Abstract
Background
Madelung deformity is a rare wrist anomaly that causes considerable pain while restricting function. In this study, we describe a radioscapholunate (RSL) arthrodesis with a neo-distal radioulnar joint (DRUJ) in Madelung deformity patients with an abnormal sigmoid notch and compare results to patients after a reverse wedge osteotomy.
Methods
Six wrists underwent RSL arthrodesis with a neo-DRUJ in a two-phase approach: (1) modified RSL arthrodesis with triquetrectomy; and (2) distal scaphoidectomy. Seven wrists underwent a reverse wedge osteotomy procedure.
Results
There were no differences found in postoperative pain, grip strength, or range of motion (ROM), apart from extension, which was decreased after RSL arthrodesis with a neo-DRUJ. Quality of life and Michigan Hand Outcomes Questionnaire scores were similar.
Conclusions
Although clinical outcome parameters are not different among the two groups, the RSL arthrodesis with construction of a neo-DRUJ could prove a valid treatment option for a subset of patients with a severely affected sigmoid notch.
Keywords: Madelung deformity, wrist, radiocarpal joint, radioulnar joint, sigmoid notch, reconstruction, reverse wedge osteotomy, radial osteotomy
Introduction
Madelung deformity is a rare wrist anomaly characterized by shortening and angulation of the distal radius articular surface, a palmar subluxation of the hand, and a prominent distal ulna.1,2 Presentation is often bilateral and includes the presence of abnormally thickened ligaments from the distal radius to the lunate and triquetral bones. 3
In the diagnostic work-up of Madelung deformity, the radiological criteria as proposed by McCarroll are often used in the quantification, early identification, monitoring of progression, and assessment after corrective surgery. 4 Indications for surgical treatment include wrist pain, restricted range of motion (ROM), loss of grip strength, and cosmetic deformity.1,5,6 Currently, there is no standardized surgical method.1,5 When evaluating the range of surgical treatment options, the spotlight has been placed on correcting length and angles to obtain a “near-normal” anatomical configuration, with a majority of case series performing osteotomies of radius and/or ulna.5,7 However, in some patients, a large discrepancy between the ulna and proximal carpal row can be found on preoperative computed tomography (CT) imaging. Additionally, the sigmoid notch can be severely underdeveloped, leaving the ulnar head with nothing to articulate with.8,9 For these patients, an osteotomy procedure could be suboptimal. The new surgical approach as introduced in this study aims to offer a solution for this subset of patients.
The primary objective of this case series study is to describe a new surgical approach to Madelung deformity, consisting of a radioscapholunate (RSL) arthrodesis and construction of a neo-distal radioulnar joint (DRUJ). Preliminary results are reported through clinical outcomes: pain intensity levels, ROM, and grip strength measurements; functional outcomes are assessed using patient-reported outcome measures (PROMs). To determine its position in the current treatment landscape, we compared outcomes after the new surgical approach to outcomes after a reverse wedge osteotomy.
Materials and Methods
Setting and Study Population
Patients diagnosed with Madelung deformity were identified by a search of our two academic tertiary referral institutions’ electronic medical record databases, using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code: 755.54. Medical record review showed that the McCarroll criteria were used in the diagnostic work-up. 4 Initially, the McCarroll criteria 4 were used to confirm the diagnosis of Madelung deformity. As part of the surgical decision-making process, preoperative CT scans were reviewed; in some patients, little to no sigmoid notch was visible, leaving the ulnar head with nothing to articulate (Figure 1). In these cases, surgeons chose to use the alternative surgical technique, aimed to remove the discrepancy between the ulna and the proximal carpal row. Patients with a “post-traumatic” Madelung deformity 10 or history of corrective wrist surgery other than an RSL arthrodesis with a neo-DRUJ or reverse wedge osteotomy were excluded; pregnancy and age under 18 at time of follow-up were additional exclusion criteria. A total of 12 patients were identified who had previously undergone RSL arthrodesis with construction of a neo-DRUJ or a reverse wedge osteotomy 11 between 2005 and 2019. Of these, 9 agreed to participate in the study. Four patients (6 wrists) had undergone RSL arthrodesis with a neo-DRUJ and 5 patients (7 wrists) had undergone a reverse wedge osteotomy. Patients were evaluated between April 2019 and February 2020 to assess their clinical and radiographic outcomes. Written informed consent was obtained from all patients.
