Abstract
Background:
Although plausible from a pathophysiological point of view, robust evidence for effects of transportation noise on mental health remains scarce. Meanwhile, psychiatric diseases are among the most prevalent noncommunicable diseases worldwide, and suicide as a mortality outcome highly connected to mental disorders presents a pressing public health issue. The aim of this study was to investigate the association between source-specific transportation noise, particulate matter (PM) air pollution, residential greenness, and suicide by means of a nationwide cohort study.
Methods:
Road traffic, railway and aircraft noise exposure as well as exposure to air pollution [PM with aerodynamic diameter ()] and greenness [normalized difference vegetation index (NDVI)] were linked to 5.1 million adults (age 15 y and older) in the Swiss National Cohort, accounting for their address history. Mean noise exposure in 5-y periods was calculated. Individuals were followed for up to 15 y (2001–2015). Time-varying Cox regression models were applied to deaths by suicide (excluding assisted suicide). Models included all three noise sources, , and NDVI plus individual and spatial covariates, including socioeconomic status. Effect modification by sex, age, socioeconomic indicators, and degree of urbanization was explored.
Results:
During the follow-up, there were 11,265 suicide deaths (10.4% poisoning, 33.3% hanging, 28.7% firearms, 14.7% falls). Road traffic and railway noise were associated with total suicides [hazard ratios: 1.040; 95% confidence interval (CI): 1.015, 1.065; and 1.022 (95% CI: 1.004, 1.041) per 10 dB day-evening-night level (Lden)], whereas for aircraft noise, a risk increase starting from 50 dB was masked by an inverse association in the very low exposure range (30–40 dB). Associations were stronger for females than males. The results were robust to adjustment for residential greenness and air pollution.
Conclusion:
In this longitudinal, nationwide cohort study, we report a robust association between exposure to road traffic and railway noise and risk of death by suicide after adjusting for exposure to air pollution and greenness. These findings add to the growing body of evidence that mental health disorders may be related to chronic transportation noise exposure. https://doi.org/10.1289/EHP11587
Introduction
Mental health disorders represent a pressing public health issue. In 2019, the prevalence of mental health disorders globally was estimated to be 13% [95% confidence interval (CI): 12.1, 14.0%], which translates to almost 1 billion people affected. In Switzerland, the estimated prevalence was slightly higher with 17.3% (95% CI: 15.9, 18.8%), translating to about 1.4 million people affected.1 Although most mental health disorders primarily lead to morbidity and decreased quality of life, a mortality outcome closely related to mental illness is suicide.2,3 Suicide is a complex, multicausal phenomenon, involving psychological, social, biological, and environmental factors. A study on suicide in the Swiss National Cohort confirmed that mental and behavioral problems were by far the most prevalent comorbidities in suicide victims across all professions, age groups, and genders.4 Only recently research has started to also explore and identify possible environmental risk factors for suicide, with reported associations of an increased suicide risk with heat,5 air pollution.6 and noise.7 On the other hand, residential greenness and urban green space have been recognized as environmental factors with protective properties.8 Although suicide rates have decreased worldwide and in Switzerland in the last 20 y, the decline is not yet on course to reach the Sustainable Development Goal (SDG) aim of a reduction by one-third by 2030. The World Health Organization (WHO) report, “Suicide Worldwide in 2019,” published in 2021, estimated that 703,000 people died from suicide in 2019 worldwide, which corresponds to 1.3% of all yearly deaths.9 On the grounds of such numbers, reducing the occurrence of mental illnesses is a primary public health interest. Hence, understanding risk factors for the development of mental disorders and therefore for suicide is of utmost importance. In light of the growing urbanization worldwide, studying the role of urban environmental stressors as such potential risk factors can potentially yield insights of consequential importance concerning the promotion of mental health and prevention of psychiatric morbidity and mortality.
In recent years, noise has been recognized as one of the most impactful environmental stressors on health and well-being.10 Among the sources of environmental noise, transportation noise and especially road traffic noise have emerged as the most prevalent and harmful. According to a European Environmental Agency (EEA) report, 20% of the European population (139 million people) in 2017 were estimated to live in areas with transportation noise levels that are considered harmful [ dB day-evening-night level (Lden)].10 A more recent study investigating noise exposure in 700 cities in Europe estimated that 42% of the adult urban population are exposed to such harmful levels.11 Due to this widespread occurrence, noise is the second most important driver of the environmental burden of disease in Europe, behind fine particulate matter (PM) air pollution. In numbers, exposure to transportation noise is estimated to be responsible for 400–1,500 disability adjusted life years lost each year per million people in Western Europe.12 However, because more evidence including more outcomes has emerged since 2014, and, for example, effects on mental health were not included in the above-mentioned calculations, these numbers might actually represent an underestimation.
Concerning negative health effects related to noise exposure, there is growing evidence for diverse nonauditory effects, such as arterial hypertension, cardiovascular and metabolic diseases such as type 2 diabetes,13–16 sleep disturbance,17 annoyance,18 as well as reduced quality of life and well-being19—and mental health and neurological disorders.20 Although the exact pathways of the influences of noise on health remain somewhat unclear, there is evidence that noise causes physiological stress reactions involving heightened amygdalar activity,21 allostatic overload,13,15 and disturbed sleep.22 Because these are all established risk factors for multiple mental health disorders, including depression,23–27 an association of noise with poor mental health seems plausible from a pathophysiological perspective. However, the systematic review on noise-related mental health outcomes used for the 2018 WHO guidelines resulted in a judgment of very low-quality evidence for aircraft noise effects on depression and anxiety and a judgment of low-quality evidence for a null effect of road traffic or railway noise.28 The review included 29 predominantly cross-sectional studies. Hence, the poor quality of evidence was attributed to a lack of robust studies investigating the mental health effects of different noise sources. A more recent meta-analysis of five studies found an increased risk of 12% (95% CI: 2%, 23%) for depression per 10 dB Lden of aircraft noise exposure.29 The same study29 also suggested a 2%–3% increased risk for depression per 10 dB Lden for railway noise based on three studies and for road traffic noise based on eleven studies. Another review and meta-analysis including nine studies showed an association between transportation noise and anxiety [; 95% CI: 0.97, 1.23 per 10 dB], while also rating the quality of evidence as low.30 Since the publication of this meta-analysis, a Swiss prospective cohort study (SAPALDIA) reported a 7% increased risk for the incidence of depression per 10 dB Lden road traffic noise [; 95% CI: 0.93, 1.22] and a 20% increased risk per 10 dB Lden aircraft noise (; 95% CI: 0.92, 1.55). So far, only one study investigating the associations between long-term exposure to environmental noise and suicide has been conducted.7 The authors examined the risk for death by suicide in relation to average nighttime noise exposure (including noise caused by transportation and industrial and recreational activities) in adults in Korea and reported an increased risk per interquartile range () of nighttime noise of 32% (95% CI: 2%, 70%) in younger adults and 43% (95% CI: 1%, 102%) in older adults. A time-series study from Spain investigating short-term effects of traffic noise exposure on suicides and emergency admission for depression and anxiety reported an increased risk for both outcomes.31
In comparison, the effects of air pollution on mental health have received more attention and have been studied more thoroughly. Air pollutants have been shown to cause oxidative stress and neuroinflammation and to trigger stress responses with stress hormone release, which are the major hypothesized mechanisms linking air pollution and adverse mental health outcomes.32,33 A systematic review and meta-analysis published in 2022 including 39 studies reported significant associations between long-term exposure to various air pollutants (, , , CO) and risk of depression. The largest risk increase was observed for PM with aerodynamic diameter () [ (95% CI: 0.988, 1.206) per increase in exposure]. Smaller effects were also reported per increase of short-term exposure to [ (95% CI: 1.007, 1.011)], [ (95% CI: 1.006, 1.012)], [ (95% CI: 0.997, 1.026)], [ (95% CI: 1.012, 1.033)] and [ (95% CI: 1.010, 1.037)].34 Another systematic review and meta-analysis from 2019 found similar results for depression, and also reported associations between short-term exposure and suicide risk [ (95% CI: 1.00, 1.03) per at lag 0–2 d, including four studies].6 These results were compiled in a more recent systematic review and meta-analysis from 2021 that included 10 studies, reporting a 2% (95% CI: 1%, 3%) risk increase for suicide per exposure.35 One limitation of these reviews is that most of the included studies have not adjusted for exposure to possible confounders such as transportation noise. A recent large cross-sectional study from the UK Biobank studying and road traffic noise exposure, however, reported an increased risk for depression associated with exposure, but no association with road traffic noise exposure was found.36
Residential greenness or green space is another exposure of interest in environmental epidemiology as a protective factor for health and well-being. For example, higher levels of greenness [normalized difference vegetation index (NDVI)] around people’s place of residence have been associated with a lower risk of natural-cause mortality [ (95% CI: 0.93, 0.95) per IQR (0.14 NDVI in a 500-m buffer)] in a large Swiss cohort study.37 Concerning mental health, a Dutch study found a decreased risk for death by suicide in communities with high green space proportion () in comparison with communities with little () green space [ (95% CI: 0.779, 0.991)].38 Beyond suicide, a systematic review from 2020 suggested several beneficial effects of access to green space on adolescents’ mental health, including fewer depressive symptoms and improved general mental health.39 Multiple pathways are posited for this positive association, including that greener living environments or green space availability encourage healthy behavior, and that such factors can aid in stress relief.40
This study investigates the association between exposure to road traffic, railway, and aircraft noise and the risk of death by suicide in a longitudinal, nationwide research cohort in Switzerland. We hypothesized that people exposed to higher levels of transportation noise are more likely to develop mental health disorders such as depression and therefore have a higher risk of death by suicide, independent of coexposure to air pollution and residential greenness as well as socioeconomic position. By using suicide as a surrogate, we aimed to add to the understanding of whether transportation noise exposure affects mental health.
