Abstract
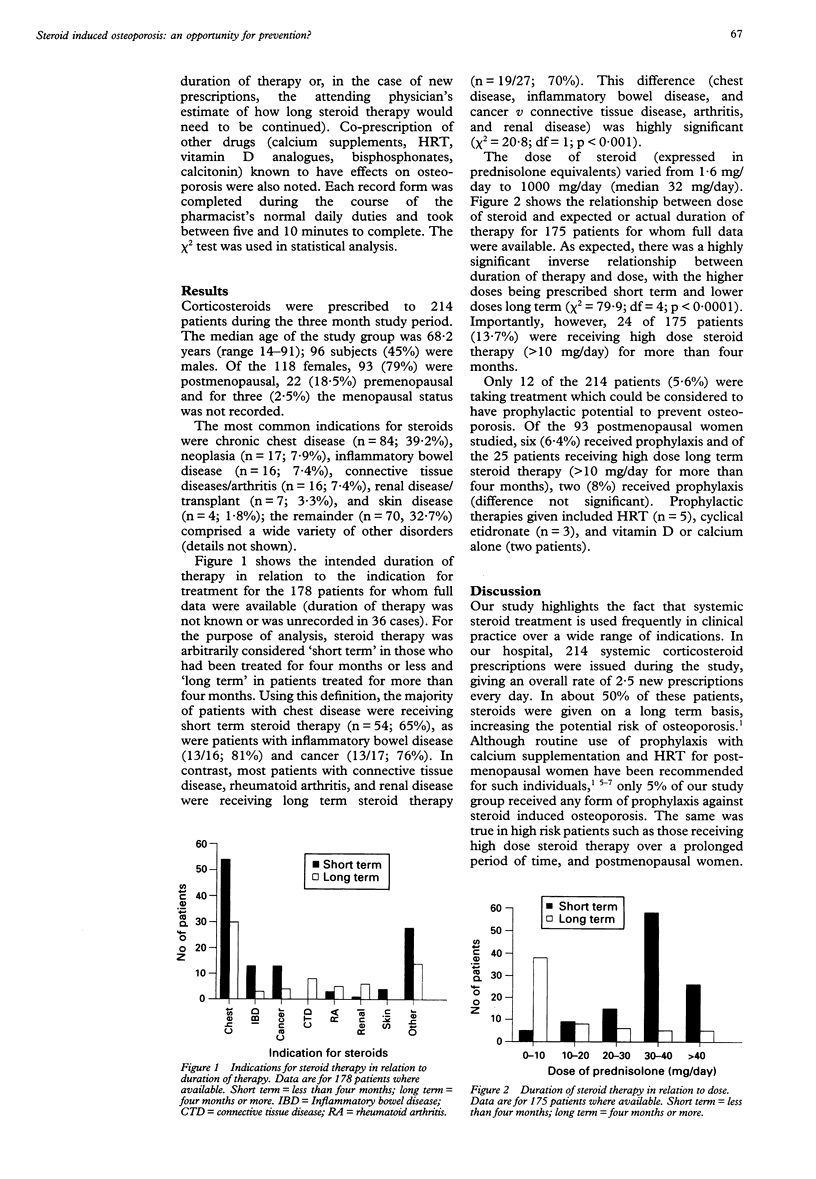
OBJECTIVE--To determine the frequency with which osteoporosis prophylaxis is given to corticosteroid treated hospital inpatients. METHODS--All patients receiving systemic corticosteroids in a large teaching hospital over a three month period were identified through routine prescription monitoring by hospital ward pharmacists. Coprescription of antiosteoporotic therapy was recorded, along with other relevant details such as steroid dose, actual, or intended duration of therapy, and indication for therapy. RESULTS--Corticosteroids were prescribed to 214 patients over the study period, giving an average rate of 2.5 new prescriptions each day. Indications included: chest disease (n = 84; 39.2%), cancer (n = 17; 7.9%), inflammatory bowel disease (n = 16; 7.5%), rheumatoid arthritis/connective tissue disease (n = 16; 7.5%), and renal diseases (n = 7; 3.3%). One hundred and twelve patients (52.3%) were receiving short term steroid therapy (less than four months); 66 (37%) were receiving medium/long term steroid therapy (four months or more). In 36 cases (16.8%) the duration of therapy was unknown. Only 12 of the 214 patients (5.6%) received any form of osteoporosis prophylaxis. The prevalence of prophylaxis was similarly low in postmenopausal women (six of 93; 6.4%) and in patients receiving high dose long term steroid therapy (two of 25; 8%). CONCLUSIONS--Systemic corticosteroids are used frequently in hospital practice for a wide range of indications, but few patients receive co-prescription of prophylaxis against osteoporosis. This is true even in high risk groups such as postmenopausal women and those on high dose long term steroid therapy. Identification of individuals by the mechanism used in this study provides an opportunity by which all corticosteroid treated patients could be detected and offered osteoporosis prophylaxis before serious loss of bone density has occurred.