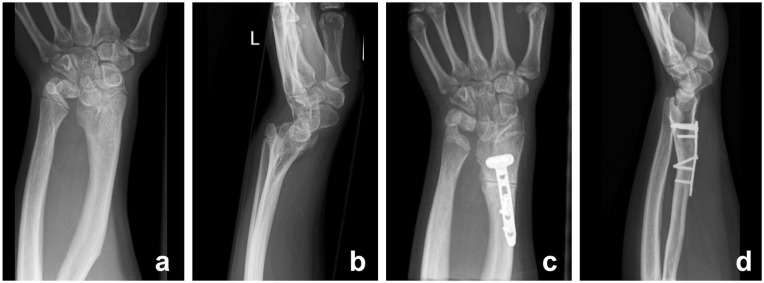
Figure 1.
Preoperative distal radioulnar joint (DRUJ) of a patient who underwent radioscapholunate arthrodesis with a neo-DRUJ (left) and preoperative DRUJ of a patient who underwent reverse wedge osteotomy (right).
Radioscapholunate Arthrodesis With Construction of a Neo-DRUJ
This two-stage surgery, which addresses the abnormal DRUJ, consists of: (1) a modified RSL arthrodesis and triquetrectomy; and (2) a distal scaphoidectomy and removal of osteosynthetic material. The time between both surgeries is imperative since the scaphoid receives the majority of its blood supply from distal branches, 12 and a waiting interval of 6 months to 1 year assures an adequate formation of collaterals before the distal scaphoidectomy is performed. 13 In the first operation (Figures 2a and 2b), a longitudinal dorsal incision is made over the fourth to fifth dorsal extensor compartment. The involved structures are released and access to the joint capsule is obtained. On the ulnar side of the fifth extensor compartment, a capsular flap is created, after which the lunate, scaphoid, and triquetrum bones are identified. Next, the radius is shortened by carving out the distal bone while leaving the radial side of the radius (containing the radial styloid) intact for stability and maintenance of vascularization. The triquetrum bone is released and excised. The scaphoid and lunate are positioned in a more dorsal stance in order to correct the volar dislocation of the hand and are fixated to the radius with a 2.4 mm dorsal L-plate and locking screws. Since the sigmoid notch in Madelung deformity is underdeveloped, a new articular surface for the ulnar head is needed; removing the triquetrum creates space for the ulnar head. By repositioning the scaphoid and lunate more dorsally before fixation, the ulnar side of the lunate bone is allowed to articulate with the ulnar head as they now form a “neo-DRUJ” (Figure 2b). Stability is achieved by suturing (Vicryl 2-0) the palmar and dorsal distal radioulnar ligaments of the triangular fibrocartilage complex (TFCC), palmarly, to the remnants of the lunotriquetral ligament and dorsally to the soft tissues of the lunate. Removal of the cartilage on the radio-lunar articular surface does not pose a risk of damaging the lunotriquetral (LT) ligament palmarly, granted that solely the contact surface of the desired arthrodesis is stripped of its cartilage. Furthermore, the cranial part of the lunate (ie, where the ligamentous part of the LT ligament attaches) is spared. The dorsal DRUJ capsule and the radiocarpal joint capsule of the fifth extensor compartment are closed; the extensor digiti minimi remains in an extra-anatomical position. Repositioning and fixation of the structures were adjusted and confirmed using intraoperative x-ray imaging. The wrist is immobilized for 6 weeks in a below-elbow cast, using a neutral position of rotation with a slight cock-up of the wrist. The range of motion after consolidation of the RSL arthrodesis is limited to a dart-throwing motion pattern with only limited flexion, extension, and radioulnar deviation.
Figure 2.
