Abstract
Over the years, several distinct pathogenic coronaviruses have emerged, including the pandemic SARS-CoV-2, which is difficult to curtail despite the availability of licensed vaccines. The difficulty in managing SARS-CoV-2 is linked to changes in the variants’ proteins, especially in the spike protein (SP) used for viral entry. These mutations, especially in the SP, enable the virus to evade immune responses induced by natural infection or vaccination. However, some parts of the SP in the S1 subunit and the S2 subunit are considered conserved among coronaviruses. In this review, we will discuss the epitopes in the SARS-CoV-2 S1 and S2 subunit proteins that have been demonstrated by various studies to be conserved among coronaviruses and may be immunogenic for the development of a vaccine. Considering the higher conservancy of the S2, we will further discuss the likely challenges that could limit the S2 subunit from inducing robust immune responses and the promising approaches to increase its immunogenicity.
Keywords: SARS-CoV-2, vaccine, spike protein, mutation, conserved epitopes
1. Introduction
In the history of humans, the Coronavirus disease (COVID-19) caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has made an indelible mark characterized by a contagious respiratory pandemic [1,2]. Consequently, 660 million cases and approximately 6.6 million deaths have been reported as of December 2022 [3]. Since its emergence, studies have been focusing on developing preventive and therapeutic measures against this disease, and several vaccines have been licensed [4,5]. However, the constant mutation of the SARS-CoV-2 virus, which results in different variants, narrows the effectiveness of the licensed vaccines against SARS-CoV-2 infections, thus suggesting a needed continuous effort in developing a SARS-CoV-2 universal vaccine [6]. Besides the pandemic caused by SARS-CoV-2, other human coronaviruses (huCoVs) including human CoV (HCoV)-229E (1962), HCoV-OC43 (1967), SARS-CoV (2002), HCoV-NL63 (2004), HCoV-HKUI (2005), Middle East respiratory syndrome coronavirus (MERS)-CoV (2012) and SARS-CoV-2 (2019) have been implicated in different outbreaks since the start of the 21st century [7,8,9,10,11]. Although the trend of the emergence of coronaviruses remains unclear, adequate preparation must be made for a possible emerging or re-emerging strain. In this case, developing an effective universal vaccine against CoVs should take advantage of the conserved portions of the virus, especially the spike protein (SP).
Levels of similarities have been observed among the emerged CoVs [12,13,14]. For instance, the SARS-CoV-2 viral genome sequence analysis revealed its phylogenetic similarity with SARS-CoV (79%) and MERS-CoV (50%) [15,16,17]. Like other betacoronaviruses, the SARS-CoV-2 genome consists of 27 proteins encoded by 14 open reading frames (ORF), including non-structural proteins (nsp) that are encoded by the ORF 1 and 2 present at the 5′-terminal regions [18,19]. More importantly, the SARS-CoV-2 structural proteins, notably the SP, envelope protein (E), membrane protein (M), nucleocapsid (N) and eight accessory proteins encoded by the 3′-terminal region of the genomes, are in like manner with other betacoronaviruses [19].
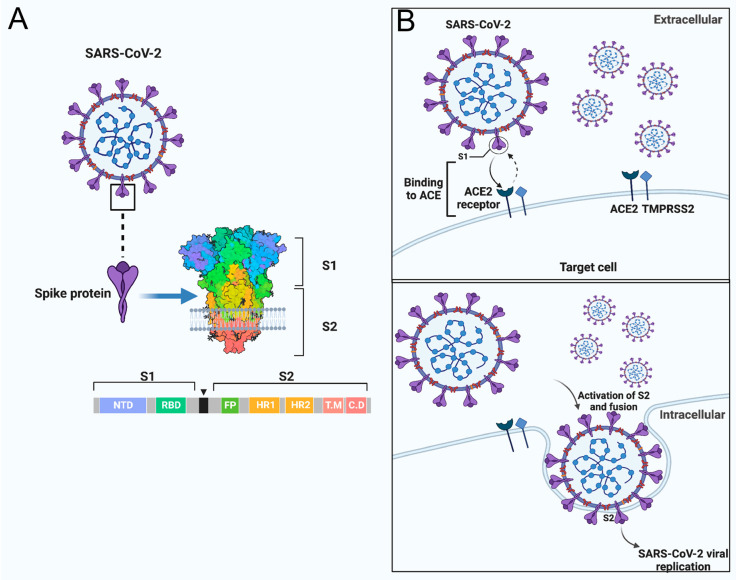
Sequence analysis of the SARS-CoV-2 SP revealed a close association with SARS-CoV regarding amino acid composition as well as comparable binding affinity to human angiotensin-converting enzyme 2 (hACE2) [20,21]. The SP, which is a highly N-glycosylated class I transmembrane fusion protein, plays a critical role during coronavirus infection. The SP mediates the attachment of the virus into the cell receptor and facilitates the viral-host membrane fusion [22,23]. The SP also assembles into trimers on the virus surface and cleaves into two subunits, S1 and S2, during the cell infection [24,25]. The large protein S1 domain contains the RBD that is responsible for binding to the host cell receptor and varies extensively in all isolates of the CoVs [20,24,25]. Meanwhile, the S2 domain, which facilitates the virus-cell fusion, is made up of the fusion peptide (FP) and heptad repeat regions (HR1 and HR2), which are conserved among the isolates of the CoVs [26,27], the conserved membrane-proximal external region (MPER) and the transmembrane domain (TM) [28,29,30,31,32,33,34]. After the binding of the S1 RBD domain to the ACE2, the S2 subunit then inserts its FP into the cell membrane leading to the assemblage of the HR1 and HR2 into a six-helix structure to drive the cellular and viral membrane closely together for viral entry (Figure 1) [35]. Notably, the major determinant of cell tropism in most coronaviruses is typically linked to the structure of the SP [21,25,36,37,38,39,40]. Phylogenetic, bioinformatic and homology structural modelling analyses showed that the RBD of SARS-CoV-2 only has 64% shared identity with the SARS-CoV, while the NTD has 51% similarity [41]. However, the study revealed that within the S2, the fusion protein (FP) is 93% identical and the HR1 is 88% identical, while the HR2 and the TM are respectively 100% and 93% similar.
Figure 1.
SARS-CoV-2 cell entry into the target cell. (A) SARS-CoV-2 virus with its SP. The SP contains the S1 and the S2 subunit. The S1 subunit comprises the NTD and RBD, while the S2 comprises the FP, HR1 and HR2. (B) The schematic summary of SARS-CoV-2 cell entry. SARS-CoV-2 binds to the host ACE receptor using the RBD domain of the S1 (upper panel). After the activation of the S2, SARS-CoV-2 uses the FP and HR for fusion and gains entry into the host (lower panel) [35,42]. Image created by Biorender.com. Adapted from “SARS-CoV-2 Targeting of ACE2 Receptor and Entry in Infected Cell” and “An In-depth Look into the Structure of the SARS-CoV2 Spike Glycoprotein”, by BioRender.com (Accessed on 22 February 2023). Retrieved from https://app.biorender.com/biorender-templates.
SARS-CoV-2 and other SARS-related coronaviruses (e.g., SARS-CoV) can utilize distinct domains within the S1 subunit to identify different attachment and entry receptors in the host cell surface [20,40]. For instance, the differences in the SPs of the known huCoVs contribute to their difference in pathogenesis and the site of infection (lower or upper respiratory) [36]. Taking a closer look at SARS-CoV-2 as an example, Laporte et al. described that the higher transmissibility experienced with the SARS-CoV-2 compared to other human coronaviruses is due to its abundant replication in the upper respiratory tracts [43]. They mentioned that the SARS-CoV-2 SP has an intrinsic temperature preference of 33 °C, like the temperature of human respiratory tracts, instead of the 37 °C required by other human CoVs. In addition to this, it was revealed that the SARS-CoV-2 has multiple cell entry activators, including TMPRSS2 and TMPRSS13 protease, broadening its tropism. As mentioned by Korber et al., a D614G mutation observed in the SARS-CoV-2 variant S1 also resulted in the wider spread of the virus at different geographical regions with higher viral loads in the respiratory tracts [44]. These differences observed in the SP of the CoVs contribute to the difficulties in developing a sustainable vaccine against the emerging variants of SARS-CoV-2. It is therefore a necessity to develop a vaccine that can prevent the spread of all present or emerging variants of SARS-CoV-2.
Notably, certain conserved epitopes in the S1 and S2 regions can be utilized to develop universal vaccines against CoV infections [45,46,47]. However, some varying challenges surround these conserved epitopes, including the presence of immunodominant epitopes [45], weak immunogens and non-neutralizing antibodies [47]. This review aims to shed light on the conserved epitopes capable of inducing a broad immune response against multiple CoVs and highlight how to circumvent the associated possible challenges with lessons gleaned from SARS-CoV-2.
2. Impact of Mutations on the SARS-CoV-2 SP to the Evasion and Resistance of Immune Responses
Understanding the possible ways by which the SARS-CoV-2 SP escapes immune responses will shed light on the importance of using the conserved regions of the SP in developing a universal vaccine against variants of coronaviruses. The SARS-CoV-2 SP has been demonstrated to regulate the innate immune response through the activation of the NF-κB pathway in human macrophages and monocytes, thus increasing the production of inflammatory responses (IL-8) [22]. Continuous mutation of the SARS-CoV-2 SP impacts innate immune responses and could further increase virulence, pathogenicity and immune evasion of the virus given that one of the strategies by which SARS-CoV-2 evades immune response is through cytokine shock [48,49]. Noteworthily, mutations in the SARS-CoV-2 ORF8 (which could modulate the SP during transmission) have been associated with inhibition of the Major Histocompatibility Complex (MHC)-1 stimulation, thus leading to the low production of cytotoxic T cells (CD8+ T cells) [50,51,52]. In our study, the SARS-CoV-2 Delta variant SP had the highest potential of stimulating the NF-κB pathway in macrophages to induce inflammatory cytokines in the monocyte-derived macrophages (MDMs) and monocyte-derived dendritic cells (MDDCs) when compared with the Wuhan strains or D614G variants. This suggests that continuous mutation of the SARS-CoV-2 SP also impacts innate immune responses and could further increase virulence, pathogenicity and immune evasion of the virus [48].
The adaptive immune response regarded as the second line of defence during infection is regulated by the antigen-presenting cells (APCs) and comprises the antibodies (B cells), T helper cells (CD4+ T cell) and CD8+ T cells [53]. In the case of SARS-CoV-2 infection, the DCs present peptides derived from the SP on the MHC-I or II for the activation of the specific T-cells (CD4+ and CD8+) [54]. The SARS-CoV-2 specific CD4+ T and CD8+ T cells help to trigger the induction of SARS-CoV-2 specific B cells that further generate most of the neutralizing antibodies as well as memory B cells and long-term humoral immunity. They also regulate antiviral activities, recruit innate cells, kill infected cells, and facilitate tissue repair [53,55,56,57,58,59]. Notably, among the SARS-CoV-2 structural proteins, the SP is the most promising antigen for the induction of neutralizing antibodies (including IgM, IgA and IgG) and cell-mediated immune responses (including CD4+ T, CD8+ T cells and T follicular helper cells (Tfh)) during COVID-19 disease [60,61,62,63,64,65,66,67,68].
However, the SARS-CoV-2 SP could escape humoral immune responses and neutralizing antibodies because of mutations in its genetic constituent, thus leading to the ineffectiveness of vaccine-induced immunity [21,69]. Vaccine development against SARS-CoV-2, like all other vaccines, depends on the induction of neutralizing, adaptive, and memory immune responses. Although the current COVID-19 vaccine reduces the severity of the disease, the re-infection of SARS-CoV-2 in previously infected people or fully vaccinated individuals has been well-documented, suggesting that the sterilizing immunity towards SARS-CoV-2 is partial, short-lived and narrow [70,71,72].
