Abstract
Purpose: Enhanced recovery after surgery (ERAS) is a surgical rehabilitation protocol of increasing interest to clinicians in recent years, with the aim of faster and better recovery of patients after surgery. Our main focus in this review is to analyze the effectiveness of ERAS rehabilitation protocols in orthopedic surgery. By comparing the post-operative recovery of patients receiving the ERAS rehabilitation program with that of patients receiving the conventional rehabilitation program, we observed whether the patients who have received the ERAS rehabilitation program could recover better and faster, thereby achieving the aim of a shorter hospital stay and reducing the incidence of complications. Methods: We conducted the literature searches in PubMed, MEDLINE, Web of Science, Cochrane Reviews, EMBASE and other databases on clinical studies related to orthopedic surgery regarding the effectiveness of rehabilitation using ERAS rehabilitation protocols compared with conventional rehabilitation protocols. A systematic review was performed in accordance with the Preferred Reporting Items of Systematic Reviews and Meta-analysis (PRISMA) statement. If there was variability in the rehabilitation data of the patients between the two subgroups, it was considered that there was a difference in the rehabilitation effect of the ERAS rehabilitation protocol and the conventional rehabilitation protocol on the patients. Conclusion: The application of ERAS rehabilitation protocols can shorten patients’ hospital stay and reduce their expenses. In addition, patients with ERAS rehabilitation protocols will have fewer postoperative complications, while patients will have less postoperative pain than those with conventional rehabilitation, facilitating better postoperative recovery.
Keywords: enhanced recovery after surgery, orthopedics, surgery, rehabilitation, systematic review
1. Introduction
Orthopedics as one of the important component departments of a general hospital, whether it is for patients with fractures, joint replacements, or spine surgery. The surgical trauma for the patient is often large and is prone to corresponding complications, which can have a definite impact on the patient’s psychological and physical function. Therefore, the rehabilitation of patients after orthopedic surgery is very important. Good rehabilitation can go a long way towards improving the patient’s prognosis and facilitating the corresponding functional recovery after surgery. It can also play an important role in maintaining the patient’s psychological well-being. If a rapid recovery plan can be developed for patients in the perioperative period from preoperative to postoperative, in order to reduce the length of hospitalization, better restore the patient’s limb function, and reduce postoperative complications, it can promote both orthopedic surgery and improve the patient’s treatment outcome and psychological recovery. It is of great clinical significance to promote the rehabilitation of patients after orthopedic surgery.
Enhanced Recovery After Surgery (ERAS) is a multimodal, interdisciplinary care improvement program designed to facilitate the recovery of patients who have undergone surgery during the perioperative period; the purpose is to shorten the length of hospital stay and reduce complications [1,2]. The ERAS rehabilitation program is a rehabilitation treatment measure that has been increasingly used in the perioperative period for patients in recent years, and its rehabilitation outcomes have gotten more widely recognized. Evidence-based standardization of the perioperative management of surgical patients through the implementation of ERAS programs to improve outcomes is the most important clinical aim.
The enhanced recovery after surgery (ERAS) program is increasingly used in orthopedic surgery. In an ERAS rehabilitation progr for orthopedic related surgery, the medical members involved usually consist of orthopedic specialists, nurses, anesthetists and rehabilitation staff. The ERAS rehabilitation program involves a series of components that combine to minimize stress and to facilitate the return of function: these include integrated pre-operative, intra-operative and post-operative management [3,4]. The preoperative management includes mainly educational programs, nutritional management, dietary management, sleep management and pain management; the intraoperative treatment includes four main aspects: selection of anesthesia, goal directed fluid therapy, temperature management and infection prevention [5]; the postoperative management includes five main aspects: pain management, rehydration management, drainage management, nausea and vomiting control and activity management [6,7,8]. The purpose of the perioperative ERAS rehabilitation program is to enhance the patient’s postoperative recovery, reduce complications, and shorten the length of hospital stay.
In order to comprehensively analyze the application and rehabilitation outcomes of ERAS rehabilitation programs in orthopedic surgery, we collected and compared the rehabilitation outcomes between patients with ERAS rehabilitation programs and those with conventional rehabilitation programs in all directions of orthopedic surgery in this review. The advantages of the ERAS rehabilitation programs over conventional rehabilitation programs were investigated. The aim of our study is to promote the better use of ERAS rehabilitation programs in orthopedic surgery and to improve patient outcomes and postoperative recovery.
2. Methods
2.1. Literature Search
We strictly followed the Preferred Reporting Items of Systematic Reviews and Meta-analysis (PRISMA) statement in conducting the relevant literature searches [9,10]. The databases searched included PubMed, MEDLINE, Web of Science, Cochrane Reviews, EMBASE. As there are no studies on postoperative ERAS in orthopedics before 1960, so the time frame for the search is from 1960 to 30 August 2022. Methods for including and excluding articles include reading the title and abstract of the article and excluding the articles that do not meet the criteria. Then we carefully read the specific content of the remaining articles, further excluded the articles that do not meet the standards, and finally determined the specific articles to be included.
2.2. Inclusion and Exclusion Criteria
We developed the following inclusion criteria based on the needs of the study: (1) published peer-reviewed reports of human studies in English; (2) publication dates between database creation and 30 August 2022; (3) complete clinical reports; and (4) clinical subgroups of patients who were rehabilitated using ERAS and conventional rehabilitation, respectively.
The following are shown as exclusion criteria: (1) reviews, hypotheses, technical articles or oral reports; (2) non-English articles; (3) patients who have previously undergone surgery; (4) cadaveric or animal studies; (5) no control group; or (6) the control group received ERAS rehabilitation therapy after surgery.
2.3. Data Extraction and Quality Assessment
We first included and excluded articles by reading the title and abstract sections of the articles, eliminating those that did not meet the requirements, and then carefully read the full text of the remaining articles. The full text was read to exclude articles that did not meet the inclusion criteria, thus identifying articles that met the inclusion criteria. After we identified the final included literature, we arranged for two researchers to conduct a quality assessment of the included articles. After completion of a risk assessment for quality and bias, the articles were subjected to data extraction, which included the first author, year of publication, study design, study period, indication for surgery, sample size, number of patients in each control group, gender, mean age, type of intervention (ERAS rehabilitation program or conventional rehabilitation program), length of hospital stay, complication profile and visual analogue scale profile.
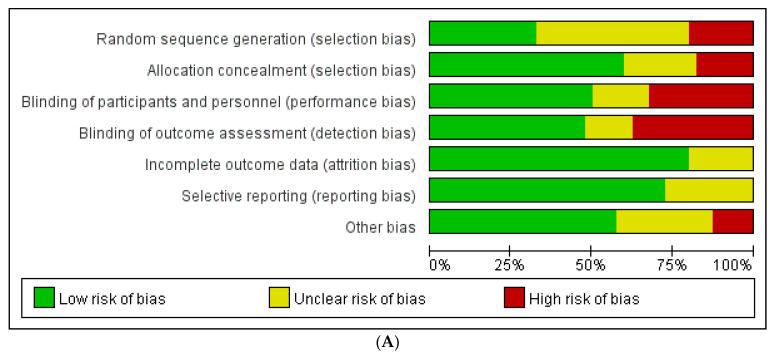
In addition, after data extraction was completed, the quality within each study was assessed. We assessed the literature for quality by referring to the assessment manual provided by the Cochrane system [11]; the tool used for quality assessment was Revman 5.4. Risk items assessed included random sequence, allocation concealment, blinding, completeness of outcome data, risk of selective reporting bias, and other biases. Each item was rated as ‘low risk’, ‘high risk’ or ‘uncertain risk’. A lower risk of bias indicates a higher quality of the included literature.
2.4. Statistical Analysis
The statistical analysis software used in our study was Stata SE-64. The main outcome indicators were compared between patients with the postoperative ERAS rehabilitation program and patients with the postoperative conventional rehabilitation program in order to analyze the differences in the postoperative rehabilitation of patients with the two different rehabilitation programs. A 95% confidence interval was used for the outcome indicators for the dichotomous variables to maintain consistency of analysis. Mean differences (MD) were expressed as 95% confidence intervals (95% CI) associated with continuous variables. If studies reported only the median, range, and size of the trial, we used the data reported in the paper to calculate the mean and standard deviation [12]. In addition, we have analyzed the heterogeneity of the included articles by I2 statistics. If the I2 value was 0% it indicated no heterogeneity, while I2 < 25% indicated low heterogeneity, the I2 value of 25–50% moderate heterogeneity and I2 > 50% high heterogeneity [13].
