ABSTRACT
The objective of this study was to critically review the cost-effectiveness (CE) of the recombinant zoster vaccine (RZV) against herpes zoster (HZ). A literature review was conducted in PubMed, Embase, and Cochrane between January 1, 2017, and February 28, 2022, and on select public healthcare agency websites to identify and collect data from CE studies comparing RZV to zoster vaccine live (ZVL) or to no vaccination. Study characteristics, inputs, and outputs were collected. The overall CE of RZV was assessed. RZV vaccination against HZ is cost-effective in 15 out of 18 studies included in the present review. Varying incremental cost-effectiveness ratios (ICERs) observed may be associated with different assumptions on the duration of protection of RZV, as well as different combinations of structural and disease-related study (model) inputs driving the estimation of ICERs.
KEYWORDS: Herpes zoster, vaccination, recombinant zoster vaccine, cost-effectiveness, older adults
Plain Language Summary
What is the context?
• Herpes zoster, also known as shingles, may cause painful rashes and skin alterations.
• Chronic pain, also referred to as post-herpetic neuralgia, may persist for months or even years after the initial rash.
• The disease is caused by reactivation of the varicella zoster virus.
• The recombinant zoster vaccine (RZV) and the zoster vaccine live (ZVL) are approved for the prevention of herpes zoster and post-herpetic neuralgia.
• We reviewed published evidence from the past 5 years on RZV.
What is new?
• Out of 18 selected studies, RZV vaccination against herpes zoster and post-herpetic neuralgia is cost-effective in 15.
• In the 15 studies establishing RZV cost-effectiveness, RZV is always cost-effective or frequently cost-saving in direct comparisons to ZVL, when applicable.
• RZV was found cost-saving in several immune-compromised populations.
What is the impact?
• The overview of the currently available body of evidence related to cost-effectiveness of RZV may help informing decision makers about the value of vaccination against herpes zoster.
Introduction
Herpes zoster (HZ), commonly referred to as shingles, is caused by the reactivation of latent varicella-zoster virus (which causes both varicella and herpes zoster). HZ frequently presents as a painful debilitating rash, including skin inflammation and blisters, and sometimes causes scarring and permanent pigment changes. Anyone with a previous record of varicella (chickenpox) is at risk of developing herpes zoster. The frequency of HZ increases with age due to age-related decline in immunity.1 The cumulative incidence of HZ was recently estimated between 2.9 and 19.5 cases per 1000 population worldwide, and the HZ incidence rate was estimated between 5.23 and 10.9 cases per 1000 person-years.2
Chronic pain persisting 3 months after initial rash detection or HZ diagnosis with an average pain score above 3 on the Likert scale3 is commonly defined as post-herpetic neuralgia (PHN) and may continue for months or even years.4 HZ and PHN have been shown to adversely affect healthy aging and quality of life (QoL).5
The recombinant zoster vaccine (RZV, Shingrix, GSK, Belgium) was approved by the Food and Drug Administration (FDA) in 20176 and was preferentially recommended by the Advisory Committee on Immunization Practices (ACIP)7 shortly thereafter for the prevention of HZ in immunocompetent adults aged 50 years and above and in immunocompetent adults who were previously vaccinated with zoster vaccine live (ZVL, Zostavax, Merck Sharp & Dohme Co, United States). It is currently also recommended by ACIP for immunocompromised adults aged 19 years and above.8 RZV was approved by the European Medicines Agency (EMA) in 20189 for the prevention of HZ and PHN in older adults aged 50 years and above and in younger adults aged 18 years and above who are at increased risk of HZ. The vaccine is recommended and reimbursed in a number of countries worldwide.10 ZVL was approved by the FDA in 200611 and by the EMA12 the same year. ZVL is no longer available for use in the United States (US) as of November 2020.13
Many health technology assessment (HTA) bodies and national immunization technical advisory groups are currently evaluating RZV worldwide. As such, it is relevant to provide an overview of the inputs, assumptions, and results presented in cost-effectiveness (CE) of RZV publications to date.
Methods
Study selection
The main literature search was performed on PubMed, Embase, and Cochrane reviews with additional queries on select governmental public health online repositories. Publication dates of interest were between January 1, 2017, and February 28, 2022. The exact search queries are shown in Appendix A. Results were analyzed individually to determine inclusion eligibility into the present study. Only CE or equivalent types of studies (i.e., cost-utility analyses) involving RZV were considered. Cost-of-illness and budget impact studies were excluded by default. Conference abstracts (indexed in Embase) were also excluded by default. Studies deemed eligible for inclusion into the present critical review were further searched manually (references) for potential identification of additional sources.
A summary of the search and screening strategy and its outcomes is depicted graphically in an adapted PRISMA-202014 (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart suitable for reviews including records from databases, registries, and other sources (Figure 1).
Figure 1.
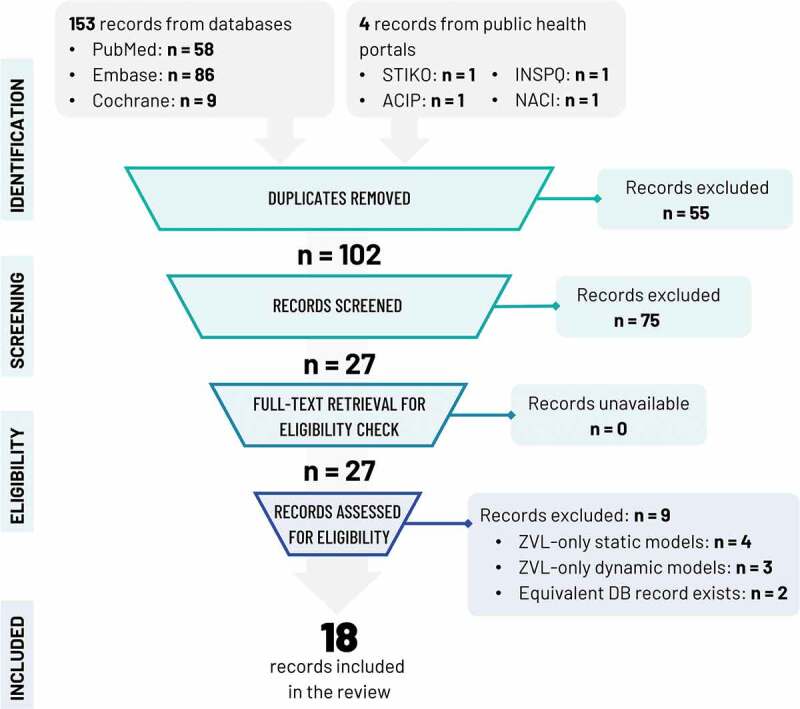
PRISMA flowchart.
Note: ACIP: Advisory Committee on Immunization Practices, DB: database, INSPQ: Institut National de Santé Publique du Québec, NACI: National Advisory Committee on Immunization, STIKO: Standing Committee on Vaccination, ZVL: zoster vaccine live.
Known governmental public health online repositories searched manually for additional sources included the Centers for Disease Control and Prevention (CDC)/ACIP (US), the National Advisory Committee on Immunization (Canada), the Institut National de Santé Publique du Québec (Canada), and the Standing Committee on Vaccination (STIKO, Germany).
Data extraction
For each study included in the review, the extracted information was study characteristics, model attributes, and CE parameters. Detailed input data were collected by type (epidemiological, vaccine profiles, costs, QoL and utilities, adverse events). Top-level and detailed CE results were also extracted.
Quality assessment
The latest version of the Consolidated Health Economic Evaluation Reporting Standards (CHEERS)15 was used to objectify and formally assess the quality of each study, incorporating a total of 28 items recommended for best reporting of health economic evaluations.
Further elaboration on the quality of selected studies forms part of the Discussion of the present review.
Aggregated and detailed CE results were compiled under separate tables. Detailed public health impact outcomes were not in scope of the review.
Results
The literature search on PubMed, Embase, and Cochrane reviews yielded 153 records; 16 studies were admitted to review.
Manual search of the public health online repositories mentioned in the Study Selection revealed four additional studies.16–19 Two16,17 were deemed equivalent to Drolet et al.20 and were excluded from further review.
The PRISMA flowchart of identification and screening is shown in Figure 1. In total, 18 studies were subjected to detailed review.
All studies explicitly stated the study objective, target population, setting, comparators, study perspective, time horizon, discount rates, and choice of health outcomes. All but one18 study explicitly described analytic methods, reported input parameters in detail, and characterized uncertainty via sensitivity analyses. In view of its outline nature, the report of Ortega-Sanchez et al.18 recapping two original CEAs on immunocompromised populations did not follow CHEERS closely; this observation does in no way speak to the quality of the original research summarized therein.
Study Characteristics
The study characteristics are summarized in Table 1. Of the 18 studies included, nine studies were performed in North America,18,20–27 five in Europe,19,28–31 and four in Asia.32–35
Table 1.