Methods
Study Population
The Swiss National Cohort (SNC) is a longitudinal, population-based research cohort. It links births, mortality, and emigration registries with the former national decennial census and, since 2010, with the annual Registry Based Census.41,42 The linkages in the SNC from 2010 onward are deterministic using a personal identifier, whereas earlier linkages were performed probabilistically based on variables such as date of birth, sex, civil status, nationality, religion, and place of residence. No validation of the probabilistic linkage is available, but comparison with the deterministic linkages from 2010 and onward allows the discovery and exclusion of mismatches. Close to complete representation of the whole population is ensured by compulsory census participation, which is reflected in 98.6% of the population being included in the 4 December 2000 census.43 The SNC was approved by the ethics committees of the Cantons of Zurich and Berne.
For the current study, we used the SNC as a closed cohort that included data from 1 January 2001 to 31 December 2015 for a total of 7.28 million individuals. After excluding individuals below 15 y of age at baseline (17.5% of the full population), data with a mismatch between probabilistic and deterministic SNC linkage (i.e., incorrect probabilistic linkage, 8.2%), missing residential coordinates or individuals living in an institution (5.4%), missing information on covariates (i.e., education or socioeconomic position) (2.5%), or missing exposure data (0.2%), the final sample used for analysis consisted of 5.1 million observations (See Supplement Table S1). No imputations were performed.
Outcome
The outcome of interest was defined as all intentional self-harm [i.e., total suicides; International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10): X60–84, excluding X61.8, X61.9, and X81–82] as cause of death. The SNC contains records from all deaths occurring in Switzerland from 1991 up to 2019 that included cause of death as ICD codes. Regarding exclusions, ICD-Codes X61.8 (right-to-die organization on death certificate) and X61.9 (Poisoning with pentobarbital; the drug used by right-to-die organizations) have been used to indicate assisted suicide since 1998.44 Additionally, we suspected suicides involving vehicles (ICD-10: X81–82) to be spuriously associated with railway noise, due to confounding by proximity and therefore availability of the method. Because preliminary analysis confirmed this suspicion (see Figure S1), these outcomes were also excluded from the main analysis. The specific suicide subclasses Poisoning (ICD10: X60–69, excluding X61.8 and X61.9), Hanging (ICD-10: X70), Firearms (ICD-10: X72–75) and Jumping (ICD-10: X80) were also investigated separately.
Noise Exposure Data
The same noise exposure data used in a previous publication investigating cardiovascular disease and transportation noise in the SNC was used in our study.45 These data were originally developed for the Short and Long Term Effects of Transportation Noise Exposure (SiRENE) project and were available for census years 2001 and 2011.46,47 The database contains modeled noise exposure levels for the three main sources of transportation noise, using the following calculation methods: road traffic (source model sonROAD48 and propagation model StL-8649) railways (source model sonRAIL50 and propagation model SEMIBEL51) and aircraft (FLULA252,53). Concerning aircraft noise, the model included estimates based on air traffic data of the three international civil airports (Zurich, Geneva, and Basel), as well as for the largest military airfield situated in Payerne.
The main noise metric used was the source-specific Lden, which is a weighted logarithmic mean of daily noise exposure with a penalty of 5 dB for evening (1900–2300 hours) and 10 dB for nighttime (2300–0700 hours) noise. The intermittency ratio (IR)54 during the night was also available. This noise metric describes how impactful single noise events are in contrast to background noise. The values of IR range from 0%, meaning single events do not substantially exceed long-term average noise, to 100%, meaning that all noise exposure is produced by individual noise events. Additionally, the number of nighttime noise events (i.e., events 3 dB louder than background noise) was available. Both nighttime IR and number of events were not source-specific but calculated considering all three noise sources. Source-specific Lden at the most exposed façade and corresponding IR as well as the number of events were assigned to participants based on residential location (geocode and floor of residence, using a default middle floor of the building if exact floor was not known55,56). To account for background noise from various sources, Lden values were left censored at 35 dB for road traffic noise and 30 dB for railway and aircraft noise.56
Noise Exposure Assignment
As described in Vienneau et al.,45 the follow-up was divided into three 5-y periods (2001–2005, 2006–2010, 2011–2015) to support time-varying analysis accounting for potential time trends and changes of residence.57 Both residential geocodes and noise estimates were available for 2001 and 2011. Hence, the 2001 noise exposure estimates were assigned for the first period (2001–2005) and the 2011 noise exposure estimates to the third period (2011–2015), based on the residential address at the beginning of the period. Using the 2010 census question “living in the same community 5 years before” and moving dates, the exposure assignment for the middle period was constructed as follows. For people who had not moved or moved after 2006, the 2001 noise data was used for the middle period (2006–2010) because these participants were believed to still be living at the same residence that they lived at in 2001. For people who moved before 2006, the 2011 noise data and updated residential geocodes were used for the middle period (2006–2010).
Covariates
A directed acyclic graph (DAG) was drawn to identify potentially confounding factors (Figure S2). This led to the identification of the following factors: degree of urban, air pollution, green space, civil status, and socioeconomic position. The following individual sociodemographic variables available from the SNC were included to represent socioeconomic position: education level (compulsory education or less, upper secondary level education, tertiary level education), mother tongue (German and Rhaeto-Romansh, French, Italian, other language), nationality (Swiss, non-Swiss), and local index of socioeconomic position (local SEP in quartiles). The local-SEP index used is calculated for a small local area of 50 nearest neighbors and considered median rent per living space, education level and type of occupation of the household head and number of inhabitants per room.58 Additionally, civil status (single, married, widowed, divorced) and degree of urban (urban, peri-urban, rural) were included as potential confounders and sex (female, male) as a covariate. The definition of degree of urban was performed for every community by the Swiss Federal Office for statistics based on morphological criteria such as population number and density as well as functional criteria such as commuter flows59 and is part of the SNC data set. Because socioeconomic status was identified as one of the most important possible confounders in this study, area-level SEP and unemployment rate were also calculated at community ( in 2001, in 2011) and cantonal () level to reflect different aspects of SEP on different levels. The community- and cantonal-level SEP variables were derived by averaging the local-SEP index of all individuals within the respective area. Unemployment rates were available from the SNC and defined as percentage of the working-age population (20–65 y) unemployed. All covariates were available at baseline in 2001, whereas some covariates were also available at the start of the third period coinciding with the 2011 census. Those updated included civil status, nationality, local SEP, area SEP, and unemployment rate, whereas for other variables the baseline values were retained.
Concerning potentially confounding environmental exposures, concentration (micrograms per cubic meter) was selected as marker for air pollution in the main model, whereas concentrations (micrograms per cubic meter) were used for sensitivity analyses. Maps for both pollutants for the year 2010 were available from validated European hybrid land use regression models developed based on AirBase routine monitoring data, satellite observations, dispersion model estimates, and land use and traffic data. The model predictions for 2010 correlated highly with predictions in other years60; thus the 2010 estimates were considered relevant for all three 5-y periods. Air pollution exposure was updated according to residence history at the beginning of each of the three time periods.
As a possible confounder, greenness measured as mean NDVI with a 500-m buffer around participants’ addresses was included as a covariate in the main model. NDVI exposure derived from a data set for 2014 previously constructed for and used in the SNC (using resolution, cloud-free Landsat scenes from summer months).37 NDVI exposure was applied to the geocodes at the beginning of each of the three time periods (2001, 2006, and 2011), thus updating residential greenness for individuals who moved during our study period.
Statistical Analysis
The Cox proportional hazards model was applied to assess associations between death by all intentional self-harm (ICD-10: X60–84, excluding X61.8, X61.9, and X81–82) as well as the specific outcome subclasses [Poisoning (ICD10: X60–69, excluding X61.8 and X61.9), Hanging (ICD-10: X70), Firearms (ICD-10: X72–75), and Jumping (ICD-10: X80)] and exposure to each transportation noise source, air pollution, and NDVI, with age as timescale and stratified by sex. Adherence to the proportional hazards assumption was tested by calculating covariate-specific Schoenfeld residuals over time. Sex, time period, local SEP, civil status, and education level were included as strata because these covariates violated the proportional hazards assumption. To consider residential history and adjust for time trends in noise exposure and mortality, calendar time was adjusted for by dividing follow-up into three periods of 5 y each (2001–2005, 2006–2010, 2011–2015). Follow-up was continued until failure (i.e., death by suicide) or censoring (i.e., death by any other cause; emigration) or end of the follow-up period on 31 December 2015. Because some participants have exposure to more than one transportation noise source, we included road traffic, railway, and aircraft noise as well as air pollution and NDVI in a single model. As done previously,55 this approach allows identification of mutually independent associations of any single exposure with the outcome. Results were calculated and reported as hazard ratio (HR) and 95% CIs per 10-dB increase in Lden for each transportation noise source, per increase in concentration and per 0.1 increase in NDVI.