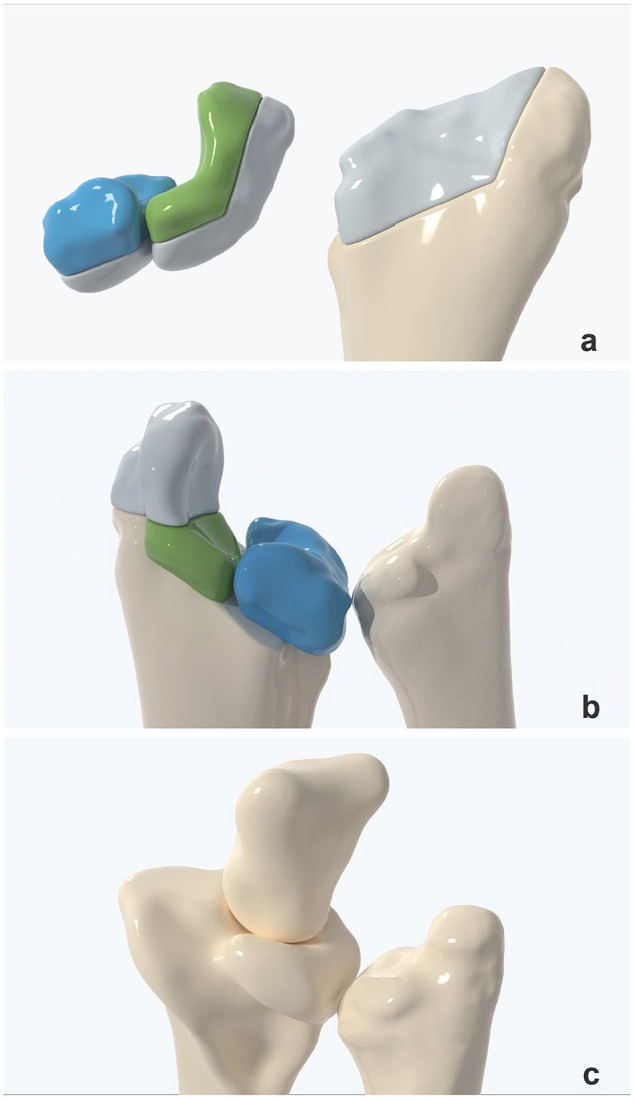
(a) The distal radius is shortened by carving out a piece of bone and replacing it by the scaphoid and lunate. The proximal articular surfaces of the lunate and scaphoid are dechondrified. The triquetrum is released and excised. (b) The scaphoid and lunate are fixated to the dorsal radius using a L-plate 2.4 and locking screws. The ulnar side of the lunate will articulate with the ulnar head as a neo-distal radioulnar joint (DRUJ). (c) Neo-DRUJ showing articulation with the capitate and ulnar bone. Note that the distal pole of the scaphoid (Figure 2b) is excised.
After confirmation of full consolidation of the partial arthrodesis on postoperative CT-scans, the distal pole of the scaphoid is excised, to improve the range of motion of the remaining joint. In this second surgery (Figure 2c), the scar from the first surgery is also excised. The structures of the third and fourth extensor compartment are released and access to the osteosynthesis plate is acquired. The plate and screws are removed, the midcarpal joint is identified and the distal scaphoid pole is exposed. The distal pole of the scaphoid is removed with a saw and extracted using a rongeur; loose fragments are removed. The wound is closed using absorbable sutures, after which a pressure bandage is applied. All patients start hand therapy 1 week postoperatively for a total of 12 weeks.
Clinical and Radiographic Evaluation
Patients were examined at our outpatient clinic to assess pain, ROM, and grip strength. Pain intensity levels were measured using a visual analogue scale (VAS) (range 0-10; lower is better). ROM was measured in degrees using a goniometer for the following motions: flexion, extension, radial deviation, ulnar deviation, pronation, and supination. Grip strength was assessed with a dynamometer, following the American Medical Association guidelines. 14 Instability of the DRUJ was assessed pre- and postoperatively by testing for anterior-posterior translation. PROMs were assessed using the 5-level EQ-5D-5 L questionnaire (range 1-5; higher is better), 15 and the Michigan Hand Outcomes Questionnaire (MHQ) (range 0-100; higher is better). 16 Follow-up for the neo-DRUJ group was defined as time since the second surgery.
