Abstract
Background
Vaccination against COVID 19 and observing COVID appropriate behavior are effective measures to control, manage and prevent COVID-19 infection. With India starting its adolescent vaccination program, this study aimed to explore the adolescents’ perception of vaccination, their COVID-appropriate behavior, compliance with two doses of COVID-19 vaccines and the experienced side effects following vaccination.
Methods
A longitudinal survey was conducted among 440 adolescents visiting the COVID Vaccination Center (CVC) of a tertiary hospital in West Bengal. In the survey, adolescents were asked about family socio-demographic characteristics, their opinions on COVID-19 vaccines, and COVID-19 Appropriate Behavior (CAB) practices. Voluntary participants were given a questionnaire to fill and a telephonic interview was taken regarding side effects experienced following the vaccination and their compliance to both doses of vaccine.
Results
The majority of adolescents (99.3%) had taken vaccines by their own wish. The reason for willingness to take the vaccine was the fear of being infected with COVID-19 infection (50.5%). Maximum adolescents got information regarding the COVID vaccination program through the internet (41.8%) followed by family members (30.5%). The majority of adolescents (70.9%) had a good perception of COVID-19 vaccination. A significant number of adolescents (44.8%) strongly disagreed with the statement that they don't need to follow COVID appropriate behavior after vaccination.
Conclusion
The majority of adolescents had a good perception regarding COVID-19.
Keywords: COVID-19, COVID Appropriate behavior, CAB, Vaccine, Adolescents
1. Introduction
Coronavirus disease (COVID-19), a declared Public Health Emergency of International Concern in January 2020 created havoc in the world due to dramatic loss of human life and presented an unprecedented challenge to the health care sector.1 While early waves showed maximum infection rates in adults, subsequent COVID waves also showed higher infections in children. As the world struggled with the COVID-19 pandemic, it became clear that vaccines and COVID appropriate behaviors are key factors in controlling COVID-19 infection.2 Because of the high infectivity and mortality rate among the adult population, the earlier focus of the COVID-19 vaccination program was on adults and the elderly. India started its vaccination drive on January 16, 2021 focusing on frontline health care workers and the elderly population.3 But now as the majority of the adult population is covered by the national vaccination program and vaccine safety has been established among adolescents, most nations around the world have started preparing for the vaccination of adolescents. The government of India started vaccinating adolescents aged 15–17 years from January 3, 2022 and children aged 12–14 years from March 16, 2022 to combat the battle against COVID-19 infection.4 Vaccination of adolescents would further reduce the disease burden and provide other significant benefits towards resuming socio-economic activity.1
Vaccine hesitancy has been a major concern for many nations,5 which is influenced by reports of vaccine safety, efficacy, and the perception of individuals toward vaccines and disease.6 Even though adolescent vaccination had been introduced but not many studies have been conducted in this particular area. The willingness of children for vaccination differs from 39% in Hong Kong, 50.1% in England, and 75.59% in China due to factors of concern regarding vaccine safety and efficacy, parental consent, and fear of getting infected.7, 8, 9 Studies conducted among parents regarding willingness to vaccinate their child also showed different values ranging from 28.9% in Turkey, 48.2% in England, 63.1% in India, 72.7% in China to 90% in Italy.10, 11, 12, 13, 14, 15 It is an essential goal of health care services to ensure good health and well-being for individuals at all stages of life. Therefore, vaccination against COVID-19 is especially important in adolescents. In the context of COVID-19 vaccine program in adolescents, we aimed to explore adolescents’ vaccination, their COVID-appropriate behavior, compliance with the two-dose COVID-19 vaccine, and the experienced side effects after receiving the vaccine.
2. Material and methods
2.1. Research design and setting
A longitudinal survey was conducted among adolescents shortly after COVID vaccination began in India. The data were collected at four different timings (day 1, day 8, day 30, and day 38) from each participant; 1) on the day of receiving the first dose of vaccination, 2) eight days after the first dose, 3) on the day of taking the 2nd dose and 4) eight days after the second dose of vaccination. The study was conducted at the COVID vaccination center of a tertiary care, teaching hospital in Nadia district, West Bengal where multi-speciality services are provided.