Studies included in the review and main study characteristics.
| PMID | Author/year | Funding | Locale | Comparisons | Population | Cohorts | CE metric | PHI/NNV |
|---|---|---|---|---|---|---|---|---|
| 29297049 | Le and Rothberg (2018)21 | Independent | US | RZV vs no vaccination RZV vs ZVL |
ARDI-60+ | 60, 70, 80 | ICER | Not reported |
| 29958739 | You et al (2018)34 | Independent | CN (HK) | RZV vs no vaccination | ARDI-50+ | 50, 60, 70 | ICER | Not reported |
| 30017145 | Curran et al (2018)22 | Industry | US | RZV vs no vaccination RZV vs ZVL |
ARDI-50+ | 50, 60, 65, 70, 80 | ICER | Reported |
| 29987323 | Le and Rothberg (2018b)27 | Independent | US | RZV vs no vaccination RZV vs prior vaccination with ZVL |
ARDI-50+ | 50–59; 60/70/80 (ZVL vaccination) |
ICER | Not reported |
| 30518427 | de Boer et al (2018)29 | Independent | NL | RZV vs no vaccination ZVL vs no vaccination ZVL+boost vs no vaccination |
ARDI-50+ | 50, 60, 70, 80 | ICER | Reported |
| 30130448 | Van Oorschot et al (2019)26 | Industry | GE | RZV vs no vaccination | ARDI-60+ | 60+, 70+, 60, 65, 70 | ICER | Reported |
| 30625011 | Curran et al (2019)23 | Industry | US | RZV vs prior vaccination with ZVL | ARDI-60+ | 60+ | ICER | Not reported |
| 30608953 | You et al (2019)35 | Independent | CN (HK) | RZV vs no vaccination | ARDI-50+ | 50–80 (31 total) | ICER | Reported |
| 30776797 | Prosser et al (2019)24 | Independent | US | RZV vs no vaccination RZV vs ZVL RZV vs prior vaccination with ZVL ZVL vs no vaccination |
ARDI-50+ | 50–59, 60–69, 70–79, 80–89, 90–99, 60+ | ICER | Not reported |
| 30929219 | Shiragami et al (2019)33 | Industry | JP | RZV vs no vaccination | ARDI-65+ | 65+, 50+, 60+, 70+ | ICER | Not reported |
| 31153691 | Hoshi et al (2019)32 | Independent | JP | RZV vs no vaccination ZVL vs no vaccination |
ARDI-65+ | 65–84, 70–84, 75–84, 80-84 | ICER, NMB | Not reported |
| 31289726 | Carpenter et al (2019)25 | Independent | US | RZV vs no vaccination ZVL vs no vaccination |
ARDI-50+ | 50, 60, 70 | ICER | Not reported |
| 31451524 | Drolet et al (2019)20 | Independent | CA | RZV vs no vaccination ZVL vs no vaccination |
ARDI-50+ | 50, 60, 65, 70, 75, 80, 85 | ICER | Reported |
| 31250218 | McGirr et al (2019)26 | Industry | CA | RZV vs no vaccination RZV vs ZVL |
ARDI-60+ | 60+ | ICER | Reported |
| 34905463 | Curran et al (2021)28 | Industry | GE | RZV vs no vaccination | ARDI-50+ | 50, 60, 65, 70, 50+, 60+, 70+ | ICER | Reported |
| 35094374 | Pieters et al (2022)30 | Independent | BE | RZV vs no vaccination ZVL vs no vaccination ZVL+boost vs no vaccination |
ARDI-50+ | 50, 60, 70, 80, 85 | ICER | Reported |
| NA | Ortega-Sanchez (2021)18 | Independent | US | RZV vs no vaccination | IC-18+ | CDC: 19–29, 30–39, 40-49 GSK: 18-49 |
ICER | Reported |
| NA | Ultsch et al (2017)19 | Independent | GE | RZV vs no vaccination ZVL vs no vaccination |
ARDI-50+ | 60, 50, 55, 65, 70, 75, 80 | ICER | Reported |
Note: For each study, costs were represented in MV and benefits in QALY.
ARDI: age-related decline in immunity; CDC: Centers for Disease Control and Prevention; CE: cost-effectiveness; IC: immunocompromised; ICER: incremental cost-effectiveness ratio; MV: monetary value; NA: not applicable; NMB: net monetary benefit; NNV: number needed to vaccinate; PHI: public health impact; PMID: PubMed identifier; QALY: quality-adjusted life year; ZVL: zoster vaccine live.
Locale abbreviations: BE: Belgium; CA: Canada; CN: China; GE: Germany; HK: Hong-Kong; JP: Japan; NL: The Netherlands; US: United States.
All but one18 study examined the CE of RZV and/or ZVL on populations of older adults 50 years and above.
All studies compared RZV to no vaccination; four studies21,22,26,32 additionally directly compared RZV to ZVL and two29,30 compared a boosting strategy for ZVL to no vaccination. Three studies21,23,24 examined the CE of RZV on cohorts previously vaccinated with ZVL. Many studies20,24,25,29,30,32 additionally performed CE analyses of ZVL vaccination vs no vaccination13.
Most studies examined cohorts aged 50 years and above; four19,26,27,31 focused on 60 years and above, and two32,33 on 65 years and above. The immunocompromised cost-effectiveness analysis (CEA)18 was performed on immunocompromised adults older than 18 years of age (YOA).
Eleven studies19–21,24,25,27,29,30,32,34,35 were funded independently; six studies22,23,26,28,31,33 were funded by the vaccine manufacturer. One study18 compared the results of two separate CEA analyses on immunocompromised populations <50 YOA (one conducted by the CDC, the other by the vaccine manufacturer).
All studies used the quality-adjusted life year (QALY) to measure health benefits and a monetary value (MV) to express costs in a currency appropriate to the study locale, and all studies reported incremental cost-effectiveness ratios (ICERs) defined as the ratio of incremental costs over incremental benefits between two interventions. One study32 additionally applied the net monetary benefit (NMB) metric. NMB is calculated as NMB = [Incremental Benefits] × WTP – [Incremental Costs], with WTP representing a known willingness-to-pay threshold36 for one unit of incremental benefit.
Model design
The studied model design parameters are shown in Table 2.
Table 2.
Core model characteristics.
| PMID | Author/year | Model type | Subtype | Implementation | Follow-up | Cycle time | M/F States | PHN | Other complications | HZ recurrence |
|---|---|---|---|---|---|---|---|---|---|---|
| 29297049 | Le and Rothberg (2018)21 | Static | Markov | TreeAge Pro 2017 | Lifetime (120 YOA) | 1 yr | Yes | Yes | Monocular blindness, monaural deafness | Equal to first-time incidence |
| 29958739 | You et al. (2018)34 | Static | Markov | TreeAge Pro 2009 | 50 years | 1 mo | Yes | Yes | Central nervous system infection, Ramsay Hunt syndrome, secondary SSTI, HZ ophthalmicus, disseminated HZ | No recurrence |
| 30017145 | Curran et al. (2018)22 | Static | Markov | Excel/VBA | Lifetime | 1 yr | No | Yes | Ocular, neurological, cutaneous, other non-pain | Equal to first-time incidence |
| 29987323 | Le and Rothberg (2018b)27 | Static | Markov | Excel/VBA | Lifetime | 1 yr | Yes | Yes | Monocular blindness, monaural deafness | Equal to first-time incidence |
| 30518427 | de Boer et al. (2018)29 | Static | Markov | Excel | 15 years | 1 yr | No | No | No | No recurrence |
| 30130448 | Van Oorschot et al. (2019)26 | Static | Markov | Excel/VBA | Lifetime | 1 yr | No | Yes | Ocular, neurological, cutaneous, other non-pain | Equal to first-time incidence |
| 30625011 | Curran et al. (2019)23 | Static | Markov | Excel/VBA | Lifetime | 1 yr | No | Yes | Ocular, neurological, cutaneous, other non-pain | Equal to first-time incidence |
| 30608953 | You et al. (2019)35 | Static | Markov | TreeAge Pro 2009 | Lifetime (100 YOA) | 1 mo | Yes | Yes | Central nervous system infection, Ramsay Hunt syndrome, secondary SSTI, HZ ophthalmicus, disseminated HZ | One-time only |
| 30776797 | Prosser et al. (2019)24 | Static | Markov | TreeAgo Pro 2017 | Lifetime | 1 yr | No | Yes | Ocular, neurological, cosmetic | Yes, cumulative rate applied |
| 30929219 | Shiragami et al. (2019)33 | Static | Markov | Excel/VBA | Lifetime | 1 yr | No | Yes | Misc non-PHN | Equal to first-time incidence |
| 31153691 | Hoshi et al. (2019)32 | Static | Markov | TreeAge Pro 2018 | Lifetime (100 YOA) | 1 yr | No* (Yes in the input data) | Yes | No | One-time only |
| 31289726 | Carpenter et al. (2019)25 | Static | Markov | Excel | Lifetime (100 YOA) | 1 yr | No | Yes | Acute ocular | Yes, unlimited |
| 31451524 | Drolet et al. (2019)20 | Static | Markov | Not specified | Lifetime | 1 yr | No | Yes | Ocular | Unclear |
| 31250218 | McGirr et al. (2019)26 | Static | Markov | Excel/VBA | Lifetime | 1 yr | No | Yes | No (not reported) | Equal to first-time incidence |
| 34905463 | Curran et al. (2021)28 | Static | Markov | Excel/VBA | Lifetime | 1 yr | No | Yes | Ocular, neurological, cutaneous, other non-pain | Equal to first-time incidence |
| 35094374 | Pieters et al. (2022)30 | Static | Markov | R | Lifetime (103 YOA) | 1 yr | No | Yes | No | Unclear |
| NA | Ortega-Sanchez (2021)18 | GSK: Excel/VBA CDC: not reported |
Lifetime or 30 years | 1 yr | No | Yes | CDC: unclear | |||
| NA | Ultsch et al. (2017)19 | Static | Markov | R | Lifetime | 3 mo | Yes | Yes | No | Yes |
CDC: Centers for Disease Control and Prevention; HZ: herpes zoster; M/F: male/female; Misc: miscellaneous; mo: month(s); NA: not applicable; PHN: post-herpetic neuralgia; PMID: PubMed identifier; SSTI: skin and soft tissue infection; VBA: Visual basic for applications; YOA: years of age; yr: year.
All studies utilized a combination of decision tree (for the different vaccination strategies under consideration) and Markov state-transition models deployed within each branch of the decision tree representing a distinct vaccination strategy or no vaccination.
Most models22,23,25,26,28,29,33 were implemented in Excel but a few24,32,35 relied on various versions of TreeAge Pro.37 Two models19,30 were implemented in R.38
All but one study utilized a lifetime horizon; de Boer et al.29 utilized a time horizon of 15 years. A few studies limited the time horizon to 10025,32,35 or 10330 years, and one34 imposed an upper limit on the follow-up period equal to 50 years.
Only a few studies19,21,34,35 incorporated state-transition diagrams distinguishing between health states for male and female (M/F) subjects. The study of Hoshi et al.32 reported core model input data differentiated between M/F subjects but no M/F health state differentiation was evident from the state transition diagram.
Model cycle time was generally 1 year; You et al.34,35 utilized a cycle time of 1 month, and Ultsch et al.19 a cycle time of 3 months.
An examination of the state transition diagrams for each study under consideration, cross-checked against model and methods description, revealed that all but one study29 associated PHN with a distinct health state. Complications were generally also taken into account with the exception of Hoshi et al.,32 Pieters et al.30 and Ultsch et al.19
The modeling of recurrent HZ varied between studies. Many analyses21–23,25,26,28,33 assumed a recurrent HZ incidence rate equal to that of first time HZ incidence. Recurrence was not implemented in the studies of de Boer et al.29 and You et al.34 or was restricted to a one-time event in the studies of You et al.35 and Hoshi et al.32 In one study,24 a cumulative recurrence rate was applied. The implementation of recurrence in the studies of Drolet et al.20 and Pieters et al.30 is unclear; the state transition diagram of Drolet et al.20 implies inclusion of recurrent HZ.
Most studies kept track of healthcare resources such as hospitalizations and general practitioner (GP) visits; in two studies34,35 a more general classification under inpatient/outpatient was preferred.
Finally, all model implementations enabled the conduct of deterministic and probabilistic sensitivity analyses (DSA/PSA). The CEA of Drolet et al.20 was probabilistic by design; all outcomes were presented as median values and percentiles from an extensive Monte-Carlo simulation encompassing 30,000 runs. A few studies24,25,29 performed 1- and 2-way DSAs; one study21 presented 1-, 2-, and 3-way DSAs.
CE parameters
CE parameters are summarized in Table 3.
Table 3.
Cost-effectiveness model parameters.
| PMID | Author/year | Perspective | WTP | WTP maximum | WTP reference | Fiscal basis | Currency | Costs discounting | Benefits discounting |
|---|---|---|---|---|---|---|---|---|---|
| 29297049 | Le and Rothberg (2018)21 | Societal | 50 K | 100 K | 2016 | USD | 3.0% | 3.0% | |
| 29958739 | You et al. (2018)34 | Societal | 44 K | 131 K | WHO | 2016 | USD | 3.0% | 3.0% |
| 30017145 | Curran et al. (2018)22 | Healthcare/Societal | 100 K | Not reported (2017 implied) | USD | 3.0% | 3.0% | ||
| 29987323 | Le and Rothberg (2018b)27 | Societal | 50 K | 100 K | 2017 | USD | 3.0% | 3.0% | |
| 30518427 | de Boer et al. (2018)29 | Societal | 20 K | NHCI NL | 2016 | EUR | 4.0% | 1.5% | |
| 30130448 | Van Oorschot et al. (2019)26 | Societal | 50 K | 2017 | EUR | 3.0% | 3.0% | ||
| 30625011 | Curran et al. (2019)23 | Societal | 100 K | 2016 | USD | 3.0% | 3.0% | ||
| 30608953 | You et al. (2019)35 | Societal | 46.153 K | 100 K | WHO | 2017 | USD | 3.0% | 3.0% |
| 30776797 | Prosser et al. (2019)24 | Healthcare/Societal | 100 K | 2016 | USD | 3.0% | 3.0% | ||
| 30929219 | Shiragami et al. (2019)33 | Healthcare/Societal | 5 M | Local | 2017 | Yen | 2.0% | 2.0% | |
| 31153691 | Hoshi et al. (2019)32 | Healthcare | 5 M | Local | 2016 | Yen | 3.0% | 3.0% | |
| 31289726 | Carpenter et al. (2019)25 | Societal | 50 K | 100 K | 2018 | USD | 3.0% | 3.0% | |
| 31451524 | Drolet et al. (2019)20 | Healthcare | 45 K | 2018 | CAD | 3.0% | 3.0% | ||
| 31250218 | McGirr et al. (2019)26 | Healthcare | 50 K | 100 K | 2016 | CAD | 1.5% | 1.5% | |
| 34905463 | Curran et al. (2021)28 | Societal | 50 K | 2020 | EUR | 3.0% | 3.0% | ||
| 35094374 | Pieters et al. (2022)30 | Healthcare | 40 K | 2018 | EUR | 3.0% | 1.5% | ||
| NA | Ortega-Sanchez (2021)18 | Healthcare/Societal | Not reported (100 K assumed) | 2020 | USD | 3.0% | 3.0% | ||
| NA | Ultsch et al. (2017)19 | Healthcare/Societal | 20 K, 30 K | 110 K | 2017 | EUR | 3.0% | 3.0% |
CAD: Canadian dollars; EUR: euro; K: thousand(s); M: million(s); NA: not applicable; NHCI NL: National Health Care Institute (The Netherlands); PMID: PubMed identifier; US: United States; USD: US dollars; WHO: World Health Organization; WTP: willingness to pay.
Most studies were conducted from the societal costing perspective; four studies20,26,30,32 were performed under the healthcare payer perspective, and four19,22,24,33 investigated both. The RZV manufacturer CEA on immunocompromised populations18 was also conducted from both perspectives.
ICERs were generally measured against known or assumed WTP thresholds. In one case,29 the WTP threshold was defined unambiguously in national health technology assessment (HTA) recommendations.39 WTPs were otherwise chosen empirically relying on either World Health Organization (WHO) guidelines40 or unofficial precedent.
Cost and benefits were generally discounted in agreement with prior health economic practice for the locale of interest. Notably, two CEAs conducted in Japan32,33 employed different discounting factors (2% vs 3% for both costs and benefits, respectively). Discounting rates of 2% have been recommended by the Japanese Ministry of Health, Labor and Welfare.41
In a similar fashion for two Canadian CEAs, Drolet et al.20 employed 3% for costs and benefits while McGirr et al.26 applied a rate of 1.5% for costs and benefits. Discounting factors of 1.5% in the base-case are recommended by the Canadian Agency for Drugs and Technologies in Health.42
Model inputs
Detailed model inputs are organized under Tables B1 to B7 of Appendix B.
Epidemiology
Epidemiological model inputs are compiled under Table B1.
All but two34,35 analyses relied on one or more local epidemiological sources for the incidence rate of HZ. The CEAs of You et al.34,35 reused international data sources excluding case reports. The study of Pieters et al.30 used local HZ incidence rates derived from medically attended HZ rates (ambulatory and hospitalized) but relative PHN incidence from a retrospective database analysis performed in the UK.43 The Canadian CEA by McGirr et al.26 utilized data from the province of British Columbia.44
Vaccine efficacy – RZV
Vaccine efficacy (VE) and waning model inputs are summarized in Table B2 for RZV and Table B3 for ZVL.
All studies relied on ZOE50 and ZOE70 clinical trial data45,46 to model RZV initial efficacy and waning over time. One recent analysis28 used updated efficacy data from the long-term follow-up (LTFU) study investigating the efficacy of RZV up to 8 years post-vaccination.47
One CEA34 reused the RZV efficacy model presented to ACIP in 2017.48
Most studies implemented simple linear modeling of RZV efficacy over time, with the exception of Drolet et al.20 and Pieters et al.,30 who investigated multiple non-linear efficacy models in addition to the linear one. In Pieters et al.,30 base-case results were reported for two distinct models: (a) an optimistic logarithmic model potentially underestimating waning effects and, (b) a pessimistic 1-minus exponential model resulting in rapid waning of efficacy over time. The CEA of Drolet et al.20 is unique in that it reports median (and percentile) ICERs from a total of 30,000 simulations, during which the VE model is sampled stochastically amongst a family of six frequently used VE model types. Model parameter values are not stated explicitly in Drolet et al.20
Vaccine efficacy – ZVL
All but one32 study modeled ZVL VE based on the Shingles Prevention Study (SPS)49 and its follow-ups.50,51 Some studies21–23 explicitly took Zoster Efficacy, Safety, and Tolerability (ZEST)52 into account. The study of Hoshi et al.32 relied on real-world evidence data from Baxter et al.53 The study of Carpenter et al.25 reused the ZVL VE modeling of a previous CEA.54
Top-up efficacy (ZVL) was implemented for the burden of illness (BOI) in the study of Le and Rothberg.27 Top-up efficacies for PHN were implemented in the studies of Le and Rothberg,21 McGirr et al,26 Ultsch et al.19 and Curran et al.22,23
Most studies resorted to linear modeling of ZVL efficacy, with the exception of the studies of de Boer et al.,29 Drolet et al.,20 Pieters et al.,30 and Hoshi et al.32 The 1-minus exponential VE model was reported to be the best fit in the studies of de Boer et al.29 and Pieters et al.30 The CEA of Drolet et al.20 reported median outcomes from a large number of stochastic simulations (30,000), during which the ZVL VE model type was sampled uniformly from a superset of six different non-linear models. Model parameter values were not reported explicitly in Drolet et al.,20 but may be inferred from earlier work.55,56
Direct costs
Direct HZ treatment costs are reported in Table B4.
