Abstract
Introduction:
Increasing disparities within and between racial/ethnic groups in overdose deaths underscore the need to identify drivers and patterns to optimize overdose prevention strategies. We assess age-specific mortality rates (ASMR) in drug overdose deaths by race/ethnicity in 2015–2019 and 2020.
Methods:
Data were from the CDC Wonder, and included information for N=411,451 deceased individuals in the United States (2015–2020) with a drug overdose-attributed cause of death (ICD-10 codes: X40–X44, X60–X64, X85, Y10–Y14). We compiled overdose death counts by age, race/ethnicity, and population estimates to derive ASMRs, mortality rate ratios (MRR), and cohort effects.
Results:
The ASMRs for Non-Hispanic Black adults (2015–2019) followed a different pattern than other racial/ethnic groups—low ASMRs among young individuals and peaking between 55–64 years—a pattern exacerbated in 2020. Younger Non-Hispanic Black individuals had lower MRRs than young Non-Hispanic White individuals, yet, older Non-Hispanic Black adults had much higher MRRs than older Non-Hispanic White adults (45–54yrs:126%, 55–64yrs:197%; 65–74yrs:314%; 75–84:148%) in 2020. American Indian/Alaska Native adults had higher MRRs than Non-Hispanic White adults in death counts compiled from pre-pandemic years (2015–2019); however, MRRs increased in 2020 (15–24yrs:134%, 25–34yrs:132%, 35–44yrs:124%, 45–54yrs:134%, 55–64yrs:118%). Cohort analyses suggested a bimodal distribution of increasing fatal overdose rates among Non-Hispanic Black individuals aged 15–24 and 65–74.
Conclusions and Relevance:
Overdose fatalities unprecedently impact older Non-Hispanic Black adults and American Indian/Alaska Native populations of all ages, deviating from the pattern found for Non-Hispanic White individuals. Findings highlight the need for targeted naloxone and low-threshold buprenorphine programs to reduce racial disparities.
Keywords: drug overdose deaths, race/ethnicity, age, cohort effects
Introduction
In 2020, during the first year of the COVID-19 pandemic, more than 90,000 individuals in the United States died of a drug overdose, a 30% increase in overdose deaths from 2019 to 2020 (CDC, 2021). Among racial/ethnic groups, overdose deaths among Black and American Indian/Alaska Native individuals now exceed White individuals by 20% and 30%, respectively (CDC, 2021; Hahn et al., Panchal et al., 2021; Friedman & Hansen, 2022).
Over the past decades, White individuals have had higher rates of opioid use and overdose deaths, yet, increasing disparities in overdose deaths among racial/ethnic minorities underscores the need to identify patterns of drug use and overdose deaths within and between racial groups (Milam et al., 2021; Jones et al., 2019; Jalal et al., 2018). Drug overdose deaths are more common among middle-aged U.S. adults (Hedegaard et al., 2020). Higher overdose deaths among middle-aged adults may be attributed to underlying cardiovascular disease, thus putting these individuals for severe adverse consequences of drug use (Han et al., 2019). Substance use has traditionally been low among older adults compared to younger ages; yet, emerging literature has evidenced new increases in overdose deaths at older ages, especially among racially/ethnically minoritized groups (Mason et al., 2022; Lippold et al., 2019). Increases in overdose deaths among older adults, particularly older minoritized individuals, have been attributed to illicitly manufactured fentanyl, lack of access to substance use treatment, and underlying substance use disorders (Lippold et al., 2019). Emergent literature on race/ethnicity, age, and overdose deaths have focused exclusively on opioids, few include the year 2020, or solely focused on older populations, thus limiting the contextual comparison to younger ages (Mason et al., 2022; Cano et al., 2021; Lippod et al., 2019; Jalal et al., 2018; Shiels et al., 2018).
Identifying age and race/ethnicity distinctions in overdose deaths is vital to optimizing overdose strategies to reduce preventable overdose deaths. This study examined age-specific mortality rates (ASMR) in drug overdose by race/ethnicity among all recorded U.S. drug overdoses in the adult population from 2015–2020, denoting patterns of overdose deaths pre-pandemic and during the pandemic.
Methods
Using 2015–2020 mortality data from the Underlying Causes of Death file available in CDC Wonder (CDC, 2021b), drug overdose deaths were assessed using the 10th revision of the International Statistical Classification of Diseases and Related Health Programs (ICD-10) codes (X40–X44, X60–X64, X85, and Y10–Y14). Detailed explanations of the deaths included within these categories are included in the Supplemental Materials. Death counts and corresponding population estimates were examined by the decedent’s age and race/ethnicity. Age was coded by 10-year groups starting at age 15 with an open-ended group of 85 and older. Race/ethnicity was coded as a mutually exclusive five-level categorical variable. Following standard defined racial/ethnic groups categorizations used in studies of racial/ethnic health disparities (Mason et al., 2022; Cano et al., 2021; Milam et al., 2021), first, deaths were categorized by decedent’s ethnicity: Hispanic or non-Hispanic. Non-Hispanic decedents were then classified by race as Non-Hispanic African American or Black (Non-Hispanic-Black), Non-Hispanic American/Indian or Alaska Native, Non-Hispanic Asian, or Non-Hispanic White individuals.
