Abstract
Persons with dementia (PWDs) often experience difficulty navigating their environments and performing out-of-home activities. Life-space mobility (LSM) is an effective way of assessing functional levels and independence. We presented a dyadic case study to explore the feasibility of using a global positioning system (GPS) watch to measure LSM of a Latino PWD. Methods included travel diary, LSM questionnaire, and qualitative interviews in addition to the GPS-based mobility characterization. GPS data indicated that the PWD made outdoor trips regularly and was active in social participation, with day-to-day variations. The caregiver and PWD interviews revealed contextual information about mobility patterns captured by other methods. The dyad held positive perceptions toward the GPS watch for tracking health and activities. This study demonstrated a use for wearable location tracking technology to support accurate LSM assessment in dementia that can inform nursing practice, policy, and research to promote wellbeing and delay functional deterioration in PWDs.
Introduction
Although cognitive decline is primary, dementia involves a range of functional deterioration. Among the most common functional changes are life-space mobility (LSM) limitations, such as reduced time spent out of the home, reduced movement areas, and shorter distances traveled (Tung et al., 2014; Wettstein et al., 2015). The LSM is a holistic approach that includes concentric areas of expanding locations (“life spaces”) with increasing requirements for independent mobility (Baker et al., 2003). There is evidence supporting the assessment of LSM as a significant indicator of cognitive decline (Crowe et al., 2008; Sartori et al., 2012).
Most research on persons with dementia (PWDs)’ mobility depends on caregiver reports or performance-based measures, which are assessed infrequently and thus may fail to differentiate varied levels of mobility limitation. Sensor-based measurements to record movement in time and space have been suggested as an effective tool for characterizing mobility in PWDs (Mc Ardle et al., 2018; Tung et al., 2014). Continuous monitoring of functional changes through sensor technologies provide a means for early detection of functional changes related to changes in cognition characteristic of incipient dementia. These devices enable obtaining information on the type, distance, size, and frequency of movements in various locations. This type of monitoring can overcome the limitations of traditional assessment of PWDs’ functional status that usually occurs in brief clinic visits.
Mobility in various community locations among minority populations remains largely unexamined. Given that mobility decisions are shaped within a certain sociocultural and environmental context due to dynamic person-space interactions (Webber et al., 2010), such inquiry is necessary for a focused context where race/ethnicity or culture are considered. Furthermore, despite the growing interest in wearable sensor-based mobility assessment in dementia, to date, we have not found documented attempts to apply this technology to ethnic minority PWDs. Therefore, we used a case study approach to examine the utility and feasibility of using a commercially available global positioning system (GPS) watch to characterize LSM patterns of a Latino PWD and to explore the acceptability of a Latino dyad towards the GPS watch use for mobility monitoring in dementia. In addition to the GPS watch, we adopted a multi-methods mobility assessment approach, where we integrated GPS tracking, travel diaries, self-report mobility questionnaire, and in-depth interviews for complementarity (Creswell & Clark, 2017). This approach enabled a better understanding of contextual factors affecting mobility performance captured by GPS in ethnic minority PWDs.
Methods
Study Design
This is a single case study involving a dementia patient/caregiver dyad (Yin, 2002). This study was approved by the Human Research Protections Office at the University of New Mexico and Institutional Review Board at Virginia Commonwealth University.
The Case Dyad
We recruited one dementia patient/caregiver dyad who lived in a mid-sized city in the United States. The city is mostly suburban and car-dependent with some walkable neighborhoods. The dyad included a 64-year old male living with early-onset Alzheimer’s disease (T.) and his 62-year-old wife (M.; note these initials are all pseudonyms). Both subjects identified as Latino and were active in out-of-home activities. M. was diagnosed with cancer and reported having neuropathy, osteoporosis, and lymphedema. She had been involved in full-time dementia caregiving for six years.
Measurements
After obtaining consent, our team’s research coordinator administered all surveys. M. was used as proxy for assessing T.’s sociodemographic and health status. We used the Montreal Cognitive Assessment (MoCA) to assess the dementia patient’s cognitive function (Cronbach’s alpha=0.80; Nasreddine et al., 2005). T.’s score on the MoCA was 13 at baseline, indicating moderate cognitive impairment. The caregiver responded to the Physical Self-Maintenance Scale items (Cronbach’s alpha=.91; Lawton & Brody, 1969), which measures independence in activities of daily living. T. scored 9, indicating nearly complete independence. We administered the Functional Activities Questionnaire (FAQ) to measure instrumental activities of daily living; the FAQ demonstrated high interrater reliability (r = .97) (Pfeffer et al., 1982). T. scored 30 on the FAQ, meaning complete dependence in instrumental activities of daily living. We used the 15-item Geriatric Depression Scale to evaluate depression (Yesavage et al., 1982). Cramm’s study (2012) reported adequate internal consistency (Cronbach’s alpha=0.78). T’s score was 9, indicating high risk of depression.