All studies incorporated local sources for estimating the direct costs of treating a case of HZ and PHN. With the exception of Le and Rothberg.,21 You et al.,34,35 Shiragami et al.,33 Carpenter et al.,25 and Drolet et al.,20 direct costs were stratified by age or age group.
For the Dutch CEA,29 hospitalization rates, one-day hospitalization rates, GP visit rates, and over-the-counter medication costs per HZ case were combined to derive our own estimates of the aggregate HZ treatment costs.
In the Belgian CEA,30 costs were reported for hospitalized and ambulatory cases of HZ and PHN based on (pain) severity; an estimation of the aggregate costs of treating HZ and/or PHN is included in Table B4. Similarly in You et al.,34,35 direct costs per PHN case were estimated from a reported flat cost per month and a PHN persistence (duration) model detailed in the original reports.
Several studies21–24,34,35 reported costs for complications explicitly, and a few22,23,26,28,33 took into account the costs of treating adverse events due to vaccination.
None of the studies included other costs such as training, communication about the vaccine or logistic costs.
Indirect costs
Indirect costs are shown in Table B5.
All but four studies20,26,30,32 reported indirect costs in line with the costing perspective chosen for the analysis (see also Table 3). Three studies29,34,35 added lifetime earning losses (attributable to HZ death) to productivity losses due to HZ illness; one study29 relied on the friction approach57 for estimating productivity losses due to HZ death specifying a friction period of 84 days.
In two studies,34,35 indirect costs were not reported explicitly but background data relating to labor force participation by gender, unemployment rates, median monthly income, and length of hospitalization by complication type were reported; the estimates shown in Table B5 are based on the same data.
Similarly for one USA CEA,25 indirect cost data per HZ and PHN case were deduced by lost time reported in hours by severity of pain and a flat average hourly wage.
QoL and utilities
QoL and utility inputs are reported in Table B6.
Several studies20–26,28,29,32,33 reported QALY losses per case of HZ directly.
In most cases QALY losses were age-specific, but two studies25,26 reported aggregate losses averaged across all age groups. Only two studies22,23 reported different QALY losses for vaccinated and unvaccinated subjects in line with the observations of the SPS49 and following the QALY loss implementation in a previous CEA for ZVL.58
The Dutch CEA29 did not distinguish between a case of HZ with or without PHN; average values were employed and reported.
In the Hong Kong CEAs,34,35 disutility values were reported for outpatient & inpatient cases of HZ with or without complications, along with a complex non-linear model for estimating the persistence of PHN beyond 12 months. These data formed the basis of HZ and PHN QALY loss estimation by case shown in Table B6.
The CEAs by Le and Rothberg21 reported QALY losses for HZ explicitly but refrained from providing concrete values for PHN. Additional pain data from a previous epidemiological study performed in the UK59 were reported by the authors for PHN, and those formed the basis of our own estimates of age-specific QALY losses for PHN included in Table B6.
HZ and PHN QALY losses in Pieters et al.30 relied on previous work60 demonstrating QALY/utility loss factors by severity of pain as well as data on the proportion of subjects in each pain state from an older epidemiological study conducted in the UK.43 These were combined to complete the estimates under Table B6.
Finally, QALY losses per HZ and PHN case were not stated explicitly in Ultsch et al.19 despite explicit reference to a previous prospective QoL study in Canada;61 the estimations shown in Table B6 were based on the same source.
Adverse events (AEs)
Model input parameters related to AEs post-vaccination are compiled in Table B7, including information on frequency by AE type, treatment costs by type, as well as utility/QALY losses by type when available. The aggregated treatment costs of AEs per inoculation are shown in Table B4 (direct costs).
Model outputs
Top-level CE results are summarized in Table 4. A more detailed list of ICERs is compiled under Table B8.
Table 4.
Cost-effectiveness results.
| Author/year | CE outcome | Parameters affecting DSA | PSA runs | PSA results |
|---|---|---|---|---|
| Le and Rothberg (2018)21 | RZV was cost-effective vs no vaccination at all ages; RZV was cost-saving vs ZVL at all ages; RZV was most cost-effective at 70 YOA with an ICER of $20K (USD) |
RZV price per dose; RZV efficacy & waning; PHN incidence (duration over 12 mo); RZV 2nd dose compliance |
10,000 | RZV had between 73% and 91% probability of being cost-effective at a WTP threshold of $50K (USD), and between 78% and 93% probability of being cost-effective at WTP of $100K (USD), depending on vaccination age |
| You et al. (2018)34 | RZV was cost-effective vs no vaccination; RZV was most cost-effective at 70/60 YOA with ICERs of $46.3K/$47.4K (USD) | RZV price per dose; 2-dose RZV efficacy waning; HZ outpatient treatment cost; QALY losses outpatient HZ |
10,000 | RZV had 100% probability of being cost-effective at all ages with a WTP threshold equal to 3 times the GDP per capita; RZV had 60.1%/53.1%/23.9% probability of being cost-effective at 70/60/50 YOA with a WTP threshold equal to the GDP per capita; RZV had 90% probability of being cost-effective at 70/60/50 YOA with WTP thresholds equal to $53.76K/$57.68K/$78.4K (USD) |
| Curran et al. (2018)22 | RZV was cost-effective at all ages vs no vaccination; RZV was cost-saving vs ZVL at 60+ YOA |
RZV efficacy waning (all ages); HZ incidence; Discount rates; 2-dose RZV efficacy waning (≥70 YOA) |
5000 | RZV vaccination at 60+ YOA vs no vaccination had 98%/99.5% probability of being cost-effective below WTP thresholds of $80K/$100K (USD); RZV vaccination at 60+ YOA vs ZVL vaccination at 60+ YOA had a 99% probability of being cost-saving |
| Le and Rothberg (2018b)27 | RZV vaccination with 56.2% second dose compliance was cost-effective vs no vaccination with ICERs below $100K (USD) at 53.2+ YOA and below $50K (USD) at 57.1+ YOA; RZV vaccination with 100% second dose compliance was cost-effective vs no vaccination with ICER below $100K (USD) at approx. 52+ YOA; Revaccination with RZV at 100% series compliance would be cost-effective at 61+ or 71+ YOA given prior ZVL vaccination at 60 or 70 YOA; Revaccination with RZV at 56% series compliance would be cost-effective at 64+ or 74+ YOA given prior ZVL vaccination at 60 or 70 YOA |
PHN incidence; QALY losses; RZV efficacy & waning; RZV price per dose |
10,000 | RZV had 23% probability of being cost-effective at 50 YOA (results for other ages not reported) |
| de Boer et al. (2018)29 | RZV was most cost-effective at 70 YOA with maximum prices at threshold estimated at €54.5/€137.45 at WTP thresholds of €20K/€50K; ZVL was most cost-effective at 60 YOA at a price of €51.37 at the WTP threshold of €20K |
QALY loss HZ; RZV efficacy waning after 4 years; HZ incidence (immunocompetent population) |
10,000 | RZV had over 90% probability of being the most cost-effective option vs no vaccination when vaccine costs per dose were kept below €49.74, €85.8, and €83.64 for 50, 60, and 70 YOA respectively; at 60 YOA, pricing scenarios dictated which vaccine is most cost-effective |
| Van Oorschot et al. (2019)26 | RZV was cost-effective vs no vaccination at 60+ and 70+ YOA; RZV was most cost-effective at 60 and 65 YOA with an ICER of approx. €29.5K |
HZ incidence; PHN incidence (initial); RZV efficacy waning (≥70 YOA); QALY loss unvaccinated case with PHN |
5000 | RZV had 84%/67% probability of being cost-effective at 60+/70+ YOA |
| Curran et al. (2019)23 | RZV revaccination at 60+ YOA was cost-effective vs control previously vaccinated with ZVL (5 years earlier) with an ICER of approx. $59K (USD); RZV revaccination was cost-saving vs ZVL revaccination at 60+ YOA |
RZV efficacy waning; RZV efficacy waning (≥70 YOA); HZ incidence; Discount rates (costs and benefits); Time elapsed between original vaccination and revaccination |
5000 | RZV vaccination vs no revaccination had 75% probability of being cost-effective |
| You et al. (2019)35 | RZV was cost-effective for M and F 50–80 YOA at a price per dose of $80 (USD); RZV was cost-effective for M 54–74 YOA and F 50–79 YOA at a price per dose of $100 (USD); RZV was cost-effective for F 58–72 YOA at a price per dose of $120 (USD) |
Age (M and F); Vaccine cost (M) |
10,000 | RZV had 85.5%/99.7%/99.7%/77% probability of being cost-effective (WTP = 1×GDP per capita) in females 50/60/70/80 YOA; RZV had 57.9%/98.6%/95.6%/26.5% probability of being cost-effective (WTP = 1×GDP per capita) in males 50/60/70/80 YOA |
| Prosser et al. (2019)24 | RZV vaccination vs no vaccination was cost-effective at all ages under the societal perspective with ICERs ranging from $10K to $47K (USD); RZV was most cost-effective at 60+ YOA with an ICER of approx. $19K (USD) under the societal perspective; under the healthcare payer perspective, RZV was most cost-effective at 60+ YOA with an ICER of approx. $29K (USD); RZV revaccination vs control previously vaccinated with ZVL was cost-effective at all age groups under the societal perspective, except for immediate revaccination at 50–59 YOA. ICERs were lower at 80–89 and 70–79 YOA |