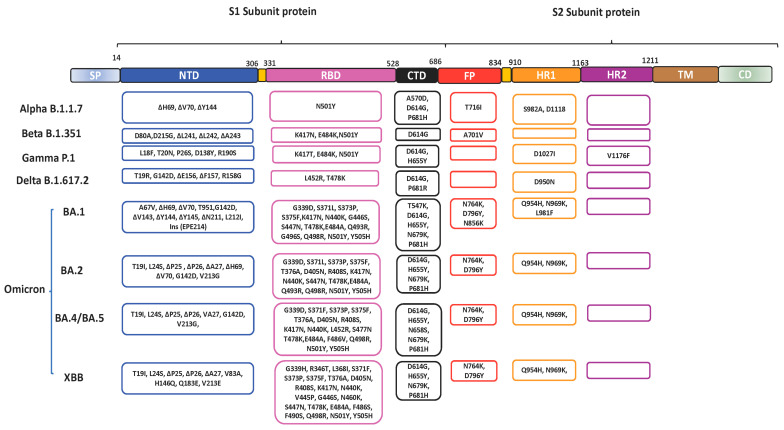
Since the emergence of the SARS-CoV-2 virus in 2019, various variants have emerged with mutations leading to amino acid changes in the SP which contribute largely to immune evasion [73,74]. Most of the mutations are found in the S1 subunit protein. SARS-CoV-2 variants include the: Alpha, having the N501Y mutation in RBD; Beta, having N501Y, K417N and E484K mutations in the RBD; Gamma, with N501Y, K417T and E484K; Delta, having T478K and L452 in the RBD and Omicron with S371L, G339D, S375F, S373P, K417N, N440K, S477N, G446S, E484A, T478K, Q493K, Q498R, G496S, N501Y and Y505H in the RBD (Figure 2) [74,75]. Among all, Omicron variants and subvariants contain the highest number of changes in the SP relative to the ancestral virus. Compared to the wild type, Delta has 9 mutations, including 3 RBD mutations (K417N, E484Q and L452R) and D614G in the SP, whereas Omicron has more than 32 mutations in the SP with 15 mutations in the RBD, thus influencing its transmissibility and infectivity [76]. The T95I, N211I, V213R, Y505H, N786K and N856K mutations in Omicron variants contribute to its pathogenicity and virulence [77]. Sub-variants of Omicron have also been identified as BA.1, BA.2, BA.2.12.1, BA.2.3, BA.2.9, BA.3, XBB, BA.4, BA.5 (BQ.1, BQ.1.1, BF.7 and BA.4.6) and recombinant BA.1/BA.2 [78,79]. The BA.2 progressively replaced BA.1, which was the most prevalent globally, while BA.3 spread is restricted. The BA.4 and BA.5, which were first isolated in South Africa, replaced the BA.2 variant, having mutations F486V and R493Q and deletion in positions 69 and 70 in the RBD [80,81].
Figure 2.
The schematic structure of the SARS-CoV-2 spike protein showing the mutations on the spike protein of selected SARS-CoV-2 variants of concern (VOC) including Alpha, Beta, Delta, Gamma and Omicron [6].
The mutations on the RBD impact its ability to bind with the host ACE2 receptors. For instance, the RBD of the SARS-CoV-2 has a greater affinity for the hACE2 than the RBD of SARS-CoV due to the differences in their amino acids [24]. These following mutations have been identified as the RBD mutations of concern present in the VOCs resulting in the compromising of immune responses by the Food and Drug Agency (FDA): P337H/L/R/T, K417E/N, E484K/Q/P/D, N439K, K444Q, S494P, V445A, N450D, L452R, Y453F, E340A/K/G, L455F, F486V, N460K/S/T, D420N, V483A, F490S, Q493K/R and N501Y/T [82]. The Omicron subvariants shared many mutations among themselves including the P681H, H655Y, N679K and D614G mutations in the S1 subunit; G339D, S371L/F, S373P, S375F, K417N, N440K, S477N, T478K, E484A, Q498R, N501Y and Y505H in RBD; G142D in N-terminal domain (NTD) and N969K, N764K, D796Y and Q954H in the S2 subunit (Figure 2) [83]. Omicron BA.1 and BA.2 have 12 common mutations on the RBD, which are G339D, S373P, S375F, K417N, N440K, S477N, T478K, E484A, Q498R, Q493R, N501Y and Y505H, whereas BA.2 has a total of 31 mutations in the SP including the unique R408S, and S371F (Figure 2). However, the BA.3 also has unique mutations T376A and D405N in the RBD [81].
A study by Hoffmann et al. showed that the Delta variant with E484Q mutation on the RBD had a reduced neutralizing sensitivity to bamlanivimab or plasma from vaccinated patients [84]. Moreover, the N439K has been demonstrated by Thomson et al. to enhance infectivity and escape humoral immune response by enhancing the binding of the RBD to hACE2 [85]. Interestingly, before the emergence of the Omicron variant, a CR3022-neutralizing antibody isolated from a SARS-CoV-2 convalescent patient was revealed to target highly conserved epitopes of the RBD of SARS-CoV-2 and SARS-CoV [73]. However, with the emergence of the Omicron variants which contain 15 mutations on the RBD, the sensitivity of CR3022 was reduced [86]. Aside from the impacts of the mutations on the RBD in the escape of the immune response, the D614G mutation on the non-RBD of the S1, found in most VOCs, also contributes to the enhancement of the virulence and immune evasion of SARS-CoV-2 variants [22,44].
Therefore, it is not surprising to find that other variants of SARS-CoV-2, such as Beta (B.1.351), Gamma (B.1.1.28), Delta (B.1.617.2) and especially Omicron (B.1.1.529), substantially escape the immune responses induced by the licensed vaccines [22,86,87,88]. Supportably, a report showed that 21 out of 33 people that have been vaccinated 3 times with the licensed vaccine were still susceptible to the Omicron variants’ infection [89]. By using a pseudotyped lentivirus system [90], a study also revealed that the Omicron SP had 26-fold resistance to neutralizing antibodies among the convalescent donor and 26- to 34-fold resistance to antibodies elicited by the Pfizer BNT162b2 and Moderna two dosage vaccines. In addition, the Omicron spike resisted most therapeutic antibodies except sotrovimab and evaded immune responses induced in the individual vaccinated with BNT162b2, with 12–44-fold resistance compared to the Delta variant. Similarly, the third dosage of BNT162b2 or vaccination with ChAdOx1 induced neutralizing antibodies against the Omicron, but fewer than against the Delta [91]. The observed compromise of the immune response by the variants is particularly due to the mutations on the RBD of the S1 [89,92].
Importantly, the Omicron BA.1, BA.2 and BA.3 are very good at escaping immune responses induced by natural infection or by one or two doses of the vaccine, while a third dose can give some protection [79,93,94]. Although the SARS-CoV-2 bivalent vaccine (wildtype and Omicron) can provide long-term protection, a BA.1 derived vaccine may not provide broad protection against SARS-CoV-2 variants [95]. Furthermore, the Omicron BA.4, BA.5 and BA.2.12.1 have been demonstrated to show more immune-response escape strategies than the BA.1 and BA.2 due to the presence of the F486V and D405N mutations [86,95]. Cao et al. [95] demonstrated that, structurally, the SP of BA.4, BA.5 and BA.2.12.1 have the same binding affinity with the ACE-2. They further revealed that BA.4, BA.5 and BA.2.12.1 could evade neutralizing antibodies from the plasma of BA.1 infected immunized patients or triple-vaccinated individuals to a greater extent than BA.2.
The SARS-CoV-2 S2 subunit protein also has about 12 mutations which are not shared among the variants and may influence the immune evasion of SARS-CoV-2 [96]. Nevertheless, the S2 region is less affected by the spontaneous mutation because of its importance in the fusion process that leads to infection [97]. Indeed, despite the variation impacted by mutations of the SP of the CoVs, some certain epitopes that could induce neutralizing antibodies, memory B cells and memory T cell responses remain conserved in the S1 and S2 subunits across the CoVs. Therefore, attention should be placed on these conserved regions for developing a universal vaccine.
3. SARS-CoV-2 S Conserved Regions as a Potential Target for Vaccine Development
Developing a vaccine for viruses with multiple strains or variants tends to take advantage of the conserved epitopes present in the virus. Conserved epitopes are epitopes that are relatively the same among different strains of a pathogen. For example, due to the multiple strains of influenza over the years, the means of developing a universal vaccine has been the use of the conserved epitopes on the hemagglutinin (HA stalk) or the matrix ectodomain (M2e) [98,99,100,101,102,103,104]. The strategy of using conserved epitopes has also been used in the development of preventative vaccines for HIV, dengue virus, Lassa fever virus (LASV), hepatitis virus and Kaposi’s sarcoma-associated herpesvirus (KSHV) [105,106,107,108,109,110,111,112,113]. Therefore, identifying the conserved regions in the SP of SARS-CoV variants will be of great importance in developing a universal vaccine against CoVs. Although mutations in SARS-CoV-2 had a great impact on the SP, studies have revealed that certain conserved epitopes in S1 can induce neutralizing antibodies [114]. Interestingly, some monoclonal antibodies (including 7B11, 18F3, S309 and its Fab, S315, 154C, S304, 240C and VHH-72) that recognize SARS-CoV and MERS-CoV could cross-react and cross-neutralize SARS-CoV-2 by recognizing the ACE2 binding sites on the SARS-CoV-2 RBD [115].
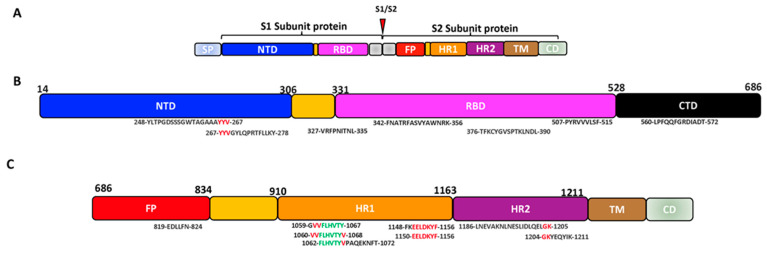
Jaiswal et al. mathematically (in-house developed PERL scripts) revealed sets of epitopes on the S1 subunit around 453 to 538 that interact with the ACE and are 99% conserved among the variants of SARS-CoV-2 [116]. Their study further identified conserved common neutralizing epitopes on the SARS-CoV-2, including YLTPGDSSSGWTAGAAAYYV (247–267 aa), TFKCYGVSPTKLNDL (376–390 aa) on S1 and LNEVAKNLNESLIDLQELGK (1186–1205 aa) on the S2 [116]. A recent immunoinformatic study predicted conserved and highly immunogenic CTL-induced epitopes on S1 VRFPNITNL (327–335 aa) and PYRVVVLSF (507–515 aa) (Table 1), while the CTL-induced epitopes on S2 were identified to be VVFLHVTYV (1060–1068 aa) and GVVFLHVTY (1059–1067 aa) (Table 2) [117]. Based on the conservancy, antigenicity, allergenicity, population coverage and transmembrane location, another study chose potential conserved epitopes from the S1 (FNATRFASVYAWNRK, 342–356 aa) (Table 1), S2 (FLHVTYVPAQEKNFT, 1062–1072 aa) (Table 2) and the E/M protein to construct a SARS-CoV-2 vaccine and revealed that it had high immunogenicity and broad neutralizing activity against the SARS-CoV-2 RBD (Figure 3) [118]. Jiang et al., with web-based analytic tools, also predicted potential T cell epitopes induced by the SARS-CoV-2 SP and narrowed them down to CD4 or CD8 T cell epitopes using ELIspot and a cytolytic assay [119]. In their observation, YYVGYLQPRTFLLKY (264–278 aa), located at the end of the NTD and the upstream of the RBD, is highly conserved among 11 variants of SARS-CoV-2 VOCs and variants of interest (VOIs) and could induce the T cells. Further studies also suggested that these epitopes could be well recognized by most HLA alleles globally [119].
Table 1.
