Abstract
Background.
School sealant programs (SSPs) increase sealant prevalence among children lacking access to oral health care. SSPs, however, are substantially underused. From 2013 through 2018, the Centers for Disease Control and Prevention funded 18 states for SSP activities in high-need schools (≥50% free and reduced-price meal program participation). From 2019 through 2020, the authors assessed SSPs’ impact in reducing caries and how states expanded SSPs. The authors also discuss potential barriers to expansion.
Methods.
For Aim 1, the authors used a published methodology and SSP baseline screening and 1-year retention data to estimate averted caries over 9 years attributable to SSPs. For Aim 2, the authors used state responses to an online survey, phone interviews, and annual administrative reports.
Results.
Using data for 62,750 children attending 18.6% of high-need schools in 16 states, the authors estimated that 7.5% of sound, unsealed molars would develop caries annually without sealants and placing 4 sealants would prevent caries in 1 molar. Fourteen states reported SSP expansion in high-need schools. The 2 most frequently reported barriers to SSP expansion were levels of funding and policies requiring dentists to be present at assessment or sealant placement.
Conclusions.
The authors found that SSPs typically served children at elevated caries risk and reduced caries. In addition, the authors identified funding levels and policies governing supervision of dental hygienists as possible barriers to SSP expansion.
Practical Implications.
Increasing SSP prevalence could reduce caries. Further research on potential barriers to SSP implementation identified in this study could provide critical information for long-term SSP sustainability.
Keywords: Caries, fissure sealants, school program, school health
By age 19 years, 65% of adolescents living in poverty have experienced caries.1 If left untreated, caries can lead to pain, infection, and problems in eating and socialization.2 Studies indicate that children with dental treatment needs miss more school and receive lower grades than children with no needs.3–5 Dental sealants prevent caries in pits and fissures, in which approximately 90% of caries in the permanent teeth occur.6,7 A 2016 systematic review of sealant effectiveness found that sealants compared with no sealants reduced the odds of developing caries by 76% up to 3 years after placement.8 Dental sealants are underused, especially among youth from low-income households; only 37.8% of these youth aged 6 through 11 years and 42.7% aged 12 through 19 years have dental sealants.1
School sealant programs (SSPs) increase sealant uptake among youth attending high-need schools (that is, schools in which ≥50% of the students participate in a free or reduced-price meal program).9 There are 2 types of SSPs: school-linked sealant programs (SLSPs), in which dental personnel screen children at the school and then refer them to participating dental offices for sealant placement, and school-based sealant programs (SBSPs) that typically have teams of dental care professionals (dentists, dental hygienists, or both) assess students’ oral health status and place sealants if indicated using portable equipment at the school.9 The Community Preventive Services Task Force recommends SBSPs, noting there is strong evidence to support the effectiveness of programs applying sealants within school settings and evidence that these programs increase the number of children who receive sealants at school.9
SSPs, however, are substantially underused.10 A Pew Charitable Trusts study conducted in 2014 found that only 11 states had SBSPs in more than 50% of high-need schools.10 One barrier to implementing SSPs is state dental policies requiring dentists’ supervision of dental hygienists during screening, sealant placement, or both.10,11 One study found these policies can increase SSP costs from 18% through 29%, depending on the size of the SSP.11 State Medicaid billing and reimbursement policies can also affect the reach of sealant programs.10
From 2013 through 2018, the Centers for Disease Control and Prevention (CDC) funded 21 states to enhance state oral health program infrastructure.1 Eighteen of these states received additional CDC funding to implement and expand SSPs serving low-income or rural schools.1 Uses of CDC funding included purchasing portable equipment and hiring a state sealant coordinator. These states also were asked to collect data regarding the percentage of high-need schools with SSPs and the impact of select SSPs on caries. Seventeen states (Colorado, Connecticut, Georgia, Iowa, Kansas, Louisiana, Maryland, Michigan, Minnesota, Mississippi, New York, North Dakota, Rhode Island, South Carolina, Virginia, West Virginia, Wisconsin) primarily worked with SBSPs, and 1 state (Vermont) worked with SLSPs. Our study had 2 aims: (1) estimate number of averted caries in permanent molars (averted caries) attributable to select SBSPs, and (2) examine how states expanded their SSPs. We also discuss potential barriers to expansion.
METHODS
For Aim 1, we used data from a nonresearch evaluation of a public health program, and thus this part of the study was not subject to institutional review board approval. For Aim 2, we obtained Office of Management and Budget approval for an online survey and telephone interviews. We have blinded state names for Aim 1 and Aim 2 throughout this article (using the same blinding scheme).
Aim 1: SBSP impact
For Aim 1, we only included data from SBSPs because of difficulty in obtaining data from dental offices participating in SLSPs. Among the 17 SBSP states, 16 collected data from local SBSPs with which they had a relationship (for example, funded or operated) for at least 1 school year from 2013 through 2018. For states that provided data for more than 1 school year, we included data from the earliest year. To explore the representativeness of our data, we calculated for each state the percentage of high-need schools for which we had SBSP data. In addition to defining need by free and reduced-price meal program participation, states also may have included schools located in rural areas per the criteria used by the National Center for Education Statistics.1,13
Data Collection and Analyses
For each state, we used a previously published Markov model14 to estimate the number of molar caries (MC) that would have occurred without and with SBSP sealants over 9 years. Averted MC attributable to SBSP sealants equals the difference in the Markov model estimates of MC without and with SBSP sealants. To obtain a measure that was comparable across states, for each state we divided averted caries over 9 years by the number of SBSP sealants to obtain averted caries per sealant.
