Abstract
Aldosterone and cortisol serve important roles in the pathogenesis of cardiovascular diseases and metabolic disorders. Epigenetics is a mechanism to control enzyme expression by genes without changing the gene sequence. Steroid hormone synthase gene expression is regulated by transcription factors specific to each gene, and methylation has been reported to be involved in steroid hormone production and disease. Angiotensin II or potassium regulates the aldosterone synthase gene, CYP11B2. The adrenocorticotropic hormone controls the 11b-hydroxylase, CYP11B1. DNA methylation negatively controls the CYP11B2 and CYP11B1 expression and dynamically changes the expression responsive to continuous stimulation of the promoter gene. Hypomethylation status of the CYP11B2 promoter region is seen in aldosterone-producing adenomas. Methylation of recognition sites of transcription factors, including cyclic AMP responsive element binding protein 1 or nerve growth factor-induced clone B, diminish their DNA-binding activity. A methyl-CpG-binding protein 2 cooperates directly with the methylated CpG dinucleotides of CYP11B2. A low-salt diet, treatment with angiotensin II, and potassium increase the CYP11B2 mRNA levels and induce DNA hypomethylation in the adrenal gland. A close association between a low DNA methylation ratio and an increased CYP11B1 expression is seen in Cushing’s adenoma and aldosterone-producing adenoma with autonomous cortisol secretion. Epigenetic control of CYP11B2 or CYP11B1 plays an important role in autonomic aldosterone or cortisol synthesis.
Keywords: aldosterone, cortisol, methylation, adrenal gland, hormone-producing adenoma
1. Introduction
Steroid hormones play a pivotal role in regulating blood pressure, cardiac function, water and electrolyte balance, and stress response [1,2,3,4]. Mineralo- and glucocorticoids are synthesized through de novo steroidogenesis in the adrenal gland. Aldosterone synthesis occurs in numerous tissues including cardiovascular tissues [5], the brain [6], adipose tissues [7], and the peripheral nerves [8]. Extra adrenal production of cortisol is reported in the immune system, skin, and intestine [9,10].
The adrenal gland utilizes cholesterol and lipoproteins for the biosynthesis of pregnenolone and the following steroids in the mitochondria. Some of the steps in steroidogenesis occur in microsomes (the endoplasmic reticulum). The adrenal cortex is able to de novo biosynthesize cholesterol [11,12].
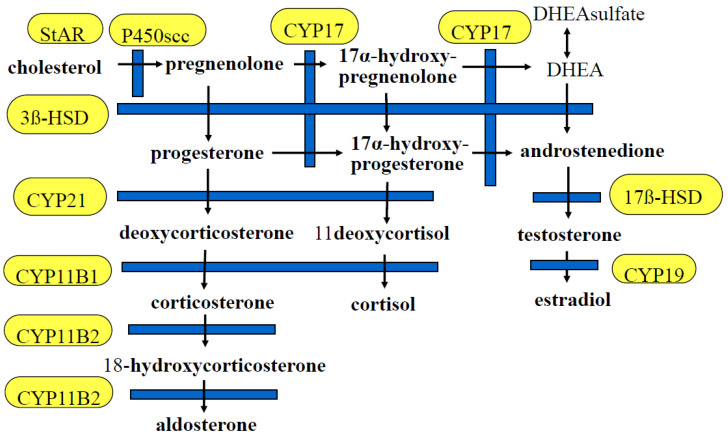
The adrenal cortex is composed of three functional zones. The zona glomerulosa, the outer zone of the gland, expresses aldosterone synthase, CYP11B2, which catalyzes the synthesis of aldosterone [13]. The renin-angiotensin system (RAS) and potassium regulate CYP11B2 expression. The zona fasciculata produces cortisol. CYP11B1 (11-hydroxylase) is highly expressed in the zona fasciculata and is regulated by ACTH [12]. The innermost layer, the zona reticularis, expresses CYP17 and produces DHEA and is also a source of androstenedione (A4, delta4), which is the primary adrenal androgen in some species (Figure 1). The hypothalamus–pituitary–adrenal axis, via a negative or positive feedback system, controls cortisol and DHEA production [14]. The 11Beta-hydroxylase gene, CYP11B1 expression, is regulated by ACTH and a cAMP-regulated signaling pathway involving the CREB protein family [15]. Although CYP11B2 and CYP11B1 are highly conserved, there are significant differences between the CYP11B1 and CYP11B2 5′upstream region, which may explain the different control of the mechanism of transcription [16].
Figure 1.
Steroid pathway. StAR, steroidogenic acute regulatory protein; P450scc, cholesterol side-chain cleavage enzyme; CYP17, 17α-hydroxylase; DHEA, dehydroepiandrosterone; 3β-HSD, 3β-hydroxysteroid dehydrogenase; CYP21, 21-hydroxylase; 17β-HSD, 17β-hydroxysteroid dehydrogenase; CYP11B1, 11 β-hydroxylase; CYP19, aromatase; CYP11B2, aldosterone synthase.
2. Epigenetic Control of Gene Expression
Epigenetic changes are inherited modifications that are not present in the DNA sequence. Gene expression is regulated at various levels, not only in response to DNA modification. Histone acetylation modifications regulate gene expression [17]. Gene silencing is induced by DNA hypermethylation [18]. Gene expression is also regulated by RNA modifications which mediate RNA metabolism [19].
3. DNA Methylation
DNA methylation at the 5′-cytosine of CpG dinucleotides is a major epigenetic modification in eukaryotic genomes and is required for mammalian development [20]. It is associated with the formation of heterochromatin and gene silencing.
Dysregulation of DNA methylation of RAS genes has been involved in the pathogenesis of hypertension and cardiovascular diseases [21]. DNA methylation is established during usual development and disease progression. However, the DNA methylation pattern is in part dynamic in response to environmental changes [22,23]. Cardiovascular disorders, diabetes mellitus, and dyslipidemia, as well as lifestyle changes, dynamically affect DNA methylation.
4. Histone Modifications
Histone modification is an epigenetic modification characterized by the addition of an acetyl group to histone proteins, specifically to the lysine residue within the N-terminal tail [24]. This histone modification is catalyzed by histone acetyl transferases (HATs) or histone deacetylases (HDACs), which are associated transcription factors (TFs) [25,26]. Huang et al. [27] reported that histone demethylase lysine-specific demethylase 1 (LSD1) deficient rodents showed increased aldosterone production.
5. Epigenetic Control of CYP11B2
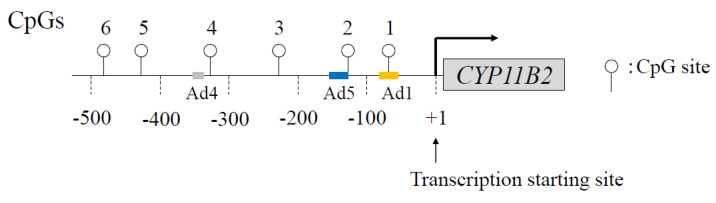
Figure 2 shows the CpG sites of the CYP11B2 promoter region. In human and rodent adrenal glands, CYP11B2 expression is regulated by not only RAS but also by endothelin and atrial natriuretic hormones [28,29,30,31]. Although potassium stimulates aldosterone biosynthesis [32,33,34], its pathophysiological roles are unclear. Angiotensin II and potassium can activate a number of cis-acting elements in the promoter of this gene, including the cAMP response element (CRE), nerve growth factor-induced clone B (NGFI-B) response element (NBRE-1), activating transcription factor 1 (ATF1), or CRE-binding protein 1 (CREB1) binding to Ad1/CRE, increasing CYP11B2 transcription [35,36] (Figure 3).
Figure 2.
Schema of CpG dinucleotides within the human CYP11B2 gene promoter. Open circle denotes CpG dinucleotides. Ad, cis-acting element.
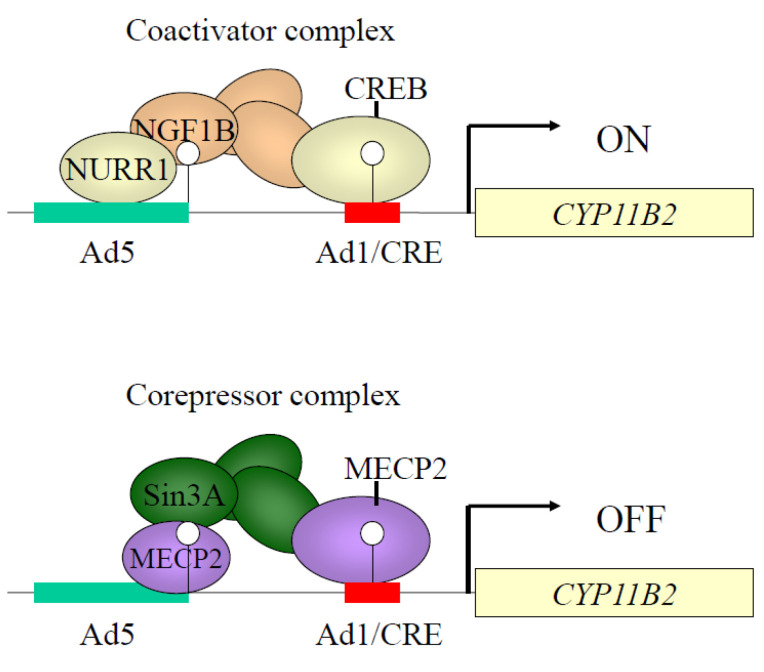
Figure 3.