After counting the data from the included articles, we analyzed the data. The statistical analysis methods included fixed effect model and random effect model. When I2 < 50% indicated little heterogeneity within the literature, a fixed effects model (FE) was chosen to analyze the data. When I2 > 50% indicated significant heterogeneity within the literature, a random effects model (RE) was chosen to analyze the data. The differences between ERAS rehabilitation and conventional rehabilitation outcome indicators were analyzed according to the resulting forest plots. Statistical significance is considered if the p-value is <0.05.
According to the description in the respective articles, the patients who had used ERAS rehabilitation in the perioperative period were included in an ERAS rehabilitation group and those who did not receive ERAS rehabilitation were grouped into a conventional rehabilitation group. Among the included studies, we summarized and aggregated the various data provided in the article, in which the more frequently reported outcome indicators were length of hospitalization, postoperative complications, and patient-related postoperative pain scores (VAS). Therefore, the primary outcome indicators in our current analysis are length of stay and complications, and the secondary outcome indicator is pain score. In the included articles, all reported postoperative complications were included in the outcome index of complications, such as postoperative gastrointestinal bleeding, infection of the surgical opening, urinary tract infection, respiratory tract infection, thrombosis and other postoperative complications. The length of stay in hospital and the presence of complications were used to analyze the recovery of patients after undergoing orthopedic surgery together with the length of recovery time. The VAS pain score allowed us to analyze the pain of orthopedic patients after surgery.
3. Results
3.1. Identification of Included Studies
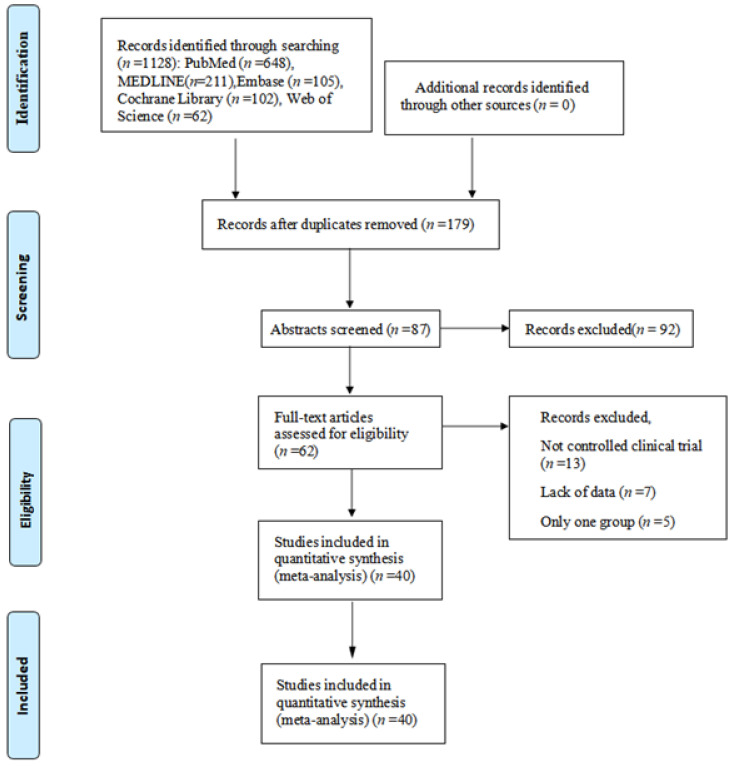
After excluding the articles that did not meet the inclusion criteria, a total of 40 articles were included. Of these articles, 11 are for fracture-related procedures [14,15,16,17,18,19,20,21,22,23,24]. There are 14 articles on joint replacement-related surgery [25,26,27,28,29,30,31,32,33,34,35,36,37,38] and 15 articles on spine surgery [39,40,41,42,43,44,45,46,47,48,49,50,51,52,53]. The relevant literature search and exclusion process is shown in Figure 1.
Figure 1.
The inclusion process of the literature search.
3.2. Quality Assessment of Included Studies
Of the 40 clinical studies included, 2 randomized controlled trials (RCT), 31 retrospective case-control studies, and 7 prospective cohort studies were included. A total of 29,856 patients were included in all articles, of which a total of 10,991 patients underwent surgery related to fracture, 3607 patients underwent surgery relating to the spine, and 15,258 patients underwent joint replacement surgery. Table 1, Table 2 and Table 3 show specific article characteristics and ratings. The assessed risk of bias in the included articles is shown in Figure 2A,B.
Table 1.
The basic characteristics of the included studies of fracture.
| Study (Ref.) | Type of Study |
Number of Participants | Age (Years) (Mean ± SD) | Intervention | Quality of the Literature |
Outcomes | |||
|---|---|---|---|---|---|---|---|---|---|
| Trial | Control | Trial | Control | Trial | Control | ||||
| Ping, 2021 [11] | Retrospective | 40 | 40 | 69.2 | 68.7 | ERAS | CR | 6 | C |
| Peng, 2021 [12] | Retrospective | 51 | 51 | 76.8 | 75.9 | ERAS | CR | 6 | C |
| Zhu, 2021 [13] | Retrospective | 92 | 98 | 78.1 | 77.3 | ERAS | CR | 7 | LOS, C |
| David, 2012 [14] | Retrospective | 117 | 115 | 82.5 | 82.7 | ERAS | CR | 7 | LOS, C |
| Mathurin, 2019 [15] | Prospective | 27 | 27 | 84.5 | 85.0 | ERAS | CR | 8 | LOS, C |
| Li, 2022 [16] | Prospective | 285 | 361 | 46.9 | 50.3 | ERAS | CR | 7 | LOS, C |
| Christian, 2019 [17] | Retrospective | 1140 | 1090 | 79.6 | 79.7 | ERAS | CR | 6 | LOS, C |
| Kristin, 2017 [18] | Retrospective | 1032 | 788 | 83.1 | 83.1 | ERAS | CR | 5 | LOS |
| Susanne, 2008 [19] | Retrospective | 178 | 357 | 83.9 | 84.2 | ERAS | CR | 6 | LOS, C |
| Yan, 2019 [20] | Prospective | 50 | 50 | 77.8 | 78.3 | ERAS | CR | 7 | LOS, C |
| Vincent, 2017 [21] | Retrospective | 2514 | 2488 | 63.2 | 62.1 | ERAS | CR | 6 | LOS, C |
ERAS: Enhanced recovery after surgery; CR: Conventional Rehabilitation; C: Complication; LOS: Length of hospitalization.
Table 2.
The basic characteristics of the included studies of joint replacement.
| Study (Ref.) | Type of Study |
Number of Participants | Age (Years) (Mean ± SD) | Intervention | Quality of the Literature |
Outcomes | |||
|---|---|---|---|---|---|---|---|---|---|
| Trial | Control | Trial | Control | Trial | Control | ||||
| Hong, 2019 [22] | Prospective | 106 | 141 | 74.2 | 75.4 | ERAS | CR | 7 | LOS, C, VAS |
| Cao, 2021 [23] | Retrospective | 183 | 178 | 66.1 | 66.0 | ERAS | CR | 6 | LOS, C |
| Li, 2020 [24] | Retrospective | 86 | 82 | 4.0 | 4.2 | ERAS | CR | 6 | LOS, C, VAS |
| Wei, 2021 [25] | Retrospective | 60 | 60 | 65.8 | 65.6 | ERAS | CR | 6 | LOS, C |
| Wang, 2019 [26] | RCT | 59 | 59 | 63.0 | 64.1 | ERAS | CR | 9 | LOS, C, VAS |
| Liao, 2022 [27] | Retrospective | 40 | 40 | 64.8 | 65.3 | ERAS | CR | 8 | C |
| Zhong, 2021 [28] | Prospective | 180 | 168 | 64.0 | 65.0 | ERAS | CR | 5 | LOS, C, VAS |
| Marinus, 2016 [29] | Retrospective | 100 | 100 | 66.7 | 65.4 | ERAS | CR | 6 | LOS, C |
| Wu, 2020 [30] | RCT | 16 | 16 | 35.6 | 31.7 | ERAS | CR | 9 | LOS, C, VAS |
| Wang, 2020 [31] | Retrospective | 91 | 105 | 66.7 | 67.0 | ERAS | CR | 7 | LOS, C |
| Xu, 2019 [32] | Retrospective | 1724 | 4923 | 66.6 | 66.7 | ERAS | CR | 5 | LOS, C, VAS |
| Zhang, 2022 [33] | Retrospective | 50 | 50 | 68.0 | 70.0 | ERAS | CR | 7 | C, VAS |
| Collett, 2021 [34] | Retrospective | 100 | 196 | 67.7 | 66.7 | ERAS | CR | 8 | C |
| Hong, 2020 [35] | Prospective | 1423 | 4902 | 66.7 | 66.6 | ERAS | CR | 7 | LOS |
ERAS: Enhanced recovery after surgery; CR: Conventional Rehabilitation; C: Complication; LOS: Length of hospitalization; VAS: Visual Analogue Scale.