A detailed description of the Markov model and its assumptions, which has been previously published, is in the appendix, eFigure, and eTable 1, available online at the end of this article. The model inputs included the number of molars receiving SBSP sealants, annual attack rate (AR) (probability that a sound, unsealed permanent molar developed caries), and 1-year sealant retention. Details on how the AR was estimated for each state, which have been previously published,14 are provided in the Appendix, eFigure, and eTable 1, available online at the end of this article. We estimated annual retention for years 2 through 9 with a published formula that included the SBSP 1-year retention estimate as an input (Appendix, eFigure, eTable 1, available online at the end of this article).15
Model inputs for each state were estimated with their SBSP data. SBSP staff members used a standardized protocol16 to assess caries and sealant status. Deidentified child-level data recorded at baseline screening before sealant placement included the child’s age and number of permanent first molars (1Ms) with untreated caries or restorations and whether the child had at least 1 sealant. After sealant placement, SBSP staff recorded the date and number of permanent 1Ms and second molars sealed. From 9 through 15 months after sealant placement, SBSP staff members in some states returned to the school to record the date and SBSP sealant retention. SBSPs recorded these data in a CDC-provided spreadsheet (Excel; Microsoft). To obtain summary model inputs for each state, these child-level data from all SBSPs within a given state then were analyzed by either the CDC or the state epidemiologist or statistician using an SAS (SAS Institute) program created by the CDC. Summary state estimates were then input into an Excel workbook with embedded formulas from the published methodology14 to estimate the AR and number of averted caries (Appendix, eFigure, and eTable 1, available online at the end of this article). We have made this workbook available on request.
SBSPs in only 5 states collected retention data from 9 through 15 months after placement, and of these, only 3 had data for more than 3% of children receiving SBSP sealants (eTable 2, available online at the end of this article). We used data from these 5 states (weighted on the basis of the number of children assessed for retention) to estimate the weighted first-year retention rate and assigned this rate to the 13 states with no or limited data (that is, SBSPs checked less than 3% of students receiving their sealants). Because of the paucity of retention data, we used a 2-way probabilistic sensitivity analysis to examine how estimated averted MC responded to changes in 1-year retention for ARs ranging from 2% through 16%. We allowed 1-year retention to vary from 60% through 90%, which is consistent with estimates from the literature.7,8 Finally, we calculated the percentage change in model-estimated averted caries attributable to a 16.7% increase (moving from 60% to 70% retention), a 14.3% increase (moving from 70% to 80% retention), and a 12.5% increase (moving from 80% to 90% retention) in retention for each AR value.
Aim 2: SSP expansion and barriers
Study Population
For this qualitative analysis, the sampling frame included all 18 states funded for SSPs.
Data Collection and Analysis
Two staff members from each state oral health program were invited to participate in an online survey at the end of the funding period, December 2018 through January 2019. On the basis of literature suggesting that changes in policies influenced SSP expansion, we also included questions to explore policy changes (that is, dental practice acts and Medicaid billing for dental hygienists) that may have affected SSP implementation (Table 1).10
Table 1.
Overview of data for Aim 2.
| EVALUATION DATA SOURCE | QUESTIONS AND TOPICS DISCUSSED |
|---|---|
| Online Survey | Were there any other changes in your state that affected the implementation of school-based or school-linked sealant programs during the 5-year funding period (that is, August 2013-August 2018)? |
| Telephone Interviews | What would make it easier for you to reach more eligible schools with dental sealant programs in your state? Probe: How can the reach of school-based or school-linked sealant program be expanded in the state? Are there any policies that have affected your work with school-based sealant programs in your state? |
| Administrative Data | Data were extracted from 2014 through 2018 state-submitted administrative reports that included a section on challenges to and successes in implementing school-based or school-linked sealant programs. |
Seven of the state oral health program directors who participated in the online survey were invited to participate in a follow-up telephone interview. These states were selected using purposive sampling17 to obtain a group of state oral health programs at varying stages of implementing oral health activities. Telephone interviews primarily assessed factors and policies perceived to be important to SSP expansion (Table 1). Interviews were recorded and ranged from 30 through 60 minutes.
We also reviewed annual administrative reports submitted by each state. Administrative reports had an open-ended section to capture successes and challenges in implementing oral health activities, including SSP activities. We extracted and coded data from these reports from 2014 through 2018 to generate common themes. We conducted a thematic analysis18 for the qualitative data from the telephone interviews and administrative reports. All data were analyzed via using Excel.
RESULTS
Aim 1
Sixteen states provided data for 67,250 students attending 2,601 schools (18.2% of all high-need schools in participating states). Among children receiving sealants, 56% were ages 6 through 9 years, 35% ages 10 through 14 years, and 9% another age. These children received a total of 205,758 sealants from SBSPs. The AR was estimated with data from 43,570 students who had no sealants before SBSP (Table 2). Participating SBSPs represented less than 10% of high-need schools in 5 states, 10% through 25% in 3 states, 25% through 50% in 7 states, and more than 50% in 1 state (Table 2). One-year sealant retention from 5 states ranged from 63% through 96% (Table 2). The weighted retention rate used to estimate averted caries for the 13 states that did not have retention data for more than 3% of children having received sealants was 73% (eTable 2, available online at the end of this article).
Table 2.
Number of schools, students, and teeth and 1-year sealant retention used in calculations for Aim 1.
| STATE | HIGH-NEED SCHOOLS, % | YOUTH RECEIVING SEALANTS, NO. | MOLARS SEALED, NO. | YOUTH USED IN ATTACK RATE CALCULATIONS, NO. | 1-YEAR RETENTION RATE, % | YOUTH REPRESENTED, % |
|---|---|---|---|---|---|---|
| A | 9.6 | 4,080 | 12,732 | 2,833 | 93.7 | 0.5 |
| B | 31.6 | 2,304 | 7,613 | 2,404 | 79.2 | 3.4 |
| C | 39.0 | 4,892 | 13,499 | 2,459 | NR* | |
| D | 28.1 | 5,650 | 18,418 | 3,223 | NR | |
| E | 10.8 | 2,801 | 8,499 | 1,402 | NR | |
| F | 28.0 | 4,119 | 13,023 | 2,186 | NR | |
| G | 5.4 | 740 | 2,511 | 784 | NR | |
| H | 69.0 | 23,826 | 70,466 | 13,396 | 96.0 | 0.5 |
| J | 2.0 | 1,275 | 3,741 | 340 | NR | |
| K | 21.1 | 1,099 | 3,372 | 246 | NR | |
| L | 4.3 | 1,933 | 1,780 | 1,219 | NR | |
| M | 43.2 | 9,573 | 35,152 | 8,559 | 63.0 | 21.3 |
| N | 32.8 | 919 | 2,890 | 1,279 | 89.6 | 100 |
| O | 27.5 | 1,604 | 4,349 | 1,470 | NR | |
| P | 3.1 | 2,121 | 6,710 | 1,525 | NR | |
| Q | 15.9 | 314 | 1,003 | 245 | NR | |
| TOTAL | Not applicable | 67,250 | 205,758 | 43,570 | Not applicable |
NR: Not reported.