Multi-Methods Mobility Assessment
GPS Watch-based Location Tracking.
We used a Garmin Vivoactive HR to assess several LSM parameters. We reviewed available products for their reliability and validity in the measurement of the parameters of interest and the ease of use. The Garmin watch had several built-in sensors, including GPS, accelerometer, and heart rate monitor, and was deemed to be the most appropriate for reporting of its accuracy and usability (Mahendran et al., 2016; Wahl et al., 2017). The GPS device captures an individual’s location in spatial coordinates (longitude, latitude) indexed by time.
Self-Report Mobility Instrument.
The Life-Space Assessment of Mobility (LSA; test-retest reliability=0.96; Baker et al., 2003) was used to measure T’s LSM. The caregiver was a proxy informant to report T.’s mobility. LSA assesses the frequency, extent, and need for equipment or help from another person for an individual’s movement in expanding life spaces for the past four weeks (see Supplemental Material 1). Total scores can range from 0 (restricted to one’s bedroom) to 120 (travelled outside one’s town daily without assistance).
Travel Diary.
We asked the caregiver to fill out a travel diary for the GPS-based monitoring period. The diary was in paper format, on which the caregiver recorded locations T. visited and the activities T. had performed outside the home.
Qualitative Interview.
The research coordinator conducted separate semi-structured interviews with T. and M. using a semi-structured interview guide. The research team developed the guide based on previous sensor technology work with older adults (Chung et al., 2017). The guide (see Supplemental Material 2) included questions about attitudes and concerns about using the GPS watch, their mobility practices and perceived changes in mobility patterns after a dementia diagnosis. The caregiver interview guide included additional questions regarding dementia caregiving activities.
Procedures
Two study visits took place in the dyad’s home in March, 2019. After administering questionnaires, we explained the process to the dyad and provided device use instructions along with the GPS watch, charging cable, and USB wall charger. We instructed T. to wear the device for approximately 12 hours/day while awake and to select “walk” tracking function that has GPS inside and outside the home. We chose a one-week monitoring period to capture T.’s mobility routine on weekdays and weekend days. We asked M. to sync the watch with the Garmin App on T.’s smartphone and charge the device every evening. The exit visit occurred 10 days after the baseline visit, during which qualitative interviews were conducted. We recorded the interviews for transcription and analysis. The participants returned the device and received a gift card for the completion of the study.
GPS Data Processing and Analysis
We downloaded the GPS and heart rate data from the Garmin website in TCX and CSV formats after the exit visit. T. used the GPS watch beyond the 1-week monitoring period until the exit visit took place, generating nine days of GPS data. Nineteen GPS tracks were imported. Pathways from the time the GPS was turned on to the time the GPS was turned off were termed “tracks”. Three tracks had extremely short activity times and were discarded, leaving 16 tracks. We computed some summary statistics for tracks with a focus on medians rather than means to discount the effect of potential outlier values.
We used GPS track plots to describe T.’s locations during the study period. Distance moved and movement speed data were plotted against time to describe his activity patterns over the course of each track. We visualized his LSM via plotting and calculating the convex hull of his GPS track points, which is the smallest convex shape that contains all points in the GPS track. The convex hull allowed us to estimate the space usage level (“compactness”), which represents the size of the area in which an individual spent time in a given GPS track. Tracks were visualized using the mapview package in R (Appelhans et al., 2020) to assess overall data quality.
For each GPS track, we computed several summary statistics. These included the amount of time T. wore the GPS watch, his total distance traveled, median speed, and heart rate during the track. We also calculated the size of the convex hull for each track as well as an indicator of whether T. was at home or not during each track point. We defined being at home as being within 1000 feet of T.’s home coordinates and calculated his average movement speed over all times in a track that he was at home. Finally, we mapped T.’s movements over the entire monitoring period to look for regularity in his movements.
Qualitative Data Analysis
All audio recordings from interviews were transcribed verbatim. When needed, we asked additional questions to elicit further details. The coding team consisted of two Ph.D. qualitative researchers (J.C., & I. P.-A.) with additional expertise in technology-based aging studies. Each researcher independently and manually assigned codes to the segments of transcripts that emerged frequently and dominantly based on research questions or emergent themes. After each of the researchers completed coding, the codes were compared and discussed until consensus was achieved. These codes were then categorized into themes that identified the meaning of mobility and sensor technology acceptance (Boyatzis, 1998).