Age-Specific Mortality Rates (ASMRs) were calculated by dividing death counts by age-group by the corresponding population estimates, and are presented per 100,000 persons from the specific racial/ethnic group. Corresponding population estimates for racial/ethnic groups were also retrieved from the CDC Wonder. To compare ASMRs by race/ethnicity, Mortality Rate Ratios (MRR) were calculated, where age-specific mortality rates (i) for racial/ethnic minorities (j) are compared with corresponding rates for Non-Hispanic White individuals.
MRR measures the magnitude and direction of differences in ASMRs. ASMRs were also calculated using overall U.S. overdose data by race/ethnicity and across the ten states with the highest overdose rates in the U.S. in 2019, namely, West Virginia, Delaware, Ohio, Maryland, Pennsylvania, Connecticut, Kentucky, Massachusetts, New Hampshire, and New Jersey (CDC, 2021c). Due to the uniqueness of the pandemic year of 2020, we deemed it necessary to assess overdose deaths this year separately than in prior years. ASMRs and MRRs were evaluated among all racial/ethnic groups with compiled death counts from 2015–2019 and separately in 2020. We then explore period and cohort differences in drug overdose deaths by year and age group for 2000–2015 and 2020 among racial/ethnic minority groups with different age and drug overdose patterns. Period analyses included in Tables 1 and 2 present the patterns by age and race/ethnicity in the period preceding the Covid-19 pandemic and the first year of the pandemic, respectively. Our approach to cohort dynamics, included in Figure 1, allows for the comparison of trends ASMR by race at different points in time. This allows for observing the emergence of opioid-related mortality within the Non-Hispanic Black and Non-Hispanic White population. A period effect would be illustrated by increases in ASMRs exacerbating existing patterns. On the other hand, a cohort effect would be illustrated by the progression or displacement of the peak age for opioid-related mortality. Because we leverage total US drug overdose deaths between 2015–2020 derived from death certificate data in conjunction to population-level estimates, statistical tests such as p-values are not warranted. This analytical approach is consistent with existing studies that leverage data from vital records and population estimates to evaluate mortality in the US (Wrigley-Field et al., 2022). The MRRs presented in our analyses illustrate population-level differences between mortality rates of decedents of racial/ethnic minority backgrounds and Non-Hispanic White decedents. All data used in this study are public, de-identified, and IRB-exempt.
Table 1.
Age-Specific Drug Overdose Mortality Rates in the United States (2015–2019) and Age-Specific Mortality Rate Ratios in comparison to Non-Hispanic White Individuals (N=320,556).
| Panel A. United States, 2015–2019 | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Age-Specific Mortality Rates | Mortality Rate Ratios (vs Non-Hispanic White Individuals) | ||||||||
|
|
|
||||||||
| Age | NH-African American or Black | Hispanic | NH-American Indian/Alaska | NH-Asian | NH-White | NH-African American or Black | Hispanic | NH-American Indian/Alaska | NH-Asian |
|
|
|
||||||||
| 15–24 | 6.24 | 6.82 | 14.39 | 3.67 | 15.24 | 40.94 | 44.75 | 94.42 | 24.08 |
| 25–34 | 21.19 | 16.53 | 38.80 | 4.43 | 47.27 | 44.83 | 34.97 | 82.08 | 9.37 |
| 35–44 | 29.90 | 17.42 | 50.56 | 4.96 | 48.01 | 62.28 | 36.28 | 105.31 | 10.33 |
| 45–54 | 39.38 | 17.95 | 46.41 | 4.96 | 40.62 | 96.95 | 44.19 | 114.25 | 12.21 |
| 55–64 | 41.86 | 15.57 | 29.24 | 3.83 | 27.33 | 153.17 | 56.97 | 106.99 | 14.01 |
| 65–74 | 19.37 | 5.75 | 9.10 | 1.88 | 8.69 | 222.90 | 66.17 | 104.72 | 21.63 |
| 75–84 | 3.69 | 2.28 | 3.74 | 1.84 | 3.99 | 92.48 | 57.14 | 93.73 | 46.12 |
| 85 + | 1.99 | 1.83 | 0.74 | 2.01 | 4.43 | 44.92 | 41.31 | 16.70 | 45.37 |
|
| |||||||||
| Panel B. Top 10 states with highest Drug Overdose Death Rates1, 2015–2019 | |||||||||
|
| |||||||||
| Age-Specific Mortality Rates | Mortality Rate Ratios (vs. Non-Hispanic White Individuals) | ||||||||
|
|
|
||||||||
| Age | NH-African American or Black | Hispanic | NH-America Indian/Alaska | NH-Asian | NH-White | NH-African American or Black | Hispanic | NH-American Indian/Alaska | NH-Asian |
|
|
|
||||||||
| 15–24 | 11.29 | 10.24 | -- | -- | 22.51 | 50.16 | 45.49 | -- | -- |
| 25–34 | 37.68 | 34.34 | -- | -- | 83.61 | 45.07 | 41.07 | -- | -- |
| 35–44 | 49.30 | 38.15 | -- | -- | 80.38 | 61.33 | 47.46 | -- | -- |
| 45–54 | 67.14 | 40.32 | -- | -- | 57.18 | 117.42 | 70.51 | -- | -- |
| 55–64 | 70.80 | 27.20 | -- | -- | 33.27 | 212.80 | 81.76 | -- | -- |
| 65–74 | 29.53 | 6.96 | -- | -- | 8.03 | 367.75 | 86.67 | -- | -- |
| 75–84 | 5.06 | -- | -- | -- | 3.14 | 161.15 | -- | -- | -- |
| 85 + | -- | -- | -- | -- | 4.14 | -- | -- | -- | -- |
Note: Rates are per 100,000 population. NH=Non-Hispanic
The Top 10 states include W.V., DE, OH, MD, PA, CT, KY, MA, NH and N.J. In Panel B, omitted sections are due to data suppression due to small counts.