2.2. Sample and sample size
Adolescents aged 15–17 years visiting COVID Vaccination Center (CVC) and willing to give consent and assent for their participation were included in the study. Adolescents who had already received 1st dose of COVID-19 vaccination and had a history of being infected with COVID-19 in the past 3 months were excluded. Due to the non-availability of a similar kind of study among adolescents in India, we assumed a 50% of vaccination acceptance rate among adolescents aged 15–17 years for calculating the sample size. With α = 0.05; 80% of power and 10% of relative precision, the initial sample size was 400. The final sample size calculated was 440 assuming a 10% non-response rate.
2.3. Data collection and analysis
The data were collected from mid-January 2022 to March 2022. Participants were requested to answer the self-reported questionnaire. The questionnaire had four sections. Section A included the demographic profile of adolescents. Section B had questions related to willingness toward COVID vaccination as well as the reason for willingness. Section C assessed the perception of adolescents towards COVID vaccination. The perception questionnaire was a five-point Likert scale ranging from strongly agree to strongly disagree. The possible minimum score was 8 and the maximum score was 40. Based on scoring, the perception was arbitrarily categorized as excellent (>32/>80%), good (25–32), average (20–24) and poor (<20). Section D had 11 statements related to COVID appropriate behavior practices based on Ministry of Family and Health Welfare, Government of India (MOHFW, GoI) guidelines. Each statement was containing a score based on practices done always/most of the time/occasionally/rare/never. The maximum and minimum possible scores were 55 and 11 respectively. The behavior of adolescents was categorized into four categories; excellent (>44), good (34–44), average (23–33) and poor (<23).
The validity of the questionnaire was established after taking suggestions and recommendations from five experts. The questionnaire was tested on 20 adolescents to assess appropriateness, feasibility and comprehensibility.
The data were collected at different intervals from the adolescents. The structured questionnaire was initially administered on the day of the first dose of vaccination. Side-effects of the first dose of vaccine were collected through telephonic interviews on the 8th day after receiving the first dose. If the adolescents received the second dose on the appropriate time (30–37 days after the first dose), we considered it compliance. On the eighth day after receiving the second dose, another telephone call was made to inquire about any side effects. Consent was taken from every participant regarding a telephonic interview at the time of receiving vaccine dose and they were informed regarding the interview. Two mobile numbers (the participants and their guardians) were collected after obtaining their consent, for the purpose of the interview. Telephone calls were made to each participants. Upon failure to answer the first telephone call, three attempts were made to contact them, and if none were answered, it was considered “not responded”.
Data were analyzed using the Statistical Package for Social Sciences (SPSS) version 22.0 Descriptive statistics were used to summarize the data. Chi-square was used for the inferential statistic. A p-value of less than 0.05% was considered significant.
2.4. Ethical considerations
Study approval was obtained from the Institutional Research Committee and Ethics Committee (IEC/AIIMS/Kalyani/2022/19). Informed assent was taken from adolescents and consent from their guardians before they participated in the survey. Privacy and confidentiality of information were maintained throughout the study. Participants were informed that their participation in the study was voluntary. In addition, they were assured that their relationship with the hospital would not be affected if they declined to participate or withdraw from the study at any point.
3. Results
3.1. Characteristics of the participants
Among 440 adolescents, more than half of the adolescents (51%) were studying in government schools, had an age of 17 years (42%), were male (60.7%), and belonged to the Hindu religion (91.6%). Most of the adolescents were from a rural background (55%) [Table 1 ].
Table 1.