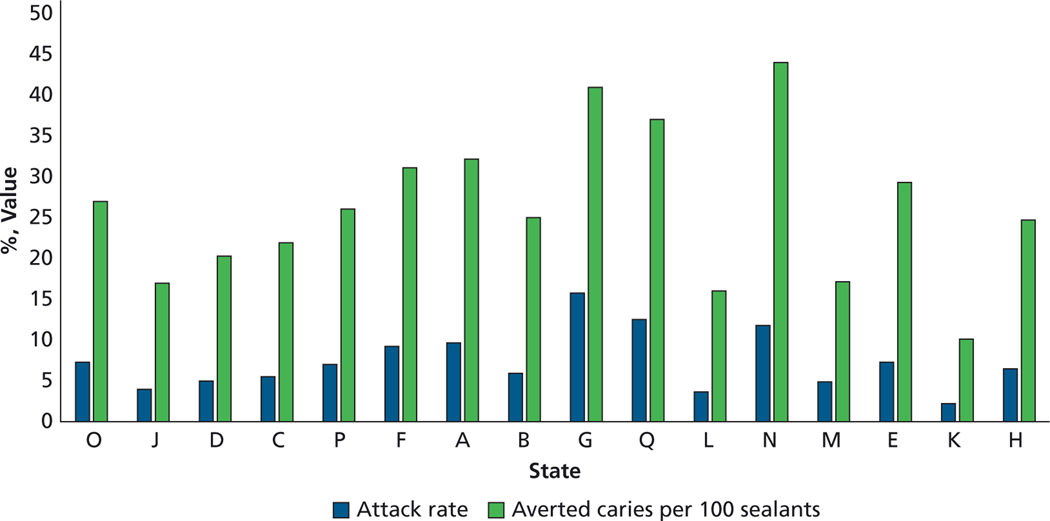
One-year caries ARs, expressed as a percentage, ranged from 2.2% to 15.8%, with a median value of 6.8% (Figure 1). The AR averaged across states was 7.5% (data not shown). Overall, these select SBSPs in funded states per year of operation prevented 49,529 caries over 9 years. The number of caries averted over 9 years from placing 1 sealant ranged from 0.10 to 0.44, with a median value of 0.26. This suggests that for every 100 sealants placed by an SBSP, approximately 26 caries would be prevented over 9 years (Figure 1).
Figure 1.
Annual first molar attack rate and averted caries per 100 sealants for 16 states funded by the Centers for Disease Control and Prevention.
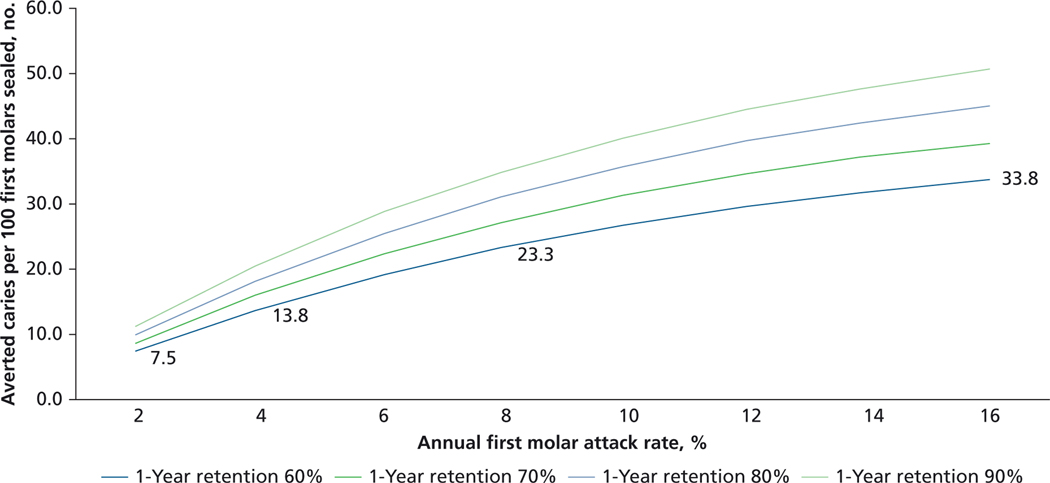
Averted caries increased as both the annual AR and 1-year retention increased (Figure 2). Regardless of the AR, the increase in averted caries was proportional to the increase in retention. For example, if the retention rate increased by 16.7% (moving from 60%−70% curve) averted caries would increase by 16.7% as well (7.5%−8.8%). Averted caries was less responsive to increases in the AR. Regardless of retention rate, increasing the AR from 2% to 4% (100% increase) resulted in an 83% increase in averted caries (for example, 7.5–13.8 averted caries for retention rate of 60%). The responsiveness of averted caries to changes in the AR decreased as the AR increased. For example, moving from 4% to 8% (100% increase) resulted in a 69% increase in averted caries, and moving from 8% to 16% resulted in a 45% increase.
Figure 2.
Sensitivity analysis of effect of annual first molar attack rate on estimated averted caries for 1-year retention rates ranging from 60% through 90%.
Aim 2
Table 3 provides a summary of the evaluation data sources and key themes discussed in this section. At least 1 of the 2 invited representatives from each state completed the online survey. Of the 36 invited state representatives, 31 (86%) participated.
Table 3.
