Abstract
The phytochemical study of the ethanolic extract of the leaf of Xeroderris stuhlmannii led to the isolation of five hitherto unreported compounds including two isoflavones (1–2), and three rotenoids (3–5), along with eight known isoflavonoid derivatives (6–13) and one pterocarpan derivative (14). The structures of the new compounds and those of the known ones were established by the spectroscopic (1D and 2D NMR) and spectrometric (HRESIMS) techniques as well as a comparison of their spectroscopic data with those reported in the literature. The leaf extract, fractions, and isolated compounds were tested for their antibacterial effects against nine bacterial strains. Compounds 3, 8, 11, and 12 showed a significant antibacterial effect, with a minimum inhibitory concentration (MIC) value of 62.5 µg/mL each, against Salmonella typhi, Staphylococcus aureus, Klessiella pneumonae, and Escherichia coli, respectively. In addition, the leaf extract, fractions, and isolated compounds were tested for their antifungal effects against four fungal strains. The hexane fraction showed a significant antifungal effect with an MIC value of 125 µg/mL against Candida parasilosis, whereas compounds 3, 8, and 12 showed significant antifungal activity with an MIC value of 62.5 µg/mL, each against Candida parasilosis, Candida albicans, and Candida krusei, respectively.
Keywords: Xeroderris stuhlmannii, Fabaceae, rotenoids, isoflavones, antibacterial, antifungal activities
1. Introduction
Xeroderris genus belongs to the Fabaceae family, commonly known as Leguminoseae, and is an extremely rich source of biologically active compounds mainly flavonoid derivatives, which is the major class of secondary metabolites found in the family [1,2]. These bioactive phytochemicals possess antibacterial, antioxidant, antifungal, and antimalarial activities [3,4,5]. Despite the existing various solutions for health care, drug resistance is common. Thus, the research of new compounds to tackle biological resistance is urgent [6]. Based on the various diversity of secondary metabolites from the Fabaceae family [3] and the ethnopharmacological report on Xeroderris stuhlmannii (Taub) Mendonça and Souza, we examined the leaves of X. stuhlmannii, one of the two species of Xeroderris genus [7]. X. stuhlmannii grows in the West Region of Cameroon and is also called “wing pod” or “wing bean” in English and “mumundu” in the South–West region of Cameroon [8,9]. X. stuhlmannii is a tree, growing up to 18–27 m tall and 120 cm in diameter. Its leaves are alternate at the tips of the branches and are 6–12 mm long, while fruits come in the form of a linear-oblong, globous, and contain one or two bean-shaped seeds [10]. The leaves of X. stuhlmannii are used in traditional folk medicine to treat colds and stomach pains, while the boiled roots are used to fight against malaria [4,9]. LC-MS analysis of the bark extract of X. stuhlmannii proposed various classes of secondary metabolites such as rotenoids, flavonoids, polyphenols, tri-terpenoids, steroids, and other phytochemicals. Moreover, bark extract indicated antibacterial activity on Salmonella appendicitis, Coliform, Staphylococcus aureus, Pseudomonas aeruginosa, and Escherishia coli [5]. We report, herein, the isolation and structure determination of isoflavones and rotenoids derivatives from the ethanolic leaf extract of X. stuhlmannii. In addition, antibacterial, antifungal, and antioxidant activities of leaf extract, fractions, and some isolated compounds were also evaluated.