MRRs are centered around 100. Sample interpretation: NH-Black individuals 15–24 yrs. had an MRR 59.06% less than NH-White individuals of the same age between 2015–2019.
Table 2.
Age-Specific Drug Overdose Mortality Rates in the United States (2020) and Age-Specific Mortality Rate Ratios in comparison to Non-Hispanic White Individuals (N=90,895)
| Crude Death Rates | Mortality Rate Ratios (vs Whites) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Age | NH-African American or Black | Hispanic | NH-American Indian/Alaska | NH-Asian | NH-White | NH-African American or Black | Hispanic | NH-American Indian/Alaska | NH-Asian |
|
|
|||||||||
| 15–24 | 15.4 | 15.0 | 25.0 | 6.6 | 18.7 | 82.35 | 80.21 | 133.69 | 35.29 |
| 25–34 | 44.0 | 30.1 | 78.1 | 8.8 | 59.1 | 74.45 | 50.93 | 132.15 | 14.89 |
| 35–44 | 57.6 | 29.6 | 83.3 | 8.5 | 67.3 | 85.59 | 43.98 | 123.77 | 12.63 |
| 45–54 | 66.0 | 26.8 | 70.3 | 8.1 | 52.3 | 126.20 | 51.24 | 134.42 | 15.49 |
| 55–64 | 70.1 | 24.7 | 42.1 | 6.0 | 35.6 | 196.91 | 69.38 | 118.26 | 16.85 |
| 65–74 | 35.2 | 8.8 | 10.3 | 3.2 | 11.2 | 314.29 | 78.57 | 91.96 | 28.57 |
| 75–84 | 5.8 | 3.7 | -- | -- | 3.9 | 148.72 | 94.87 | -- | -- |
| 85 + | -- | -- | -- | -- | 4.4 | -- | -- | -- | -- |
Source: CDC WONDER
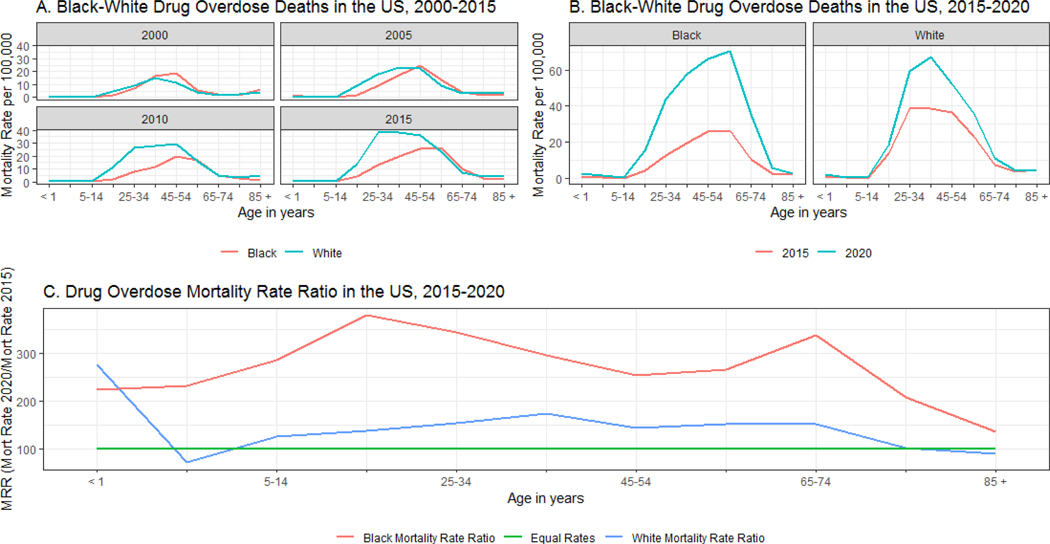
Figure 1.