Pre- and postoperative x-ray images were obtained for both patient groups (Figures 3 and 4), with patients being evaluated 1 week and 6 weeks after surgery. The degree of deformity was radiographically quantified using the McCarroll criteria, 4 measuring ulnar tilt, lunate subsidence, lunate fossa angle, palmar tilt, and palmar carpal displacement. Postoperative measurements could not be performed in RSL arthrodesis patients as the anatomical configuration was radically altered. At 6 weeks, all osteotomy cases showed partial consolidation on x-ray imaging, after which bone healing was not further evaluated. In the neo-DRUJ group, bone healing was actively monitored at 6 months on CT imaging due to the procedure’s novelty and the inability to assess consolidation of the RSL arthrodesis on x-ray imaging accurately. If the partial arthrodesis was not fully consolidated, CT imaging was repeated at 9 months; full consolidation was seen after an average of 7.5 months (SD = 1.9).
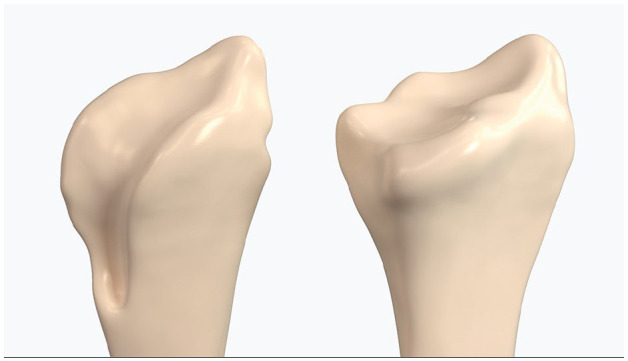
Figure 3.
Preoperative (a) posteroanterior and (b) lateral radiographs, and postoperative (c) posteroanterior and (d) lateral radiographs of a patient who underwent radioscapholunate arthrodesis with a neo-distal radioulnar joint.
Figure 4.
Preoperative (a) posteroanterior and (b) lateral radiographs, and postoperative (c) posteroanterior and (d) lateral radiographs of a patient who underwent reverse wedge osteotomy.
Statistical Analysis
Mean postoperative outcomes of pain, ROM, grip strength, MHQ scores, and EQ-5D-5 L scores were compared between the RSL arthrodesis with a neo-DRUJ and reverse wedge osteotomy groups. Grip strength data was unavailable for two patients. Data distribution was evaluated using a Shapiro-Wilk test to assess normality. Normally distributed variables were analyzed with an independent samples t-test (variances equal) or Welch’s test (variances not equal). Equality of variances was assessed using Levene’s test. Non-normally distributed variables were compared with a Mann-Whitney U test.
Results
Patients that had undergone RSL arthrodesis with a neo-DRUJ (n = 4) had a mean age of 15 (SD = 0.8) years with a follow-up of 47.6 (SD = 18.6, range 13-62) months; reverse wedge osteotomy patients (n = 5) had a mean age of 13.8 (SD = 2.2) years with a follow-up of 105.4 (SD = 80.6, range 17-174) months (Table 1). Average time between surgeries in the RSL arthrodesis group was 10.5 (SD = 2.0) months.
Table 1.
Patient Characteristics.
| Variable | RSL-arthrodesis with a neo-DRUJ (n = 4) | Reverse wedge osteotomy (n = 5) |
|---|---|---|
| Wrists | 6 | 7 |
| Age at time of (first) surgery, mean (SD), y | 15 (0.8) | 13.8 (2.2) |
| Follow-up, mean (SD), range, m | 47.6 (18.6), 13-62 | 105.4 (80.6), 17-174 |
| Female | 4 | 5 |
| Right dominant hand | 4 | 5 |
| Bilateral deformity | 4 | 5 |
| Confirmed genetic cause | 2 | 0 |
| Additional procedures | 1 | 1 |
Note. RSL = radioscapholunate; DRUJ = distal radioulnar joint.
Primary preoperative complaints included pain, decreased grip strength, and cosmetic deformity. Radiographic evaluation revealed no differences in preoperative measurements (Supplemental Table S1).
No differences in ROM were found between cases after RSL arthrodesis with a neo-DRUJ (n = 6) and cases after a reverse wedge osteotomy (n = 7), except for extension (54.3, SD = 11 versus 34.2, SD = 15.3) (Table 2). In regard to postoperative pain and grip strength, no differences were found (Table 3).
