Abstract
Exposure to infant crying is a well-established predictor of mothers’ mental health. However, this association may reflect many potential mechanisms. Capturing dynamic fluctuations in mothers’ states simultaneously with caregiving experiences is necessary to identify the real-time processes influencing mental health. In this study, we leveraged ecological momentary assessments (EMA) and infant-worn audio recorders to capture variability in mothers’ mental health symptoms and their exposure to infant crying over one week in a racially and socio-economically diverse urban North-American sample (N = 53). We use multilevel modeling to characterize within- and between-person effects of crying on maternal negative affect and symptoms of depression and anxiety. Within participants, when infants cried more than average in the 10 minutes, 1 hour, and 8 hours prior to an EMA report, mothers’ negative affect subsequently increased, controlling for mean levels of infant crying. In contrast to findings from laboratory studies, in everyday settings crying exposure did not immediately increase feelings of depression. Only when crying was above average for eight hours prior to EMA did mothers report increases in subsequent depression symptoms, suggesting that the effects of crying on maternal mental health take hours to unfold in ecologically valid home settings. Between participants, mothers of infants who cried more on average did not report higher negative affect or symptoms of depression or anxiety. Overall, our findings reveal that crying exposure dynamically influences maternal negative affect and depression but not anxiety in ecologically valid real-world settings.
Keywords: maternal mental health, infant crying, LENA wearable audio recorders, ecological momentary assessment, multilevel modeling
Infant crying is a salient feature of a mother’s postpartum environment and has well-established associations with maternal mental health (Young et al., 2012). Crying duration peaks with nearly three hours of crying per day when infants are four to six weeks of age and stabilizes to approximately one hour per day by three months (Vermillet et al., 2022; Wolke et al., 2017). However, there are large individual differences in daily crying duration (Kurth et al., 2011; St James-Roberts & Plewis, 1996) and 5 – 25% of infants are identified with colic, or excessive crying (Lucassen et al., 2001; Wolke et al., 2017). Mothers who report their infants cry excessively also report experiencing higher levels of caregiver frustration (Barr et al., 2014; Fujiwara et al., 2011) and emotional distress (Miller et al., 1993), as well as higher concurrent depression and anxiety symptoms (Petzoldt, 2018). Furthermore, mothers of infants with a temperament profile which includes high levels of irritability and crying also exhibit higher levels of depression and anxiety symptoms (Britton, 2011).
Theoretical models propose that crying exposure influences maternal mental health directly, at the level of individual processes (Kurth et al., 2011; Papoušek & von Hofacker, 1995). For example, Dix’s Affective Organization of Parenting Model proposes that infant crying behaviors can activate immediate emotional reactions in caregivers (Dix, 1991). However, few studies examine how individual mothers’ mental health may fluctuate over real time, and we found no published work that examined the real-world, real-time individual processes by which crying exposure influences maternal mental health. This is critical as there are many potential mechanisms that could lead to group-level associations, i.e., associations between individuals vs. within individuals. Researchers increasingly recognize the need to disaggregate within- and between-persons effects to examine processes of change central to psychology (Berry & Willoughby, 2017; Curran & Bauer, 2011; Hoffman & Stawski, 2009). Infant crying may be associated broadly with elevated maternal distress due to stable or “trait-like” differences that increase risks for both factors (Shackman et al., 2016). For example, maternal anxiety and depression may be associated with caregiving behaviors thought to intensify infant crying, such as maternal intrusiveness or inefficiency of soothing interactions (Papoušek & von Hofacker, 1995), respectively. Thus, although mothers whose infants cry more may have more symptoms of depression or anxiety, by virtue of examining differences between mothers, whether cross-sectionally or longitudinally, extant studies do not permit inferences about the processes leading to these associations.
Experimental crying exposures in a laboratory setting lend initial evidence to the immediate causal effects of crying on maternal affect. Women exposed to 10-minute audio recordings of uncontrollable infant crying reported immediate increases in negative affect, including feelings of irritability, guilt, and hopelessness (Barr et al., 2014; Bruning & McMahon, 2009). However, mothers in Barr et al. (2014) were not exposed to their own infant’s crying and the women in Bruning and McMahon (2009) were female undergraduates not mothers, both of which may not fully represent the association between maternal affect and her infant’s crying. Additionally, these experimental paradigms distort crying in ways that are not representative of everyday crying exposures. For example, infant crying in everyday settings is more likely to occur in intense but relatively short bursts – lasting on average 3.6 seconds (Irwin, 2003) – compared to a continuous 10 minutes. Additionally, mothers’ actions can and often do help to soothe infant crying (Hubbard & van IJzendoorn, 1991), meaning that “everyday” crying is not necessarily uncontrollable. Thus, exposure to ecologically valid crying may be less likely to immediately induce caregiver distress. It is also possible that lab-based exposures are too short to fully characterize the effect of crying exposure over the course of a day. Clinical observations suggest that persistent crying (i.e., crying that extends for many hours in a day) may be a particular risk factor for maternal distress (Papoušek & von Hofacker, 1995). Extended periods of crying accumulated over hours may have distinct effects on maternal affect relative to immediate or short-term effects. We found no published study that systematically characterized the impact of exposure to infant crying over minutes and hours on maternal mental health in an ecologically valid setting.
Daily diary or ecological momentary assessment (EMA) studies are one approach that can be leveraged to access maternal mental health symptoms in the everyday context. In EMA studies, participants are repeatedly surveyed about their experiences on their mobile phones as they go about their lives. Relative to retrospective surveys in which participants are asked to report upon their experiences from the past few days or weeks, EMAs can reduce recall bias, which is especially common in assessments of emotional experience (Trull & Ebner-Priemer, 2013). Critically, EMA studies also allow researchers to document the processes by which mood and emotion may fluctuate over time (Ebner-Priemer & Trull, 2009). Research designs that combine mood reports with objective measures of experience can be used to test theories of real-time effects of everyday contexts on mental health (Buhler-Wassmann & Hibel, 2021; Hamaker & Wichers, 2017; Shiffman et al., 2008). For example, time-varying measures of crying exposure can be time-locked to self-report surveys to assess lagged associations between infant crying and maternal mental health. Such high-density multimodal datasets can test precisely to what extent and at what timescales dynamic fluctuations in cry exposure explain subsequent within-person changes in maternal affect and mental health.
Advances in wearable sensors, paired with algorithms that can automatically detect markers of interest, provide a relatively low-burden method for capturing large volumes of objective measures of context, including infant crying (de Barbaro, 2019; Micheletti et al., 2022). Researchers have successfully used sensors to assess objective measures of sleep, physical activity, and even geographic location as real-time predictors of mental health (Mohr et al., 2017). We build on this work by collecting automatically detected infant crying as a predictor of women’s mental health postpartum. Parent reports are known to over-estimate crying by a factor of three (Cabana et al., 2021) and maternal psychological distress has been shown to have a small but significant biasing effect on reports of child crying behaviors (Atella et al., 2003). As such, objective markers of infants’ crying can reduce shared measurement bias between assessments of maternal mental health and this common caregiving experience. Additionally, by virtue of providing precise, quantitative data about the amount of crying experienced by caregivers in the minutes and hours prior to EMA mood reports, wearable sensors could be used to examine potentially distinct effects of naturally occurring crying immediately vs. at longer timescales on mothers’ mental health.
We considered objective markers of cry duration as independent, continuous predictors of maternal mental health. Most past work examined associations between maternal mental health and exposure to excessive infant crying, defined as more than two or three hours of crying per day, for 2-3 days per week over the course of multiple months, as reported by the mother (Wessel et al., 1954). However, inconsistencies between parent-reported and objectively detected amounts of infant crying mean it is unclear how to validly translate this threshold to objective cry data. Additionally, if crying exposure has continuous effects on women’s mental health, this would suggest that women could more broadly benefit from interventions aimed to either reduce infant crying or reduce mothers’ crying-related distress. As such, reviews of this literature (Kurth et al., 2011) suggest that new studies should examine the continuous effects of crying on maternal mental health.