Some predicted conserved epitopes on the SARS-CoV-2 S1 subunit that could induce neutralizing antibodies and/or adaptive immune responses.
| Conserved Epitopes | Position | Immune Response Induced | Type of Study | Refs. | |
|---|---|---|---|---|---|
| B cells/Neutralizing antibodies | T cells | ||||
| YLTPGDSSSGWTAGAAAYYV | 248–267 aa | Yes | Yes | Mathematically (in-house developed PERL scripts), in vivo | [116,120] |
| YYVGYLQPRTFLLKY | 264–278 aa | NT | Yes | Web-based analytic tools | [119] |
| VRFPNITNL | 327–335 aa | NT | Yes | Immunoinformatic, in vivo | [117,121] |
| FNATRFASVYAWNRK | 342–356 aa | Yes | Yes | In silico, T-cell epitope mapping, molecular dynamics simulations, immunoinformatic | [118,122,123] |
| TFKCYGVSPTKLNDL | 376–390 aa | Yes | Yes | Mathematically (in-house developed PERL scripts), bioinformatics, monoclonal antibody targeting | [116,124] |
| PYRVVVLSF | 507–515 aa | NT | Yes | Immunoinformatic | [117] |
| LPFQQFGRDIADT | 560–572 aa | Yes | Yes | PepSeq Analysis | [125] |
NT—Not tested.
Table 2.
Some predicted conserved epitopes on the SARS-CoV-2 S2 subunit that could induce neutralizing antibodies and/or adaptive immune responses.
| Conserved Epitopes | Position | Immune Response Induced | Type of Study | Refs. | |
|---|---|---|---|---|---|
| Neutralizing antibodies | T cells | ||||
| EDLLFN | 819–824 aa | Yes | NT | Epitope-resolved profiling, structural and functional test | [125,126] |
| EELDKYF | 1150–1156 aa | Yes | NT | Epitope-resolved profiling, structural and functional | [125,126] |
| GVVFLHVTY | 1059–1067 aa | NT | Yes | Immunoinformatic | [117,127] |
| VVFLHVTYV | 1060–1068 aa | NT | Yes | Immunoinformatic | [117,127] |
| FLHVTYVPAQEKNFT | 1062–1072 aa | Yes | Yes | In silico, in vivo | [118] |
| SPDVDLGDISGINAS | 1161–1175 aa | Yes | NT | In vivo | [128] |
| LNEVAKNLNESLIDLQELGK | 1186–1205 aa | Yes | Yes | Mathematically (in-house developed PERL scripts), bioinformatic, in vivo | [116,120,129] |
| GKYEQYIK | 1204–1211 aa | NT | NT | Antiviral inhibitory activity | [34] |
NT—Not tested.
Figure 3.
The schematic representation of some possible conserved epitopes on the SARS-CoV-2 SP (Black: positions occurring in a set of predicted epitopes; Red: positions occurring in 2 sets of predicted epitopes; Green: positions present in 3 sets of predicted epitopes). (A) Schematic structure of the SARS-CoV-2 spike protein. (B) Structure of the SARS-CoV-2 S1 subunit showing the conserved epitopes on the NTD and RBD. (C) Structure of the SARS-CoV-2 S2 subunit showing the conserved epitopes on the FP and HR.
Considering the role played by the S2 subunit during SARS-CoV-2 infection, it could also be targeted to induce immune responses against SARS-CoV-2. Interestingly, Ladner et al. generated an epitope-resolved analysis of IgG cross-reactivity among all CoVs in COVID-19-negative and recovered patients using a highly multiplexed peptide assay (PepSeq) and discovered that the epitopes at the FP, which is 93% similar among strains of betacoronaviruses and alphacoronaviruses, produced broadly neutralizing antibodies against the endemic coronaviruses, including SARS-CoV, MERS-CoV and SARS-CoV-2 [41,125]. Likewise, the HR2 region of the S2 is 100% conserved among the variants of the SARS-CoV-2 [41,128]. The S2 subunit proteins could also induce cross-reactive antibodies against the SARS-CoV SP and the endemic CoVs [130]. The S2 has been reported to induce neutralizing antibodies or T cell responses targeting the FP proximal region and HR2 domain of S2 in COVID-19 patients or animals vaccinated or infected with different CoVs [131,132,133,134]. Interestingly, due to prior population exposure to common cold coronaviruses, nAbs and memory B and T cells against SARS-CoV-2 were found in some individuals who have never been infected by SARS-CoV-2 [135,136]. Pre-existing antibodies against conserved epitopes of S2, such as residues 901–906, 810–816, 851–856, 1040–1044 and 1205–1212, showed the greatest cross-reactivity and hindered SARS-CoV-2 entry into cells [135]. Other identified regions that are most widely recognized among SARS-CoV-2 linear epitopes in convalescent donors are EELDKYF (1150–1156 aa) within the stem helix of the HR2 terminal and EDLLFN (819–824 aa), which overlaps the FP and is adjacent to the S2 cleavage [125,126]. Moreover, a study conducted by Song et al. revealed that monoclonal antibody CC9.3 isolated from individuals before SARS-CoV-2 infection was characterized to recognize the S2 subunit of the SARS-CoV-2 and other huCoVs [137].
From the sera of patients recovered from SARS-CoV-2, Pinto et al. isolated five monoclonal antibodies that could recognize the stem-helix (SH) of the S2 subunits of other betacoronaviruses including the OC43 strain [126]. In addition, Lu et al. identified and crystallized T cell follicle helper cells (cTfh) among patients that recovered from the mild symptoms of COVID-19 and revealed that these cTfh could recognize SARS-CoV-2 S2 subunit epitopes (864–882 aa) that are conserved among the emerging variants [57]. In a recent publication, Wu et al. identified a monoclonal antibody hMab5.17 that could recognize the SARS-CoV-2 HR2 domain that is adjacent to TM (SPDVDLGDISGINAS; 1161–1175 aa) and could protect against SARS-CoV-2 in the Syrian hamster. They further cloned the mAb hMab5.17 and demonstrated that it could neutralize SARS-CoV-2 variants [128].
Another highly conserved region located at S2 region is the SARS-CoV-2 MPER-like region (MPER) (GKYEQYIK; 1204–1211 aa), which has great potential for being used as an antigen for broadly neutralizing antibodies (bnAbs) [34,76,138]. Yu et al. have demonstrated that a cholesterol-conjugated lipopeptide containing SARS-CoV-2 MPER prepared by using cholesteryl succinate monoester could inhibit viral entry, indicating the importance of MPER in viral entry and fusion [34]. Like the MPER of HIV-1, the MPER of SARS-CoV-2 could possibly induce bnAbs against the variants of SARS-CoV-2. Studies have shown that bnAbs 4E10, 2F5, 10E8 and LN01 could interact with the MPER of the HIV-1 gp41 to prevent infection [139,140,141]. Likewise, the SARS-CoV-2 MPER could be a suitable immunogen for inducing neutralizing antibodies [34,138].
The above findings suggested that the S2 subunit of the SARS-CoV-2 is conserved among the previous strains of human coronaviruses and the SARS-CoV-2 variants and can induce cross-reactive antibodies.
4. Possible Challenges and Promising Approaches with the Conserved SARS-CoV-2 S2 Subunit in Vaccine Development
Structural positioning and immunodominance: The structural positioning of the S2 subunit might limit its ability to induce sterilizing immunity. The S2 is hidden under the S1 subunit protein, thereby being masked by the S1 subunit protein, resulting in the induction of weak immune responses during natural infection or when the whole spike protein is used in the vaccine development [142]. Studies have demonstrated that a vaccine targeting the S2 can induce IgG, but in a lesser amount when compared with the S1 subunit protein [143,144]. Wang et al. also demonstrated that the S1 of MERS-CoV in a DNA-based vaccine regimen elicited more neutralizing antibodies than the S2 subunit of the MERS-CoV vaccine [145,146]. Notably, the S1 could induce stronger neutralizing antibodies, but they might not be as broad due to mutation; however, the S2 neutralizing epitopes can induce broader neutralizing antibodies, but they may not be as strong as the S1 epitopes. Using an in vitro pseudotyped neutralization assay, a study revealed that combined human monoclonal antibodies against the HR1, HR2 and S1 of SARS-CoV had better cell-entry inhibition compared with the human monoclonal antibody against HR2. Interestingly, human monoclonal antibodies against HR1 or HR2 of the SARS-CoV have more broadly neutralization activity against different strains of human coronaviruses than the monoclonal antibodies of the S1 ectodomain [147], suggesting the SARS-CoV S2 subunit protein is a very promising epitope for developing a universal vaccine against the various strains of coronaviruses.
The immunodominance epitopes on the S1 subunit protein could also contribute to the induction of immune responses toward the S2. The analysis of the immunodominant and immunoprevalent SARS-CoV-2 epitopes of CD4 T cell or CD8 T cell revealed that SARS-CoV-2 has conserved immunodominant epitopes in the SP, M and the ORF1 [148,149,150]. Three immunodominant epitopes (TRFASVYAWNRKRISNCVAD; 345–364 aa, DEVRQIAPGQTGKIADYNYK; 420–439 aa and ERDISTEIYQAGSTPCNGVE; 480–499 aa) located at the SARS-CoV-2 RBD have been identified [151]. The epitopes 350VYAWN354 and 407VRQIAP412 are highly conserved for the variants of SARS-CoV-2 and SARS-CoV, while 473YQAGSTP479 within the RBD is only conserved among strains of SARS-CoV. In addition, Polyiam et al. also highlighted some immunodominant epitopes in the SARS-CoV-2 RBD, including NNLDSKVGGNYNYLYRLFRKSNLKPFERDISTEIYQAGST (439–478 aa.) and LFRKSNLKPFERDISTEIYQAGST (455–478 aa.) [152].
Short epitopes and low immunogenicity: Another possible challenge for using the S2 subunit protein as a universal vaccine is the shortness of the highly conserved epitopes in the S2 subunit. Examples include the FP (788–806 aa; 18 amino acids), HR2 (1127–1177 aa; 50 amino acids) and MPER (1204–1211 aa; 7 amino acids) [153]. These epitopes are too short to induce immune response except if they are used with adjuvants or fused with other immunogenic proteins as observed in the influenza HA stalk universal vaccine designs [102,104,154].
Despite the concerns mentioned above and other associated concerns, such as the antibody binding affinity, weak immunogenicity, etc., there are possible ways to increase the immunogenicity of the S2 protein.
Repeating epitopes or multiple epitopes: The fusion of the conserved epitopes can be used to develop an immunogen to induce broad and neutralizing antibodies. As observed in the licensed dengue multi-epitope-based vaccine Dengvaxia®, which carries the prM and E genes of different dengue virus serotypes, a high amount of B cells and T cells are induced [155]. We have also generated influenza vaccines that carried M2 ectodomains and/or HA stalk epitopes and could protect mice from influenza H1N1 and H3N2 challenges. In this study, four M2e sequences from human (two copies), swine (one copy) and bird (one copy) were fused by a GGG linker to form tM2e, while a copy of M2e from the human influenza strain was combined with the conserved regions of the HA stalk using a GSA linker to form HM2e. Then the tM2e or HM2e was further fused with an Ebola glycoprotein dendritic cell (DC)-targeting domain (E∆M) to form E∆M-tM2e or E∆M-HM2e, respectively. Animal studies showed that VSV carrying E∆M-tM2e or E∆M-HM2e mediated rapid and potent induction of M2 or/and HA antibodies in mice sera and mucosa [104]. This technique can also be used to fuse the selected conserved epitopes in the S1 region and/or S2 region into a multi-epitope-based vaccine.
Dendritic cell (DC)-targeting approach: The development of a vaccine using the DC-targeting approach has recently gained much attention [154,156,157]. Targeting SARS-CoV-2 S2 conserved antigens to antigen-presenting cells (APCs) could increase the immunogenicity of the antigens. In a study by Marlin et al., the SARS-CoV-2 RBD was targeted to the cluster of differentiation (CD)-40 (αCD40.RBD) to increase the immunogenicity of the RBD [158]. The formed vaccine candidate αCD40.RBD induced significantly high amounts of T and B cells in humanized mice, while a single dose of the αCD40.RBD rapidly increased broadly neutralizing antibodies in previously SARS-CoV-2-exposed convalescent non-human primates. Moreover, CoVs SPs can also be targeted to DCs by using CpG or CD205 (DEC-205) to increase the immunogenicity of the SPs [154,159]. Our recent publication has demonstrated another technology for targeting DCs with the use of the DC targeting domain of the Ebola GP [68,160,161]. We demonstrated that targeting the SARS-CoV-2 S2 subunit protein to DCs using the DC-targeting domain of the Ebola glycoprotein could induce protective immune responses in hamsters [68].