2. Results and Discussion
2.1. Structural Elucidation of the Isolated Compounds
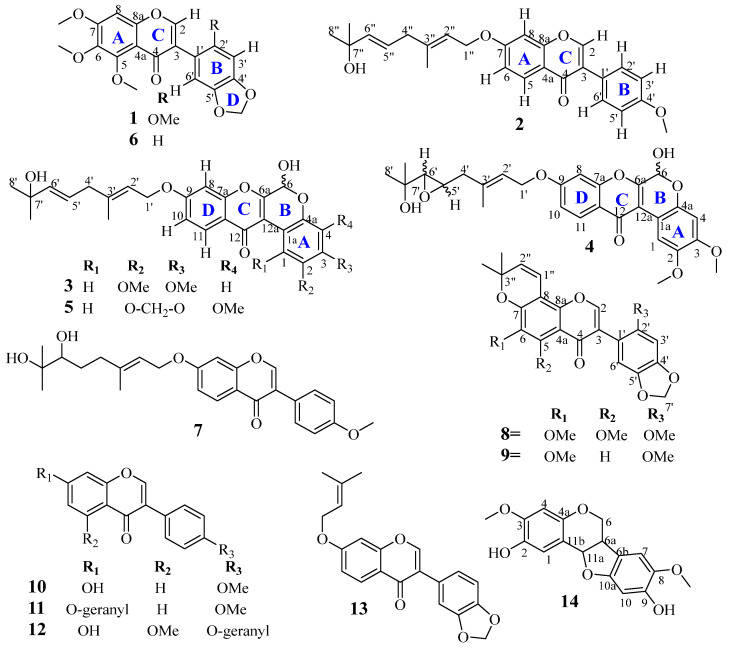
The ethanolic extract of the leaf of X. stuhlmannii was fractionated and purified by successive chromatographic techniques to afford two new isoflavones (1–2), three new rotenoids (3–5) (Figure 1), together with nine known compounds (6–14). All the compounds were characterized and identified by the spectroscopic (1D and 2D NMR) and spectrometric (HRESIMS) techniques, as well as a comparison of their spectroscopic and physical data with that published in the literature. The known isolated compounds were identified as odoratin (6) [1], griffonianone D (7) [11], conrauinone A (8) [12], ichthynone (9) [13,14], formononetin (10) [15], 7-O-geranylformononetin (11) [16], conrauinone C (12) [17], maximaisoflavone B (13) [18], and abrusprecatin A (14) [19].
Figure 1.
Structures of isolated compounds (1–14).
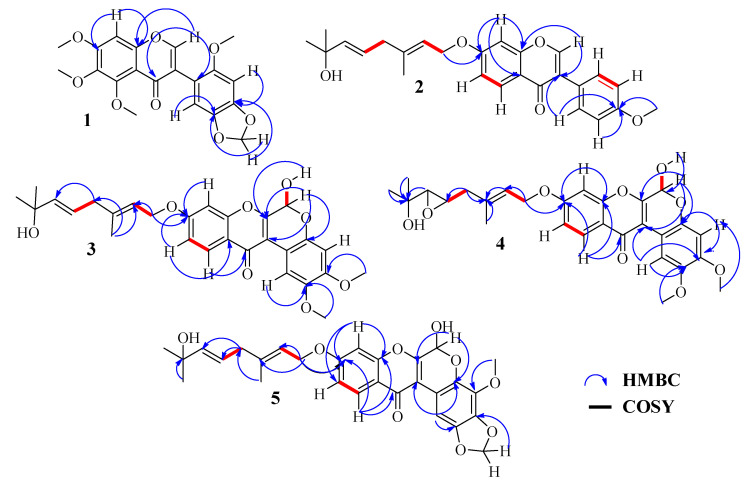
Compound 1 was obtained as a white powder, and gave a positive test with Shinoda reagent. Its molecular formula C20H18O8 was established from the (+)-HRESIMS which showed the pseudomolecular ion peak [M+H]+ at m/z 387.1082 (calcd. for C20H19O8 387.1080), indicating 12 double bond equivalents. Its 1H NMR spectrum (Table 1) exhibited proton signals of flavonoids, and the signal depicted at ẟH 7.80 (1H, s, H-2), characteristic of the proton H-2 of the isoflavonoid skeleton [20]. This spectrum further displayed a singlet for an aromatic proton at ẟH 6.72 (1H, s, H-8), together with a singlet of a methylene dioxyl group at ẟH 5.97 (2H, s, O-CH2-O) and three sharps singlets at ẟH 3.98 (3H, s), 3.97 (3H, s), 3.75 (3H, s), a set of signals characteristic of an odoratin derivative [1]. In addition, the 1H NMR spectrum displayed one more singlet for the methoxyl group at ẟH 3.93 (3H, s) and two more aromatic proton singlets at ẟH 6.63 (1H, s) and 6.85 (1H, s), assignable to two para-coupled protons of the B-ring. The broadband decoupled 13C NMR spectrum combined with the DEPT 135 spectrum displayed 20 carbon signals including the characteristic signals of an isoflavone skeleton at ẟC 175.0 (C-4) and 152.5 (C-2). The other carbon signals were grouped as six aromatic carbons, seven oxygenated aromatic carbons, four methoxyl carbons, and one methylene dioxyl carbon. In the 13C NMR spectrum, the occurrence of all quaternary oxygenated sp2 carbons in the range of 140–150 ppm suggested the presence of oxygen on adjacent