The current study
To understand the extent of naturally occurring fluctuations in women’s mental health and the extent to which they can be predicted by recent crying exposure, we combined ecological momentary assessments of maternal mental health with automatically detected markers of infant crying collected from audio recorders worn by infants in their naturalistic environments for up to 72 hours over the course of one week. Drawing from clinical observations (Papoušek & von Hofacker, 1995), we tested whether crying exposure had distinct effects when occurring immediately prior to an EMA report (10 minutes or 1 hour) vs. when it was accumulated over multiple hours of the day (8 hours).
Study hypotheses
Our first hypothesis was that mothers’ mental health, indexed as negative affect and symptoms of depression and anxiety, would fluctuate over the course of the week. Second, we hypothesized that exposure to more infant crying would lead to mothers reporting higher negative affect, depression symptoms, and anxiety symptoms, both between- and within-persons. Third, we hypothesized that mothers who were exposed to more-than-average infant crying in recent minutes as well as persistently over the course of hours would report higher negative affect, depression symptoms, and anxiety symptoms. The alternative hypothesis was that crying exposure poses only immediate, short-term effects on mothers, which do not persist after one or more hours.
Methods
Participants
We recruited a diverse population of mothers and infants via convenience sampling from the Austin, Texas metropolitan area. We advertised the study using Facebook, online university event calendars, and fliers posted in local community health centers. Exclusion criteria included infants older than 12 months, infants with congenital birth defects or a genetic condition affecting development (e.g., Down syndrome), multiple birth infants, and families with a primary residence located over 20 miles from the research center.
Mother-infant dyads (n = 87) were recruited in the context of a broader study leveraging wearable sensors to measure mother and infant behavior in the home. After an initial piloting phase with n = 28 mothers who tested the survey platform and provided feedback on user experience and feasibility, n = 59 mothers received mobile surveys asking about their mental health. Three mothers were excluded because they did not answer any surveys. An additional three mothers were excluded because they responded to only two surveys. The final sample included n = 53 mother-infant dyads. Table 1 shows participant characteristics. Infants were on average 3.9 months of age (SD = 2.2, range = 0.9-10.6 months) and 53% were female; 57% of dyads were Non-Hispanic white.
Table 1.
Participant characteristics (n = 53)
| M (SD), Range or N (%) | |
|---|---|
| Infant | |
| Age, months | 3.9 (2.2), 0.9 – 10.6 |
| Gestational age, weeks | 39 (2), 31 – 41 |
| Female sex | 29 (52%) |
| Mother | |
| Age, years | 31(6), 18 – 43 |
| Female sex | 53 (100%) |
| Education | |
| High school or less | 9 (17%) |
| Some college or trade school | 14 (26%) |
| College | 14 (26%) |
| Graduate School | 16 (31%) |
| Race/Ethnicity | |
| White, Hispanic | 6 (11%) |
| White, Non-Hispanic | 30 (57%) |
| Black | 4 (8%) |
| Hispanic | 10 (19%) |
| Asian | 1 (2%) |
| Multiracial | 2 (4%) |
| Employment | |
| Full-time | 21 (40%) |
| Part-time | 10 (19%) |
| Not employed out of the home | 22 (41%) |
| Family Status | |
| Married | 38 (72%) |
| Divorced | 1 (2%) |
| Single Parent | 5 (9%) |
| Living with a partner without marriage | 9 (17%) |
| Household Income | |
| Under $25k | 9 (17%) |
| $25k – 49k | 8 (15%) |
| $50k – 74k | 10 (19%) |
| $75k – 99k | 9 (17%) |
| Over $100k | 17 (32%) |
| Primary Household Language | |
| English | 44 (83%) |
| Spanish | 9 (17%) |
| First-time mothers | 19 (36%) |
Overall column includes mean (standard deviation), range or frequency count (%)
Procedure
The University of Texas at Austin’s Institutional Review Board approved the study design and data collection (Protocol: 2017-06-0026). Data were collected from September 2018 to February 2020.
Introductory session.
A research assistant conducted a 90-minute study introduction in each participant’s home. Research assistants obtained written informed consent, configured devices, and collected baseline information from mothers and infants while they wore the devices. The study was conducted in English or Spanish depending on the household’s primary language.
Home-recording session.
Following the introductory session, research assistants instructed mothers how to record 72 hours of data over the course of the following week (Figure 1). Mothers were asked to record one 48-hour shift during which they planned to be with their child, typically the weekend, and two 12-hour shifts overnight. We selected these recording windows because they were largely feasible for mothers working full-time out of the home, while still allowing for ample continuous device wear time. To maximize adherence to the recording paradigm, mothers selected their recording windows during the introductory session and were reminded to record during the week by text messages from a research assistant. Following the session, we compensated mothers $100 for participation and infants received a small toy.
Figure 1. Study protocol.
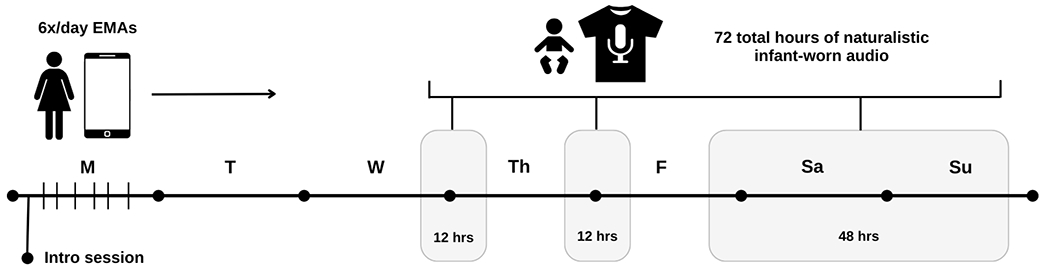
Note. Following a 90-minute introductory session in the home, mothers completed 6 EMAs per day and infants wore audio recorders for a total of 72 hours over the course of 7 days. EMA = ecological momentary assessment; audio = LENA recording device.1
Measures
Given evidence that negative affect shifts dynamically throughout the day (Trull & Ebner-Priemer, 2013), we used ecological momentary assessments (EMAs) to capture mothers’ immediate reports of negative affect six times per day. Mothers’ anxiety and depression symptoms were assessed once per day in the evening. Anxiety and depression symptoms are not commonly assessed with high-density EMA designs (see reviews by ann het Rot et al., 2012; Ebner-Priemer & Trull, 2009), likely because they are theorized to reflect more stable or slowly changing clinical states. Indeed, a recent study that collected morning and evening depression surveys for six weeks found that morning and evening depression symptom levels were highly correlated (Targum et al., 2021). As such, we collected depression and anxiety symptoms by EMA one time per day in the evening, between 19:10 – 22:00. All surveys were delivered to the mothers via a text message containing a link to a two- to three-minute online Qualtrics survey (Hofmann & Patel, 2014). Signals were considered semi-random because they were delivered at least two hours apart, but at otherwise random times between 05:00 – 07:49, 07:50 – 10:39, 10:40 – 13:29, 13:30 – 16:19, 16:20 – 19:09, and 19:10 – 22:00.
Negative affect.
Mothers were asked to report momentary feelings of negative affect six times per day by responding to a subset of items on the Positive and Negative Affect Schedule, PANAS (Peeters et al., 2003; Watson et al., 1988). Mothers read each of the following words and responded on a scale from 1 (not at all) to 7 (very) to indicate how strongly they felt that affect in the present moment: tense, anxious, guilty, irritable, and easily distracted. Following Peeters and colleagues (2006) we included the item ‘easily distracted’ as their research suggests it is important to include activation/arousal dimensions (in addition to traditional pleasantness/unpleasantness dimensions) in measures of momentary negative affect because they capture clinically relevant aspects of daily emotional experience. To minimize response burden of our dense EMA sampling schedule, we excluded three of the eight items from the original scale (irritated, restless, and agitated) based on their overlap with the remaining items. To obtain a single negative affect score, we summed mothers’ responses at each EMA administration with scores ranging from 5 – 35; higher scores indicate higher levels of momentary negative affect. Between-person (ω = 0.93) and within-person (ω = 0.77) reliabilities were high.