The use of adjuvants: Adjuvants, such as chemokine encoding plasmids, co-stimulatory molecule encoding plasmids, plasmids encoding pathogen-recognition receptor (PRR) ligands and immune-signalling molecules, can be incorporated into plasmids and either co-express with SARS-CoV-2 antigens or be administered separately during immunization [162]. Hui et al. demonstrated that the co-expression of IL-2 with the SARS-CoV S protein in a DNA vaccine increased the immunogenicity of the SP by inducing a higher amount of IgG than the SARS-CoV S protein alone [163]. In addition, their study revealed that the electroporation method of immunization had better immune responses than intramuscular or oral administration. Gary et al. also demonstrated that the co-formulation of the plasmid-encoded mucosal chemokine cutaneous T cell-attracting chemokine (pCTACK; CCL27) with the SARS-CoV-2 SP in a DNA vaccine increased the immunogenicity against SARS-CoV-2 and conferred 100% protection against the Delta VOC in mice [164]. An adjuvant can also act as a delivery system, e.g., the nanoparticles increase the immunogenicity of the conserved S2 epitopes to boost T cells’ and B cells’ immune responses [165,166,167]. The LNP-based vaccine can induce both Th1- and Th2-based immune responses with more dominant Th1-type B cells and biased Th2-type B cells [167,168]. Ma et al. developed a nanoparticle-based vaccine with the fusion of the self-assembling 24-mer ferritin with the RBD and HR or the RBD alone [147]. They showed that nanoparticle immunization in rhesus hACE2 transgenic mice reduced the lung viral loads and induced persistent neutralizing antibodies, T cells and B cells in rhesus macaques [166].
The routes of administration: The effectiveness of vaccines also depends on the route of administration. Routes of vaccine administration include oral, intranasal, intramuscular and subcutaneous [169]. The route of vaccine delivery may affect the protection conferred by the vaccine. The current route of SARS-CoV-2 vaccine administration is intramuscularly, however, intranasal vaccination that targets the local mucosal site of infection would be preferable. Although intramuscular vaccination can induce systemic immune responses, the induced immune responses can only get to the low respiratory tracts and not the upper respiratory tracts, while intranasal immunization can induce immune responses to both the upper and lower part [170,171]. Moreover, the intranasal delivery of the SARS-CoV-2 S2 can induce memory T cells and IgA within the nasal mucosal, as well as systemic IgG antibodies [68,172]. Neutralizing antibodies produced at the site of infection can immediately protect against the further spread of the virus into the body. Hassan et al. [173] demonstrated that a single dose of intranasal immunization protected the upper and respiratory tracts against SARS-CoV-2. We have also demonstrated that intranasal administration could protect against influenza in mice using a VSV-based vaccine [68]. It is important to note that the type of vaccine can additionally influence the effectiveness of intranasal vaccine delivery. The intranasal administering of DNA vaccines and human-neutralizing antibodies protected the lungs but did not reduce the viral load [174]. Oral immunization can also induce mucosal immunization against SARS-CoV-2. We have shown that oral immunization could induce substantial immune responses against SARS-CoV-2 but not as strongly as intranasal immunization (not yet published). Another study has also demonstrated that the orally delivered Saccharomyces cerevisae SARS-CoV-2-based vaccine induced mucosal immune responses and T cells in mice [175]. More investigations are still required to validate the use of intranasal or oral administrations of the SARS-CoV-2 S2-based vaccine.
5. Conclusions
Herd immunity is achieved either through natural infection and/or immunization, and it is expected to reduce or effectively eliminate the infection in a community [176]. Despite the high threshold of COVID-19 infection and massive vaccination of the public, it still seems unlikely to achieve herd immunity due to the emergence of several variants of SARS-CoV-2 [177,178,179,180]. Developing a universal vaccine against all SARS-CoV-2 variants, other endemic CoVs and potential emerging CoVs looks promising with highly conserved epitopes on the SARS-CoV-2 SP, especially the S2 subunit which can induce broadly neutralizing antibodies and humoral and cell-mediated immune responses.
Although these conserved regions in the S2 can be weak immunogens or inaccessible, these antigens can be strengthened to increase their immunogenicity in vaccine design. Moreover, intranasal delivery of the SARS-CoV-2 S2 to the mucosal may be more reliable in inducing long-term immune responses. Although different in silico, immunoinformatic or bioinformatic and immunophenotyping studies have demonstrated the presence of conserved epitopes and their immunogenicity among CoVs, more in vivo studies are required to validate the broad immunogenicity of these epitopes for viral designs. Nevertheless, the SARS-CoV-2 S2 antigen can be used to develop a universal vaccine that could neutralize variants of SARS-CoV-2 as well as other betacoronaviruses. Though S2 is very promising, neutralizing epitopes on the S1 subunit is equally important. Therefore, in designing a multi-epitope universal antigen against SARS-CoV-2 variants, the highly conserved HR2 and other identified conserved epitopes on NTD, RBD, FP and HR1 should be considered.
Author Contributions
T.A.O., Z.A. and R.U.: Writing-Original Draft Preparation; T.A.O., Z.A. and B.W.: review and revision; D.K. and X.Y. provided conceptual advice to the manuscript, reviewed and revised the paper. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing is not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
T.A.O. is a recipient of the Allan Rolland Studentship Award of the Department of Medical Microbiology and Infectious Diseases. This work was supported by the Mitacs Accelerate Award in collaboration with North Forge and Lab2Market West to X-J.Y and T.A.O. This work was also supported by the Canadian 2019 Novel Coronavirus (COVID-19) Rapid Research Funding (OV5-170710) by the Canadian Institutes of Health Research and Research Manitoba, and a CIHR COVID-19 Variant Supplement grant (VS1-175520).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Gralinski L.E., Menachery V.D. Return of the Coronavirus: 2019-nCoV. Viruses. 2020;12:135. doi: 10.3390/v12020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Worldometer Coronavirus Disease. [(accessed on 29 September 2022)]. Available online: https://www.google.com/search?q=coronavirus+death+toll&rlz=1C5CHFA_enCA1017CA1017&oq=coronavirus+death&aqs=chrome.0.0i131i433i512j69i57j0i512l8.6462j1j4&sourceid=chrome&ie=UTF-8-colocmid=/m/02j71&coasync=0.
- 4.Lopez Bernal J., Andrews N., Gower C., Gallagher E., Simmons R., Thelwall S., Stowe J., Tessier E., Groves N., Dabrera G. Effectiveness of COVID-19 vaccines against the B. 1.617. 2 (Delta) variant. N. Engl. J. Med. 2021;385:585–594. doi: 10.1056/NEJMoa2108891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar S., Saurabh M.K., Maharshi V. Efficacy and safety of potential vaccine candidates against coronavirus disease 2019: A systematic review. J. Adv. Pharm. Technol. Res. 2021;12:215. doi: 10.4103/japtr.JAPTR_229_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao F., Zai X., Zhang Z., Xu J., Chen W. Challenges and developments in universal vaccine design against SARS-CoV-2 variants. Npj Vaccines. 2022;7:1–12. doi: 10.1038/s41541-022-00597-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Den Brand J.M., Smits S.L., Haagmans B.L. Pathogenesis of Middle East respiratory syndrome coronavirus. J. Pathol. 2015;235:175–184. doi: 10.1002/path.4458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mackay I.M., Arden K.E. MERS coronavirus: Diagnostics, epidemiology and transmission. Virol. J. 2015;12:1–21. doi: 10.1186/s12985-015-0439-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alharbi N.K., Kulkarni S.S., Falzarano D. Microbial Pathogenesis. Springer; Berlin/Heidelberg, Germany: 2021. Immune Responses to MERS-CoV in Humans and Animals; pp. 85–97. [DOI] [PubMed] [Google Scholar]
- 10.Cui J., Li F., Shi Z.-L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019;17:181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cueno M.E., Imai K. Structural comparison of the SARS-CoV 2 spike protein relative to other human-infecting coronaviruses. Front. Med. 2021;7:594439. doi: 10.3389/fmed.2020.594439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Salian V.S., Wright J.A., Vedell P.T., Nair S., Li C., Kandimalla M., Tang X., Carmona Porquera E.M., Kalari K.R., Kandimalla K.K. COVID-19 transmission, current treatment, and future therapeutic strategies. Mol. Pharm. 2021;18:754–771. doi: 10.1021/acs.molpharmaceut.0c00608. [DOI] [PubMed] [Google Scholar]
- 13.Petrosillo N., Viceconte G., Ergonul O., Ippolito G., Petersen E. COVID-19, SARS and MERS: Are they closely related? Clin. Microbiol. Infect. 2020;26:729–734. doi: 10.1016/j.cmi.2020.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen Y., Liu Q., Guo D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J. Med. Virol. 2020;92:418–423. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gorbalenya A.E., Baker S.C., Baric R.S., de Groot R.J., Drosten C., Gulyaeva A.A., Haagmans B.L., Lauber C., Leontovich A.M., Neuman B.W. Severe acute respiratory syndrome-related coronavirus: The species and its viruses–a statement of the Coronavirus Study Group. Nat. Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., Wang W., Song H., Huang B., Zhu N. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beyer D.K., Forero A. Mechanisms of antiviral immune evasion of SARS-CoV-2. J. Mol. Biol. 2022;434:167265. doi: 10.1016/j.jmb.2021.167265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu A., Peng Y., Huang B., Ding X., Wang X., Niu P., Meng J., Zhu Z., Zhang Z., Wang J. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe. 2020;27:325–328. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malik Y.S., Sircar S., Bhat S., Sharun K., Dhama K., Dadar M., Tiwari R., Chaicumpa W. Emerging novel coronavirus (2019-nCoV)—Current scenario, evolutionary perspective based on genome analysis and recent developments. Vet. Q. 2020;40:68–76. doi: 10.1080/01652176.2020.1727993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lan J., Ge J., Yu J., Shan S., Zhou H., Fan S., Zhang Q., Shi X., Wang Q., Zhang L. Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor. Nature. 2020;581:215–220. doi: 10.1038/s41586-020-2180-5. [DOI] [PubMed] [Google Scholar]
