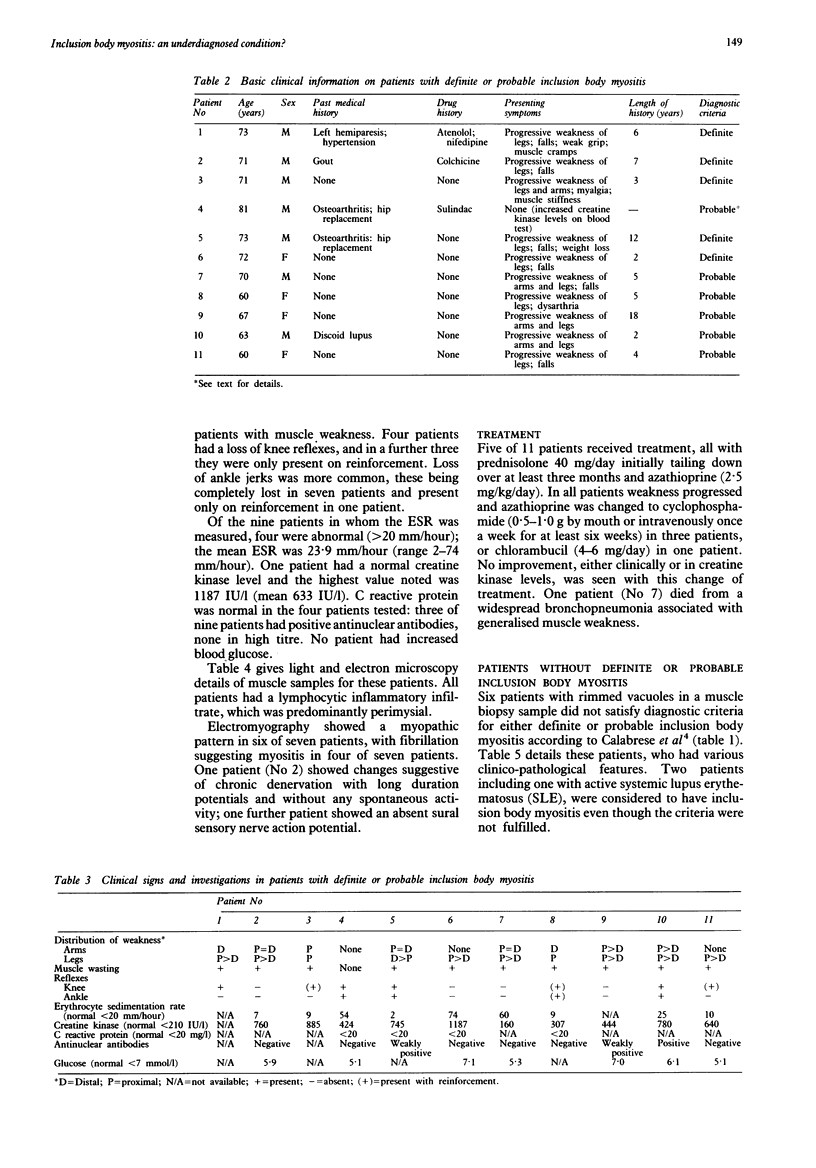
Inclusion body myositis is an increasingly recognised form of inflammatory myopathy with characteristic clinical and histopathological features which has seldom been reported in the United Kingdom. This paper presents the clinicopathological features of a series of patients diagnosed in Nottingham from 1986 to 1990. During this period, 1319 muscle biopsy samples were processed by this laboratory and rimmed vacuoles were seen in 17 patients. Eleven patients had definite or probable inclusion body myositis according to published criteria. The mean age of the group was 69.4 years with a male to female ratio of 8:3. Typical clinical features were a slowly progressive painless, proximal lower limb weakness, with muscle wasting and early loss of reflexes. The median duration of illness from first symptom to presentation was five years (range 2-18 years). Falls were a prominent symptom in six patients and distal weakness occurred in nine patients. Creatine kinase was increased in 10 patients but only one had a level > 1000 IU/l; the erythrocyte sedimentation rate was normal in five patients. Treatment with steroids or cytotoxic drugs, or both, did not prevent disease progression. It is confirmed that inclusion body myositis is a distinct cause of inflammatory myopathy which is probably underdiagnosed in the United Kingdom. Clinically, it should be suspected in older patients presenting with muscle weakness of insidious onset. Pathologically, a careful search should be made for rimmed vacuoles and inflammation; ultrastructurally, the presence of inclusions will confirm the diagnosis.