Evaluation questions and data sources.
| EVALUATION QUESTION AND THEME | RESPONSES | DATA SOURCES |
||
|---|---|---|---|---|
| Online Survey (18 States) | Telephone Interviews (7 States) | Administrative Data (18 States) | ||
| Expansion of Dental Sealant Programs in High-Need Schools | Fourteen states (77.7%) reported an increase in school sealant program coverage in terms of more high-need schools or students served over the 5-year funding period. | NA* | Interviewees from states O and F reported using mobile units to reach more schools. | Thirteen states (A, B, C, D, E, F, G, H, I, L, N, P, Q) discussed their successes in expanding their school-based sealant programs. |
| Increased Number of Students Receiving Dental Sealants | Fourteen states (77.7%) reported an increase in school sealant program coverage in terms of more high-need schools or students served over the 5-year funding period. | State E discussed an increase in the number of students receiving sealants. | NA | Three states (G, H, I) highlighted success in increasing the number of students receiving dental sealants within high-need schools. |
| Obtaining Supplemental Funding to Support Expansion | In addition to Centers for Disease Control and Prevention funding, 8 states reported receiving funding from other federal, state, or private entities. | NA | NA | Eight states (A, D, E, F, H, J, P, R) successfully obtained funding from more than 1 source to support expansion of school-based dental sealant programs targeting high-need schools. |
| Factors for Expanding Reach of School Sealant Programs | ||||
| Policy changes reducing dentists' supervision | ● Ten states cited existing state policies as barriers to expanding school sealant programs. Elevated operating costs due to policies requiring dentists' supervision of dental hygienists providing sealants in school settings were a barrier to implementing and expanding school sealant programs. Another barrier was a state policy that did not allow dental hygienists to bill Medicaid for sealants delivered in school sealant programs. ● Three states reported policy changes allowing school sealant programs to substitute less costly for more costly labor. Two of these states that already allowed dental hygienists to provide sealants without a dentist’s supervision in certain settings expanded settings to include schools. ● One state reported removing the requirement for dentists’ supervision of dental hygienists in school settings during assessment of students’ need for sealants. |
Ten states (B, C, D, F, H, I, J, L, M, Q) discussed the role of a state policy allowing dental hygienists to provide school-based services without the supervision of a dentist in facilitating the implementation and expansion of school-based sealant program. | NA | NA |
| Increased efficiency | States reported efforts to decrease their labor costs. One state collaborated with dental hygiene education programs, engaging dental hygiene students to assist in sealant placement. | NA | NA | Two states (A, E) reported either hiring dental hygiene teams to place sealants in remote geographic areas or dental hygiene students to assist in sealant placement. |
| Strengthen school sealant program data collection and reporting | Strengthening school sealant program data collection and reporting allowed states to better monitor local programs and prioritize schools to be served by school sealant programs. One state noted that to reach more students at current funding levels they were planning on diverting resources away from schools with lower student participation rates to those with higher rates. | NA | NA | Six states (B, H, J, M, N, O) reported working with local programs to strengthen school sealant program data collection and reporting. |
| Challenges | ||||
| Medicaid payment levels or provider and location requirements for dental hygienist services | Two states noted that Medicaid reimbursements for sealant placement were “…not adequate to cover the cost of transportation, supplies and other logistics.” | Two states (B, C) described Medicaid payment levels as a barrier to school sealant program expansion. | NA | NA |
| Funding | Six states (33%) discussed funding as a key challenge to expanding school sealant programs. Several states indicated that “…it costs a lot for schools and dentists to implement sealant programs” and that there are not enough resources and dedicated staff to launch broader statewide efforts. Some states noted that “current funding levels not only impede expansion efforts but threaten the sustainability of existing programs.” One state noted, “Without additional funds, we would have to reallocate. We plan to look at programs that are not as productive as others….” | State A's survey response also highlighted this challenge. In addition, open-ended survey respondents from states C and I noted that limited funding was a major barrier for their sealant programs. | Interviewees from states A, B, and F noted that additional funding is required to reach more eligible schools with dental sealant programs. | Three states (A, B, R) indicated in their annual program reports that funding remains a key challenge to implementing their school sealant programs. |
| Working with mobile providers | Survey respondents from 4 states discussed challenges in working with mobile providers in their states. Mobile programs often did not share data with the state oral health program. As a result, larger mobile programs sometimes served the same schools as state-sponsored school sealant programs. | States A, G, H, and J discussed challenges in working with mobile providers in their states. | NA | NA |
NA: Not applicable. The data source did not include this question.
Main Themes
Expansion of SBSPs
In addition to CDC funding, 8 states reported receiving funding from other federal, state, or private entities. Fourteen states (77.7%) reported an increase in SSP coverage in terms of more high-need schools or students served over the 5-year funding period. Successful activities contributing to the increase in school participation included building and leveraging partnerships with schools and dental and medical providers and providing informational materials about dental sealants to school superintendents, principals, clinicians, and teachers (data not shown). Four states reported increasing student participation rates at served schools by means of providing incentives to teachers to increase the number of consent forms returned (data not shown).
Facilitators to expansion
SSP expansion was accomplished via obtaining and using more resources (that is, equipment and labor) and using resources more efficiently (data not shown). Two states reported purchasing additional portable sealant stations, and 2 reported an increase in mobile dental programs within their state. One of these states reported that community health centers with mobile dental programs or SBSPs had the highest number of children receiving dental sealants. Another of these states noted that school staff members and parents appreciated the mobile unit because many parents found it difficult to take time off from work to take their children to a dental office.
States also reported efforts to decrease their labor costs. One state reported collaborating with dental hygiene education programs, engaging dental hygiene students to assist in sealant placement. Two states reported either hiring dental hygiene teams to place sealants in remote geographic areas or dental hygiene students to assist in sealant placement. Three states also reported policy changes that allowed SSPs to substitute less costly for more costly labor. Two of these states that already allowed dental hygienists to provide sealants without a dentist’s supervision in certain settings expanded settings to include schools. One state reported removing the requirement for dentists’ supervision of dental hygienists in school settings during assessment of students’ need for sealants.
Six states reported that they worked with local programs to strengthen SSP data collection and reporting. This information allowed states to better monitor local programs and prioritize schools to be served by SSPs. One state, for example, noted that to reach more students at current funding levels, they were planning on diverting resources away from schools with lower student participation rates to those with higher rates.
Barriers to expansion
One-third of the states (6 of 18) discussed funding as a key challenge to expanding SSPs. Several states indicated that current funding levels would not cover the cost of launching broader statewide efforts. As 1 state respondent put it, “...it costs a lot for schools and dentists to implement sealant programs,” and current funding did not support statewide expansion. Some states reported that existing funding does not cover the cost of current programs. One state respondent noted, “Without additional funds, we would have to reallocate. We plan to look at programs that are not as productive as others....” In addition, 2 states identified Medicaid reimbursement rates for sealant placement as a barrier to SSPs; 1 respondent explained that payment levels are “...not adequate to cover the cost of transportation, supplies, and other logistics.”
Survey respondents from 4 states discussed challenges in working with mobile providers in their states. Mobile programs often did not share data with the state oral health program. As a result, larger mobile programs sometimes served the same schools as state-sponsored SSPs.
Some states also cited existing state policies as barriers to expanding SSPs (Table 3). Ten states discussed how increased operating costs due to policies requiring dentists’ supervision of dental hygienists providing sealants in school settings were a barrier to implementing and expanding SSPs.
CONCLUSIONS
To our knowledge, this is the first study to use SBSP data from several states to examine caries risk among children served by SSPs and SSP impact. Data representing 62,750 children attending 18.6% of high-need schools in 16 states indicate that SBSPs served children at a relatively high risk of developing caries. The estimated AR in our study, 7.5%, is similar to that for low-income children with no sealants nationally, 7.3%.19 One study estimated that SBSPs serving children at similar risk (AR, 7.8%) were cost-saving from a societal perspective over 4 years.19 We also found that sealing 4 1Ms would prevent 1 MC over 9 years. If we ignore the time value of money, this would suggest that from a provider perspective (for example, Medicaid) SBSPs would save money if the cost of restoring 1 MC were at least 4 times that of placing the sealant.
Many low-income children are not receiving topical fluoride or dental sealants during dental visits.20 An analysis of national data from 2011 through 2014 estimated that approximately 6.5 million low-income children aged 6 through 11 years were not receiving the preventive benefits of dental sealants and that providing sealants to these children could prevent 3.4 million MC over 4 years.21 SSPs are an effective strategy to reduce income disparities in sealant prevalence.9
We found that states developed partnerships and used multisector approaches to expand SSPs, in addition to CDC funding. A key factor for program sustainability is that the program’s revenue (for example, Medicaid reimbursements) covers its cost.22 States used CDC funding to support labor and equipment costs for SSPs and to build partnerships to have access to lower-cost labor. As labor accounts for approximately 85% of SSP costs,23 implementing policies to allow dental hygienists to assess need for and place sealants can lower costs substantially—one study found it reduced SSP costs by18% through 29% depending on the program size.11 There is also evidence that sealants delivered by SSPs are of high quality. For example, systematic reviews have found that sealant longevity does not vary by type of dental provider9 and visual-tactile assessment (typically used by SSPs) is sufficient to detect cavitated lesions, the cutoff point at which sealants would no longer be indicated.24
Some states highlighted the need for adequate Medicaid reimbursement for sealants. This is consistent with a study that found increasing Medicaid dental reimbursements was associated with increased acceptance of Medicaid patients by dental offices25 and a survey of state dental directors that found low Medicaid reimbursement rates negatively affected SBSPs.26
Our study has limitations. First, for Aim 1 we used a convenience sample as we did not know the number of SBSPs in most funded states. Thus, our findings could be biased. Second, state administrative data are self-reported, limiting generalizability. Finally, sampling for the telephone interviews was through purposive sampling (nonprobability-based sampling), and thus findings from the interviews may not be generalizable.
PRACTICAL IMPLICATIONS.
Our analysis suggests that SSPs in CDC-funded states served children at elevated risk of developing caries and were effective in preventing caries. In addition, we identified funding levels and Medicaid payments as well as policies governing dentists’ supervision of dental hygienists as possible barriers to SSP expansion.
ABBREVIATION KEY
- 1M
First molar
- AR
Attack rate
- CDC
Centers for Disease Control and Prevention
- DF1M
Decayed and filled first molar
- MC
Molar caries
- NA
Not applicable
- NR
Not reported
- SBSP
School-based sealant program
- SLSP
School-linked sealant program
- SSP
School sealant program
Appendix. Estimating averted molar caries (methodology originally published in the Journal of Public Health Dentistrye1).
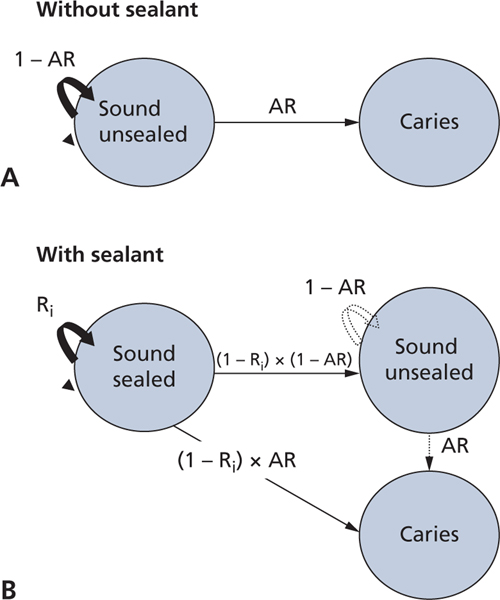
MODEL
We used a Markov model with 1-year cycle times to simulate new caries in permanent molars with and without school-based sealant program (SBSP) sealants. The states and transition probabilities in the model are shown in the eFigure. We used a 9-year analytic horizon (that is, ran the model for 9 1-year cycles) as this is the longest period for a study included in a Cochrane review of sealant effectiveness.e2
Without SBSP sealants (eFigure, A), molars are initially in the sound state. At the end of each cycle a molar could remain in the sound state with probability 1 attack rate (AR) or transition to the caries state with probability AR. For the model with SBSP sealants (eFigure, B), molars are initially in the sound, sealed state and at the end of the first cycle could remain in that state with probability R1 or transition to either the sound, unsealed state with probability (1 – R1) × (1 – AR) or to the caries state with probability (1 – R1) × AR. In cycles 2 through 9, molars in the sound, sealed state could remain in that state with probability Ri or transition to the sound unsealed state with probability (1 – AR) × (1 – Ri in which i represents the cycle) or to the caries state with probability AR × (1 – Ri); molars in the sound unsealed state could remain in that state with probability (1 – AR) or transition to the caries state with probability AR. Molars could not transition out of the caries state.
We made the following assumptions for the model:
SBSPs are the only source of sealants.
SBSPs place resin-based sealant, which are not replaced. In 2014, 15 of 16 states reported that SBSPs in their state used resin-based sealants (Susan Griffin, PhD, personal oral communication, July 14, 2019).
A retained resin-based sealant is 100% effective,e3 that is, only unsealed molars can develop caries.
The annual probability of a sound unsealed molar developing caries (AR) is constant.e4,e5
The AR and retention rates for permanent second molars were the same as that for permanent first molars. As most permanent molars sealed were first molars (84%), we calculated the AR and 1-year retention from data for permanent first molars and applied these values to permanent first and second molars.
The monthly sealant loss rate after 1 year decreased over time and took on the functional form of 0.01 × e(−0.012×M) in which M equals the number of months since placement and e is the base of the natural logarithm, a constant of approximately 2.71828.e6 The annual loss rate for cycles 2 through 9 (1 – Ri), where i is the number of months and Π is the cumulative product, would equal
For example, if program data indicated that the 1-year loss rate (1 – R1) was 10%, 18% of sealants would be lost at 2 years (average annual loss rate equals 9%, calculated by means of dividing cumulative loss rate by number of years); 34% of sealants would be lost at 5 years (average annual loss rate equals 7%); and 45% of sealants would be lost at 9 years (average annual loss rate equals 5%). The Markov cycle rather than the age of the sealant would determine the sealant loss rate. 7. The probability that a molar that loses its sealant develops caries (AR) is the same as that for a molar that never received a sealant.e7
The cavities averted owing to SBSPs in each cycle equaled the number of new molar caries expected that year in the absence of SBSP sealants less the number of new cavities expected that year in the presence of SBSP sealants.
ESTIMATING THE PROBABILITY THAT AN UNSEALED MOLAR DEVELOPS CARIES (AR)
The Markov model in the eFigure, A and B, requires 3 pieces of SBSP information: the number of molars receiving sealants, 1-year retention rate, and the annual molar AR. The AR was calculated from SBSP data (for permanent first molars [1Ms] for children aged 7–13 years with no sealants at baseline screening before sealant placement). These data included the child’s age, whether the child had any sealed 1Ms, and the number of decayed and filled 1Ms. Because 1Ms typically erupt at age 6 yearse8 and because we assumed a constant 1M AR over time (Assumption 4), the annual AR for children of the same age can be calculated with the following formula:
in which
1M ARAge represents the annual 1M AR among children without sealants at a specified age
Age represents the children’s age in years (so Age – 6 represents the time a 1M has been in the mouth). The formula is applied separately for each age represented in the program patient population.
DF1M represents the number of 1Ms with caries (carious or filled) among children with no sealants at screening before sealant placement
#screened represents the number of children with no sealants on their permanent 1M at screening (multiplying this value by 4 represents the number of 1Ms initially at risk of developing caries)
The part of the formula in parentheses represents the cumulative probability a never-sealed, sound 1M remains sound during the time it has been in the mouth. To obtain the annual probability that a 1M remains sound, we raised the cumulative probability to 1 divided by the time the 1M has been in the mouth. Subtracting this annual probability from 1 yields the annual 1M AR. The AR used in the Markov model was the weighted average across all age groups (7–8, 8–9, 9–10, 10–11, 11–12, 12–13, 13–14 years). eTable 1 provides an example of AR calculations for 1 state. For each age group, the number of children (column C) and decayed and filled first molars (DF1Ms) (column D) were used to estimate the cumulative AR. For example, for children aged 8 years, the 1Ms would have been at risk for caries for 2 years on average. The 2-year AR in column E (12.32%) equaled DF1M in column D (1,803) divided by the total number of 1Ms (4 × 3,659 from column C). The annual AR calculated with formula would equal 1 – (1 – 12.83%)^(1/2) or 6.36% in column F. The AR used in the Markov model for this state would equal the sum of the ARs weighted by age, 6.54%. Data used for state AR calculations across all states indicated children aged 7 through 8 years had the highest weight (35% of sample used to estimate AR) followed by those aged 8 through 9 (25%), 9 through 10 (12%), 10 through 11 (10%), 11 through 12 (8%), 12 through 13 (6%), and 13 through 14 (4%) years.
WORKBOOK TO ESTIMATE ATTACK RATE AND AVERTED CARIES FOR EACH STATE
Formulas to estimate the AR and the number of averted caries (caries with and without the SBSP) for the model in the eFigure were embedded into an Excel (Microsoft) workbook. The workbook was used by the Centers for Disease Control and Prevention (CDC) or provided to the state epidemiologist or statistician. Included in the workbook were 2 spreadsheets, 1 that estimated the AR and was autopopulated once summary values for number of children with no sealants at baseline screening by age and each age group’s total DF1M (eTable 1) were provided, and another that estimated averted caries and was autopopulated once summary values for the AR and 1-year retention rate were provided. We have made this workbook available on request.
OBTAINING SUMMARY VALUES USED IN THE WORKBOOK
Participating SBSPs recorded deidentified child-level data on caries and sealant status before sealant placement using the Basic Screening Survey criteria.e9 Directly after sealant placement, the SBSP recorded the number of molar sealants it placed and, from 9 through 15 months after placement, the number of SBSP sealants retained. Combined data for all SBSPs within a state were analyzed using an SAS program created by the CDC. States varied by whether the analysis of the data was conducted by the CDC or their own epidemiologist or statistician.
eFigure.
Markov model of caries progression without sealant (A) and with sealant (B). Solid black lines indicate transitions that occur in all cycles. Dotted gray lines indicate transitions that occur in cycles 2 through 9. AR: Attack rate; annual permanent first molar attack rate. Ri: Sealant retention rate in cycles 1 through 9.
eTable 1.
Example of permanent first molar attack rate calculations for a state.
| REPORTED AGE, Y (A) | TIME FIRST MOLAR IN MOUTH ON AVERAGE, Y (B) | CHILDREN WITH NO SEALANTS AND VALID DATA FOR DF1M* AT BASELINE SCREENING, NO. (C) | SUM OF DF1M AMONG CHILDREN IN COLUMN C (D) | ATTACK RATE FOR YEARS ELAPSED, % (E) | ATTACK RATE FOR 1 YEAR, % (F) | WEIGHTED BY PROPORTION OF OBSERVATIONS IN AGE GROUP, % (G) |
|---|---|---|---|---|---|---|
| 7 | 1 | 5,287 | 1,390 | 6.57 | 6.57 | 2.59 |
| 8 | 2 | 3,659 | 1,803 | 12.32 | 6.36 | 1.74 |
| 9 | 3 | 1,280 | 1,074 | 20.98 | 7.55 | 0.72 |
| 10 | 4 | 1,262 | 1,309 | 25.93 | 7.23 | 0.68 |
| 11 | 5 | 1,039 | 1,105 | 26.59 | 5.99 | 0.46 |
| 12 | 6 | 593 | 714 | 30.10 | 5.79 | 0.26 |
| 13 | 7 | 276 | 276 | 25.00 | 4.03 | 0.08 |
| Total | NA† | 13,396 | NA | NA | NA | 6.54 |
DF1M: Decayed and filled permanent first molar.
NA: Not applicable.
eTable 2.
Weighted 1-year retention rate calculations.
| STATE | CHECKED FOR RETENTION WITHIN 9 THROUGH 15 MONTHS AFTER SEALANT PLACEMENT, NO. | RETENTION RATE, % | WEIGHT,* % | WEIGHTED RETENTION,† % |
|---|---|---|---|---|
| A | 19 | 93.7 | 0.6 | 0.6 |
| B | 78 | 79.2 | 2.5 | 1.9 |
| C | 0 | NR‡ | 0.0 | 0.0 |
| D | 0 | NR | 0.0 | 0.0 |
| E | 0 | NR | 0.0 | 0.0 |
| F | 0 | NR | 0.0 | 0.0 |
| G | 0 | NR | 0.0 | 0.0 |
| H | 126 | 96.0 | 4.0 | 3.8 |
| J | 0 | NR | 0.0 | 0.0 |
| K | 0 | NR | 0.0 | 0.0 |
| L | 0 | NR | 0.0 | 0.0 |
| M | 2,041 | 63.0 | 64.1 | 40.4 |
| N | 919 | 89.6 | 28.9 | 25.9 |
| O | 0 | NR | 0.0 | 0.0 |
| P | 0 | NR | 0.0 | 0.0 |
| Q | 0 | NR | 0.0 | 0.0 |
| Total | 3,183 | Not applicable | 100.0 | 72.6 |
Weight equals number of children checked for retention in state divided by total number of children checked for retention, 3,183.
Weights do not total 100 due to rounding.
Weighted retention for state equals weightstate times 1-year retentionstate.
NR: Not reported.
Footnotes
SUPPLEMENTAL DATA
Supplemental data related to this article can be found at https://doi.org/10.1016/j.adaj.2022.05.011.
Disclosures. None of the authors reported any disclosures.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Dr. Nita Patel, Division of Oral Health, Centers for Disease Control and Prevention, Atlanta, GA..
Dr. Susan O. Griffin, Division of Oral Health, Centers for Disease Control and Prevention, Atlanta, GA..
Ms. Molly Linabarger, Oak Ridge Institute for Science and Education fellow, Division of Oral Health, Centers for Disease Control and Prevention, Atlanta, GA, when the work described in this article was conducted. She is now a project delivery specialist, Deloitte Consulting, Atlanta, GA..
Mr. Srdjan Lesaja, DB Consulting Group, Atlanta, GA..
References
- 1.Lin M, Griffin SO, Gooch BF, et al. ; Centers for Disease Control and Prevention (CDC). Oral Health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States, 1999–2004 to 2011–2016. Centers for Disease Control and Prevention. Accessed September 4, 2020. https://www.cdc.gov/oralhealth/pdfs_and_other_files/Oral-HealthSurveillance-Report-2019-h.pdf [Google Scholar]
- 2.Oral Health in America: A Report of the Surgeon General. US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [Google Scholar]
- 3.Jackson SL, Vann WF Jr., Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children’s school attendance and performance. Am J Public Health. 2011; 101(10):1900–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agaku IT, Olutola BG, Adisa AO, Obadan EM, Vardavas CI. Association between unmet dental needs and school absenteeism because of illness or injury among U.S. school children and adolescents aged 6–17 years, 2011–2012. Prev Med. 2015;72:83–88. [DOI] [PubMed] [Google Scholar]
- 5.Seirawan H, Faust S, Mulligan R. The impact of oral health on the academic performance of disadvantaged children. Am J Public Health. 2012;102(9): 1729–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beauchamp J, Caufield PW, Crall JJ, et al. Evidence-based clinical recommendations for the use of pit-and-fissure sealants: a report of the American Dental Association Council on Scientific Affairs. JADA. 2008;139(3):257–268. [DOI] [PubMed] [Google Scholar]
- 7.Ahovuo-Saloranta A, Forss H, Walsh T, Nordblad A, Mäkelä M, Worthington HV. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst Rev. 2017;7:CD001830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wright JT, Tampi MP, Graham L, et al. Sealants for preventing and arresting pit-and-fissure occlusal caries in primary and permanent molars: a systematic review of randomized controlled trials—a report of the American Dental Association and the American Academy of Pediatric Dentistry. JADA. 2016;147(8):631–645, e18. [DOI] [PubMed] [Google Scholar]
- 9.Community Preventive Services Task Force. Preventing dental caries: school-based dental sealant delivery programs, Task Force findings and rationale statement. The Community Guide. Accessed June 15, 2021. https://www.thecommunityguide.org/sites/default/files/assets/Oral-Health-Caries-School-based-Sealants_0.pdf [Google Scholar]
- 10.States stalled on dental sealant programs: a 50-state report. The Pew Charitable Trusts. Accessed June 15, 2021. https://www.pewtrusts.org/-/media/assets/2015/04/dental_sealantreport_final.pdf [Google Scholar]
- 11.Scherrer CR, Griffin PM, Swann JL. Public health sealant delivery programs: optimal delivery and the cost of practice acts. Med Decis Making. 2007;27(6):762–771. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. State Oral Disease Prevention Program Logic Model (DP13–1307). Centers for Disease Control and Prevention; 2013. [Google Scholar]
- 13.Locale definitions: National Center for Education Statistics (NCES) locale classifications and data. National Center for Education Statistics. Accessed June 13, 2022. https://nces.ed.gov/surveys/annualreports/topical-studies/locale/definitions [Google Scholar]
- 14.Griffin SO, Jones K, Crespin M. Calculating averted caries attributable to school-based sealant programs with a minimal dataset. J Public Health Dent. 74(3):202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Quiñonez RB, Downs SM, Shugars D, Christensen J, Vann WF Jr. Assessing cost-effectiveness of sealant placement in children. J Public Health Dent. 2005;65(2): 82–89. [DOI] [PubMed] [Google Scholar]
- 16.ASTDD basic screening surveys. Association of State & Territorial Dental Directors. Accessed June 15, 2021. https://www.astdd.org/basic-screening-survey-tool
- 17.Oliver P.Purposive sampling. In: Jupp V, ed. The SAGE Dictionary of Social Research Methods. SAGE Research Methods; 2013. Accessed June 15, 2021. https://methods.sagepub.com/reference/the-sage-dictionaryof-social-research-methods [Google Scholar]
- 18.Patton MQ. Qualitative Evaluation and Research Methods. SAGE Publications; 1990. [Google Scholar]
- 19.Griffin S, Naavaal S, Scherrer C, Griffin PM, Harris K, Chattopadhyay S. School-based dental sealant programs prevent cavities and are cost-effective. Health Aff (Millwood). 2016;35(12):2233–2240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Griffin SO, Barker LK, Gooch BF, et al. ; Centers for Disease Control and Prevention (CDC). Use of dental care and preventive services effective in preventing tooth decay among U.S. children and adolescents: Medical Expenditure Panel Survey, United States, 2003–2009 and National Health and Nutrition Examination Survey, United States, 2005–2010. MMWR Suppl. 2014;63(2):54–60. [PubMed] [Google Scholar]
- 21.Griffin SO, Wei L, Gooch BF, Weno K, Espinoza L. Vital signs: dental sealant use and untreated tooth decay among U.S. school-aged children. MMWR Morb Mortal Wkly Rep. 65(41):1141–1145. [DOI] [PubMed] [Google Scholar]
- 22.Nicholson W, Snyder CM. Microeconomic Theory: Basic Principles and Extensions. 12th ed.) Cangage Learning; 2016. [Google Scholar]
- 23.Griffin SO, Naavaal S, Scherrer C, Patel M, Chattopadhyay S; Community Preventive Services Task Force. Evaluation of school-based dental sealant programs: an updated community guide systematic economic review. Am J Prev Med. 2017;52(3):407–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fontana M, Zero DT, Beltrán-Aguilar ED, Gray SK. Techniques for assessing tooth surfaces in school-based sealant programs. JADA. 2010;141(7):854–860. [DOI] [PubMed] [Google Scholar]
- 25.Decker SL. Medicaid payment levels to dentists and access to dental care among children and adolescents. JAMA. 2011;306(2):187–193. [DOI] [PubMed] [Google Scholar]
- 26.When regulations block access to oral health care, children at risk suffer: the school dental sealant program dilemma. The Pew Charitable Trusts. Accessed June 24, 2021. https://www.pewtrusts.org/-/media/assets/2018/08/schooldentalsealant_brief_final.pdf [Google Scholar]
References
- e1.Griffin SO, Jones K, Crespin M. Calculating averted caries attributable to school-based sealant programs with a minimal dataset. J Public Health Dent. 2014;74(3):202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e2.Ahovuo-Saloranta A, Hiiri A, Nordblad A, Makela M, Worthington HV. Pit and fissure sealants for preventing decay in the permanent teeth of children and adolescents. Cochrane Database Syst Rev. 2008;4:CD001830. [DOI] [PubMed] [Google Scholar]
- e3.National Institutes of Health Consensus Development conference statement: dental sealants in the prevention of tooth decay. J Dent Educ. 2008;48(suppl):126–131. [PubMed] [Google Scholar]
- e4.Harkanen T, Larmas MA, Virtanen JI, Arjas E. Applying modern survival analysis methods to longitudinal dental caries studies. J Dent Res. 2002;81(2):144–148. [PubMed] [Google Scholar]
- e5.Changes Virtanen J. and trends in attack distributions and progression of dental caries of three age cohorts in Finland. J Epidemiol Biostat. 2001;6(4):325–329. [DOI] [PubMed] [Google Scholar]
- e6.Quinonez RB, Downs SM, Shugars D, Christensen J, Vann WF. Assessing cost-effectiveness of sealant placement in children. J Public Health Dent. 2005;65(2):82–89. [DOI] [PubMed] [Google Scholar]
- e7.Griffin SO, Gray SK, Malvitz DM, Gooch BF. Caries risk in formerly sealed teeth. JADA. 2009;140(4):415–423. [DOI] [PubMed] [Google Scholar]
- e8.Macek MD, Beltrán-Aguilar ED, Lockwood SA, Malvitz DM. Updated comparison of the caries susceptibility of various morphological types of permanent teeth. J Public Health Dent. 2003;63(3):174–182. [DOI] [PubMed] [Google Scholar]
- e9.ASTDD basic screening surveys. Association of State and Territorial Dental Directors. Accessed June 15, 2019. https://www.astdd.org/basic-screening-survey-tool/