carbons (namely, C-4′and C-5′, C-6, and C-7) [21]. The assignation of the singlet resonance at ẟH 6.72 to the aromatic proton H-8 was supported by the HMBC correlations between H-2 (ẟH 7.80), H-8 (ẟH 6.72), and carbon C-8a at ẟC 154.6. Whereas that at ẟH 6.85 was assigned to H-6′ on the basis of the strong HBMC correlation between H-6′, H-2 and carbon C-3 at ẟC 122.5. Therefore, the para coupling between H-6′ at ẟH 6.85 (1H, s) and H-3′ at ẟH 6.63 (1H, s) inferred the positions of the methylene dioxyl to be C-4′ and C-5′ and that of the fourth methoxyl group C-2′. The HMBC spectrum (Figure S5) further supported these positions by the neighboring correlations (Figure 2) among H-3′ and H-6′ with carbons C-3 (ẟC 122.5), C-5′ (ẟc 141.1), C-4′ (ẟc 148.4), and then the correlation between 2′-OMe with C-2′ (ẟC 140.5). Consequently, the structure of 1 was elucidated as 5,6,7-trimethoxy-3-(6-methoxybenzo[d][1,3]dioxol-5-yl)-4H-chromen-4-one, which we trivially named Stuhlmannione A.
Table 1.
1H-(500 MHz) and 13C (125 MHz) NMR spectroscopic data of 1 and 2 recorded in CDCl3 (ẟ in ppm).
| Compound 1 | Compound 2 | |||||
|---|---|---|---|---|---|---|
| Position | ẟ C | ẟ H | HMBC | ẟ C | ẟ H | HMBC |
| 2 | 152.5 | 7.80 | 3, 4, 8a, 1′ | 152.0 | 7.94 | 3, 4, 8a, 1′ |
| 3 | 122.5 | - | 124.3 | - | ||
| 4 | 175.0 | - | 175.9 | - | ||
| 4a | 113.7 | - | 118.4 | - | ||
| 5 | 153.0 | - | 127.8 | 8.22 | 4, 7, 8, 8a | |
| 6 | 152.9 | - | 115.0 | 7.01 | 8, 4a | |
| 7 | 157.6 | - | 163.2 | - | ||
| 8 | 96.1 | 6.72 | 4, 6, 7 | 100.9 | 6.88 | 7, 4a, 8a |
| 8a | 154.6 | - | 157.9 | - | ||
| 1′ | 112.8 | - | 124.9 | - | ||
| 2′ | 140.5 | - | 130.2 | 7.52 | 3, 3′, 4′ | |
| 3′ | 95.3 | 6.63 | 2′, 4′, 5′ | 114.0 | 6.99 | 1′, 2′, 4′, 5′ |
| 4′ | 148.4 | - | 159.6 | - | ||
| 4′-OMe | - | - | 55.4 | 3.86 | 4′ | |
| 5′ | 141.1 | - | 114.0 | 6.99 | 1′, 2′, 4′, 5′ | |
| 6′ | 111.4 | 6.85 | 2′, 4′, 5′ | 130.2 | 7.52 | 3, 3′, 4′ |
| O-CH2-O | 101.3 | 5.97 | 4′, 5′ | - | - | |
| 5-OMe | 56.3 | 3.98 | 5 | - | - | |
| 6-OMe | 56.8 | 3.75 | 6 | - | - | |
| 7-OMe | 62.1 | 3.97 | 6, 7 | - | - | |
| 2′-OMe | 61.6 | 3.93 | 2′ | - | - | |
| 1″ | - | - | 65.5 | 4.66 | 7, 2″, 3″ | |
| 2″ | - | - | 119.3 | 5.55 | 3″-Me, 3″, 4″ | |
| 3″ | - | - | 141.1 | - | ||
| 3″-Me | - | - | 16.8 | 1.78 | 2″, 3″, 4″ | |
| 4″ | - | - | 42.2 | 2.82 | 2″, 3″-Me, 6″ | |
| 5″ | - | - | 140.5 | 5.70 | 4″, 6″, 7″ | |
| 6″ | - | - | 123.9 | 5.66 | 4″ | |
| 7″ | - | - | 70.7 | - | ||
| 8″ | - | - | 29.9 | 1.35 | 6″, 7″ | |
Figure 2.