Demographic profile of participant n = 440.
| Variables | Frequency(f) | Percentage (%) | |
|---|---|---|---|
| Age (in years) | 15 | 104 | 23.6 |
| 16 | 151 | 34.3 | |
| 17 | 185 | 42.0 | |
| Gender | Male | 267 | 60.7 |
| Female | 173 | 39.3 | |
| Religion | Hindu | 403 | 91.6 |
| Muslim | 28 | 6.4 | |
| Christian | 8 | 1.8 | |
| Others | 1 | 0.2 | |
| Place of residence | Rural | 242 | 55 |
| Urban | 198 | 45 | |
| Monthly income (in Rupees) | ≤6174 | 49 | 11.1 |
| 6175–18,496 | 121 | 27.5 | |
| 18,497–30,830 | 129 | 29.3 | |
| 30,831–46,128 | 34 | 7.7 | |
| 46,129–61,662 | 56 | 12.7 | |
| 61,663–1,23,321 | 48 | 10.9 | |
| ≥1,23,322 | 3 | 0.7 | |
| Educational standard | 8th | 2 | 0.5 |
| 9th | 48 | 10.9 | |
| 10th | 172 | 39.1 | |
| 11th | 135 | 30.7 | |
| 12th | 53 | 12 | |
| College | 24 | 5.5 | |
| Dropped out | 6 | 1.4 | |
| Educational institution | Government | 225 | 51.1 |
| Private | 209 | 47.5 | |
| Dropped out | 6 | 1.4 | |
3.2. Willingness and awareness toward COVID vaccination
The maximum number of adolescents (99.3%) had taken vaccinations on their own initiative. They got information regarding the initiation of the COVID vaccination program for adolescents aged 15–17 years through multiple sources such as the internet (41.8%), family members (30.5%), television & radio (25.9%), friends (19.8%), school teachers (17.5%), Newspaper (13.4%), social media (11.1%), health workers (10%) and posters (5.5%).
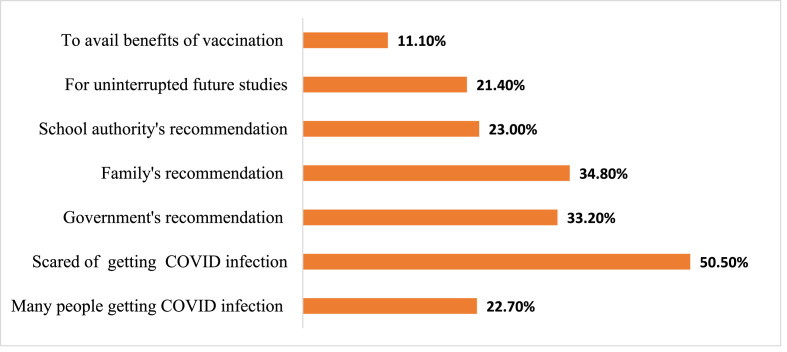
The reason for vaccination was fear of getting COVID-19 infection (50.5%) followed by family recommendation (34.8%) as shown in Fig. 1 .
Fig. 1.
Reasons for willingness toward vaccination.
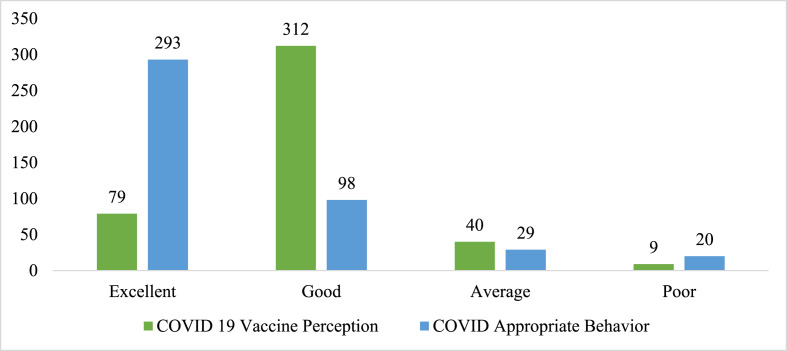
3.3. Perception toward COVID-19 vaccination
The median perception to the COVID-19 vaccination score of the participants was 30. The interquartile range was Q3-Q1 (32–28). Most of the adolescents (70.9%) had a good perception of COVID-19 vaccination [Fig. 2 , Table 2 ].