Table 3.
The basic characteristics of the included studies of spine.
| Study (Ref.) | Type of Study |
Number of Participants | Age (Years) (Mean ± SD) | Intervention | Quality of the Literature |
Outcomes | |||
|---|---|---|---|---|---|---|---|---|---|
| Trial | Control | Trial | Control | Trial | Control | ||||
| Cui, 2022 [36] | Prospective | 46 | 54 | 79.1 | 79.2 | ERAS | CR | 5 | LOS, C, VAS |
| Adrien, 2021 [37] | Retrospective | 44 | 44 | 55.1 | 55 | ERAS | CR | 7 | LOS |
| Li, 2020 [38] | Retrospective | 91 | 169 | 69.6 | 73.3 | ERAS | CR | 6 | LOS, C |
| Wang, 2021 [39] | Retrospective | 60 | 60 | 47.9 | 46.6 | ERAS | CR | 8 | LOS, C, VAS |
| Gong, 2021 [40] | Retrospective | 46 | 45 | 55.2 | 56.8 | ERAS | CR | 8 | LOS, C |
| Bertrand, 2020 [41] | Retrospective | 271 | 268 | 49.5 | 47.3 | ERAS | CR | 7 | LOS, C |
| Wang, 2020 [42] | Retrospective | 95 | 95 | 72.4 | 70.8 | ERAS | CR | 7 | LOS, C |
| Li, 2021 [43] | Retrospective | 60 | 67 | 73.6 | 74.3 | ERAS | CR | 6 | LOS, C, VAS |
| Feng, 2019 [44] | Retrospective | 44 | 30 | 61 | 59 | ERAS | CR | 6 | LOS, C |
| Kristen, 2021 [45] | Retrospective | 39 | 78 | 15.0 | 14.3 | ERAS | CR | 5 | LOS, VAS |
| Zuo, 2021 [46] | Retrospective | 84 | 95 | 71.3 | 71.6 | ERAS | CR | 6 | LOS, C |
| Xue, 2022 [47] | Retrospective | 70 | 73 | 53.2 | 52.1 | ERAS | CR | 6 | LOS, C, VAS |
| Wang, 2022 [48] | Retrospective | 530 | 530 | 65.0 | 64.2 | ERAS | CR | 7 | C |
| Armagan, 2018 [49] | Retrospective | 183 | 267 | 61.0 | 60.0 | ERAS | CR | 6 | LOS |
| Li, 2018 [50] | Retrospective | 114 | 110 | 58.5 | 56.9 | ERAS | CR | 7 | LOS, C, VAS |
ERAS: Enhanced recovery after surgery; CR: Conventional Rehabilitation; C: Complication; LOS: Length of hospitalization; VAS: Visual Analogue Scale.
Figure 2.
(A): Risk of bias assessment in studies. (B): Risk of bias assessment in each study [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53].
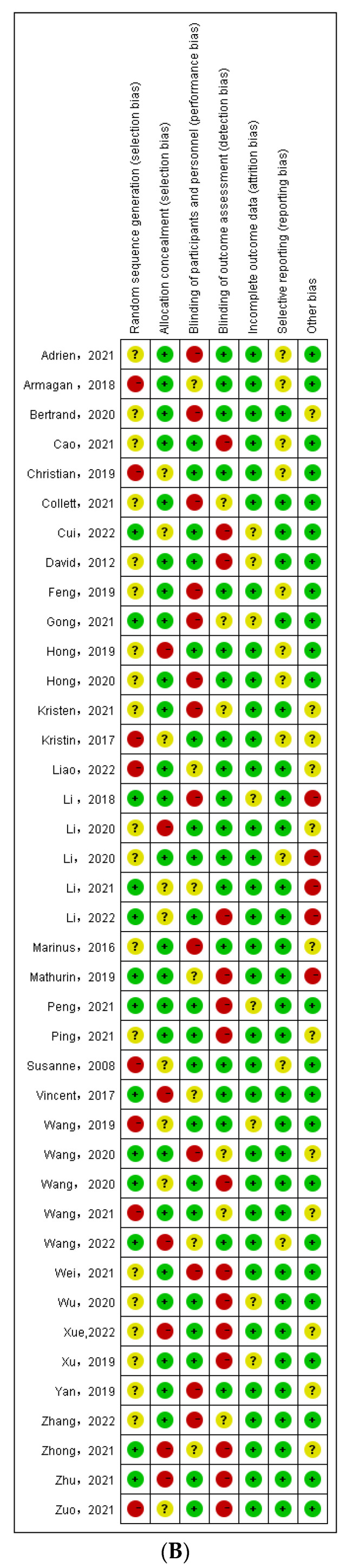
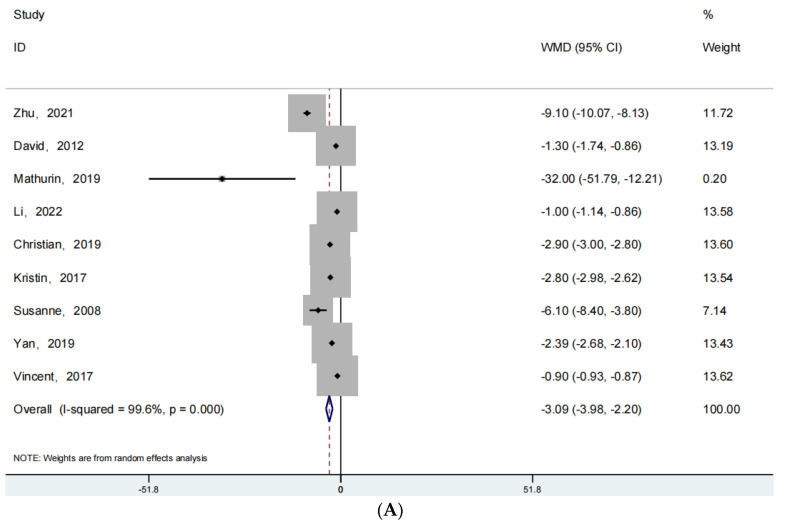
3.3. Length of Hospitalization
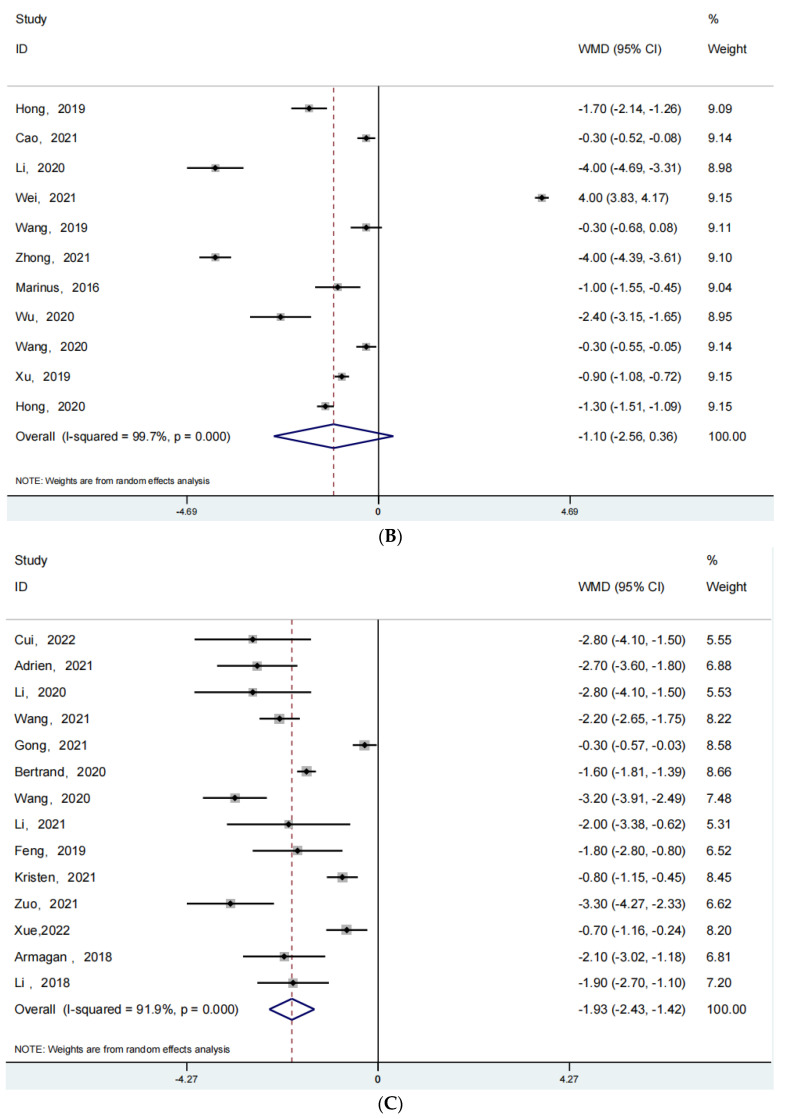
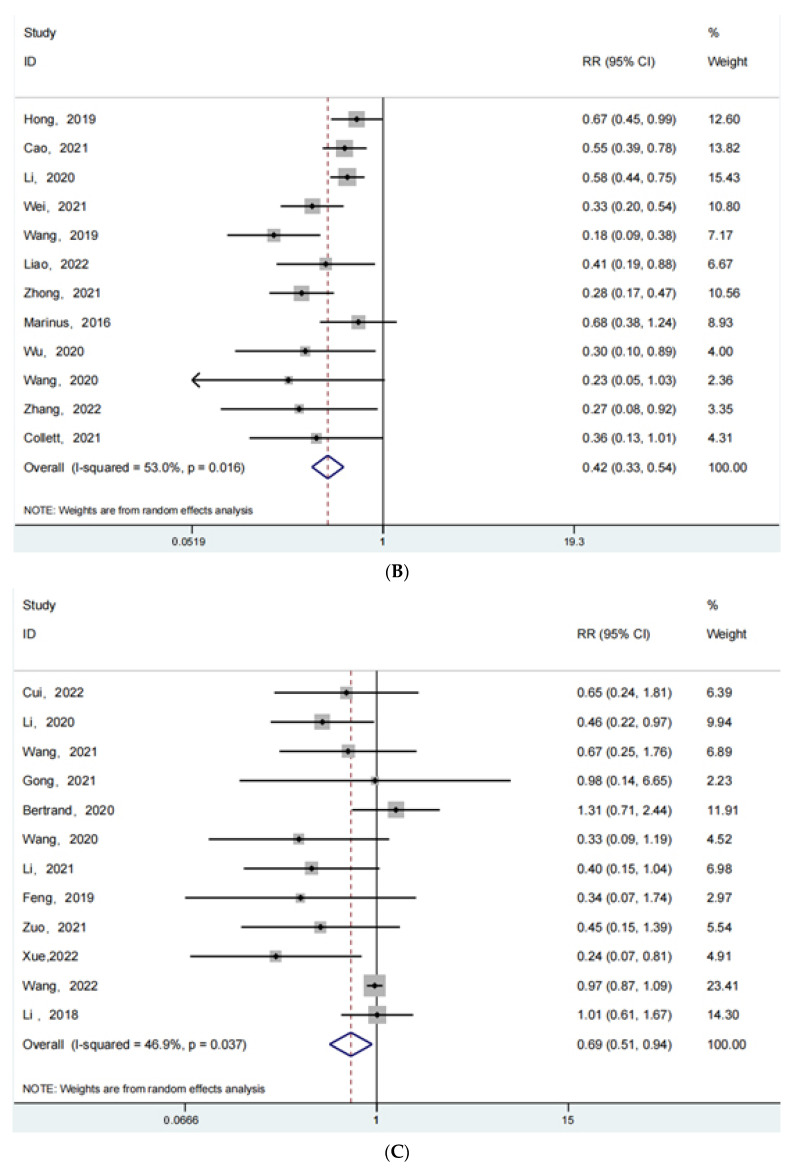