- 21.Li Q., Wu J., Nie J., Zhang L., Hao H., Liu S., Zhao C., Zhang Q., Liu H., Nie L. The impact of mutations in SARS-CoV-2 spike on viral infectivity and antigenicity. Cell. 2020;182:1284–1294.e1289. doi: 10.1016/j.cell.2020.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ao Z., Ouyang M.J., Olukitibi T.A., Yao X. SARS-CoV-2 Delta spike protein enhances the viral fusogenicity and inflammatory cytokine production. Iscience. 2022;25:104759. doi: 10.1016/j.isci.2022.104759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daniloski Z., Jordan T.X., Ilmain J.K., Guo X., Bhabha G., Sanjana N.E. The Spike D614G mutation increases SARS-CoV-2 infection of multiple human cell types. Elife. 2020;10:e65365–e65379. doi: 10.7554/eLife.65365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walls A.C., Park Y.-J., Tortorici M.A., Wall A., McGuire A.T., Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020;181:281–292.e286. doi: 10.1016/j.cell.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li W., Moore M.J., Vasilieva N., Sui J., Wong S.K., Berne M.A., Somasundaran M., Sullivan J.L., Luzuriaga K., Greenough T.C. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reguera J., Mudgal G., Santiago C., Casasnovas J.M. A structural view of coronavirus–receptor interactions. Virus Res. 2014;194:3–15. doi: 10.1016/j.virusres.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang T., Bidon M., Jaimes J.A., Whittaker G.R., Daniel S. Coronavirus membrane fusion mechanism offers a potential target for antiviral development. Antivir. Res. 2020;178:104792. doi: 10.1016/j.antiviral.2020.104792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Poston D., Weisblum Y., Wise H., Templeton K., Jenks S., Hatziioannou T., Bieniasz P. Absence of severe acute respiratory syndrome coronavirus 2 neutralizing activity in prepandemic sera from individuals with recent seasonal coronavirus infection. Clin. Infect. Dis. 2021;73:e1208–e1211. doi: 10.1093/cid/ciaa1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elko E.A., Nelson G.A., Mead H.L., Kelley E.J., Carvalho S.T., Sarbo N.G., Harms C.E., Le Verche V., Cardoso A.A., Ely J.L. COVID-19 vaccination elicits an evolving, cross-reactive antibody response to epitopes conserved with endemic coronavirus spike proteins. Cell Rep. 2022;40:111022. doi: 10.1016/j.celrep.2022.111022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grobben M., van der Straten K., Brouwer P.J., Brinkkemper M., Maisonnasse P., Dereuddre-Bosquet N., Appelman B., Lavell A.A., van Vught L.A., Burger J.A. Cross-reactive antibodies after SARS-CoV-2 infection and vaccination. Elife. 2021;10:e70330. doi: 10.7554/eLife.70330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Millet J.K., Whittaker G.R. Physiological and molecular triggers for SARS-CoV membrane fusion and entry into host cells. Virology. 2018;517:3–8. doi: 10.1016/j.virol.2017.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chambers P., Pringle C.R., Easton A.J. Heptad repeat sequences are located adjacent to hydrophobic regions in several types of virus fusion glycoproteins. J. Gen. Virol. 1990;71:3075–3080. doi: 10.1099/0022-1317-71-12-3075. [DOI] [PubMed] [Google Scholar]
- 33.Xia S., Xu W., Wang Q., Wang C., Hua C., Li W., Lu L., Jiang S. Peptide-based membrane fusion inhibitors targeting HCoV-229E spike protein HR1 and HR2 domains. Int. J. Mol. Sci. 2018;19:487. doi: 10.3390/ijms19020487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu D., Zhu Y., Jiao T., Wu T., Xiao X., Qin B., Chong H., Lei X., Ren L., Cui S. Structure-based design and characterization of novel fusion-inhibitory lipopeptides against SARS-CoV-2 and emerging variants. Emerg. Microbes Infect. 2021;10:1227–1240. doi: 10.1080/22221751.2021.1937329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang Q., Zhang Y., Wu L., Niu S., Song C., Zhang Z., Lu G., Qiao C., Hu Y., Yuen K.-Y. Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell. 2020;181:894–904.e899. doi: 10.1016/j.cell.2020.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Masters P.S. The molecular biology of coronaviruses. Adv. Virus Res. 2006;66:193–292. doi: 10.1016/S0065-3527(06)66005-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Glowacka I., Bertram S., Müller M.A., Allen P., Soilleux E., Pfefferle S., Steffen I., Tsegaye T.S., He Y., Gnirss K. Evidence that TMPRSS2 activates the severe acute respiratory syndrome coronavirus spike protein for membrane fusion and reduces viral control by the humoral immune response. J. Virol. 2011;85:4122–4134. doi: 10.1128/JVI.02232-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lu G., Hu Y., Wang Q., Qi J., Gao F., Li Y., Zhang Y., Zhang W., Yuan Y., Bao J. Molecular basis of binding between novel human coronavirus MERS-CoV and its receptor CD26. Nature. 2013;500:227–231. doi: 10.1038/nature12328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang N., Shi X., Jiang L., Zhang S., Wang D., Tong P., Guo D., Fu L., Cui Y., Liu X. Structure of MERS-CoV spike receptor-binding domain complexed with human receptor DPP4. Cell Res. 2013;23:986–993. doi: 10.1038/cr.2013.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hulswit R.J., Lang Y., Bakkers M.J., Li W., Li Z., Schouten A., Ophorst B., Van Kuppeveld F.J., Boons G.-J., Bosch B.-J. Human coronaviruses OC43 and HKU1 bind to 9-O-acetylated sialic acids via a conserved receptor-binding site in spike protein domain A. Proc. Natl. Acad. Sci. USA. 2019;116:2681–2690. doi: 10.1073/pnas.1809667116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jaimes J.A., André N.M., Chappie J.S., Millet J.K., Whittaker G.R. Phylogenetic analysis and structural modeling of SARS-CoV-2 spike protein reveals an evolutionary distinct and proteolytically sensitive activation loop. J. Mol. Biol. 2020;432:3309–3325. doi: 10.1016/j.jmb.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hoffmann M., Kleine-Weber H., Schroeder S., Kruger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.-H., Nitsche A. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280.e278. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Laporte M., Raeymaekers V., Van Berwaer R., Vandeput J., Marchand-Casas I., Thibaut H.-J., Van Looveren D., Martens K., Hoffmann M., Maes P. The SARS-CoV-2 and other human coronavirus spike proteins are fine-tuned towards temperature and proteases of the human airways. PLoS Pathog. 2021;17:e1009500. doi: 10.1371/journal.ppat.1009500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Korber B., Fischer W.M., Gnanakaran S., Yoon H., Theiler J., Abfalterer W., Hengartner N., Giorgi E.E., Bhattacharya T., Foley B. Tracking changes in SARS-CoV-2 spike: Evidence that D614G increases infectivity of the COVID-19 virus. Cell. 2020;182:812–827.e819. doi: 10.1016/j.cell.2020.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lu S., Xie X.-x., Zhao L., Wang B., Zhu J., Yang T.-r., Yang G.-w., Ji M., Lv C.-p., Xue J. The immunodominant and neutralization linear epitopes for SARS-CoV-2. Cell Rep. 2021;34:108666. doi: 10.1016/j.celrep.2020.108666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.VanBlargan L.A., Adams L.J., Liu Z., Chen R.E., Gilchuk P., Raju S., Smith B.K., Zhao H., Case J.B., Winkler E.S. A potently neutralizing SARS-CoV-2 antibody inhibits variants of concern by utilizing unique binding residues in a highly conserved epitope. Immunity. 2021;54:2399–2416.e2396. doi: 10.1016/j.immuni.2021.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lv H., Wu N.C., Tsang O.T.-Y., Yuan M., Perera R.A., Leung W.S., So R.T., Chan J.M.C., Yip G.K., Chik T.S.H. Cross-reactive antibody response between SARS-CoV-2 and SARS-CoV infections. Cell Rep. 2020;31:107725. doi: 10.1016/j.celrep.2020.107725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Taefehshokr N., Taefehshokr S., Hemmat N., Heit B. COVID-19: Perspectives on innate immune evasion. Front. Immunol. 2020;11:580641. doi: 10.3389/fimmu.2020.580641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dosch S.F., Mahajan S.D., Collins A.R. SARS coronavirus spike protein-induced innate immune response occurs via activation of the NF-κB pathway in human monocyte macrophages in vitro. Virus Res. 2009;142:19–27. doi: 10.1016/j.virusres.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chou J.-M., Tsai J.-L., Hung J.-N., Chen I.-H., Chen S.-T., Tsai M.-H. The ORF8 protein of SARS-CoV-2 modulates the spike protein and its implications in viral transmission. Front. Microbiol. 2022;13:883597. doi: 10.3389/fmicb.2022.883597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rubio-Casillas A., Redwan E.M., Uversky V.N. SARS-CoV-2: A master of immune evasion. Biomedicines. 2022;10:1339. doi: 10.3390/biomedicines10061339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moriyama M., Lucas C., Monteiro V.S., Yale SARS-CoV-2 Genomic Surveillance Initiative. Iwasaki A. SARS-CoV-2 Omicron subvariants evolved to promote further escape from MHC-I recognition. bioRxiv. 2022 doi: 10.1101/2022.05.04.490614. [DOI] [Google Scholar]
- 53.Sette A., Crotty S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell. 2021;184:861–880. doi: 10.1016/j.cell.2021.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.O’Connell P., Aldhamen Y.A. Systemic innate and adaptive immune responses to SARS-CoV-2 as it relates to other coronaviruses. Hum. Vaccin. Immunother. 2020;16:2980–2991. doi: 10.1080/21645515.2020.1802974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu X., Nurieva R.I., Dong C. Transcriptional regulation of follicular T-helper (Tfh) cells. Immunol. Rev. 2013;252:139–145. doi: 10.1111/imr.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kaneko N., Kuo H.-H., Boucau J., Farmer J.R., Allard-Chamard H., Mahajan V.S., Piechocka-Trocha A., Lefteri K., Osborn M., Bals J. Loss of Bcl-6-expressing T follicular helper cells and germinal centers in COVID-19. Cell. 2020;183:143–157.e113. doi: 10.1016/j.cell.2020.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lu X., Hosono Y., Nagae M., Ishizuka S., Ishikawa E., Motooka D., Ozaki Y., Sax N., Maeda Y., Kato Y. Identification of conserved SARS-CoV-2 spike epitopes that expand public cTfh clonotypes in mild COVID-19 patients. J. Exp. Med. 2021;218:e20211327. doi: 10.1084/jem.20211327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Crotty S. T follicular helper cell differentiation, function, and roles in disease. Immunity. 2014;41:529–542. doi: 10.1016/j.immuni.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Crotty S. T follicular helper cell biology: A decade of discovery and diseases. Immunity. 2019;50:1132–1148. doi: 10.1016/j.immuni.2019.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moderbacher C.R., Ramirez S.I., Dan J.M., Grifoni A., Hastie K.M., Weiskopf D., Belanger S., Abbott R.K., Kim C., Choi J. Antigen-specific adaptive immunity to SARS-CoV-2 in acute COVID-19 and associations with age and disease severity. Cell. 2020;183:996–1012.e1019. doi: 10.1016/j.cell.2020.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Meckiff B.J., Ramírez-Suástegui C., Fajardo V., Chee S.J., Kusnadi A., Simon H., Eschweiler S., Grifoni A., Pelosi E., Weiskopf D. Imbalance of regulatory and cytotoxic SARS-CoV-2-reactive CD4+ T cells in COVID-19. Cell. 2020;183:1340–1353.e1316. doi: 10.1016/j.cell.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Meyer B., Drosten C., Müller M.A. Serological assays for emerging coronaviruses: Challenges and pitfalls. Virus Res. 2014;194:175–183. doi: 10.1016/j.virusres.2014.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Suthar M.S., Zimmerman M.G., Kauffman R.C., Mantus G., Linderman S.L., Hudson W.H., Vanderheiden A., Nyhoff L., Davis C.W., Adekunle O. Rapid generation of neutralizing antibody responses in COVID-19 patients. Cell Rep. Med. 2020;1:100040. doi: 10.1016/j.xcrm.2020.100040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Burbelo P.D., Riedo F.X., Morishima C., Rawlings S., Smith D., Das S., Strich J.R., Chertow D.S., Davey Jr R.T., Cohen J.I. Sensitivity in detection of antibodies to nucleocapsid and spike proteins of severe acute respiratory syndrome coronavirus 2 in patients with coronavirus disease 2019. J. Infect. Dis. 2020;222:206–213. doi: 10.1093/infdis/jiaa273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Grifoni A., Weiskopf D., Ramirez S.I., Mateus J., Dan J.M., Moderbacher C.R., Rawlings S.A., Sutherland A., Premkumar L., Jadi R.S. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020;181:1489–1501.e1415. doi: 10.1016/j.cell.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Juno J.A., Tan H.-X., Lee W.S., Reynaldi A., Kelly H.G., Wragg K., Esterbauer R., Kent H.E., Batten C.J., Mordant F.L. Humoral and circulating follicular helper T cell responses in recovered patients with COVID-19. Nat. Med. 2020;26:1428–1434. doi: 10.1038/s41591-020-0995-0. [DOI] [PubMed] [Google Scholar]