Initial RZV efficacy; HZ incidence; PHN incidence; RZV cost per dose; PHN cost; |
10,000 | RZV had 84%/95%/99% probability of being cost-effective at 50-79/60-69/70–99 YOA |
| Shiragami et al. (2019)33 | RZV was cost-effective at 65+ YOA with ICERs of ¥4316K/¥4036K under the payer/societal perspective | RZV efficacy waning (≥70 YOA); PHN incidence; HZ incidence; Vaccine price per dose |
5000 | RZV had 72.2%/79.7% probability of being cost-effective under the payer/societal perspective at a WTP threshold of ¥5 M |
| Hoshi et al. (2019)32 | RZV was marginally cost-effective at 80–84 YOA with an ICER of approx. ¥5.26 M per QALY gained; ZVL was more cost-effective than RZV at all age groups and most cost-effective at 80–84 YOA with an ICER of approx. ¥2.6 M |
RZV price per dose; RZV waning duration (2-dose); QALY losses HZ (with or without PHN) |
1000 | RZV had 43.8% probability of being cost-effective at 65–84 YOA at the WTP threshold of ¥5 M; ZVL had 56.2% probability of being cost-effective at 65–84 YOA at the WTP threshold of ¥5 M |
| Carpenter et al. (2019)25 | RZV was more cost-effective than ZVL at all age groups; RZV was most cost-effective at 70/60 YOA with ICERs of $1.4K/$19.3K (USD) |
1-way: efficacy waning; 2-way: efficacy waning and age of vax |
RZV had 82%/69% probability of being cost-effective at WTP thresholds of $100K/$50K (USD) for all ages (weighed average) | |
| Drolet et al. (2019)20 | RZV was cost-saving or cost-effective at all ages; RZV was more cost-effective than ZVL at all ages; RZV was most cost-effective at 75/70/65 YOA with approx. ICERs of $0.8K/$4.2K/$5.3K (CAD) |
NA | 30,000 | RZV had 75% probability of being cost-effective at all ages ≥60 with a vaccine price per dose of $100 (CAD) |
| McGirr et al. (2019)26 | RZV was cost-effective vs no vaccination at 60+ YOA with an ICER of $28.36K (CAD); RZV was cost-effective vs ZVL with an ICER of $2.4K (CAD) | RZV vs control: 2-dose RZV efficacy waning (≥70 YOA); HZ incidence; PHN incidence (first time) RZV vs ZVL: RZV second dose compliance; 2-dose RZV efficacy waning (≥70 YOA); RZV price per dose |
5000 | RZV had 63.5%/99.2%/100% probability of being cost-effective vs no vaccination at WTP thresholds of $30K/$50K/$100K (CAD); RZV had 100% probability of being cost-effective vs ZVL at the WTP threshold of $50K (CAD), and 48.2% probability of being cost-neutral or cost-saving |
| Curran et al. (2021)28 | RZV was cost-effective at all ages investigated at the revised price of €133.62 per dose and most cost-effective at 50+ YOA with an ICER of €31.7K | HZ incidence; PHN incidence; Annual waning of RZV; QALY loss of unvaccinated HZ case with PHN |
5000 | RZV had a 94%/92.9% probability of being cost-effective at 50+/60+ YOA; at 60+ YOA the maximum RZV price per dose retaining cost-effectiveness below the WTP threshold of €50K was estimated at €163 |
| Pieters et al. (2022)30 | RZV was generally not cost-effective; Under the logarithmic VE model for RZV at a price per dose of €140.26 and at 50 YOA, RZV would only be cost-effective at a WTP threshold of €90K or higher; At 50 YOA the maximum cost-effective price per dose with a WTP threshold of €40K was €55.4 |
RZV price per dose Duration of protection (VE model) |
No explicit ICER acceptability results were discussed | |
| Ortega-Sanchez (2021)18 | RZV was cost-saving in HSCT patients by both models (industry/CDC); RZV was cost-saving in renal transplant patients (industry model) and multiple myeloma (CDC model); RZV was cost-effective in hematologic malignancy and HIV (CDC model) with ICERs of $10K and $79K (USD) respectively; RZV was cost-effective in HIV, breast cancer, and Hodgkin’s lymphoma (industry model) with ICERs of $33K, $68K, and $96K (USD) respectively |
Not elaborated | RZV had a 72% probability of being cost-effective (CDC model); RZV had a 90% probability of being cost-effective and a 50% probability of being cost-saving (industry model) |
|
| Ultsch et al. (2017)19 | RZV was most cost-effective at 60 and 65 YOA with an ICER of approx. €24K; ZVL at 60 YOA was not cost-effective with an ICER exceeding €88K. | Vaccination age; Max duration of protection 5 years, Vaccination costs; PHN incidence; Discounting factors; Recurrent HZ; Baseline utilities |
10,000 | RZV had a 90%/50% probability of being cost-effective at WTP thresholds of €30K/€20K; ZVL had a 90%/50% probability of being cost-effective only at substantially higher WTP thresholds (€110K/€90K) |
CAD: Canadian dollars; CDC: Centers for Disease Control and Prevention; CE: cost-effectiveness; DSA: deterministic sensitivity analysis; GDP: gross domestic product; HIV: human immunodeficiency virus; HSCT: hematopoietic stem cell transplantation; HZ: herpes zoster; ICER: incremental cost effectiveness ratio; K: thousand(s); M/F: male/female; M: million(s); PHN: post-herpetic neuralgia; PSA: probabilistic sensitivity analysis; QALY: quality-adjusted life year; RZV: recombinant zoster vaccine; US: United States; USD: US dollars; VE: vaccine efficacy; WTP: willingness to pay; YOA: years of age; ZVL: zoster vaccine live.
Top-level CE results
All but three studies29,30,32 demonstrated the cost-effectiveness of RZV vaccination vs no vaccination or vaccination with ZVL.
Three studies established the cost-effectiveness of RZV revaccination for subjects previously vaccinated with ZVL.21,23,24
Many studies19–22,24–26,28,33 demonstrated the CE of RZV across all age groups investigated.
In immunocompromised populations,18 RZV was found cost-saving in hematopoietic stem cell transplantation (HSCT) patients by two models (industry/CDC). RZV was also found cost-saving in renal transplant (industry model) and multiple myeloma (CDC model); RZV was cost-effective in hematologic malignancy and human immunodeficiency virus (HIV) patients (CDC model), and HIV, breast cancer, Hogkin lymphoma patients (industry model).
Sensitivity analyses
All studies provided a number of model input parameters with the greatest effect on CE. Those included structural model inputs such as discount rates, but also vaccination costs (i.e., vaccine prices per dose), vaccine efficacy and waning parameters, HZ and PHN incidence, QALY losses, and direct treatment costs. A non-exhaustive list by study is shown in Table 4.
Detailed CE results
A non-exhaustive list of ICERs reported by each study by age group, costing perspective, com-parison type (i.e., RZV vs no vaccination or RZV vs ZVL, etc.), and corresponding vaccine price per dose is compiled under Table B8.
Discussion
The CE of HZ vaccination in older adults has been reviewed in the past.62–64 The present study focuses on the CE of HZ vaccination with RZV. While one and nine manuscripts on the CE of RZV vaccination were identified in the systematic reviews of Chiyaka et al.62 and Udayachalerm et al.,64 respectively, our search has in the meantime identified an additional nine records, for a total of 18 studies included in the present review. All studies were performed in high-income countries, consistent with the observation of Chiyaka et al.62 The CHEERS checklist indicates studies of high quality, with the exception of the presentation to the CDC,18 which does not reflect on the quality of the original research contained within (two unrelated CE models on select immunocompromised cohorts, one by the CDC, the other by the vaccine manufacturer). Our CE findings are generally in good agreement with previous reports.62,64 Overall, RZV was found cost-effective in 15 out of 18 studies, cost-effective or cost-saving in the subset of the aforementioned 15 studies where a direct comparison to ZVL was applicable, and cost-effective in revaccinating cohorts previously vaccinated with ZVL. RZV was additionally found cost-effective or cost-saving in a variety of immunocompromising conditions.
A quantitative exploration of CE outcomes such as the meta-analysis of net monetary benefits in Udayachalerm et al.64 was not attempted. Instead, a critical review of variations in CE levels based on an in-depth look into modeling structure and model input data was undertaken, and main findings are discussed below.
All 18 models in this review were static models, i.e., no dynamic models evaluating RZV were identified. The comparison of CE analyses performed under varying assumptions is difficult in view of variation in methodological approaches. While a typical static multi-cohort health economic model using state transition probabilities (Markov model) is straightforward to construct for HZ and PHN, ICER estimation is invariably non-linear in nature and remains sensitive to the range of inputs. Structural parameters such as discounting rates and model time horizon (follow-up period) are known to have a pronounced effect on ICERs, rendering the direct comparison of models developed for different locales under different prevailing HTA guidelines challenging. In addition, ICERs are not directly comparable when key inputs vary between models, including RZV price per dose and 2nd dose RZV series compliance.