Fig. 2.
Perception of Participants regarding COVID Vaccination and COVID appropriate behavior.
Table 2.
Perception regarding COVID-19 vaccine n = 440.
| Perception regarding COVID vaccination statements | Strongly agree f (%) |
Agree f (%) |
Neutral f (%) |
Disagree f (%) |
Strongly disagree f (%) |
|---|---|---|---|---|---|
| Will not have COVID-19 infection after vaccination. | 27 (6.1) | 93 (21.1) | 106 (24.1) | 134 (30.5) | 80 (18.2) |
| My vaccination will be beneficial to others | 143 (32.5) | 210 (47.7) | 39 (8.9) | 22 (5) | 26 (5.9) |
| The vaccine may produce side effects | 23 (5.2) | 134 (30.5) | 149 (33.9) | 59 (13.4) | 75 (17) |
| No need to follow COVID appropriate behavior after vaccination | 26 (5.9) | 56 (12.7) | 37 (8.4) | 124 (28.2) | 197 (44.8) |
| After vaccination one can lead a normal life. | 48 (10.9) | 187 (42.5) | 67 (15.2) | 42 (9.5) | 96 (21.8) |
| The vaccine will reduce the severity of COVID -19 infection | 118 (26.8) | 204 (46.4) | 55 (12.5) | 21 (4.8) | 42 (9.5) |
| The vaccine is essential for reopening schools | 226 (51.4) | 165 (37.5) | 22 (5) | 6 (1.4) | 21 (4.8) |
| The vaccine is available in all government health facilities. | 170 (38.6) | 180 (40.9) | 53 (12) | 14 (3.2) | 23 (5.2) |
3.4. COVID appropriate behavior (CAB)
COVID appropriate behavior scores ranged from 12 to 55 and the median score was 47.5. The interquartile range was Q3-Q1 (52–41). Most adolescents (69.8%) had excellent behavior. Detailed COVID Appropriate Behavior (CAB) statement-wise findings are presented [Fig. 2, Table 3 ]. Many adolescents strongly disagree with the statement that they don't need to follow COVID appropriate behavior after vaccination. Half of them (51.4%) perceive that vaccination is essential for reopening schools.
Table 3.
COVID Appropriate Behavior n = 440.
| COVID Appropriate Behavior | Always f (%) | Most of the time f (%) | Occasionally f (%) | Rarely f (%) | Never f (%) |
|---|---|---|---|---|---|
| Greet friends without physical contact. | 145 (33) | 109 (24.8) | 82 (18.6) | 60 (13.6) | 44 (10) |
| Maintain a physical distance of 6 ft from others in public. | 166 (37.7) | 124 (28.2) | 75 (17) | 49 (11.1) | 26 (5.9) |