- 67.Peng Y., Mentzer A.J., Liu G., Yao X., Yin Z., Dong D., Dejnirattisai W., Rostron T., Supasa P., Liu C. Broad and strong memory CD4+ and CD8+ T cells induced by SARS-CoV-2 in UK convalescent individuals following COVID-19. Nat. Immunol. 2020;21:1336–1345. doi: 10.1038/s41590-020-0782-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ao Z., Ouyang M.J., Olukitibi T.A., Warner B., Vendramelli R., Truong T., Meilleur C., Zhang M., Kung S., Fowke K.R. A Recombinant VSV-Based Bivalent Vaccine Effectively Protects against Both SARS-CoV-2 and Influenza A Virus Infection. J. Virol. 2022;96:e01337-22. doi: 10.1128/jvi.01337-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sahni C., Chowdhury P.B.R., Devadas D., Ashish A., Singh N.K., Yadav A., Kaur M., Mishra S., Vishwakarma S., Singh R. SARS-CoV-2 Mutations Responsible for Immune Evasion Leading to Breakthrough Infection. Cureus. 2022;14:e29544. doi: 10.7759/cureus.29544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Watson O.J., Barnsley G., Toor J., Hogan A.B., Winskill P., Ghani A.C. Global impact of the first year of COVID-19 vaccination: A mathematical modelling study. Lancet Infect. Dis. 2022;22:1293–1302. doi: 10.1016/S1473-3099(22)00320-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hall V.J., Foulkes S., Charlett A., Atti A., Monk E.J., Simmons R., Wellington E., Cole M.J., Saei A., Oguti B. SARS-CoV-2 infection rates of antibody-positive compared with antibody-negative health-care workers in England: A large, multicentre, prospective cohort study (SIREN) Lancet. 2021;397:1459–1469. doi: 10.1016/S0140-6736(21)00675-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ao D., Lan T., He X., Liu J., Chen L., Baptista-Hon D.T., Zhang K., Wei X. SARS-CoV-2 Omicron variant: Immune escape and vaccine development. MedComm. 2022;3:e126. doi: 10.1002/mco2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yuan M., Wu N.C., Zhu X., Lee C.-C.D., So R.T., Lv H., Mok C.K., Wilson I.A. A highly conserved cryptic epitope in the receptor binding domains of SARS-CoV-2 and SARS-CoV. Science. 2020;368:630–633. doi: 10.1126/science.abb7269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mohammadi M., Shayestehpour M., Mirzaei H. The impact of spike mutated variants of SARS-CoV2 [Alpha, Beta, Gamma, Delta, and Lambda] on the efficacy of subunit recombinant vaccines. Braz. J. Infect. Dis. 2021;25:101606. doi: 10.1016/j.bjid.2021.101606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cherian S., Potdar V., Jadhav S., Yadav P., Gupta N., Das M., Rakshit P., Singh S., Abraham P., Panda S., et al. SARS-CoV-2 Spike Mutations, L452R, T478K, E484Q and P681R, in the Second Wave of COVID-19 in Maharashtra, India. Microorganism. 2021;9:1542–1553. doi: 10.3390/microorganisms9071542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shah M., Woo H.G. Omicron: A heavily mutated SARS-CoV-2 variant exhibits stronger binding to ACE2 and potently escapes approved COVID-19 therapeutic antibodies. Front. Immunol. 2022;12:6031. doi: 10.3389/fimmu.2021.830527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kumar S., Karuppanan K., Subramaniam G. Omicron (BA. 1) and sub-variants (BA. 1.1, BA. 2, and BA. 3) of SARS-CoV-2 spike infectivity and pathogenicity: A comparative sequence and structural-based computational assessment. J. Med. Virol. 2022;94:4780–4791. doi: 10.1002/jmv.27927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Mohapatra R.K., Kandi V., Sarangi A.K., Verma S., Tuli H.S., Chakraborty S., Chakraborty C., Dhama K. The recently emerged BA. 4 and BA. 5 lineages of Omicron and their global health concerns amid the ongoing wave of COVID-19 pandemic–Correspondence. Int. J. Surg. 2022;103:106698. doi: 10.1016/j.ijsu.2022.106698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chatterjee S., Bhattacharya M., Nag S., Dhama K., Chakraborty C. A Detailed Overview of SARS-CoV-2 Omicron: Its Sub-Variants, Mutations and Pathophysiology, Clinical Characteristics, Immunological Landscape, Immune Escape, and Therapies. Viruses. 2023;15:167. doi: 10.3390/v15010167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Callaway E. Are COVID surges becoming more predictable. Nature. 2022;605:204–206. doi: 10.1038/d41586-022-01240-x. [DOI] [PubMed] [Google Scholar]
- 81.Tegally H., Moir M., Everatt J., Giovanetti M., Scheepers C., Wilkinson E., Subramoney K., Moyo S., Amoako D.G., Althaus C.L. Continued emergence and evolution of Omicron in South Africa: New BA. 4 and BA. 5 lineages. MedRxiv. 2022 doi: 10.1101/2022.05.01.22274406. [DOI] [Google Scholar]
- 82.LLC G. Fact Sheet for Healthcare Providers Emergency Use Authorization (EUA) of Sotrovimab. [(accessed on 29 September 2022)];2022 Available online: https://www.fda.gov/media/149534/download.
- 83.Mohseni Afshar Z., Tavakoli Pirzaman A., Karim B., Rahimipour Anaraki S., Hosseinzadeh R., Sanjari Pireivatlou E., Babazadeh A., Hosseinzadeh D., Miri S.R., Sio T.T. SARS-CoV-2 Omicron (B. 1.1. 529) Variant: A Challenge with COVID-19. Diagnostics. 2023;13:559. doi: 10.3390/diagnostics13030559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hoffmann M., Hofmann-Winkler H., Krüger N., Kempf A., Nehlmeier I., Graichen L., Arora P., Sidarovich A., Moldenhauer A.-S., Winkler M.S. SARS-CoV-2 variant B. 1.617 is resistant to bamlanivimab and evades antibodies induced by infection and vaccination. Cell Rep. 2021;36:109415. doi: 10.1016/j.celrep.2021.109415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Thomson E.C., Rosen L.E., Shepherd J.G., Spreafico R., da Silva Filipe A., Wojcechowskyj J.A., Davis C., Piccoli L., Pascall D.J., Dillen J. Circulating SARS-CoV-2 spike N439K variants maintain fitness while evading antibody-mediated immunity. Cell. 2021;184:1171–1187.e1120. doi: 10.1016/j.cell.2021.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cao Y., Wang J., Jian F., Xiao T., Song W., Yisimayi A., Huang W., Li Q., Wang P., An R. Omicron escapes the majority of existing SARS-CoV-2 neutralizing antibodies. Nature. 2022;602:657–663. doi: 10.1038/s41586-021-04385-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Edara V.V., Norwood C., Floyd K., Lai L., Davis-Gardner M.E., Hudson W.H., Mantus G., Nyhoff L.E., Adelman M.W., Fineman R. Infection-and vaccine-induced antibody binding and neutralization of the B. 1.351 SARS-CoV-2 variant. Cell Host Microbe. 2021;29:516–521.e513. doi: 10.1016/j.chom.2021.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Emary K.R., Golubchik T., Aley P.K., Ariani C.V., Angus B., Bibi S., Blane B., Bonsall D., Cicconi P., Charlton S. Efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 variant of concern 202012/01 (B. 1.1. 7): An exploratory analysis of a randomised controlled trial. Lancet. 2021;397:1351–1362. doi: 10.1016/S0140-6736(21)00628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Helmsdal G., Hansen O.K., Møller L.F., Christiansen D.H., Petersen M.S., Kristiansen M.F. Omicron outbreak at a private gathering in the Faroe Islands, infecting 21 of 33 triple-vaccinated healthcare workers. Clin. Infect. Dis. 2022;75:893–896. doi: 10.1093/cid/ciac089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tada T., Zhou H., Dcosta B.M., Samanovic M.I., Chivukula V., Herati R.S., Hubbard S.R., Mulligan M.J., Landau N.R. Increased resistance of SARS-CoV-2 Omicron variant to neutralization by vaccine-elicited and therapeutic antibodies. EBioMedicine. 2022;78:103944. doi: 10.1016/j.ebiom.2022.103944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hoffmann M., Krüger N., Schulz S., Cossmann A., Rocha C., Kempf A., Nehlmeier I., Graichen L., Moldenhauer A.-S., Winkler M.S. The Omicron variant is highly resistant against antibody-mediated neutralization: Implications for control of the COVID-19 pandemic. Cell. 2022;185:447–456.e411. doi: 10.1016/j.cell.2021.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mengist H.M., Kombe A.J.K., Mekonnen D., Abebaw A., Getachew M., Jin T. Mutations of SARS-CoV-2 spike protein: Implications on immune evasion and vaccine-induced immunity. Semin. Immunol. 2021;55:101533. doi: 10.1016/j.smim.2021.101533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wu M., Wall E.C., Carr E.J., Harvey R., Townsley H., Mears H.V., Adams L., Kjaer S., Kelly G., Warchal S. Three-dose vaccination elicits neutralising antibodies against omicron. Lancet. 2022;399:715–717. doi: 10.1016/S0140-6736(22)00092-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ng K.W., Faulkner N., Finsterbusch K., Wu M., Harvey R., Hussain S., Greco M., Kjaer S., Swanton C. SARS-CoV-2 S2–targeted vaccination elicits broadly neutralizing antibodies. Sci. Transl. Med. 2022;14:eabn3715. doi: 10.1126/scitranslmed.abn3715. [DOI] [PubMed] [Google Scholar]
- 95.Cao Y., Yisimayi A., Jian F., Song W., Xiao T., Wang L., Du S., Wang J., Li Q., Chen X. BA. 2.12. 1, BA. 4 and BA. 5 escape antibodies elicited by Omicron infection. Nature. 2022;608:593–602. doi: 10.1038/s41586-022-04980-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Simon-Loriere E., Schwartz O. Towards SARS-CoV-2 serotypes? Nat. Rev. Microbiol. 2022;20:187–188. doi: 10.1038/s41579-022-00708-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Walls A.C., Tortorici M.A., Snijder J., Xiong X., Bosch B.-J., Rey F.A., Veesler D. Tectonic conformational changes of a coronavirus spike glycoprotein promote membrane fusion. Proc. Natl. Acad. Sci. USA. 2017;114:11157–11162. doi: 10.1073/pnas.1708727114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Erbelding E.J., Post D.J., Stemmy E.J., Roberts P.C., Augustine A.D., Ferguson S., Paules C.I., Graham B.S., Fauci A.S. A universal influenza vaccine: The strategic plan for the National Institute of Allergy and Infectious Diseases. J. Infect. Dis. 2018;218:347–354. doi: 10.1093/infdis/jiy103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Nachbagauer R., Krammer F. Universal influenza virus vaccines and therapeutic antibodies. Clin. Microbiol. Infect. 2017;23:222–228. doi: 10.1016/j.cmi.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Neirynck S., Deroo T., Saelens X., Vanlandschoot P., Jou W.M., Fiers W. A universal influenza A vaccine based on the extracellular domain of the M2 protein. Nat. Med. 1999;5:1157–1163. doi: 10.1038/13484. [DOI] [PubMed] [Google Scholar]
- 101.Saelens X. The role of matrix protein 2 ectodomain in the development of universal influenza vaccines. J. Infect. Dis. 2019;219:S68–S74. doi: 10.1093/infdis/jiz003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Uranowska K., Tyborowska J., Jurek A., Szewczyk B.a., Gromadzka B. Hemagglutinin stalk domain from H5N1 strain as a potentially universal antigen. Acta Biochim. Pol. 2014;61:541–550. doi: 10.18388/abp.2014_1876. [DOI] [PubMed] [Google Scholar]
- 103.Turley C.B., Rupp R.E., Johnson C., Taylor D.N., Wolfson J., Tussey L., Kavita U., Stanberry L., Shaw A. Safety and immunogenicity of a recombinant M2e–flagellin influenza vaccine (STF2. 4xM2e) in healthy adults. Vaccine. 2011;29:5145–5152. doi: 10.1016/j.vaccine.2011.05.041. [DOI] [PubMed] [Google Scholar]