Drug Overdose deaths in the US, 2000–2020. Panel A shows the Drug Overdose Mortality Rates for the Non-Hispanic Black and Non-Hispanic White population from 2000 to 2015. Panel B compares the Drug Overdose Mortality Rates for the Non-Hispanic Black and Non-Hispanic White population in 2015 with those observed in 2020. Panel C shows the Mortality Rate Ratio by age-group for the Non-Hispanic Black and Non-Hispanic White population. An MRR over 100 indicates an increase in the rates in 2020, and vice versa. The distance between the MRR and the Equal Rates line indicates the magnitude of the increase or decrease. The farthest from the line of equality the higher the change in comparison to 2015.
Results
The ASMRs for all racial/ethnic groups—except Non-Hispanic Black individuals—steadily increased by age group and were highest among adults between 35–44yrs, then decreased considerably among individuals of older ages in both pre-pandemic 2015–2019 (Table 1) and in 2020 (Table 2). The ASMRs for Non-Hispanic Black adults followed an different pattern—lower ASMRs among younger age groups (15–24 yrs: 6.24 per 100,000; 25–34 yrs: 21.19 per 100,000) and highest among the 55–64 age group—a pattern exacerbated during the pandemic year of 2020 (2015–2019: 41.86 per 100,000; 2020: 70.1 per 100,000). Younger Non-Hispanic Black individuals (15–24 yrs. and 25–34 yrs.) had 40%−55% lower MRRs than their Non-Hispanic White counterparts from 2015–2019; in 2020, this difference reduced to 15%−25%. Conversely, older Non-Hispanic Black adults aged 55–74 had higher ASMRs than their Non-Hispanic White counterparts from 2015–2019, a pattern exacerbated in 2020. As such, Non-Hispanic Black adults aged 55–64 (197%), 65–74 (314%), and 75–84 (149%) had MRRs that were greater than their Non-Hispanic White counterparts. Notably, the ASMRs for Non-Hispanic Black adults aged 65–74 (35.2) were over two times higher than that of Non-Hispanic Black individuals aged 15–24 (15.4), whereas Non-Hispanic White adults aged 65–74 (11.2) had an ASMR 60% lower than of Non-Hispanic White individuals aged 15–24 (18.7).
Among Non-Hispanic American Indian/Alaska Native populations in 2015–2019, ASMRs were comparable to Non-Hispanic White individuals, except those aged 25–34 (NH-AI/AN:38.8 vs. NH-White:47.3) and those aged 45–54 (NH-AI/AN:38.8 vs. NH-White:47.3). However, in 2020, the ASMRs and corresponding MRRs for drug overdose deaths for Non-Hispanic American Indian/Alaska Native populations were much higher than Non-Hispanic White individuals. Individuals aged 15–24, 25–34, and 45–54 had MRRs over 30% greater than Non-Hispanic White individuals, while those aged 35–44 and 55–64 had around 20% greater MRRs than Non-Hispanic White individuals. Pre-pandemic MRR for drug overdose in Non-Hispanic American Indian/Alaska Native individuals aged 25–34 was 20% lower than Non-Hispanic White individuals, but in 2020 was 32% greater than Non-Hispanic White individuals.
We further assessed age and racial/ethnic patterns in drug overdose among the 10 states with the highest drug overdose death rates to examine if the patterns found in the nationwide data existed within these states (Table 1, Panel B). We focused on drug overdose deaths among Non-Hispanic Black, Non-Hispanic White, and Hispanic individuals due to the small number of events occurring to Non-Hispanic American Indian/Alaska Native and Non-Hispanic Asian individuals in these states. We found that the Black/White and age patterns were not only present but exacerbated in these states. Specifically, the ASMRs were as follows ages 45–54 (NH-Black: 67.14, NH-White: 57.18), 55–64 (NH-Black: 70.80; NH-White: 33.27), 65–74 (NH-Black: 29.53; NH-White: 8.03), 75–84 (NH-Black: 5.06, NH-White: 3.14). The corresponding MRRs for older Non-Hispanic Black adults were 117% (45–54 yrs.), 212% (55–64 yrs.), 367.75% (65–74 yrs.), and 161.15% (75–84 yrs.) higher than their same-aged Non-Hispanic White counterparts. The racial differences in the ASMRs (2015–2019) between middle-aged and older Non-Hispanic Black and Non-Hispanic White Americans among these ten states were comparable to the exacerbated nationwide rates seen in 2020 alone.