E-values were calculated for the main findings. The e-value is a measure for the potential effect of residual confounding, which is interpreted as the strength of association that an unmeasured confounder would need to have with both the exposure and the outcome, conditional on the measured covariates in the model, to be fully responsible for the observed exposure–outcome association.61 The absolute excess risk for the main findings was calculated by multiplying the suicides/100,000 person-years (PY) by the excess risk (HR-1). Natural splines with 3 degrees of freedom (df) were used to assess the exposure–response relationship.
Incremental model adjustments were applied. Model 0, or the base model, included the Lden variables for the three noise sources, age as time scale, strata sex, and 5-y period. In model 1, the individual sociodemographic covariates (civil status, education, mother tongue, nationality, local-SEP index) were added. Model 2 added to model 1 the area-SEP and unemployment variables. Model 3 additionally adjusted for air pollution measured as continuous exposure and NDVI. As a sensitivity analysis, Model 3b included continuous exposure instead of . Two additional models also included noise eventfulness at night, parameterized in model 4a as quartiles of IR and in model 4b as quartiles of number of events. Variance inflation factor () was used a posteriori to evaluate multicollinearity between the three Lden variables, IR, number of events, and the air pollution variables.62,63 Pearson correlation coefficient was calculated to describe correlation between the different exposures.
The main analysis was conducted for the full cohort, combining both sexes and all ages. Separate HRs were also calculated for males and females, and for three separate age groups (15–29, 30–65, over 65 y). Effect modification by SEP was explored by stratifying the analysis by quartiles of the local-SEP index. Additional analyses included stratified analysis by degree of urban and civil status (married vs. single/divorced/widowed). Interaction between air pollution and road traffic noise was investigated using a model with categorical exposures corresponding to quartiles. Likelihood-ratio testing was applied to test whether the interaction term improved model fit. A separate analysis was conducted that investigated the risk in groups exposed to one, two, or three noise sources above 50 dB Lden in comparison with that of participants with exposure to all sources below 50 dB (). This cutoff was determined based on the shape of the exposure–response functions we derived in this study, as well as the distribution of noise in our sample. This last analysis was adjusted for , NDVI, and the same individual sociodemographic and regional covariates as in the main analysis.
Analyses were conducted in Stata 16 (StataCorp LLC), and plots and splines were developed in R (version 4.0; R Development Core Team).
Results
Study Population
A total of 5,084,838 individuals living in Switzerland and age 15 y or older at baseline (1 January 2001) were included (Table 1). Follow-up lasted until 31 December 2015, resulting in 69,440,133 PY. Our sample consisted of slightly more females (51.6%), individuals with mostly Swiss nationality (81.4%), and predominantly speaking German (or Rhaeto-Romansh) as native language (65.1%). A majority were married (60.3%) and had more than compulsory education (71.7%). Almost half of the study population lived in peri-urban settings (45%), with more similar proportions living in urban (29.1%) and rural (25.9%) areas.
Table 1.
Population characteristics of the eligible participants from the Swiss National Cohort at baseline (2001).
| Characteristic | 2001 (Baseline) |
|---|---|
| Number of participants | 5,084,838 |
| Sex [% (n)] | |
| Female | 51.6% (2,624,262) |
| Male | 48.4% (2.460,576) |
| Age [% (n)] | |
| 15–29 y | 18.7% (948,618) |
| 30–64 y | 62.2% (3,163,489) |
| 19.1% (972,731) | |
| Mother tongue [% (n)] | |
| German and Rhaeto-Romansh | 65.1% (3,312,465) |
| French | 19.7% (999,495) |
| Italian | 7.1% (360,538) |
| Other | 8.1% (412,340) |
| Education [% (n)] | |
| Compulsory education or less | 27.5% (1,398,715) |
| Upper secondary level | 51.8% (2,633,811) |
| Tertiary level education | 19.9% (1,011,479) |
| Child/unknown | 0.8% (40,833) |
| Urbanization [% (n)] | |
| Urban | 29.1% (1,478,470) |
| Peri-urban | 45% (2,289,923) |
| Rural | 25.9% (1,316,445) |
| Marital status [% (n)] | |
| Single | 26% (1,321,024) |
| Married | 60.3% (3,066,705) |
| Divorced | 7% (355,994) |
| Widowed | 6.7% (341,115) |
| Nationality [% (n)] | |
| Swiss | 81.4% (4,137,934) |
| Non-Swiss | 18.6% (946,904) |
| Local-SEP [mean (SD)] | 63.0 (10.6) |
| Area SEP region [mean (SD)] | 62.8 (4.2) |
| Area SEP community-region [mean (SD)] | 0.04 (5.2) |
| Area unemployment community [%, mean (SD)] | 3.5 (0.7) |
| Area unemployment community-region [%, mean (SD)] | 0 (1.2) |
Note: SD, standard deviation; SEP, socioeconomic position.
During the 15-y follow-up period, 11,265 deaths from intentional self-harm (excluding assisted suicide and suicide involving vehicles) occurred. Of these, 14.0% concerned people between 15 and 30 y of age, 64.8% people between 31 and 65 y, and 21.2% people older than 65 y. Roughly three-quarters (74.1%) of the deceased by suicide were males.
The mean exposure for road traffic noise was highest (54.4 dB Lden), followed by railway noise (38.6 dB) and aircraft noise (34.5 dB) (Table 2). Correlations between the different noise sources were low (Pearson ). Both and concentrations were somewhat correlated with aircraft noise ( and 0.40, respectively), although only showed some correlation with road traffic noise (; for ). Correlation between the two air pollutants was high (). See Figure S3 for the full correlation matrix.
Table 2.
Levels of the different environmental exposures of the eligible participants from the Swiss National Cohort at baseline (2001).
| Exposure | Mean (SD) |
|---|---|
| Road traffic noise [Lden (dB)] | 54.4 (8.2) |
| Railway noise [Lden (dB)] | 38.6 (11.1) |
| Aircraft noise [Lden (dB)] | 34.5 (7.8) |
| concentration () [mean (SD)] | 15.9 (2.4) |
| concentration () [mean (SD)] | 23.7 (7.5) |
| NDVI exposure (no unit) [mean (SD)] | 0.57 (0.11) |
Note: dB, decibel; ICD, International Statistical Classification of Diseases and Related Health Problems, 10th Revision; Lden, day-evening-night level; NDVI, normalized difference vegetation index; SD, standard deviation.
Main Findings
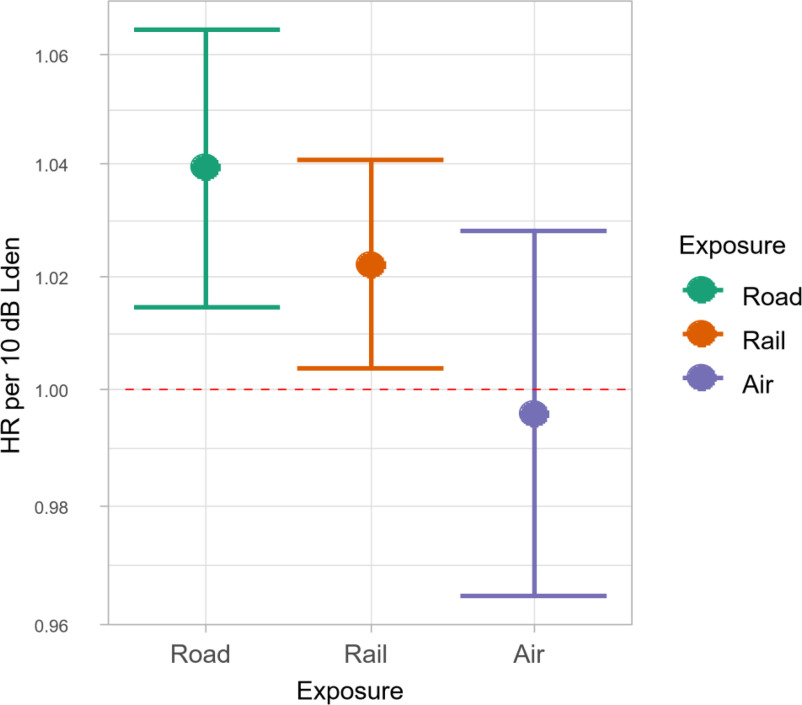
Road traffic noise was associated with an increased risk of death by suicide in all of the models, with an HR of 1.040 (95% CI: 1.015, 1.065) per 10-dB increase in noise exposure in the full model (Model 3) adjusting for SEP, exposure, and NDVI at place of residence (Figure 1; Table 3). Railway noise exposure was also associated with an increased risk of death by intentional self-harm, but it was of a smaller magnitude (; 95% CI: 1.004, 1.041). For aircraft noise, no linear association was observed (; 95% CI: 0.965, 1.029). These results were robust across models, with smaller effect estimates mainly for road traffic noise after adding individual sociodemographic covariates (Model 0 to Model 1), but otherwise no major changes in the tendencies of the observed associations (Table S2). The observed increased risks translate to an absolute excess risk of 0.63 additional suicide deaths/100,000 PY for each 10-dB increase in road traffic noise and 0.36 additional suicide deaths/100,000 PY for each 10-dB increase in railway noise.
Figure 1.