For the outcome indicator of length of stay, 9 articles were reported for fracture surgery, 11 articles for joint replacement surgery, and 14 articles for spine-oriented surgery. Figure 3 shows the forest plot obtained after our analysis of this data. Figure 3A shows the forest plot for fracture surgery (RR: −3.09; 95% Cl: −3.98, −2.20; p < 0.001, I2 = 99.6%), Figure 3B shows the forest plot related to joint replacement (RR: −1.30; 95% Cl: −2.56, 0.36; p = 0.141 > 0.05, I2 = 99.7%), and Figure 3C shows the forest plot related to spine orientation surgery-related forest plot (RR: −1.93; 95% Cl: −2.43, −1.42; p < 0.001, I2 = 91.9%). As for the analysis of the length of hospitalization, the length of hospital stay in patients with fracture or spinal surgery undergoing ERAS rehabilitation is found to be shorter than that of patients undergoing conventional rehabilitation, p < 0.05. There is no difference in the length of hospital stay for patients undergoing joint replacement regardless of the rehabilitation program.
Figure 3.
(A): The forest plot for fracture surgery of length of hospitalization. (B): The forest plot for joint replacement surgery of length of hospitalization. (C):The forest plot for spine surgery of length of hospitalization [25,26,27,28,29,30,31,32,33,34,35,36,37,38].
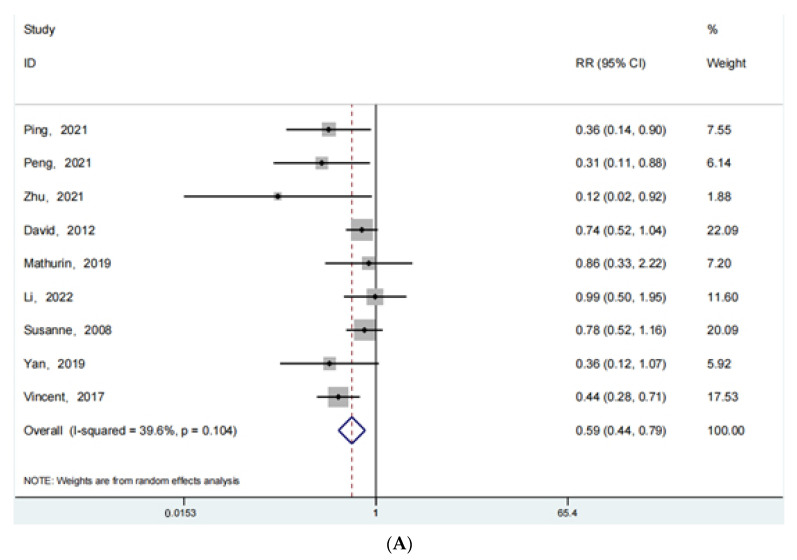
3.4. Complications
The clinical outcome of complications occurring after surgery was reported in 9 articles for fracture surgery, 13 articles for joint replacement surgery, and 12 articles for spine-oriented surgery. Figure 4 shows the forest plot obtained from the analysis of this data set. Figure 4A shows the forest plot for fracture surgery (RR: 0.59; 95% Cl: 0.44, 0.79; p < 0.001, I2 = 39.6%), Figure 4B shows the forest plot related to joint replacement (RR: 0.42; 95% Cl: 0.33, 0.54; p < 0.001, I2 = 53.0%), and Figure 4C shows the forest plot related to spine-oriented surgery (RR: 0.69; 95% Cl: 0.51, 0.94; p = 0.017 < 0.05, I2 = 46.9%). Regardless of the type of surgery (fracture, spine, joint), the postoperative complications were significantly less in patients receiving ERAS rehabilitation than in patients receiving conventional rehabilitation, p < 0.05. The use of ERAS rehabilitation can significantly reduce the occurrence of postoperative complications.