Because vaccine efficacy and waning over time coupled with HZ incidence rates determine the number of incident HZ cases as a function of time, the RZV vaccine efficacy model chosen by each study (and the corresponding ZVL vaccine efficacy model for direct comparisons) was an important input in the reviewed CE analyses. As an example, three CEAs conducted in the US22,24,25 predicted widely varying ICERs at 50 (or 50–59) YOA: $14.9K, $46.8K, and $91.2K, respectively. A simple estimation of the RZV duration of protection (from initial efficacy to zero) in the three studies from the VE data of Table B2 suggests 35, 19.4, and 17.8 years respectively. However, updated clinical trial data28,47 estimate a vaccine efficacy of 84.1% eight-year post-vaccination with 2-doses of RZV, indicating that waning of efficacy to zero after 17.8 or even 19.4 years is unlikely.
A quick comparison of other inputs between Curran et al.22 and Prosser et al.24 reveals slightly lower HZ incidence rates in Prosser et al.,24 lower QALY losses per HZ case in Curran et al.,22 and higher costs per HZ case in Prosser et al.24 (but lower for PHN). Similarly, the estimated QALY losses per HZ and PHN case are higher in Carpenter et al.25 than in Curran et al.,22 and HZ incidence is identical. Yet ICER in Carpenter et al.25 is several times higher than in Curran et al.,22 specifically for the 50–59-year-old age group, due to the differences in the duration of protection as outlined above.
The optimal age of vaccination with RZV varied between studies. In the German CEA of Curran et al.,28 which made use of 8-year long VE data for RZV, the cohort of 50+ YOA was established as the most cost-effective under the societal perspective, while the independent investigation of Prosser et al.48 estimated the CE-optimal vaccination cohort at 60+ YOA.
Two alternative CEAs conducted in the setting of Japan32,33 also deserve a more detailed comparative analysis and interpretation. The study of Shiragami et al.33 supports RZV CE, while Hoshi et al.32 indicates marginal CE for RZV at 80+ YOA only (see Table B8 for the details). A careful investigation of structural model parameters reveals that Hoshi et al.32 utilized discounting rates of 3% vs 2% in Shiragami et al.33 The RZV price per dose in Hoshi et al.32 was approximately 16% higher than the one quoted in Shiragami et al.33 Costs were comparable across the two studies but QALY losses for HZ and PHN were slightly lower in Hoshi et al.32 Most importantly, RZV efficacy modeling in Hoshi et al.32 assumed faster waning over time resulting in diminished (zero) protection after 19.4 years, which is not supported by the latest RZV vaccine efficacy data.28,47 At the same time, efficacy and waning of ZVL in Hoshi et al.32 followed Baxter et al.,53 which estimates VE at 31.8% (95% confidence interval [CI] 15.1% to 45.2%) after 8 years, while a similar RWE study65 indicates only 4.2% (95% CI 24.0% to 25.9%) at year 8, and the long-term persistence substudy51 reports a vaccine efficacy for incidence of HZ of 31.1% (22.4% to 36.2%) at year 8, but only 6.8% (−4.9% to 13.4%) at year 9, and already negative at −1.7% (−14.2% to 4.8%) 11 years post-vaccination.
In the case of one CEA conducted in the Netherlands,29 low RZV CE levels may similarly follow as the synergistic effect of the following factors: (a) a modeled time-horizon restricted to 15 years, (b) assumed RZV vaccine efficacy waning of 4.1% annually for 50–69 YOA after 4 years post-vaccination and for 70+ YOA, (c) recurrent HZ incidence not included in the model, (d) adjustment (lowering) of the nationally reported HZ incidence by 10% for possible false-positive diagnoses, and, (e) low relative PHN incidence, which implicitly affects the estimation of QALY losses.66
In the Belgian CEA,30 the atypically low RZV CE outcomes may be traced to adjustments performed on the overall HZ incidence rates to immunocompetent specific incidence rates, using a simplistic calculation (the overall HZ incidence rates are presented in Bilcke et al.67) Appropriate adjustments would rely on knowledge of the true proportion of immunocompetent individuals in the population, as well as on appropriate risk ratios, i.e., the risk of HZ in the immunocompromised population versus the risk of HZ in the immunocompetent population. Consequently, the adjustments performed resulted in artificially low HZ incidence rates leading to low RZV CE outcomes. Moreover, RZV is indicated in individuals who are immunocompromised. As such, an analysis of the cost-effectiveness of RZV could be done on all patients applying overall HZ incidence rates, making the need to perform adjustments on the overall incident rates redundant.
In a previous review of HZ vaccine cost-effectiveness manuscripts, Szucks et al noted that a limitation of most modeling studies was that outdated input data were used.68 The authors further noted that cost-effectiveness models should be updated when new evidence becomes available to support the effect on a potential vaccination recommendation. In the case of RZV, because longer-term follow-up study results on the efficacy of the vaccine become continuously available,69 future studies examining the CE of RZV in different settings should be expected, potentially exhibiting less variability in outcomes as a consequence of reduced uncertainty in vaccine efficacy estimates over time.
Most cost-effectiveness models focused on costs of administering a vaccine (e.g. vaccine and administration costs, costs of treating adverse events) and did not include other costs such as training, communication about the vaccine, and logistics.
As a final point, most analyses did not include differential utility losses for vaccinated and unvaccinated cases. Similar to other vaccine preventable diseases, it has been demonstrated that in breakthrough cases of HZ following vaccination there is an attenuation in the severity of the disease,70 and future studies would be expected to implement utility loss values differentiating between vaccinated and unvaccinated subjects accordingly.
Supplementary Material
Acknowledgements
The authors would like to thank Dr Ioannis Polios (independent consultant) for valuable comments and insightful review during manuscript development. The authors would also like to thank Business & Decision Life Sciences platform for editorial assistance and manuscript coordination, on behalf of GSK.
Funding Statement
GlaxoSmithKline Biologicals SA funded this study/research (GSK study identifier: VeevaHO: VEO-000338) and was involved in all stages of study conduct, including analysis of the data. GlaxoSmithKline Biologicals SA also took in charge all costs associated with the development and publication of this manuscript.
Disclosure statement
NG, CN and DC are employed by GSK. NG and DC hold shares in GSK. All authors declare no other financial and non-financial relationships and activities.
Contributorship
All authors were involved in the design of the study, collected or generated the data, analyzed and/or interpreted the data and participated to the development of this manuscript and in its critical review with important intellectual contributions. All authors had full access to the data and gave approval of the final manuscript before submission. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The work described was carried out in accordance with ICMJE recommendations for conduct, reporting, editing and publications publishing of scholarly work in medical journals. The corresponding author had the final responsibility to submit for publication.
Trademark
Shingrix is a trademark owned by or licensed to GSK.
Zostavax is a trademark of Merck Sharp & Dohme Corp.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2023.2168952
References
- 1.Schmader K. Herpes Zoster. Ann Intern Med. 2018;169(3):1–13. doi: 10.7326/AITC201808070. [DOI] [PubMed] [Google Scholar]
- 2.van Oorschot D, Vroling H, Bunge E, Diaz-Decaro J, Curran D, Yawn B. A systematic literature review of herpes zoster incidence worldwide. Hum Vacc Immunotherap. 2021;17(6):1714–32. doi: 10.1080/21645515.2020.1847582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coplan PM, Schmader K, Nikas A, Chan ISF, Choo P, Levin MJ, Johnson G, Bauer M, Williams HM, Kaplan KM, et al. Development of a measure of the burden of pain due to herpes zoster and postherpetic neuralgia for prevention trials: adaptation of the brief pain inventory. J Pain. 2004;5(6):344–56. doi: 10.1016/j.jpain.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 4.Johnson RW, Wasner G, Saddier P, Baron R. Postherpetic neuralgia: epidemiology, pathophysiology and management. Expert Rev Neurother. 2007;7(11):1581–95. doi: 10.1586/14737175.7.11.1581. [DOI] [PubMed] [Google Scholar]
- 5.Lang P-O, Aspinall R. Vaccination for quality of life: herpes–zoster vaccines. Aging Clin Exp Res. 2021;33(4):1113–22. doi: 10.1007/s40520-019-01374-5. [DOI] [PubMed] [Google Scholar]
- 6.US Food & Drug Administration . Biologics License Application (BLA) approval for Zoster vaccine recombinant. Adjuvanted; 2017. [accessed 2022 Jul 6]. https://www.fda.gov/media/108274/download [Google Scholar]
- 7.Dooling KL, Guo A, Patel M, Lee GM, Moore K, Belongia EA, Harpaz R. Recommendations of the advisory committee on immunization practices for use of Herpes Zoster vaccines. Morb Mort Wkly Rep. 2018;67(3):103–08. doi: 10.15585/mmwr.mm6703a5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson TC, Masters NB, Guo A, Shepersky L, Leidner AJ, Lee GM, Kotton CN, Kotton KL. Use of recombinant Zoster vaccine in immunocompromised adults aged ≥19 years: recommendations of the Advisory Committee on Immunization Practices — United States, 2022. Morb Mort Wkly Rep. 2022;71(3):80–84. doi: 10.15585/mmwr.mm7103a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.European Medicines Agency . Shingrix. Authorisation Details. [accessed 2022. Jul 6]. https://www.ema.europa.eu/en/medicines/human/EPAR/shingrix#authorisation-details-section [Google Scholar]
- 10.Parikh R, Widenmaier R, Lecrenier N. A practitioner’s guide to the recombinant zoster vaccine: review of national vaccination recommendations. Expert Rev Vacc. 2021;20(9):1065–75. doi: 10.1080/14760584.2021.1956906. [DOI] [PubMed] [Google Scholar]
- 11.US Food & Drug Administration . Biologics License Application (BLA) approval for Zoster vaccine. Live; 2006. [accessed 2022 Jul 6]. http://wayback.archive-it.org/7993/20170722150959/https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm132873.htm [Google Scholar]
- 12.European Medicines Agency Zostavax. Authorisation Details. [accessed 2022. Jul 6]. https://www.ema.europa.eu/en/medicines/human/EPAR/zostavax#authorisation-details-section [Google Scholar]
- 13.Centers for Disease Control and Prevention . Zostavax (Zoster Vaccine Live) recommendations; 2020. [accessed 2022 Jul 15]. https://www.cdc.gov/vaccines/vpd/shingles/hcp/zostavax/recommendations.html.