Association (HR and 95% CI) between transportation noise source (Lden) and mortality from all intentional self-harm (Main Model 3). Results from main model (M3) including noise exposures (road traffic noise, railway noise, and aircraft noise), exposure, NDVI, age as timescale, sex as strata, individual sociodemographic covariates (civil status, education, mother tongue, nationality, urbanization, local SEP) and area covariates (area SEP-Index and unemployment rate). Outcome is mortality from intentional self-harm (ICD-10: X60–84, excl. ICD-10 X61.8, X61.9, X81–82). The numerical values of the results displayed in this figure can be found in Table 3. Note: CI, confidence interval; HR, hazard ratio; ICD-10, International Statistical Classification of Diseases and Related Health Problems, 10th Revision; NDVI, normalized difference vegetation index; SEP, socioeconomic position.
Table 3.
HR (95% CI) per 10-dB increase in Lden, 10- increase in , and 0.1 increase per 0.1 NDVI for death by intentional self-harm, in mutually adjusted models.
| All intentional self-harm (ICD-10: X60–84, excluding X61.8, X61.9 and X81–82; N ) | Poisoning (X60–69) | Hanging (X70) | Firearms (X72–75) | Jumping (X80) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All () | Male () | Female () | Age 15–30 y () | Age y () | Age () | All () | All () | All () | All () | |
| Road traffic noise | 1.040 (1.015, 1.065)a | 1.034 (1.006, 1.063) | 1.058 (1.007, 1.112) | 1.079 (1.011, 1.152) | 1.05 (1.019, 1.082) | 0.994 (0.944, 1.046) | 1.106 (1.025, 1.193) | 1.060 (1.017, 1.105) | 1.007 (0.963, 1.053) | 1.009 (0.964, 1.055) |
| Railway noise | 1.022 (1.004, 1.041)b | 1.021 (1.000, 1.043) | 1.028 (0.992, 1.066) | 0.982 (0.934, 1.032) | 1.027 (1.004, 1.051) | 1.037 (0.998, 1.077) | 1.053 (0.997, 1.111) | 1.006 (0.974, 1.039) | 1.014 (0.980, 1.050) | 1.015 (0.98, 1.051) |
| Aircraft noise | 0.997 (0.965, 1.029) | 0.995 (0.959, 1.032) | 1.005 (0.943, 1.071) | 0.983 (0.901, 1.072) | 1.015 (0.976, 1.056) | 0.950 (0.887, 1.017) | 0.994 (0.902, 1.094) | 0.970 (0.917, 1.027) | 0.989 (0.933, 1.049) | 0.991 (0.935, 1.051) |
| 0.900 (0.811, 0.998) | 0.899 (0.798, 1.012) | 0.918 (0.74, 1.137) | 0.978 (0.734, 1.303) | 0.882 (0.776, 1.002) | 0.915 (0.729, 1.149) | 0.943 (0.671, 1.324) | 0.913 (0.767, 1.086) | 0.961 (0.792, 1.167) | 0.906 (0.745, 1.101) | |
| NDVI | 0.999 (0.978, 1.020) | 1.016 (0.992, 1.041) | 0.946 (0.908, 0.986) | 1.002 (0.948, 1.058) | 0.986 (0.961, 1.012) | 1.036 (0.991, 1.084) | 0.923 (0.868, 0.982) | 1.042 (1.005, 1.081) | 1.051 (1.009, 1.094) | 1.048 (1.007, 1.091) |
Note: Results from main model (M3) including noise exposures (road traffic noise, railway noise, and aircraft noise), exposure, NDVI within 500 m around the residence, age as timescale, sex as strata, individual sociodemographic covariates (civil status, education, mother tongue, nationality, urbanization, local SEP) and area covariates (area SEP-Index and unemployment rate). CI, confidence interval; HR, hazard ratio; Lden, day-evening-night level; NDVI, normalized difference vegetation index.
The E-value is a measure for the minimum strength of association that an unmeasured confounder would need to have with both the exposure and the outcome, conditional on the measured covariates, to fully explain the observed exposure–outcome association.
E-Value for point estimate = 1.24.
E-Value for point estimate = 1.17.
The observed tendencies were consistent across all outcome subgroups, with the exception of intentional self-harm involving guns, where no associations with transportation noise from any source were observed (Figure S4). The strongest associations were observed for poisoning, which is also referred to as a nonviolent suicide method [road traffic: (95% CI: 1.025, 1.193), railway: (95% CI: 0.997, 1.111)]. See Table S3 for all HRs and CIs. No association was found between measures for eventfulness of noise at night (number of events or IR) and risk for death by suicide (Table S4). In the analysis considering the number of noise sources above 50 dB Lden as exposure, a notable upward trend in risk was observed [One: (95% CI: 1.006, 1.102), Two: (95% CI: 1.049, 1.192), Three: (95% CI: 0.969, 1.619); Figure S5].
For air pollution, the main results (from Model 3) indicated a negative association of exposure with death by intentional self-harm with large CIs [All individuals: (95% CI: 0.811, 0.998), Males: (95% CI: 0.798, 1.012), Females: (95% CI: 0.740, 1.137)] after adjustment for the sources of transportation noise and NDVI (Table 3).
Investigation of an interaction between road traffic noise and exposure using a categorical model (quartiles as exposure categories) did not indicate an interaction between these two exposures (see Table S5). Likelihood-ratio testing revealed that adding the interaction term did not significantly improve model fit ().
After adjusting for the three transportation noise sources and , residential greenness at the place of residence, measured as NDVI with a 500-m buffer, showed a negative association with risk of death by suicide in females, whereas no clear associations where observed in males or the total sample [All individuals: (95% CI: 0.978, 1.020), Males: (95% CI: 0.992, 1.041), Females: (95% CI: 0.908, 0.986)] (Table 3).
Exposure–Response Relationship
Based on the main Model 3, natural splines with 3 df showed a near linear association between intentional self-harm mortality and exposure to road traffic noise starting at around 50 dB Lden (Figure 2). For railway noise, a linear risk increase was observed beginning below 35 dB. Similarly, the risk started to increase linearly from just below 45 dB Lden for aircraft noise; however, below this value, where most of the observations were located, the exposure–response association was inverse.
Figure 2.
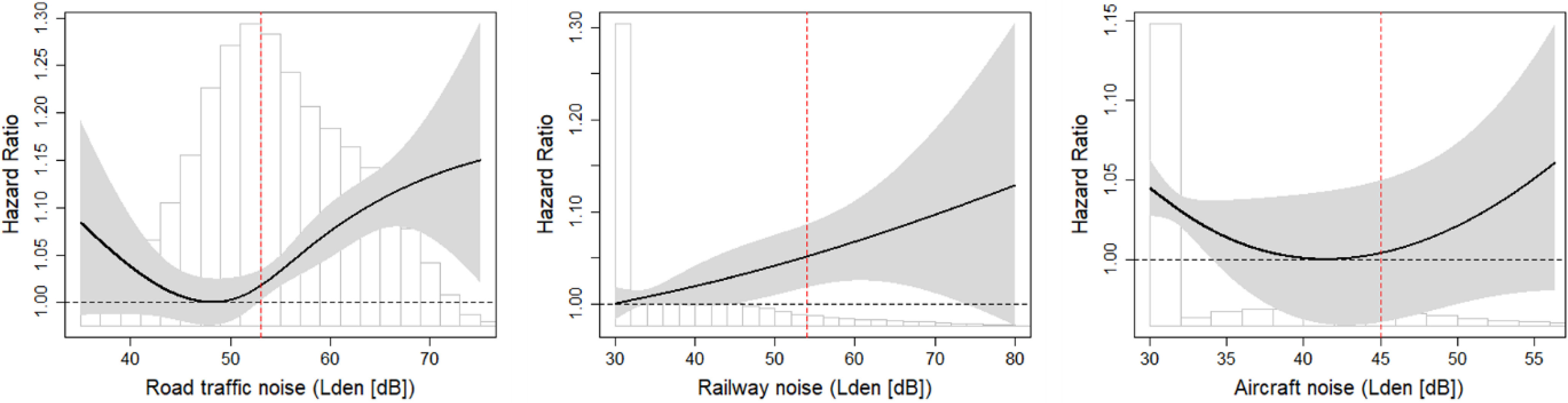
Exposure–response relationships for the association between transportation noise source [Lden (dB)] and mortality from intentional self-harm (ICD-10: X60–84, excl. ICD-10 X61.8, X61.9, X81–82). Natural splines (3 df, knots placed at tertiles of noise distribution) for the association between road traffic, railway, or aircraft noise (Lden, dB) and mortality from all intentional self-harm (ICD-10: X60–84, excluding ICD-10 X61.8, X61.9, X81–82). Same adjustments as in main model (M3), including noise exposures (road traffic noise, railway noise, and aircraft noise), exposure, NDVI within 500 m around the residence, age as timescale, sex as strata, individual sociodemographic covariates (civil status, education, mother tongue, nationality, urbanization, local SEP, area SEP, and unemployment rate) were used. Vertical dashed red lines show source-specific WHO guideline levels: , , . (For interpretation of the references to color in this figure legend, see the web version of this article.) Internal knots placed at the following values (tertiles of respective noise distribution): road traffic noise: 50.64 dB, 57.84 dB; railway noise: 30 dB (lower bound and first tertile), 39.66 dB; aircraft noise: 30 dB (lower bound and first tertile), 32.62 dB. Mean and SD of the noise distribution can be found in Table 2. HR and 95% CI at Lden values indicated on the x-axis can be found in Table S9A–C. Note: CI, confidence interval; dB, decibel; df, degrees of freedom; HR, hazard ratio; ICD, International Statistical Classification of Diseases and Related Health Problems, 10th Revision; Lden, day-evening-night level; NDVI, normalized difference vegetation index; SD standard deviation; SEP, socioeconomic position; WHO, World Health Organization.