Figure 4.
(A): The forest plot for fracture surgery of complications. (B): The forest plot for joint replacement surgery of complications. (C):The forest plot for spine surgery of complications [39,40,41,42,43,44,45,46,47,48,49,50,51,52,53].
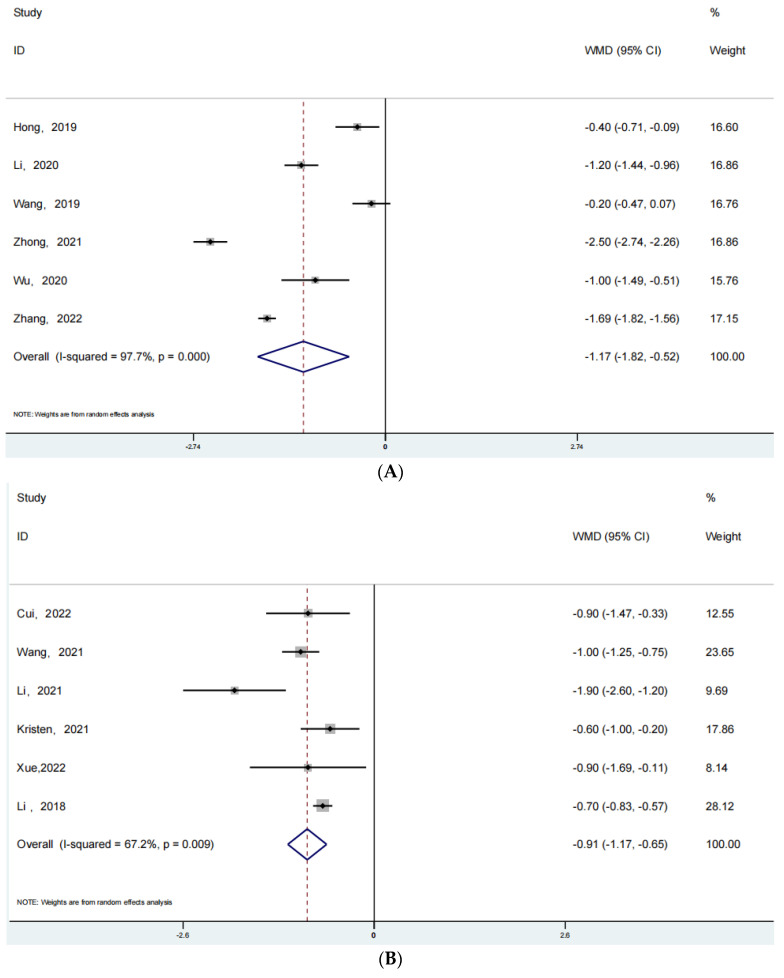
3.5. Visual Analogue Scale (VAS)
There are relatively few data on this indicator of VAS pain score, and only data related to joint replacement and spine surgery are summarized. A total of 6 of these articles were reported for joint replacement surgery and a total of 6 articles were reported for spine-oriented surgery. Figure 5 shows the forest plot we obtained after analyzing this data. Figure 5A shows the forest plot related to joint replacement (RR: −1.17; 95% Cl: −1.82, −0.52; p < 0.001, I2 = 97.7%) and Figure 5B shows the forest plot related to spine-oriented surgery (RR: −0.91; 95% Cl: −1.17, −0.65; p < 0.001, I2 = 67.2%). After joint replacement or spine-related surgery, the patients with ERAS rehabilitation have significantly lower pain scores than those in the conventional rehabilitation group.
Figure 5.
(A): The forest plot for joint replacement surgery of VAS. (B): The forest plot for spine surgery of VAS [39,40,41,42,43,44,45,46,47,48,49,50,51,52,53].
4. Discussion
According to the forest plots we obtained and the results of the analysis, there was no difference in the length of stay in patients who underwent joint replacement, either with the ERAS rehabilitation protocol or with the conventional rehabilitation protocol (p > 0.05). The LOS was approximately the same in both rehabilitation groups. However, there was a significant difference in postoperative complications between the two rehabilitation groups of patients in joint replacement surgery (p < 0.001). There was also significant variability in postoperative pain among arthroplasty patients who had received different rehabilitation protocols (p < 0.05). These results suggest that the patients who had received the ERAS rehabilitation program experienced less postoperative pain and complications than those who had received conventional rehabilitation. The use of the ERAS rehabilitation program can help patients to reduce the incidence of post-operative complications and reduce their pain and discomfort. This can go a long way in promoting better post-operative recovery for patients. There was no significant variability in the length of hospital stay for patients in the joint replacement group, which may be related to the patient’s age, underlying disease, psychological status, and intraoperative blood loss, which can lead to a longer postoperative hospital stay [54,55,56].
Overall, there were significant differences in outcome indicators, except for the length of hospital stay in joint replacement. In patients who had undergone fracture surgery and spine surgery, there was a significant difference in all outcome indicators between the ERAS rehabilitation group and patients in the conventional rehabilitation group (p < 0.05). The analysis results for patients who had undergone fracture surgery and spinal surgery show that the two different rehabilitation protocols had different effects on the patients’ post-operative recovery. The use of the ERAS rehabilitation program can help patients to recover better after surgery. These advantages are fully reflected in terms of length of stay, postoperative complications and VAS scores. The results of our analysis were consistent with those of some current studies. The ERAS rehabilitation program provides comprehensive rehabilitation management of patients before, during, and after surgery, and can improve postoperative outcomes, reduce complications, shorten hospital stays, and reduce the impact of postoperative pain in patients [4,57].
For the patients who had undergone joint replacement surgery, the length of stay in hospital was somewhat shorter for those with the ERAS rehabilitation program than for those in the conventional rehabilitation group. These results suggested that the ERAS rehabilitation can improve the patient’s post-operative condition and achieve the clinical requirements for discharge from hospital more quickly. These could show that the ERAS rehabilitation program can help patients recover better and faster, and thus return to normal life and work more quickly. For the patients in the ERAS rehabilitation group and the conventional rehabilitation group, there was a significant difference in post-operative complications and pain between the two. It could be that the two methods of rehabilitation have different factors affecting postoperative complications and pain,, or it may be that there were differences in the specific implementation process in the clinical setting which has an impact on the outcome. For example, the differences in the clinician’s surgical experience and technique, or differences in the specific pain relief protocols and pain medication used, may also have an impact on post-operative complications and pain. The impact of an ERAS rehabilitation program on complications, pain and even function after arthroplasty is a question that clinicians will need to consider and explore in the future, and deserves further evidence from more clinical trials.
In addition, as a multimodal management, the ERAS rehabilitation program can reduce the length of hospitalization of patients while also reducing the cost of patients’ expenses and reducing medical stress [58]. The results of related studies have also shown that the application of ERAS rehabilitation protocols not only reduces postoperative complications, but also decreases mortality and rehospitalization rates, improves joint and limb motility and neurological function, promotes muscle strength recovery, and improves patient prognosis more significantly [24,59]. For patients who had undergo the ERAS rehabilitation program, the pain symptoms that occur after surgery were much less severe. It can reduce the use of pain medication to some extent, thereby reducing some of the adverse effects associated with pain medication. In particular, reducing the use of addictive drugs such as opioid painkillers can greatly reduce some of the adverse reactions and complications caused by these drugs after surgery. This is of great clinical significance to the rapid and good recovery of patients after surgery [60,61,62]. To improve the postoperative status of orthopedic patients by reducing postoperative complications and pain is an aspect that clinicians need to pay attention to in the perioperative period. This can not only improve the overall therapeutic effect of patients, but also improve patients’ trust in doctors and form a habit of good medical compliance, which can play a positive role in promoting doctors’ clinical work. Therefore, the good application of the ERAS rehabilitation program may be a direction that doctors need to consider more in future clinical work.