| Wear a face- mask outside the home | 355 (80.7) | 24 (5.5) | 15 (3.4) | 17 (3.9) | 29 (6.6) |
| Avoid touching eyes, nose, and mouth with unwashed hands | 277 (63) | 63 (14.3) | 31 (7) | 26 (5.9) | 43 (9.8) |
| Cover mouth and nose with a cloth while coughing and sneezing | 321 (73) | 60 (13.6) | 18 (4.1) | 10 (2.3) | 31 (7) |
| Wash hands frequently | 297 (67.5) | 66 (15) | 37 (8.4) | 11 (2.5) | 29 (6.6) |
| Regularly disinfect frequently touched surfaces. | 212 (48.2) | 80 (18.2) | 69 (15.7) | 42 (9.5) | 37 (8.4) |
| No spit in the open space. | 292 (66.4) | 49 (11.1) | 22 (5) | 21 (4.8) | 56 (12.7) |
| Avoid unnecessary travel. | 243 (55.2) | 69 (15.7) | 57 (13) | 33 (7.5) | 38 (8.6) |
| Avoid crowd | 237 (53.9) | 89 (20.2) | 62 (14.1) | 26 (5.9) | 26 (5.9) |
| Do not circulate fake social media posts | 297 (67.5) | 39 (8.9) | 32 (7.3) | 12 (2.7) | 60 (13.6) |
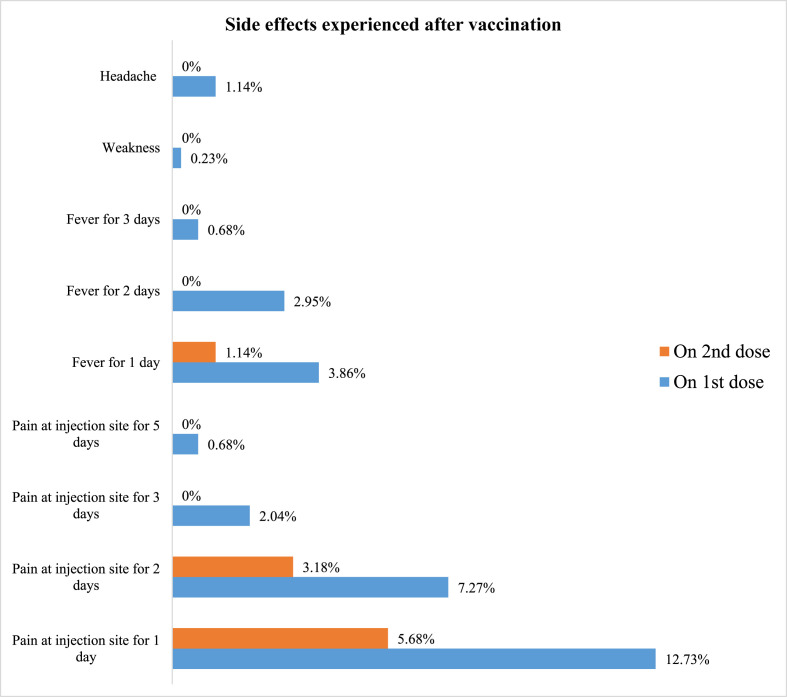
3.5. Compliance with vaccination and post COVID vaccination experience
All participants received two doses of the vaccine. The post-COVID vaccination experiences were collected through telephonic interviews. The telephonic response rate was 95.23% after the 1st dose and 93.64% after the 2nd dose of COVID vaccine. A greater number of participants reported symptoms after their first dose of vaccination than after the 2nd dose [Fig. 3 ]. They experienced pain and fever ranging from one to five days. Pain at the injection site was the most common complaint of adolescents after the first (19.31%) and second (8.63%) doses of vaccination. Commonly reported side effects were headache, body weakness, and fever after the first dose of vaccination but not after the second dose.
Fig. 3.
Symptoms experienced after vaccination.
3.6. Relationship of the perception of COVID vaccination and COVID appropriate behaviors with socio-demographic factors
Perception of COVID vaccination was significantly associated with the residence of the participants and the type of school they were attending. Perception of COVID appropriate behavior was significantly associated with the gender of the participants [Table 4 ]
Table 4.
Relationship of the perception of COVID vaccination and COVID appropriate behaviors with socio-demographic factors.