Full text
PDF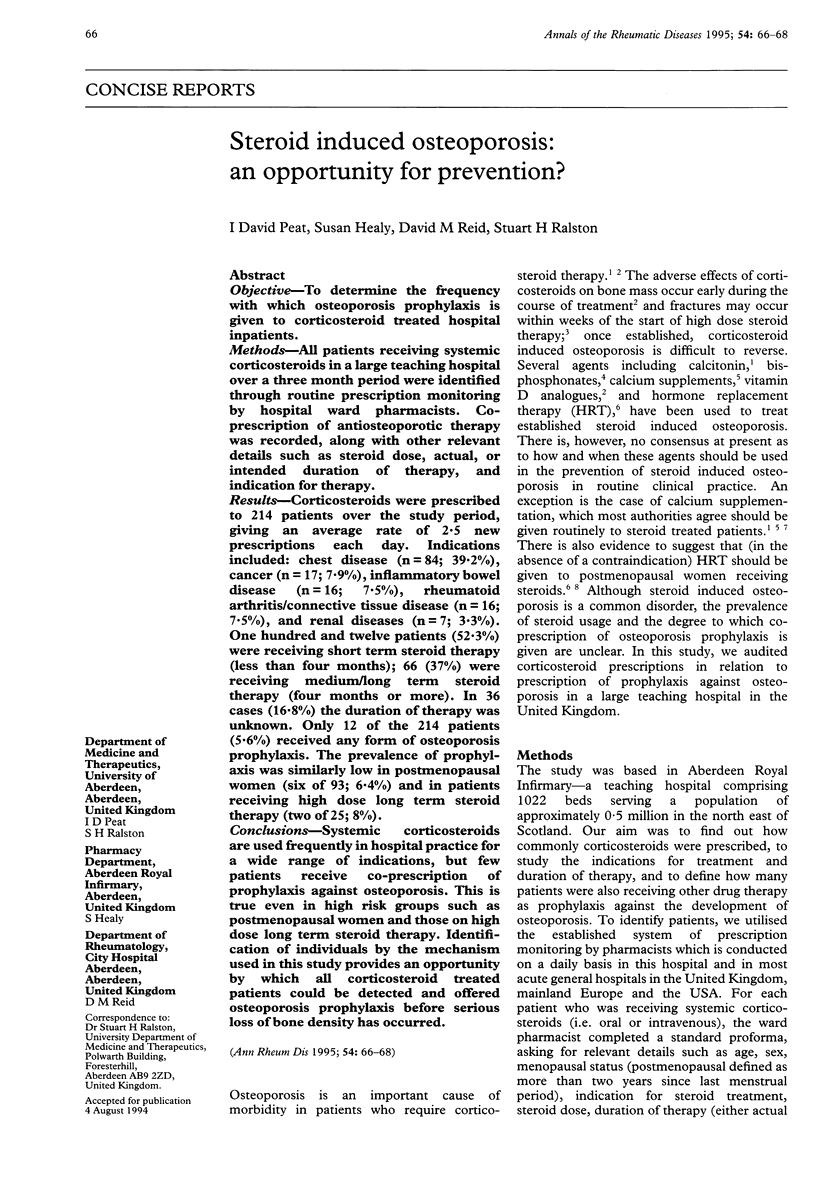

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BOLAND E. W., HEADLEY N. E. Management of rheumatoid arthritis with smaller (maintenance) doses of cortisone acetate. J Am Med Assoc. 1950 Sep 30;144(5):365–372. doi: 10.1001/jama.1950.02920050005002. [DOI] [PubMed] [Google Scholar]
- Bath P. M., Prasad A., Brown M. M., MacGregor G. A. Survey of use of anticoagulation in patients with atrial fibrillation. BMJ. 1993 Oct 23;307(6911):1045–1045. doi: 10.1136/bmj.307.6911.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukert B. P., Johnson B. E., Robinson R. G. Estrogen and progesterone replacement therapy reduces glucocorticoid-induced bone loss. J Bone Miner Res. 1992 Sep;7(9):1063–1069. doi: 10.1002/jbmr.5650070909. [DOI] [PubMed] [Google Scholar]
- Meunier P. J. Is steroid-induced osteoporosis preventable? N Engl J Med. 1993 Jun 17;328(24):1781–1782. doi: 10.1056/NEJM199306173282411. [DOI] [PubMed] [Google Scholar]
- Mulder H., Struys A. Intermittent cyclical etidronate in the prevention of corticosteroid-induced bone loss. Br J Rheumatol. 1994 Apr;33(4):348–350. doi: 10.1093/rheumatology/33.4.348. [DOI] [PubMed] [Google Scholar]
- Reid I. R., Ibbertson H. K. Calcium supplements in the prevention of steroid-induced osteoporosis. Am J Clin Nutr. 1986 Aug;44(2):287–290. doi: 10.1093/ajcn/44.2.287. [DOI] [PubMed] [Google Scholar]
- Reid I. R., King A. R., Alexander C. J., Ibbertson H. K. Prevention of steroid-induced osteoporosis with (3-amino-1-hydroxypropylidene)-1,1-bisphosphonate (APD). Lancet. 1988 Jan 23;1(8578):143–146. doi: 10.1016/s0140-6736(88)92721-3. [DOI] [PubMed] [Google Scholar]
- Sambrook P., Birmingham J., Kelly P., Kempler S., Nguyen T., Pocock N., Eisman J. Prevention of corticosteroid osteoporosis. A comparison of calcium, calcitriol, and calcitonin. N Engl J Med. 1993 Jun 17;328(24):1747–1752. doi: 10.1056/NEJM199306173282404. [DOI] [PubMed] [Google Scholar]