Panel A in Figure 1 displays drug overdose mortality rates by age and period for 2000, 2005, 2010, and 2015 among Non-Hispanic Black and White decedents. We observe that the peak age for decedents from both racial groups differed since earlier stages of the ongoing U.S. drug overdose epidemic, with Non-Hispanic Black decedents being older than Non-Hispanic White decedents. In 2005, we observed an increase in the mortality rates for both groups, yet the increase is more pronounced for Non-Hispanic White decedents in younger age groups 15–40, while such a pronounced increase is not observed for the same-aged Non-Hispanic Black decedents. Rather, the increase in deaths among Non-Hispanic Black individuals occurred in the age group of 45–54. In 2010, we observed a substantial increase in drug overdose deaths for Non-Hispanic White decedents, highly clustered in mid-adulthood. For Non-Hispanic Black decedents, we observe stability in the peak age for drug overdose mortality and a notable increase in deaths occurring at ages 55–64. In 2015, we observed the peak ages for Non-Hispanic White decedents established at ages 25–34 and 35–44; for Non-Hispanic Black decedents, higher mortality rates were observed for respondents aged 45 to 64. The varying peaks in ages suggest that the current drug overdose epidemic has manifested differently by race, with higher impact observed among Non-Hispanic White individuals in younger ages and for older Non-Hispanic Black individuals. The patterns observed in Panel A indicates that period effects seem to be shaping mortality curves for Non-Hispanic White decedents. In contrast, the pattern observed for Non-Hispanic Black individuals, and the progression in the peak age, suggests that this phenomenon is shaped by cohort effects.
Panel B in Figure 1 illustrates the Black-White mortality curves for drug overdose deaths for 2015 and 2020. We focus on the most recent year of data on U.S. drug overdose deaths (2020) and include 2015, during the rise of synthetic opioid-attributed overdose deaths, for comparison. We find substantial increases in drug overdose deaths for Non-Hispanic Black and White population in 2020 compared to 2015, with the observed age and fatal drug overdose patterns corroborating the results depicted in Panel A. We observe more pronounced mortality rates for Non-Hispanic White decedents aged 25–34 and 35–44, with notable increases also observed in older ages. In contrast, the increases observed for Non-Hispanic Black individuals are more pronounced in ages 45–64, with the modal age shifting to the population aged 55–64.
Finally, Panel C in Figure 1, we quantify within-group shifts in mortality rates for Non-Hispanic White and Black individuals by illustrating the comparative MRRs for drug overdose rates for 2015 and 2020. In this regard, an MRR above 100 indicates the mortality rate for 2020 was higher than those observed in 2015 for the particular racial group. The green line indicates the point at which the mortality rates are the same (Equal Rates or MRR=100). Except for the population under 1 year, we observed a higher magnitude in the death rates for Non-Hispanic Black individuals in 2020, compared to 2015, with all but one of the rates exceeding a 100% increase. Drug overdose patterns by age suggest higher increases are observed for Non-Hispanic White adults in line with the increases observed in previous periods and concentrated among 25–34 and 35–44 years.
On the contrary, the increase observed for Non-Hispanic Blacks decedents follows a bimodal distribution. The highest increase is found among ages 15–24, ages where no substantial increase has been observed previously. The second peak is observed for the population aged 65–74 years, reinforcing the notion of a strong cohort effect shaping drug overdose deaths in the U.S among the Non-Hispanic Black population.
Discussion
This study examined overdose death rates at the intersection of age and race/ethnicity and accounts for pre-COVID-19 pandemic patterns and during the COVID-19 pandemic. We found elevated ASMRs and corresponding MRRs for all racial/ethnic groups in 2020 compared to the pre-pandemic years of 2015–2019. Yet, ASMRs were highest among older Black individuals and American Indian/Alaska Native sub-populations. Drug overdose rates were elevated among older Non-Hispanic Black adults, compared to younger Non-Hispanic Black individuals, and older Non-Hispanic White adults in all years assessed. However, the magnitude of this pattern increased in 2020, and a sub-analysis assessing ten states with the highest overdose rates from 2015–2019. Our analyses found a bimodal distribution of increasing fatal overdose rates among Non-Hispanic Black individuals aged 15–24 and 65–74. The bimodal distribution in growth in overdose deaths needs further evaluation, as the emergence of higher rates of increase in younger age groups for Non-Hispanic Black individuals deviates from the patterns found before the onset of the COVID-19 pandemic.