| Perception | Factor | Group | Excellent F |
Good f |
Average F |
Poor f |
Chi-Square Statistic, p-value |
|---|---|---|---|---|---|---|---|
| Perception of COVID vaccination | Gender | Male | 44 | 190 | 24 | 9 | 6.436, .092 |
| Female | 34 | 123 | 16 | 0 | |||
| Residence | Rural | 41 | 165 | 31 | 5 | 9.030, .029* | |
| Urban | 37 | 148 | 9 | 4 | |||
| Age | 15 y | 21 | 70 | 10 | 3 | 1.379, .967 | |
| 16 y | 25 | 110 | 13 | 3 | |||
| 17 y | 32 | 133 | 17 | 3 | |||
| Type of School | Government | 33 | 167 | 19 | 6 | 16.98, .01* | |
| Private | 45 | 143 | 18 | 3 | |||
| Not enrolled | 0 | 3 | 3 | 0 | |||
| COVID Appropriate Behavior | Gender | Male | 160 | 75 | 19 | 13 | 15.289, .002* |
| Female | 133 | 23 | 10 | 7 | |||
| Residence | Rural | 155 | 59 | 15 | 13 | 2.528, .470 | |
| Urban | 138 | 39 | 14 | 7 | |||
| Age (Years) | 15 | 68 | 27 | 4 | 5 | 4.270, .640 | |
| 16 | 102 | 29 | 11 | 9 | |||
| 17 | 123 | 42 | 14 | 6 | |||
| Type of School | Government | 144 | 55 | 17 | 9 | 11.65, .07 | |
| Private | 147 | 41 | 10 | 11 | |||
| Not enrolled | 2 | 2 | 2 | 0 |
* Statistically significant (p < 0.05).
4. Discussions
Every country in the world has been challenged by the COVID-19 pandemic with more than half a billion cases and around 6 million mortality reported worldwide.16 Health care systems are already overburdened by newer and more infectious variants. It has now become crucial to prevent and slow down the surge of disease. The vaccine is the hope and an effective tool to combat COVID-19. WHO recommends vaccinating at least 70% of the world's population, accounting for most adults and adolescents and for the vast majority of those at risk of serious disease by June 2, 022.1
Willingness toward the COVID-19 vaccine in this study was found to be 99.3%. These findings are much higher than studies done in other places. For instance, 39% of adolescents in Hong Kong,7 50% of children in England,9 75.59% of adolescents in China8 and 80% of adolescents in West Bengal17 accepted COVID vaccine. This indicates that adolescents were well aware of the COVID vaccination drive and wished to take the vaccine to protect themselves and others from COVID-19 which is very beneficial for developing nations like India. Adolescents in this study used various resources to gain information regarding COVID vaccination programs through the internet (41.8%) followed by family members (30.5%), television & radio (25.9%), and only 10% by healthcare workers which is, in contrast, to a study conducted in Jordan where the majority of adults trusted health workers (45.4%), followed by the internet (17.4%), media (16.6%) and family members (3.1%) regarding COVID 19 vaccine.18 Another similar study conducted in Bengal observed that 41.5% of adolescents gained information from TV and 36.9% from the internet.17 This indicates that adolescents are more digitally literate and accept the internet as a source of information. Since the Internet can shape people's minds and act as a strong social force, it is imperative to provide accurate and reliable information through this medium.
In our study, 50.5% of adolescents were willing to take the vaccine due to fear of getting infected with COVID. These findings are consistent with a study conducted in Hong Kong, where 59% of adolescents showed a willingness to vaccinate due to being worried about becoming infected.7 However, our result is lower than a study conducted in China in which 89.7% of people were vaccinated for fear of a COVID infection.8 Nevertheless, these findings are higher than those reported by Bhowmick S,17 in which 19% of adolescents accepted the vaccine for fear of being infected with COVID-19, and 21.5% accepted that many people in their vicinity were infected with COVID-19 infection. In our study, 33.2% of adolescents accepted vaccination as it is recommended by the government which is higher than the findings reported by Bhowmick S17 where 22.7% of adolescents accepted vaccine as per government recommendation. This finding indicates adolescents are concerned about their health and hence, they are taking measures to maintain optimum health.