Table 2.
Range of Motion.
| Variable | RSL-arthrodesis with a neo-DRUJ (n = 6) | Reverse wedge osteotomy (n = 7) | P |
|---|---|---|---|
| Flexion, mean (SD), degrees | 55.8 (3.8) | 53.6 (10.7) | .63 |
| Extension, mean (SD), degrees | 34.2 (15.3) | 54.3 (11) | .04 |
| Radial deviation, mean (SD), degrees | 15 (6.3) | 17.6 (11.1) | .63 |
| Ulnar deviation, mean (SD), degrees | 23.3 (6.1) | 28.4 (8.2) | .23 |
| Pronation, mean (SD), degrees | 79.2 (9.7) | 77.1 (10.7) | .73 |
| Supination, mean (SD), degrees | 82 (10.9) | 76.6 (17.5) | .45 |
Note. RSL = radioscapholunate; DRUJ = distal radioulnar joint.
Bold indicates statistical significance (P < 0.05).
Table 3.
Effectiveness of Treatment.
| Variable | RSL-arthrodesis with a neo-DRUJ (n = 6) | Reverse wedge osteotomy (n = 7) | P |
|---|---|---|---|
| Pain VAS, mean (SD) | 2.3 (1.9) | 3.9 (3.7) | .30 |
| Grip strength, mean (SD), kg | 17 (10.3) | 22.6 (1.8) | .29 |
| Michigan hand outcomes questionnaire score mean (SD) | 66.8 (11.5) | 71.3 (15.9) | .58 |
| EQ-5D-5 L, mean (SD) | 0.89 (0.1) | 0.86 (0.1) | .67 |
| EQ VAS, mean (SD) | 88.3 (13.1) | 81 (14.3) | .46 |
Note. RSL = radioscapholunate; DRUJ = distal radioulnar joint; VAS = visual analogue scale.
There were no postoperative differences in functional outcomes between RSL arthrodesis with a neo-DRUJ and reverse wedge osteotomy patients (Table 3).
Discussion
This case-control study describes early outcomes of RSL arthrodesis with a neo-DRUJ, a new surgical technique for the corrective treatment of Madelung deformity. The described surgical approach offers an alternative for patients with a severely affected sigmoid notch. Short-term results were compared to a group that underwent a reverse wedge osteotomy. In regard to clinical and radiographic parameters, the results were similar. Compared to reverse wedge osteotomy patients, patients after RSL arthrodesis and construction of a neo-DRUJ had similar grip strength measurements and ROM, except for extension, which was lower in the latter group. Quality of life (EQ-5D-5L) and overall MHQ scores were similar.
A strength of this study is that we used a structured protocol to report on postoperative outcomes. 5 A limitation was the small number of cases; low statistical power limited detecting differences that might prove clinically relevant. In addition, differences in preoperative anatomical configuration and follow-up between the two groups could lead to significant confounding. That being said, the purpose of this study was to introduce a new surgical approach rather than determining the best treatment by comparing outcomes. Another limitation was that preoperative measurements were not performed consistently; therefore, comparisons between the pre- and postoperative anatomical configurations were not possible, preventing the assessment of relative improvement. Lastly, while sufficient time elapsed for proper bone healing 17 our study’s follow-up was relatively limited.
The mean range of motion in the RSL arthrodesis with a neo-DRUJ group was similar compared to the reverse wedge osteotomy group, except for extension which was lower. During extension, the radiocarpal joint contributes to 66.5%, and the midcarpal joint to 33.5% of the total motion pattern. 18 In contrast, during flexion, this balance shifts to 60% and 40% for radiocarpal and midcarpal, respectively. Therefore, it is not unexpected that after fixation of the proximal carpal row, flexion would be less affected after fusion, which corresponds with the results of both our study (55.8° and 53.6° in respective groups) and previous studies reporting outcomes after osteotomy procedures.6,19 Notable were the relatively intact pronation and supination measurements in both groups compared to normal reference values. 20 Other studies reported a mean supination of 75° after distal radial dome osteotomy 19 and 72° 6 after various osteotomies of the distal radius.