Sensitivity Analysis
For all outcomes, adjusting for instead of did not change the associations with exposure to the different noise sources (see Figure S6). Not adjusting for transportation noise in the sensitivity analysis did not influence the null air pollution associations found in the main model 3, which included copollutant adjustment (Figure S7).
Effect Modification
The observed increased risk of death by suicide in the main model (Model 3) for road traffic and railway noise was higher in females [road traffic: (95% CI: 1.007, 1.112), railway: (95% CI: 0.992, 1.066)] than in males [road traffic: (95% CI: 1.006, 1.063), railway: (95% CI: 1.000, 1.043)] (Table 3). These tendencies were robust across all outcome subcategories, with an association also seen in females among suicides using firearms (see Table S3; Figure S8).
Concerning age groups, the effect of road traffic noise was comparable in the two younger age groups [15–30 y: (95% CI: 1.011, 1.152), 30–65 y: (95% CI: 1.019, 1.082)], whereas no effect was observed for individuals older than 65 y [ (95% CI: 0.944, 1.047)]. For railway noise, associations were observed only in the two older age groups [30–65 y: (95% CI: 1.004, 1.051), : (95% CI: 0.998, 1.077)], whereas again no association was observed for aircraft noise in any age group (see Table 3; Figure S9).
Looking at effect modification by local-SEP index, an increased risk for both road traffic and railway noise was observed across all local-SEP quartiles, with the largest association with road traffic noise in the second quartile (; 95% CI: 1.035, 1.138) and with railway noise in the third quartile (; 95% CI: 0.996, 1.071). There were no indications of a trend toward lower or higher SEP categories (Figure S10; Table S6). No relevant differences were observed according to civil status (Table S7).
Stratified analysis according to urbanization revealed larger risk increases for suicide deaths associated with road traffic noise in urban (; 95% CI: 1.004, 1.098) and peri-urban (; 95% CI: 1.005, 1.087) areas than in rural settings (; 95% CI: 0.979, 1.066). For railway noise, the largest risk increase was seen in the peri-urban setting (; 95% CI: 1.014, 1.072). NDVI showed a negative association with risk of death by suicide in the urban setting (; 95% CI: 0.912, 0.973), whereas no association was observed in the peri-urban setting and a positive association in the rural areas (; 95% CI: 1.027, 1.119) (Table S8; Figure S11).
Discussion
Our findings suggest an association between exposure to transportation noise at the place of residence and the risk of death by intentional self-harm. Risk started to increase at levels of 50 dB or even lower, i.e., below the current WHO guideline levels for all noise sources. The observed associations were stronger in females than in males. We did not find any evidence for an increased risk of death by intentional self-harm due to air pollution. An inverse association with residential greenness was observed in females and in the urban setting.
There is hardly any research investigating long-term exposure to transportation noise and risk of suicide. The only previous study that investigated long-term noise exposure and suicide was conducted in Korea using environmental noise measurement data from a nationwide noise monitoring system, and not differentiating the exposure by noise source (e.g., noise caused by transportation and industrial and recreational activities). Mean monthly nighttime noise levels from the closest measurement stations were used as exposure. The authors reported a significantly increased risk for death by suicide per IQR increase of nighttime noise of 32% (95% CI: 2%, 70%) in younger adults (20–54 y, ) and 43% (95% CI: 1%, 102%) in older adults (, ).7 Although these results are difficult to directly compare to ours, it is notable that both suggest a risk increase for death by suicide in relation to noise exposure.
Overall, however, we believe our results should not be interpreted as suggesting that transportation noise has a direct influence on suicide or suicidal behavior, but rather that suicide as a surrogate for underlying mental health disorders is associated with transportation noise exposure. There is conclusive evidence that mental and behavioral disorders are the predominant comorbidities in suicide victims.2,64 Hence, we reasoned to use suicide as a surrogate for underlying mental health disorders. The advantage of this approach is that it enables the use of the extensive mortality data in the SNC to study mental disorders. However, it is clear that there are also some limitations. For example, deaths by suicide represent only the “tip of the iceberg.” Estimations suggest that worldwide, there are suicide attempts for every death by suicide,9 and a Swiss study even noted 32 attempts for each death.65 Additionally, suicide is a highly complex issue with many influencing factors, however, with psychiatric diseases and especially depressive disorders representing an important factor.64
When comparing our results on associations of transportation noise with suicide to existing literature on transportation noise and mental health, there is mixed agreement. For example, a systematic review and meta-analysis from 2020 reported an association between exposure to road traffic noise and anxiety [odds ratio ; 95% CI: 1.01, 1.15 per 10 dB Lden], whereas no effect was found for railway and aircraft noise.30 Another systematic review and meta-analysis from the same year, in contrast, reported an association of aircraft noise exposure with risk for depression [12% (95% CI: 2%, 23%) increased risk per 10 dB Lden], whereas smaller risk increases were found for road traffic [3% (95% CI: −1%, 6%) per 10 dB Lden] and railway noise [2% (95% CI: −5%, 8%) per 10 dB Lden].29 A more recent longitudinal study reported an association of road traffic noise and psychological ill health.66 A study from Switzerland, also published after the above-mentioned reviews, found an association between incidence of depression and noise annoyance, whereas no significant association was found with noise exposure of any source.67 An interesting observation is that results from a 2022 UK Biobank study suggested the opposite of the results in our study. In their large cross-sectional study, the authors reported an increased risk for major depression associated with exposure but not an association with transportation noise exposure.36 Although numerous studies report associations of transportation noise and mental health, the quality of evidence is considered low due to study design (mostly cross-sectional) and small sample sizes.28,68,69 Additionally, heterogeneity in exposure assessments, outcome definitions and effect measures complicate a conclusive comparison of results. The consensus from the existing literature, however, is that an impact of transportation noise on mental health is highly probable,70 which our findings further support.
One difference in our results from existing evidence is that we did not find a clear association between aircraft noise and death by intentional self-harm. This finding in particular contradicts the results from the previously mentioned meta-analysis by Hegewald et al.,29 which reported a rather large increased risk of depression per 10 dB aircraft noise. These results are mainly driven by one study by Seidler et al.71 (Weight 98%), which was set around the airport of Frankfurt before the night flying ban was established in 2011. In contrast, in Zurich, the largest airport in Switzerland, a ban had already been established in 1972.72 Hence, an interpretation of this contrasting result could be that noise (and specifically aircraft noise) during the night is the main contributor of negative effects on mental health. This finding is in agreement with the study by Min and Min,7 which reported an increased risk of suicide with increasing nighttime environmental noise exposure. Additionally, this conclusion is supported by psychiatric literature judging sleep disturbances as an independent risk factor for most psychiatric disorders.73 Alternatively, the absence of an association between aircraft noise and risk for death by suicide might also be due to residual confounding and exposure distribution, because aircraft noise in our study area (Switzerland) is mostly concentrated around larger cities (Basel, Geneva, Zurich), areas for which a 2016 mortality atlas of Switzerland showed average to lower suicide rates.74 Additionally, the exposure–response curve for aircraft noise showed an inverse association in the very low exposure. Areas with low aircraft noise exposure are also more likely very rural, which might contribute to confounding. This theory is supported by results from another SNC study by Guseva Canu et al.75 that identified men working in agriculture, hunting, and forestry, who tend to live in more rural settings, to be at an increased suicide risk in comparison with the risk found for men working in other professions.
Concerning effect modification, we consistently saw stronger associations of transportation noise and suicide risk in females than in males and also a protective effect of greenness exclusively in females in the main analysis. Because gender differences in suicide are well known, these associations are not surprising. In general, women make more suicide attempts, but suicide mortality is generally higher in men.76 Accordingly, in our nationwide sample, 74.1% of the suicide victims were male. This discrepancy is often referred to as the “gender paradox of suicide.” Among other factors, differences in psychopathology have been proposed as possible reasons for these gender differences.77 Already in 2004, differences in underlying psychiatric disorders in male and female suicides were reported: although diagnoses with personality, childhood, and alcohol or substance disorders were more common in males, females had more often been diagnosed with depressive or affective disorders.2 This underlying psychopathology may partly explain the observed effect modification in our results. The suspected mechanisms linking transportation noise exposure with mental health (prolonged stress reactions,21 allostatic overload,15 and sleep disturbances22) are thought to mostly increase the risk for affective disorders such as depression and anxiety disorders,24,25,27 whereas effects on personality disorders and other psychiatric disorders such as schizophrenia seem less plausible. This evidence is also consistent with the existing, albeit limited, evidence investigating transportation noise exposure and mental health outcomes.28 Hence, we interpret our results indicating a stronger effect of road traffic noise exposure on suicide risk in females as suggesting that such associations are mostly mediated through an increased risk for affective and anxiety disorders. Because reliable data on psychiatric diagnosis or medication prescription were not available, this hypothesis could not be tested with mediation analysis. Further studies are needed to elucidate the pathways through which transportation noise influences mental health.