The majority of adolescents (53.4%) in this study believed that they could return to normal life after the COVID-19 vaccination, which is higher than the previous research reported in West Bengal17 where 33.8% of adolescents and in Hong Kong7 where 42% of adolescents accepted the vaccine to return to normal life before COVID-19. Vaccine safety is a concern for various national immunization programs. Nearly half of the adolescents (48.7%) in the study opined that vaccine would not prevent COVID-19 infection or reduce the severity of COVID (14.3%), which is very higher than the report17 where only 8.07% of adolescents believed that they would not have COVID-19 after vaccination. These findings are much lower than those of the findings by Wong WHS and Leung D7 where 52% of adolescents were concerned about vaccine efficiency. In our study, 35.7% of adolescents perceived that vaccine might produce serious side effects which is higher than Chinese study,8 where only 2.8% of adolescents considered that the COVID-19 vaccine is not safe as it produces obvious side effects and much lower than that of Hong Kong7 study where 79% had a concern about vaccine safety. Around 30.9% of adolescents in the study believed that vaccines are safe which is higher than that of the Chinese study8 in which 20.9% of adolescents regarded that the COVID 19 vaccine is safe and produces a minimal side effect. These findings are significantly lower than that of Bengal study findings where 78.8% of adolescents regarded the COVID-19 vaccine as safe.17 Hence disseminating accurate and transparent information regarding the COVID-19 vaccine through appropriate media is essential to increase coverage as well as acceptance among adolescents. Most adolescents (80.2%) believed that their vaccination would be beneficial to others. There is a wide range of perceptions around vaccine benefit for community members and family members, ranging from 42.5% to 79.4% in US.19, 20, 21
Most adolescents (88.9%) in this study believed that adolescent vaccination is necessary to reopen the school which is consistent with reports in West Bengal17 where 81.9% of adolescents considered vaccination important for resuming school activities.
Around 66.6% of adolescents reported excellent while 22.3% of adolescents reported good practice related to CAB which is much higher than a study conducted in West Bengal17 where 58.0% of adolescents reported good practice related to CAB. The majority of adolescents (70.9%) had a good perception of the COVID-19 vaccine which is consistent with findings reported by Bhowmick S17 were that 74.6% of adolescents had a good attitude towards the COVID-19 vaccine.
This is the first study of its kind that explore the adolescents’ perception of vaccination, their COVID-appropriate behavior, compliance with two doses of COVID-19 vaccines and the experienced side effects. There are a few limitations to the study, including study conducting in single-center and self-reported behavior. As a result, generalizability of the study is limited. The possibility of socially desirable responses can also not be ruled out due to the COVID Vaccination Center being the site for data collection. A similar study in different settings needs to be replicated.
5. Conclusion
The majority of adolescents had a good perception regarding COVID-19 vaccination demonstrating a high level of acceptance toward COVID 19 vaccine and excellent COVID Appropriate behavior.
Funding details
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical consideration
Ethical approval was obtained from the Institutional Ethical Committee (IEC/AIIMS Kalyani/2022/19).Administrative permission was taken from appropriate authority.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
Our sincere thanks to COVID Vaccination Centre AIIMS Kalyani for their cooperation.