Key HMBC and 1H-1H COSY correlations for compounds 1–5.
Compound 2 was obtained as a white powder and gave a positive test with Shinoda reagent. Its molecular formula C26H28O5 was deduced from the (+)-HRESI-MS, which highlighted a protonated molecular ion peak at m/z 421.2023 [M+H]+ (calcd. for C26H29O5 421.2015). The analysis of the low field region of 1D NMR and HSQC experiment pointed out a signal H-2/C-2 at 7.94 (1H, s)/ẟc 152.0 suggestive of an isoflavone type skeleton [20]. Its 1H NMR spectrum also showed three aromatic protons consistent in an ABX system at ẟH 7.01 (dd, J = 8.9, 2.3 Hz, H-6), 8.22 (d, J = 8.9 Hz, H-5) and 6.88 (d, J = 2.3 Hz, H-8). The ABX system was easily located on the A-ring, due to the deshielded value of H-8 induced by the anisotropic effect of the carbonyl C-4. Moreover, the AA’BB’ spin coupled system appearing at ẟH 7.52 (2H, dd, J = 8.8 Hz, H-2′/6′) and ẟH 6.99 (2H, dd, J = 8.8 Hz, H-3′/5′) indicated a para-substituted B-ring. Furthermore, the 1H NMR spectrum displayed singlet protons at ẟH 3.86 (3H, s) for the O-Me group, while a side-chain moiety was shown by 13C (Table 1) and DEPT data analysis to contain 10 carbons and one hydroxy-group, suggesting the presence of either a geraniol or nerol moiety [22]. Fuendjiep et al. showed that 13C data, particularly the chemical shift of the methyl at the CH3-9″ and that of the methylene C-4″, aid to distinguish a geranyl side chain [12]. The chemical shift at ẟC 16.8 and 42.2 ppm observed for methyl and methylene, respectively, combined with the biogenetic consideration confirmed the presence of a geraniol side chain in compound 2 [12]. The positions of these two units were determined using the HMBC spectrum. In fact, the correlation between the methoxy protons at ẟH 3.86 and the aromatic protons H-2′/6′ with carbon C-4′at ẟc 159.6 allowed us to locate the methoxy group at C-4′, and otherwise, the cross-peaks observed between H-8 (ẟH 8.22), the oxymethylenic protons H-1″ (ẟH 4.66) and carbon C-7 (ẟc 163.2) highlighted that the geranyloxy moiety was located at C-7. On the basis of the above spectroscopic evidence, the structure of 2 was deduced to be 7-(((2E,5E)-7-hydroxy-3,7-dimethylocta-2,5-dien-1-yl)oxy)-3-(4-methoxyphenyl)-4H-chromen-4-one and trivially named Stuhlmannione B.