Another interesting finding from our study concerns those on greenness. We observed a substantial risk reduction [ (95% CI: 0.912, 0.973) per 0.1 NDVI] in the urban setting. This finding is in line with the findings of a Dutch longitudinal case–control study,8 which also reported a reduced risk for suicide associated with more residential green space in urban but not rural regions. Conversely, however, we saw a strong association of higher NDVI with increased risk of suicide in the rural setting. We argue that this association might be spurious, because those areas with the highest NDVI in the rural setting are probably very rural areas, where a higher percentage of the population are agricultural workers. As mentioned above, this population is among the most at-risk professional groups in Switzerland.75 Also, remote regions showed above-average suicide mortality in a 2016 mortality atlas.74
Regarding air pollution, we found no association between either or and suicide mortality. The lack of association was found in models both with and without adjusting for transportation noise (Figure S6). This lack of association is in contrast to many studies reporting an association between long-term and short-term exposure to air pollution and an increased risk for depression, as well as effects on suicides.6,34–36 Most of these studies, except for the UK Biobank study,36 however, did not adjust for exposure to transportation noise. It may thus also be that some of these previous results on air pollution have been confounded by transportation noise. Future studies exploring either the effects of air pollution or transportation noise exposure on mental health should consider that both exposures may play a role.
Strengths and Limitations
To our knowledge, this is the first study investigating long-term exposure to source-specific transportation noise and suicide mortality. The use of the Swiss National Cohort enabled following more than 5 million Swiss residents over 15 y of age in combination with high-quality noise models providing energy-based metrics is a strength of this study. This, in combination with adjustment for air pollution exposure using data from a validated land use regression model as well as NDVI, is a further asset.
Even though this study is based on very comprehensive data and noise exposure assessment, some exposure misclassification is unavoidable, for instance, for individuals who have moved during the study period. To minimize this, we implemented an approach to account for this spatial change using census data and address history to update the estimated noise exposure at the beginning of each 5-y period. Additionally, as is always the case when using noise exposure estimates at participants’ home addresses, our estimated exposures do not reflect the exposure the participants experienced when away from home.78
Some residual confounding, mostly by SEP, can also not be dismissed. To diminish this, we adjusted for SEP on different levels. The rationale behind this approach was that some levels might better correspond to different types of possible confounders. For example, regional markers might better reflect the quality of health services, community markers contribute information about the population mix, and the near-individual local-SEP index plus actual individual covariates (e.g., civil status and education) would correspond best with health behavior. However, this probably still did not result in a perfect reflection of individual participants’ SEP. Another possible source of residual confounding is urbanization. However, considering the spatial pattern of suicide in Switzerland, urban/rural differences mostly occur in specific age groups, vary across language regions,74 and might also partially be related to religion.79 We do not assume that such patterns are systematically correlated with transportation noise. One exception could be in the very rural setting, where noise (and air pollution) exposure is typically very low, but suicide risk might be higher. Such confounding would, however, have led to an underestimation of our effect estimates. Looking at the e-value of 1.24 for our main findings, we conclude that it is unlikely that uncaptured features of urbanization or SEP could be that strongly correlated with both transportation noise and suicide across our sample of more than 5 million individuals.
Additional limitations are the lack of data on medical records regarding psychiatric diagnoses and medication intake as well as lifestyle factors such as smoking or alcohol consumption in the SNC. Knowledge about suicide attempts as an additional outcome reflective of underlying severe mental health disorders would have further improved our study.
Conclusion
In this nationwide administrative cohort study, we found a robust association of exposure to transportation noise and the risk for death by intentional self-harm. Though information on mental health status was not available, these findings suggest that suicide as a surrogate for mental health disorders may be related to transportation noise, adding to the growing body of evidence for such effects. Further research is needed to solidify the understanding of the complex relationship between noise exposure, other environmental stressors such as air pollution, socioeconomic factors, and mental health. However, our results emphasize the public health importance of efforts to reduce the population exposed to high levels of transportation noise.
Supplementary Material
Acknowledgments
The authors thank the Federal Statistical Office (FSO) for providing mortality and census data and for the support that made the Swiss National Cohort and this study possible. This work was supported by the Swiss National Science Foundation (grant nos. 3347CO-108806, 33CS30_134273 and 33CS30_148415). The members of the Swiss National Cohort Scientific Board are M. Zwahlen (University of Berne), M. Egger (University of Berne), V. von Wyl (University of Zurich), O. Hämmig (University of Zurich), M. Bochud (University of Lausanne), M. Röösli (University of Basel), and M. Schwyn (Federal Statistical Office).
The SNC was approved by the Ethics Committees of the Canton Bern (No KeK 153/2014, PB_2020-00050).
B.W., D.V., and M.R. worked on study concept and study design; D.V. conducted data preparation; B.W. and D.V. performed statistical modeling; and B.W. wrote and revised manuscript and performed all data interpretation, review, and commentary on the manuscript.
This work was supported by the Swiss National Science Foundation (grant nos. 3347CO-108806, 33CS30_134273 and 33CS30_148415, 324730B_201272).
References
- 1.Institute for Health Metrics and Evaluation. 2019. GBD Results. https://vizhub.healthdata.org/gbd-results/ [accessed 21 December 2022].
- 2.Arsenault-Lapierre G, Kim C, Turecki G. 2004. Psychiatric diagnoses in 3275 suicides: a meta-analysis. BMC Psychiatry 4:37, PMID: , 10.1186/1471-244X-4-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henriksson MM, Aro HM, Marttunen MJ, Heikkinen ME, Isometsä ET, Kuoppasalmi KI, et al. 1993. Mental disorders and comorbidity in suicide. Am J Psychiatry 150(6):935–940, PMID: , 10.1176/ajp.150.6.935. [DOI] [PubMed] [Google Scholar]
- 4.Schmid M, Michaud L, Bovio N, Guseva Canu I, Swiss National Cohort (SNC). 2020. Prevalence of somatic and psychiatric morbidity across occupations in Switzerland and its correlation with suicide mortality: results from the Swiss National Cohort (1990–2014). BMC Psychiatry 20(1):324, PMID: , 10.1186/s12888-020-02733-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bär S, Bundo M, de Schrijver E, Müller TJ, Vicedo-Cabrera AM. 2022. Suicides and ambient temperature in Switzerland: a nationwide time-series analysis. Swiss Med Wkly 152:w30115, PMID: , 10.4414/smw.2022.w30115. [DOI] [PubMed] [Google Scholar]
- 6.Braithwaite I, Zhang S, Kirkbride JB, Osborn DPJ, Hayes JF. 2019. Air pollution (particulate matter) exposure and associations with depression, anxiety, bipolar, psychosis and suicide risk: a systematic review and meta-analysis. Environ Health Perspect 127(12):126002, PMID: , 10.1289/EHP4595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Min JY, Min KB. 2018. Night noise exposure and risk of death by suicide in adults living in metropolitan areas. Depress Anxiety 35(9):876–883, PMID: , 10.1002/da.22789. [DOI] [PubMed] [Google Scholar]
- 8.Helbich M, O’Connor RC, Nieuwenhuijsen M, Hagedoorn P. 2020. Greenery exposure and suicide mortality later in life: a longitudinal register-based case-control study. Environ Int 143:105982, PMID: , 10.1016/j.envint.2020.105982. [DOI] [PubMed] [Google Scholar]
- 9.WHO (World Health Organization). 2021. Suicide Worldwide in 2019: Global Health Estimates. Geneva, Switzerland: World Health Organziation. [Google Scholar]
- 10.EEA (European Environment Agency). 2020. Healthy Environment, Healthy Lives: How the Environment Influences Health and Well-Being in Europe. European Environment Agency, Denmark, Copenhagen. https://www.eea.europa.eu/publications/healthy-environment-healthy-lives [accessed 16 March 2023]. [Google Scholar]
- 11.Khomenko S, Cirach M, Barrera-Gómez J, Pereira-Barboza E, Iungman T, Mueller N, et al. 2022. Impact of road traffic noise on annoyance and preventable mortality in european cities: a health impact assessment. Environ Int 162:107160, PMID: , 10.1016/j.envint.2022.107160. [DOI] [PubMed] [Google Scholar]
- 12.Hänninen O, Knol AB, Jantunen M, Lim T-A, Conrad A, Rappolder M, et al. 2014. Environmental burden of disease in Europe: assessing nine risk factors in six countries. Environ Health Perspect 122(5):439–446, PMID: , 10.1289/ehp.1206154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eriksson C, Pershagen G, Nilsson M. 2018. Biological mechanisms related to cardiovascular and metabolic effects by environmental noise. World Health Organization. Regional Office for Europe. https://apps.who.int/iris/handle/10665/346548 [accessed 16 March 2023].