Credibility and Confirmability of the Qualitative Data.
Trustworthiness and accuracy of the interpretations of the data collected were based on the use of two reviewers and the consensus achieved with coding. The consensus was reached with the addition of two new codes to the original lists, while the thematic groupings remained intact. Confirmability of the data was established upon bringing study findings back to the participants to confirm what they said (Nowell et al., 2017).
Results
GPS-Based Mobility Characteristics of the Person with Dementia
Table 1 shows the track-level monitoring time data, mobility characteristics, and heart rates captured by the GPS watch. The daily device use time was variable, ranging from 1.39 to 8.16 hours (Supplemental Material 3). T. made out-of-home movements every day, lasting from 0.04 to 6.77 hours. He engaged in out-of-home activities throughout the day, from late morning until evening. He moved 0.45 to 38.62 km per track by any transportation means, and the proportion of time spent outside the home based on each GPS track ranged from 0.06 to 1. The size of the convex hull area per each track was 0 to 31 km2 (example Convex Hull in Figure 1). The movement speeds were based on both vehicular and non-vehicle travels. Some of T’s average in-home gait speed per track were faster than 1.0 m/s.
Table 1.
GPS-Based Life-Space Mobility Measures (N = 16 tracks)
| Track | Start Time | End Time | Activity Hours | Total Distance (km) | Median Speed (m/s) | Median HR | Hull Area (km2) | Hours out of home | Prop. time in home | Avg In-Home Gait Speed (m/s) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 3/25/2019 17:56 | 3/25/2019 19:20 | 1.39 | 18.64 | 12.21 | 93 | 25.27 | 1.26 | 0.09 | 1.61 |
| 2 | 3/26/2019 13:45 | 3/26/2019 14:01 | 0.27 | 7.42 | 16.50 | 65 | 4.55 | 0.25 | 0.06 | 0 |
| 3 | 3/26/2019 14:01 | 3/26/2019 20:24 | 6.38 | 14.50 | 0.18 | 78 | 5.69 | 5.57 | 0.13 | 0 |
| 4 | 3/27/2019 10:38 | 3/27/2019 11:11 | 0.55 | 0.45 | 0.17 | 97 | 0.002 | 0.55 | 1.00 | 0 |
| 5 | 3/27/2019 12:30 | 3/27/2019 20:06 | 7.61 | 17.29 | 0.22 | 80 | 5.66 | 6.78 | 0.11 | 0 |
| 6 | 3/28/2019 11:06 | 3/28/2019 13:08 | 2.03 | 2.00 | 0.17 | 107 | 0.002 | 2.03 | 1.00 | 0.01 |
| 7 | 3/28/2019 13:58 | 3/28/2019 17:08 | 3.17 | 24.83 | 7.79 | 94 | 14.33 | 2.56 | 0.19 | 1.4 |
| 8 | 3/28/2019 17:58 | 3/28/2019 20:01 | 2.05 | 34.48 | 12.27 | 109 | 31.36 | 1.93 | 0.06 | 0 |
| 9 | 3/29/2019 10:07 | 3/29/2019 13:22 | 3.25 | 25.26 | 8.33 | 85 | 17.88 | 2.35 | 0.28 | 1.33 |
| 10 | 3/29/2019 18:57 | 3/29/2019 20:06 | 1.14 | 4.58 | 0.12 | 97 | 1.75 | 0.46 | 0.60 | 0 |
| 11 | 3/30/2019 13:12 | 3/30/2019 14:43 | 1.53 | 1.10 | 0.17 | 83 | 0.002 | 1.53 | 1.00 | 0 |
| 12 | 3/30/2019 14:44 | 3/30/2019 15:29 | 0.75 | 0.92 | 0.178 | 89 | 0.01 | 0.04 | 0.95 | 1.44 |
| 13 | 3/30/2019 16:57 | 3/30/2019 17:59 | 1.04 | 15.82 | 14.33 | 76 | 6.43 | 1.03 | 0.01 | 1.31 |
| 14 | 3/31/2019 15:04 | 3/31/2019 18:14 | 3.16 | 9.15 | 0.16 | 91 | 6.18 | 2.48 | 0.22 | 0.01 |
| 15 | 4/1/2019 14:10 | 4/1/2019 20:00 | 5.83 | 19.79 | 0.12 | 75 | 5.77 | 5.17 | 0.11 | 0 |
| 16 | 4/2/2019 12:38 | 4/2/2019 20:00 | 7.37 | 38.62 | 0.24 | 76 | 27.37 | 6.77 | 0.08 | 0 |
Note. HR = heart rates, Prop. = proportion, m/s = meters per second, km = kilometers.