Compound 3 was isolated as yellow powder. Its molecular formula, C28H30O8, was determined from (+)-HRESIMS ion peak at m/z 477.1931 [M+H-H2O]+ (calcd. for C28H29O7 477.1913). The 1H NMR spectra displayed a singlet for the deshielded aromatic proton at ẟH 8.51 (1H, s, H-1) and a doublet for the hemiketal proton at ẟH 6.20 (1H, d, J = 7.0 Hz), which together with the two methoxy singlet protons at ẟH 3.78 (3H, s) and 3.80 (3H, s) suggested that the structure 3 was similar to that of 6-hydroxy-2,3,9-trimethoxy-[1]-benzopyrano [3,4-b][1]benzopyran-12(6H)-one (rotenoid) [23,24]. The 13C NMR spectrum of 3 (Table 2) supported the presence of the rotenoid skeleton as it exhibited signals at ẟC155.8 (C-6a), 110.1 (C-12a), and 88.7 (C-6). In addition, 1H NMR and 1H-1H COSY spectra of 3 exhibited an ABX system formed by signals at ẟH 7.13 (1H, dd, J = 8.9, 2.4 Hz, H-10), ẟH 7.24 (1H, d, J = 2.4 Hz, H-8) and ẟH 8.07 (1H, d, J = 8.9 Hz, H-11). The ABX system was clearly located on the D-ring, due to the deshielded value of H-11 induced by the anisotropic effect of the carbonyl C-12. Moreover, the 1H NMR spectrum displayed one more singlet for aromatic proton at ẟH 6.73 (1H, s), which according to the multiplicity was unequivocally located in a para position of H-1. Furthermore, a geraniol side chain attached was evident in compound 3 from the 1H and 13C NMR signals at δ 1.17 (6H, s), 1.73 (1H, dd, J = 1.3 Hz), 4.73 (2H, m, J = 6.5 Hz), 2.74 (2H, d, J = 6.7Hz), 5.50 (t), 5.53 (m), and 5.61 (dt), and a hydroxyl signal at δ 4.49 (Table 2) and also from the HRESIMS in which a fragment ion at m/z 153 was observed. The geraniol was evidenced at C-9 by the HMBC correlations depicted between H-11 (ẟH 8.07), oxymethylene H-1′ (ẟH 4,73), and carbon C-9 (ẟc 163.6), whereas the positions of the two methoxys were deduced from the para coupled protons H-1 and H-4, further supported by the HMBC correlations between -OCH3-2 (ẟH 3.78), H-1 (ẟH 8.51), and carbon C-2 (ẟC 143.9), and then between -OCH3-3 (ẟH 3.80), H-4 (ẟH 6.73), and C-3 (ẟC 149.8). Compound 3 exhibited [α]D = 0, thus, we propose it is racemic at the single chiral center, C-6. On the basis of the above spectroscopic studies, compound 3 was established as 6-hydroxy-9-(((2E,5E)-7-hydroxy-3,7-dimethylocta-2,5-dien-1-yl) oxy)-2,3-dimethoxy-[1]-benzopyrano [3,4-b[1] benzopyran-12(6H)-one, trivially named Stuhlmarotenoid A.
Table 2.
1H-(500 MHz) and 13C (125 MHz) NMR spectroscopic data of 3 and 4 recorded in DMSO-d6 and 5 recorded in CDCl3 (ẟ in ppm).
| Compound 3 | Compound 4 | Compound 5 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Position | ẟ C | ẟ H | HMBC | ẟ C | ẟ H | HMBC | ẟ C | ẟ H | HMBC |
| 1a | 108.8 | - | 108.8 | - | 127.1 | - | |||
| 1 | 110.3 | 8.51 | 2, 3, 12a | 110.3 | 8.51 | 2, 3, 12a | 105.4 | 8.33 | 1a, 2, 4a, 12a |
| 2 | 143.9 | - | 143.9 | - | 140.5 | - | |||
| 2-OMe | 56.5 | 3.78 | 2 | 56.1 | 3.79 | 2 | - | - | |
| 3 | 149.8 | - | 149.7 | - | 136.4 | - | |||
| 3-OMe | 56.1 | 3.80 | 3 | 56.5 | 3.80 | 3 | - | - | |
| 4 | 102.2 | 6.73 | 1a, 2, 3 | 102.2 | 6.74 | 1a, 2, 3 | 139.4 | - | |
| (2/3)-OCH2 | - | - | - | - | 102.4 | 6.07 | 3 | ||
| 4a | 143.8 | - | 143.8 | - | 127.2 | - | |||