Mean postoperative pain was similar and considered “mild” for both groups. 21 Pain was mainly localized to the areas between the distal radius and ulna, and the ulnar side of the wrist. One recent case series study, describing outcomes after a Sauvé-Kapandji procedure, 22 reported mean VAS scores of 2.3 (SD = 0.6) 23 with a mean follow-up of 16 months. Other studies described only the presence or absence of pain without any quantification.6,11,19
Regarding grip strength, both groups scored below average reference values for healthy females in the same age range (age 18-19 years, mean grip strength 31.4 kg). 24 Arthrodesis procedures are associated with loss of grip strength, 25 restoring up to 75% of strength at best; the leading causes being a loss of radiocarpal and intercarpal bone movement, relative lengthening of musculotendinous units after bone removal, 25 and a suboptimal wrist position after fusion. 26 The few case series studies that have measured grip strength, report means of 22.1 kg after a combination of an opening wedge osteotomy and modified Darrach, 27 and 24.2 kg after reverse wedge osteotomy 11 ; 1 study reported grip strength as a percentage of expected normal values (68%). 28
In our study, total MHQ-scores after RSL arthrodesis were similar to our control group. The use of PROMs in Madelung deformity research has been limited. The few studies that implement PROMs either use the Disabilities of the Arm, Shoulder and Hand (DASH), 29 QuickDASH, 30 or Patient-Rated Wrist/Hand Evaluation11,19,23,27; overall, patients reported being satisfied with both functional outcomes and esthetics. For future studies, we would recommend using the Patient Reported Outcomes Measurement Information System, as it has been shown to have high validity and reliability in congenital hand research. 31
The approach in this study aims to create a neo-DRUJ from the ulnar joint surface of the lunate, in which the relatively long ulna1,2 can articulate. The DRUJ is responsible for the articulation of the distal ulnar head in the sigmoid notch of the distal radius, enabling rotation of the wrist. 32 Problems can occur due to an uneven surface, bowing of the distal radius, and a smaller sigmoid notch, 33 which have all shown to be abnormal in Madelung deformity wrists. 34 Madelung deformity has a spectrum of presentation, including patients whose anatomy is more severely affected than others.2,9 Although there were no statistical differences in radiographic measurements, patients who underwent RSL arthrodesis with a neo-DRUJ appeared to have a more deformed radius in comparison to the control group (Figure 1). The proposed procedure resulted in a DRUJ geometry which seemed more anatomical compared to the preoperative state. Future studies are required to establish if there is quantitative evidence for this observation. 34 Since existing techniques focus mainly on remodeling the radiocarpal joint, the new approach could provide an alternative treatment option for patients with a severely deformed DRUJ.8,9 To the best of our knowledge, the approach described in this study is the only procedure that results in a functional sigmoid notch in patients with a preoperatively abnormal DRUJ in Madelung deformity.
While enough time was granted for adequate bone healing 17 the complex anatomical changes can alter biomechanics.35,36 Therefore, it is paramount to continue observation of the long-term effects of these altered forces on the wrist joint to confirm the benefits of this procedure, primarily since patients are operated on at a young age. 1 Additionally, future studies should further focus on the soft-tissue reconstruction, considering Madelung’s ligamentous abnormalities. Furthermore, inconsistent reporting of outcomes in Madelung deformity has prevented any objective comparisons. 5 Therefore, future studies should adhere to a structured protocol to compare different procedures through meta-analyses. Since the deformity can present on a wide spectrum, the surgical management of Madelung deformity patients will most likely necessitate an individualized treatment algorithm. Quantification of the sigmoid notch could aid in the selection of patients to undergo the new surgical approach. Lastly, it is recommended to perform cost-effectiveness studies, as a 2-step approach will be associated with higher initial treatment costs.
In this study, we introduced and assessed a new surgical approach for the corrective treatment of Madelung deformity. Since the DRUJ in Madelung deformity can be severely deformed, this approach could provide an alternative treatment option for a subset of patients. While short-term postoperative outcomes seem satisfactory and similar to outcomes after reverse wedge osteotomy, longer follow-up studies will be required to confirm the procedure’s durability.