Full text
PDF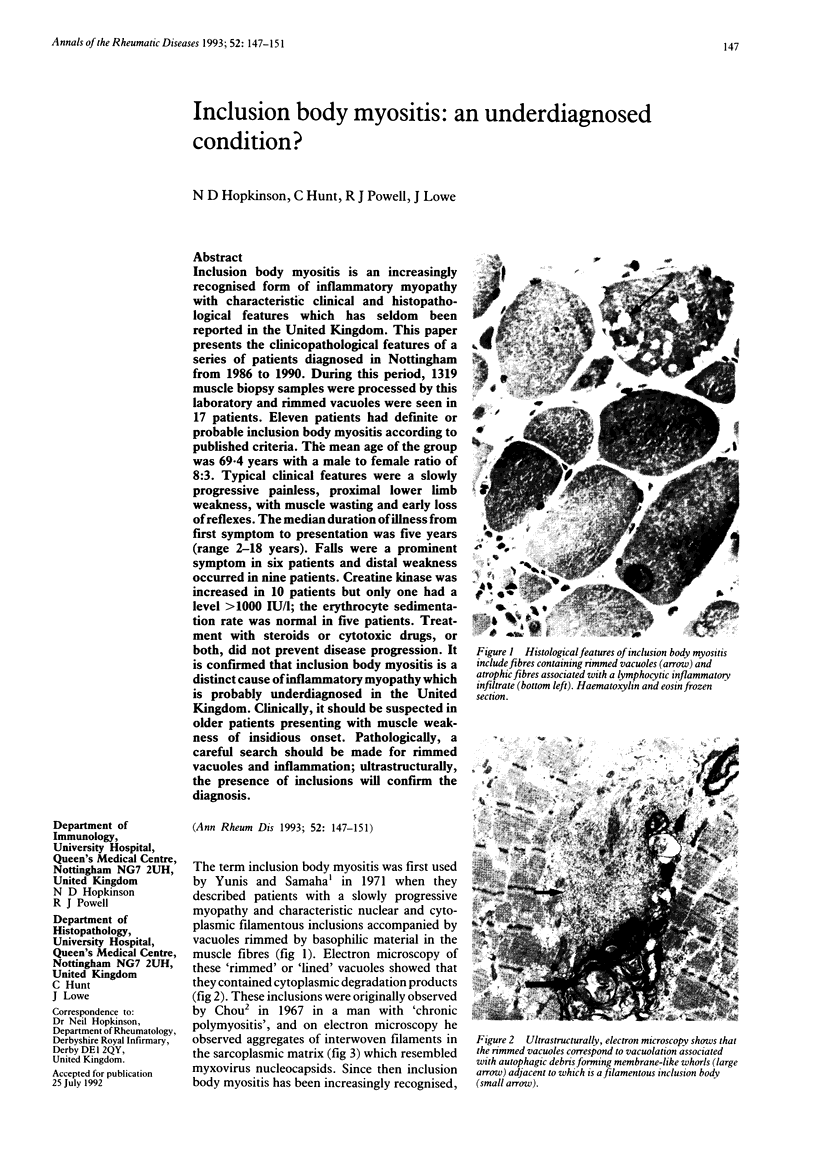

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arahata K., Engel A. G. Monoclonal antibody analysis of mononuclear cells in myopathies. I: Quantitation of subsets according to diagnosis and sites of accumulation and demonstration and counts of muscle fibers invaded by T cells. Ann Neurol. 1984 Aug;16(2):193–208. doi: 10.1002/ana.410160206. [DOI] [PubMed] [Google Scholar]
- Askanas V., Engel W. K., Alvarez R. B., Glenner G. G. beta-Amyloid protein immunoreactivity in muscle of patients with inclusion-body myositis. Lancet. 1992 Feb 29;339(8792):560–561. doi: 10.1016/0140-6736(92)90388-j. [DOI] [PubMed] [Google Scholar]
- Calabrese L. H., Mitsumoto H., Chou S. M. Inclusion body myositis presenting as treatment-resistant polymyositis. Arthritis Rheum. 1987 Apr;30(4):397–403. doi: 10.1002/art.1780300406. [DOI] [PubMed] [Google Scholar]
- Carpenter S., Karpati G., Heller I., Eisen A. Inclusion body myositis: a distinct variety of idiopathic inflammatory myopathy. Neurology. 1978 Jan;28(1):8–17. doi: 10.1212/wnl.28.1.8. [DOI] [PubMed] [Google Scholar]
- Chad D., Good P., Adelman L., Bradley W. G., Mills J. Inclusion body myositis associated with Sjögren's syndrome. Arch Neurol. 1982 Mar;39(3):186–188. doi: 10.1001/archneur.1982.00510150056014. [DOI] [PubMed] [Google Scholar]
- Cohen M. R., Sulaiman A. R., Garancis J. C., Wortmann R. L. Clinical heterogeneity and treatment response in inclusion body myositis. Arthritis Rheum. 1989 Jun;32(6):734–740. doi: 10.1002/anr.1780320611. [DOI] [PubMed] [Google Scholar]
- Danon M. J., Reyes M. G., Perurena O. H., Masdeu J. C., Manaligod J. R. Inclusion body myositis. A corticosteroid-resistant idiopathic inflammatory myopathy. Arch Neurol. 1982 Dec;39(12):760–764. doi: 10.1001/archneur.1982.00510240022006. [DOI] [PubMed] [Google Scholar]
- Fukuhara N., Kumamoto T., Tsubaki T., Mayuzumi T., Nitta H. Oculopharyngeal muscular dystrophy and distal myopathy. Intrafamilial difference in the onset and distribution of muscular involvement. Acta Neurol Scand. 1982 May;65(5):458–467. doi: 10.1111/j.1600-0404.1982.tb03103.x. [DOI] [PubMed] [Google Scholar]