| 4-OMe | - | - | - | - | 56.6 | 3.97 | 4 | ||
| 6 | 88.7 | 6.20 | 4a, 6a, 12a | 88.7 | 6.20 | 4a, 6a, 12a | 89.2 | 6.27 | 4a, 6a |
| 6-OH | - | 7.97 | 6a | - | 7.98 | 6, 6a | - | n. d | |
| 6a | 155.8 | - | 155.9 | - | 154.5 | - | |||
| 7a | 156.8 | - | 156.8 | - | 156.5 | - | |||
| 8 | 101.7 | 7.24 | 7a, 9, 10, 12 | 101.7 | 7.24 | 7a, 9 | 100.8 | 6.89 | 7a, 9, 10 |
| 9 | 163.6 | - | 163.6 | - | 163.5 | - | |||
| 10 | 116.0 | 7.13 | 8, 9, 11a | 116.0 | 7.13 | 9, 11a | 115.7 | 7.02 | 8, 11a |
| 11 | 127.3 | 8.07 | 7a, 9, 12 | 127.4 | 8.07 | 7a, 9, 12 | 127.5 | 8.17 | 7a, 9, 12 |
| 11a | 117.8 | - | 117.8 | - | 118.0 | - | |||
| 12 | 174.8 | - | 174.8 | - | 175.4 | - | |||
| 12a | 110.1 | - | 110.1 | - | 110.7 | - | |||
| 1′ | 66.0 | 4.73 | 9, 2′, 3′ | 65.7 | 4.75 | 9, 2′ | 65.7 | 4.69 | 9, 2′, 3′ |
| 2′ | 119.5 | 5.50 | 1′, 3′-Me, 3′ | 119.4 | 5.51 | 1′, 3′ | 119.3 | 5.54 | 3′-Me, 4′ |
| 3′ | 141.4 | - | 141.4 | - | 141.2 | - | |||
| 3′-Me | 17.0 | 1.73 | 2′, 3′, 4′ | 17.0 | 1.78 | 3′ | 16.8 | 1.80 | 2′, 4′, 5′ |
| 4′ | 41.9 | 2.74 | 3′-Me, 3′, 5′ | 41.6 | 2.74/2.25 | 3′ | 42.1 | 2.83 | 2′, 3′-Me, 5′, 6′ |
| 5′ | 122.6 | 5.53 | 4′, 7′ | 53.8 | 2.96 | 4′ | 140.5 | 5.71 | 4′, 7′, 8′ |
| 6′ | 142.0 | 5.61 | 4′, 5′, 7′, 8′ | 64.8 | 2.67 | 7′ | 123.9 | 5.66 | 4′, 7′ |
| 7′ | 69.3 | - | 67.6 | - | 70.8 | - | |||
| 8′ | 30.5 | 1.17 | 6′, 7′, 8′ | 26.8 | 1.07 | 7′, 8′ | 29.8 | 1.34 | 5′,7′, 8′ |
| 8′-Me | 30.5 | 1.17 | 6′, 7′, 8′ | 30.5 | 1.17 | 8′-Me, 7′ | 29.8 | 1.36 | 5′,7′, 8′ |
| 8′-OH | - | 4.49 | 6′, 7′, 8′ | - | n. d | - | 4.18 | 7′ | |
Compound 4 was obtained as a yellow powder. The (+)-HRESIMS m/z 493.1873 (calcd. for C28H29O8, 493.1863) depicted the molecular formula C28H30O9, whereas the 1H NMR spectrum showed a similar pattern to that of 3 through para coupled aromatic protons H-1 at ẟH 8.51 (1H) and H-4 at ẟH 6.74 (1H), an ABX system caused by protons H-8 at ẟH 7.24 (1H, d, J = 2.4 Hz), H-10 at ẟH 7.13 (1H, dd, J = 8.9, 2.4 Hz) and H-11 at ẟH 8.07 (1H, d, J = 8.9 Hz), a signal for a hemiketal at ẟH 6.20, and the two methoxy groups -OCH3-2 ẟH 3.79 and -OCH3-3 ẟH 3.80. The 13C NMR data supported the similarity as it displayed carbon signals at ẟC155.9 (C-6a), 110.1 (C-12a), and 88.7 (C-6). The side chain geraniol group in 3 differed from that of 4 by the lack of an alkene bond replaced by an epoxide linked to carbons H-5′/C-5′ (ẟH 2.96/ẟC 53.8) and H-6′/C-6′ (ẟH 2.67/ẟC 64.8). The position of the epoxide was supported by the HMBC correlation between H-5′ (ẟH 2.96) and C-3′ (ẟc 141.4), whereas the side chain was clearly located at C-9, by the correlation between H-11 (ẟH 8.07), oxymethylene H-1′ (ẟH 4,75) and carbon C-9 (ẟc 163.6). The relative configuration of the epoxide in the side chain was deduced to be α on the basis of the 1H and 13C chemical shift values of H-5′ and H-6′ compared to those of reported data [25], further supported by the coupling constants between H-5′ and H-6′ (J = 2.2 Hz) and the biogenic consideration. Based on the above spectral evidence, the structure of compound 4 was established as 6-hydroxy-9-(((2E)4-(3-(2-hydroxypropan-2-yl)oxiran-2-yl)-3-methylbut-2-en-1-yl) oxy)-2,3-dimethoxychromeno[3,4-b]chromen-12(6H)-one and trivially named Stuhlmarotenoid B.
Compound 5 was obtained as a brown oil, and its molecular formula was established as C28H28O9 from its (+)-HRESIMS, which showed a pseudo molecular ion peak [M+Na]+ at 531.1630 (calcd. for C28H28O9Na 531.1631). The 1H NMR spectrum displayed a signal for a deshieled aromatic proton at ẟH 8.33 (1H, s, H-1) and a signal for an hemiketal proton at ẟH 6.27, which together with signals of geraniol suggested that the structure of 5 was similar to that of 3. 13C NMR supported the similarity as it displayed carbon signals at ẟC 154.5 (C-6a), 110.7 (C-12a) and 89.2 (C-6). The differences between the 1D NMR data of 5 and 3 were the lack of the aromatic proton signal for H-4 and one methoxy group, in contrast the appearance of a proton signal for the methylene dioxyl -OCH2-(2/3) at ẟH 6.07/ẟC 102.4. The position of the methylene dioxyl were deduced to be C-2 and C-3 by the HMBC correlation between H-1 (ẟH 8.33), -OCH2-(2/3) (ẟH 6.07), and the carbon C-2 (ẟC 140.5) and C-3 (ẟC 136.4), inferring the methoxy group -OCH3-4 (ẟH 3.97/ẟC 56.6) to be C-4. The position of the methoxy group -OCH3-4 was further supported by the HMBC correlation between methoxy group -OCH3-4, H-1 and C-4 (ẟC 139.4). Compound 5 exhibited [α]D = 0, thus, we propose it as racemic at the single chiral center, C-6. The structure of compound 5 was therefore unambiguously established as 6-hydroxy-9-(((2E,5E)-7-hydroxy-3,7-dimethylocta-2,5-dien-1-yl)oxy)-4-methoxychromeno[2,3-c]-[1,3]-dioxolo[4,5-g]-chromen-12(6H)-one and trivially named Stuhlmarotenoid C (5).
2.2. Biological Activities
2.2.1. Antibacterial Evaluation
The antibacterial effects of the EtOH leaf extract, hexane, and AcOEt fractions as well as all the isolated compounds were evaluated against ATCC strains using the microtiter broth dilution method to determine the MIC and MBC (minimal inhibitory and bactericidal concentration) [26]. The results (Table 3) showed that the ethanol leaf extract exhibited moderate activity against Pseudomonas aeruginosa and Salmonella enteritidis with MIC values of 250 µg/mL each and bactericidal effects with MBC/MIC ratios of 2 each. Compound 12 indicated moderate activity against Escherichia coli with an MIC value of 62.5 µg/mL and weak activity against Staphylococcus aureus and Salmonella typhimurium with MIC values of 125 µg/mL each. Compound 12 evoked bactericidal effect ratios (MBC/MIC) of 2, 4, and 2, respectively against S. aureus, E. coli, and S. typhimurium. Compound 3 indicated weak activity against Shigella flexineri and Shigella dysenteria with MIC values of 125 µg/mL, moderate activity against Salmonella typhi with MIC value of 62.5 µg/mL, and bactericidal effect ratios (MBC/MIC) of 2, 2, and 4, respectively. Compound 8 highlighted moderated activity against S. aureus with an MIC value of 62.5 µg/mL, weak activity against S. typhi with an MIC value of 125 µg/mL, and bactericidal effects with MBC/MIC ratios of 4 and 2, respectively. Compound 11 showed moderated activity against S. aureus and Klessiella pneumonae with MIC values of 62.5 µg/mL, weak activity against E. coli with an MIC value of 125 µg/mL and bactericidal effects with MBC/MIC ratios of 4, 2, and 4, respectively. The other compounds were found to be either weakly active or inactive on the tested strains.