Supplemental Material
Supplemental material, sj-pdf-1-han-10.1177_15589447211017223 for Madelung Deformity: Radioscapholunate Arthrodesis With a Neo-DRUJ by Annelinde R. Piek, Abbas Peymani, Johannes G. G. Dobbe, Geert A. Buijze, Michel Chammas, Geert J. Streekstra and Simon D. Strackee in HAND
Acknowledgments
We would like to thank Sybren van Rijn for creating the figures that illustrate the described surgical technique.
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: Ethical approval for this study was obtained from Medical Ethics Committee (NL66957.018.18) of the Amsterdam University Medical Center.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Written informed consent was obtained from all subjects before the study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The co-first author (A.P.) received a PhD scholarship (2017) from the Amsterdam University Medical Center (Location AMC, Amsterdam, The Netherlands) supporting this research.
ORCID iDs: Annelinde R. Piek  https://orcid.org/0000-0002-8752-846X
https://orcid.org/0000-0002-8752-846X
Abbas Peymani  https://orcid.org/0000-0002-3312-0469
https://orcid.org/0000-0002-3312-0469
References
- 1. Arora AS, Chung KC. Madelung and the recognition of Madelung’s deformity. J Hand Surg Am. 2006;31(2):177-182. [DOI] [PubMed] [Google Scholar]
- 2. Kozin SH, Zlotolow DA. Madelung deformity. J Hand Surg Am. 2015;40(10):2090-2098. [DOI] [PubMed] [Google Scholar]
- 3. Hanson TJ, Murthy NS, Shin AY, et al. MRI appearance of the anomalous volar radiotriquetral ligament in true Madelung deformity. Skeletal Radiol. 2019;48(6):915-918. [DOI] [PubMed] [Google Scholar]
- 4. McCarroll HR, Jr, James MA, Newmeyer WL, 3rd, et al. Madelung’s deformity: quantitative assessment of x-ray deformity. J Hand Surg Am. 2005;30(6):1211-1220. [DOI] [PubMed] [Google Scholar]
- 5. Peymani A, Johnson AR, Dowlatshahi AS, et al. Surgical management of Madelung deformity: a systematic review. Hand. 2019;14(6):725-734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Saffar P, Badina A. Treatment of Madelung’s deformity. Chir Main. 2015;34(6):279-285. [DOI] [PubMed] [Google Scholar]
- 7. Ali S, Kaplan S, Kaufman T, et al. Madelung deformity and Madelung-type deformities: a review of the clinical and radiological characteristics. Pediatr Radiol. 2015;45(12):1856-1863. [DOI] [PubMed] [Google Scholar]
- 8. Coffey MJ, Scheker LR, Thirkannad SM. Total distal radioulnar joint arthroplasty in adults with symptomatic Madelung’s deformity. Hand. 2009;4(4):427-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ghatan AC, Hanel DP. Madelung deformity. J Am Acad Orthop Surg. 2013;21(6):372-382. [DOI] [PubMed] [Google Scholar]
- 10. Knutsen EJ, Goldfarb CA. Madelung’s deformity. Hand. 2014;9(3):289-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mallard F, Jeudy J, Rabarin F, et al. Reverse wedge osteotomy of the distal radius in Madelung’s deformity. Orthop Traumatol Surg Res. 2013;99(4 suppl):S279-S283. [DOI] [PubMed] [Google Scholar]
- 12. Handley RC, Pooley J. The venous anatomy of the scaphoid. J Anat. 1991;178:115-118. [PMC free article] [PubMed] [Google Scholar]
- 13. LaStayo PC, Winters KM, Hardy M. Fracture healing: bone healing, fracture management, and current concepts related to the hand. J Hand Ther. 2003;16(2):81-93. [DOI] [PubMed] [Google Scholar]
- 14. Brigham CR. AMA Guides to the Evaluation of Permanent Impairment. Chicago, IL: American Medical Association; 2006. [Google Scholar]
- 15. Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727-1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chung KC, Pillsbury MS, Walters MR, et al. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg Am. 1998;23(4):575-587. [DOI] [PubMed] [Google Scholar]