Depression.
Mothers reported daily levels of depression symptoms once per day in the evening. Depression was measured with the well-validated Patient Health Questionnaire-2 (PHQ-2; Kroenke et al., 2009), a two-item measure used to assess depression symptom severity. Mothers were prompted to “think about today” and on a scale from 0 (very slightly or not at all) to 4 (extremely) rate the extent to which they had felt “little interest or pleasure in doing things” and “down, depressed, or hopeless.” Total scores ranged from 0 – 8, with higher scores indicating higher symptomatology. The anhedonia criterion for depression was defined by “little interest or pleasure in doing things” and the depressed mood criterion was represented by “down, depressed, or hopeless.” Between-person reliability (ω = 0.88) was higher than within-person reliability (ω = 0.32), meaning that responses on the PHQ-2 were not consistent within individual measurement occasions. However, this is expected given that the two items capture different criteria for depression symptomatology.
Anxiety.
Anxiety symptoms were measured once per day in the evening using the well-validated Generalized Anxiety Disorder 2-item (GAD-2; Kroenke et al., 2009). On a scale from 0 (very slightly or not all) to 4 (extremely), mothers rated the extent to which they were “feeling nervous, anxious, or on edge” and “not being able to stop or control worrying” thinking about today. Scores ranged from 0 – 8 where higher scores reflect more anxiety symptoms. Between-person (ω = 0.89) and within-person (ω = 0.68) reliabilities were high.
Infant crying.
Objective measures of infant crying duration were obtained using Language EnviroNment Analysis (LENA) technology (Xu et al., 2009). The LENA device is a small, child-safe recorder worn in a vest over the infant’s clothing. The device records the infant’s voice as well as other voices and sounds in the environment up to 10 feet away. We collaborated with LENA technology to increase the device’s storage capacity so it can record for a continuous 24 hours. During infant bathing and sleep, mothers removed the vest but kept it nearby and recording to continue capturing ambulatory audio.
To capture infant crying in recent minutes as well as persistent crying over the course of hours, we calculated time-varying measures of crying across three different time intervals preceding each survey response for each mother: 10 minutes, 1 hour, and 8 hours. We selected these intervals a priori because they allowed us to examine the short-term effects of crying (similar to lab-based experiments where 10-minute audio recordings were played for mothers) as well as explore a potential long-term effect of crying over the course of the day, where persistent crying may be more distressing. We chose 8 hours to maximize usable data within our recording paradigm; we could not evaluate the effect of crying in the past 24 hours on negative affect and symptoms of depression and anxiety because the LENA device was often not worn continuously for a full day prior to each survey response. We also considered including crying in the 3 hours preceding survey response as an additional predictor, but it was highly correlated to 1 hour (r = .73) and 8 hours (r = .80), so we did not include it given our relatively small sample size.
Infants had to be wearing LENA for at least 70% of the intended time interval (i.e., in the previous 10 minutes, 1 hour, or 8 hours) for their data to be included in each analysis. Crying values were normalized per minute and scaled up to the full interval. For example, if an infant wore LENA for 7 of the last 8 hours, cry duration was normalized per minute and scaled up to the full 8 hours.
Any nonverbal vocal expression of negative emotion, including cries, fusses, whines, and whimpers were automatically identified by LENA as “crying” (Fields-Olivieri & Cole, 2019). As LENA’s cry algorithm has been shown to underestimate crying time relative to human annotations (Micheletti et al., 2022), we compared LENA’s cry output to human annotations of cry for 40% of our participants. Trained human coders annotated 24-hour recordings for n = 22 participants quasi-randomly selected to represent the age distribution of our overall sample. A cry had to have a minimum duration of three seconds and fusses/whines/whimpers had no minimum duration (Gilkerson et al., 2017); all were combined and referred to as cries. Human coders achieved a Cohen’s kappa of 0.77 for detecting cry and non-cry episodes, which represents a moderate to strong level of agreement (McHugh, 2012). We found that LENA underestimated cry duration by a factor of three, missing up to 48 minutes of crying every 24 hours. Given this sizeable discrepancy, we estimated a linear regression model to predict human-annotated cry durations from LENA outputs at each time interval. Then, we used the parameters of this regression to predict human-annotated crying from LENA output at each time interval (see Table 2 for regression equations). In effect, we multiplied all original durations by approximately a factor of three which resulted in cry estimates that more closely approximate the gold-standard human-annotated values for each time frame. Converging evidence suggests that a correction factor should be applied to LENA crying data to compensate for its underestimation of child vocalizations (Cristia et al., 2020; Micheletti et al., 2022). This transformation is equivalent to changing from one unit to another and thus has no effect on our results. The main benefit is that it provides a more accurate estimate of infant crying duration – that is, the transformed values are more representative of the true durations of crying as coded by trained research assistants.
Table 2.
Correlations and linear regressions between LENA and human-annotated crying by time interval
| Time Interval Preceding EMA Response | R | Regression Equation |
|---|---|---|
| 10 minutes | 0.68 | y = 2.8268x + 0.2253 |
| 1 hour | 0.72 | y = 2.9304x + 0.6545 |
| 8 hours | 0.73 | y = 2.8488x + 10.743 |
Note. Linear regression where y = human-annotated crying and x = LENA-detected crying.
In addition to cry duration, we also considered evaluating cry frequency, or the number of cries in each time interval. However, cry frequency was highly correlated with cry duration at 10 minutes (r = 0.92), 1 hour (r = 0.90) and 8 hours (r = 0.72). To minimize our total number of comparisons, and because much of the existing literature focuses on total crying time, we evaluated cry duration only (Kurth et al., 2011).
Data Analysis
All data analyses were conducted in R (4.2.1) and R Studio (v2022.07.1). First, we calculated single rater, one-way random effects intra-class correlation coefficients (Bliese, 2000) to describe the percentage of total variance in negative affect, depression and anxiety symptom scores accounted for by between- and within-person differences. We also calculated correlations between negative affect, depression symptoms, and anxiety symptoms to evaluate the extent to which our outcomes were associated in real time.
Given the skewness of our observed data, we calculated which transformation (log, square root, or exponential) would result in the most normally distributed data for each predictor and outcome variable (Peterson & Cavanaugh, 2020). We then applied the best normalizing transformation to each predictor and outcome variable to prepare for multilevel regression analyses (see Table 3). Next, we used two-level multilevel modeling with maximum likelihood estimation and robust standard errors to account for repeated observations nested within persons. Random intercepts were allowed for level 2 (participant) membership. We tested infant crying in the prior 10 minutes, 1 hour, and 8 hours as a predictor of subsequent negative affect, depression symptoms, and anxiety symptoms. Each model included within-person variability in crying and person-centered mean crying calculated across all observations.
Table 3.
Estimated Normality Statistic by Transformation Type
| log | square root | exponential | |
|---|---|---|---|
| Negative affect | 5.5526 | 5.2018 | 178.2202 |
| Depression symptoms | 15.2903 | 15.1315 | 25.9884 |
| Anxiety symptoms | 7.2528 | 7.1515 | 24.6302 |
| 10 min cry duration | 30.0647 | 32.3507 | 43.1608 |
| 1 hr cry duration | 11.0131 | 11.341 | 13.88 |
| 8 hr cry duration | 11.247 | 6.4279 | 56.496 |
Note. Estimated normality statistic is measured by Pearson P / degrees of freedom, where lower values reflect a more normal distribution. The best normalizing transformation (in bold) was applied to each variable prior to multilevel modeling.