- 14.Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, Shamseer L, Tetzlaff J, Akl E, Brennan S, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. 2021. J Clin Epidemiol. 2021;134:178–89. doi: 10.1016/j.jclinepi.2021.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Husereau D, Drummond M, Augustovski F, de Bekker-Grob E, Briggs AH, Carswell C, Caulley L, Chaiyakunapruk N, Greenberg D, Loder E, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) 2022 explanation and elaboration: a report of the ISPOR CHEERS II good practices task force. Value Health. 2022;25(1):10–31. doi: 10.1016/j.jval.2021.10.008. [DOI] [PubMed] [Google Scholar]
- 16.An Advisory Committee Statement (ACS) . National Advisory Committee on Immunization (NACI). Updated recommendations on the use of Herpes Zoster vaccines. 2018. [accessed 2022 May 10]. https://www.canada.ca/content/dam/phac-aspc/documents/services/publications/healthy-living/updated-recommendations-use-herpes-zoster-vaccines-eng.pdf.
- 17.Institut national de santé publique du Québec . Avis sur la pertinence d’ajouter la vaccination contre le zona au Programme québécois d’immunisation; 2018. [accessed 2022 May 10]. https://www.inspq.qc.ca/publications/2381.
- 18.Ortega-Sanchez IR Economics of vaccinating immunocompromised 19–49-years-old adults against herpes zoster in the US; 2021. [accessed 2022 May 10]. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2021-09-29/02-ZosterVaccines-OrtegaSanchez-508.pdf.
- 19.Ultsch B, Weidemann F, Koch J, Siedler A. Modellierung von epidemiologischen und gesundheitsökonomischen: Effekten von Impfungen zur Prävention von Herpes zoster; 2017. [access 2022 May 10]. https://www.rki.de/DE/Content/Infekt/Impfen/ImpfungenAZ/Zoster/Modellierung_Zoster_Impfung.pdf?__blob=publicationFile.
- 20.Drolet M, Zhou Z, Sauvageau C, DeWals P, Gilca V, Amini R, Bénard É, Brisson M. Effectiveness and cost-effectiveness of vaccination against herpes zoster in Canada: a modelling study. Can Med Assoc J. 2019;191(34):E932–9. doi: 10.1503/cmaj.190274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Le P, Rothberg MB. Cost-effectiveness of the adjuvanted Herpes Zoster subunit vaccine in older adults. JAMA Intern Med. 2018;178(2):248–58. doi: 10.1001/jamainternmed.2017.7431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Curran D, Patterson B, Varghese L, Van Oorschot D, Buck P, Carrico J, Hicks K, Lee B, Yawn B. Cost-effectiveness of an adjuvanted recombinant Zoster vaccine in older adults in the United States. Vaccine. 2018;36(33):5037–45. doi: 10.1016/j.vaccine.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 23.Curran D, Patterson BJ, Van Oorschot D, Buck PO, Carrico J, Hicks KA, Lee B, Yawn BP. Cost-effectiveness of an adjuvanted recombinant zoster vaccine in older adults in the United States who have been previously vaccinated with zoster vaccine live. Hum Vacc Immunotherap. 2019;15(4):765–71. doi: 10.1080/21645515.2018.1558689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prosser LA, Harpaz R, Rose AM, Gebremariam A, Guo A, Ortega-Sanchez IR, Zhou F, Dooling K. A cost-effectiveness analysis of vaccination for prevention of Herpes Zoster and related complications: input for national recommendations. Ann Intern Med. 2019;170(6):380–88. doi: 10.7326/M18-2347. [DOI] [PubMed] [Google Scholar]
- 25.Carpenter CF, Aljassem A, Stassinopoulos J, Pisacreta G, Hutton D. A cost-effectiveness analysis of an adjuvanted subunit vaccine for the prevention of Herpes Zoster and post-herpetic neuralgia. Open Forum Infect Dis. 2019;6(7):ofz219. doi: 10.1093/ofid/ofz219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGirr A, Van Oorschot D, Widenmaier R, Stokes M, Ganz ML, Jung H, Varghese L, Curran D. Public health impact and cost-effectiveness of non-live adjuvanted recombinant Zoster vaccine in Canadian adults. Appl Health Econ Health Policy. 2019;17(5):723–32. doi: 10.1007/s40258-019-00491-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Le P, Rothberg MB. Cost-effectiveness of the recommendations of the Advisory Committee on immunization practices for the recombinant adjuvanted Zoster subunit vaccine. JAMA Intern Med. 2018;178(9):1277–78. doi: 10.1001/jamainternmed.2018.3200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Curran D, Van Oorschot D, Matthews S, Hain J, Salem AE, Schwarz M. Long-term efficacy data for the recombinant zoster vaccine: impact on public health and cost effectiveness in Germany. Hum Vacc Immunotherap. 2021;17(12):5296–303. doi: 10.1080/21645515.2021.2002085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Boer PT, van Lier A, de Melker H, van Wijck AJM, Wilschut JC, van Hoek AJ, Postma MJ, de Boer PT, van Wijck AJM, van Hoek AJ. Cost-effectiveness of vaccination of immunocompetent older adults against herpes zoster in the Netherlands: a comparison between the adjuvanted subunit and live-attenuated vaccines. BMC Med. 2018;16(1):228. doi: 10.1186/s12916-018-1213-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pieters Z, Ogunjimi B, Beutels P, Bilcke J. Cost-effectiveness analysis of Herpes Zoster vaccination in 50- to 85-year-old immunocompetent Belgian cohorts: a comparison between no vaccination, the adjuvanted subunit vaccine, and live-attenuated vaccine. PharmacoEconomics. 2022;40(4):461–76. doi: 10.1007/s40273-021-01099-2. [DOI] [PubMed] [Google Scholar]
- 31.Van Oorschot D, Anastassopoulou A, Poulsen Nautrup B, Varghese L, von Krempelhuber A, Neine M, Lorenc S, Curran D. Cost-effectiveness of the recombinant zoster vaccine in the German population aged ≥60 years old. Hum Vacc Immunotherap. 2019;15(1):34–44. doi: 10.1080/21645515.2018.1509645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoshi S-L, Seposo X, Shono A, Okubo I, Kondo M. Cost-effectiveness of recombinant Zoster vaccine (RZV) and Varicella Vaccine Live (VVL) against herpes zoster and post-herpetic neuralgia among adults aged 65 and over in Japan. Vaccine. 2019;37(27):3588–97. doi: 10.1016/j.vaccine.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 33.Shiragami M, Mizukami A, Kaise T, Curran D, Van Oorschot D, Bracke B, Watanabe D. Cost-effectiveness of the adjuvant recombinant Zoster vaccine in Japanese adults aged 65 years and older. Dermatol Ther (Heidelb). 2019;9(2):281–97. doi: 10.1007/s13555-019-0291-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.You JHS, Ming W-K, Lee C-F, Tsang O-Y, Chan P-S. Potential cost-effectiveness of adjuvanted herpes zoster subunit vaccine for older adults in Hong Kong. Vaccine. 2018;36(31):4610–20. doi: 10.1016/j.vaccine.2018.06.049. [DOI] [PubMed] [Google Scholar]
- 35.You JHS, Ming W-K, Tsang O-Y, Chan P-S. Optimal gender-specific age for cost-effective vaccination with adjuvanted herpes zoster subunit vaccine in Chinese adults. PLOS One. 2019;14(1):e0210005. doi: 10.1371/journal.pone.0210005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Trippoli S. Incremental cost-effectiveness ratio and net monetary benefit: current use in pharmacoeconomics and future perspectives. Eur J Intern Med. 2017;43:e36. doi: 10.1016/j.ejim.2017.05.015. [DOI] [PubMed] [Google Scholar]
- 37.TreeAge . 2022. TreeAge Pro. Willamstown, MA: TreeAge Software [Google Scholar]
- 38.R Core Team . R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 39.Zorginstituut Nederland . Guideline for economic evaluations in healthcare; 2016. [accessed 2022 May 10]. https://english.zorginstituutnederland.nl/binaries/zinl-eng/documenten/reports/2016/06/16/guideline-for-economic-evaluations-in-healthcare/Guideline+for+economic+evaluations+in+healthcare.pdf.
- 40.World Health Organization . Making choices in health: wHO guide to cost-effectiveness analysis. In: Tan-Torres Edejer T, Baltussen R, Adam T, Hutubessy R, Acharya A, Evans DB, Murray CJL, editors. 2003. Geneva:World Health Organization. [Google Scholar]
- 41.Japanese Ministry of Health LaW . Analysis guidelines on cost-effectiveness evaluation in Central Social Insurance Medical Council. 2016. [accessed 2022 Oct 10]. http://www.mhlw.go.jp/file/05-Shingikai-12404000-Hokenkyoku-Iryouka/0000109789.pdf.
- 42.Canada’s Drug and Health Technology Agency . Guidelines for the economic evaluation of health technologies: Canada; 2017. [accessed 2022 May 10]. https://www.cadth.ca/sites/default/files/pdf/guidelines_for_the_economic_evaluation_of_health_technologies_canada_4th_ed.pdf.