These findings suggest that fatal drug overdoses disproportionately impact older Non-Hispanic Black adults, a pattern that deviates from those observed among decedents from other racial/ethnic groups in the U.S. Among other racial/ethnic groups, those at higher risk for fatal overdoses are younger and middle-aged. Existing evidence from urban areas corroborate our findings of elevated deaths among older Black individuals (Gross, 2020; New York City Department of Health and Mental Hygiene, 2020). Other recent publications have also found general increases in drug overdose deaths among racially and ethnically minoritized populations in the U. S. (Burke et al., 2022; Furr-Holden et al., 2020) These increases in fatalities have been attributed to the adulteration of illicit drugs with fentanyl, lack of access to adequate treatment and harm reduction services, and social isolation which may increases the risk of individuals using drugs alone---all factors that have been exacerbated by the COVID-19 pandemic restrictions (Burke et al., 2022; Jones et al., 2022; Furr-Holden et al., 2020, Volkow, 2020). Further, these findings need to be understood in the context of increasing toxic and tainted drug supplies spurred by COVID-19-related border shutdowns that impacted supply chains (Stephenson, 2021). These hypotheses, however, need further exploration and are beyond the scope of the present study. Specific to individuals of older ages who use drugs, factors such as episodic drug use, reduced awareness of fentanyl, other health comorbidities, and less access to harm reduction efforts may be driving the increased overdose risk--- these hypotheses also need further exploration in future scholarship. Yet, available information outlines the urgent need to provide overdose prevention efforts across age groups and attend to culturally tailored needs, not just for youth.
Culturally tailored substance use treatment and overdose prevention are especially needed for American Indian/Alaska Natives, as fatal drug overdoses sharply increased among this population. In 2015–2019, American Indian/Alaska Natives aged 15–34 had ASMRs 10%−20% less than Non-Hispanic White individuals, yet in 2020, this group had much higher ASMRs and MRRs than Non-Hispanic White individuals. The reported increases in overdose deaths among American Indian/Alaska Native individuals are unprecedented and warrant dire attention underscoring the need to involve indigenous communities in opioid prevention and treatment strategies.
Existing data on American Indian/Alaska Native populations suggest that sharp increases in drug overdose deaths parallel the rise in suicides in this population, particularly among those aged 15–34 (Ivanich et al., 2021). Unlike the pattern of suicidality among other racial/ethnic groups that illustrate suicides occur in older ages, American Indian/Native Alaska individuals aged 15–34 have suicide rates two and half times greater than individuals of all other racial/ethnic groups (Ivanich et al., 2021). Historical trauma is embedded in the history of American Indian/Alaska Native and Black population, and the cumulative effect has been linked with adverse consequences, including substance use and suicidality (Brave Heart et al., 2011; Ivanich et al., 2021).
Our findings underscore the need to focus substance use treatment and overdose prevention efforts on older Black adults and American Indian/Alaska Native individuals, particularly targeted naloxone distribution-based overdose preventions programs (Cox et al., 2021; Jones et al., 2021; Dayton et al., 2020; Barboza & Angulski, 2020). Studies have shown that Black people who inject drugs (PWID) in Baltimore, typically older than White PWID, are less likely to have access to and possess naloxone (Dayton et al., 2020; Jones et al., 2021). However, racialized disparities in naloxone dissipated when Black PWID were clients of a syringe service program, as such programs are known to distribute naloxone and provide overdose response training (Jones et al., 2021). Such evidence also denotes syringe services’ utility in reaching older Black PWID and should be explored. In addition, the availability of buprenorphine, a type of medication for the treatment of opioid use disorder, has been shown to increase positive treatment outcomes among Black individuals, yet minoritized individuals are less likely to be prescribed buprenorphine than White individuals (Pro et al., 2022; Lagisetty et al., 2019). Access to buprenorphine treatment programs may be expanded using telemedicine, an innovative adaptation during this COVID-19 pandemic that has proven very effective in minoritized populations (Harris et al., 2022). Yet, known economic and social determinants of health continue to prevail as the main barriers to treatment and poor outcomes among minoritized groups (Friedman & Hansen, 2022).
In this current stage of the drug overdose crisis, markers of community distress, such as high unemployment, vacant homes, and lack of educational opportunity, present as leading factors perpetuating racial disparities in the treatment of drug addiction—with Black and Native American patients more likely from areas with high community distress (Pro et al., 2022; Ivanich et al., 2021). Moreover, racism in healthcare contributes to inequitable treatment access among Black and American Indian/Alaska Native individuals. These populations receive worse care in upwards of 40% of measures of quality (Maina et al., 2018). Specific to drug overdoses, research by Charron et al. (2019) found that Non-Hispanic Black individuals hospitalized for a non-fatal drug overdose were significantly less likely to be discharged to psychiatric facilities than Non-Hispanic White individuals also hospitalized for a non-fatal overdose. There is an urgent need to better address structural racism and systematic discrimination alongside the social determinants of health to inform and implement culturally competent substance use treatment initiatives to curb the drug overdose epidemic among minoritized populations.
Limitations and Strengths
Our study findings should be interpreted in the context of several important limitations. While this study utilized multiple years of national drug overdose data, assessing age by race/ethnicity-specific overdose deaths created data suppression for some racial/ethnic groups in the sub-analysis of the top 10 states. Second, we could not assess age-specific overdose death rates for those who identify as multiracial as this data is not available in CDC Wonder. We also use 2020 as the pandemic year; while an official pandemic declaration had not been issued pre-April, there were clear signs that the pandemic was ensuing in the U.S. and worldwide. In addition, we are limited by the availability of data, and the analysis of monthly deaths focusing on changes since the onset of the COVID-19 pandemic would require synthetic controls or causal modeling, which is beyond the scope of our article, and worthy of attention by itself. Moreover, we do not have individual-level and other contextualizing data that could provide insight into these age and race patterns observed. Even with these limitations, to our knowledge, this is the first study to assess race/ethnicity by age group differences in all national drug overdose deaths, along with using the drug overdose mortality data from 2020 the first year of the COVID-19 pandemic.
Conclusion
Overdose deaths pre-COVID-19, between 2015–2019, are unprecedently concentrated among older Black adults and American Indian/Alaska Natives of most ages compared to same-aged White individuals, a pattern exacerbated in the first year of the COVID-19 pandemic. Interventions for substance use disorders, expanding telemedicine-based buprenorphine programs, and naloxone-based overdose prevention programs for older Black adults and American Indian/Alaska Natives are crucial. Failure to do so will continue to have dire ramifications for the health and well-being of these communities. Future studies are needed to examine contextual factors leading to the disproportionately high rates of drug overdose deaths among older Black adults and American Indian/Alaska Natives, along with the impact of COVID-19 related to social isolation, tainted supply, and other health issues known to co-occur with fatal and non-fatal drug overdoses.
Supplementary Material
Highlights.
We assess age-specific mortality rates in overdose deaths by race/ethnicity
We use CDC Wonder data to produce nationally generalizable results and across time
Overdoses are elevated among older Non-Hispanic Black adults and Indigenous populations
Findings indicate that period effects shape mortality dynamics for NH-White decedents
Findings suggest that cohort effects shape mortality dynamics for NH-Black decedents
Funding:
K01DA051715 (P.I.: Jones)
Footnotes
Conflict of Interests: Abenaa Jones (None) Alexis Santos (None), Amaya Perez-Brumer (None), Carl Latkin (None), Steve Shoptaw (None), Nabila El-Bassel (None)
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barboza GE, & Angulski K. (2020). A descriptive study of racial and ethnic differences of drug overdoses and naloxone administration in Pennsylvania. International Journal of Drug Policy, 78, 102718. [DOI] [PubMed] [Google Scholar]
- Brave Heart MYH, Chase J, Elkins J, & Altschul DB (2011). Historical trauma among indigenous peoples of the Americas: Concepts, research, and clinical considerations. Journal of Psychoactive drugs, 43(4), 282–290. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Drug Overdose Deaths in the U.S. Up 30% in 2020 (2021a) https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20210714.htm
- Centers for Disease Control and Prevention. CDC Wonder - Underlying Cause of Death, 1999–2019. (2021b) http://wonder.cdc.gov/
- Centers for Disease Control and Prevention. Drug Overdose Mortality by State. (2021c.) https://www.cdc.gov/nchs/pressroom/sosmap/drug_poisoning_mortality/drug_poisoning.htm
- Charron E, Francis EC, Heavner-Sullivan SF, & Truong KD (2019). Disparities in access to mental health services among patients hospitalized for deliberate drug overdose. Psychiatric Services, 70(9), 758–764. [DOI] [PubMed] [Google Scholar]
- Cox ME, Smith MA, Patel AR, Proescholdbell S, & Bell RA (2021). Sidebar: Community-driven Approaches to Preventing Overdoses Among American Indians. North Carolina Medical Journal, 82(6), 409–411. [DOI] [PubMed] [Google Scholar]
- Cremer LJ, Board A, Guy G, Schieber L, Asher A, & Parker EM (2021). Trends in Pharmacy-Based Dispensing of Buprenorphine, Extended-Release Naltrexone, and Naloxone During the COVID-19 Pandemic by Age and Sex–United States, March 2019–December 2020. Drug and Alcohol Dependence, 109192. [DOI] [PMC free article] [PubMed]
- Dayton L, Tobin K, Falade-Nwulia O, Davey-Rothwell M, Al-Tayyib A, Saleem H, & Latkin C. (2020). Racial disparities in overdose prevention among people who inject drugs. Journal of Urban Health, 97,823–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman J, & Hansen H. (2022). Far From a “White Problem”: Responding to the Overdose Crisis as a Racial Justice Issue. American Journal of Public Health, 112(S1), S30-S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furr‐Holden D, Milam AJ, Wang L, & Sadler R. (2021). African Americans now outpace whites in opioid‐involved overdose deaths: a comparison of temporal trends from 1999 to 2018. Addiction, 116(3), 677–683. [DOI] [PubMed] [Google Scholar]
- Gross Jonathan. (2020). Update on the Opioid Epidemic in Baltimore City. Baltimore City Health Department Epidemiological Services. https://health.baltimorecity.gov/node/23
- Han B, Compton WM, Jones CM, Einstein EB, Volkow ND. (2021). Methamphetamine Use, Methamphetamine Use Disorder, and Associated Overdose Deaths Among U.S. Adults. JAMA Psychiatry 78(12), 1329–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han BH, Tuazon E, Kunins HV, Mantha S, & Paone D. (2019). Unintentional drug overdose deaths involving cocaine among middle-aged and older adults in New York City. Drug and Alcohol Dependence, 198, 121–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris R, Rosecrans A, Zoltick M, Willman C, Saxton R, Cotterell M, Bell J, Blackwell I, & Page KR (2022). Utilizing telemedicine during COVID-19 pandemic for a low-threshold, street-based buprenorphine program. Drug and Alcohol Dependence, 230, p.109187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Miniño AM, & Warner M. Drug overdose deaths in the United States, 1999–2018. (2020). https://www.cdc.gov/nchs/data/databriefs/db394-H.pdf [PubMed]
- Ivanich JD, Weckstein J, Nestadt PS, Cwik MF, Walls M, Haroz EE, O’Keefe VM, Goklish N, & Barlow A. (2021). Suicide and the opioid overdose crisis among American Indian and Alaska Natives: a storm on two fronts demanding swift action. The American Journal of Drug and Alcohol Abuse, 47(5), 527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, & Burke DS (2018). Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science, 361(6408), eaau1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones AA, Schneider KE, Brighthaupt SC, Johnson JK, Linton SL, & Johnson RM (2019). Heroin and nonmedical prescription opioid use among high school students in urban school districts. Drug and Alcohol Dependence;205,107664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones AA, Park JN, Allen ST, Schneider KE, Weir BW, Hunt D, & Sherman SG (2021). Racial differences in overdose training, naloxone possession, and naloxone administration among clients and nonclients of a syringe services program. Journal of Substance Abuse Treatment, 129, 108412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones AA, Schneider KE, Mahlobo CT, Maggs JL, Dayton L, Tobin KE, & Latkin CA (2022). Fentanyl overdose concerns among people who inject drugs: The role of sex, racial minority status, and overdose prevention efforts. Psychology of Addictive Behaviors. [DOI] [PMC free article] [PubMed]
- Lagisetty PA, Ross R, Bohnert A, Clay M, & Maust DT (2019). Buprenorphine treatment divide by race/ethnicity and payment. JAMA Psychiatry, 76(9), 979–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippold KM, Jones CM, Olsen EOM, & Giroir BP (2019). Racial/ethnic and age group differences in opioid and synthetic opioid–involved overdose deaths among adults aged≥ 18 years in metropolitan areas—United States, 2015–2017. Morbidity and Mortality Weekly Report, 68(43), 967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maina IW, Belton TD, Ginzberg S, Singh A, & Johnson TJ (2018). A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Social Science & Medicine, 199, 219–229. [DOI] [PubMed] [Google Scholar]
- Mason M, Soliman R, Kim HS, & Post LA (2022). Disparities by sex and race and ethnicity in death rates due to opioid overdose among adults 55 years or older, 1999 to 2019. JAMA Network Open, 5(1), e2142982-e2142982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milam AJ, Furr-Holden D, Wang L, & Simon KM (2021). Health data disparities in opioid-involved overdose deaths from 1999 to 2018 in the United States. American Journal of Public Health, 111(9), 1627–1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York City Department of Health and Mental Hygiene. Unintentional Drug Poisoning (Overdose) Deaths in New York City in 2019. (2020). https://www1.nyc.gov/assets/doh/downloads/pdf/epi/databrief122.pdf
- Panchal N, Garfield R, Cox C, & Artiga S. Substance Use Issues Are Worsening Alongside Access to Care. Kaiser Family Foundation. (2021). https://www.kff.org/policywatch/substance-use-issues-are-worsening-alongside-access-to-care [Google Scholar]
- Pro G, Hayes C, Brown CC, Goree J, & Zaller N. (2022). Individual and Health Policy Factors Associated With Positive Heroin and Opioid Treatment Response: United States, 2018. American Journal of Public Health, 112(S1), S66–S76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson J. (2021, January). CDC warns of surge in drug overdose deaths during COVID-19. In JAMA Health Forum (Vol. 2, No. 1, pp. e210001-e210001). American Medical Association. [DOI] [PubMed] [Google Scholar]
- Wrigley-Field E, Berry KM, Stokes AC, & Leider JP (2022). COVID-19 Vaccination and Racial/Ethnic Inequities in Mortality at Midlife in Minnesota. American Journal of Preventive Medicine. [DOI] [PMC free article] [PubMed]
- Volkow ND (2020). Collision of the COVID-19 and addiction epidemics. Annals of Internal Medicine, 173(1), 61–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.