References
- 1.WHO Strategy to Achieve Global Covid-19 Vaccination by mid-2022. 2022:1–16. https://cdn.who.int/media/docs/default-source/immunization/covid-19/strategy-to-achieve-global-covid-19-vaccination-by-mid-2022.pdf Who [Internet] [Google Scholar]
- 2.https://www.who.int/health-topics/coronavirus#tab=tab_1 WHO. Coronavirus Disease [Internet]. World Health Organisation. WHO Coronavirus (COVID-19). 2022. Available from:
- 3.The Hindu. World's largest vaccination programme begins in India on January 16. Hindu. 2021 https://www.thehindu.com/news/national/coronavirus-worlds-largest-vaccination-programme-begins-in-india-on-january-16/article33582069.ece [Internet] [Google Scholar]
- 4.Bbc . 2022. Covid Vaccine: India Starts Jabs for 12- to 14-Year-Olds.https://www.bbc.com/news/world-asia-india-56345591 BBC [Internet] [Google Scholar]
- 5.Chandani S., Jani D., Sahu P.K., et al. COVID-19 vaccination hesitancy in India: state of the nation and priorities for research. Brain, Behav Immun - Heal. 2021;18(October doi: 10.1016/j.bbih.2021.100375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.MacDonald N.E., Eskola J., Liang X., et al. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 7.Wong W.H.S., Leung D., Chua G.T., et al. Adolescents' attitudes to the COVID-19 vaccination. Vaccine. 2022;40(7):967–969. doi: 10.1016/j.vaccine.2022.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cai H., Bai W., Liu S., et al. Attitudes toward COVID-19 vaccines in Chinese adolescents. Front Med. 2021;8(July:1–6. doi: 10.3389/fmed.2021.691079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fazel M., Puntis S., White S.R., et al. Willingness of children and adolescents to have a COVID-19 vaccination: results of a large whole schools survey in England. eClinicalMedicine. 2021:40. doi: 10.1016/j.eclinm.2021.101144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yigit M., Ozkaya-Parlakay A., Senel E. Evaluation of COVID-19 vaccine refusal in parents. Pediatr Infect Dis J. 2021;40(4):E134–E136. doi: 10.1097/INF.0000000000003042. [DOI] [PubMed] [Google Scholar]
- 11.Bell S., Clarke R., Mounier-Jack S., Walker J.L., Paterson P. Parents' and guardians' views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. 2020;38(49):7789–7798. doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pierantoni L., Lenzi J., Lanari M., et al. Nationwide COVID-19 survey of Italian parents reveals useful information on attitudes to school attendance, medical support, vaccines and drug trials. Acta Paediatr Int J Paediatr. 2021;110(3):942–943. doi: 10.1111/apa.15614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yucheng X., Ruiyin Z., Zhifeng Z., et al. Parental psychological distress and attitude toward COVID-19 vaccination: a cross sectional survey in Shenzhen,China. J Affect Disord. 2021;291:552–558. doi: 10.1016/j.jad.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chandani S., Jani D., Sahu P.K., et al. COVID-19 vaccination hesitancy in India: state of the nation and priorities for research. Brain, Behav Immun - Heal. 2021;18(October doi: 10.1016/j.bbih.2021.100375. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kishore J., U V., Ghai G., Heena Prem K. Perception and attitude towards COVID-19 vaccination: a preliminary online survey from India. J Fam Med Prim Care. 2021;10(8):3116–3121. doi: 10.4103/jfmpc.jfmpc_2530_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO. WHO COVID Dashboard https://covid19.who.int/ WHO [Internet]
- 17.Bhowmick S., Dhankher R., Mukhopadhyay A. An exploratory study to assess the acceptance and attitude towards COVID-19 vaccination among school-going adolescents aged 15-17 years in selected schools of Nadia district an exploratory study to assess the acceptance and attitude towards COVID-19 vaccine. Int J Community Med Public Heal. 2022;9(6):2701–2705. [Google Scholar]
- 18.El-Elimat T., AbuAlSamen M.M., Almomani B.A., Al-Sawalha N.A., Alali F.Q. Acceptance and attitudes toward COVID-19 vaccines: a cross-sectional study from Jordan. PLoS One. 2021;16(4 April):1–15. doi: 10.1371/journal.pone.0250555. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohamed N.A., Solehan H.M., Mohd Rani M.D., Ithnin M., Isahak C.I.C. Vaccine Among Malaysians: A Web-Based Survey. Vol. 16. PLoS ONE; 2021. Knowledge, acceptance and perception on COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Danabal K.G.M., Magesh S.S., Saravanan S., Gopichandran V. Attitude towards COVID 19 vaccines and vaccine hesitancy in urban and rural communities in Tamil Nadu, India – a community based survey. BMC Health Serv Res. 2021;21(1):1–10. doi: 10.1186/s12913-021-07037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daly M., Robinson E. Willingness to vaccinate against COVID-19 in the U.S.: representative longitudinal evidence from april to october 2020. Am J Prev Med [Internet] 2021;60(6):766–773. doi: 10.1016/j.amepre.2021.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]