Coactivator and corepressor complexes of CYP11B2 promoter region. Binding activities of coactivator complexes, such as CREB (cyclic AMP responsive element binding protein), NURR1 (nuclear receptor-related factor 1), and corepressor complex MECP2 (methyl-CpG-binding protein 2) are regulated by DNA methylation. Methylation of CpG1 greatly decreased CREB1 binding to Ad1 (cis-acting element 1). DNA methylation at CpG2 reduced basal binding activities of NGF1B (nerve growth factor-induced clone B) (NR4A1) and NURR1 (NR4A2) with Ad5. DNA methylation increased MECP2 binding to CpG1 and CpG2. NR4A, nuclear receptor 4 group A; Sin3A, SIN3 transcription regulator family member A.
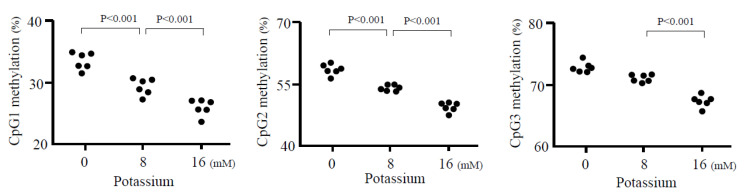
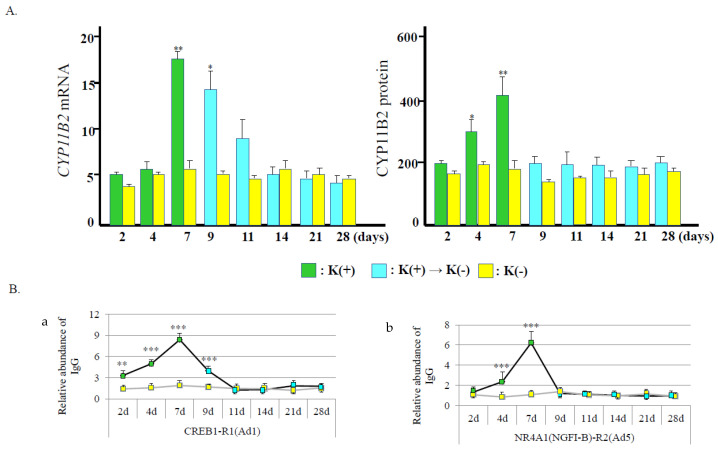
We have reported that angiotensin II dynamically changed DNA methylation patterns in the CYP11B2 promoter [37]. DNA methylation patterns are unstable in CpG in several circumferences [38]. However, where and how do changes in DNA methylation take place in non-CpG promoter sites? We reported that stimulatory signals of potassium treatment led to DNA demethylation around transcription factor binding sites and a transcription start site, where the chromatin structure was relaxed [39] (Figure 4). DNA demethylation was observed during two days of potassium treatment, while the highest level of demethylation was evident by seven days. The CYP11B2 promoter demethylation increased gene expression [39] (Figure 5A).
Figure 4.
Effect of potassium on methylation of CYP11B2 promoter in H295R cells. Potassium decreased in dose-dependent methylation ratio in CpG1, 2, and 3 sites.
Figure 5.
(A) Effect of potassium on CYP11B2 mRNA and protein level. In CYP11B2 mRNA level, results are given as fold change normalized to ACTB. * p < 0.01 and ** p < 0.005 vs. K(−). K(−) indicates H295R cells treated with no additional potassium. (B) Potassium-induced recruitment of CREB1 and NR4A1 in the CYP11B2 promoter. (a), CREB1 recruitment to Ad1; (b), NR4A1 (NGFI-B) recruitment to Ad5. ** p < 0.005 and *** p < 0.0001 vs. K(−).
The CREB1/ATF and NR4A family members lead to the activation of transcription. In our study, DNA demethylation, CREB1 recruitment, and chromatin relaxation at Ad1 were detected within two days after potassium treatment (Figure 5B). In contrast, Ad5 lagged two days behind Ad1 in chromatin accessibility. CREB1/ATF family members start chromatin remodeling by DNA demethylation at Ad1. CREB1/ATF family members may help NR4A family members initiate chromatin remodeling. This combination leads to gained gene expression with DNA demethylation about the transcription start site (TSS) in this gene. Cooperative action collectively undertaken by the CREB1/ATF family and NR4A family plays a pump-priming function in the control chromatin remodeling and DNA methylation in the CYP11B2 promoter [37].
After potassium withdrawal, DNA methylation, NR4A1 (NGFI-B) recruitment, and chromatin accessibility at Ad5 immediately returned to normal levels. In contrast, DNA hypomethylation, CREB1 recruitment, and chromatin relaxation at Ad1 continued for several days after the stop of the stimulation. CREB1/ATF family members are retained at Ad1, acting to hold the DNA hypomethylation and chromatin relaxation. A memory of the potassium stimulation in the CYP11B2 promotor is functioning by the epigenetic mechanism [39].
DNA methyltransferases (DNMTs), DNMT3A and 3B, establish and maintain DNA methylation. DNMT1 serves DNA methylation patterns through sequential rounds of cell division [40]. In our study, DNA demethylation of the CYP11B2 promoter was associated with decreased DNA methylation activities. The balance between DNA demethylation and methylation activities is a major factor in the DNA methylation pattern.
A low-sodium diet or treatment with Angiotensin II increases CYP11B2 mRNA levels and aldosterone production in the cardiovascular tissues as well as in the adrenal gland [41]. We reported that an angiotensin II infusion in rats decreased the methylation ratio of CYP11B2 and increased the gene expression in the adrenal gland [37]. Treatment with angiotensin II in the cultured adrenal cells showed the same results. A low-salt diet induces hypomethylation of rat CYP11B2 and increases CYP11B2 mRNA levels parallel with aldosterone synthesis. A high-salt diet or treatment with a type 1 angiotensin II receptor blocker increases the methylation ratio of this gene. Taken together, angiotensin II is a major contributing factor to CYP11B2 methylation. The rat zona glomerulosa transcriptome is changed by dietary sodium intake, involving more than 280 differentially regulated genes [42]. Nishimoto et al. [42] suggest that a change in salt intake affects the transcriptome by neurological responses as well as by RAS activation.
Aldosterone plays an important role in the pathogenesis of cardiovascular and renal disease in experimental and clinical studies [43,44,45,46]. Treatment with angiotensin-converting enzyme (ACE) inhibitors or angiotensin II type 1 receptor blockers (ARBs) for a long time increases plasma aldosterone to above pretreated levels, which is called “aldosterone breakthrough” [47]. This phenomenon has important clinical consequences, especially in congestive heart failure [48]. Involvement of various in vivo factors such as ACTH, electrolytes, endothelins, and angiotensin II type 2 receptor actions [49] have been proposed to explain this breakthrough phenomenon; however, details concerning the underlying mechanism remain unknown. We have reported that although both the direct renin inhibitor and ARB caused aldosterone breakthroughs, plasma endothelin levels were not increased [50]. Treatment with ARB influences CYP11B2 methylation. It would be interesting to know whether or not the treatment with an ACE inhibitor or ARB for a long time influences the methylation status of CYP11B2 and leads to aldosterone breakthrough.
Hughes-Austin et al. [51] reported that serum high potassium levels are associated with an increased risk for all-cause mortality independent of renal function or other cardiovascular risk factors. Weir et al. [52] reported that patiomer, a nonabsorbed potassium binder, decreased circulating aldosterone as well as serum potassium levels in patients with chronic kidney disease (CKD) taking renin-angiotensin system (RAS) inhibitors. These data suggest that potassium regulates aldosterone synthesis independent of RAS. It is interesting to look at whether treatment with patiomer prevents cardiovascular events in CKD patients. Sakthiswary et al. [53] reported that urinary potassium excretion was increased in patients with aldosterone breakthrough. Potassium may be important for aldosterone synthesis during treatment with RAS inhibitors. The pathophysiologic importance of epigenetic modification of CYP11B2 by potassium should be further studied.