Infant age (in weeks), first-time mothers (1=yes; 0=no), and maternal education (high school or less, some college or trade school, college, graduate school) were selected a priori to be included as covariates in all models. We included infant age because crying in a younger vs. older infant could have different effects on maternal mood and mental health, e.g., as older infants spend less time crying per day (Vermillet et al., 2022; Wolke et al., 2017), crying more than usual for an older infant may be more unexpected and thus more distressing. We also controlled for first-time mothers, considering that first-time mothers may have less caregiving experience and may be more affected by their infant’s crying. For example, first-time mothers have been shown to be less confident in interpreting their infant’s cues and more likely to report crying as a problem relative to multiparous mothers (Canivet et al., 2005; Drummond et al., 1993). Lastly, we included maternal education to serve as a marker of socioeconomic status, particularly because lower maternal education has been associated with higher parenting stress (Fang et al., 2022), and higher parenting stress may contribute to a reduced reactivity to an infant’s cries (Kim et al., 2020).
Given our relatively small sample size and the issue of multicollinearity we did not include all remaining demographic variables in our models. Thus, for the remaining demographic variables we took a bottom-up approach and tested the association between all potential covariates via regression or chi-squared test. We found that maternal education was significantly related to income (X2= 1286.9, p<.001), family status (X2= 559.01, p<.001), employment (X2= 322.58, p<.001), and maternal age (B=2.5, p<.001). Specifically, higher maternal education was associated with higher family income, more married couples, more mothers working full-time, and older mothers, so we included only maternal education as a marker of socioeconomic status in each model.
A power analysis based on 1,000 Monte Carlo simulations showed that this study was powered at an average of 87% to detect medium-sized effects of 0.5 and powered at an average of 52% to detect small-sized effects of 0.2 with an alpha level of .05 (Green & MacLeod, 2016). Given the normalizing transformations applied to our data, estimated beta values cannot be directly interpreted. Thus, to facilitate comparison across predictors, for all models we report standardized coefficients (β), equivalent to the change in the outcome variable associated with a standard deviation change in the predictor variable (Snijders & Berkhof, 2008).
This study was not preregistered. Data and study materials from this study are not publicly available. Syntax for our linear mixed effects models is presented in the supplementary information.
Results
Mothers responded to an average of 33 of 42 planned EMA survey signals (SD = 11, median = 33, range = 10 – 52). Considering only the last EMA of the day (where depression and anxiety were reported), mothers responded to an average of 6 of 7 planned surveys signals (SD = 2, range 0 – 10). Out of the scheduled 72 hours of device wear time, infants wore the LENA for a mean 71 hours (SD =17, range = 17 – 103). As common in ambulatory assessment research, we observed large ranges in the amount of EMA and LENA data collected per participant. However, EMA-audio pairs were only included in each analysis if there was sufficient overlap in the timing between the EMA and the cry detection windows (i.e., at least 70% of audio available for each time-locked window). Note that due to technical difficulties, we scheduled an additional 1-3 days of data collection to obtain concurrent LENA and EMA data for n = 11 participants. This means that some participants completed surveys for more than 7 days, which accounts for the high end of some ranges.
Table 4 shows descriptive summaries of EMA responses and infant crying at the person-centered mean level. Given that the PHQ-2 and GAD-2 were validated on a retrospective report of the past 2 weeks, while we ask about the current day, we cannot compare clinical cutoffs directly. However, 35 mothers (66%) reported a PHQ-2 score greater than 0 on at least one occasion, endorsing symptoms “a little”, while 18 mothers (34%) reported a 3 or higher on at least one occasion, indicating symptoms “quite a bit” to “extremely”. For the GAD-2, 44 mothers (83%) reported a score greater than 0 at least once and 28 mothers (53%) reported a 3 or higher at least once.
Table 4.
Descriptive statistics on survey responses and infant crying durations at the person-centered mean level
| n | M (SD) | Range | |
|---|---|---|---|
| EMA Survey | |||
| Negative affect | 53 | 11.5 (4.6) | 5.6 – 24.4 |
| Depression symptoms | 52 | 0.9 (1.3) | 0 – 5.3 |
| Anxiety symptoms | 52 | 1.4 (1.4) | 0 – 6 |
| Infant crying (minutes) | |||
| 10 minutes | 45 | 0.4 (0.2) | 0.2 – 1.0 |
| 1 hour | 45 | 2.1 (0.7) | 1.3 – 4.9 |
| 8 hours | 45 | 13.0 (4.0) | 6.2 – 23.4 |
After correcting for skewness, we found that reports of negative affect were correlated with depression symptoms at r = 0.47 and anxiety symptoms at r = 0.65. Symptoms of depression and anxiety were also correlated at r = 0.56. This suggests that although there is some shared variance in our measures, as is expected given their high rates of co-occurrence (Brown et al., 2001), our main outcomes measures do not entirely overlap and therefore additional variance in scores could be explained by exposure to infant crying.
Intraclass Correlation Coefficients
Variance attributable to between-person differences was 0.62 for negative affect, 0.63 for depression symptoms, and 0.53 for anxiety symptoms. The inverse of these values is attributable to within-person differences. Figure 2 shows the range and variability of EMA responses and crying durations at 1 hour between and within persons. For example, there is more within-person variability in anxiety symptoms (0.47) than depression symptoms (0.37), meaning that mothers in our sample showed more day-to-day variability in their reports of anxiety symptoms compared to depression symptoms.
Figure 2. Within-person variability in maternal negative affect, depression and anxiety symptoms, and infant crying.
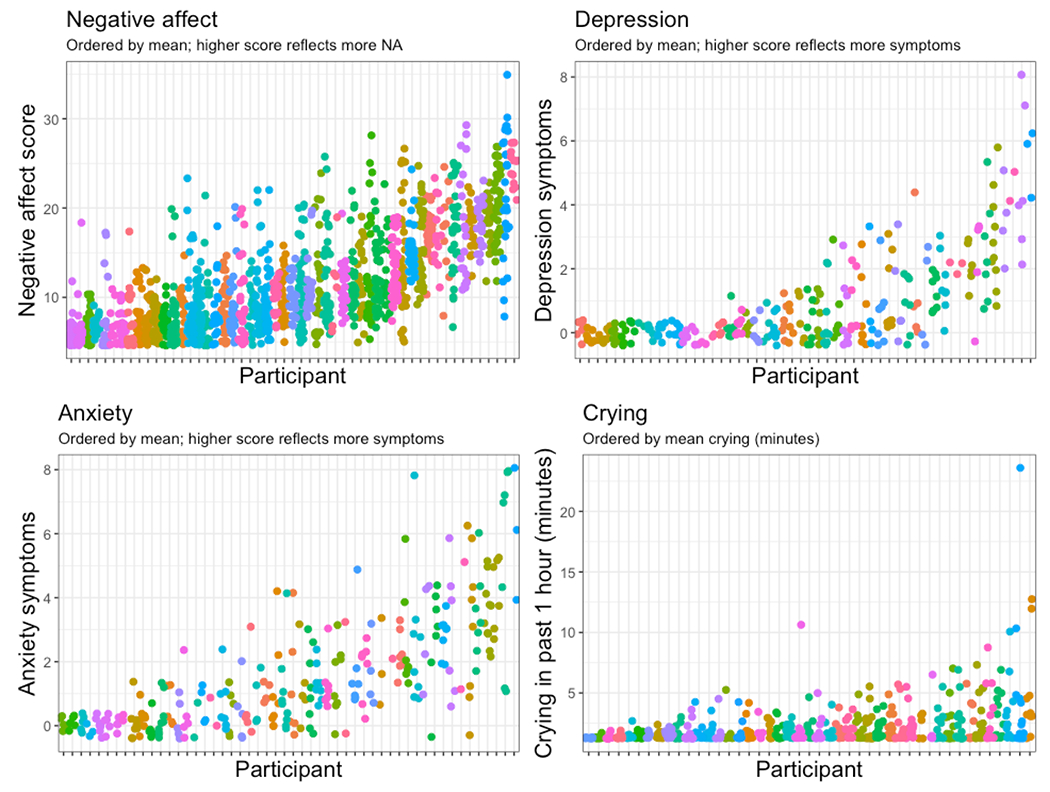
Within-person variability in negative affect, 38%; depression symptoms, 37%; anxiety symptoms, 47%; and crying duration in the past 1 hour, 93%. Each column represents one participant’s data, reflecting either raw mental health scores from each completed survey or crying detected in the 1 hour prior to each completed survey. Scores are jittered and participants are ordered from left to right by mean level to illustrate within-person variability.