- Fukuhara N., Kumamoto T., Tsubaki T. Rimmed vacuoles. Acta Neuropathol. 1980;51(3):229–235. doi: 10.1007/BF00687390. [DOI] [PubMed] [Google Scholar]
- Henriksson K. G., Sandstedt P. Polymyositis--treatment and prognosis. A study of 107 patients. Acta Neurol Scand. 1982 Apr;65(4):280–300. doi: 10.1111/j.1600-0404.1982.tb03087.x. [DOI] [PubMed] [Google Scholar]
- Lotz B. P., Engel A. G., Nishino H., Stevens J. C., Litchy W. J. Inclusion body myositis. Observations in 40 patients. Brain. 1989 Jun;112(Pt 3):727–747. doi: 10.1093/brain/112.3.727. [DOI] [PubMed] [Google Scholar]
- Matsubara S., Tanabe H. Hereditary distal myopathy with filamentous inclusions. Acta Neurol Scand. 1982 Apr;65(4):363–368. doi: 10.1111/j.1600-0404.1982.tb03093.x. [DOI] [PubMed] [Google Scholar]
- Mendell J. R., Sahenk Z., Gales T., Paul L. Amyloid filaments in inclusion body myositis. Novel findings provide insight into nature of filaments. Arch Neurol. 1991 Dec;48(12):1229–1234. doi: 10.1001/archneur.1991.00530240033013. [DOI] [PubMed] [Google Scholar]
- Mhiri C., Gherardi R. Inclusion body myositis in French patients. A clinicopathological evaluation. Neuropathol Appl Neurobiol. 1990 Aug;16(4):333–344. doi: 10.1111/j.1365-2990.1990.tb01267.x. [DOI] [PubMed] [Google Scholar]
- Nonaka I., Sunohara N., Ishiura S., Satoyoshi E. Familial distal myopathy with rimmed vacuole and lamellar (myeloid) body formation. J Neurol Sci. 1981 Jul;51(1):141–155. doi: 10.1016/0022-510x(81)90067-8. [DOI] [PubMed] [Google Scholar]
- Ringel S. P., Kenny C. E., Neville H. E., Giorno R., Carry M. R. Spectrum of inclusion body myositis. Arch Neurol. 1987 Nov;44(11):1154–1157. doi: 10.1001/archneur.1987.00520230042011. [DOI] [PubMed] [Google Scholar]
- Tomé F. M., Fardeau M. Nuclear inclusions in oculopharyngeal dystrophy. Acta Neuropathol. 1980;49(1):85–87. doi: 10.1007/BF00692226. [DOI] [PubMed] [Google Scholar]
- Yunis E. J., Samaha F. J. Inclusion body myositis. Lab Invest. 1971 Sep;25(3):240–248. [PubMed] [Google Scholar]