Of course, there are still some concerns and controversies about some of the measures in the current ERAS rehabilitation program. For example, the ERAS Society often advocates a reduction in the use of anti-inflammatory analgesics along with early parenteral nutrition, which may increase the risk of postoperative inflammation. In terms of preventing post-operative thrombosis, the ERAS Society recommended that adequate thromboprophylaxis should be provided during the patient’s post-operative recovery period. Thromboprophylaxis can be gradually reduced and discontinued after the patient has fully resumed activity [63]. However, as some patients consider thromboprophylaxis to be non-essential, pharmacological thromboprophylaxis may increase the risk of bleeding. Adequate thromboprophylaxis may therefore partly lead to patient refusal [64]. Therefore, a well-developed ERAS rehabilitation program that allows patients to receive more comprehensive and complete management in the perioperative period, such as reducing the risk of postoperative thrombosis through preoperative intervention, may be more acceptable to patients. In addition, the ERAS Society strongly recommended the use of balanced crystalloids and avoidance of 0.9% saline, which may increase the incidence of postoperative hyperchloremia and hypotension [63]. For the above mentioned possible accompanying risks, potential adverse reactions can be avoided by adjusting the relevant steps. For example, the use of analgesic and anti-inflammatory drugs and infusion protocols can be adapted to the patient’s condition to achieve a better postoperative recovery while reducing the associated risks.
Based on our comprehensive analysis of postoperative patients in all directions of orthopedics, comprehensive rehabilitation management of patients by using ERAS in the perioperative period can provide clear benefits for patients. Compared to conventional rehabilitation, ERAS rehabilitation programs can significantly improve the overall postoperative condition of patients. Of course, in addition to improving length of stay, post-operative complications and pain, ERAS rehabilitation may also can improve other post-operative indicators for patients, such as the patient’s functional recovery and functional scores after surgery, the need for postoperative blood transfusions and the readmission rate after discharge. Improvements in all these indicators can make an important contribution to the patient’s postoperative recovery. More consideration can be given to the exploration of these indicators in future clinical studies on ERAS, together with a more comprehensive analysis of the benefits and drawbacks of ERAS rehabilitation programs for patients, thus promoting better clinical application of ERAS rehabilitation programs.
5. Limitations
Of course, there are some limitations to the current review. First, the vast majority of the included clinical research articles were retrospective, with fewer randomized controlled studies, which may have confounded the results. Second, the specific measures of ERAS rehabilitation protocols used by individual departments or hospitals vary to some extent and cannot be completely standardized, which may also cause bias in the final outcome.
6. Conclusions
In the perioperative period in all directions of orthopedics, the application of ERAS rehabilitation protocols can shorten the length of stay and reduce the cost of patients’ expenses compared to conventional rehabilitation protocols. In addition, patients benefiting from the ERAS rehabilitation program will have fewer postoperative complications, and patients will have less postoperative pain than those with conventional rehabilitation, which is more conducive to better postoperative recovery. Therefore, ERAS rehabilitation protocols deserve more consideration in the perioperative period for orthopedic patients.
Author Contributions
Conceptualization, J.L., J.T. and Z.Y.; investigation and data curation, G.B.; writing—original draft preparation, J.T. and Z.Y.; writing—review and editing, J.T. and Z.Y.; project administration, G.B. and H.Z., J.T. and Z.Y. contributed equally to this work. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
As for the Ethics Committee approval, since it is a review and not a research or intervention study involving humans, we normally do not ask for an Ethics Committee approval.
Informed Consent Statement
Not applicable.
Data Availability Statement
The articles and data are available on PubMed, MEDLINE, Web of Science, Cochrane Reviews, EMBASE, etc.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by Effects of kidney-tonifying Chinese herbs on epigenome and bone formation in osteogenic differentiation of BMSCs (Grant No: 20221129) in the form of covering the consultation fees of data statistical analysis. Hua Zhang received scientific funding from Effects of kidney-tonifying Chinese herbs on epigenome and bone formation in osteogenic differentiation of BMSCs (20221129).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Ljungqvist O. ERAS—Enhanced recovery after surgery: Moving evidence-based perioperative care to practice. J. Parenter. Enter. Nutr. 2014;38:559–566. doi: 10.1177/0148607114523451. [DOI] [PubMed] [Google Scholar]
- 2.Wainwright T.W., Gill M., McDonald D.A., Middleton R.G., Reed M., Sahota O., Yates P., Ljungqvist O. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop. 2019;91:3–19. doi: 10.1080/17453674.2019.1683790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rollins K.E., Lobo D.N., Joshi G.P. Enhanced recovery after surgery: Current status and future progress. Best Pract. Res. Clin. Anaesthesiol. 2020;35:479–489. doi: 10.1016/j.bpa.2020.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Soffin E.M., Wetmore D.S., Barber L.A., Vaishnav A.S., Beckman J.D., Albert T.J., Gang C.H., Qureshi S.A. An enhanced recovery after surgery pathway: Association with rapid discharge and minimal complications after anterior cervical spine surgery. Neurosurg. Focus. 2019;46:E9. doi: 10.3171/2019.1.focus18643. [DOI] [PubMed] [Google Scholar]
- 5.Wainwright T.W. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta Orthop. 2020;91:363. doi: 10.1080/17453674.2020.1724674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Debono B., Wainwright T.W., Wang M.Y., Sigmundsson F.G., Yang M.M., Smid-Nanninga H., Bonnal A., Le Huec J.-C., Fawcett W.J., Ljungqvist O., et al. Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Spine J. 2021;21:729–752. doi: 10.1016/j.spinee.2021.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Liu Z., Zhang J., He K., Zhang Y., Zhang Y. Optimized clinical practice for superaged patients with hip fracture: Significance of damage control and enhanced recovery program. Burn. Trauma. 2019;7:s41038-019-0159-y. doi: 10.1186/s41038-019-0159-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen K.K., Chan J.J., Zubizarreta N.J., Poeran J., Chen D.D., Moucha C.S. Enhanced recovery after surgery protocols in lower extremity joint arthroplasty: Using observational data to identify the optimal combination of components. J. Arthroplast. 2021;36:2722–2728. doi: 10.1016/j.arth.2021.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J. Clin. Epidemiol. 2021;134:178–189. doi: 10.1016/j.jclinepi.2021.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Kotz D., West R. Key concepts in clinical epidemiology: Addressing and reporting sources of bias in randomized controlled trials. J. Clin. Epidemiol. 2021;143:197–201. doi: 10.1016/j.jclinepi.2021.09.029. [DOI] [PubMed] [Google Scholar]
- 12.Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barili F., Parolari A., Kappetein P.A., Freemantle N. Statistical Primer: Heterogeneity, random- or fixed-effects model analyses?†. Interact. Cardiovasc. Thorac. Surg. 2018;27:317–321. doi: 10.1093/icvts/ivy163. [DOI] [PubMed] [Google Scholar]