Multi-level modeling
Each model included the within-person variability in crying and the person-centered mean crying calculated across all observations. Separating crying exposure at each occasion into these two variables allows us to distinguish whether mothers’ mental health symptoms are associated with between-persons differences in mean crying exposure (e.g., mothers of infants who on average tend to cry more vs. less) or whether mothers’ mental health symptoms shift as a function of within-person changes in crying exposure (i.e., when a mother is exposed to more or less crying than usual, for that mother). Within-person deviations are equivalent to centering each participants’ crying exposure at zero to examine how positive vs. negative deviations from their own mean continuously predict our outcomes. Table 5 summarizes model results.
Table 5.
Standardized beta coefficients from linear mixed models predicting momentary reports of mental health from infant crying at varying timescales
| Negative affect | Depression symptoms | Anxiety symptoms | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| Infant crying | n | Beta | CI | p | n | Beta | CI | p | n | Beta | CI | p |
| Within-person variation | ||||||||||||
| 10 minutes | 44 | 0.10*** | 0.18, 0.55 | <.001 | 43 | 0.11 | −0.20, 0.62 | .323 | 43 | −0.01 | −0.58, 0.52 | .881 |
| 1 hour | 44 | 014*** | 0.35, 0.78 | <.001 | 42 | 0.11 | −0.18, 0.70 | .248 | 42 | 0.02 | −0.38, 0.50 | .800 |
| 8 hours | 44 | 0.07** | 0.02, 0.10 | .006 | 36 | 0.35* | 0.02, 0.29 | .027 | 36 | 0.18 | −0.05, 0.23 | .236 |
| Person-centered mean | ||||||||||||
| 10 minutes | 44 | −0.02 | −2.55, 2.20 | .884 | 43 | 0.01 | −1.33, 1.39 | .964 | 43 | −0.01 | −1.97, 1.87 | .955 |
| 1 hour | 44 | 0.17 | −0.81, 3.74 | .216 | 42 | 0.12 | −0.71, 1.86 | .385 | 42 | 0.23 | −0.46, 3.14 | .154 |
| 8 hours | 44 | 0.02 | −0.30, 0.36 | .859 | 36 | 0.06 | −0.17, 0.25 | .708 | 36 | 0.09 | −0.30, 0.46 | .585 |
Note. Significance thresholds:
p < .05,
p <.01,
p <.001.
Within each model, we included the within-person variation and person-centered mean as predictors. Infant age, first-time mothers, and maternal education were included as covariates in all models.
Negative affect.
Within-person, mothers reported significantly higher negative affect on the occasions when their infant cried more-than-average in the 10 minutes (b=.102, p<.001), 1 hour (b=.138, p<.001), and 8 hours (b=.074, p=.006) prior to completion of individual mood reports. That is, on occasions when mothers were exposed to more infant crying than usual in the prior 10 minutes, 1 hour, and 8 hours, they reported significantly higher negative affect as compared to occasions when their infants cried less. Ratings of negative affect were not related to infants’ mean crying duration in the 10 minutes, 1 hour, or 8 hours prior to EMA response. None of our covariates significantly predicted negative affect across models.
Depression symptoms.
Within-person, on occasions that infants cried more than average in the 8 hours prior to the evening EMA, mothers reported higher ratings of depression symptoms relative to occasions when their infants cried less over the prior 8 hours (b=.354, p=.027). In this model, we also found that that when exposed to the same amount of crying, mothers with some college reported higher depression symptoms than mothers with a college degree when exposed to more than average crying in the past 8 hours (p=.015). Within-person changes in crying in the 10 minutes or 1 hour prior to the evening EMA did not predict depression symptoms. Between-person, infants’ mean crying, relative to other infants, did not predict symptoms of maternal depression at 10 minutes, 1 hour, or 8 hours.
As the PHQ-2 is comprised of two items that capture different criteria for depression – anhedonia (“little interest or pleasure in doing things”) and low mood (“sad, depressed, or hopeless”) – we conducted a post hoc analysis to evaluate if one item was driving our within-person results at the 8-hour timescale. We found that within-person increases in infant crying in the 8 hours prior to the evening EMA predicted higher reports of anhedonia relative to occasions in which infants cried less (b=.236, p=.021), but not low mood (b=.049, p=.558).
Anxiety symptoms.
No within-person changes in crying predicted daily symptoms of anxiety. Similarly, symptoms of anxiety were not predicted by infants who cried on average more in the 10 minutes, 1 hour, or 8 hours prior to EMA response.
Discussion
To observe the real-time processes by which crying exposure influences maternal mental health in the everyday context, we used objective markers of infant crying to predict in-the-moment reports of mothers’ negative affect and symptoms of depression and anxiety over the course of one week. Overall, our results indicated that recent within-person increases in exposure to infant crying predicted higher maternal negative affect and depression symptoms, controlling for mean levels of our predictors. We also observed that mean levels of crying exposure did not predict mothers’ reports of negative affect or symptoms of depression or anxiety. Our findings reveal a dynamic within-person relationship between crying exposure and maternal mental health, providing the first evidence that infant crying influences mother’s mental health at the level of the individual process in an ecologically valid setting.
Ecological momentary assessments indicated that mothers’ negative affect and symptoms of depression and anxiety were not static; they fluctuated over the course of the week with 38-47% of variance attributable to within-person change. This meaningful within-person variability in mental health symptoms is broadly consistent with findings from the EMA literature (Ebner-Priemer & Trull, 2009), however, this is one of the first studies to examine such variability in a community sample of postpartum women (see also Bowen et al., 2012; Mendez et al., 2019).
We also found that dynamic fluctuations in infant crying, controlling for mean levels of crying, predicted mothers’ feelings of negative affect and depression symptoms with distinct patterns across timescales. Variability in crying predicted negative affect at all time intervals, indicating that when mothers were exposed to more-than-average crying they subsequently felt worse mood immediately (at 10 minutes and 1 hour) as well as throughout the day (at 8 hours), relative to occasions when their infants cried less. Thus, we extend findings from the laboratory (Barr et al., 2014; Bruning & McMahon, 2009) to an everyday caregiving setting, that crying exposure can lead to increases in negative affect.
Additionally, our findings indicate distinct effects of crying over longer relative to shorter timescales. Within-person exposure to crying was associated with increases in depression symptoms, but only when crying was higher-than-average summing across the prior eight hours (i.e., when crying was more persistent than usual for the entire day). This effect was significant only for the anhedonia item of the PHQ-2, not low mood, which suggests that exposure to higher-than-average crying over the course of the day may manifest in postpartum women as more anhedonia (e.g., losing interest or pleasure in activities) vs. a depressed mood state (e.g., feeling sad, hopeless, empty, or overwhelmed). We also found that within person, higher amounts of crying for shorter periods of time i.e., 10 minutes or 1 hour – even when above average – did not appear to increase mothers’ feelings of depression relative to when their infants cried less. It is possible that mothers can cope or self-regulate when crying is above average for short periods of time, but as this time increases, mothers’ resources become depleted and we begin to observe effects on mental health, similar to the cumulative negative effects of stress on mental health over prolonged periods of time (Mcewen, 2004). These findings are not possible to obtain with traditional laboratory studies in which it is practically infeasible to manipulate exposure to crying for hours at a time.