- 43.Gauthier A, Breuer J, Carrington D, Martin M, Rémy V. Epidemiology and cost of herpes zoster and post-herpetic neuralgia in the United Kingdom. Epidemiol Infect. 2009;137(1):38–47. doi: 10.1017/S0950268808000678. [DOI] [PubMed] [Google Scholar]
- 44.Marra F, Chong M, Najafzadeh M. Increasing incidence associated with herpes zoster infection in British Columbia, Canada. BMC Infect Dis. 2016;16(1):589. doi: 10.1186/s12879-016-1898-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lal H, Cunningham AL, Godeaux O, Chlibek R, Diez-Domingo J, Hwang S-J, Levin MJ, McElhaney JE, Poder A, Puig-Barberà J, et al. Efficacy of an adjuvanted Herpes Zoster subunit vaccine in older adults. N Engl J Med. 2015;372(22):2087–96. doi: 10.1056/NEJMoa1501184. [DOI] [PubMed] [Google Scholar]
- 46.Cunningham AL, Lal H, Kovac M, Chlibek R, Hwang S-J, Díez-Domingo J, Godeaux O, Levin MJ, McElhaney JE, Puig-Barberà J, et al. Efficacy of the Herpes Zoster subunit vaccine in adults 70 years of age or older. N Engl J Med. 2016;375(11):1019–32. doi: 10.1056/NEJMoa1603800. [DOI] [PubMed] [Google Scholar]
- 47.Boutry C, Hastie A, Diez-Domingo J, Tinoco JC, Yu C-J, Andrews C, Beytout J, Caso C, Cheng H-S, Cheong HJ, et al. The adjuvanted recombinant Zoster vaccine confers long-Term Protection Against Herpes Zoster: interim Results of an Extension Study of the Pivotal phase 3 clinical trials ZOE-50 and ZOE-70. Clin Infect Dis. 2022;74(8):1459–67. doi: 10.1093/cid/ciab629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Prosser LA. Economic evaluation of vaccination for prevention of Herpes Zoster and related complications. Atlanta, GA: University of M; 2017. [Google Scholar]
- 49.Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD, Arbeit RD, Simberkoff MS, Gershon AA, Davis LE, et al. A vaccine to prevent Herpes Zoster and postherpetic neuralgia in older adults. N Engl J Med. 2005;352(22):2271–84. doi: 10.1056/NEJMoa051016. [DOI] [PubMed] [Google Scholar]
- 50.Schmader KE, Oxman MN, Levin MJ, Johnson G, Zhang JH, Betts R, Morrison VA, Gelb L, Guatelli JC, Harbecke R, et al. Persistence of the efficacy of Zoster vccine in the Shingles prevention study and the short-term persistence substudy. Clin Infect Dis. 2012;55(10):1320–28. doi: 10.1093/cid/cis638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morrison VA, Johnson GR, Schmader KE, Levin MJ, Zhang JH, Looney DJ, Betts R, Gelb L, Guatelli JC, Harbecke R, et al. Long-term persistence of Zoster vaccine efficacy. Clin Infect Dis. 2015;60(6):900–09. doi: 10.1093/cid/ciu918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schmader KE, Levin MJ, Gnann JW Jr., McNeil SA, Vesikari T, Betts RF, Keay S, Stek JE, Bundick ND, S-C S, et al. Efficacy, safety, and tolerability of Herpes Zoster vaccine in persons aged 50–59 years. Clin Infect Dis. 2012;54(7):922–28. doi: 10.1093/cid/cir970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baxter R, Bartlett J, Fireman B, Marks M, Hansen J, Lewis E, Aukes L, Chen Y, Klein NP, Saddier P. Long-term effectiveness of the live Zoster vaccine in preventing Shingles: a cohort study. Am J Epidemiol. 2018;187(1):161–69. doi: 10.1093/aje/kwx245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Le P, Rothberg MB. Cost-effectiveness of Herpes Zoster vaccine for persons aged 50 years. Ann Intern Med. 2015;163(7):489–97. doi: 10.7326/M15-0093. [DOI] [PubMed] [Google Scholar]
- 55.Brisson M, Pellissier JM, Camden S, Quach C, De Wals P. The potential cost-effectiveness of vaccination against herpes zoster and post-herpetic neuralgia. Hum Vaccin. 2008;4(3):238–45. doi: 10.4161/hv.4.3.5686. [DOI] [PubMed] [Google Scholar]
- 56.Bilcke J, Ogunjimi B, Hulstaert F, Van Damme P, Hens N, Beutels P. Estimating the age-specific duration of herpes zoster vaccine protection: a matter of model choice? Vaccine. 2012;30(17):2795–800. doi: 10.1016/j.vaccine.2011.09.079. [DOI] [PubMed] [Google Scholar]
- 57.Kigozi J, Jowett S, Lewis M, Barton P, Coast J. Valuing productivity costs using the friction-cost approach: estimating friction-period estimates by occupational classifications for the UK. Health Econ. 2017;26(12):1862–68. doi: 10.1002/hec.3513. [DOI] [PubMed] [Google Scholar]
- 58.Pellissier JM, Brisson M, Levin MJ. Evaluation of the cost-effectiveness in the United States of a vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. Vaccine. 2007;25(49):8326–37. doi: 10.1016/j.vaccine.2007.09.066. [DOI] [PubMed] [Google Scholar]
- 59.Edmunds WJ, Brisson M, Rose JD. The epidemiology of herpes zoster and potential cost-effectiveness of vaccination in England and Wales. Vaccine. 2001;19(23–24):3076–90. doi: 10.1016/S0264-410X(01)00044-5. [DOI] [PubMed] [Google Scholar]
- 60.van Hoek AJ, Gay N, Melegaro A, Opstelten W, Edmunds WJ. Estimating the cost-effectiveness of vaccination against herpes zoster in England and Wales. Vaccine. 2009;27(9):1454–67. doi: 10.1016/j.vaccine.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 61.Drolet M, Brisson M, Schmader KE, Levin MJ, Johnson R, Oxman MN, Patrick D, Blanchette C, Mansi JA. The impact of herpes zoster and postherpetic neuralgia on health-related quality of life: a prospective study. Can Med Assoc J. 2010;182(16):1731–36. doi: 10.1503/cmaj.091711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chiyaka E, Nghiem V, Zhang L, Deshpande A, Mullen P, Le P. Cost-Effectiveness of Herpes Zoster vaccination: a systematic review. Pharmacoeconomics. 2019;37(2):169–200. doi: 10.1007/s40273-018-0735-1. [DOI] [PubMed] [Google Scholar]
- 63.Kawai K, Preaud E, Baron-Papillon F, Largeron N, Acosta C. Cost-effectiveness of vaccination against herpes zoster and postherpetic neuralgia: a critical review. Vaccine. 2014;32(15):1645–53. doi: 10.1016/j.vaccine.2014.01.058. [DOI] [PubMed] [Google Scholar]
- 64.Udayachalerm S, Renouard M, Anothaisintawee T, Thakkinstian A, Veettil S, Chaiyakunapruk N. Incremental net monetary benefit of herpes zoster vaccination: a systematic review and meta-analysis of cost-effectiveness evidence. J Med Econ. 2022;25(1):26–37. doi: 10.1080/13696998.2021.2008195. [DOI] [PubMed] [Google Scholar]
- 65.Tseng HF, Harpaz R, Luo Y, Hales CM, Sy LS, Tartof SY, Bialek S, Hechter RC, Jacobsen SJ. Declining effectiveness of Herpes Zoster vaccine in adults aged ≥60 years. J Infect Dis. 2016;213(12):1872–75. doi: 10.1093/infdis/jiw047. [DOI] [PubMed] [Google Scholar]
- 66.van Wijck AJM, Aerssens YR. Pain, Itch, quality of life, and costs after Herpes Zoster. Pain Practice. 2017;17(6):738–46. doi: 10.1111/papr.12518. [DOI] [PubMed] [Google Scholar]
- 67.Bilcke J, Ogunjimi B, Marais C, de Smet F, Callens M, Callaert K, van Kerschaver E, Ramet J, van Damme P, Beutels P. The health and economic burden of chickenpox and herpes zoster in Belgium. Epidemiol Infect. 2012;140(11):2096–109. doi: 10.1017/S0950268811002640. [DOI] [PubMed] [Google Scholar]
- 68.Szucs TD, Pfeil AM. A systematic review of the cost effectiveness of Herpes Zoster vaccination. PharmacoEconomics. 2013;31(2):125–36. doi: 10.1007/s40273-012-0020-7. [DOI] [PubMed] [Google Scholar]
- 69.A long-term follow-up study (ZOE-LTFU) of two studies 110390 (ZOSTER-006) and 113077 (ZOSTER-022) to assess the efficacy, safety, and immunogenicity persistence of GSK biologicals’ Herpes Zoster subunit (HZ/su) vaccine and assessment of 1 or 2 additional doses in two subgroups of older adults. 2016. [accessed 2022 Oct 10]. https://clinicaltrials.gov/ct2/show/record/NCT02723773?view=record.
- 70.Curran D, Oostvogels L, Heineman T, Matthews S, McElhaney J, McNeil S, Diez-Domingo J, Lal H, Andrews C, Athan E, et al. Quality of life impact of an adjuvanted recombinant Zoster vaccine in adults aged 50 years and older. J Gerontol: Ser A. 2019;74:(8):1231–38. doi: 10.1093/gerona/gly150. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