6. Epigenetic Modification of CYP11B2 in Aldosterone-Producing Adenoma
Primary aldosteronism (PA) is recognized as a common secondary hypertension and accounts for approximately 5–15% of the hypertension population [54]. The most common clinical subtypes of PA are aldosterone-producing adenoma (APA) and bilateral adrenocortical hyperplasia [55]. We and others previously reported a lower degree of methylation of CYP11B2 in APAs than in adrenal tissues or non-functioning adrenal adenomas. A negative correlation between the CYP11B2 methylation ratio and mRNA levels was identified [37,56,57]. Di Dalmazi et al. [58] evaluated DNA methylation levels of CYP11A1, CYP11B1, CYP11B2, CYP17A1, CYP21A2, HSD3B, NR5A1, and STAR in benign adrenocortical tumors. They found that the methylation rates of CYP11B2 were decreased in APAs compared with non-functioning adenomas. Epigenetic control of CYP11B2 expression may play an important role in aldosterone synthesis in APA. Yoshii et al. [59] reported that the methylation rate in several CpG sites was lower in APAs than in non-functioning adrenocortical adenomas. They found no significant relationship between methylation rates and mRNA levels. They also reported that KCNJ5 mutation in APAs did not affect the methylation status. Nishimoto et al. [60] reported an interesting case of a patient with PA. The patient’s adrenal subcapsular aldosterone-producing cell clusters (APCCs) developed into nodules, which caused hyperaldosteronism. Some of the APCCs possess somatic gene mutations known to increase aldosterone synthesis [61,62]. These findings suggest that APCCs may play a part in the pathogenesis of PA. However, Omata et al. [63] reported that APCCs are frequent in the adrenal glands of nonhypertensive Japanese individuals in which somatic mutations (most commonly in the calcium voltage-gated channel subunit alpha1 D (CACNA1D)) were detected. We found the KCNJ5 mutation in aldosterone-producing microadenoma and APCCs, in which methylation rates of CYP11B2 were decreased compared with adjacent adrenal tissues. However, Di Dalmazi et al. [58] reported that the methylation status of CYP11B2 did not differ markedly between APCCs and adjacent adrenal tissues or non-functioning tumors. Sun et al. [64] reported specific subgroups of APCCs with markedly variant distribution patterns of metabolites. Further study is necessary to clarify the mechanism of overproduction of aldosterone in the APCC and APA, including epigenome and metabolome.
Mineralocorticoid receptors (MRs) are expressed in cardiovascular tissues and the kidneys. MR antagonists (MRA) (spironolactone, eplerenone, esaxerenone) have been used for the treatment of PA [65,66]. Several papers have reported cases of idiopathic hyperaldosteronism with spontaneous remission during MRA therapy [67]. We have reported a case of APA with remission after long-term spironolactone therapy [68]. We compared the remission rate between spironolactone and eplerenone therapy in essential hypertension and found no difference between the two groups (unpublished data). Ye et al. [69] reported that spironolactone inhibited basal- and angiotensin-II-stimulated aldosterone synthesis in human adrenal cells. However, eplerenone did not inhibit aldosterone synthesis in H295R cells. We have reported that eplerenone inhibited tissue RAS [49]. The effect of MRA on the methylation of CYP11B2 in the cardiovascular tissues as well as in the adrenal gland should be clarified.
7. Extra-Adrenal Mineralo- and Glucocorticoid Synthesis
Aldosterone synthesis at extra-adrenal sites is regulated by the RAS [70]. The mRNA of the StAR gene, CYP11A, 3β-hydroxysteroid dehydrogenase, CYP21, CYP11B1, and CYP11B2 are expressed in blood vessels and the heart [71,72]. We found that the CYP11B2 mRNA levels were lower in renal arteries than in the adrenal gland and a hypermethylation status was seen in renal arteries [37].
Briones et al. [7] reported that the aldosterone synthase gene and protein were detected in 3T3-L1 and mature adipocytes, which produce aldosterone basally and in response to angiotensin II. In 3T3-L1 “adipocytes”, angiotensin II increased the CYP11B2 expression. Treatment with ARB or inhibitors of calcineurin blunted the angiotensin II effects. FAD286 (an aldosterone synthase inhibitor) inhibited adipocyte differentiation.
We previously reported that the expressions of protein and mRNA of the mineralocorticoid receptor in the peripheral nerve were equal to those in the kidney. The nerve conduction velocity (NCV) in diabetic rats was significantly improved by treatment with a mineralocorticoid receptor antagonist [73]. Mohamed et al. [8] reported that aldosterone immunoreactivity, CYP11B2 gene expression, and MR protein were abundant in peptidergic nociceptive neurons of the dorsal root ganglia. Furthermore, aldosterone and CYP11B2 were significantly upregulated in peripheral sensory neurons under inflammatory conditions. They also showed that inhibition of aldosterone synthesis in peripheral sensory neurons attenuated nociceptive behavior after hind paw inflammation.
Aldosterone synthesis and the CYP11B2 gene expression are upregulated in cardiac tissues during hypertrophic cardiomyopathy (HCM), which are recognized as major HCM phenotype modifiers [74]. Aldosterone directly affects cardiac hypertrophy and fibrosis. We previously reported that aldosterone locally produced in cardiovascular tissues exerts its effects via paracrine or intracrine mechanisms [75]. Garnier et al. [76] reported that transgenic mice overexpressing CYP11B2 in the heart showed coronary endothelium-independent dysfunction without hypertrophy. Alesutan et al. [77] showed CYP11B2 expression in the human coronary arteries as well as smooth muscle cells. CYP11B2 mRNA levels were higher in the aortic tissues of klotho-hypomorphic (kl/kl) mice than in control mice. Spironolactone ameliorated aortic osteoinduction occurred in adrenalectomized (kl/kl) mice. We have reported that the treatment with spironolactone improved cardiac hypertrophy in adrenalectomized hypertensive rats [78]. Yoshimura et al. [79] reported increased CYP11B2 expression in the hearts of patients with cardiac failure. We found a clear association between the CpG methylation and the CYP11B2 gene expression in the cardiac tissues of HCM [57]. We predict that DNA methylation at CpGs 1 and 2 is a key determinant of the CYP11B2 mRNA levels in the heart. Hypomethylation of the CYP11B2 promoter causes an aberrant increase in CYP11B2 gene expression, which induces cardiac hypertrophy or cardiomyopathy [57]. The molecular mechanisms regulating the demethylation of CpGs 1 and 2 in the heart should be established.
Cortisol, a life-sustaining adrenal hormone, is an endogenous glucocorticoid (GC) that maintains human homeostasis. This hormone is synthesized from cholesterol in the adrenal cortex by five enzymatic steps, and CYP11B1 catalyzes the final step of cortisol biosynthesis [11]. Cortisol exerts its action through binding to a GC receptor (GR) expressed in a variety of organs, and regulates hydro-mineral metabolism, blood pressure, and carbohydrate, protein, and fat metabolisms [12]. Cortisol also serves a pivotal role in anti-inflammation and immunosuppression [80].
Extra-adrenal GC synthesis has been reported in blood vessels, the skin, the brain, the immune system, and the intestine [9,10,81,82]. Circulating GC levels often do not reflect local GC levels. An adrenalectomy eliminates serum GC but not in the hippocampus or cerebral cortex [83]. The potential clinical importance of tissue GC synthesis should be further clarified.
8. Epigenetic Control of CYP11B1
Excess cortisol causes various disorders. Cushing’s syndrome is caused either by excessive medication of cortisol-like compounds or by tumors, such as pituitary and adrenal adenomas, which express high levels of the cortisol synthase gene CYP11B1 and thereby produce a high level of cortisol [84,85]. Previous reports have demonstrated the overexpression of CYP11B1 in adrenal Cushing’s syndrome [86]. However, the molecular mechanism underlying the CYP11B1 overexpression in adrenal Cushing’s syndrome remains unclear.
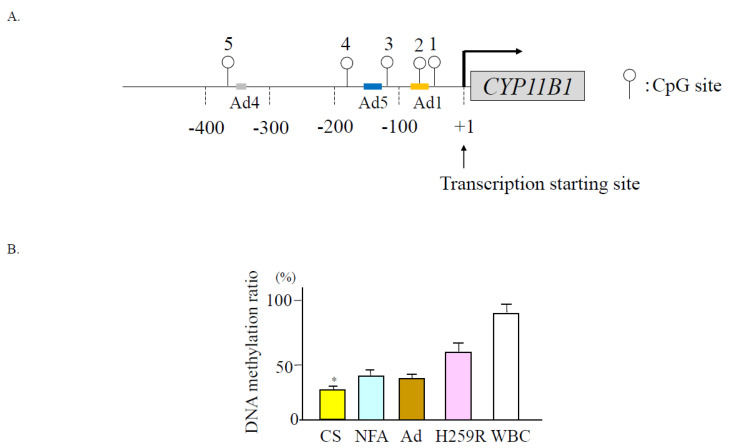
The DNA methylation inhibitor, 5′-aza-2 deoxycytidine, increases CYP11B1 expression in the adrenocortical cells [87], which suggests that its expression is regulated by DNA methylation. Figure 6A shows the CpG sites of the CYP11B1 promoter region. When we treated cultured adrenal cells with the cAMP analog, 2′-O-dibutyladenosine 3′, 5′-cyclic monophosphate (dibutyric cAMP; dbcAMP), CYP11B1 mRNA levels were increased in parallel with a decreased DNA methylation ratio [88].