More broadly, reports of depression symptom severity were less labile relative to negative affect, perhaps reflecting underlying differences in the process and rate at which affect and mood vary within individuals as a result of recent caregiving experiences. Of note, the null effects on depression and anxiety at shorter timescales may be the result of these reports being collected only once per day (vs. negative affect six times per day). As such, there may not have been enough samples at the 10 minute and 1 hour timescales to detect results, a point we explore further in the limitations section.
Our between-person findings revealed that mean levels of crying exposure in the previous 10 minutes, 1 hour, and 8 hours did not predict mothers’ reports of negative affect or symptoms of depression or anxiety. This is in contrast to previous findings that show longer and more frequent infant crying is associated with postpartum depression and anxiety (Britton, 2011; Petzoldt et al., 2016). However, these studies often relied on parent reports of infant crying, which may have led to shared measurement bias, and used thresholds for excessive or persistent infant crying, which our non-clinical, community sample of infants may not have met. Of note, a large systematic review of longitudinal studies of maternal depression, anxiety, and infant crying (Petzoldt, 2018) reported that excessive crying predicts future depression but not anxiety, which is consistent with our findings that within-person exposure to more crying is associated with real-time and same-day increases in negative affect and depression symptoms, but not anxiety symptoms, at the level of individual processes.
We also note that two models revealed a significant effect of maternal education, such that women with some college education exhibited more symptoms of depression, and specifically reports of anhedonia, compared to women with a college degree when exposed to more than average crying in the past 8 hours. This speaks to a possible risk factor associated with lower levels of maternal education, which is consistent with existing literature (Britton, 2008; Wesselhoeft et al., 2020). However, we interpret these results with caution as we find differences among women who all received some college education or higher; further research with a sample more diverse in levels of education is warranted.
Strengths and Limitations
The main strengths of this study are its use of a high-density, multimodal dataset to capture crying exposure and measures of affect and mood in real time, thus minimizing recall or reporting bias, as well as utilizing multilevel modeling to disaggregate and test hypotheses about between- and within-person effects. The simultaneous evaluation of negative affect, depression, and anxiety also facilitated our ability to examine the specificity of mother’s mental health experiences in respect to crying exposure at different timescales. We also controlled for infant age, being a first-time mother, and maternal education in our statistical models. As such, our results are unlikely to simply reflect a mother’s level of experience with a crying infant or her level of education, or only extend to a specific developmental window in infancy. Finally, the community-based nature of our sample supports the generalization of our findings to the broader population.
The present study also had several limitations. Participants were obtained through convenience sampling, meaning the sample is not representative of any specific postpartum community, despite representing socio-economic and racial diversity (Table 1). Additionally, by relying on a community sample with minimal eligibility criteria, our findings may not generalize to women who are currently or at elevated risk for experiencing postpartum mood or anxiety disorders. As such, further research is required to extend these findings to women with current or elevated risks for the development of postpartum depression and anxiety, including history of stressful life experiences, traumatic birth, or prior depressive episodes (O’Hara & McCabe, 2013). Our two-item measures for depression and anxiety symptoms were also brief, which allowed us to ask them repeatedly via EMA over the course of one week, but they did not capture the full spectrum of depression and anxiety symptomatology. Further research is needed to extend these findings to additional aspects of mothers’ mental health as well as confirm that our findings reflect different mechanisms unique to depression and anxiety vs. a general psychopathology factor.
Further research is also needed to determine whether our results would generalize to a sample of infants reported to be excessive criers. We focused on cry duration over other features of crying that could differentially impact mental health, like crying pitch or amplitude (LaGasse et al., 2005) as well as the inconsolability of infant crying (Barr et al., 2014). It is possible that within- and between-person changes in other features of crying could reveal differential effects on mental health, for example, perhaps it is the inability to soothe an infant that relates more to maternal anxiety compared to crying duration.
Our study was also underpowered to detect small-sized effects (0.20), particularly for depression and anxiety measured once per day relative to negative affect measured six times per day. A series of 1,000 Monte Carlo simulations revealed we were powered to detect a small-sized effect of within-person variability in crying on negative affect at 62% for 10 minutes, 53% for 1 hour, and 100% for 8 hours. We were powered to detect a small-sized effect of within-person variability in crying on symptoms of depression at 26% for 10 minutes, 21% for 1 hour, and 82% for 8 hours; for anxiety symptoms, power calculations were 26% for 10 minutes, 18% for 1 hour, and 77% for 8 hours. This means that there could still be a true effect of crying exposure on feelings of depression and anxiety – particularly at the 10 minute and 1 hour timescales – that this study could not detect, so our null results should be interpreted with caution.
Finally, our study focused on linear, group-wide, unidirectional analyses. However, bidirectional, person-specific, and non-linear effects also likely play a role in the maintenance and exacerbation of mothers’ mental health and well-being (Papoušek & von Hofacker, 1995; Sadeh et al., 2010). Future studies should use person-specific and cross-lagged effects models to characterize more individualized, bidirectional dynamics between daily experience and maternal mental health.
Implications and future work
This study suggests that infant crying is variable between and within infants, and this within-person variability in crying produces real-time effects on mother’s emotions in a community sample that was not selected on the basis of clinical levels of depression or anxiety. While the beneficial effects of social support on mental health in postpartum women is well-documented (e.g., Beck, 2001), our study suggests that mothers in general – that is, the broad community of mothers, irrespective of their mental health history – could benefit from support in caring for their crying infant and/or developing helpful skills to cope with the demands of caregiving. Having someone to provide emotional support or instrumental support, like actively responding to a distressed infant, could reduce the risk of worse affect following cry exposure. In extreme cases, excessive infant crying can lead to shaking and abusive head trauma, or Shaken Baby Syndrome (SBS), which is most likely to occur between four and six weeks as infant crying peaks (Barr et al., 2006). Teaching mothers how to regulate their emotions and modify their expectations and beliefs around crying, e.g., viewing crying as a normal part of infant behavior, have been shown to prevent SBS (Stewart et al., 2011), and may provide mothers with in-the-moment tools to cope with stressful demands. Our findings of within-person effects of crying on maternal mental health suggest that such coping tools may be universally helpful rather than only for high-risk families. Future work may investigate possible moderators of the effect of crying on mental health, like perceived social support, parenting self-efficacy, and parenting stress, as well as the specific strategies by which mothers effectively regulate their emotions in the presence of infant crying.
Conclusion
Overall, exposure to infant crying is not a static feature of mothers’ experience but, rather, variable day-by-day and even minute-by-minute. We found that within-person increases in infant crying exposure (across minutes as well as hours) increased mothers’ reported negative affect and symptoms of depression. Insofar as ambulatory sensing methods can provide more systematic access to time-varying markers of experience, they open new possibilities to reveal the real-time processes linking the structure of an individual’s ecological context with their mental health. Additionally, our within-person findings provide evidence that interventions to modify risk factors such as infant crying and reactions to infant cries are likely to provide direct benefits to individual mothers.
Supplementary Material
Public significance statement.
This study used cellphone surveys and infant-worn audio recorders to reveal that exposure to infant crying increases maternal negative affect and symptoms of depression, but not symptoms of anxiety, in real-world settings. In contrast to findings from laboratory experiments, we found that the effects of crying on maternal depression symptoms take hours (rather than minutes) to emerge. Studying mother-infant interactions in everyday home settings is necessary to understand and support maternal mental health.
Funding
This work was supported by the National Institute of Mental Health K01 Award (1K01MH111957- 01A1) to K. de Barbaro and a National Science Foundation Graduate Research Fellowship (DGE-1610403) to M. Micheletti.
Footnotes
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
Approval was obtained from the ethics committee of The University of Texas at Austin. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to participate
Written informed consent was obtained from all legal guardians.
Copyright via Canva.com (see References for citations).
Data and/or code Availability
We did not preregister our study. Data and code are not available on a public repository.
References
- Atella LD, DiPietro JA, Smith BA, & St James-Roberts I (2003). More than meets the eye: Parental and infant contributors to maternal and paternal reports of early infant difficultness. Parenting, 3(4), 265–284. 10.1207/s15327922par0304_1 [DOI] [Google Scholar]
- Barr RG, Fairbrother N, Pauwels J, Green J, Chen M, & Brant R (2014). Maternal frustration, emotional and behavioural responses to prolonged infant crying. Infant Behavior and Development, 37(4), 652–664. 10.1016/j.infbeh.2014.08.012 [DOI] [PubMed] [Google Scholar]
- Barr RG, Trent RB, & Cross J (2006). Age-related incidence curve of hospitalized Shaken Baby Syndrome cases: Convergent evidence for crying as a trigger to shaking. Child Abuse & Neglect, 30(1), 7–16. 10.1016/j.chiabu.2005.06.009 [DOI] [PubMed] [Google Scholar]
- Berry D, & Willoughby MT (2017). On the practical interpretability of cross-lagged panel models: Rethinking a developmental workhorse. Child Development, 88(4), 1186–1206. 10.1111/cdev.12660 [DOI] [PubMed] [Google Scholar]
- Bliese P (2000). Within-group agreement, non-independence, and reliability. In Klein KJ & Kozlowski SW (Eds.), Multilevel Theory, Research, and Methods in Organizations. Foundations, Extensions, and New Directions (pp. 249–381). San Francisco Jossey-Bass. https://www.kellogg.northwestern.edu/rc/workshops/mlm/Bliese_2000.pdf [Google Scholar]
- Bowen A, Bowen R, Balbuena L, & Muhajarine N (2012). Are pregnant and postpartum women moodier? Understanding perinatal mood instability. Journal of Obstetrics and Gynaecology Canada, 34(11), 1038–1042. 10.1016/S1701-2163(16)35433-0 [DOI] [PubMed] [Google Scholar]
- Britton JR (2008). Maternal anxiety: Course and antecedents during the early postpartum period. Depression and Anxiety, 25(9), 793–800. 10.1002/da.20325 [DOI] [PubMed] [Google Scholar]
- Britton JR (2011). Infant temperament and maternal anxiety and depressed mood in the early postpartum period. Women & Health, 51(1), 55–71. 10.1080/03630242.2011.540741 [DOI] [PubMed] [Google Scholar]
- Bruning S, & McMahon C (2009). The impact of infant crying on young women: A randomized controlled study. Journal of Reproductive and Infant Psychology, 27(2), 206–220. 10.1080/02646830802350856 [DOI] [Google Scholar]
- Buhler-Wassmann AC, & Hibel LC (2021). Studying caregiver-infant co-regulation in dynamic, diverse cultural contexts: A call to action. Infant Behavior and Development, 64, 101586. 10.1016/j.infbeh.2021.101586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabana MD, Wright P, Scozzafava I, Olarte A, DiSabella M, Liu X, & Gelfand AA (2021). Newborn daily crying time duration. Journal of Pediatric Nursing, 56, 35–37. 10.1016/j.pedn.2020.10.003 [DOI] [PubMed] [Google Scholar]
- Canivet CA, Ostergren P-O, Rosén A-S, Jakobsson IL, & Hagander BM (2005). Infantile colic and the role of trait anxiety during pregnancy in relation to psychosocial and socioeconomic factors. Scandinavian Journal of Public Health, 33(1), 26–34. 10.1080/14034940410028316 [DOI] [PubMed] [Google Scholar]
- Cristia A, Lavechin M, Scaff C, Soderstrom M, Rowland C, Räsänen O, Bunce J, & Bergelson E (2020). A thorough evaluation of the Language Environment Analysis (LENA) system. Behavior Research Methods. 10.3758/s13428-020-01393-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ, & Bauer DJ (2011). The disaggregation of within-person and between-person effects in longitudinal models of change. Annual Review of Psychology, 62(1), 583–619. 10.l146/annurev.psych.093008.100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Barbaro K (2019). Automated sensing of daily activity: A new lens into development. Developmental Psychobiology, 61(3), 444–464. 10.1002/dev.21831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drummond JE, McBride ML, & Wiebe CF (1993). The development of mothers’ understanding of infant crying. Clinical Nursing Research, 2(4), 396–410. 10.1177/105477389300200403 [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, & Trull TJ (2009). Ecological momentary assessment of mood disorders and mood dysregulation. Psychological Assessment, 21(4), 463–475. 10.1037/a0017075 [DOI] [PubMed] [Google Scholar]
- Fang Y, Luo J, Boele M, Windhorst D, van Grieken A, & Raat H (2022). Parent, child, and situational factors associated with parenting stress: A systematic review. European Child & Adolescent Psychiatry, 10.1007/s00787-022-02027-l [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields-Olivieri MA, & Cole PM (2019). Sequences of toddler negative emotion and parent–toddler verbal communication during a waking day. Infancy, 24(6), 857–880. 10.Ill1/infa.12310 [DOI] [PubMed] [Google Scholar]
- Fujiwara T, Barr RG, Brant R, & Barr M (2011). Infant distress at five weeks of age and caregiver frustration. The Journal of Pediatrics, 159(3), 425–430.e2. 10.1016/j.jpeds.2011.02.010 [DOI] [PubMed] [Google Scholar]
- Gan L (n.d.). Baby icon [Graphic], Retrieved from Canva.com.
- Green P, & MacLeod CJ (2016). SIMR: An R package for power analysis of generalized linear mixed models by simulation. Methods in Ecology and Evolution, 7(4), 493–498. 10.1111/2041-210X.12504 [DOI] [Google Scholar]
- Hamaker EL, & Wichers M (2017). No time like the present: Discovering the hidden dynamics in intensive longitudinal data. Current Directions in Psychological Science, 26(1), 10–15. 10.1177/0963721416666518 [DOI] [Google Scholar]
- Hoffman L, & Stawski RS (2009). Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Research in Human Development, 6(2–3), 97–120. 10.1080/15427600902911189 [DOI] [Google Scholar]
- Hofmann W, & Patel PV (2014). SurveySignal: A convenient solution for experience sampling research using participants’ own smartphones. Social Science Computer Review. 10.1177/0894439314525117 [DOI] [Google Scholar]
- Hubbard FO, & van IJzendoorn MH (1991). Maternal unresponsiveness and infant crying across the first 9 months: A naturalistic longitudinal study. Infant Behavior and Development, 14(3), 299–312. [Google Scholar]
- Irwin JR (2003). Parent and nonparent perception of the multimodal infant cry. Infancy, 4(4), 503–516. 10.1207/S15327078IN0404_06 [DOI] [Google Scholar]
- Kim P, Tribble R, Olsavsky AK, Dufford AJ, Erhart A, Hansen M, Grande L, & Gonzalez DM (2020). Associations between stress exposure and new mothers’ brain responses to infant cry sounds. NeuroImage, 223, 117360. 10.1016/j.neuroimage.2020.117360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurth E, Kennedy HP, Spichiger E, Hosli I, & Zemp Stutz E (2011). Crying babies, tired mothers: What do we know? A systematic review. Midwifery, 27(2), 187–194. 10.1016/j.midw.2009.05.012 [DOI] [PubMed] [Google Scholar]
- LaGasse LL, Neal AR, & Lester BM (2005). Assessment of infant cry: Acoustic cry analysis and parental perception. Mental Retardation and Developmental Disabilities Research Reviews, 11(1), 83–93. 10.1002/mrdd.20050 [DOI] [PubMed] [Google Scholar]
- Lucassen PL, Assendelft WJ, van Eijk JT, Gubbels JW, Douwes AC, & van Geldrop WJ (2001). Systematic review of the occurrence of infantile colic in the community. Archives of Disease in Childhood, 84(5), 398–403. 10.1136/adc.84.5.398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcewen BS (2004). Protection and Damage from Acute and Chronic Stress: Allostasis and Allostatic Overload and Relevance to the Pathophysiology of Psychiatric Disorders. Annals of the New York Academy of Sciences, 1032(1), 1–7. 10.1196/annals.1314.001 [DOI] [PubMed] [Google Scholar]
- McHugh ML (2012). Interrater reliability: The kappa statistic. Biochemia Medica, 22(3), 276–282. [PMC free article] [PubMed] [Google Scholar]
- Mendez DD, Sanders SA, Karimi HA, Gharani P, Rathbun SL, Gary-Webb TL, Wallace ML, Gianakas JJ, Burke LE, & Davis EM (2019). Understanding pregnancy and postpartum health using ecological momentary assessment and mobile technology: Protocol for the Postpartum Mothers Mobile Study. JMIR Research Protocols, 8(6), e13569. 10.2196/13569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micheletti M, Yao X, Johnson M, & de Barbaro K (2022). Validating a model to detect infant crying from naturalistic audio. Behavior Research Methods. 10.3758/s13428-022-01961-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AR, Barr RG, & Eaton WO (1993). Crying and motor behavior of six-week-old infants and postpartum maternal mood. Pediatrics, 92(4), 551–558. [PubMed] [Google Scholar]
- Mohr DC, Zhang M, & Schueller SM (2017). Personal sensing: Understanding mental health using ubiquitous sensors and machine learning. Annual Review of Clinical Psychology, 13(1), 23–47. 10.n46/annurev-clinpsy-032816-044949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Hara MW, & McCabe JE (2013). Postpartum depression: Current status and future directions. Annual Review of Clinical Psychology, 9(1), 379–407. 10.1146/annurev-clinpsy-050212-185612 [DOI] [PubMed] [Google Scholar]
- Papoušek M, & von Hofacker N (1995). Persistent crying and parenting: Search for a butterfly in a dynamic system. Early Development and Parenting, 4(4), 209–224. 10.1002/edp.2430040406 [DOI] [Google Scholar]
- Pixabay, 420494. (n.d.). Microphone Flat Icon [Graphic]. Retrieved from Canva.com.
- Pixabay, Clker-free-vector-images. (n.d.). Black T-Shirt Flat Icon [Graphic]. Retrieved from Canva.com.
- Pixabay, MTZD. (n.d.). Mobile Phone Icon [Graphic]. Retrieved from Canva.com.
- Pixeden. (n.d.). Female Icon [Graphic]. Retrieved from Canva.com.
- Peeters F, Nicolson NA, Berkhof J, Delespaul P, & deVries M (2003). Effects of daily events on mood states in major depressive disorder. Journal of Abnormal Psychology, 112(2), 203–211. 10.1037/0021-843x.112.2.203 [DOI] [PubMed] [Google Scholar]
- Peterson RA, & Cavanaugh JE (2020). Ordered quantile normalization: A semiparametric transformation built for the cross-validation era. Journal of Applied Statistics, 47(13–15), 2312–2327. 10.1080/02664763.2019.1630372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petzoldt J (2018). Systematic review on maternal depression versus anxiety in relation to excessive infant crying: It is all about the timing. Archives of Women’s Mental Health, 21(1), 15–30. 10.1007/s00737-017-0771-4 [DOI] [PubMed] [Google Scholar]
- Petzoldt J, Wittchen H-U, Einsle F, & Martini J (2016). Maternal anxiety versus depressive disorders: Specific relations to infants’ crying, feeding and sleeping problems. Child: Care, Health and Development, 42(2), 231–245. 10.1111/cch.12292 [DOI] [PubMed] [Google Scholar]
- Petzoldt J, Wittchen H-U, Wittich J, Einsle F, Hofler M, & Martini J (2014). Maternal anxiety disorders predict excessive infant crying: A prospective longitudinal study. Archives of Disease in Childhood, 99(9), 800–806. 10.1136/archdischild-2013-305562 [DOI] [PubMed] [Google Scholar]
- Sadeh A, Tikotzky L, & Scher A (2010). Parenting and infant sleep. Sleep Medicine Reviews, 14(2), 89–96. 10.1016/j.smrv.2009.05.003 [DOI] [PubMed] [Google Scholar]
- Shackman AJ, Tromp DPM, Stockbridge MD, Kaplan CM, Tillman RM, & Fox AS (2016). Dispositional negativity: An integrative psychological and neurobiological perspective. Psychological Bulletin, 142(12), 1275–1314. 10.1037/bul0000073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological momentary assessment. Annual Review of Clinical Psychology, 4, 1–32. 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- Snijders TAB, & Berkhof J (2008). Diagnostic checks for multilevel models. In de Leeuw J & Meijer E (Eds.), Handbook of Multilevel Analysis (pp. 141–175). Springer; New York. 10.1007/978-0-387-73186-5_3 [DOI] [Google Scholar]
- St James-Roberts I, & Plewis I (1996). Individual differences, daily fluctuations, and developmental changes in amounts of infant waking, fussing, crying, feeding, and sleeping. Child Development, 67(5), 2527–2540. JSTOR. 10.2307/1131638 [DOI] [PubMed] [Google Scholar]
- Stewart TC, Polgar D, Gilliland J, Tanner DA, Girotti MJ, Parry N, & Fraser DD (2011). Shaken Baby Syndrome and a triple-dose strategy for its prevention. Journal of Trauma: Injury, Infection & Critical Care, 71(6), 1801–1807. 10.1097/TA.0b013e31823c484a [DOI] [PubMed] [Google Scholar]
- Targum SD, Sauder C, Evans M, Saber JN, & Harvey PD (2021). Ecological momentary assessment as a measurement tool in depression trials. Journal of Psychiatric Research, 136, 256–264. 10.1016/jjpsychires.2021.02.012 [DOI] [PubMed] [Google Scholar]
- Trull TJ, & Ebner-Priemer U (2013). Ambulatory assessment. Annual Review of Clinical Psychology, 9, 151–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermillet A-Q, Tolboll K, Litsis Mizan S, C. Skewes J, & Parsons CE (2022). Crying in the first 12 months of life: A systematic review and meta-analysis of cross-country parent-reported data and modeling of the “cry curve.” Child Development, 93(4), 1201–1222. 10.1111/cdev.13760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063. [DOI] [PubMed] [Google Scholar]
- Wessel MA, Cobb JC, Jackson EB, Harris GS, & Detwiler AC (1954). Paroxysmal fussing in infancy, sometimes called “colic.” Pediatrics, 14(5), 421–435. [PubMed] [Google Scholar]
- Wesselhoeft R, Madsen FK, Lichtenstein MB, Sibbersen C, Manongi R, Mushi DL, Nguyen HTT, Van TN, Kyhl H, Bilenberg N, Meyrowitsch DW, Gammeltoft TM, & Rasch V (2020). Postnatal depressive symptoms display marked similarities across continents. Journal of Affective Disorders, 261, 58–66. 10.1016/jjad.2019.09.075 [DOI] [PubMed] [Google Scholar]
- Wolke D, Bilgin A, & Samara M (2017). Systematic review and meta-analysis: Fussing and crying durations and prevalence of colic in infants. The Journal of Pediatrics, 185, 55–61.e4. 10.1016/jjpeds.2017.02.020 [DOI] [PubMed] [Google Scholar]
- Xu D, Yapanel U, & Gray S (2009). Reliability of the LENATM Language Environment Analysis System in young children’s natural home environment. LENA Foundation Technical Report LTR-05-02). Retrieved from http://www.lenafoundation.org/TechReport.aspx/Reliability/LTR-05-2.
- Young KS, Parsons CE, Stein A, & Kringelbach ML (2012). Interpreting infant vocal distress. Emotion, 12(6), 1200–1205. 10.1037/a0028705 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
We did not preregister our study. Data and code are not available on a public repository.