- 14.Recio A, Linares C, Banegas JR, Díaz J. 2016. Road traffic noise effects on cardiovascular, respiratory, and metabolic health: an integrative model of biological mechanisms. Environ Res 146:359–370, PMID: , 10.1016/j.envres.2015.12.036. [DOI] [PubMed] [Google Scholar]
- 15.Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. 2014. Auditory and non-auditory effects of noise on health. Lancet 383(9925):1325–1332, PMID: , 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Münzel T, Hahad O, Sørensen M, Lelieveld J, Duerr GD, Nieuwenhuijsen M, et al. 2022. Environmental risk factors and cardiovascular diseases: a comprehensive expert review. Cardiovasc Res 118(14):2880–2902, PMID: , 10.1093/cvr/cvab316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brink M, Schäffer B, Vienneau D, Pieren R, Foraster M, Eze IC, et al. 2019. Self-reported sleep disturbance from road, rail and aircraft noise: exposure-response relationships and effect modifiers in the SiRENE study. Int J Environ Res Public Health 16(21):4186, PMID: , 10.3390/ijerph16214186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Kamp I, Simon S, Notley H, Baliatsas C, van Kempen E. 2020. Evidence relating to environmental noise exposure and annoyance, sleep disturbance, cardio-vascular and metabolic health outcomes in the context of IGCB (N): a scoping review of new evidence. Int J Environ Res Public Health 17(9):3016, PMID: , 10.3390/ijerph17093016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cerletti P, Eze IC, Schaffner E, Foraster M, Viennau D, Cajochen C, et al. 2020. The independent association of source-specific transportation noise exposure, noise annoyance and noise sensitivity with health-related quality of life. Environ Int 143:105960, PMID: , 10.1016/j.envint.2020.105960. [DOI] [PubMed] [Google Scholar]
- 20.Hahad O, Bayo Jimenez MT, Kuntic M, Frenis K, Steven S, Daiber A, et al. 2022. Cerebral consequences of environmental noise exposure. Environ Int 165:107306, PMID: , 10.1016/j.envint.2022.107306. [DOI] [PubMed] [Google Scholar]
- 21.Hahad O, Daiber A, Münzel T. 2021. Heightened amygdalar activity mediates the cardiometabolic effects of transportation noise stress. Psychoneuroendocrinology 131:105347, PMID: , 10.1016/j.psyneuen.2021.105347. [DOI] [PubMed] [Google Scholar]
- 22.Smith MG, Cordoza M, Basner M. 2022. Environmental noise and effects on sleep: an update to the WHO systematic review and meta-analysis. Environ Health Perspect 130(7):76001, PMID: , 10.1289/EHP10197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harvey AG, Murray G, Chandler RA, Soehner A. 2011. Sleep disturbance as transdiagnostic: consideration of neurobiological mechanisms. Clin Psychol Rev 31(2):225–235, PMID: , 10.1016/j.cpr.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guidi J, Lucente M, Sonino N, Fava GA. 2021. Allostatic load and its impact on health: a systematic review. Psychother Psychosom 90(1):11–27, PMID: , 10.1159/000510696. [DOI] [PubMed] [Google Scholar]
- 25.Beck MDAT, Alford PDBA. Depression: Causes and Treatment. Philadelphia, PA: University of Pennsylvania Press. [Google Scholar]
- 26.Bebbington P. 1987. Misery and the of disease theories of depression. Int J Soc Psychiatry 33(1):13–20, PMID: , 10.1177/002076408703300102. [DOI] [PubMed] [Google Scholar]
- 27.Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, et al. 2016. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull 142(9):969–990, PMID: , 10.1037/bul0000053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clark C, Paunovic K. 2018. WHO environmental noise guidelines for the european region: a systematic review on environmental noise and quality of life, wellbeing and mental health. Int J Environ Res Public Health 15(11):2400, PMID: , 10.3390/ijerph15112400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hegewald J, Schubert M, Freiberg A, Romero Starke K, Augustin F, Riedel-Heller SG, et al. 2020. Traffic noise and mental health: a systematic review and meta-analysis. Int J Environ Res Public Health 17(17):6175, PMID: , 10.3390/ijerph17176175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lan Y, Roberts H, Kwan M-P, Helbich M. 2020. Transportation noise exposure and anxiety: a systematic review and meta-analysis. Environ Res 191:110118, PMID: , 10.1016/j.envres.2020.110118. [DOI] [PubMed] [Google Scholar]
- 31.Díaz J, López-Bueno JA, López-Ossorio JJ, Gónzález JL, Sánchez F, Linares C. 2020. Short-term effects of traffic noise on suicides and emergency hospital admissions due to anxiety and depression in Madrid (Spain). Sci Total Environ 710:136315, PMID: , 10.1016/j.scitotenv.2019.136315. [DOI] [PubMed] [Google Scholar]
- 32.Babadjouni RM, Hodis DM, Radwanski R, Durazo R, Patel A, Liu Q, et al. 2017. Clinical effects of air pollution on the central nervous system; a review. J Clin Neurosci 43:16–24, PMID: , 10.1016/j.jocn.2017.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li H, Cai J, Chen R, Zhao Z, Ying Z, Wang L, et al. 2017. Particulate matter exposure and stress hormone levels. Circulation 136(7):618–627, PMID: , 10.1161/CIRCULATIONAHA.116.026796. [DOI] [PubMed] [Google Scholar]
- 34.Borroni E, Pesatori AC, Bollati V, Buoli M, Carugno M. 2022. Air pollution exposure and depression: a comprehensive updated systematic review and meta-analysis. Environ Pollut 292(pt A):118245, PMID: , 10.1016/j.envpol.2021.118245. [DOI] [PubMed] [Google Scholar]
- 35.Liu Q, Wang W, Gu X, Deng F, Wang X, Lin H, et al. 2021. Association between particulate matter air pollution and risk of depression and suicide: a systematic review and meta-analysis. Environ Sci Pollut Res Int 28(8):9029–9049, PMID: , 10.1007/s11356-021-12357-3. [DOI] [PubMed] [Google Scholar]
- 36.Hao G, Zuo L, Xiong P, Chen L, Liang X, Jing C. 2022. Associations of PM2.5 and road traffic noise with mental health: evidence from UK Biobank. Environ Res 207:112221, PMID: , 10.1016/j.envres.2021.112221. [DOI] [PubMed] [Google Scholar]
- 37.Vienneau D, de Hoogh K, Faeh D, Kaufmann M, Wunderli JM, Röösli M. 2017. More than clean air and tranquillity: residential green is independently associated with decreasing mortality. Environ Int 108:176–184, PMID: , 10.1016/j.envint.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 38.Helbich M, de Beurs D, Kwan M-P, O’Connor RC, Groenewegen PP. 2018. Natural environments and suicide mortality in The Netherlands: a cross-sectional, ecological study. Lancet Planet Health 2(3):e134–e139, PMID: , 10.1016/S2542-5196(18)30033-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Y, Mavoa S, Zhao J, Raphael D, Smith M. 2020. The association between green space and adolescents’ mental well-being: a systematic review. Int J Environ Res Public Health 17(18):6640, PMID: , 10.3390/ijerph17186640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang R, Zhang CQ, Rhodes RE. 2021. The pathways linking objectively-measured greenspace exposure and mental health: a systematic review of observational studies. Environ Res 198:111233, PMID: , 10.1016/j.envres.2021.111233. [DOI] [PubMed] [Google Scholar]
- 41.Bopp M, Spoerri A, Zwahlen M, Gutzwiller F, Paccaud F, Braun-Fahrländer C, et al. 2009. Cohort profile: the Swiss National Cohort—a longitudinal study of 6.8 million people. Int J Epidemiol 38(2):379–384, PMID: , 10.1093/ije/dyn042. [DOI] [PubMed] [Google Scholar]
- 42.Spoerri A, Zwahlen M, Egger M, Bopp M. 2010. The Swiss National Cohort: a unique database for national and international researchers. Int J Public Health 55(4):239–242, PMID: , 10.1007/s00038-010-0160-5. [DOI] [PubMed] [Google Scholar]
- 43.Renaud AS. 2004. Coverage Estimation for the Swiss Population Census 2000: Estimation Methodology and Results, Neuchatel, Switzerland. https://www.bfs.admin.ch/bfsstatic/dam/assets/341896/master [accessed 16 March 2023].
- 44.Steck N, Zwahlen M, Egger M, Swiss National Cohort. 2015. Time-trends in assisted and unassisted suicides completed with different methods: Swiss National Cohort. Swiss Med Wkly 145:w14153, PMID: , 10.4414/smw.2015.14153. [DOI] [PubMed] [Google Scholar]
- 45.Vienneau D, Saucy A, Schäffer B, Flückiger B, Tangermann L, Stafoggia M, et al. 2022. Transportation noise exposure and cardiovascular mortality: 15-years of follow-up in a nationwide prospective cohort in Switzerland. Environ Int 158:106974, PMID: , 10.1016/j.envint.2021.106974. [DOI] [PubMed] [Google Scholar]
- 46.Karipidis I, Vienneau D, Habermacher M, Köpflii M, Brink M, Probst-Hensch N, et al. 2014. Reconstruction of historical noise exposure data for environmental epidemiology in Switzerland within the SiRENE project. Noise Mapping 1(1):000010247820140002, 10.2478/noise-2014-0002. [DOI] [Google Scholar]
- 47.Röösli M, Wunderli J, Brink M, Cajochen C, Probst-Hensch N. 2019. Die SiRENE-Studie. Swiss Med Forum 19(0506):77–82, 10.4414/smf.2019.03433. [DOI] [Google Scholar]
- 48.Heutschi K. 2004. SonRoad: new Swiss road traffic noise model. Acta Acustica United with Acustica 90(3):548–554. [Google Scholar]
- 49.FOEN (Federal Office for the Environment). 1987. Computermodell zur Berechnung von Strassenlärm. Bern, Switzerland. https://www.bafu.admin.ch/bafu/en/home/topics/noise/publications-studies/publications/computermodell-berechnung-strassenlaerm.html [accessed 16 March 2023]. [Google Scholar]
- 50.Thron T, Hecht M. 2010. The sonRAIL emission model for railway noise in Switzerland. Acta Acustica United with Acustica 96(5):873–883, 10.3813/AAA.918346. [DOI] [Google Scholar]
- 51.BUWAL (Bundesamt für Umwelt, Wald und Landschaft). 1990. Schweizerisches Emissions- und Immisionsmodell für die Berechnung von Eisenbahnlärm (SEMIBEL). Schriftenreihe Umweltschutz Nr. 116, Bern, Switzerland.