- 14.Ping H., Ling X., Xue Y., Dong F. Effect of ERAS combined with comfortable nursing on quality of life and complications in femoral neck fractures of the aged people. Evid.-Based Complement. Altern. Med. 2021;2021:8753076. doi: 10.1155/2021/8753076. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Peng N., Li J. Application effect of case management mode combined with ERAS in elderly patients with hip fracture. Evid.-Based Complement. Altern. Med. 2021;2021:1175020. doi: 10.1155/2021/1175020. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 16.Zhu W., Yan Y., Sun Y., Fan Z., Fang N., Zhang Y., Yin M., Wan H., Mo W., Lu W., et al. Implementation of ENHANCED RECOVERY AFTER SURGERY (ERAS) protocol for elderly patients receiving surgery for intertrochanteric fracture: A propensity score-matched analysis. J. Orthop. Surg. Res. 2021;16:469. doi: 10.1186/s13018-021-02599-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Macfie D., Zadeh R.A., Andrews M., Crowson J., Macfie J. Perioperative multimodal optimisation in patients undergoing surgery for fractured neck of femur. Surgeon. 2012;10:90–94. doi: 10.1016/j.surge.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 18.Gomez M., Marc C., Talha A., Ruiz N., Noublanche S., Gillibert A., Bergman S., Rony L., Maynard V., Hubert L., et al. Fast track care for pertrochanteric hip fractures: How does it impact length of stay and complications? Orthop. Traumatol. Surg. Res. 2019;105:979–984. doi: 10.1016/j.otsr.2019.04.017. [DOI] [PubMed] [Google Scholar]
- 19.Li T., Sun Z.-J., Zhou Y., Sun W.-T., Wang P.-C., Cai X.-Y., Liang J.-B., Dong J.-M., Zhou D.-P., Yu K., et al. Perioperative protocol of ankle fracture and distal radius fracture based on enhanced recovery after surgery program: A multicenter prospective clinical controlled study. Pain Res. Manag. 2022;2022:3458056. doi: 10.1155/2022/3458056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pollmann C.T., Røtterud J.H., Gjertsen J.E., Dahl F.A., Lenvik O., Årøen A. Fast track hip fracture care and mortality—An observa-tional study of 2230 patients. BMC Musculoskelet. Disord. 2019;20:248. doi: 10.1186/s12891-019-2637-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haugan K., Johnsen L.G., Basso T., Foss O.A. Mortality and readmission following hip fracture surgery: A retrospective study comparing conventional and fast-track care. BMJ Open. 2017;7:e015574. doi: 10.1136/bmjopen-2016-015574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pedersen S.J., Borgbjerg F.M., Schousboe B., Pedersen B.D., Jørgensen H.L., Duus B.R., Lauritzen J.B., Hip Fracture Group of Bispebjerg Hospital A Comprehensive Hip Fracture Program Reduces Complication Rates and Mortality. J. Am. Geriatr. Soc. 2008;56:1831–1838. doi: 10.1111/j.1532-5415.2008.01945.x. [DOI] [PubMed] [Google Scholar]
- 23.Kang Y., Liu J., Chen H., Ding W., Chen J., Zhao B., Yin X. Enhanced recovery after surgery (ERAS) in elective intertrochanteric fracture patients result in reduced length of hospital stay (LOS) without compromising functional outcome. J. Orthop. Surg. Res. 2019;14:209. doi: 10.1186/s13018-019-1238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu V.X., Rosas E., Hwang J., Cain E., Foss-Durant A., Clopp M., Huang M., Lee D.C., Mustille A., Kipnis P., et al. Enhanced Recovery after surgery program implementation in 2 surgical populations in an integrated health care delivery system. JAMA Surg. 2017;152:e171032. doi: 10.1001/jamasurg.2017.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jiang H., Jian X., Shangguan Y., Qing J., Chen L. Effects of enhanced recovery after surgery in total knee arthroplasty for patients older than 65 years. Orthop. Surg. 2019;11:229–235. doi: 10.1111/os.12441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cao G., Xiang S., Yang M., Quan S., Yao J., Cai L., Feng W., Yang X., Xu H., Huang Z., et al. Risk factors of opioid use associated with an enhanced-recovery programme after total knee arthroplasty. BMC Musculoskelet. Disord. 2021;22:1046. doi: 10.1186/s12891-021-04937-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li J., Rai S., Ze R., Tang X., Liu R., Hong P. Enhanced recovery care versus traditional non-ERAS care following osteotomies in developmental dysplasia of the hip in children: A retrospective case-cohort study. BMC Musculoskelet. Disord. 2020;21:234–237. doi: 10.1186/s12891-020-03243-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wei B., Tang C., Li X., Lin R., Han L., Zheng S., Xu Y., Yao Q., Wang L. Enhanced recovery after surgery protocols in total knee arthroplasty via midvastus approach: A randomized controlled trial. BMC Musculoskelet. Disord. 2021;22:856. doi: 10.1186/s12891-021-04731-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang H.-Y., Wang L., Luo Z.-Y., Wang D., Tang X., Zhou Z., Pei F.-X. Intravenous and subsequent long-term oral tranexamic acid in enhanced-recovery primary total knee arthroplasty without the application of a tourniquet: A randomized placebo-controlled trial. BMC Musculoskelet. Disord. 2019;20:478. doi: 10.1186/s12891-019-2885-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liao X., Xu X. The effect of cold therapy combined with ERAS in the postoperative care of patients undergoing total knee arthroplasty. Am. J. Transl. Res. 2022;14:3154–3163. [PMC free article] [PubMed] [Google Scholar]
- 31.Zhong M., Liu D., Tang H., Zheng Y., Bai Y., Liang Q., Yang X. Impacts of the perioperative fast track surgery concept on the physical and psychological rehabilitation of total hip arthroplasty: A prospective cohort study of 348 patients. Medicine. 2021;100:e26869. doi: 10.1097/MD.0000000000026869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stowers M.D.J., Manuopangai L., Hill A.G., Gray J.R., Coleman B., Munro J.T. Enhanced recovery after surgery in elective hip and knee arthroplasty reduces length of hospital stay. ANZ J. Surg. 2016;86:475–479. doi: 10.1111/ans.13538. [DOI] [PubMed] [Google Scholar]
- 33.Wu Y., Xue H., Zhang W., Wu Y., Yang Y., Ji H. Application of enhanced recovery after surgery in total knee arthroplasty in patients with haemophilia A: A pilot study. Nurs. Open. 2020;8:80–86. doi: 10.1002/nop2.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang H.-Y., Yuan M.-C., Pei F.-X., Zhou Z.-K., Liao R. Finding the optimal control level of intraoperative blood pressure in no tourniquet primary total knee arthroplasty combine with tranexamic acid: A retrospective cohort study which supports the enhanced recovery strategy. J. Orthop. Surg. Res. 2020;15:350. doi: 10.1186/s13018-020-01887-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu H., Xie J., Lei Y., Huang Q., Huang Z., Pei F. Closed suction drainage following routine primary total joint arthroplasty is associated with a higher transfusion rate and longer postoperative length of stay: A retrospective cohort study. J. Orthop. Surg. Res. 2019;14:163. doi: 10.1186/s13018-019-1211-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang T., Liu H., Li H., He S., Xiao L., Qin T., Xu W.L. Effect of early electroacupuncture combined with enhanced recovery after surgery (ERAS) on pain perception and dysfunction in patients after total knee arthroplasty (TKA) BioMed Res. Int. 2022;2022:6560816. doi: 10.1155/2022/6560816. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 37.Collett G., Insley A.P., Michaelis S., Shaji S., Feierstein B., Martell J.R., Jr. Reduction of opioid use with enhanced recovery program for total knee arthroplasty. Fed. Pract. 2021;38:212–219. doi: 10.12788/fp.0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xu H., Yang J., Xie J., Huang Z., Huang Q., Cao G., Pei F. Tourniquet use in routine primary total knee arthroplasty is associated with a higher transfusion rate and longer postoperative length of stay: A real-world study. BMC Musculoskelet. Disord. 2020;21:620. doi: 10.1186/s12891-020-03623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cui P., Wang P., Kong C., Li X.Y., Wang S.K., Wang J.L., Liu X., Lu S.B. Patients older than 75 years undergoing polysegmental lumbar fusion surgery can also benefit from enhanced recovery after surgery program. Clin. Interv. Aging. 2022;ume 17:245–252. doi: 10.2147/CIA.S353511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lampilas A., Bouyer B., Ferrero E., Khalifé M., Bergeot A., Guigui P., Lonjon G. Evaluation of enhanced recovery after spine surgery: Specificities in an academic public hospital. Orthop. Traumatol. Surg. Res. 2021;107:103027. doi: 10.1016/j.otsr.2021.103027. [DOI] [PubMed] [Google Scholar]