Figure 6.
(A) Schema of CpG dinucleotides within the human CYP11B1 gene promoter. Open circle denotes CpG dinucleotides (cited from Ref. [88]). (B) Methylation ratios of CYP11B1 were significantly decreased in adenomas of Cushing’s syndrome. * p < 0.05 compared to other tissues; NFA, non-functioning adrenal adenoma; Ad, adjacent adrenal tissue; WBC, white blood cell.
9. Epigenetic Modification of CYP11B1 in Cortisol-Producing Adenoma
Cortisol-producing adenoma (CPA) expresses CYP11B1 entirely but not CYP11B2 [87]. Kubota-Nakayama et al. [85] reported that gene and protein expression of CYP11B1 were increased in CPAs. We reported higher mRNA levels of CYP11B1 in concomitant with a lower methylation ratio in CPAs compared to adrenal tissues or nonfunctioning adenomas [88] (Figure 6B). However, Di Dalmazi et al. [58] reported that the CYP11B1 mRNA levels and methylation status did not differ between Cushing’s adenoma and non-functioning adrenal adenoma. According to previous studies, the heterogeneity of the molecular and gene abnormalities exist in Cushing’s syndrome or subclinical Cushing’s syndrome (SCS) [89], in which epigenetic regulatory mechanisms of CYP11B1 play an important role in cortisol overproduction.
10. Epigenetic Modification of CYP11B1 in Aldosterone-Producing Adenoma with Autonomous Cortisol Secretion
SCS is an adrenal incidentaloma with autonomous cortisol secretion. The current diagnostic criteria of SCS in Japan are proposed by Yanase et al. [90]. They reported 14.4% of patients with adrenal incidentalomas [91]. SCS is much more complicated with obesity, diabetes mellitus, hypertension, and cardiovascular diseases compared with non-functioning adrenal adenomas [92]. Katabami et al. [93] reported 26% of patients with PA had mild autonomous cortisol secretion in a recent Japanese large cohort study. They reported that PA with SCS increases renal complications compared to PA without SCS. Autonomous cortisol secretion in PA also contributes to metabolic risk or cardiovascular complications [94,95]. We found that six of the sixteen APAs evaluated were associated with autonomous cortisol secretion [88]. These APAs tended to be larger in size and associated with an increased prevalence in cerebrovascular diseases than APAs without autonomous cortisol secretion. The KCNJ5 gene mutation was found in six APAs with autonomous cortisol secretion and eight of the ten APAs without autonomous cortisol secretion. The CYP11B1 promoter region was less methylated in APAs with autonomous cortisol secretion than in those without autonomous cortisol secretion. These findings further suggest the significant role of DNA methylation of the CYP11B1 promoter on gene expression.
Inoue et al. [96] recently reported the correlation between plasma aldosterone concentration and blood pressure in patients with SCS. We did not find any differences in the DNA methylation state of CYP11B2 between APAs with autonomous cortisol secretion and those without autonomous cortisol secretion. The mechanism of aldosterone synthesis in SCS with hypertension should be clarified.
11. MicroRNAs (miRNAs) in Post-Transcriptional Regulation
There is increasing evidence that miRNAs play an important role in the regulation of CYP11B1 and CYP11B2 gene expression as well as for the derived proteins [97]. miRNAs are single-stranded noncoding RNA molecules of approximately 22 nucleotides. They target specific nucleotides on the mRNA of protein-coding genes and directly repress post-transcription [98,99]. Recently, the role of miRNAs was investigated with a focus on genes of the human CYP11B subfamily [12]. Dicer1 is a key enzyme in miRNA maturation. It affects the function of miRNA miR-24, which binds to the 3′-untranslated region of CYP11B1 and CYP11B2 mRNAs [98]. Lenzini et al. [99] reported that components of the Wnt/-catenin pathway, which were downregulated by miR-23 and miR-43a, change aldosterone synthesis. Vetrivel et al. [100] reported that miR-1247-5p was upregulated in cortisol-producing adenoma (CPA). MiR-379-5p was upregulated in primary bilateral macronodular adrenocortical hyperplasia (PBMAH). Both miR-1247-5p and miR-379-5p targeted specific components in the WNT signaling pathway. Whether or not the silencing of CYP11B2 or CYP11B1 using siRNAs can be applied for treating PA or Cushing’s syndrome should be studied.
12. Epigenesis of the Other Steroid Hormone Synthase Genes
12.1. Steroidogenic Acute Regulatory Protein (StAR)
The epigenetic regulation of the StAR in the ovary is reported. Luteinizing hormone (LH) stimulation increases StAR gene expression and histone modifications are involved in its regulation. Methylation has been reported to be involved in the regulation of StAR gene expression by changes in the ovarian cycle [101].
12.2. Cytochrome P450 Family 11, Subfamily A, Polypeptide 1 (CYP11A1)
Okada et al. [102] examined methylation and histone modification of CYP11A1 by acute stimulation of hCG in ovarian granulosa cells and reported that both were affected by hCG and thus involved in gene expression. In a rat model of multiple cystic ovary syndrome, hypomethylation of a portion of the CpG site of the CYP11A1 promoter region has been reported [103].
12.3. Aromatase (CYP19A1)
An increased CYP19A1 expression and hypomethylated state in the follicle are reported [104]. In the corpus luteum, CYP19A1 is highly methylated and gene expression is low. CpG islands were found in the CRE (cAMP-responsive element) region, suggesting a relationship between cAMP-stimulated CYP19A1 gene expression and methylation [105].
12.4. 17α-Hydroxylase (CYP17A1)
In humans, CYP17A1 plays an important role in cortisol biosynthesis, while in rodents, 3β-HSD is important for corticosterone biosynthesis. CpG islands are reported to be present in rodents but absent in humans, and methylation and gene expression are reported to be related in rodents. However, the homology of genes between humans and rodents is about 45% and they share a common regulatory mechanism [106]. It is possible that some kind of methylation regulatory mechanism exists in humans as well.
13. Conclusions
The gene expression of CYP11B2 and CYP11B1 in the adrenal gland is regulated by epigenetic modification. Salt intake and potassium influence the methylation of the CYP11B2 gene. A negative correlation between DNA methylation and CYP11B1 expression is seen in Cushing’s adenoma and APA with autonomous cortisol secretion. These results suggest that the epigenetic regulation of both CYP11B2 and CYP11B1 contributes to the pathogenesis of autonomous aldosterone and cortisol synthesis.