- 104.Olukitibi T., Ao Z., Azizi H., Mahmoudi M., Coombs K., Kobasa D., Kobinger G., Yao X. Development and characterization of influenza M2 ectodomain and/or hemagglutinin stalk-based dendritic cell-targeting vaccines. Front. Microbiol. 2022;13:937192–937206. doi: 10.3389/fmicb.2022.937192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chauhan V., Rungta T., Goyal K., Singh M.P. Designing a multi-epitope based vaccine to combat Kaposi Sarcoma utilizing immunoinformatics approach. Sci. Rep. 2019;9:1–15. doi: 10.1038/s41598-019-39299-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Guest J.D., Pierce B.G. Structure-based and rational design of a hepatitis C virus vaccine. Viruses. 2021;13:837. doi: 10.3390/v13050837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ahmed S.F., Quadeer A.A., Barton J.P., McKay M.R. Cross-serotypically conserved epitope recommendations for a universal T cell-based dengue vaccine. PLoS Negl. Trop. Dis. 2020;14:e0008676. doi: 10.1371/journal.pntd.0008676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Dixit N.K. Design of Monovalent and Chimeric Tetravalent Dengue Vaccine Using an Immunoinformatics Approach. Int. J. Pept. Res. Ther. 2021;27:2607–2624. doi: 10.1007/s10989-021-10277-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ali M., Pandey R.K., Khatoon N., Narula A., Mishra A., Prajapati V.K. Exploring dengue genome to construct a multi-epitope based subunit vaccine by utilizing immunoinformatics approach to battle against dengue infection. Sci. Rep. 2017;7:1–13. doi: 10.1038/s41598-017-09199-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sampath A., Padmanabhan R. Molecular targets for flavivirus drug discovery. Antivir. Res. 2009;81:6–15. doi: 10.1016/j.antiviral.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mateo M., Reynard S., Journeaux A., Germain C., Hortion J., Carnec X., Picard C., Baillet N., Borges-Cardoso V., Merabet O. A single-shot Lassa vaccine induces long-term immunity and protects cynomolgus monkeys against heterologous strains. Sci. Transl. Med. 2021;13:eabf6348. doi: 10.1126/scitranslmed.abf6348. [DOI] [PubMed] [Google Scholar]
- 112.ter Meulen J., Badusche M., Satoguina J., Strecker T., Lenz O., Loeliger C., Sakho M., Koulemou K., Koivogui L., Hoerauf A. Old and New World arenaviruses share a highly conserved epitope in the fusion domain of the glycoprotein 2, which is recognized by Lassa virus-specific human CD4+ T-cell clones. Virology. 2004;321:134–143. doi: 10.1016/j.virol.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 113.ter Meulen J., Badusche M., Kuhnt K., Doetze A., Satoguina J., Marti T., Loeliger C., Koulemou K., Koivogui L., Schmitz H. Characterization of human CD4+ T-cell clones recognizing conserved and variable epitopes of the Lassa virus nucleoprotein. J. Virol. 2000;74:2186–2192. doi: 10.1128/JVI.74.5.2186-2192.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sankaranarayanan S., Mohkhedkar M., Janakiraman V. Mutations in spike protein T cell epitopes of SARS-COV-2 variants: Plausible influence on vaccine efficacy. Biochim. Et Biophys. Acta (BBA)-Mol. Basis Dis. 2022;1868:166432. doi: 10.1016/j.bbadis.2022.166432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kombe Kombe A.J., Zahid A., Mohammed A., Shi R., Jin T. Potent molecular feature-based neutralizing monoclonal antibodies as promising therapeutics against SARS-CoV-2 infection. Front. Mol. Biosci. 2021;8:670815. doi: 10.3389/fmolb.2021.670815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jaiswal V., Lee H.-J. Conservation and Evolution of Antigenic Determinants of SARS-CoV-2: An Insight for Immune Escape and Vaccine Design. Front. Immunol. 2022;13:832106. doi: 10.3389/fimmu.2022.832106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bagherzadeh M.A., Izadi M., Baesi K., Jahromi M.A.M., Pirestani M. Considering epitopes conservity in targeting SARS-CoV-2 mutations in variants: A novel immunoinformatics approach to vaccine design. Sci. Rep. 2022;12:1–17. doi: 10.1038/s41598-022-18152-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kibria K., Faruque M., Islam M., Ullah H., Mahmud S., Miah M., Saleh A.A. A conserved subunit vaccine designed against SARS-CoV-2 variants showed evidence in neutralizing the virus. Appl. Microbiol. Biotechnol. 2022;106:4091–4114. doi: 10.1007/s00253-022-11988-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jiang S., Wu S., Zhao G., He Y., Guo X., Zhang Z., Hou J., Ding Y., Cheng A., Wang B. Identification of a promiscuous conserved CTL epitope within the SARS-CoV-2 spike protein. Emerg. Microbes Infect. 2022;11:730–740. doi: 10.1080/22221751.2022.2043727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Vishwakarma P., Yadav N., Rizvi Z.A., Khan N.A., Chiranjivi A.K., Mani S., Bansal M., Dwivedi P., Shrivastava T., Kumar R. Severe acute respiratory syndrome coronavirus 2 spike protein based novel epitopes induce potent immune responses in vivo and inhibit viral replication in vitro. Front. Immunol. 2021;12:613045. doi: 10.3389/fimmu.2021.613045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Muraoka D., Situo D., Sawada S.-i., Akiyoshi K., Harada N., Ikeda H. Identification of a dominant CD8+ CTL epitope in the SARS-associated coronavirus 2 spike protein. Vaccine. 2020;38:7697–7701. doi: 10.1016/j.vaccine.2020.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lin J., Law R., Korosec C.S., Zhou C., Koh W.H., Ghaemi M.S., Samaan P., Ooi H.K., Yue F., Gingras A.-C. Longitudinal Assessment of SARS-CoV-2 Specific T Cell Cytokine-Producing Responses for 1 Year Reveals Persistence of Multi-Cytokine Proliferative Responses, with Greater Immunity Associated with Disease Severity. Int. J. Mol. Sci. 2022;23:4341. doi: 10.1128/jvi.00509-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Martin W.R., Cheng F. A rational design of a multi-epitope vaccine against SARS-CoV-2 which accounts for the glycan shield of the spike glycoprotein. J. Biomol. Struct. Dyn. 2021;40:7099–7113. doi: 10.1080/07391102.2021.1894986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lim H.X., Masomian M., Khalid K., Kumar A.U., MacAry P.A., Poh C.L. Identification of B-Cell Epitopes for Eliciting Neutralizing Antibodies against the SARS-CoV-2 Spike Protein through Bioinformatics and Monoclonal Antibody Targeting. Int. J. Mol. Sci. 2022;23:4341. doi: 10.3390/ijms23084341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ladner J.T., Henson S.N., Boyle A.S., Engelbrektson A.L., Fink Z.W., Rahee F., D’ambrozio J., Schaecher K.E., Stone M., Dong W. Epitope-resolved profiling of the SARS-CoV-2 antibody response identifies cross-reactivity with endemic human coronaviruses. Cell Rep. Med. 2021;2:100189. doi: 10.1016/j.xcrm.2020.100189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Pinto D., Sauer M.M., Czudnochowski N., Low J.S., Tortorici M.A., Housley M.P., Noack J., Walls A.C., Bowen J.E., Guarino B. Broad betacoronavirus neutralization by a stem helix–specific human antibody. Science. 2021;373:1109–1116. doi: 10.1126/science.abj3321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Mallavarpu Ambrose J., Priya Veeraraghavan V., Kullappan M., Chellapandiyan P., Krishna Mohan S., Manivel V.A. Comparison of immunological profiles of SARS-CoV-2 variants in the COVID-19 pandemic trends: An immunoinformatics approach. Antibiotics. 2021;10:535. doi: 10.3390/antibiotics10050535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wu W.-L., Chiang C.-Y., Lai S.-C., Yu C.-Y., Huang Y.-L., Liao H.-C., Liao C.-L., Chen H.-W., Liu S.-J. Monoclonal antibody targeting the conserved region of the SARS-CoV-2 spike protein to overcome viral variants. JCI Insight. 2022;7:e157597. doi: 10.1172/jci.insight.157597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cuspoca A.F., Estrada P.I., Velez-van-Meerbeke A. Molecular mimicry of SARS-CoV-2 spike protein in the nervous system: A bioinformatics approach. Comput. Struct. Biotechnol. J. 2022;20:6041–6054. doi: 10.1016/j.csbj.2022.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ng K.T., Mohd-Ismail N.K., Tan Y.-J. Spike S2 subunit: The dark horse in the race for prophylactic and therapeutic interventions against SARS-CoV-2. Vaccines. 2021;9:178. doi: 10.3390/vaccines9020178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Li Y., Lai D.-y., Zhang H.-n., Jiang H.-w., Tian X., Ma M.-l., Qi H., Meng Q.-f., Guo S.-j., Wu Y., et al. Linear epitopes of SARS-CoV-2 spike protein elicit neutralizing antibodies in COVID-19 patients. Cell. Mol. Immunol. 2020;17:1095–1097. doi: 10.1038/s41423-020-00523-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Poh C.M., Carissimo G., Wang B., Amrun S.N., Lee C.Y.-P., Chee R.S.-L., Fong S.-W., Yeo N.K.-W., Lee W.-H., Torres-Ruesta A., et al. Two linear epitopes on the SARS-CoV-2 spike protein that elicit neutralising antibodies in COVID-19 patients. Nat. Commun. 2020;11:2806. doi: 10.1038/s41467-020-16638-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Xia S., Yan L., Xu W., Agrawal A.S., Algaissi A., Tseng C.K., Wang Q., Du L., Tan W., Wilson I.A., et al. A pan-coronavirus fusion inhibitor targeting the HR1 domain of human coronavirus spike. Sci. Adv. 2019;5:eaav4580. doi: 10.1126/sciadv.aav4580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Smith T.R.F., Patel A., Ramos S., Elwood D., Zhu X., Yan J., Gary E.N., Walker S.N., Schultheis K., Purwar M., et al. Immunogenicity of a DNA vaccine candidate for COVID-19. Nat. Commun. 2020;11:2601. doi: 10.1038/s41467-020-16505-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ng K.W., Faulkner N., Cornish G.H., Rosa A., Harvey R., Hussain S., Ulferts R., Earl C., Wrobel A.G., Benton D.J. Preexisting and de novo humoral immunity to SARS-CoV-2 in humans. Science. 2020;370:1339–1343. doi: 10.1126/science.abe1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Nguyen-Contant P., Embong A.K., Kanagaiah P., Chaves F.A., Yang H., Branche A.R., Topham D.J., Sangster M.Y. S protein-reactive IgG and memory B cell production after human SARS-CoV-2 infection includes broad reactivity to the S2 subunit. MBio. 2020;11:e01991-20. doi: 10.1128/mBio.01991-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Song G., He W.-t., Callaghan S., Anzanello F., Huang D., Ricketts J., Torres J.L., Beutler N., Peng L., Vargas S. Cross-reactive serum and memory B-cell responses to spike protein in SARS-CoV-2 and endemic coronavirus infection. Nat. Commun. 2021;12:2938. doi: 10.1038/s41467-021-23074-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zhu Y., Yu D., Hu Y., Wu T., Chong H., He Y. SARS-CoV-2-derived fusion inhibitor lipopeptides exhibit highly potent and broad-spectrum activity against divergent human coronaviruses. Signal Transduct. Target. Ther. 2021;6:294. doi: 10.1038/s41392-021-00698-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Pinto D., Fenwick C., Caillat C., Silacci C., Guseva S., Dehez F., Chipot C., Barbieri S., Minola A., Jarrossay D. Structural basis for broad HIV-1 neutralization by the MPER-specific human broadly neutralizing antibody LN01. Cell Host Microbe. 2019;26:623–637.e628. doi: 10.1016/j.chom.2019.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Zhang L., Irimia A., He L., Landais E., Rantalainen K., Leaman D.P., Vollbrecht T., Stano A., Sands D.I., Kim A.S. An MPER antibody neutralizes HIV-1 using germline features shared among donors. Nat. Commun. 2019;10:1–16. doi: 10.1038/s41467-019-12973-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Pietzsch J., Scheid J.F., Mouquet H., Seaman M.S., Broder C.C., Nussenzweig M.C. Anti-gp41 antibodies cloned from HIV-infected patients with broadly neutralizing serologic activity. J. Virol. 2010;84:5032–5042. doi: 10.1128/JVI.00154-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ma C., Su S., Wang J., Wei L., Du L., Jiang S. From SARS-CoV to SARS-CoV-2: Safety and broad-spectrum are important for coronavirus vaccine development. Microb. Infect. 2020;22:245–253. doi: 10.1016/j.micinf.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Zeng F., Hon C.C., Yip C.W., Law K.M., Yeung Y.S., Chan K.H., Peiris J.S.M., Leung F.C.C. Quantitative comparison of the efficiency of antibodies against S1 and S2 subunit of SARS coronavirus spike protein in virus neutralization and blocking of receptor binding: Implications for the functional roles of S2 subunit. FEBS Lett. 2006;580:5612–5620. doi: 10.1016/j.febslet.2006.08.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Guo Y., Sun S., Wang K., Zhang S., Zhu W., Chen Z. Elicitation of immunity in mice after immunization with the S2 subunit of the severe acute respiratory syndrome coronavirus. DNA Cell Biol. 2005;24:510–515. doi: 10.1089/dna.2005.24.510. [DOI] [PubMed] [Google Scholar]