- 52.Krebs W, Bütikofer R, Plüss S, Thomann G. 2004. Sound source data for aircraft noise simulation. Acta Acustica United with Acustica 90(1):91–100. [Google Scholar]
- 53.Krebs W, Thomann G, Bütikofer R. 2010. FLULA2, Ein Verfahren zur Berechnung und Darstellung der Fluglärmbelastung, Version 4. Dübendorf, Switzerland: Empa. https://www.empa.ch/documents/56129/103151/SaT_FLULA2_Dokument/62e3c7e1-e395-4975-9eba-fda3adf17962 [accessed 16 March 2023]. [Google Scholar]
- 54.Wunderli JM, Pieren R, Habermacher M, Vienneau D, Cajochen C, Probst-Hensch N, et al. 2016. Intermittency ratio: a metric reflecting short-term temporal variations of transportation noise exposure. J Expo Sci Environ Epidemiol 26(6):575–585, PMID: , 10.1038/jes.2015.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Héritier H, Vienneau D, Foraster M, Eze IC, Schaffner E, Thiesse L, et al. 2017. Transportation noise exposure and cardiovascular mortality: a nationwide cohort study from Switzerland. Eur J Epidemiol 32(4):307–315, PMID: , 10.1007/s10654-017-0234-2. [DOI] [PubMed] [Google Scholar]
- 56.Vienneau D, Héritier H, Foraster M, Eze IC, Schaffner E, Thiesse L, et al. 2019. Façades, floors and maps—influence of exposure measurement error on the association between transportation noise and myocardial infarction. Environ Int 123:399–406, PMID: , 10.1016/j.envint.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 57.Canchola AJ, Stewart SL, Bernstein L, West DW, Ross RK, Deapen D, et al. 2003. Cox regression using different time-scales. Western users of SAS software annual meeting. SAS Institute, San Francisco, CA, USA, 2003.
- 58.Panczak R, Galobardes B, Voorpostel M, Spoerri A, Zwahlen M, Egger M. 2012. A Swiss neighbourhood index of socioeconomic position: development and association with mortality. J Epidemiol Community Health 66(12):1129–1136, PMID: , 10.1136/jech-2011-200699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Raum mit städtischem Charakter der Schweiz 2012. Neuchâtel, Switzerland: Bundesamt für Statistik (BFS). [Google Scholar]
- 60.de Hoogh K, Chen J, Gulliver J, Hoffmann B, Hertel O, Ketzel M, et al. 2018. Spatial PM2.5, NO2, O3 and BC models for Western Europe—evaluation of spatiotemporal stability. Environ Int 120:81–92, PMID: , 10.1016/j.envint.2018.07.036. [DOI] [PubMed] [Google Scholar]
- 61.VanderWeele TJ, Ding P. 2017. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med 167(4):268–274, PMID: , 10.7326/M16-2607. [DOI] [PubMed] [Google Scholar]
- 62.Héritier H, Vienneau D, Foraster M, Eze IC, Schaffner E, de Hoogh K, et al. 2019. A systematic analysis of mutual effects of transportation noise and air pollution exposure on myocardial infarction mortality: a nationwide cohort study in Switzerland. Eur Heart J 40(7):598–603, PMID: , 10.1093/eurheartj/ehy650. [DOI] [PubMed] [Google Scholar]
- 63.Vienneau D, de Hoogh K, Bechle MJ, Beelen R, van Donkelaar A, Martin RV, et al. 2013. Western European land use regression incorporating satellite- and ground-based measurements of NO2 and PM10. Environ Sci Technol 47(23):13555–13564, PMID: , 10.1021/es403089q. [DOI] [PubMed] [Google Scholar]
- 64.Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, et al. 2017. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull 143(2):187–232, PMID: , 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- 65.Peter C, Tuch A. 2019. Suizidgedanken und Suizidversuche in der Schweizer Bevölkerung Obsan Bulletin 7/2019. Schweizerisches Gesund-heitsobservatorium Obsan, Neuchâtel, Switzerland. [Google Scholar]
- 66.Stansfeld S, Clark C, Smuk M, Gallacher J, Babisch W. 2021. Road traffic noise, noise sensitivity, noise annoyance, psychological and physical health and mortality. Environ Health 20(1):32, PMID: , 10.1186/s12940-021-00720-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Eze IC, Foraster M, Schaffner E, Vienneau D, Pieren R, Imboden M, et al. 2020. Incidence of depression in relation to transportation noise exposure and noise annoyance in the SAPALDIA study. Environ Int 144:106014, PMID: , 10.1016/j.envint.2020.106014. [DOI] [PubMed] [Google Scholar]
- 68.Dickerson AS, Wu AC, Liew Z, Weisskopf M. 2020. A scoping review of non-occupational exposures to environmental pollutants and adult depression, anxiety, and suicide. Curr Environ Health Rep 7(3):256–271, PMID: , 10.1007/s40572-020-00280-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dzhambov AM, Lercher P. 2019. Road traffic noise exposure and depression/anxiety: an updated systematic review and meta-analysis. Int J Environ Res Public Health 16(21):4134, PMID: , 10.3390/ijerph16214134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hahad O, Beutel ME, Gilan DA, Michal M, Daiber A, Münzel T. 2020. Auswirkungen von umweltrisikofaktoren wie lärm und luftverschmutzung auf die psychische gesundheit: was wissen wir? Dtsch Med Wochenschr 145(23):1701–1707, PMID: , 10.1055/a-1201-2155. [DOI] [PubMed] [Google Scholar]
- 71.Seidler A, Hegewald J, Seidler AL, Schubert M, Wagner M, Dröge P, et al. 2017. Association between aircraft, road and railway traffic noise and depression in a large case-control study based on secondary data. Environ Res 152:263–271, PMID: , 10.1016/j.envres.2016.10.017. [DOI] [PubMed] [Google Scholar]
- 72.Bissegger M. 2013. Noise management in the light of airport development. In: Proceedings of the Inter-Noise 2013, 42nd International Congress and Exposition on Noise Control Engineering, Noise Control for Quality of Life, 15–18 September 2013. ÖAL Österreichischer Arbeitsring für Lärmbekämpfung, eds. Innsbruck, Austria: Institute of Noise Control Engineering, 247(3):5070.–. [Google Scholar]
- 73.Freeman D, Sheaves B, Waite F, Harvey AG, Harrison PJ. 2020. Sleep disturbance and psychiatric disorders. Lancet Psychiatry 7(7):628–637, PMID: , 10.1016/S2215-0366(20)30136-X. [DOI] [PubMed] [Google Scholar]
- 74.Chammartin F, Probst-Hensch N, Utzinger J, Vounatsou P. 2016. Mortality atlas of the main causes of death in Switzerland, 2008–2012. Swiss Med Wkly 146:w14280, PMID: , 10.4414/smw.2016.14280. [DOI] [PubMed] [Google Scholar]
- 75.Guseva Canu I, Bovio N, Mediouni Z, Bochud M, Wild P, Swiss National Cohort (SNC). 2019. Suicide mortality follow-up of the Swiss National Cohort (1990–2014): sex-specific risk estimates by occupational socio-economic group in working-age population. Soc Psychiatry Psychiatr Epidemiol 54(12):1483–1495, PMID: , 10.1007/s00127-019-01728-4. [DOI] [PubMed] [Google Scholar]
- 76.Värnik A, Kõlves K, van der Feltz-Cornelis CM, Marusic A, Oskarsson H, Palmer A, et al. 2008. Suicide methods in Europe: a gender-specific analysis of countries participating in the “European Alliance Against Depression”. J Epidemiol Community Health 62(6):545–551, PMID: , 10.1136/jech.2007.065391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Schrijvers DL, Bollen J, Sabbe BG. 2012. The gender paradox in suicidal behavior and its impact on the suicidal process. J Affect Disord 138(1–2):19–26, PMID: , 10.1016/j.jad.2011.03.050. [DOI] [PubMed] [Google Scholar]
- 78.Helbich M. 2018. Toward dynamic urban environmental exposure assessments in mental health research. Environ Res 161:129–135, PMID: , 10.1016/j.envres.2017.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Steck N, Egger M, Zwahlen M, Swiss National Cohort. 2016. Assisted and unassisted suicide in men and women: longitudinal study of the Swiss population. Br J Psychiatry 208(5):484–490, PMID: , 10.1192/bjp.bp.114.160416. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.