Robotic surgery has transformed current practice within specialities such as Head and Neck surgery whereas uptake has been much more limited within ophthalmology [1–3]. Robotic assisted surgery offers multiple advantages over conventional surgical techniques, such as high definition 3-dimensional optics, dextrous wristed instruments, motion scaling and tremor filtration.
We present a case of an 85-year-old woman with a medial canthal basal cell carcinoma recurrence who had multiple procedures elsewhere. We utilised the Da Vinci XI system to perform a robotically-assisted wide local excision of the tumour preserving the patient’s globe, extraocular muscles and vision in a case otherwise recommended for orbital exenteration. In 2005 she was first treated with a wide local excision with close surgical margins, then Mohs micrographic surgery in 2013. A CT scan confirmed a right medial canthal mass invading the orbit, with possible extension down the proximal nasolacrimal duct. (Fig. 1). The patient had normal vision and motility. The conjunctiva and lacrimal caruncle were disease free. Her case was discussed at the head and neck multidisciplinary team meeting (MDT) for consideration of orbital exenteration. We elected to utilise the DaVinci XI system to perform Robotic Assisted Orbital Surgery (RAOS) to clear the tumour whilst preserving vital orbital structures. Reconstruction was staged to check margin status. The Da Vinci Xi system was positioned, and 3 arms of the system were deployed. A wide local excision was performed using the robot. A skin incision was made and the medial canthal ligament was divided with dissection down the medial orbital wall and exposure of the lacrimal crest. (Fig. 2). The globe was laterally retracted by the bed-side surgeon. Dissection along the medial aspect of the globe preserved the medial rectus muscle. An osteotomy of the medial orbital wall including the lacrimal bone, lacrimal sac and nasolacrimal duct was performed with a Piezo saw. An en-bloc resection of the tumour was performed. The patient made an uneventful recovery with preservation of eye movements and vision. Histology showed a 16 mm basal cell carcinoma with associated perineural invasion. There were clear surgical margins at the orbital and deep resection margins. There was a close surgical margin medially. As planned the patient underwent subsequent further excision of the medial resection margin and reconstruction with medial sural artery perforator free flap. The patient has remained disease free with preserved vision at 1 year follow up.
Fig. 1. Axial CT scan of the orbit confirming recurrent BCC.

Infiltrative BCC extending along medial wall.
Fig. 2.
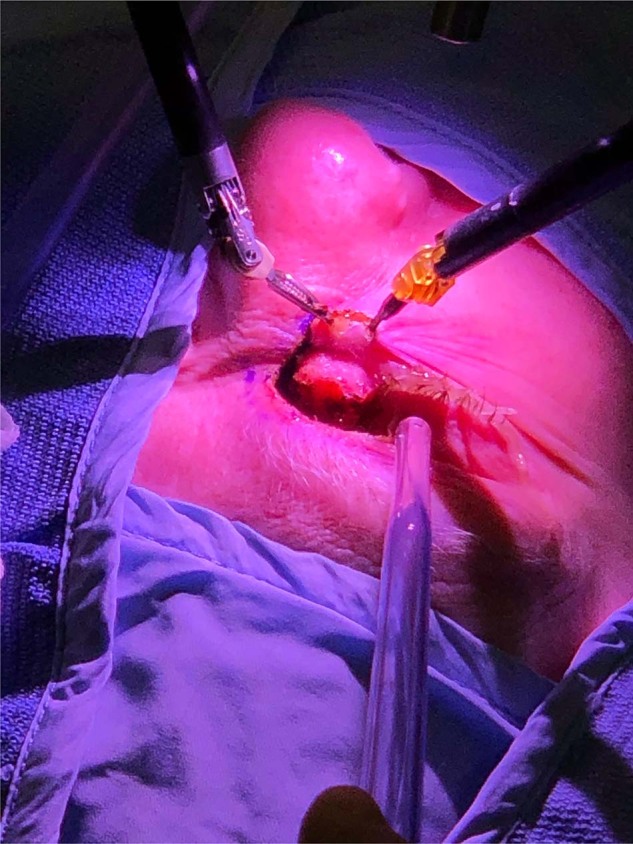
Photograph demonstrating the external extent of resection.
This case was initially recommended for orbital exenteration however we believe the use of the robotic system facilitated a safe globe-preserving approach. We believe that all the intrinsic benefits of robotic surgery such as enhanced 3-dimensional vision, precision calibrated fine movements & tremor free instrumentation are applicable for operating in the small confines of the orbital cavity. Robotics allowed dissection along the surface of the globe and extraocular muscles under a highly magnified view. Further applications such as finer instrumentation and utilizing the 4th arm as a retractor will improve this emerging field in orbital surgery. To our knowledge this is the first application of robotic assisted surgery within the orbit and may have wider applications within ophthalmology.
Author contributions
JPJ developed this project and participated in writing of the manuscript JF contributed to the writing and revising of the manuscript JU contributed to the revision of the manuscript and provided the clinical photographs CD contributed in drafting and revising the manuscript AA is head of head and neck robotic surgery at GSTT and has contributed to the writing of the manuscript.
Data availability
All data and materials can be provided on request.
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Approval from the trust risk and assurance committee (TRAC) and local robotic steering group (RSG) was provided for use of the DaVinci surgical system for orbital and periorbital tumours prior to this case. The patient provided informed consent for to undergo this treatment.
Consent for publication
The patient has provided written consent for publication of this manuscript including consent of publication of all images and clinical pictures.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rassweiller JJ, Autorino R, Klein J, Mottrie A, Serda Goezen A, Stolzenburg JU, et al. Future of robotic surgery in urology. BJU Int. 2017;120:822–41. doi: 10.1111/bju.13851. [DOI] [PubMed] [Google Scholar]
- 2.Pandey SK, Sharma V. Robotics and ophthalmology: are we there yet? Indian J Ophthalmol. 2019;67:988–94. doi: 10.4103/ijo.IJO_1131_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gerber MJ, Pettenkofer M, Hubschma JP. Advanced robotic surgical systems in ophthalmology. Eye. 2020;34:1554–62. doi: 10.1038/s41433-020-0837-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data and materials can be provided on request.