- 145.Wang L., Shi W., Joyce M.G., Modjarrad K., Zhang Y., Leung K., Lees C.R., Zhou T., Yassine H.M., Kanekiyo M. Evaluation of candidate vaccine approaches for MERS-CoV. Nat. Commun. 2015;6:1–11. doi: 10.1038/ncomms8712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Chen Y., Lu S., Jia H., Deng Y., Zhou J., Huang B., Yu Y., Lan J., Wang W., Lou Y. A novel neutralizing monoclonal antibody targeting the N-terminal domain of the MERS-CoV spike protein. Emerg. Microbes Infect. 2017;6:e60. doi: 10.1038/emi.2017.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Elshabrawy H.A., Coughlin M.M., Baker S.C., Prabhakar B.S. Human monoclonal antibodies against highly conserved HR1 and HR2 domains of the SARS-CoV spike protein are more broadly neutralizing. PLoS ONE. 2012;7:e50366. doi: 10.1371/journal.pone.0050366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Li H., Chen Z., Liu X., Hu P. T cell epitopes are largely conserved in the SARS-CoV-2 Omicron subvariant (BA. 1, BA. 2, BA. 3, and GKA) J. Med. Virol. 2022;94:4591–4592. doi: 10.1002/jmv.27925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tarke A., Sidney J., Kidd C.K., Dan J.M., Ramirez S.I., Yu E.D., Mateus J., da Silva Antunes R., Moore E., Rubiro P. Comprehensive analysis of T cell immunodominance and immunoprevalence of SARS-CoV-2 epitopes in COVID-19 cases. Cell Rep. Med. 2021;2:100204. doi: 10.1016/j.xcrm.2021.100204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Saini S.K., Hersby D.S., Tamhane T., Povlsen H.R., Hernandez S.P.A., Nielsen M., Gang A.O., Hadrup S.R. SARS-CoV-2 genome-wide T cell epitope mapping reveals immunodominance and substantial CD8+ T cell activation in COVID-19 patients. Sci. Immunol. 2021;6:eabf7550. doi: 10.1126/sciimmunol.abf7550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Jiang M., Zhang G., Liu H., Ding P., Liu Y., Tian Y., Wang Y., Wang A. Epitope profiling reveals the critical antigenic determinants in SARS-CoV-2 RBD-based antigen. Front. Immunol. 2021;12:707977. doi: 10.3389/fimmu.2021.707977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Polyiam K., Phoolcharoen W., Butkhot N., Srisaowakarn C., Thitithanyanont A., Auewarakul P., Hoonsuwan T., Ruengjitchatchawalya M., Mekvichitsaeng P., Roshorm Y.M. Immunodominant linear B cell epitopes in the spike and membrane proteins of SARS-CoV-2 identified by immunoinformatics prediction and immunoassay. Sci. Rep. 2021;11:1–17. doi: 10.1038/s41598-021-99642-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Duan L., Zheng Q., Zhang H., Niu Y., Lou Y., Wang H. The SARS-CoV-2 spike glycoprotein biosynthesis, structure, function, and antigenicity: Implications for the design of spike-based vaccine immunogens. Front. Immunol. 2020;11:576622. doi: 10.3389/fimmu.2020.576622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Olukitibi T.A., Ao Z., Mahmoudi M., Kobinger G.A., Yao X. Dendritic cells/macrophages-targeting feature of Ebola glycoprotein and its potential as immunological facilitator for antiviral vaccine approach. Microorganisms. 2019;7:402. doi: 10.3390/microorganisms7100402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Lim H.X., Lim J., Poh C.L. Identification and selection of immunodominant B and T cell epitopes for dengue multi-epitope-based vaccine. Med. Microbiol. Immunol. 2021;210:1–11. doi: 10.1007/s00430-021-00700-x. [DOI] [PubMed] [Google Scholar]
- 156.Brandão J.G., Scheper R.J., Lougheed S.M., Curiel D.T., Tillman B.W., Gerritsen W.R., van den Eertwegh A.J.M., Pinedo H.M., Haisma H.J., de Gruijl T.D. CD40-targeted adenoviral gene transfer to dendritic cells through the use of a novel bispecific single-chain Fv antibody enhances cytotoxic T cell activation. Vaccine. 2003;21:2268–2272. doi: 10.1016/S0264-410X(03)00050-1. [DOI] [PubMed] [Google Scholar]
- 157.Fossum E., Gradeland G., Terhorst D., Tveita A.A., Vikse E., Mjaaland S., Henri S., Malissen B., Bogen B. Vaccine molecules targeting Xcr1 on cross-presenting DCs induce protective CD8+ T-cell responses against influenza virus. Eur. J. Immunol. 2014;45:624–635. doi: 10.1002/eji.201445080. [DOI] [PubMed] [Google Scholar]
- 158.Marlin R., Godot V., Cardinaud S., Galhaut M., Coleon S., Zurawski S., Dereuddre-Bosquet N., Cavarelli M., Gallouët A.-S., Maisonnasse P. Targeting SARS-CoV-2 receptor-binding domain to cells expressing CD40 improves protection to infection in convalescent macaques. Nat. Commun. 2021;12:1–9. doi: 10.1038/s41467-021-25382-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Deng Y., Lan J., Bao L., Huang B., Ye F., Chen Y., Yao Y., Wang W., Qin C., Tan W. Enhanced protection in mice induced by immunization with inactivated whole viruses compare to spike protein of middle east respiratory syndrome coronavirus. Emerg. Microbes Infect. 2018;7:1–10. doi: 10.1038/s41426-018-0056-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Ao Z., Wang L., Mendoza E.J., Cheng K., Zhu W., Cohen E.A., Fowke K., Qiu X., Kobinger G., Yao X. Incorporation of Ebola glycoprotein into HIV particles facilitates dendritic cell and macrophage targeting and enhances HIV-specific immune responses. PLoS ONE. 2019;14:e0216949–e0217067. doi: 10.1371/journal.pone.0216949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ao Z., Wang L., Azizi H., Olukitibi T.A., Kobinger G., Yao X. Development and Evaluation of an Ebola Virus Glycoprotein Mucin-Like Domain Replacement System as a New DC-Targeting Vaccine Approach Against HIV-1. J. Virol. 2021;95:e02368-20. doi: 10.1128/JVI.02368-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Sabbaghi A., Ghaemi A. DNA Vaccines. Springer; Berlin/Heidelberg, Germany: 2021. Molecular adjuvants for DNA vaccines: Application, design, preparation, and formulation; pp. 87–112. [DOI] [PubMed] [Google Scholar]
- 163.Hu H., Lu X., Tao L., Bai B., Zhang Z., Chen Y., Zheng F., Chen J., Chen Z., Wang H. Induction of specific immune responses by severe acute respiratory syndrome coronavirus spike DNA vaccine with or without interleukin-2 immunization using different vaccination routes in mice. Clin. Vaccine Immunol. 2007;14:894–901. doi: 10.1128/CVI.00019-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Gary E.N., Tursi N.J., Warner B., Parzych E.M., Ali A.R., Frase D., Moffat E., Embury-Hyatt C., Smith T.R., Broderick K.E. Mucosal chemokine adjuvant enhances synDNA vaccine-mediated responses to SARS-CoV-2 and provides heterologous protection in vivo. Cell Rep. Med. 2022;3:100693. doi: 10.1016/j.xcrm.2022.100693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Eusébio D., Neves A.R., Costa D., Biswas S., Alves G., Cui Z., Sousa Â. Methods to improve the immunogenicity of plasmid DNA vaccines. Drug Discov. Today. 2021;26:2575–2592. doi: 10.1016/j.drudis.2021.06.008. [DOI] [PubMed] [Google Scholar]
- 166.Ma X., Zou F., Yu F., Li R., Yuan Y., Zhang Y., Zhang X., Deng J., Chen T., Song Z. Nanoparticle vaccines based on the receptor binding domain (RBD) and heptad repeat (HR) of SARS-CoV-2 elicit robust protective immune responses. Immunity. 2020;53:1315–1330.e1319. doi: 10.1016/j.immuni.2020.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Swaminathan G., Thoryk E.A., Cox K.S., Meschino S., Dubey S.A., Vora K.A., Celano R., Gindy M., Casimiro D.R., Bett A.J. A novel lipid nanoparticle adjuvant significantly enhances B cell and T cell responses to sub-unit vaccine antigens. Vaccine. 2016;34:110–119. doi: 10.1016/j.vaccine.2015.10.132. [DOI] [PubMed] [Google Scholar]
- 168.Dong Y., Dai T., Wei Y., Zhang L., Zheng M., Zhou F. A systematic review of SARS-CoV-2 vaccine candidates. Signal Transduct. Target. Ther. 2020;5:1–14. doi: 10.1038/s41392-020-00352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Clark E.M., Pippin M.M. StatPearls [Internet] StatPearls Publishing; Tampa, FL, USA: 2022. Safe And Effective Administration Of Vaccines And Epinephrine Autoinjection. [PubMed] [Google Scholar]
- 170.Park J.H., Lee H.K. Delivery routes for COVID-19 vaccines. Vaccines. 2021;9:524. doi: 10.3390/vaccines9050524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Van Doremalen N., Purushotham J.N., Schulz J.E., Holbrook M.G., Bushmaker T., Carmody A., Port J.R., Yinda C.K., Okumura A., Saturday G. Intranasal ChAdOx1 nCoV-19/AZD1222 vaccination reduces shedding of SARS-CoV-2 D614G in rhesus macaques. Sci. Transl. Med. 2021;13:eabh0755. doi: 10.1126/scitranslmed.abh0755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Gebhardt T., Wakim L.M., Eidsmo L., Reading P.C., Heath W.R., Carbone F.R. Memory T cells in nonlymphoid tissue that provide enhanced local immunity during infection with herpes simplex virus. Nat. Immunol. 2009;10:524–530. doi: 10.1038/ni.1718. [DOI] [PubMed] [Google Scholar]
- 173.Hassan A.O., Kafai N.M., Dmitriev I.P., Fox J.M., Smith B.K., Harvey I.B., Chen R.E., Winkler E.S., Wessel A.W., Case J.B. A single-dose intranasal ChAd vaccine protects upper and lower respiratory tracts against SARS-CoV-2. Cell. 2020;183:169–184.e113. doi: 10.1016/j.cell.2020.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zhou D., Chan J.F.-W., Zhou B., Zhou R., Li S., Shan S., Liu L., Zhang A.J., Chen S.J., Chan C.C.-S. Robust SARS-CoV-2 infection in nasal turbinates after treatment with systemic neutralizing antibodies. Cell Host Microbe. 2021;29:551–563.e555. doi: 10.1016/j.chom.2021.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Gao T., Ren Y., Li S., Lu X., Lei H. Immune response induced by oral administration with a Saccharomyces cerevisiae-based SARS-CoV-2 vaccine in mice. Microb. Cell Factories. 2021;20:95. doi: 10.1186/s12934-021-01584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Desai A.N., Majumder M.S. What is herd immunity? JAMA. 2020;324:2113. doi: 10.1001/jama.2020.20895. [DOI] [PubMed] [Google Scholar]
- 177.Aschwanden C. Five reasons why COVID herd immunity is probably impossible. Nature. 2021;591:520–522. doi: 10.1038/d41586-021-00728-2. [DOI] [PubMed] [Google Scholar]
- 178.Morens D.M., Folkers G.K., Fauci A.S. The concept of classical herd immunity may not apply to COVID-19. J. Infect. Dis. 2022;226:195–198. doi: 10.1093/infdis/jiac109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Ashton J. COVID-19 and herd immunity. J. R. Soc. Med. 2022;115:76–77. doi: 10.1177/01410768221080824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.MacIntyre C.R., Costantino V., Trent M. Modelling of COVID-19 vaccination strategies and herd immunity, in scenarios of limited and full vaccine supply in NSW, Australia. Vaccine. 2022;40:2506–2513. doi: 10.1016/j.vaccine.2021.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable.