In the nutrition, obesity, and eating disorder (ED) fields, polarizing discourse exists around whether treating obesity and reducing weight stigma and ED psychopathology are mutually exclusive. 1,2,3,4,5,6,7 The objective of this commentary was to examine and synthesize evidence surrounding the relationship between obesity treatment and weight stigma and ED risk to combat the false dichotomy that exists between treating obesity and reducing weight stigma and ED risk. First, an overview of obesity, weight stigma, and ED are introduced, followed by discussion of self-directed dieting vs evidence-based obesity treatments and their relation to factors that influence ED risk. The commentary ends with a call to action for all clinicians to promote access to evidence-based care, combat weight stigma and minimize the risk of ED development.
Obesity
Traditionally, obesity has been defined as a body mass index (BMI; calculated as kg/m2) of >30.2, 8 Using this definition, obesity prevalence is high and has been rising; as of 2018, 42% of US adults are living with obesity. 9 Disproportionate prevalence is observed among traditionally marginalized groups, including Black and Hispanic/Latinx populations and those with lower socioeconomic status (SES). 10,11,12 Obesity is associated with adverse health outcomes, including impaired daily functioning, decreased health-related quality of life, increased stress, 4,13 and increased risks of cardiometabolic disease and cancer. 14,15,16,17 Additionally, as severity of obesity increases, so does the severity of health problems. 18
BMI serves as a screening tool and not a diagnostic tool, as a patient’s BMI does not distinguish between lean and fat mass. 19 Moreover, the association between BMI and health outcomes can differ by racial and ethnic groups. 19 Based on these discrepancies, a new definition has been proposed with Canadian guidelines, and the World Health Organization, defining obesity as the state of excess adiposity that is associated with adverse impacts to quality of life or physical health (Figure 1). 8,20 This new definition takes a health-focused rather than a weight-focused approach, allowing for improved sensitivity to the nuance of the relationship between weight and health status. From a clinical perspective, BMI can still be a complementary piece of data when assessing whether someone has obesity, but these data alone are not enough to define obesity at the individual level. Importantly, obesity should be treated like other chronic conditions and afforded access to evidence-based and effective treatment options to improve health-related outcomes. 21
Figure 1a.
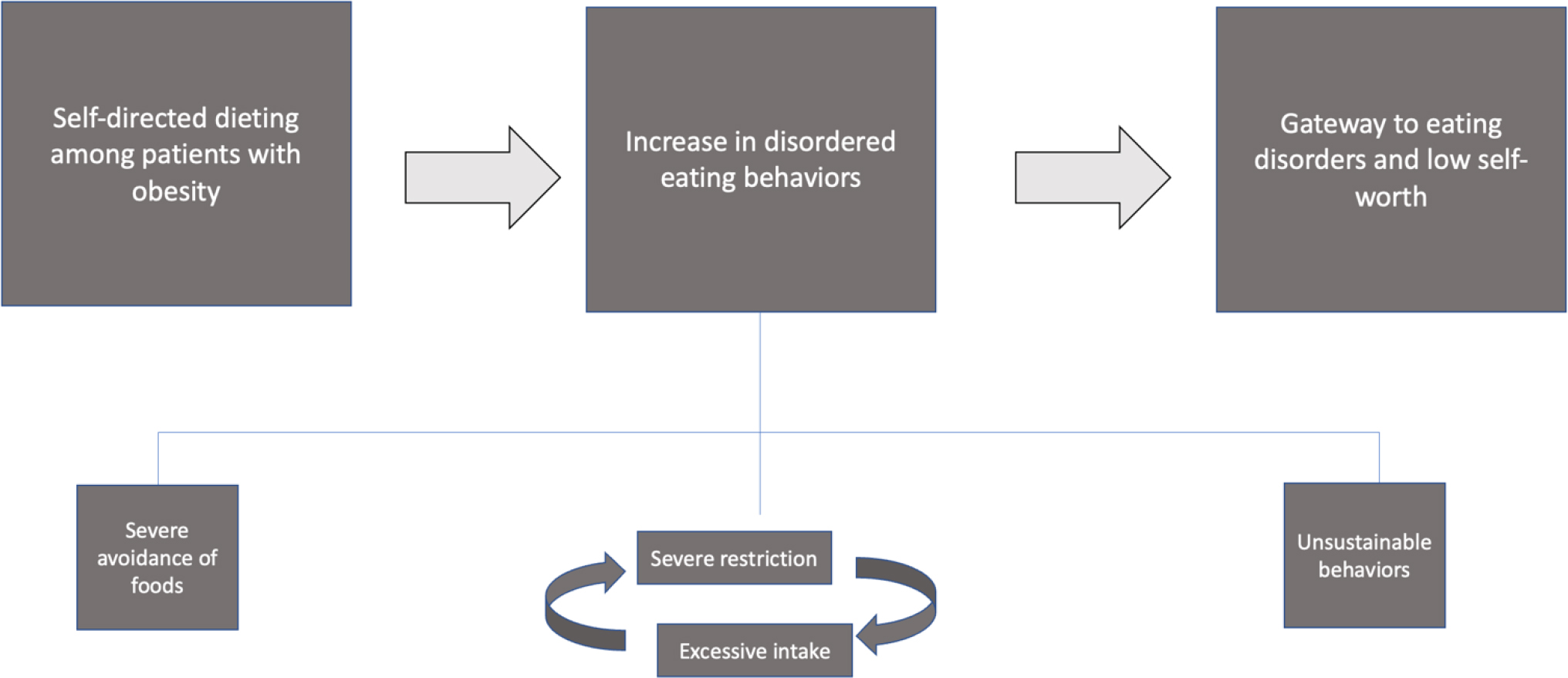
The Relationship between Self-Directed Dieting and Health-Related Outcomes60–66
There is debate surrounding whether obesity or weight stigma might be the true cause of adverse outcomes related to obesity, 4 and that the previous definition of obesity erroneously prioritized BMI and weight status alone as the diagnostic criteria for obesity. Further research is needed to better understand how to operationalize this new definition of obesity when doing population level research and to examine whether this revised definition facilitates a decrease in weight stigma and bias.
Weight Stigma
Weight stigma, defined as devaluation of a person based on weight, is pervasive (Figure 1). 22 Twenty-five to fifty percent of youth experience bullying due to their weight, and 13 to 32% have been discriminated against based on their weight. 23,24,25,26,27,28,29 Among adults, estimates of weight stigma prevalence have ranged from 44% to 57%.30,31
Weight stigma increases the risk of high allostatic load, psychiatric and substance use disorders, and suicidality. 32,33,34,35 Complicating these risks, more than one-half of healthcare providers attribute overweight and obesity to a lack of willpower, reinforcing negative stereotypes33 and dissuading people with obesity across the globe from seeking medical care. 36 Rather than motivating healthy behaviors, weight stigma contributes to avoidance of healthcare, healthcare inequities, increased weight gain, and EDs. 4,22,37,38,39 Therefore, preventing weight stigma should be prioritized in health-care settings.
EDs
EDs are serious psychiatric disorders that occur across the body weight and size spectrum and include anorexia nervosa, bulimia nervosa, and binge ED (Figure 1). 40 EDs affect 8.6% of girls and women and 4.1% of boys and men at some point in their lives41 and occur across diverse racial and ethnic groups and the socioeconomic spectrum. 42 Adverse consequences of EDs include premature death (particularly by suicide), osteoporosis, gastrointestinal issues, liver and kidney damage, hypo- and hypertension, dyslipidemia, and glucose dysregulation. 40,43,44,45,46,47,48 A childhood history of overweight or obesity and substantial weight gain during adolescence increase risk for EDs, with increased weight concerns as a mechanism. 49,50,51
It is also important to note that weight stigma is a known risk factor for disordered eating. 52 Both children and adults who experience weight stigma have an increased risk of low self-esteem and poor body image. 52,53,54,55,56,57 The impact of weight stigma on disordered eating can be seen in children as early as elementary school. 58 Internalization of the thin ideal can moderate the relationship between experiencing weight stigma and disordered eating behavior. 59 However, more work remains to be done to establish the link between weight stigma and anorexia nervosa, bulimia nervosa, and binge ED. 52
Dieting VS Supervised Treatment for Obesity
Self-Directed Diets
The word diet has been used counterintuitively. In colloquial use, it describes self-directed efforts to lose weight by restricting the amount and/or types of food consumed. Fad diets, often oriented toward achieving appearance ideals rather than improving physical health, are often promoted in media. Cyclical in nature, these diets promise unrealistic benefits and may promote disordered eating behaviors. Early studies indicated self-directed dieting and EDs were associated; whether this relationship was causal, however, became controversial almost 2 decades ago. 60,61,62 Strict rules about avoiding certain foods, common in self-directed diets, can lead to alternating between severe restriction and excessive food intake, promoting subsequent weight gain after weight loss. 63,64 These practices can result in low self-worth and stricter rules about calorie restriction. 64 This pattern mirrors symptoms observed in bulimia nervosa, some forms of anorexia nervosa, and many cases of binge ED. Thus, self-directed dieting itself can be a gateway to EDs. 60,65,66
Currently, self-directed dieting among patients with obesity has been implicated in increasing disordered eating behaviors and promoting development of EDs. Figure 2 presents clear distinctions between self-directed diets and supervised evidence-based obesity treatment (i.e. diets monitored and administered by health professionals) that have significant implications for increasing vs decreasing ED risk. 7,16,17,20,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87 Clear overlap in core features of evidence-based obesity and ED treatment in improving nutrition and body image lead to the following conclusion: treating obesity and reducing weight stigma and ED psychopathology are not mutually exclusive.
Supervised evidence-based Obesity Treatment
In contrast to self-directed diets, which often promote reaching an “ideal” body size by implementing overly restrictive changes, supervised evidence-based behavioral weight management encourages sustainable changes to promote long-term health. 67 These multicomponent interventions are based on several theories68,69 and incorporate dietary, activity, and behavior change strategy components. Treatment also focuses on modifying socioenvironmental factors, including stimulus control in the home environment, seeking out support networks, and active problem-solving skill development. Current behavioral treatments for obesity typically produce weight losses of 5% to 10% of initial body weight, 21,88 and improvements are observed regarding quality of life, body image, daily functioning and mobility, and modest reductions in depression and anxiety. 7,16,17,70,71 This level of weight loss may result in a state of weight suppression, which can increase the risk of EDs. 89,90,91 Notably, the link between weight suppression and ED risk is mediated by increased drive for thinness, and interventions that increase body acceptance may prevent negative consequences of weight loss. 65,92,93 Rarely, evidence-based obesity treatment can lead to, or exacerbate, pre-existing distorted or obsessive thoughts and behaviors around weight and food, which potentially increase risk of EDs (Figure 1). 7,94 Overall, however, participation in treatment for obesity has been associated with reductions in disordered eating behaviors. 7,71,72 Evidence-based obesity treatment is compatible with a patient-centered treatment approach as these treatments focus on improving overall health, rather than weight loss alone, and can reduce ED risk. 20,73,74,75
Many individuals regain weight after obesity treatment, 95,96 leading to concern about weight cycling. 75,97 Early research indicated patterns of weight loss and regain are associated with higher all-cause mortality and morbidity from cardiovascular disease; however, much of this research did not control for unintentional weight loss from underlying health conditions. 98,99,100,101 More recent findings support that treatments for obesity produce significant and sustained physical and mental health improvements, despite potential weight regain, and challenge the notion that losing and regaining causes more harm than never losing weight. 76,77,78,79,80,81 In fact, increased frequency of weight loss attempts when at least 5 lb were lost is associated with lower mortality than no attempt. 80
Compatibility between Obesity Treatment and ED Treatment and Prevention
Robust analyses have demonstrated that treatment for obesity may reduce ED prevalence and risk. 7,72 Supervised behavioral childhood obesity treatment may have a protective effect via treatment carryover by addressing emotional eating. 7,71 Both meal planning and regular eating are components of obesity treatment that overlap with cognitive behavioral therapy (CBT) for EDs. 82 Meal planning ensures nutrient-rich foods are available when it is time to eat, mirroring efforts to identify and reduce triggers for disordered eating. Regular eating is prescribed to prevent excessive hunger, which contributes to dysregulated eating. 102
Regular weigh-ins represent another component shared between supervised evidence-based obesity treatments and CBT for EDs. Weekly weighing replaces too frequent or complete avoidance of weighing, either of which can perpetuate disordered eating. 83,84,103 In individuals without EDs, self-weighing helps facilitate clinically significant weight loss without leading to ED symptoms. 83,84,103 Among those with EDs, being aware of weight can counteract irrational beliefs that can motivate disordered behaviors or create ambivalence about treatment. 102,104,105
Treatments for obesity also emphasize improving diet quality, 86,87 suggesting a flexible eating style in which more nutrient-dense foods and fewer nutrient-poor, energy-dense foods are consumed, while moderately restricting caloric intake. No foods are prohibited and a balanced dietary pattern is recommended. This avoids triggering cognitive distortions linked to EDs, such as dividing foods into “good” vs. “bad.” 106 This approach is identical to that used in CBT for EDs.
The few studies examining obesity treatments that assess weight stigma have all shown modest yet significant short- and long-term reductions in weight stigma. 59,107,108,109,110 Behavioral and CBT interventions for weight often address negative cognitions that affect self-esteem and body image, which may minimize internalized weight stigma. 81,111,112 For example, increasing self-efficacy by meeting behavioral goals enables a person to challenge and reject negative beliefs about one’s capabilities. 113,114 Furthermore, group interventions or interactions with others with similar experiences engenders camaraderie, which decreases loneliness, increases a sense of belonging (counteracting stigma), and may provide validation and support not otherwise available. 110,114,115,116 A recent randomized controlled trial compared changes in internalized weight stigma between a standard group weight management treatment and one that also included a weight stigma reduction intervention in a diverse sample of adults with obesity who reported a high level of weight stigma at baseline. Participants who received the weight stigma intervention reported greater reductions in aspects of weight self-stigma (i.e. self-devaluation), but internalized weight stigma was significantly reduced in both groups. 114 Further study of mechanisms for stigma-reduction are needed; still, these findings reveal internalized weight stigma reduces, rather than increases, with behavioral weight management treatment alone.
Summary
Shared components between supervised evidence-based obesity treatment mirror interventions for ED by including overall concepts of diet quality vs quantity, physical activity/sedentary activity, self-monitoring, and building a healthy body image. Specifically, evidence-based obesity treatments focus on improving overall diet quality and increasing the consumption of nutrient dense foods. 111 This is similar to ED interventions that promote a flexible eating style and challenge avoidance of “forbidden” foods. 111,117 Physical activity goals in obesity treatment include increasing enjoyable activities and reducing sedentary time, which parallels recommendations in ED treatment. 118,119 Regular self-weighing is a mainstay of evidence-based ED treatment and replaces too frequent or avoidance of weighing, either of which can perpetuate disordered eating thoughts and behaviors. 83,84,103 Self-weighing as part of obesity treatment leads to clinically significant weight loss without resulting in adverse psychological outcomes. 83,84,85 Finally, evidence-based obesity treatment encourages patients to participate in activities to reduce the overvaluation of weight and shape and promote self-efficacy, similar to ED interventions that promote these activities to reduce the risk of relapse. 111,120 Thus, there are several similarities between evidence-based obesity treatment and interventions for disordered eating, dispelling the commonly believed narrative that obesity treatments can increase ED risk.
In summary, self-directed diets can promote unhealthy practices (eg, fasting or rigid food restriction) that can cause great harm. 60,63,64,65,66 Conversely, supervised evidence-based obesity treatment improves health and reduces ED symptoms without increasing internalized weight stigma. 7,59,77,107,108,109,110
Call to Action
It is critical that evidence-based and compassionate care be accessible for individuals seeking treatment for obesity, EDs, and comorbid obesity and EDs. Given existing debate between obesity treatment advocates and advocates for Health at Every Size (HAES), a call to action for clinicians is issued in this section of the commentary. Suggestions described herein are guided by the Belmont principles of beneficence (ie, maximize benefits while minimizing risks) and justice (ie, equitable distribution of care). 121 Health professionals should acknowledge what an intervention entails, and its range of outcomes, while respecting patients’ decisions, whether that includes a weight-related goal or not. Health professionals on both sides of the debate should aim to improve access to compassionate, evidence-based, and patient-centered care, to actively fight weight stigma, and to end diet culture by placing emphasis on health rather than weight.
Focus on Patient-centered Approaches in Obesity Treatment
Given the multiple complications of obesity, withholding evidence-based obesity treatment from patients for whom it is medically indicated and who desire it is unethical. 122,123 A respectful, compassionate, and patient-centered approach requires a thorough review of treatment options. Treatment should be based on weight history, family history, comorbidities, ED risk, psychosocial factors, and prognosis. 20
A fully informed treatment decision may require conversations that reframe expectations. Due to stigma, many patients may erroneously believe that, regardless of their starting weight, they must achieve a BMI < 25 through behavioral strategies alone. Therefore, it is critical to explain the limitations of BMI as a measure of health, that some weight regain is normal after treatment for obesity if treatment is discontinued, and that long-term maintenance of reduced weight requires more effort than expended by those who have never experienced overweight and obesity. A metaphor for this pattern is the role of diet and exercise in treatment of type 2 diabetes. If patients with type 2 diabetes discontinue exercise and/or increase consumption of simple carbohydrates, an increase in blood glucose will be observed. Similarly, if behaviors incorporated in obesity treatments are stopped, weight regain is likely. Therefore, it is important for individuals to modify their shared home environment and social-environmental contextual cues to support eating, activity, and behavior changes that can be sustained in the long term.
If a patient with obesity does not wish to discuss weight status or pursue treatments for obesity, healthcare providers should respect this decision without judgment. Many other behavioral changes can improve health in the absence of weight loss, such as increases in physical activity and consumption of fruits and vegetables, and improvements in sleep and stress management. These factors can also be beneficial in prevention of future excess weight gain. Improved body image has numerous positive consequences and should be pursued regardless of body size or decisions about weight loss.
Misinformation about the nature of evidence-based obesity treatment has fueled the debate between the obesity and ED fields, largely due to limited access to treatment for each. To reduce misinformation and utilization of fad diets and other potentially dangerous weight loss strategies, evidence-based treatments for obesity need to be accessible, effective, and affordable. Despite the U.S. Preventive Services Task Force recommendation to provide behavioral treatment to youth and adults with obesity, access remains limited. 123,124,125 Indeed, 96.4% of US adults with obesity have an unmet need for obesity care, with most individuals attempting to lose weight through self-directed dieting. 126 Furthermore, few persons with EDs receive evidence-based care. 127
Barriers to ED treatment include misperception of the severity of disorder, lack of insurance, physicians not recognizing EDs, stigma surrounding mental health, and geographical proximity to treatment. 128 Also, persons with EDs are more likely to seek and receive treatment for obesity than for EDs, 129 illustrating a clear need for providers of obesity treatment to screen for EDs and make referrals for ED treatment as needed. 129
Despite Medicaid coverage of US Preventive Services Task Force recommendations for adults, insurance coverage remains a primary barrier to treatments for both obesity and EDs. 130 The Centers for Medicare and Medicaid Services have made provisions for reimbursing obesity treatment in primary care; however, additional focus on translation to clinical care is needed118,131 as utilization of the benefit remains low. Moreover, little treatment guidance exists, only certain types of providers can offer services, and interpretation and implementation of Centers for Medicare and Medicaid Service guidelines vary by state. 118,130,131,132,133 In addition, insurance coverage for childhood obesity is lacking. 134 Access to care for obesity and EDs is especially problematic among marginalized populations. This is particularly concerning given higher obesity prevalence among Black, Hispanic, and Latinx patients and those with lower SES, 135 and that EDs do not discriminate on the basis of race or SES. 10,41 Traditionally marginalized racial and ethnic groups and those with lower SES may receive differential treatment, have different cultural perspectives on eating and weight, and face other barriers including transportation and language. 136,137 Furthermore, availability of weight loss information via the internet can lead to further disparities in treatment; for example, web searches done in Spanish have been found to contain more misinformation than those in English. 138 Technology, financial incentives, and cultural tailoring may improve access to evidence-based treatment. 136,137
Weight-based stigma and discrimination remain pervasive139,140,141 and highly prevalent in healthcare settings. 142 Efforts to reduce weight stigma should be data-driven and initiated through broad policies such as laws against weight-based discrimination in all 50 states. A multifaceted approach to reduce weight stigma in health care provider education is essential143,144 to develop an understanding within health care and the general public that numerous factors beyond “self-control” affect weight. For example, training for health care providers should include nonstereotypical case examples and information about uncontrollable causes of obesity and biological and physiological challenges to weight loss and weight regain. 143 During training, contact with patients with obesity sharing their lived experience can evoke empathy. 145 Most of the techniques tested to reduce weight bias have been marginally effective in the short-term, so new strategies to eradicate this form of prejudice in health care are still needed. Overall, public health and clinical messages that frame weight loss as solely a matter of willpower, promote extreme dietary or exercise behaviors, or encourage weight loss for the primary purpose of changing appearance do a significant disservice to advancing effective care.
Embracing body diversity as a movement has gained widespread recognition through fat-acceptance and Health at Every Size efforts, bringing weight stigma to the forefront of the conversation. 146,147 Respect for a diversity of body shapes and sizes by healthcare providers and society at large is needed and, for those seeking obesity treatment, conversations with health care providers should emphasize overall health rather than weight alone. This is not a new concept; as early as 1982, The Dieter’s Dilemma: Eating Less and Weighing More argued for replacing weight goals with health goals. 148 However, it clearly bears repeating given ongoing discrimination against those living in larger bodies and promotion of “quick fixes.” Rejecting diet culture may prevent internalization of unhealthy, aesthetic, Western, thin ideals and will discourage disordered behaviors.
Conclusions
Providers and researchers need to present a united front to eliminate the false dichotomy between prevention and treatment of obesity and EDs. 149 Using a patient-centered approach, public health complications associated with obesity and EDs can be reduced while actively fighting weight stigma at the individual and population levels. All conversations on obesity, EDs, and weight stigma should utilize person-first, compassionate, and non-stigmatizing language. The scientific community should highlight complex systems that contribute to obesity, advocate for patients’ rights to choose or refuse treatment for obesity, and promote access to evidence-based treatments. 150 Moreover, addressing social determinants that create barriers to care is also high priority in implementing behavioral treatments for obesity and EDs. 151 Successful development and implementation of evidence-based behavioral obesity interventions that assess and mitigate ED prevalence and risk, while combating weight stigma, can be achieved when health care providers from the obesity and ED fields work together for the benefit of patients.
Figure 1b.
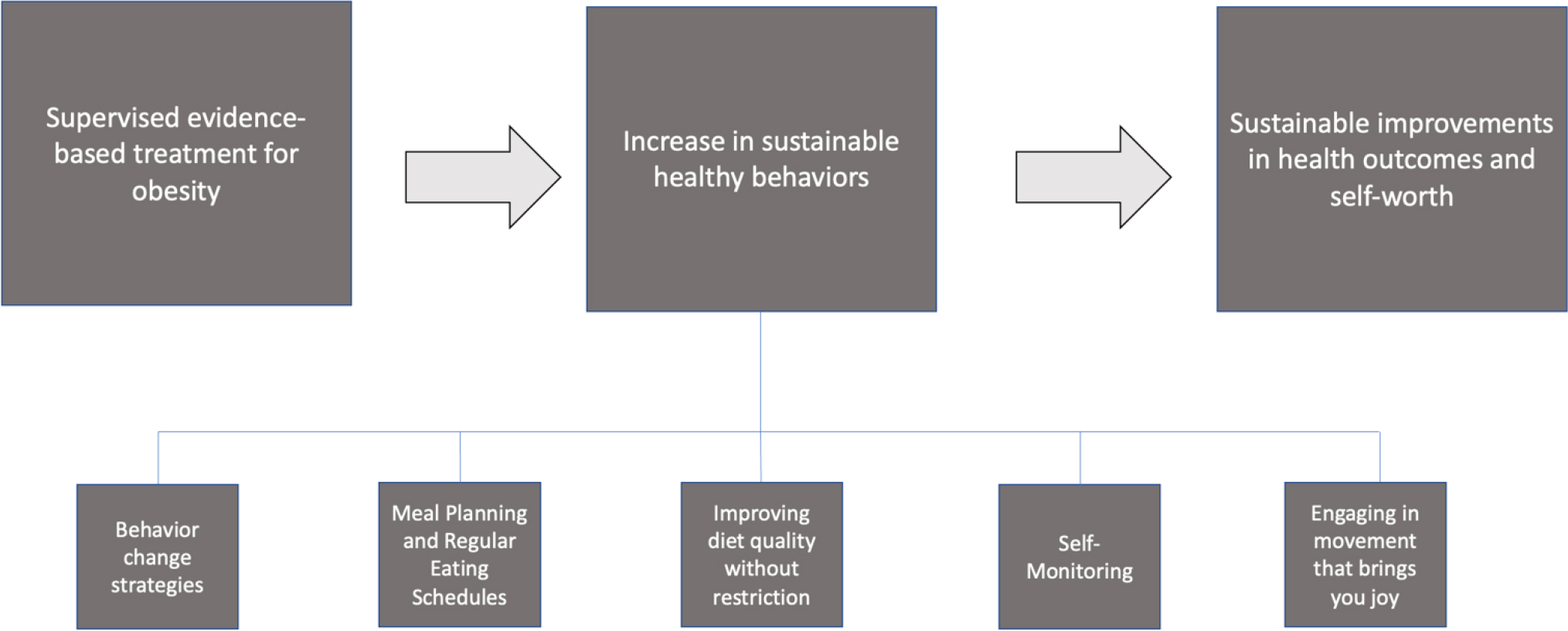
The Relationship between Supervised, Evidence-based Obesity Treatment and Health-Related Outcomes7,16,17,20,67–87
Table 1:
Definitions, Comorbidities, and High-risk Populations Associated with Obesity, Weight Stigma, and Eating Disorders
| Definition | Prevalent Health Concerns152,153,154 | High-Risk Populations153,155,156 | |
|---|---|---|---|
| Obesity | A disease defined by excess adipose tissue that is associated with adverse impacts to quality of life or physical health.8,9 | • Cancer • Cardiovascular disease • Chronic kidney disease • Dementia • Dyslipidemia • Gastroesophageal reflux disease • Hepatobiliary disease • Hypertension • Infection • Osteoarthritis • Psychological illnesses (e.g., anxiety and depression) • Stroke • Type 2 diabetes |
• Individuals from lower socioeconomic status backgrounds • Middle-aged adults (i.e., 40–59 years) • Traditionally marginalized racial/ethnic groups (e.g., Non-Hispanic Black adults and Hispanic adults) |
| Weight Stigma | Devaluation of a person due to their body weight, shape, or size, including discriminatory attitudes, actions, or policies. 157 | • Anxiety • Depression • Eating disorders • Cardiometabolic disease risk factors (e.g., heightened inflammation) 158,159 • Suicidal ideation |
• People with overweight/obesity, especially those with severe obesity (BMI of ≥40 kg/m2) • Women and minoritized genders |
| Eating Disorders | A variety of behavioral illnesses marked by frequent, extreme, unhealthy eating patterns to compensate for difficult feelings. Examples include anorexia nervosa, bulimia nervosa, and binge eating disorder. 160 | • Alcohol use disorder • Chronic pain • Generalized anxiety disorder • Hypertension • Obsessive-compulsive disorder • Phobia (e.g., social phobia) • Post-traumatic stress disorder • Type 2 diabetes • Unipolar major depression |
• Adolescents • People focused on body image (e.g., athletes, models, and those partaking in diet culture) • People with overweight/obesity • Women and minoritized genders |
Funding and Financial Disclosures:
There was no external funder for this study. MIC is supported by the National Institute of Health (NIH) National Heart, Lung, and Blood Institute (K01HL141535). RLP is supported by the NIH National Heart, Lung, and Blood Institute (K23HL140176). JFH is supported by NIH National Heart, Lung, and Blood Institute (T32 HL076134). KNB is supported by NIH National Institute of Diabetes and Digestive and Kidney Diseases (K01 DK120778). PKK is supported by the NIH National Institute of Mental Health (R01 MH111263). KR is supported by NIDDK R01DK119244 and NHLBI R03HL154272.
Footnotes
COI Disclosures: MIC is an employee at WW International, Inc. and has served as a consultant for Novo Nordisk (but did not accept personal fees for this work), all outside of the submitted work. FAN reports personal fees from Novo Nordisk, outside the submitted work. RLP has received grant funding from WW International, Inc. and has served as a consultant for WW International, Inc. and Novo Nordisk, outside of the submitted work. EJD is an employee of Obthera, Inc. No other potential conflicts of interest relevant to this article were reported.
References
- 1.Cardel MI, Taveras EM. Let’s Not Just Dismiss the Weight Watchers Kurbo App. Child Obes. 2020;16(8):547–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Research Risk/Benefit Ethics Position Statement. Academy for Eating Disorders. Published March 1, 2019. https://higherlogicdownload.s3.amazonaws.com/AEDWEB/05656ea0-59c9-4dd4-b832-07a3fea58f4c/UploadedImages/Advocate/Research_Risk-Benefit_Ethics_Position_Statement_2_28_19_-_FINAL.pdf
- 3.Raynor HA, Champagne CM. Position of the Academy of Nutrition and Dietetics: Interventions for the Treatment of Overweight and Obesity in Adults. J Acad Nutr Diet. 2016;116(1):129–147. [DOI] [PubMed] [Google Scholar]
- 4.Tomiyama AJ, Carr D, Granberg EM, et al. How and why weight stigma drives the obesity ‘epidemic’ and harms health. BMC Med. 2018;16(1):123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leme ACB, Thompson D, Lenz Dunker KL, et al. Obesity and eating disorders in integrative prevention programmes for adolescents: protocol for a systematic review and meta-analysis. BMJ Open. 2018;8(4):e020381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Da Luz F, Hay P, Touyz S, Sainsbury A. Obesity with Comorbid Eating Disorders: Associated Health Risks and Treatment Approaches. Nutrients. 2018;10(7):829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jebeile H, Gow ML, Baur LA, Garnett SP, Paxton SJ, Lister NB. Treatment of obesity, with a dietary component, and eating disorder risk in children and adolescents: A systematic review with meta-analysis. Obes Rev. 2019;20(9):1287–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Overweight and Obesity. 2021. Accessed November 9, 2021. https://www.who.int/health-topics/obesity#tab=tab_1
- 9.Hales C, Carroll M, Fryar C, Ogden C. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018. Centers for Disease Control and Prevention. Published February 20, 2020. Accessed on November 9, 2021. https://www.cdc.gov/nchs/products/databriefs/db360.htm
- 10.Mclaren L Socioeconomic Status and Obesity. Epidemiol Rev. 2007;29(1):29–48. [DOI] [PubMed] [Google Scholar]
- 11.Fradkin C, Wallander JL, Elliott MN, Tortolero S, Cuccaro P, Schuster MA. Associations between socioeconomic status and obesity in diverse, young adolescents: variation across race/ethnicity and gender. Health Psychol. 2015;34(1):1–9. [DOI] [PubMed] [Google Scholar]
- 12.Adult Obesity Prevalence Maps. Centers for Disease Control and Prevention. Accessed January 20, 2022. https://www.cdc.gov/obesity/data/prevalence-maps.html
- 13.Kolotkin R, Haaz S, Fontaine K. Assessment of health-related quality of life in obesity and eating disorders. Handbook of Assessment Methods for Eating Behaviors and Weight Related Problems: Sage Publications; 2009:33–78. [Google Scholar]
- 14.Saliba LJ, Maffett S. Hypertensive Heart Disease and Obesity: A Review. Heart Fail Clin. 2019;15(4):509–517. [DOI] [PubMed] [Google Scholar]
- 15.Maggio CA, Pi-Sunyer FX. Obesity and type 2 diabetes. Endocrinol Metab Clin North Am. 2003;32(4):805–822. viii. [DOI] [PubMed] [Google Scholar]
- 16.Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. for the International Agency for Research on Cancer Hanbook Working Group. Body Fatness and Cancer — Viewpoint of the IARC Working Group. N Engl J Med. 2016;375(8) 794–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kushner RF, Foster GD. Obesity and quality of life. Nutrition. 2000;16(10):947–952. [DOI] [PubMed] [Google Scholar]
- 18.Sturm R Increases in morbid obesity in the USA: 2000–2005. Public Health. 2007;121(7):492–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adab P, Pallan M, Whincup PH. Is BMI the best measure of obesity? BMJ. 2018; 360:k1274. [DOI] [PubMed] [Google Scholar]
- 20.Wharton S, Lau DCW, Vallis M, et al. Obesity in adults: a clinical practice guideline. CMAJ. 2020;192(31):E875–E891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults. Circulation. 2014-June-24 2014;129(25 suppl 2):S102–S138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andreyeva T, Puhl RM, Brownell KD. Changes in Perceived Weight Discrimination Among Americans, 1995–1996 Through 2004–2006. Obesity. 2008;16(5):1129–1134. [DOI] [PubMed] [Google Scholar]
- 23.Puhl RM, Lessard LM. Weight Stigma in Youth: Prevalence, Consequences, and Considerations for Clinical Practice. Curr Obes Rep. 2020;9(4):402–411. [DOI] [PubMed] [Google Scholar]
- 24.Bucchianeri MM, Gower AL, McMorris BJ, Eisenberg ME. Youth experiences with multiple types of prejudice-based harassment. J AdolesC. 2016;51:68–75. [DOI] [PubMed] [Google Scholar]
- 25.Puhl RM, Wall MM, Chen C, Bryn Austin S, Eisenberg ME, Neumark-Sztainer D. Experiences of weight teasing in adolescence and weight-related outcomes in adulthood: A 15-year longitudinal study. Prev Med. 2017;100:173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thompson I, Hong JS, Lee JM, Prys NA, Morgan JT, Udo-Inyang I. A review of the empirical research on weight-based bullying and peer victimisation published between 2006 and 2016. Educ Rev. 2018;72(1):88–110. [Google Scholar]
- 27.Salmon S, Turner S, Taillieu T, Fortier J, Afifi TO. Bullying victimization experiences among middle and high school adolescents: Traditional bullying, discriminatory harassment, and cybervictimization. J Adolesc. 2018;63:29–40. [DOI] [PubMed] [Google Scholar]
- 28.Golaszewski NM, Pasch KE, Fernandez A, Poulos NS, Batanova M, Loukas A. Perceived Weight Discrimination and School Connectedness Among Youth: Does Teacher Support Play a Protective Role? J Sch Health. 2018;88(10):754–761. [DOI] [PubMed] [Google Scholar]
- 29.Juvonen J, Lessard LM, Schacter HL, Suchilt L. Emotional Implications of Weight Stigma Across Middle School: The Role of Weight-Based Peer Discrimination. J Clin Child Adolesc Psychol. 2017;46(1):150–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prunty A, Clark KM, Hahn A, Edmonds S, O’Shea A. Enacted weight stigma and weight self stigma prevalence among 3821 adults. Obes Res Clin Pract. 2020;14(5):421–427. [DOI] [PubMed] [Google Scholar]
- 31.Puhl RM, Himmelstein MS, Quinn DM. Internalizing Weight Stigma: Prevalence and Sociodemographic Considerations in US Adults. Obesity. 2018;26(1):167–175. [DOI] [PubMed] [Google Scholar]
- 32.Vadiveloo M, Mattei J. Perceived Weight Discrimination and 10-Year Risk of Allostatic Load Among US Adults. Ann Behav Med. 2017;51(1):94–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9(12):788–805. [DOI] [PubMed] [Google Scholar]
- 34.Emmer C, Bosnjak M, Mata J. The association between weight stigma and mental health: A meta‐analysis. Obes Rev. 2020;21(1): e12935. [DOI] [PubMed] [Google Scholar]
- 35.Brochu PM. Weight stigma as a risk factor for suicidality. Int J Obes. 2020;44(10):1979–1980. [DOI] [PubMed] [Google Scholar]
- 36.Puhl RM, Lessard LM, Himmelstein MS, Foster GD. The roles of experienced and internalized weight stigma in healthcare experiences: Perspectives of adults engaged in weight management across six countries. PLoS ONE. 2021;16(6):e0251566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Puhl RM, Heuer CA. Obesity Stigma: Important Considerations for Public Health. Am J Public Health. 2010;100(6):1019–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Puhl RM, Himmelstein MS, Pearl RL. Weight stigma as a psychosocial contributor to obesity. Am Psychol. 2020;75(2):274–289. [DOI] [PubMed] [Google Scholar]
- 39.Callahan D Obesity: Chasing an Elusive Epidemic. Hastings Cent Rep. 2013;43(1):34–40. [DOI] [PubMed] [Google Scholar]
- 40.Klump KL, Bulik CM, Kaye WH, Treasure J, Tyson E. Academy for eating disorders position paper: eating disorders are serious mental illnesses. Int J Eat Disord. 2009;42(2):97–103. [DOI] [PubMed] [Google Scholar]
- 41.The Social and Economic Cost of Eating Disorders in the United States of America: A Report for the Strategic Training Initiative for the Prevention of Eating Disorders and the Academy of Eating Disorders. Deloitte Access Economics. Published June 2020. Accessed November 9, 2021. https://cdn1.sph.harvard.edu/wp-content/uploads/sites/1267/2020/07/Social-Economic-Cost-of-Eating-Disorders-in-US.pdf [Google Scholar]
- 42.Rodgers RF, Berry R, Franko DL. Eating Disorders in Ethnic Minorities: an Update. Curr Psychiatry Rep. 2018;20(10):90. [DOI] [PubMed] [Google Scholar]
- 43.Jenkins PE, Hoste RR, Meyer C, Blissett JM. Eating disorders and quality of life: a review of the literature. Clin Psychol Rev. 2011;31(1):113–121. [DOI] [PubMed] [Google Scholar]
- 44.Hudson JI, Hiripi E, Pope HG, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. Feb 2007;61(3):348–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Udo T, Grilo CM. Prevalence and Correlates of DSM-5–Defined Eating Disorders in a Nationally Representative Sample of U.S. Adults. Biol Psychiatry. 2018;84(5):345–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7):724–731. [DOI] [PubMed] [Google Scholar]
- 47.Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2006;19(4):438–443. [DOI] [PubMed] [Google Scholar]
- 48.Olguin P, Fuentes M, Gabler G, Guerdjikova AI, Keck PE, McElroy SL. Medical comorbidity of binge eating disorder: response. Eat Weight Disord. 12 2017;22(4):725–726. [DOI] [PubMed] [Google Scholar]
- 49.Thomas JG, Butryn ML, Stice E, Lowe MR. A prospective test of the relation between weight change and risk for bulimia nervosa. Int J Eat Disord. 2011;44(4):295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lebow J, Sim LA, Kransdorf LN. Prevalence of a History of Overweight and Obesity in Adolescents With Restrictive Eating Disorders. J Adolesc Health.2015;56(1):19–24. [DOI] [PubMed] [Google Scholar]
- 51.Hilbert A, Pike KM, Goldschmidt AB, et al. Risk factors across the eating disorders. Psychiatry Res. 2014;220(1–2):500–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Puhl R, Suh Y. Stigma and Eating and Weight Disorders. Curr Psychiatry Rep. 2015;17(3). [DOI] [PubMed] [Google Scholar]
- 53.Vartanian LR, Novak SA. Internalized Societal Attitudes Moderate the Impact of Weight Stigma on Avoidance of Exercise. Obesity. 2011;19(4):757–762. [DOI] [PubMed] [Google Scholar]
- 54.Greenleaf C, Petrie TA, Martin SB. Relationship of Weight-Based Teasing and Adolescents’ Psychological Well-Being and Physical Health. J Sch Health. 2014;84(1):49–55. [DOI] [PubMed] [Google Scholar]
- 55.Bucchianeri MM, Eisenberg ME, Wall MM, Piran N, Neumark-Sztainer D. Multiple Types of Harassment: Associations With Emotional Well-Being and Unhealthy Behaviors in Adolescents. J Adolesc Health. 2014;54(6):724–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Puhl RM, Luedicke J. Weight-Based Victimization Among Adolescents in the School Setting: Emotional Reactions and Coping Behaviors. J Youth Adolesc. 2012;41(1):27–40. [DOI] [PubMed] [Google Scholar]
- 57.Harriger JA, Thompson JK. Psychological consequences of obesity: Weight bias and body image in overweight and obese youth. Int Rev Psychiatry. 2012;24(3):247–253. [DOI] [PubMed] [Google Scholar]
- 58.Jendrzyca A, Warschuburger P. Weight stigma and eating behaviours in elementary school children: A prospective population-based study. Appetite. 2016;102:51–59. [DOI] [PubMed] [Google Scholar]
- 59.Mensinger JL, Calogero RM, Tylka TL. Internalized weight stigma moderates eating behavior outcomes in women with high BMI participating in a healthy living program. Appetite. 2016;102:32–43. [DOI] [PubMed] [Google Scholar]
- 60.Stice E, Gau JM, Rohde P, Shaw H. Risk factors that predict future onset of each DSM-5 eating disorder: Predictive specificity in high-risk adolescent females. J Abnorml Psych. 2017;126(1):38–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dakanalis A, Clerici M, Bartoli F, et al. Risk and maintenance factors for young women’s DSM-5 eating disorders. Arch Womens Ment Health. 2017;20(6):721–731. [DOI] [PubMed] [Google Scholar]
- 62.Risk Stice E. and maintenance factors for eating pathology: a meta-analytic review. Psychol Bull. 2002; 128(5):825–848. [DOI] [PubMed] [Google Scholar]
- 63.Polivy J, Herman CP. Dieting and binging. A causal analysis. Am Psychol. Feb 1985;40(2):193–201. [DOI] [PubMed] [Google Scholar]
- 64.Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychol Bull. Jul 1991;110(1):86–108. [DOI] [PubMed] [Google Scholar]
- 65.Bodell LP, Brown TA, Keel PK. Weight suppression predicts bulimic symptoms at 20-year follow-up: The mediating role of drive for thinness. J Abnorm Psychol. 2017;126(1):32–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wilson GT, Fairburn CC, Agras WS, Walsh BT, Kraemer H. Cognitive-behavioral therapy for bulimia nervosa: time course and mechanisms of change. J Consult Clin Psychol. 2002;70(2):267–274. [PubMed] [Google Scholar]
- 67.Steinbeck KS, Lister NB, Gow ML, Baur LA. Treatment of adolescent obesity. Nat Rev Endocrinol. 2018;14(6):331–344. [DOI] [PubMed] [Google Scholar]
- 68.Samdal GB, Eide GE, Barth T, Williams G, Meland E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int J Behav Nutr Phys Act. 2017;14(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kwasnicka D, Dombrowski SU, White M, Sniehotta F. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychol Rev. 2016;10(3):277–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yeh HC, Bantle JP, Cassidy-Begay M, et al. Intensive Weight Loss Intervention and Cancer Risk in Adults with Type 2 Diabetes: Analysis of the Look AHEAD Randomized Clinical Trial. Obesity (Silver Spring). 2020;28(9):1678–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jebeile H, Gow ML, Baur LA, Garnett SP, Paxton SJ, Lister NB. Association of Pediatric Obesity Treatment, Including a Dietary Component, With Change in Depression and Anxiety: A Systematic Review and Meta-analysis. JAMA Pediatr. 2019;173(11):e192841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Grilo CM, White MA, Masheb RM, Ivezaj V, Morgan PT, Gueorguieva R. Randomized controlled trial testing the effectiveness of adaptive “SMART” stepped-care treatment for adults with binge-eating disorder comorbid with obesity. Am Psychol. 2020;75(2):204–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ryan DH, Yockey SR. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. Curr Obes Rep. 2017;6(2):187–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Webb V, Wadden T. Intensive Lifestyle Intervention for Obesity: Principles, Practices, and Results. Gastroenterology. 2017;152(7):1752–1764. [DOI] [PubMed] [Google Scholar]
- 75.Maclean PS, Wing RR, Davidson T, et al. NIH working group report: Innovative research to improve maintenance of weight loss. Obesity. 2015;23(1):7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Diabetes Prevention Program Research Group, Nathan DM, Barrett-Conner E, et al. Long-term Effects of Lifestyle Intervention or Metformin on Diabetes Development and Microvascular Complications: The DPP Outcomes Study. Lancet Diabetes Endocrinol. 2015;3(11):866–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lindström J, Peltonen M, Eriksson JG, et al. Improved lifestyle and decreased diabetes risk over 13 years: long-term follow-up of the randomised Finnish Diabetes Prevention Study (DPS). Diabetologia. 2013;56(2):284–293. [DOI] [PubMed] [Google Scholar]
- 79.Gong Q, Zhang P, Wang J, et al. Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing Diabetes Prevention Outcome Study. Lancet Diabetes Endocrinol. 2019;7(6):452–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Willis EA, Huang W-Y, Saint-Maurice PF, et al. Increased frequency of intentional weight loss associated with reduced mortality: a prospective cohort analysis. BMC Medicine. 2020;18(1): 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.The Look AHEAD Study: A Description of the Lifestyle Intervention and the Evidence Supporting It. Obesity. 2006;14(5):737–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sivyer K, Allen E, Cooper Z, et al. Mediators of change in cognitive behavior therapy and interpersonal psychotherapy for eating disorders: A secondary analysis of a transdiagnostic randomized controlled trial. Int J Eat Dis. 2020;53(12):1928–1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gorin AA, Gokee LaRose J, Espeland MA, et al. Eating pathology and psychological outcomes in young adults in self-regulation interventions using daily self-weighing. Health Psychol. 2019;38(2):143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. The efficacy of a daily self-weighing weight loss intervention using smart scales and e-mail. Obesity. 2013;21(9):1789–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. Daily Self-Weighing and Adverse Psychological Outcomes. Am J Prev Med. 2014;46(1):24–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bray G, Frühbeck G, Ryan D, Wilding J. Management of Obesity. Lancet. 2016;387(10031):1947–1956. [DOI] [PubMed] [Google Scholar]
- 87.Looney SM, Raynor HA. Behavioral lifestyle intervention in the treatment of obesity. Health Serv Insights. 2013;6:15–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stice E, Rohde P, Shaw H, Desjardins C. Weight suppression increases odds for future onset of anorexia nervosa, bulimia nervosa, and purging disorder, but not binge eating disorder. Am J Clin Nutr. 2020;112(4):941–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Keel P, Heatherton T. Weight suppression predicts maintenance and onset of bulimic syndromes at 10-year follow-up. J Abnorm Psychol. 2010;9(2):268–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Keel P, Bodell L, Forney K, Appelbaum J, Williams D. Examining weight suppression as a transdiagnostic factor influencing illness trajectory in bulimic eating disorders. Physiol Behav. 2019;208:112565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Butryn ML, Juarascio A, Lowe MR. The relation of weight suppression and BMI to bulimic symptoms. Int J Eat Dis. 2011;44(7):612–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Call CC, D’Adamo L, Butryn ML, Stice E. Examining weight suppression as a predictor and moderator of intervention outcomes in an eating disorder and obesity prevention trial: A replication and extension study. Behav Res Ther. 2021;141:103850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Leite PB, Dâmaso AR, Poli VS, et al. Long-term interdisciplinary therapy decreases symptoms of binge eating disorder and prevalence of metabolic syndrome in adults with obesity. Nutr Res. 2017;40:57–64. [DOI] [PubMed] [Google Scholar]
- 95.Dombrowski SU, Knittle K, Avenell A, Araújo-Soares V, Sniehotta FF. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ. 2014;348:g2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Loveman E, Frampton GK, Shepherd J, et al. The clinical effectiveness and cost-effectiveness of long-term weight management schemes for adults: a systematic review. Health Technol Assess. 2011;15(2):1–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Rogge MM, Gautam B. Biology of obesity and weight regain. J Am Assoc Nurse Pract. 2017;29(S1):S15–S29. [DOI] [PubMed] [Google Scholar]
- 98.Blair SN, Shaten J, Brownell K, Collins G, Lissner L. Body weight change, all-cause mortality, and cause-specific mortality in the Multiple Risk Factor Intervention Trial. Ann Intern Med. 1993;119(7 Pt 2):749–757. [DOI] [PubMed] [Google Scholar]
- 99.Lee I-M, Paffenbarger RS. Change in Body Weight and Longevity. JAMA. 1992;268(15):2045–2209. [PubMed] [Google Scholar]
- 100.Hamm P, Shekelle RB, Stamler J. Large fluctuations in body weight during young adulthood and twenty-five-year risk of coronary death in men. Am J Epidemiol. Feb 1989;129(2):312–318. [DOI] [PubMed] [Google Scholar]
- 101.Cycling Weight. National Task Force on the Prevention and Treatment of Obesity. JAMA. 1994;272(15):1196–1202. [PubMed] [Google Scholar]
- 102.Fairburn C, Wilson G, Schleimer K. Binge eating: Nature, Assessment and treatment. New York: Guilford Press; 1993. [Google Scholar]
- 103.Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, Ward DS. Daily self-weighing and adverse psychological outcomes: a randomized controlled trial. Am J Prev Med. 2014;46(1):24–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Waller G, Mountford VA. Weighing patients within cognitive-behavioural therapy for eating disorders: How, when and why. Behav Res Ther. 2015;70:1–10. [DOI] [PubMed] [Google Scholar]
- 105.Sysko R, Hildebrandt T. Enhanced cognitive behavioural therapy for an adolescent with purging disorder: A case report. Eur Eat Disord Rev. 2011;19(1):37–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wilfley DE, Saelens BE, Stein RI, et al. Dose, Content, and Mediators of Family-Based Treatment for Childhood Obesity. JAMA Pediatr. 2017;171(12):1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Durso LE, Latner JD. Understanding self-directed stigma: development of the weight bias internalization scale. Obesity (Silver Spring). 2008;16 Suppl 2:S80–86. [DOI] [PubMed] [Google Scholar]
- 108.Lillis J, Luoma JB, Levin ME, Hayes SC. Measuring weight self-stigma: the weight self-stigma questionnaire. Obesity (Silver Spring). 2010;18(5):971–976. [DOI] [PubMed] [Google Scholar]
- 109.Pearl RL, Wadden TA, Chao AM, et al. Weight Bias Internalization and Long-Term Weight Loss in Patients With Obesity. Ann Behav Med. 2019;53(8):782–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lillis J, Thomas JG, Olson K, Wing RR. Weight self-stigma and weight loss during behavioural weight loss intervention. Obes Sci Pract. 2019;5(1):21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Diabetes Prevention Program (DPP) Research Groupp. The Diabetes Prevention program (DPP): Description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Brownell K The LEARN Program for Weight Management. American Health Publishing Company; 2004. [Google Scholar]
- 113.Pearl RL, Wadden TA, Bach C, et al. Effects of a cognitive-behavioral intervention targeting weight stigma: A randomized controlled trial. J Consult Clin Psychol. 2020;88(5):470–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pearl RL, Wadden TA, Bach C, Tronieri JS, Berkowitz RI. Six-Month Follow-up from a Randomized Controlled Trial of the Weight BIAS Program. Obesity (Silver Spring). 2020;28(10):1878–1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yalom I, Lescze M. Specialized Therapy groups. In The Theory and Practice of Group Psychotherapy. 5th ed: Basic Books/Hachette Book Group; 2005: 475–524. [Google Scholar]
- 116.Goffman E Stigma: Notes on the Management of a Spoiled Identity. Prentice Hall; 1963. [Google Scholar]
- 117.Pereira RF, Alvarenga M. Disordered Eating: Identifying, Treating, Preventing, and Differentiating It From Eating Disorders. Diabetes Spectr. 2007;20(3):141–148. [Google Scholar]
- 118.Wadden TA, Tsai AG, Tronieri JS. A Protocol to Deliver Intensive Behavioral Therapy (IBT) for Obesity in Primary Care Settings: The MODEL-IBT Program. Obesity (Silver Spring). 2019;27(10):1562–1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Goldschmidt AB, Aspen VP, Sinton MM, Tanofsky-Kraff M, Wilfley DE. Disordered Eating Attitudes and Behaviors in Overweight Youth. Obesity. 2008;16(2):257–264. [DOI] [PubMed] [Google Scholar]
- 120.Pearson AN, Follette VM, Hayes SC. A Pilot Study of Acceptance and Commitment Therapy as a Workshop Intervention for Body Dissatisfaction and Disordered Eating Attitudes. Cogn Behav Pract. 2012;19:181–197. [Google Scholar]
- 121.National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont Report. Ethnical Principles and Guidelines for the Protection of Human Subjects of Research. Department of Health, Education, and Welfare. 1979. [Google Scholar]
- 122.Cardel MI, Atkinson MA, Taveras EM, Holm JC, Kelly AS. Obesity Treatment among Adolescents: A Review of Current Evidence and Future Directions. JAMA Pediatr. 2020;174(6):609–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Moyer V Screening for and Management of Obesity in Adults: US Preventive Task Force Recommendation Statement. Ann Intern Med. 2012;157(5):373–378. [DOI] [PubMed] [Google Scholar]
- 124.O’Connor EA, Evans CV, Burda BU, Walsh ES, Eder M, Lozano P. Screening for Obesity and Intervention for Weight Management in Children and Adolescents. JAMA. 2017;317(23):2427. [DOI] [PubMed] [Google Scholar]
- 125.Newsome FA, Dilip A, Armstrong SC, Salloum RG, Cardel MI. Scaling‐up Stage 4 Pediatric Obesity Clinics: Identifying Barriers and Future Directions Using Implementation Science. Obesity. 2021;29(6):941–943. [DOI] [PubMed] [Google Scholar]
- 126.Stokes A, Collins JM, Grant BF, et al. Prevalence and Determinants of Engagement with Obesity Care in the United States. Obesity (Silver Spring). 2018;26(5):814–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kazdin AE, Fitzsimmons-Craft EE, Wilfley DE. Addressing critical gaps in the treatment of eating disorders. Int J Eat Disord. 2017;50(3):170–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Thompson C, Park S. Barriers to access and utilization of eating disorder treatment among women. Arch Women’s Ment Health. 2016;19(5):753–760. [DOI] [PubMed] [Google Scholar]
- 129.Hart LM, Granillo MT, Jorm AF, Paxton SJ. Unmet need for treatment in the eating disorders: a systematic review of eating disorder specific treatment seeking among community cases. Clin Psychol Rev. 2011;31(5):727–735. [DOI] [PubMed] [Google Scholar]
- 130.Jannah N, Hild J, Gallagher C, Dietz W. Coverage for Obesity Prevention and Treatment Services: Analysis of Medicaid and State Employee Health Insurance Programs. Obesity (Silver Spring). 2018;26(12):1834–1840. [DOI] [PubMed] [Google Scholar]
- 131.Wadden TA, Walsh OA, Berkowitz RI, et al. Intensive Behavioral Therapy for Obesity Combined with Liraglutide 3.0 mg: A Randomized Controlled Trial. Obesity (Silver Spring). 2019;27(1):75–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Dewar S, Bynum J, Batsis JA. Uptake of Obesity Intensive Behavioral Treatment Codes in Medicare Beneficiaries, 2012–2015. J Gen Intern Med. 2020;35(1):368–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Batsis JA, Huyck KL, Bartels SJ. Challenges with the Medicare obesity benefit: practical concerns & proposed solutions. J Gen Intern Med. 2015;30(1):118–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wilfley DE, Staiano AE, Altman M, et al. Improving access and systems of care for evidence-based childhood obesity treatment: Conference key findings and next steps. Obesity (Silver Spring). 2017;25(1):16–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Petersen R, Pan L, Blanck HM. Racial and Ethnic Disparities in Adult Obesity in the United States: CDC’s Tracking to Inform State and Local Action. Prev Chron Dis. 2019;16: E46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lewis KH, Gudzune KA, Fischer H, Yamamoto A, Young DR. Racial and ethnic minority patients report different weight-related care experiences than non-Hispanic Whites. Prev Med Rep. 2016;4:296–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Harvey JR, Ogden DE. Obesity treatment in disadvantaged population groups: Where do we stand and what can we do? Prev Med. 2014;68:71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Cardel MI, Chavez S, Bian J, et al. Accuracy of weight loss information in Spanish search engine results on the internet. Obesity. 2016;24(11):2422–2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sartorius N Stigmatized Illnesses and Health Care. Croat Med J. 2007;48(3):2396–2397. [PMC free article] [PubMed] [Google Scholar]
- 140.Crapanzano K, Hammarlund R, Ahmad B, Hunsinger N, Kullar R. The association between perceived stigma and substance use disorder treatment outcomes: a review. Subst Abuse Rehabil. 2018;10:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Stergiou-Kita M, Pritlove C, Kirsh B. The “Big C”—stigma, cancer, and workplace discrimination. J Cancer Surviv. 2016;10(6):1035–1050. [DOI] [PubMed] [Google Scholar]
- 142.Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16(4):319–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Alberga AS, Pickering BJ, Alix Hayden K, et al. Weight bias reduction in health professionals: a systematic review. Clin Obes. 2016;6(3):175–188. [DOI] [PubMed] [Google Scholar]
- 144.Pearl RL. Weight Bias and Stigma: Public Health Implications and Structural Solutions. Soc Iss Pol Rev. 2018;12(1):146–182. [Google Scholar]
- 145.Alberga AS, Edache IY, Forhan M, Russell-Mayhew S. Weight bias and health care utilization: a scoping review. Prim Health Care Research Dev. 2019;20: E116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Bacon L Health at Every Size (The Surprising Truth about Your Weight). Dallas: BenBella Books, Inc.; 2008. [Google Scholar]
- 147.Size diversity & health at every size. National Eating Disorder Association. Accessed January 18, 2021. https://www.nationaleatingdisorders.org/size-diversity-health-every-size
- 148.Bennet W, Gurin J. The Dieter’s Dilemma: Eating Less and Weighing More. New York: Basic Books; 1982. [Google Scholar]
- 149.McCormack L, Sheridan S, Lewis M, et al. Communication and dissemination strategies to facilitate the use of health-related evidence. Evid Rep Technol Assess (Full Rep). 2013(213):1–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Huang TT, Drewnosksi A, Kumanyika S, Glass TA. A systems-oriented multilevel framework for addressing obesity in the 21st century. Prev Chronic Dis. 2009;6(3):A82. [PMC free article] [PubMed] [Google Scholar]
- 151.Kumanyika SK. A Framework for Increasing Equity Impact in Obesity Prevention. Am J Public Health. 2019;109(10):1350–1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Perreault L, Laferrére B. Overweight and obesity in adults: Health consequences. 2020. Accessed February 3, 2022. https://www.uptodate.com/contents/overweight-and-obesity-in-adults-health-consequences?search=comorbidities-and-complications-of-obesity-in-&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1,
- 153.World Health Organization. Weight bias and obesity stigma: considerations for the WHO European Region. Accessed February 3, 2022. https://www.euro.who.int/__data/assets/pdf_file/0017/351026/WeightBias.pdf#:~:text=Weight%20bias%20and%20obesity%20stigma%3A%20considerations%20for%20the,and%2For%20prejudice%20towards%20people%20with%20overweight%20and%20obesity
- 154.Yager J Eating disorders: Overview of epidemiology, clinical features, and diagnosis. 2020. Accessed February 3, 2022. https://www.uptodate.com/contents/eating-disorders-overview-of-epidemiology-clinical-features-and-diagnosis?search=comorbidites%20eating%20disorder&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1, 2021.
- 155.Centers for Disease Control and Prevention. Adult Obesity Facts. 2021. Accessed February 3, 2022. https://www.cdc.gov/obesity/data/adult.html
- 156.National Eating Disorder Information Centre. General Information. Accessed February 3, 2022. https://nedic.ca/general-information/ [Google Scholar]
- 157.World Obesity Federation, Weight Stigma. Accessed February 3, 2022. https://www.worldobesity.org/what-we-do/our-policy-priorities/weight-stigma
- 158.Pearl RL, Wadden TA, Hopkins CM, et al. Association between weight bias internalization and metabolic syndrome among treatment-seeking individuals with obesity. Obesity. 2017;25(2):317–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kahan S, Puhl RM. The damaging effects of weight bias internalization. Obesity. 2017;25(2):280–281. [DOI] [PubMed] [Google Scholar]
- 160.American Psychiatric Association. What Are Eating Disorders? Accessed February 3, 2022. https://www.psychiatry.org/patients-families/eating-disorders/what-are-eating-disorders