Figure 1.
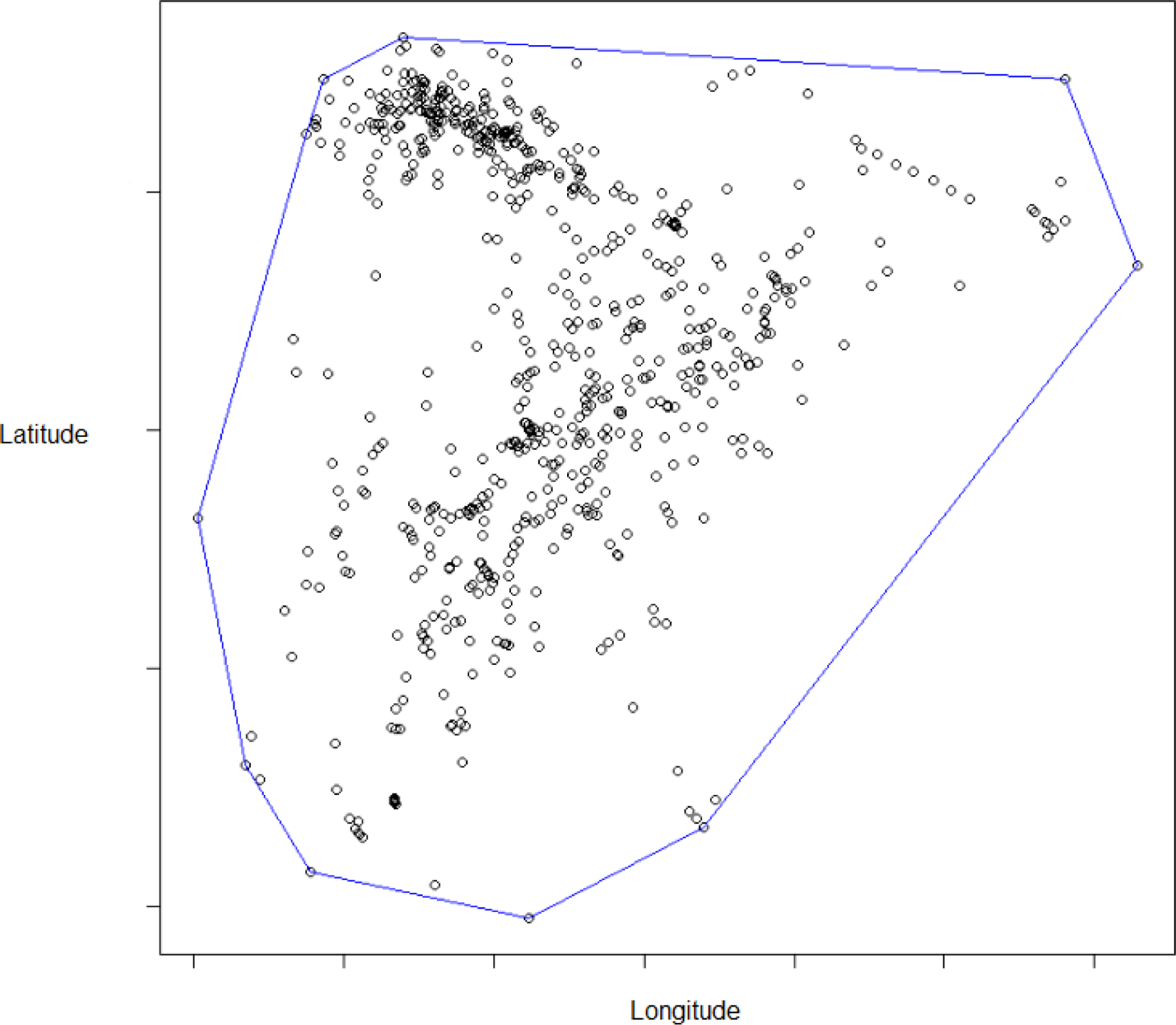
Example Convex Hull of one GPS track.
T.’s movement paths are drawn in Figure 2, with different color codes being used for different days. This map shows T.’s everyday mobility practice and varied route patterns, reflecting his engagement in various activities and trip behaviors, all of which were confined in the city.
Figure 2.

A comprehensive track map of T’s life-space mobility behaviors.
Note. We removed the road network to protect the participant’s anonymity. A black star indicates participants’ home.
Self-Report Mobility Assessment
T’s score on the LSA was 80 (range: 0–120), indicating that he made movements in his life spaces over the past four weeks, extending from his bedroom to within town. His movement was not beyond the town or geographic region (Baker et al., 2003).
Travel Diary
The travel diary data shows different activities performed by T. in various locations, such as adult daycare center visits, visiting a hair salon, meeting friends, clinic visits, etc. The adult daycare center visits occurred twice a week during the monitoring period. T. regularly spent time in the front porch once to three times a day to smoke a cigar. The diary shows his out-of-home activities usually ended at around 4 – 8 pm. The diary data enhanced the understanding of the differing time-geographies of the individual throughout the monitoring period.
Qualitative Results
Thirty-five codes were grouped into categories that supported three specific themes: perceived mobility, perceptions of technology and suggestions, and privacy and security concerns of the data and the device. Although we explored sociocultural factors as it relates to mobility and technology, this did not emerge as a theme.
Perceived Mobility
Participants shared their stories on how Alzheimer’s impacted their lives in terms of mobility and dependence on others.
The Person with Dementia.
T. perceived mobility as “the free movement of yourself” that allowed him “to be more free”. He recognized the increasing need for depending on his wife’s help when going out because he knew that he was not allowed to drive due to his dementia. He expressed fear about outdoor trips: “it’s kinda like a fear factor where, you know, I-I’m gonna—think I’m gonna get lost or something like that. You know, not know my way back home or something like that.” He commented that it is okay for dementia patients to go outside and walk around but “there’s limitations to it, I mean, depending on, um, where you’re at—you’re at that per—uh, that specific day and stuff like that.”
Family Caregiver.
M.s interview provided the contextual information of T.’s mobility practices. For example, M. explained the frequency and type of outdoor activities T. had been having regularly: “Um, he goes out with a buddy for lunch every other week. And he keeps him for two hours. They go to all the bars and do, you know. So I have that set up for him. … And they pick him up and drop him off.” M. perceived that T.’s mobility level had been increased since dementia diagnosis, which she related to T.’s behavioral symptoms of dementia: “Honestly, I think he moves around more now with the Alzheimer’s and the pacing than he’s ever moved around, because he never stops. … But most times he’s walking. Front door, back door. Y-you know, the pacing.” In addition, M. made a comment on T.’s involvement in some errands (e.g., walking the dog, yard work) or wandering behaviors, which enhanced our understanding of clusters of GPS points captured near the home location.
Perception of Technology and Suggestions
Overall usefulness, ease of use, drawbacks and suggestions regarding the GPS device were shared by both participants.
The Person with Dementia.
T. held a positive attitude toward the GPS watch use for dementia care. He reported that “it was pretty easy to use” and it would be convenient to have a watch-type health monitor for him. He commented that it would be helpful to see the data that show how active he is in his home and community. He also admitted that the device “confounded me at times” as he would unintentionally turn it off throughout the day.
Family Caregiver.
M. thought her husband liked the device as well: “Appealing to T., he was so intrigued by it. … He was playing with it all the time, so it’s kind of a cool device. In fact, he wanted to keep it.” When asked about her thoughts about the device, M. commented “it was a pretty good device” and it was “easy to use” and the directions on programming were “pretty easy to follow”. She also noted drawbacks of the device as it pertained to use in dementia care: “Uh, the only—I mean, it’s a cool thing if you don’t have Alzheimer’s. But if you have Alzheimer’s, I had an issue where he would press the buttons and set it off or not save it. And before you know it, he was recording something else…if he turns it off, I can’t track him.” To ease this burden, she suggested a wearable sensor device that could track dementia patients’ activity levels and heart rate in a way that “they can’t take it off.” She also wished that “…it shouldn’t have buttons” and that only she could control it using a smart phone.
Privacy and Security Concerns of Data and Device
The participants were asked if they had concerns about the device in terms of privacy, security, loss of device, and sharing of data with healthcare providers and family members.
The Person with Dementia.
T. had no difficulty sharing the GPS data with “Just my own doctor” or others as long as they asked him.
Family Caregiver.
M. explicitly stated that she did not have any privacy concerns about sensor-based monitoring. Regarding the sharing of data with healthcare providers and family she responded “I wouldn’t have a problem. The more information they have, the better.” To data security questions, “I like the idea that you can download it. Because if they lose the watch …. you still have the information. So that’s the part I really liked.” She also shared her concerns about the loss of the device when used by someone with Alzheimer’s: “It’s useless if they can take it off, to me. That’s my biggest concern…. I want to have reassurance that it’s going to stay on him.”
Discussion
This is one of the first studies to examine the utility, feasibility, and acceptability of GPS watches for mobility assessment in ethnic minority PWDs and to examine situated details about mobility behaviors based on multiple data collection methods. There are several noteworthy results. First, the GPS data combined with the travel diary and interviews show that T. navigated the community and made outdoor trips nearly every day to participate in social events and perform recreational activities. Second, despite out-of-home movements being made nearly every day, the distance moved, convex hull area, the paths taken, and the proportion of time spent in home fluctuated within the monitoring period, indicating day-to-day variability. Third, the LSA, GPS, and travel diary data provided distinct, but complementary information regarding the individual’s mobility behaviors. For example, the diary data revealed the details of daily, routine activities, especially performed in an outside area close to the home (e.g., staying on the porch to smoke a cigarette, walking the dog, or yard work), in contrast to the broader spatial or temporal frame assessed by other methods.
The qualitative interviews provided interesting information on both the perceived usefulness of the GPS watch and feasibility. We found the dyad’s overall acceptance of using the GPS watch to monitor physical activity levels and keep track of the PWD. They thought the design of the device was appealing and it was easy to use. The caregiver especially liked that the device offered several tracking features, including heart rates and physical exercise. We did not find any feelings of stigmatization induced by the GPS device use, which is suggested as a critical factor affecting tracking technology acceptance in PWDs and caregivers (Faucounau et al., 2009). However, due to the single case study nature, it was hard to determine whether this attitude is common among Latino PWDs and caregivers. Despite the positive attitudes, we found some technical issues. Among the most important were the caregiver’s concerns about how easily the setting can be changed by pushing buttons or touching the display. She preferred a device that is controlled only by the caregiver to make sure her loved one is being tracked without any interruptions.
Studies indicate the predictive ability of gait speeds faster than 1m/s for survival and positive health outcomes (Studenski et al., 2011; Xu et al., 2009). T’s in-home gait speeds were either zero or faster than 1.3 m/s. Sensor-based studies reported an average out-of-home gait speed of 3.7 – 3.9 km/h (1.03 – 1.09 m/s) (Wettstein et al., 2015; Wettstein, Wahl, et al., 2014) and average in-home gait speed of 0.51 m/s in older adults (Stone et al., 2015). The fact that T. was fairly young (64 years old) at the time of data collection might provide a plausible explanation for his faster gait speeds in some tracks. Also, this may indicate that the GPS data captured T.’s signs of pacing, one of the behavioral symptoms of dementia, as noted in the caregiver interview. As such, GPS-based daily monitoring could provide a tool for assessing the onset or display of mobility-related behavioral symptoms, such as wandering, pacing, or slow movement.
The current study demonstrates the need for family members’ help in wearable GPS technology utilization for PWDs. T. needed his wife’s help in turning on and off the GPS watch and syncing the device with his smartphone app. Additionally, we found that M. was actively planning for T’s out-of-home activities because she knew how to appropriately manage T’s behavioral symptoms. This is not consistent with the results of the previous study that reported confusion about the disease and unmet needs for support among Hispanic dementia caregivers (Iribarren et al., 2019). Family members have a critical role in deciding the level and type of community navigation and activity participation for their loved ones. The GPS tracks data show that T. was active in out-of-home activities, and he was aware of the need for transportation and scheduling assistance from M. Given 83% of dementia care is provided at home by informal caregivers (Friedman et al., 2015) and many informal caregivers share a routine with their loved ones (Sefcik et al., 2018), PWDs’ mobility can be influenced not only by their functional levels but also by caregivers’ preferences, characteristics, life styles and beliefs (Chung et al., 2020). Thus, family members, in addition to PWDs, should be included as targets of technology-based interventions designed to increase mobility and social participation among PWDs.
This study had some limitations. First, the sample size was limited to one dyad. Therefore, this study does not offer generalizable conclusions. It is necessary to conduct studies examining potential barriers to or concerns about participating in tracking technology trials among ethnic minority PWDs and their caregivers. Second, although the GPS data offer insight into how the PWD navigated his environment, the lack of adherence to the device use protocol due to his cognitive impairment resulted in inconsistent GPS watch use hours. There should be efforts to consider user characteristics (e.g., cognitive function) and preferences before selecting the device.
Conclusion
This study indicates that various mobility assessment methods contribute to the comprehensive portrayal of mobility, providing insights that could be useful in tailoring activity recommendations at the individual and programmatic levels. This study has clinical implications for gerontology nurses. The GPS-based LSM data could be integrated into mobility assessments with clinical decision support that will allow remote functional assessment and proactive intervention to improve the level of mobility among PWDs. Furthermore, the study findings will inform the development of a comprehensive monitoring system for early detection of mobility changes and for personalized notification about the potential risks. Future research should examine LSM characteristics with a larger sample of Latino PWDs to identify sociocultural factors influencing LSM performance. Such information then can be used to improve mobility outcomes and delay functional deterioration in this population. Furthermore, researchers should be motivated to investigate potential concerns and usability issues related to wearable location tracking devices and factors contributing to adherence to GPS monitoring protocols and user concerns to maximize the benefits of GPS tracking technologies for PWDs and caregivers.
Supplementary Material
Acknowledgement:
The authors would like to express our gratitude to Ms. Erika L. Partridge for her administrative support.
Funding:
Research reported in this publication was supported by the National Institute on Aging of the National Institutes of Health under Award Number P30AG043097. The sponsor was not involved in study design, data collection, analysis, and interpretation of data, and writing the report. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of Conflicting Interests: The authors declare no conflicts of interest.
Contributor Information
Jane Chung, Department of Family and Community Health Nursing, School of Nursing, Virginia Commonwealth University, Richmond, VA.
Joseph Boyle, Department of Biostatistics, School of Medicine, Virginia Commonwealth University, Richmond, VA.
Ingrid Pretzer-Aboff, Department of Adult Health and Nursing Systems, School of Nursing, Virginia Commonwealth University, Richmond, VA.
Janice Knoefel, Departments of Neurology and Internal Medicine (Geriatrics), School of Medicine, University of New Mexico, Albuquerque, NM.
Heather M. Young, Betty Irene Moore School of Nursing, University of California Davis, Sacramento, CA.
David C. Wheeler, Department of Biostatistics, School of Medicine, Virginia Commonwealth University, Richmond, VA.
References
- Appelhans T, Detsch F, Reudenback C, Woellauer S, Forteva S, Nauss T, Pebesma E, Russell K, Sumner M, Darley J, Roudier P, Schratz P, Environmental Informatics Marburg, & Busetto, L. (2020). mapview: Interactive Viewing of Spatial Data in R https://cran.r-project.org/web/packages/mapview/index.html
- Baker PS, Bodner EV, & Allman RM (2003). Measuring life-space mobility in community-dwelling older adults. Journal of the American Geriatrics Society, 51(11), 1610–1614. 10.1046/j.1532-5415.2003.51512.x [DOI] [PubMed] [Google Scholar]
- Boyatzis RE (1998). Transforming qualitative information: Thematic analysis and code development SAGE Publications, Inc. [Google Scholar]
- Chung J, Lee J, & Elswick RK Jr. (2020). Life-space mobility in dementia patients and family caregivers: A dyadic approach. International Journal of Older People Nursing, 15(4), e12341. 10.1111/opn.12341 [DOI] [PubMed] [Google Scholar]
- Chung J, Thompson HJ, Joe J, Hall A, & Demiris G (2017). Examining Korean and Korean American older adults’ perceived acceptability of home-based monitoring technologies in the context of culture. Informatics for Health & Social Care, 42(1), 61–76. 10.3109/17538157.2016.1160244 [DOI] [PubMed] [Google Scholar]
- Creswell JW, & Clark VLP (2017). Designing and conducting mixed methods research (3rd ed.). SAGE Publications, Inc. [Google Scholar]
- Cramm JM, Hartgerink JM, de Vreede PL, Bakker TJ, Steyerberg EW, Mackenbach JP, & Nieboer, a P. (2012). The relationship between older adults’ self-management abilities, well-being and depression. European Journal of Ageing, 9(4), 353–360. 10.1007/s10433-012-0237-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe M, Andel R, Wadley VG, Okonkwo OC, Sawyer P, & Allman RM (2008). Life-space and cognitive decline in a community-based sample of African American and Caucasian older adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 63(11), 1241–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faucounau V, Riguet M, Orvoen G, Lacombe A, Rialle V, Extra J, & Rigaud AS (2009). Electronic tracking system and wandering in Alzheimer’s disease: A case study. Annals of Physical and Rehabilitation Medicine, 52(7–8), 579–587. 10.1016/j.rehab.2009.07.034 [DOI] [PubMed] [Google Scholar]
- Friedman EM, Shih RA, Langa KM, & Hurd MD (2015). US prevalence and predictors of informal caregiving for dementia. Health Affairs, 34(10), 1637–1641. 10.1377/hlthaff.2015.0510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iribarren S, Stonbraker S, Suero-Tejeda N, Granja M, Luchsinger JA, Mittelman M, Bakken S, & Lucero RJ (2019). Information, communication, and online tool needs of Hispanic family caregivers of individuals with Alzheimer’s disease and related dementias. Informatics for Health and Social Care, 44(2), 115–134. 10.1080/17538157.2018.1433674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton MP, & Brody EM (1969). Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist, 9(3), 179–186. http://www.ncbi.nlm.nih.gov/pubmed/5349366 [PubMed] [Google Scholar]
