Abstract
Disparities in SLE rates and outcomes have been attributed to genetic and hormonal factors, cigarette smoking and environmental pollutants. However, a growing body of research indicates that social determinants of health (SDH) also have substantial impact on the disparities that characterize SLE. According to the World Health Organization, SDH are defined as ‘the conditions in which people are born, grow, work, live, and age’, account for 30–55% of health outcomes, and adversely impact health outcomes among those of low socioeconomic status and stigmatized racial/ethnic groups. We reviewed the impact of key SDH on SLE presentation, management and outcomes, including income, education, neighbourhood factors, healthcare access, discrimination and social support. We found that adverse SDH conditions may lead to more severe SLE with increased morbidity and mortality, and that SDH affect SLE management by dictating the most feasible monitoring and treatment plan for each individual patient based on his or her specific life circumstances (for example, based on health insurance status, distance to nearest provider and/or drug affordability). SDH also have a significant impact on SLE outcomes, with worse disease and psychosocial outcomes associated with lower income level, lower educational attainment, disadvantaged neighbourhoods, lack of health insurance or public health insurance in the USA, travel burden to nearest provider, anti-Black racism and lower social support. Future efforts to improve the management and outcomes of patients with SLE must combat the societal, economic and political forces that perpetuate these inequities.
Rheumatology key messages.
Social determinants of health (SDH) have a substantial impact on the disparities that characterize SLE.
Adverse SDH conditions may lead to more severe SLE and may limit patients’ treatment options.
Worse SLE outcomes are associated with lower healthcare access, income, education and social support.
Introduction
SLE is a multisystem autoimmune disease that disproportionally affects demographic groups that have suffered from social, economic, political, and healthcare marginalization and oppression. SLE is 9 times more prevalent among females [1], with typical age of onset during reproductive years [2]. SLE is 2–4 times more common in non-White populations globally [3], and in the USA, up to 67% of patients with SLE are non-White [4–9]. Additionally, areas of the USA with the lowest county-level socioeconomic status (SES) have the highest prevalence of SLE, even after adjusting for age, sex and race/ethnicity [9].
Non-White patients are also more likely to have severe SLE. Though a rare disease with an estimated US prevalence of 161 000–322 000 adults [7], SLE is the fifth leading cause of death in the USA for Black and Hispanic females aged 15–24 years and the sixth leading cause of death for Black and Hispanic females aged 25–34 years [10]. Black, Asian/Pacific Islander and Hispanic patients with SLE have significantly higher rates of LN [11]. Black and Hispanic patients with LN are also more likely to progress to end-stage kidney disease (ESKD) [12, 13]. Further examples of racial/ethnic disparities in SLE include higher rates of pregnancy complications among Black and Hispanic women with SLE [14], worse physical functioning among Black patients with SLE [15], and higher death rates, occurring sooner after diagnosis and at a younger age, among Black patients with SLE [16].
Disparities in SLE rates and outcomes have been attributed to genetic and hormonal factors, cigarette smoking and environmental pollutants [17]. However, a growing body of research indicates that social determinants of health (SDH) also have a substantial impact on the disparities that characterize SLE [18]. According to the World Health Organization, SDH are defined as ‘the conditions in which people are born, grow, work, live, and age’, account for 30–55% of health outcomes, and adversely impact health outcomes among those of low SES [19] and stigmatized racial/ethnic groups [20]. This article will review the impact of key SDH on SLE presentation, management and outcomes, including income, education, neighbourhood factors, healthcare access, discrimination and social support.
Income
In multinational studies, lower income level and poverty have been found to be associated with multiple adverse outcomes in SLE, including increased disease activity, organ damage, mortality, depression, and work loss or disability, as well as decreased physical functioning and quality of life [21–31]. Higher levels of financial strain have also been associated with depression onset among 682 women with SLE in the US-based Lupus Outcomes Study [32]. A subset of patients from this study who were living in poverty frequently reported that they were only able to manage their SLE during disease flares given daily competing demands, such as food and housing insecurity [33].
Education
A growing body of research indicates that lower educational attainment is associated with poor SLE outcomes. In a study of 562 Canadian adults with SLE, those that did not complete high school had an increased risk of work disability (30% vs 14%, P = 0.0001) and increased disease activity at study enrolment, after adjusting for age, race/ethnicity and sex (P = 0.014) [34]. A Chinese study of 904 therapy-naïve patients with SLE demonstrated that after adjusting for age, sex and disease duration, lower educational level (<9 years) was associated with higher disease activity (P = 0.001) [35]. Lower educational attainment has also been associated with work loss, medication nonadherence, missed appointments, lower health-related quality of life, lower physical functioning, and increased depression and anxiety among patients with SLE [27, 36–40]. We hypothesize that the association between lower educational attainment and work disability or loss is due to the types of jobs that people with lower education hold, which may be difficult to perform with a chronic illness. Indeed, a 2022 systematic review of work participation among 3800 employed adults with SLE found that more physical jobs and low job control were associated with increased work loss or disability [29].
Neighbourhood factors
Bartels et al. found that Black patients with SLE were 10 times more likely to live in the most disadvantaged neighbourhoods as compared with White patients with SLE, which was the strongest predictor for poor retention in SLE care [41]. Other studies have found that SLE patients report neighbourhood crime as a stressor that leads to higher disease activity [33], racial segregation and low neighbourhood SES are associated with depression in SLE [27, 42], and HCQ adherence is lower in residential codes with a higher percentage of Black residents and a lower percentage of hospitals [43]. Among patients with SLE, rural residence has also been associated with higher disease activity [44, 45], renal disease [44], mucocutaneous and musculoskeletal manifestations [45], and depression [46]. We hypothesize that higher disease activity among rural SLE populations is associated with poorer access to specialized care.
Healthcare access
Multiple studies have demonstrated an association between lack of health insurance or public insurance and poor outcomes among patients with SLE in the USA. The association between public health insurance and adverse SLE outcomes has not been described outside of the USA [47] and may be related to the lack of universal healthcare and an underfunded public healthcare system within the USA. Patients with Medicare or Medicaid insurance have been shown to have higher rates of 30-day readmissions and preventable lupus hospitalizations as compared with privately insured patients with SLE [48–51]. Public insurance has also been associated with healthcare fragmentation (receipt of care across multiple institutions), which is itself associated with increased risk of infections, cardiovascular disease, LN, ESKD and stroke [52]. Among patients with paediatric-onset SLE, public insurance has been associated with a >6-fold increased risk of ESKD or death [53]. In US nationwide studies of patients with ESKD due to LN, Medicaid and uninsured patients are less likely to be referred for kidney transplant [54] and less likely to receive initial peritoneal dialysis [55]. In addition to insurance status, studies of patients with SLE have found that travel burden to receive SLE care may lead to missed appointments, medication nonadherence, and higher levels of anxiety and depression among patients with SLE [56–58].
Discrimination
In a study of 427 Black women with SLE residing in Atlanta [Black Women’s Experiences Living with Lupus (BeWELL), derived from the GOAL (Georgians Organized Against Lupus) cohort], higher frequency of self-reported experiences of racial discrimination in domains such as employment, housing and medical settings was associated with higher SLE activity and damage [59]. In follow-up studies from the BeWELL cohort, hearing about or observing (vicarious) racism was also associated with increased SLE activity, even after adjusting for personal experiences of racism [60]. There was also a significant association between anticipating racism and SLE activity, and smoking was found to exacerbate this association [61]. Psychological distress was found to mediate the relationship between racism-related stress and SLE disease activity in the BeWELL cohort [62].
Social support
Multiple international studies have demonstrated that lower levels of social support are associated with adverse mental health and disease outcomes in SLE. A survey-based study of 246 patients with SLE in China found that age <18 years, single marital status, unemployed status and higher damage were associated with lower levels of social support, and patients with lower social support had significantly more anxiety and depression [63]. In the GOAL cohort of 437 Black women with SLE, limited social support was significantly associated with depression (P < 0.001) [64]. An Egyptian cross-sectional study of 80 patients with SLE found that perception of worse neighbourhood social cohesion was associated with depressive symptoms and higher disease activity [46]. Other studies have found associations between lower levels of social support and lower health-related quality of life and mental health scores [65, 66]. Qualitative studies of patients with SLE have also demonstrated that many patients with SLE feel their disease is invisible to others and report inadequate SLE care and validation [67] as well as negative social support including denial of illness and unwanted advice from others [68, 69].
Conclusion
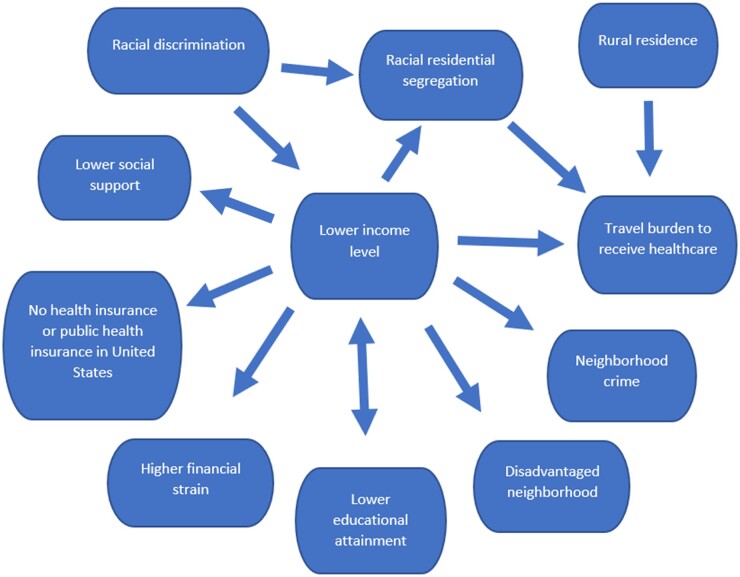
In summary, SDH interact in complex ways (Fig. 1) and play a key role in SLE presentation as adverse SDH conditions may lead to more severe disease. SDH also contribute to SLE management by dictating the most feasible monitoring and treatment plan for each individual patient based on his or her specific life circumstances (for example, based on health insurance status, distance to nearest provider and/or drug affordability). SDH also have a significant impact on SLE outcomes, with worse disease and psychosocial outcomes associated with lower income level, lower educational attainment, disadvantaged neighbourhoods, lack of health insurance or public health insurance in the USA, travel burden to nearest provider, anti-Black racism and lower social support. The associations between SDH and adverse SLE outcomes are summarized in Table 1. Future efforts to improve the management and outcomes of patients with SLE must combat the societal, economic and political forces that perpetuate these inequities.
Figure 1.
Directed acyclic graph of the relationships between social determinants of health factors
Table 1.
Social determinants of health (SDH) factors that have been associated with adverse SLE outcomes
| Adverse SLE outcome | SDH factor [References] |
|---|---|
| Increased SLE activity | Lower income level [27, 31] |
| Lower educational attainment [34, 35] | |
| Neighbourhood crime [33] | |
| Rural residence [44, 45] | |
| Racial discrimination [59–62] | |
| Lower social support [46] | |
| Increased SLE damage | Lower income level [21, 22, 25–28] |
| Racial discrimination [59] | |
| Lower social support [63] | |
| Mortality | Lower income level [21, 24, 26, 30] |
| US Medicaid or Medicare insurance [53] | |
| End-stage kidney disease | US Medicaid or Medicare insurance [53] |
| Lack of referral for kidney transplant | US Medicaid insurance or no insurance [54] |
| Failure to receive initial peritoneal dialysis | US Medicaid insurance or no insurance [55] |
| Decreased physical functioning | Lower income level [23, 27] |
| Lower educational attainment [27] | |
| Decreased quality of life | Lower income level [21] |
| Decreased health-related quality of life | Lower educational attainment [40] |
| Lower social support [65, 66] | |
| Depression | Lower income level [27] |
| Higher financial strain [32] | |
| Lower educational attainment [38, 39] | |
| Racial segregation [42] | |
| Disadvantaged neighbourhood [27] | |
| Rural residence [46] | |
| Travel burden to receive SLE care [56–58] | |
| Lower social support [63, 64] | |
| Anxiety | Lower educational attainment [38] |
| Travel burden to receive SLE care [56–58] | |
| Lower social support [63] | |
| Increased work disability or loss | Lower income level [29] |
| Lower educational attainment [34] | |
| Medication nonadherence | Lower educational attainment [36] |
| Racial segregation [43] | |
| Disadvantaged neighbourhood [43] | |
| Travel burden to receive SLE care [56–58] | |
| Missed appointments/poor retention in SLE care | Lower educational attainment [37] |
| Disadvantaged neighbourhood [41] | |
| Travel burden to receive SLE care [56–58] | |
| 30-day hospital readmissions | US Medicaid or Medicare insurance [48, 51] |
| Preventable lupus hospitalizations | US Medicaid or Medicare insurance [49, 50] |
| Healthcare fragmentation | US Medicaid or Medicare insurance [52] |
Contributor Information
Jessica N Williams, Division of Rheumatology, Department of Medicine, Emory University School of Medicine, Atlanta, GA, USA.
Cristina Drenkard, Division of Rheumatology, Department of Medicine, Emory University School of Medicine, Atlanta, GA, USA.
S Sam Lim, Division of Rheumatology, Department of Medicine, Emory University School of Medicine, Atlanta, GA, USA.
Data availability
No new data were generated or analyzed in support of this article.
Funding
This paper was published as part of a supplement financially supported by Janssen Medical Affairs Global Services, LLC, a part of the Janssen pharmaceutical companies of Johnson & Johnson.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1. Izmirly PM, Parton H, Wang L. et al. Prevalence of systemic lupus erythematosus in the united states: estimates from a meta-analysis of the centers for disease control and prevention national lupus registries. Arthritis Rheumatol 2021;73:991–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Division of Population Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention. https://www.cdc.gov/lupus/features/lupus-awareness/index.htm (15 July 2022, date last accessed).
- 3. Pons-Estel GJ, Alarcón GS, Scofield L, Reinlib L, Cooper GS.. Understanding the epidemiology and progression of systemic lupus erythematosus. Semin Arthritis Rheum 2010;39:257–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Somers EC, Marder W, Cagnoli P. et al. Population-based incidence and prevalence of systemic lupus erythematosus: the Michigan Lupus Epidemiology and Surveillance program. Arthritis Rheumatol 2014;66:369–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lim SS, Bayakly AR, Helmick CG. et al. The incidence and prevalence of systemic lupus erythematosus, 2002-2004: the Georgia Lupus Registry. Arthritis Rheumatol 2014;66:357–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Izmirly PM, Wan I, Sahl S. et al. The incidence and prevalence of systemic lupus erythematosus in New York County (Manhattan), New York: the Manhattan Lupus Surveillance Program. Arthritis Rheumatol 2017;69:2006–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Helmick CG, Felson DT, Lawrence RC. et al. ; National Arthritis Data Workgroup. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part I. Arthritis Rheum 2008;58:15–25. [DOI] [PubMed] [Google Scholar]
- 8. Dall’Era M, Cisternas MG, Snipes K. et al. The incidence and prevalence of systemic lupus erythematosus in San Francisco County, California: the California Lupus Surveillance Project. Arthritis Rheumatol 2017;69:1996–2005. [DOI] [PubMed] [Google Scholar]
- 9. Feldman CH, Hiraki LT, Liu J. et al. Epidemiology and sociodemographics of systemic lupus erythematosus and lupus nephritis among US adults with Medicaid coverage, 2000-2004. Arthritis Rheum 2013;65:753–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yen EY, Singh RR.. Brief report: lupus-an unrecognized leading cause of death in young females: a population-based study using nationwide death certificates, 2000-2015. Arthritis Rheumatol 2018;70:1251–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Maningding E, Dall’Era M, Trupin L, Murphy LB, Yazdany J.. Racial and ethnic differences in the prevalence and time to onset of manifestations of systemic lupus erythematosus: the California lupus surveillance project. Arthritis Care Res (Hoboken) 2020;72:622–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Contreras G, Lenz O, Pardo V. et al. Outcomes in African Americans and Hispanics with lupus nephritis. Kidney Int 2006;69:1846–51. [DOI] [PubMed] [Google Scholar]
- 13. Plantinga L, Lim SS, Patzer R. et al. Incidence of end-stage renal disease among newly diagnosed systemic lupus erythematosus patients: the Georgia lupus registry. Arthritis Care Res (Hoboken) 2016;68:357–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Clowse ME, Grotegut C.. Racial and ethnic disparities in the pregnancies of women with systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2016;68:1567–72. [DOI] [PubMed] [Google Scholar]
- 15. Kiani AN, Strand V, Fang H, Jaranilla J, Petri M.. Predictors of self-reported health-related quality of life in systemic lupus erythematosus. Rheumatology (Oxford) 2013;52:1651–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lim SS, Helmick CG, Bao G. et al. Racial disparities in mortality associated with systemic lupus erythematosus - Fulton and Dekalb counties, Georgia, 2002-2016. MMWR Morb Mortal Wkly Rep 2019;68:419–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Parks CG, de Souza Espindola Santos A, Barbhaiya M, Costenbader KH.. Understanding the role of environmental factors in the development of systemic lupus erythematosus. Best Pract Res Clin Rheumatol 2017;31:306–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lim SS, Drenkard C.. Understanding lupus disparities through a social determinants of health framework: the Georgians organized against lupus research cohort. Rheum Dis Clin North Am 2020;46:613–21. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 (15 July 2022, date last accessed).
- 20. Williams DR, Priest N, Anderson NB.. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol 2016;35:407–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. DeQuattro K, Yelin E.. Socioeconomic status, health care, and outcomes in systemic lupus erythematosus. Rheum Dis Clin North Am 2020;46:639–49. [DOI] [PubMed] [Google Scholar]
- 22. Mendoza-Pinto C, Méndez-Martínez S, Soto-Santillán P. et al. Socioeconomic status and organ damage in Mexican systemic lupus erythematosus women. Lupus 2015;24:1227–32. [DOI] [PubMed] [Google Scholar]
- 23. Hoge C, Bowling CB, Lim SS, Drenkard C, Plantinga LC.. Association of poverty income ratio with physical functioning in a cohort of patients with systemic lupus erythematosus. J Rheumatol 2020;47:983–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Peschken CA, Katz SJ, Silverman E. et al. ; Canadian Network for Improved Outcomes in Systemic Lupus Erythematosus (CaNIOS). The 1000 Canadian faces of lupus: determinants of disease outcome in a large multiethnic cohort. J Rheumatol 2009;36:1200–8. [DOI] [PubMed] [Google Scholar]
- 25. Yelin E, Trupin L, Yazdany J.. A prospective study of the impact of current poverty, history of poverty, and exiting poverty on accumulation of disease damage in systemic lupus erythematosus. Arthritis Rheumatol 2017;69:1612–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yelin E, Yazdany J, Trupin L.. Relationship between poverty and mortality in systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2018;70:1101–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Trupin L, Tonner MC, Yazdany J. et al. The role of neighborhood and individual socioeconomic status in outcomes of systemic lupus erythematosus. J Rheumatol 2008;35:1782–8. [PMC free article] [PubMed] [Google Scholar]
- 28. Cooper GS, Treadwell EL, St Clair EW, Gilkeson GS, Dooley MA.. Sociodemographic associations with early disease damage in patients with systemic lupus erythematosus. Arthritis Rheum 2007;57:993–9. [DOI] [PubMed] [Google Scholar]
- 29. Blomjous BS, Gajadin GRS, Voskuyl AE. et al. Work participation in patients with systematic lupus erythematosus: a systematic review. Rheumatology (Oxford) 2022;61:2740–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Alarcón GS, McGwin G Jr, Bastian HM. et al. ; LUMINA Study Group. Systemic lupus erythematosus in three ethnic groups. VII [correction of VIII]. Predictors of early mortality in the LUMINA cohort. Arthritis Rheum 2001;45:191–202. Erratum in: Arthritis Rheum 2001;45:306. [DOI] [PubMed] [Google Scholar]
- 31. Alarcón GS, McGwin G Jr, Sanchez ML. et al. Systemic lupus erythematosus in three ethnic groups. XIV. Poverty, wealth, and their influence on disease activity. Arthritis Rheum 2004;51:73–7. [DOI] [PubMed] [Google Scholar]
- 32. McCormick N, Trupin L, Yelin EH, Katz PP.. Socioeconomic predictors of incident depression in systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2018;70:104–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yelin E, Trupin L, Bunde J, Yazdany J.. Poverty, neighborhoods, persistent stress, and systemic lupus erythematosus outcomes: a qualitative study of the patients' perspective. Arthritis Care Res (Hoboken) 2019;71:398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. George A, Wong-Pack A, Peschken CA. et al. ; 1000 Canadian Faces of Lupus Investigators. Influence of education on disease activity and damage in systemic lupus erythematosus: data from the 1000 Canadian faces of lupus. Arthritis Care Res (Hoboken) 2017;69:124–32. [DOI] [PubMed] [Google Scholar]
- 35. Cheng Y, Li M, Zhao J. et al. ; CSTAR co-authors. Chinese SLE Treatment and Research Group (CSTAR) registry: VIII. Influence of socioeconomic and geographical variables on disease phenotype and activity in Chinese patients with SLE. Int J Rheum Dis 2018;21:716–24. [DOI] [PubMed] [Google Scholar]
- 36. Mehat P, Atiquzzaman M, Esdaile JM, AviÑa-Zubieta A, De Vera MA.. Medication nonadherence in systemic lupus erythematosus: a systematic review. Arthritis Care Res (Hoboken) 2017;69:1706–13. [DOI] [PubMed] [Google Scholar]
- 37. Son MB, Sergeyenko Y, Guan H, Costenbader KH.. Disease activity and transition outcomes in a childhood-onset systemic lupus erythematosus cohort. Lupus 2016;25:1431–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Auerbach C, Beckerman NL.. What social workers in health care should know about lupus: a structural equation model. Health Soc Work 2011;36:269–78. [DOI] [PubMed] [Google Scholar]
- 39. Knight AM, Trupin L, Katz P, Yelin E, Lawson EF.. Depression risk in young adults with Juvenile- and adult-onset lupus: twelve years of followup. Arthritis Care Res (Hoboken) 2018;70:475–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Elera-Fitzcarrald C, Fuentes A, González LA. et al. Factors affecting quality of life in patients with systemic lupus erythematosus: important considerations and potential interventions. Expert Rev Clin Immunol 2018;14:915–31. [DOI] [PubMed] [Google Scholar]
- 41. Bartels CM, Rosenthal A, Wang X. et al. Investigating lupus retention in care to inform interventions for disparities reduction: an observational cohort study. Arthritis Res Ther 2020;22:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Martz CD, Hunter EA, Kramer MR. et al. Pathways linking census tract typologies with subjective neighborhood disorder and depressive symptoms in the Black Women’s Experiences Living with Lupus (BeWELL) Study. Health Place 2021;70:102587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Feldman CH, Costenbader KH, Solomon DH, Subramanian SV, Kawachi I.. Area-level predictors of medication nonadherence among US Medicaid beneficiaries with lupus: a multilevel study. Arthritis Care Res (Hoboken) 2019;71:903–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pons-Estel GJ, Saurit V, Alarcon GS. et al. The impact of rural residency on the expression and outcome of systemic lupus erythematosus: data from a multiethnic Latin American cohort. Lupus 2012;21:1397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Gergianaki I, Fanouriakis A, Adamichou C. et al. Is systemic lupus erythematosus different in urban versus rural living environment? Data from the Cretan Lupus Epidemiology and Surveillance Registry. Lupus 2019;28:104–13. [DOI] [PubMed] [Google Scholar]
- 46. Abdul-Sattar AB, Abou El Magd S.. Association of perceived neighborhood characteristics, socioeconomic status and rural residency with health outcomes in Egyptian patients with systemic lupus erythematosus: one center study. Int J Rheum Dis 2017;20:2045–52. [DOI] [PubMed] [Google Scholar]
- 47. Carter EE, Barr SG, Clarke AE.. The global burden of SLE: prevalence, health disparities and socioeconomic impact. Nat Rev Rheumatol 2016;12:605–20. [DOI] [PubMed] [Google Scholar]
- 48. Yazdany J, Marafino BJ, Dean ML. et al. Thirty-day hospital readmissions in systemic lupus erythematosus: predictors and hospital- and state-level variation. Arthritis Rheumatol 2014;66:2828–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Brown EA, Gebregziabher M, Kamen DL, White BM, Williams EM.. Examining racial differences in access to primary care for people living with lupus: use of ambulatory care sensitive conditions to measure access. Ethn Dis 2020;30:611–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Brown EA, Dismuke-Greer CE, Ramakrishnan V, Faith TD, Williams EM.. Impact of the affordable care act Medicaid expansion on access to care and hospitalization charges for lupus patients. Arthritis Care Res (Hoboken) 2020;72:208–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Najjar R, Alexander SA, Hughes GC, Yazdany J, Singh N.. Predictors of thirty-day hospital readmissions in systemic lupus erythematosus in the US: a nationwide study. Arthritis Care Res (Hoboken) 2022. doi: 10.1002/acr.24900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Walunas TL, Jackson KL, Chung AH. et al. Disease outcomes and care fragmentation among patients with systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2017;69:1369–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bitencourt N, Makris UE, Solow EB. et al. Predictors of adverse outcomes in patients with systemic lupus erythematosus transitioning to adult care. Semin Arthritis Rheum 2021;51:353–9. [DOI] [PubMed] [Google Scholar]
- 54. Plantinga LC, Drenkard C, Patzer RE. et al. Sociodemographic and geographic predictors of quality of care in United States patients with end-stage renal disease due to lupus nephritis. Arthritis Rheumatol 2015;67:761–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Devlin A, Waikar SS, Solomon DH. et al. Variation in initial kidney replacement therapy for end-stage renal disease due to lupus nephritis in the United States. Arthritis Care Res (Hoboken) 2011;63:1642–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Williams EM, Ortiz K, Zhang J, Zhou J, Kamen D.. The systemic lupus erythematosus travel burden survey: baseline data among a South Carolina cohort. BMC Res Notes 2016;9:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. White AA, Smalls BL, Ba A. et al. The effect of travel burden on depression and anxiety in African American women living with systemic lupus. Healthcare (Basel) 2021;9:1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Williams EM, Ortiz K, Flournoy-Floyd M, Bruner L, Kamen D.. Systemic lupus erythematosus observations of travel burden: a qualitative inquiry. Int J Rheum Dis 2015;18:751–60. [DOI] [PubMed] [Google Scholar]
- 59. Chae DH, Martz CD, Fuller-Rowell TE. et al. Racial discrimination, disease activity, and organ damage: the Black Women’s Experiences Living With Lupus (BeWELL) study. Am J Epidemiol 2019;188:1434–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Martz CD, Allen AM, Fuller-Rowell TE. et al. Vicarious racism stress and disease activity: the Black Women’s Experiences Living with Lupus (BeWELL) Study. J Racial Ethn Health Disparities 2019;6:1044–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Spears EC, Allen AM, Chung KW. et al. Anticipatory racism stress, smoking and disease activity: the Black women's experiences living with lupus (BeWELL) study. J Behav Med 2021;44:760–71. [DOI] [PubMed] [Google Scholar]
- 62. Hunter EA, Spears EC, Martz CD. et al. Racism-related stress and psychological distress: Black Women’s Experiences Living with Lupus study. J Health Psychol 2021;26:2374–89. [DOI] [PubMed] [Google Scholar]
- 63. Xu Q, Liu D, Zeng F. et al. [Social support and management strategies for chronic disease in patients with systemic lupus erythematosus]. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2019;44:67–73. [DOI] [PubMed] [Google Scholar]
- 64. Jordan J, Thompson NJ, Dunlop-Thomas C, Lim SS, Drenkard C.. Relationships among organ damage, social support, and depression in African American women with systemic lupus erythematosus. Lupus 2019;28:253–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Bae SC, Hashimoto H, Karlson EW, Liang MH, Daltroy LH.. Variable effects of social support by race, economic status, and disease activity in systemic lupus erythematosus. J Rheumatol 2001;28:1245–51. [PubMed] [Google Scholar]
- 66. Zheng Y, Ye DQ, Pan HF. et al. Influence of social support on health-related quality of life in patients with systemic lupus erythematosus. Clin Rheumatol 2009;28:265–9. [DOI] [PubMed] [Google Scholar]
- 67. Brennan KA, Creaven AM.. Living with invisible illness: social support experiences of individuals with systemic lupus erythematosus. Qual Life Res 2016;25:1227–35. [DOI] [PubMed] [Google Scholar]
- 68. Leung J, Ra J, Baker EA, Kim AHJ.. “…Not Having the Real Support That We Need”: patients’ experiences with ambiguity of systemic lupus erythematosus and erosion of social support. ACR Open Rheumatol 2019;1:135–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Mazzoni D, Cicognani E.. Problematic social support from patients’ perspective: the case of systemic lupus erythematosus. Soc Work Health Care 2014;53:435–45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analyzed in support of this article.