- 41.Li Z.-E., Lu S.-B., Kong C., Sun W.-Z., Wang P., Zhang S.-T. Impact of compliance with an enhanced recovery after surgery program on the outcomes among elderly patients undergoing lumbar fusion surgery. Clin. Interv. Aging. 2020;ume 15:2423–2430. doi: 10.2147/CIA.S286007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Duojun W., Hui Z., Zaijun L., Yuxiang G., Haihong C. Enhanced recovery after surgery pathway reduces the length of hospital stay without additional complications in lumbar disc herniation treated by percutaneous endoscopic transforaminal discectomy. J. Orthop. Surg. Res. 2021;16:461. doi: 10.1186/s13018-021-02606-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gong J., Luo L., Liu H., Li C., Tang Y., Zhou Y. How much benefit can patients acquire from enhanced recovery after surgery protocols with percutaneous endoscopic lumbar interbody fusion? Int. J. Gen. Med. 2021;14:3125–3132. doi: 10.2147/IJGM.S318876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Debono B., Sabatier P., Boniface G., Bousquet P., Lescure J.P., Garnaud V., Hamel O., Lonjon G. Implementation of enhanced re-covery after surgery (ERAS) protocol for anterior cervical discectomy and fusion: A propensity score-matched analysis. Eur Spine J. 2021;30:560–567. doi: 10.1007/s00586-020-06445-0. [DOI] [PubMed] [Google Scholar]
- 45.Wang P., Wang Q., Kong C., Teng Z., Li Z., Zhang S., Sun W., Feng M., Lu S. Enhanced recovery after surgery (ERAS) program for elderly patients with short-level lumbar fusion. J. Orthop. Surg. Res. 2020;15:299. doi: 10.1186/s13018-020-01814-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li Z.-E., Lu S.-B., Kong C., Sun W.-Z., Wang P., Zhang S.-T. Comparative short-term outcomes of enhanced recovery after surgery (ERAS) program and non-ERAS traditional care in elderly patients undergoing lumbar arthrodesis: A retrospective study. BMC Musculoskelet. Disord. 2021;22:283. doi: 10.1186/s12891-021-04166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Feng C., Zhang Y., Chong F., Yang M., Liu C., Liu L., Huang C., Huang C., Feng X., Wang X., et al. Establishment and implementation of an enhanced recovery after surgery (ERAS) pathway tailored for minimally invasive transforaminal lumbar interbody fusion surgery. World Neurosurg. 2019;129:e317–e323. doi: 10.1016/j.wneu.2019.05.139. [DOI] [PubMed] [Google Scholar]
- 48.Rao K.E., Krodel D., Toaz E.E., Fanelli J., Hajduk J., Kato K., Rychlik K., King E., Sarwark J., Grayhack J., et al. Introduction of an enhanced recovery pathway results in decreased length of stay in patients with adolescent idiopathic scoliosis undergoing posterior spinal fusion: A description of implementation strategies and retrospective before-and-after study of outcomes. J. Clin. Anesthesia. 2021;75:110493. doi: 10.1016/j.jclinane.2021.110493. [DOI] [PubMed] [Google Scholar]
- 49.Zuo X., Wang L., He L., Li P., Zhou D., Yang Y. Enhanced recovery after surgery protocol accelerates recovery of lumbar disc herniation among elderly patients undergoing discectomy via promoting gastrointestinal function. Pain Res. Manag. 2021;2021:3573460. doi: 10.1155/2021/3573460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leng X., Zhang Y., Wang G., Liu L., Fu J., Yang M., Chen Y., Yuan J., Li C., Zhou Y., et al. An enhanced recovery after surgery pathway: LOS reduction, rapid discharge and minimal complications after anterior cervical spine surgery. BMC Musculoskelet. Disord. 2022;23:252. doi: 10.1186/s12891-022-05185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang S., Wang P., Li X., Sun W., Kong C., Lu S. Enhanced recovery after surgery pathway: Association with lower incidence of wound complications and severe hypoalbuminemia in patients undergoing posterior lumbar fusion surgery. J. Orthop. Surg. Res. 2022;17:178. doi: 10.1186/s13018-022-03070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dagal A., Bellabarba C., Bransford R., Zhang F., Chesnut R.M., O’Keefe G.E., Wright D.R., Dellit T.H., Painter I., Souter M.J. Enhanced perioperative care for major spine surgery. Spine. 2019;44:959–966. doi: 10.1097/BRS.0000000000002968. [DOI] [PubMed] [Google Scholar]
- 53.Li J., Li H., Xv Z.K., Wang J., Yu Q.F., Chen G., Li F.C., Ren Y., Chen Q.X. Enhanced recovery care versus traditional care following laminoplasty: A retrospective case-cohort study. Medicine. 2018;97:e13195. doi: 10.1097/MD.0000000000013195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sibia U.S., MacDonald J.H., King P.J. Predictors of hospital length of stay in an enhanced recovery after surgery program for primary total hip arthroplasty. J. Arthroplast. 2016;31:2119–2123. doi: 10.1016/j.arth.2016.02.060. [DOI] [PubMed] [Google Scholar]
- 55.Zhang J., Che J., Sun X., Ren W. Clinical application of perioperative anaesthesia management based on enhanced recovery after surgery concept to elderly patients undergoing total knee replacement. Comput. Intell. Neurosci. 2022;2022:8039358. doi: 10.1155/2022/8039358. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 56.Bardgett M., Lally J., Malviya A., Kleim B., Deehan D. Patient-reported factors influencing return to work after joint replacement. Occup. Med. 2015;66:215–221. doi: 10.1093/occmed/kqv187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Garriga C., Murphy J., Leal J., Price A., Prieto-Alhambra D., Carr A., Arden N., Rangan A., Cooper C., Peat G., et al. Impact of a national enhanced recovery after surgery programme on patient outcomes of primary total knee replacement: An interrupted time series analysis from “The National Joint Registry of England, Wales, Northern Ireland and the Isle of Man”. Osteoarthr. Cartil. 2019;27:1280–1293. doi: 10.1016/j.joca.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 58.Pritchard M.G., Murphy J., Cheng L., Janarthanan R., Judge A., Leal J. Enhanced recovery following hip and knee arthroplasty: A systematic review of cost-effectiveness evidence. BMJ Open. 2020;10:e032204. doi: 10.1136/bmjopen-2019-032204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Li Z., Li B., Wang G., Wang K., Chen J., Liang Y., Tang X., Yang Y. Impact of enhanced recovery nursing combined with limb training on knee joint function and neuro-logical function after total knee arthroplasty in patients with knee osteoarthritis. Am. J. Transl. Res. 2021;13:6864–6872. [PMC free article] [PubMed] [Google Scholar]
- 60.Kerolus M.G., Yerneni K., Witiw C.D., Shelton A., Canar W.J., Daily D., Fontes R.B.V., Deutsch H., Fessler R.G., Buvanendran A., et al. Enhanced recovery after surgery pathway for single-level minimally invasive transforaminal lumbar interbody fusion decreases length of stay and opioid consumption. Neurosurgery. 2021;88:648–657. doi: 10.1093/neuros/nyaa493. [DOI] [PubMed] [Google Scholar]
- 61.YaDeau J.T., Soffin E.M., Tseng A., Zhong H., Dines D.M., Dines J.S., Gordon M.A., Lee B.H., Kumar K., Kahn R.L., et al. A comprehensive enhanced recovery pathway for rotator cuff surgery reduces pain, opioid use, and side effects. Clin. Orthop. Relat. Res. 2021;479:1740–1751. doi: 10.1097/CORR.0000000000001684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ljungqvist O., de Boer H.D., Balfour A., Fawcett W.J., Lobo D.N., Nelson G., Scott M.J., Wainwright T.W., Demartines N. Opportunities and challenges for the next phase of enhanced recovery after surgery. JAMA Surg. 2021;156:775–784. doi: 10.1001/jamasurg.2021.0586. [DOI] [PubMed] [Google Scholar]
- 63.Agarwal V., Divatia J.V. Enhanced recovery after surgery in liver resection: Current concepts and controversies. Korean J. Anesthesiol. 2019;72:119–129. doi: 10.4097/kja.d.19.00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Weiss M.J., Kim Y., Ejaz A., Spolverato G., Haut E.R., Hirose K., Wolfgang C.L., Choti M.A., Pawlik T.M. Venous thromboembolic prophylaxis after a hepatic resection: Patterns of care among liver surgeons. HPB. 2014;16:892–898. doi: 10.1111/hpb.12278. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The articles and data are available on PubMed, MEDLINE, Web of Science, Cochrane Reviews, EMBASE, etc.