- Mahendran N, Kuys SS, Downie E, Ng P, & Brauer SG (2016). Are accelerometers and GPS devices valid, reliable and feasible tools for measurement of community ambulation after stroke? Brain Impairment, 17(2), 151–161. 10.1017/brimp.2016.13 [DOI] [Google Scholar]
- Mc Ardle R, Morris R, Hickey A, Del Din S, Koychev I, Gunn RN, Lawson J, Zamboni G, Ridha B, Sahakian BJ, Rowe JB, Thomas A, Zetterberg H, MacKay C, Lovestone S, & Rochesteron L (2018). Gait in mild Alzheimer’s disease: Feasibility of multi-center measurement in the clinic and home with body-worn sensors: A pilot study. Journal of Alzheimer’s Disease : JAD, 63(1), 331–341. 10.3233/JAD-171116 [DOI] [PubMed] [Google Scholar]
- Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, & Chertkow H (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53(4), 695–699. 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- Nowell LS, Norris JM, White DE, & Moules NJ (2017). Thematic analysis: Striving to meet the trustworthiness criteria. International Journal of Qualitative Methods, 16(1), 1–13. 10.1177/1609406917733847 [DOI] [Google Scholar]
- Pfeffer RI, Kurosaki TT, Harrah CH, Chance JM, & Filos S (1982). Measurement of functional activities in older adults in the community. Journal of Gerontology, 37(3), 323–329. http://www.ncbi.nlm.nih.gov/pubmed/7069156 [DOI] [PubMed] [Google Scholar]
- Sartori AC, Wadley VG, Clay OJ, Parisi JM, & Crowe M (2012). The relationship between cognitive function and life space: The potential role of personal control beliefs. Psychology and Aging, 27(2), 364–374. 10.1037/a0025212.The [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sefcik JS, Johnson MJ, Yim M, Lau T, Vivio N, Mucchiani C, & Cacchione PZ (2018). Stakeholders’ perceptions sought to inform the development of a low-cost mobile robot for older adults: A qualitative descriptive study. Clinical Nursing Research, 27(1), 61–80. 10.1177/1054773817730517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone E, Skubic M, Rantz M, Abbott C, & Miller S (2015). Average in-home gait speed: Investigation of a new metric for mobility and fall risk assessment of elders. Gait & Posture, 41(1), 57–62. 10.1016/j.gaitpost.2014.08.019 [DOI] [PubMed] [Google Scholar]
- Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, Brach J, Chandler J, Cawthon P, Connor EB, Nevitt M, Visser M, Kritchevsky S, Badinelli S, Harris T, Newman AB, Cauley J, Ferrucci L, & Guralnik J (2011). Gait speed and survival in older adults. JAMA : The Journal of the American Medical Association, 305(1), 50–58. 10.1001/jama.2010.1923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung JY, Rose RV, Gammada E, Lam I, Roy EA, Black SE, & Poupart P (2014). Measuring life space in older adults with mild-to-moderate Alzheimer’s disease using mobile phone GPS. Gerontology, 60(2), 154–162. 10.1159/000355669 [DOI] [PubMed] [Google Scholar]
- Wahl Y, Düking P, Droszez A, Wahl P, & Mester J (2017). Criterion-validity of commercially available physical activity tracker to estimate step count, covered distance and energy expenditure during sports conditions. Frontiers in Physiology, 8(SEP). 10.3389/fphys.2017.00725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webber SC, Porter MM, & Menec VH (2010). Mobility in older adults: a comprehensive framework. Gerontologist, 50(4), 443–450. 10.1093/geront/gnq013 [DOI] [PubMed] [Google Scholar]
- Wettstein M, Wahl H-W, Shoval N, Oswald F, Voss E, Seidl U, Frolich L, Auslander G, Heinik J, & Landau R (2015). Out-of-home behavior and cognitive impairment in older adults: Findings of the SenTra Project. Journal of Applied Gerontology, 34(1), 3–25. 10.1177/0733464812459373 [DOI] [PubMed] [Google Scholar]
- Wettstein M, Wahl HW, & Diehl MK (2014). A multidimensional view of out-of-home behaviors in cognitively unimpaired older adults: Examining differential effects of socio-demographic, cognitive, and health-related predictors. European Journal of Ageing, 11(2), 141–153. 10.1007/s10433-013-0292-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, & Leirer VO (1982). Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research, 17(1), 37–49. 10.1016/0022-3956(82)90033-4 [DOI] [PubMed] [Google Scholar]
- Yin RK (2002). Case Study Research: Design and Methods (3rd editio). SAGE Publications, Inc. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