Abbreviations
| ACE | angiotensin converting enzyme; |
| Ad | cis-acting element; |
| AMP | adenocine monophosphate; |
| ARB | AT1R blocker; |
| APA | aldosterone-producing adenoma; |
| APCC | aldosterone-producing cell cluster; |
| ATF | activating transcription factor; |
| AT1R | type2 angiotensin II receptor; |
| CACNA1D | Calcium Voltage-Gated Channel Subunit Alpha1 D |
| CEBP | CCAAT enhancer binding protein; |
| CPA | coerisol-producing adenoma |
| CREB | cyclic AMP responsive element binding protein; |
| CYP11B1 | 11β-hydroxylase |
| CYP11B2 | aldosterone synthetase; |
| GR | glucocorticoid receptor; |
| GRE | GR element; |
| HNF1A | hepatocyte nuclear factor1 homeobox A; |
| HPA | hypothalamic-pituitary-adrenal; |
| KCNJ | potassium inwardly rectifying channel subfamily J; |
| MBD | methyl-CpG-binding domain; |
| MECP | methyl-CpG-binding protein; |
| miRNA | microRNA; |
| Mi2 | chromodomain-helicase-DNA-binding protein Mi-2 homolog; |
| MR | mineralocorticoid receptor; |
| MRA | mineralocorticoid receptor antagonist; |
| NGFI-B | nerve growth factor-induced clone B; |
| NBRE-1 | NGFI-B response element; |
| NFA | non-functioning adenoma; |
| NR4A | nuclear receptor 4 group A; |
| NURR1 | nuclear receptor-related factor 1; |
| PA | primary aldosteronism; |
| RAS | renin-angiotensin system; |
| SETDB | histone-lysine N-methyltransferase; |
| Sin3A | SIN3 transcription regulator family member A; |
| STAT | signal transducer and activation transcription factor; |
| TSS | transcription start site. |
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Chong C., Hamid A., Yao T., Garza A.E., Pojoga L.H., Adler G.K., Romero J.R., Williams G.H. Regulation of aldosterone secretion by mineralocorticoid receptor-mediated signaling. J. Endocrinol. 2017;232:525–534. doi: 10.1530/JOE-16-0452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller B.S., Auchus R.J. Evaluation and treatment of patients with hypercortisolism: A review. JAMA Surg. 2020;155:1152–1159. doi: 10.1001/jamasurg.2020.3280. [DOI] [PubMed] [Google Scholar]
- 3.Karaca Z., Grossman A., Kelestimur F. Investigation of the hypothalamo-pituitary-adrenal (HPA) axis: A contemporary synthesis. Rev. Endocr. Metab. Disord. 2021;22:179–204. doi: 10.1007/s11154-020-09611-3. [DOI] [PubMed] [Google Scholar]
- 4.Buffolo F., Tetti M., Mulatero P., Monticone S. Aldosterone as a mediator of cardiovascular damage. Hypertension. 2022;79:1899–1911. doi: 10.1161/HYPERTENSIONAHA.122.17964. [DOI] [PubMed] [Google Scholar]
- 5.Takeda Y. Vascular synthesis of aldosterone: Role in hypertension. Mol. Cell Endocrinol. 2004;217:75–79. doi: 10.1016/j.mce.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 6.Gomez-Sanchez E.P., Gomez-Sanchez C.M., Plonczynski M., Gomez-Sanchez C.E. Aldosterone synthesis in the brain contributes to Dahl salt-sensitive rat hypertension. Exp. Physiol. 2010;95:120–130. doi: 10.1113/expphysiol.2009.048900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Briones A.M., Nguyen Dinh Cat A., Callera G.E., Yogi A., Burger D., He Y., Corrêa J.W., Gagnon A.M., Gomez-Sanchez C.E., Gomez-Sanchez E.P., et al. Adipocytes produce aldosterone through calcineurin-dependent signaling pathways: Implications in diabetes mellitus-associated obesity and vascular dysfunction. Hypertension. 2012;59:1069–1078. doi: 10.1161/HYPERTENSIONAHA.111.190223. [DOI] [PubMed] [Google Scholar]
- 8.Mohamed D.M., Shaqura M., Li X., Shakibaei M., Beyer A., Treskatsch S., Schäfer M., Mousa S.A. Aldosterone synthase in peripheral sensory neurons contributes to mechanical hypersensitivity during local inflammation in rats. Anesthesiology. 2020;132:867–880. doi: 10.1097/ALN.0000000000003127. [DOI] [PubMed] [Google Scholar]
- 9.Phan T.S., Schink L., Mann J., Merk V.M., Zwicky P., Mundt S., Simon D., Kulms D., Abraham S., Legler D.F., et al. Keratinocytes control skin immune homeostasis through de novo-synthesized glucocorticoids. Sci. Adv. 2021;7:eabe0337. doi: 10.1126/sciadv.abe0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mueller M., Cima I., Noti M., Fuhrer A., Jakob S., Dubuquoy L., Schoonjans K., Brunner T. The nuclear receptor LRH-1 critically regulates extra-adrenal glucocorticoid synthesis in the intestine. J. Exp. Med. 2006;203:2057–2062. doi: 10.1084/jem.20060357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller W.L. Steroidogenesis: Unanswered questions. Trends Endocrinol. Metab. 2017;28:771–793. doi: 10.1016/j.tem.2017.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Schiffer L., Anderko S., Hannemann F., Eiden-Plach A., Bernhardt R.J. The CYP11B subfamily. J. Steroid. Biochem. Mol. Biol. 2015;151:38–51. doi: 10.1016/j.jsbmb.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 13.Van de Wiel E., Chaman Baz A.H., Küsters B., Mukai K., van Bonzel L., van Erp M., Deinum J., Langenhuijsen J. Changes of the CYP11B2 expressing zona glomerulosa in human adrenals from birth to 40 years of age. Hypertension. 2022;79:2565–2572. doi: 10.1161/HYPERTENSIONAHA.122.19052. [DOI] [PubMed] [Google Scholar]
- 14.Rosenfield R.L. Normal and premature adrenarche. Endocr. Rev. 2021;42:783–814. doi: 10.1210/endrev/bnab009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rainey W. E Adrenal zonation: Clues from 11beta-hydroxylase and aldosterone synthase. Mol. Cell. Endocrinol. 1999;151:151–160. doi: 10.1016/S0303-7207(99)00051-9. [DOI] [PubMed] [Google Scholar]
- 16.Bassett M.H., Zhang Y., White P.C., Rainey W.E. Regulation of human CYP11B2 and CYP11B1: Comparing the role of the common CRE/Ad1 element. Endocr. Res. 2000;26:941–951. doi: 10.3109/07435800009048620. [DOI] [PubMed] [Google Scholar]
- 17.Sabari B.R., Zhang D., Allis C.D., Zhao Y. Metabolic regulation of gene expression through histone acylations. Nat. Rev. Mol. Cell Biol. 2017;18:90–101. doi: 10.1038/nrm.2016.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Köhler F., Rodríguez-Paredes M. DNA methylation in epidermal differentiation, aging, and cancer. J. Investig. Dermatol. 2020;140:38–47. doi: 10.1016/j.jid.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 19.Ghanbarian H., Yıldız M.T., Tutar Y. MicroRNA targeting. Methods Mol. Biol. 2022;2257:105–130. doi: 10.1007/978-1-0716-1170-8_6. [DOI] [PubMed] [Google Scholar]
- 20.Salameh Y., Bejaoui Y., El Hajj N. DNA methylation biomarkers in aging and age-related diseases. Front Genet. 2020;11:171. doi: 10.3389/fgene.2020.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liang M. Epigenetic mechanisms and hypertension. Hypertension. 2018;72:1244–1254. doi: 10.1161/HYPERTENSIONAHA.118.11171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Demura M., Demura Y., Takeda Y., Saijoh K. Dynamic regulation of the angiotensinogen gene by DNA methylation, which is influenced by various stimuli experienced in daily life. Hypertens. Res. 2015;38:519–527. doi: 10.1038/hr.2015.42. [DOI] [PubMed] [Google Scholar]
- 23.Parry A., Rulands S., Reik W. Active turnover of DNA methylation during cell fate decisions. Nat. Rev. Genet. 2021;22:59–66. doi: 10.1038/s41576-020-00287-8. [DOI] [PubMed] [Google Scholar]
- 24.Stillman B. Histone modifications: Insights into their influence on gene expression. Cell. 2018;175:6–9. doi: 10.1016/j.cell.2018.08.032. [DOI] [PubMed] [Google Scholar]
- 25.McClure J.J., Li X., Chou C.J. Advances and challenges of HDAC inhibitors in cancer therapeutics. Adv. Cancer Res. 2018;138:183–211. doi: 10.1016/bs.acr.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 26.Gu F., Lin Y., Wang Z., Wu X., Ye Z., Wang Y., Lan H. Biological roles of LSD1 beyond its demethylase activity. Cell Mol. Life Sci. 2020;77:3341–3350. doi: 10.1007/s00018-020-03489-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang Y., Ting P.Y., Yao T.M., Homma T., Brooks D., Katayama Rangel I., Adler G.K., Romero J.R., Williams J.S., Pojoga L.H., et al. Histone demethylase LSD1 deficiency and biological sex: Impact on blood pressure and aldosterone production. J Endocrinol. 2019;240:111–122. doi: 10.1530/JOE-18-0247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takeda Y., Miyamori I., Yoneda T., Hatakeyama H., Inaba S., Furukawa K., Mabuchi H., Takeda R. Regulation of aldosterone synthase in human vascular endothelial cells by angiotensin II and adrenocorticotropin. J. Clin. Endocrinol. Metab. 1996;81:2797–2800. doi: 10.1210/jcem.81.8.8768832. [DOI] [PubMed] [Google Scholar]
- 29.Guagliardo N.A., Klein P.M., Gancayco C.A., Lu A., Leng S., Makarem R.R., Cho C., Rusin C.G., Breault D.T., Barrett P.Q., et al. Angiotensin II induces coordinated calcium bursts in aldosterone-producing adrenal rosettes. Nat. Commun. 2020;11:1679. doi: 10.1038/s41467-020-15408-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ali Y., Dohi K., Okamoto R., Katayama K., Ito M. Novel molecular mechanisms in the inhibition of adrenal aldosterone synthesis: Action of tolvaptan via vasopressin V2 receptor-independent pathway. Br. J. Pharmacol. 2019;176:1315–1327. doi: 10.1111/bph.14630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vanderriele P.E., Caroccia B., Seccia T.M., Piazza M., Lenzini L., Torresan F., Iacobone M., Unger T., Rossi G.P. The angiotensin type 2 receptor in the human adrenocortical zona glomerulosa and in aldosterone-producing adenoma: Low expression and no functional role. Clin. Sci. 2018;132:627–640. doi: 10.1042/CS20171593. [DOI] [PubMed] [Google Scholar]
- 32.Lauber M., Boni-Schnetzler M., Miiller J. Potassium raises cytochrome P-450 mRNA level in zona glomerulosa of rat adrenals. Mol. Cell Endocrinol. 1990;72:159–166. doi: 10.1016/0303-7207(90)90140-4. [DOI] [PubMed] [Google Scholar]
- 33.Holland O.B., Carr B. Modulation of aldosterone synthase messenger ribonucleic acid levels by dietary sodium and potassium and by adrenocorticotropin. Endocrinology. 1993;132:2666–2673. doi: 10.1210/endo.132.6.8389287. [DOI] [PubMed] [Google Scholar]
- 34.Peters B., Teubner P., Clausmeyer S., Puschner T., Maser-Gluth C., Wrede H.J., Kränzlin B., Peters J. StAR expression and the long-term aldosterone response to high-potassium diet in Wistar-Kyoto and spontaneously hypertensive rats. Am. J. Physiol. Endocrinol. Metab. 2007;292:E16–E23. doi: 10.1152/ajpendo.00454.2005. [DOI] [PubMed] [Google Scholar]
- 35.Demura M., Wang F., Yoneda T., Karashima S., Mori S., Oe M., Kometani M., Sawamura T., Cheng Y., Maeda Y., et al. Multiple noncoding exons 1 of nuclear receptors NR4A family (nerve growth factor-induced clone B, Nur-related factor 1 and neuron-derived orphan receptor 1) and NR5A1 (steroidogenic factor 1) in human cardiovascular and adrenal tissues. J. Hypertens. 2011;29:1185–1195. doi: 10.1097/HJH.0b013e32834626bb. [DOI] [PubMed] [Google Scholar]
- 36.Dierks A.D., Urs D., Lichtenauer U.D., Sackmann S., Spyroglou A., Shapiro I., Geyer M., Manonopoulou J., Reincke M., Hantel C., et al. Identification of adrenal genes regulated in a potassium-dependent manner. J. Mol. Endocrinol. 2010;45:193–206. doi: 10.1677/JME-09-0171. [DOI] [PubMed] [Google Scholar]
- 37.Takeda Y., Demura M., Wang F., Karashima S., Yoneda T., Kometani M., Hashimoto A., Aono D., Horike S., Meguro-Horike M., et al. Epigenetic regulation of aldosterone synthase gene by sodium and angiotensin II. J. Am. Heart Assoc. 2018;7:e008281. doi: 10.1161/JAHA.117.008281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang F., Demura M., Cheng Y., Zhu A., Karashima S., Yoneda T., Demura Y., Maeda Y., Namiki M., Ono K., et al. Dynamic CCAAT/enhancer binding protein-associated changes of DNA methylation in the angiotensinogen gene. Hypertension. 2014;63:281–288. doi: 10.1161/HYPERTENSIONAHA.113.02303. [DOI] [PubMed] [Google Scholar]
- 39.Takeda Y., Demura M., Wang F., Karashima S., Yoneda T., Kometani M., Aomo D., Hashimoto A., Horike S., Meguro-Horike M., et al. Effect of potassium on DNA methylation of aldosterone synthase gene. J. Hypertens. 2021;39:1018–1024. doi: 10.1097/HJH.0000000000002742. [DOI] [PubMed] [Google Scholar]
- 40.Edwards J.R., Yarychkivska O., Boulard M., Bestor T.H. DNA methylation and DNA methyltransferases. Epigenetics Chromatin. 2017;8:10–23. doi: 10.1186/s13072-017-0130-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nogueira E.F., Vargas C.A., Otis M., Gallo-Payet N.G., Bollag W.B., Rainey W.E. Angiotensin-II acute regulation of rapid response genes in human, bovine, and rat adrenocortical cells. J. Molec. Endocrinol. 2007;39:365–374. doi: 10.1677/JME-07-0094. [DOI] [PubMed] [Google Scholar]
- 42.Nishimoto K., Harris R.B.S., Rainey W.E., Seki T. Sodium deficiency regulates rat adrenal zona glomerulosa gene expression. Endocrinology. 2014;155:1363–1372. doi: 10.1210/en.2013-1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carey R.M. Aldosterone and cardiovascular disease. Curr. Opin. Endocrinol. Diabetes Obes. 2010;17:194–198. doi: 10.1097/MED.0b013e3283390fa4. [DOI] [PubMed] [Google Scholar]
- 44.Reincke M., Bancos I., Mulatero P., Scholl U.I., Stowasser M., Williams T.A. Diagnosis and treatment of primary aldosteronism. Lancet Diabetes Endocrinol. 2021;9:876–892. doi: 10.1016/S2213-8587(21)00210-2. [DOI] [PubMed] [Google Scholar]
- 45.Lyubarova R., Gosmanova E.O. Mineralocorticoid receptor blockade in end-stage renal disease. Curr. Hypertens. Rep. 2017;19:40. doi: 10.1007/s11906-017-0737-y. [DOI] [PubMed] [Google Scholar]
- 46.Gao X., Yamazaki Y., Tezuka Y., Omata K., Ono Y., Morimoto R., Nakamura Y., Suzuki T., Satoh F., Sasano H. Pathology of Aldosterone Biosynthesis and its Action. Tohoku J. Exp. Med. 2021;254:1–15. doi: 10.1620/tjem.254.1. [DOI] [PubMed] [Google Scholar]
- 47.Mogi M. Aldosterone breakthrough from a pharmacological perspective. Hypertens Res. 2022;45:967–997. doi: 10.1038/s41440-022-00913-4. [DOI] [PubMed] [Google Scholar]
- 48.Vergaro G., Passino C., Emdin M.J. No aldosterone breakthrough with the neprilysin inhibitor sacubitril. Am. Coll. Cardiol. 2019;73:3037–3038. doi: 10.1016/j.jacc.2019.03.508. [DOI] [PubMed] [Google Scholar]
- 49.Takeda Y. Effects of eplerenone, a selective mineralocorticoid receptor antagonist, on clinical and experimental salt-sensitive hypertension. Hypertens. Res. 2009;32:321–324. doi: 10.1038/hr.2009.29. [DOI] [PubMed] [Google Scholar]
- 50.Hashimoto A., Takeda Y., Karashima S., Kometani M., Aono D., Higashikata T., Konishi S., Yoneda T., Takeda Y. Impact of mineralocorticoid receptor blockade with direct renin inhibition in angiotensin II-dependent hypertensive mice. Hypertens. Res. 2020;43:1099–1104. doi: 10.1038/s41440-020-0458-5. [DOI] [PubMed] [Google Scholar]
- 51.Hughes-Austin J.M., Rifkin D.E., Beben T., Katz R., Sarnak M.J., Deo R., Hoofnagle A.N., Homma S., Siscovick D.S., Sotoodehnia N., et al. The relation of serum potassium concentration with cardiovascular events and mortality in community-living individuals. Clin. J. Am. Soc. Nephrol. 2017;12:245–252. doi: 10.2215/CJN.06290616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Weir M.R., Bushinsky D.A., Benton W.W., Woods S.D., Mayo M.R., Arthur S.P., Pitt B., Bakris G.L. Effect of patiromer on hyperkalemia recurrence in older chronic kidney disease patients taking RAAS inhibitors. Am. J. Med. 2018;131:555–564. doi: 10.1016/j.amjmed.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 53.Sakthiswary R., Wong M., Nor Azmi K. Spot urine potassium as a potential screening test for aldosterone breakthrough. Clin. Ter. 2012;163:195–198. [PubMed] [Google Scholar]
- 54.Vaidya A., Mulatero P., Baudrand R., Adler G.K. The expanding spectrum of primary aldosteronism: Implications for diagnosis, pathogenesis, and treatment. Endocr Rev. 2018;39:1057–1088. doi: 10.1210/er.2018-00139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Funder J.W., Carey R.M. Primary aldosteronism: Where are we now? Where to from here? Hypertension. 2022;79:726–735. doi: 10.1161/HYPERTENSIONAHA.121.18761. [DOI] [PubMed] [Google Scholar]
- 56.Howard B., Wang Y., Xekouki P., Faucz F.R., Jain M., Zhang L., Meltzer P.G., Stratakis C.A., Kebebew E. Integrated analysis of genome-wide methylation and gene expression shows epigenetic regulation of CYP11B2 in aldosteronomas. J. Clin. Endocrinol. Metab. 2014;99:E536–E543. doi: 10.1210/jc.2013-3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Takeda Y., Demura N., Yoneda T., Takeda Y. DNA Methylation of the Angiotensinogen Gene, AGT, and the Aldosterone Synthase Gene, CYP11B2 in Cardiovascular Diseases. Int. J. Mol. Sci. 2021;22:4587. doi: 10.3390/ijms22094587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Di Dalmazi G., Morandi L., Rubin B., Pilon C., Asioli S., Vicennati V., De Leo A., Ambrosi F., Santini D., Pagotto U., et al. DNA methylation of steroidogenic enzymes in benign adrenocortical tumors: New insights in aldosterone-producing adenomas. J. Clin. Endocrinol. Metab. 2020;105:dgaa585. doi: 10.1210/clinem/dgaa585. [DOI] [PubMed] [Google Scholar]
- 59.Yoshii Y., Oki K., Gomez-Sanchez C.E., Ohno H., Itcho K., Kobuke K., Yoneda M. Hypomethylation of CYP11B2 in aldosterone-producing adenoma. Hypertension. 2016;68:1432–1437. doi: 10.1161/HYPERTENSIONAHA.116.08313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nishimoto K., Seki T., Kurihara I., Yokota K., Omura M., Nishikawa T., Shibata H., Kosaka T., Oya M., Suematsu M., et al. Case report: Nodule development from subcapsular aldosterone producing cell clusters causes hyperaldosteronism. J. Clin. Endocrinol. Metab. 2016;101:6–9. doi: 10.1210/jc.2015-3285. [DOI] [PubMed] [Google Scholar]
- 61.Murakami M., Yoshimoto T., Nakabayashi K., Nakano Y., Fukaishi T., Tsuchiya K., Minami I., Bouchi R., Okamura K., Fujii Y., et al. Molecular characteristics of the KCNJ5 mutated aldosterone-producing adenomas. Endocr. Relat. Cancer. 2017;24:531–541. doi: 10.1530/ERC-17-0117. [DOI] [PubMed] [Google Scholar]
- 62.De Sousa K., Boulkroun S., Baron S., Nanba K., Wack M., Rainey W.E., Rocha A., Giscos-Douriez I., Meatchi T., Amar L., et al. Genetic, cellular, and molecular heterogeneity in adrenals with aldosterone-p ne-producing adenoma. Hypertension. 2020;75:1034–1044. doi: 10.1161/HYPERTENSIONAHA.119.14177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Omata K., Anand S.K., Hovelson D.H., Liu C.J., Yamazaki Y., Nakamura Y., Ito S., Satoh F., Sasano H., Rainey W.E., et al. Aldosterone-producing cell clusters frequently harbor somatic mutations and accumulate with age in mormal adrenals. J. Endocr. Soc. 2017;1:787–799. doi: 10.1210/js.2017-00134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sun N., Meyer L.S., Feuchtinger A., Kunzke T., Knösel T., Reincke M., Walch A., Williams T.A. Mass spectrometry imaging establishes 2 distinct metabolic phenotypes of aldosterone-producing cell clusters in primary aldosteronism. Hypertension. 2020;75:634–644. doi: 10.1161/HYPERTENSIONAHA.119.14041. [DOI] [PubMed] [Google Scholar]
- 65.Rossi G.P. Primary aldosteronism: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2019;74:2799–2811. doi: 10.1016/j.jacc.2019.09.057. [DOI] [PubMed] [Google Scholar]
- 66.Vaidya A., Hundemer G.L., Nanba K., Parksook W.W., Brown J.M. Primary aldosteronism: State-of-the-art review. Am. J. Hypertens. 2022;35:967–988. doi: 10.1093/ajh/hpac079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fischer E., Beuschlein F., Degenhart C., Jung P., Bidlingmaier M., Reincke M. Spontaneous remission of idiopathic aldosteronism after long-term treatment with spironolactone: Results from the German Conn’s Registry. Clin. Endocrinol. 2012;76:473–477. doi: 10.1111/j.1365-2265.2011.04243.x. [DOI] [PubMed] [Google Scholar]
- 68.Yoneda T., Demura M., Takata H., Kometani M., Karashima S., Yamagishi M., Takeda Y. Unilateral primary aldosteronism with spontaneous remission after long-term spironolactone therapy. J. Clin. Endocrinol. Metab. 2012;97:1109–1113. doi: 10.1210/jc.2011-2563. [DOI] [PubMed] [Google Scholar]
- 69.Ye P., Yamashita T., Pollock D.M., Sasano H., Rainey W.E. Contrasting effects of eplerenone and spironolactone on adrenal cell steroidogenesis. Horm. Metab. Res. 2009;41:35–39. doi: 10.1055/s-0028-1087188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.MacKenzie S.M., Connell J.M., Davies E. Non-adrenal synthesis of aldosterone: A reality check. Mol. Cell. Endocrinol. 2012;350:163–167. doi: 10.1016/j.mce.2011.06.026. [DOI] [PubMed] [Google Scholar]
- 71.Takeda Y. Role of cardiovascular aldosterone in hypertension. Curr. Med. Chem. Cardiovasc. Hematol. Agents. 2005;3:261–266. doi: 10.2174/1568016054368151. [DOI] [PubMed] [Google Scholar]
- 72.Fujisaki M., Nagoshi T., Nishikawa T., Date T., Yoshimura M. Rapid induction of aldosterone synthesis in cultured neonatal rat cardiomyocytes under high glucose conditions. Biomed. Res. Int. 2013;2013:161396. doi: 10.1155/2013/161396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Takata H., Takeda Y., Zhu A., Cheng Y., Yoneda T., Demura M., Yagi K., Karashima S., Yamagishi M. Protective effects of mineralocorticoid receptor blockade against neuropathy in experimental diabetic rats. Diabetes Obes. Metab. 2012;14:155–162. doi: 10.1111/j.1463-1326.2011.01499.x. [DOI] [PubMed] [Google Scholar]
- 74.Tsybouleva N., Zhang L., Chen S., Patel R., Lutucuta S., Nemoto S., De Freitas G., Entman M., Carabello B.A., Roberts R., et al. Aldosterone, through novel signaling proteins, is a fundamental molecular bridge between the genetic defect and the cardiac phenotype of hypertrophic cardiomyopathy. Circulation. 2009;109:1284–1291. doi: 10.1161/01.CIR.0000121426.43044.2B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Takeda Y., Yoneda T., Demura M., Usukura M., Mabuchi H. Calcineurin inhibition attenuates mineralocorticoid-induced cardiac hypertrophy. Circulation. 2002;105:677–679. doi: 10.1161/hc0602.104675. [DOI] [PubMed] [Google Scholar]
- 76.Garnier A., Bendall J.K., Fuchs S., Escoubet B., Rochais F., Hoerter J., Delcayre C. Cardiac specific increase in aldosterone production induces coronary dysfunction in aldosterone synthase-transgenic mice. Circulation. 2004;110:1819–1825. doi: 10.1161/01.CIR.0000142858.44680.27. [DOI] [PubMed] [Google Scholar]
- 77.Alesutan I., Voelkl J., Feger M., Kratschmar D.V., Castor T., Mia S., Sacherer M., Viereck R., Borst O., Leibrock C., et al. Involvement of vascular aldosterone synthase in phosphate-induced osteogenic transformation of vascular smooth muscle cells. Sci. Rep. 2017;7:2059. doi: 10.1038/s41598-017-01882-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Takeda Y., Yoneda T., Demura M., Miyamori I., Mabuchi H. Cardiac aldosterone production in genetically hypertensive rats. Hypertension. 2000;36:495–500. doi: 10.1161/01.HYP.36.4.495. [DOI] [PubMed] [Google Scholar]
- 79.Yoshimura M., Nakamura S., Ito T., Nakayama M., Harada E., Mizuno Y., Sakamoto T., Yamamuro M., Saito Y., Nakao K., et al. Expression of aldosterone synthase gene in failing human heart: Quantitative analysis using modified real-time polymerase chain reaction. J. Clin. Endocrinol. Metab. 2002;87:3936–3940. doi: 10.1210/jcem.87.8.8731. [DOI] [PubMed] [Google Scholar]
- 80.Kater C.E., Giorgi R.B., Costa-Barbosa F.A. Classic and current concepts in adrenal steroidogenesis: A reappraisal. Arch. Endocrinol. Metab. 2022;66:77–87. doi: 10.20945/2359-3997000000438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Slominski R.M., Tuckey R.C., Manna P.R., Jetten A.M., Postlethwaite A., Raman C., Slominski A.T. Extra-adrenal glucocorticoid biosynthesis: Implications for autoimmune and inflammatory disorders. Genes. Immun. 2020;21:150–168. doi: 10.1038/s41435-020-0096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Takeda Y., Miyamori I., Yoneda T., Iki K., Hatakeyama H., Blair I.A., Hsieh F.Y., Takeda R. Synthesis of corticosterone in the vascular wall. Endocrinology. 1994;135:2283–2286. doi: 10.1210/endo.135.5.7956952. [DOI] [PubMed] [Google Scholar]
- 83.Salehzadeh M., Soma K. K Glucocorticoid production in the thymus and brain: Immunosteroids and neurosteroids. Brain Behav Immun. Health. 2021;18:100352. doi: 10.1016/j.bbih.2021.100352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bassett M.H., Mayhew B., Rehman K., White P.C., Mantero F., Arnaldi G., Stewart P.M., Bujalska I., Rainey W.E. Expression profiles for steroidogenic enzymes in adrenocortical disease. J. Clin. Endocrinol. Metab. 2005;90:5446–5455. doi: 10.1210/jc.2005-0836. [DOI] [PubMed] [Google Scholar]
- 85.Kubota-Nakayama F., Nakamura Y., Konosu-Fukaya S., Azmahani A., Ise K., Yamazaki Y., Kitawaki Y., Felizola S.J., Ono Y., Omata K., et al. Expression of steroidogenic enzymes and their transcription factors in cortisol-producing adrenocortical adenomas: Immunohistochemical analysis and quantitative real-time polymerase chain reaction studies. Hum. Pathol. 2016;54:165–173. doi: 10.1016/j.humpath.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 86.Ahn C.H., Na H.Y., Park S.Y., Yu H.W., Kim S.J., Choi J.Y., Lee K.E., Kim S.W., Jung K.C., Kim J.H. Expression of CYP11B1 and CYP11B2 in adrenal adenoma correlates with clinical characteristics of primary aldosteronism. Clin. Endocrinol. 2022;96:30–39. doi: 10.1111/cen.14628. [DOI] [PubMed] [Google Scholar]
- 87.Liu J., Li X.-D., Vaheri A., Voutilainen R. DNA methylation affects cell proliferation, cortisol secretion and steroidogenic gene expression in human adrenocortical NCI-H295R cells. J. Mol. Endocrinol. 2004;33:651–662. doi: 10.1677/jme.1.01560. [DOI] [PubMed] [Google Scholar]
- 88.Kometani M., Yoneda T., Demura M., Koide H., Nishimoto K., Mukai K., Gomez-Sanchez C.E., Akagi T., Yokota T., Horike S.I., et al. Cortisol overproduction results from DNA methylation of CYP11B1 in hypercortisolemia. Sci. Rep. 2017;7:11205. doi: 10.1038/s41598-017-11435-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ronchi C.L., Di Dalmazi G., Faillot S., Sbiera S., Assié G., Weigand I., Calebiro D., Schwarzmayr T., Appenzeller S., Rubin B., et al. Genetic landscape of sporadic unilateral adrenocortical adenomas without PRKACA p.leu 206arg mutation. J. Clin. Endocrinol. Metab. 2016;101:3526–3538. doi: 10.1210/jc.2016-1586. [DOI] [PubMed] [Google Scholar]
- 90.Yanase T., Oki Y., Katabami T., Otsuki M., Kageyama K., Tanaka T., Kawate H., Tanabe M., Doi M., Akehi Y., et al. New diagnostic criteria of adrenal subclinical Cushing’s syndrome: Opinion from the Japan Endocrine Society. Endocr. J. 2018;65:83–393. doi: 10.1507/endocrj.EJ17-0456. [DOI] [PubMed] [Google Scholar]
- 91.Abe I., Sugimoto K., Miyajima T., Ide T., Minezaki M., Takeshita K., Takahara S., Nakagawa M., Fujimura Y., Kudo T., et al. Clinical investigation of adrenal incidentalomas in Japanese patients of the fukuoka Rregion with updated diagnostic criteria for sub-clinical Cushing’s syndrome. Intern. Med. 2018;57:2467–2472. doi: 10.2169/internalmedicine.0550-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ichijo T., Ueshiba H., Nawata H., Yanase T. A nationwide survey of adrenal incidentalomas in Japan: The first report of clinical and epidemiological features. Endocr. J. 2020;67:141–152. doi: 10.1507/endocrj.EJ18-0486. [DOI] [PubMed] [Google Scholar]
- 93.Katabami T., Matsuba R., Kobayashi H., Nakagawa T., Kurihara I., Ichijo T., Tsuiki M., Wada N., Ogawa Y., Sone M., et al. Primary aldosteronism with mild autonomous cortisol secretion increases renal complication risk. Eur. J. Endocrinol. 2022;186:645–655. doi: 10.1530/EJE-21-1131. [DOI] [PubMed] [Google Scholar]
- 94.Arlt W., Lang K., Sitch A.J., Dietz A.S., Rhayem Y., Bancos I., Feuchtinger A., Chortis V., Gilligan L.C., Ludwig P., et al. Steroid metabolome analysis reveals prevalent glucocorticoid excess in primary aldosteronism. JCI Insight. 2017;2:e93136. doi: 10.1172/jci.insight.93136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Akehi Y., Yanase T., Motonaga R., Umakoshi H., Tsuiki M., Takeda Y., Yoneda T., Kurihara I., Itoh H., Katabami T., et al. Japan Primary Aldosteronism Study Group. High prevalence of diabetes in patients with primary aldosteronism (PA) associated with subclinical hypercortisolism and prediabetes more prevalent in bilateral than unilateral PA: A large, multicenter cohort study in Japan. Diabetes Care. 2019;42:938–945. doi: 10.2337/dc18-1293. [DOI] [PubMed] [Google Scholar]
- 96.Inoue K., Horikoshi H., Omura M., Tsurutani Y., Saito J., Nishikawa T. Association between aldosterone and hypertension among patients with overt and subclinical hypercortisolism. J. Endoc. Soc. 2023;7:bvac167. doi: 10.1210/jendso/bvac167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Nusrin S., Tong S.K., Chaturvedi G., Wu R.S., Giesy J.P., Kong R.Y. Regulation of CYP11B1 and CYP11B2 steroidogenic genes by hypoxia-inducible miR-10b in H295R cells. Mar. Pollut. Bull. 2014;85:344–351. doi: 10.1016/j.marpolbul.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 98.Robertson S., MacKenzie S.M., Alvarez-Madrazo S., Diver L.A., Lin J., Stewart P.M., Fraser R., Connell J.M., Davies E. MicroRNA-24 is a novel regulator of aldosterone and cortisol production in the human adrenal cortex. Hypertension. 2013;62:572–578. doi: 10.1161/HYPERTENSIONAHA.113.01102. [DOI] [PubMed] [Google Scholar]
- 99.Lenzini L., Caroccia B., Campos A.G., Fassina A., Belloni A.S., Seccia T.M., Kuppusamy M., Ferraro S., Skander G., Bader M., et al. Lower expression of the TWIK-related acid-sensitive K+ channel 2 (TASK-2) gene is a hallmark of aldosterone-producing adenoma causing human primary aldosteronism. J. Clin. Endocrinol. Metab. 2014;99:E674–E682. doi: 10.1210/jc.2013-2900. [DOI] [PubMed] [Google Scholar]
- 100.Vetrivel S., Zhang R., Engel M., Oßwald A., Watts D., Chen A., Wielockx B., Sbiera S., Reincke M., Riester A. Characterization of adrenal miRNA-based dysregulations in Cushing’s syndrome. Int. J. Mol. Sci. 2022;23:7676. doi: 10.3390/ijms23147676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Sugino N. Molecular mechanisms of luteinization. Obstet. Gynecol. Sci. 2014;57:93–101. doi: 10.5468/ogs.2014.57.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Okada M., Lee L., Maekawa R., Sato S., Kajimura T., Shinagawa M., Tamura T., Taketani T., Asada H., Tamura H., et al. Epigenetic changes of the cyp11a1 promoter region in granulosa cells undergoing luteinization during ovulation in female rats. Endocrinology. 2016;157:3344–3354. doi: 10.1210/en.2016-1264. [DOI] [PubMed] [Google Scholar]
- 103.Li H., Chen Y., Yan L., Qiao J. Increased expression of P450scc and CYP17 in development of endogenous hyperandrogenism in a rat model of PCOS. Endocrine. 2013;43:184–190. doi: 10.1007/s12020-012-9739-3. [DOI] [PubMed] [Google Scholar]
- 104.Krasic J., Fucic A., Sincic N., Sindicic Dessardo N., Starcevic M., Guszak V., Ceppi M., Bruzzone M., Kralik S. Comparison of estradiol, testostosterone, and CYP19 methylation levels between full-term and preterm newborns. Horm. Res. Paediatr. 2021;94:168–175. doi: 10.1159/000518112. [DOI] [PubMed] [Google Scholar]
- 105.Spitschak M., Vanselow J. Bovine large luteal cells show increasing de novo DNA methylation of the main ovarian CYP19A1 promoter P2. Gen. Comp. Endocrinol. 2012;178:7–45. doi: 10.1016/j.ygcen.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 106.Ding Y., He F., Wen H., Li J., Ni M., Chi M., Qian K., Bu Y., Zhang D., Si Y., et al. DNA methylation status of cyp17-II gene correlated with its expression pattern and reproductive endocrinology during ovarian development stages of Japanese flounder (Paralichthys olivaceus) Gene. 2013;527:82–88. doi: 10.1016/j.gene.2013.05.037. [DOI] [PubMed] [Google Scholar]