- 17. Islam O, Soboleski D, Symons S, et al. Development and duration of radiographic signs of bone healing in children. AJR Am J Roentgenol. 2000;175(1):75-78. [DOI] [PubMed] [Google Scholar]
- 18. Sarrafian SK, Melamed JL, Goshgarian GM. Study of wrist motion in flexion and extension. Clin Orthop Relat Res. 1977(126):153-159. [PubMed] [Google Scholar]
- 19. Steinman S, Oishi S, Mills J, et al. Volar ligament release and distal radial dome osteotomy for the correction of Madelung deformity: long-term follow-up. J Bone Joint Surg Am. 2013;95(13):1198-1204. [DOI] [PubMed] [Google Scholar]
- 20. Soucie JM, Wang C, Forsyth A, et al. Range of motion measurements: reference values and a database for comparison studies. Haemophilia. 2011;17(3):500-507. [DOI] [PubMed] [Google Scholar]
- 21. Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. 2003;4(7):407-414. [DOI] [PubMed] [Google Scholar]
- 22. Taleisnik J. The Sauve-Kapandji procedure. Clin Orthop Relat Res. 1992(275):110-123. [PubMed] [Google Scholar]
- 23. Eid A, Abdel Salam MA, Elgawhary S. Management of idiopathic Madelung deformity with the Sauve-Kapandji procedure. Current Orthopaedic Practice. 2018;29(5):491-496. [Google Scholar]
- 24. Werle S, Goldhahn J, Drerup S, et al. Age- and gender-specific normative data of grip and pinch strength in a healthy adult Swiss population. J Hand Surg Eur Vol. 2009;34(1):76-84. [DOI] [PubMed] [Google Scholar]
- 25. Bhardwaj P, Nayak SS, Kiswar AM, et al. Effect of static wrist position on grip strength. Indian J Plast Surg. 2011;44(1):55-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. O’Driscoll SW, Horii E, Ness R, et al. The relationship between wrist position, grasp size, and grip strength. J Hand Surg Am. 1992;17(1):169-177. [DOI] [PubMed] [Google Scholar]
- 27. Kampa R, Al-Beer A, Axelrod T. Madelung’s deformity: radial opening wedge osteotomy and modified Darrach procedure using the ulnar head as trapezoidal bone graft. J Hand Surg Eur Vol. 2010;35(9):708-714. [DOI] [PubMed] [Google Scholar]
- 28. Murphy MS, Linscheid RL, Dobyns JH, et al. Radial opening wedge osteotomy in Madelung’s deformity. J Hand Surg Am. 1996;21(6):1035-1044. [DOI] [PubMed] [Google Scholar]
- 29. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29(6):602-608. [DOI] [PubMed] [Google Scholar]
- 30. Beaton DE, Wright JG, Katz JN, et al. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(5):1038-1046. [DOI] [PubMed] [Google Scholar]
- 31. Waljee JF, Carlozzi N, Franzblau LE, et al. Applying the patient-reported outcomes measurement information system to assess upper extremity function among children with congenital hand differences. Plast Reconstr Surg. 2015;136(2):200e-207e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Arias DG, Varacallo M. Anatomy, Shoulder and Upper Limb, Distal Radioulnar Joint. Treasure Island, FL: StatPearls; 2019. [Google Scholar]
- 33. Bruno RJ, Blank JE, Ruby LK, et al. Treatment of Madelung’s deformity in adults by ulna reduction osteotomy. J Hand Surg Am. 2003;28(3):421-426. [DOI] [PubMed] [Google Scholar]
- 34. Peymani A, Dobbe JGG, Streekstra GJ, et al. Quantitative three-dimensional assessment of Madelung deformity. J Hand Surg Eur Vol. 2019;44(10):1041-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Eschweiler J, Hawlitzky J, Quack V, et al. Biomechanical model based evaluation of total hip arthroplasty therapy outcome. J Orthop. 2017;14(4):582-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Friedman RJ. Biomechanics of total shoulder arthroplasty: a preoperative and postoperative analysis. Semin Arthroplasty. 1995;6(4):222-232. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-han-10.1177_15589447211017223 for Madelung Deformity: Radioscapholunate Arthrodesis With a Neo-DRUJ by Annelinde R. Piek, Abbas Peymani, Johannes G. G. Dobbe, Geert A. Buijze, Michel Chammas, Geert J. Streekstra and Simon D. Strackee in HAND