Table 3.
Minimal inhibitory and bactericidal concentration (MIC and MBC) of ethanolic leaf extract, hexane fraction, and 11 isolated compounds of X. stuhlmannii.
| Microbial Organisms | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Test Substance | Parameters | PA | SA | EC | KP | SF | SD | Stm | St | Se |
| Leaf extract | MIC | 250 | >500 | >500 | >500 | >500 | >500 | >500 | >500 | 250 |
| MBC | 500 | ND | ND | ND | ND | ND | ND | ND | 500 | |
| MBC/MIC | 2 | ND | ND | ND | ND | ND | ND | ND | 2 | |
| Hexane fraction | MIC | >500 | >500 | >500 | >500 | >500 | 125 | >500 | >500 | >500 |
| MBC | ND | ND | ND | ND | ND | 250 | ND | ND | ND | |
| MBC/MIC | ND | ND | ND | ND | ND | 2 | ND | ND | ND | |
| 12 | MIC | >125 | 125 | 62.5 | >125 | >125 | >125 | 125 | >125 | >125 |
| MBC | ND | 250 | 250 | ND | ND | ND | 250 | ND | ND | |
| MBC/MIC | ND | 2 | 4 | ND | ND | ND | 2 | ND | ND | |
| 3 | MIC | >125 | >125 | >125 | >125 | 125 | 125 | >125 | 62.5 | >125 |
| MBC | ND | ND | ND | ND | 250 | 250 | ND | 250 | ND | |
| MBC/MIC | ND | ND | ND | ND | 2 | 2 | ND | 4 | ND | |
| 10 | MIC | >125 | >125 | >125 | >125 | >125 | >125 | 125 | >125 | >125 |
| MBC | ND | ND | ND | ND | ND | ND | 250 | ND | ND | |
| MBC/MIC | ND | ND | ND | ND | ND | ND | 2 | ND | ND | |
| 6 | MIC | >125 | >125 | >125 | 125 | >125 | >125 | >125 | >125 | >125 |
| MBC | ND | ND | ND | 250 | ND | ND | ND | ND | ND | |
| MBC/MIC | ND | ND | ND | 2 | ND | ND | ND | ND | ND | |
| 8 | MIC | >125 | 62.5 | >125 | >125 | >125 | >125 | >125 | 125 | >125 |
| MBC | ND | 250 | ND | ND | ND | ND | ND | 250 | ND | |
| MBC/MIC | ND | 4 | ND | ND | ND | ND | ND | 2 | ND | |
| 2 | MIC | >125 | >125 | >125 | >125 | >125 | 125 | 125 | 125 | >125 |
| MBC | ND | ND | ND | ND | ND | 250 | 250 | 250 | ND | |
| MBC/MIC | ND | ND | ND | ND | ND | 2 | 2 | 2 | ND | |
| 13 | MIC | >125 | >125 | >125 | 125 | 125 | >125 | >125 | >125 | >125 |
| MBC | ND | ND | ND | 250 | 250 | ND | ND | ND | ND | |
| MBC/MIC | ND | ND | ND | 2 | 2 | ND | ND | ND | ND | |
| 11 | MIC | >125 | 62.5 | 125 | 62.5 | >125 | >125 | >125 | >125 | >125 |
| MBC | ND | 250 | 250 | 250 | ND | ND | ND | ND | ND | |
| MBC/MIC | ND | 4 | 2 | 4 | ND | ND | ND | ND | ND | |
| Amoxicillin | MIC | 0.5 | ||||||||
| MBC | 1 | |||||||||
| MBC/MIC | 2 | |||||||||
| Cipro | MIC | 1 | 0.25 | 0.5 | 0.25 | 0.5 | 0.5 | 0.5 | 0.5 | |
| MBC | 4 | 1 | 2 | 2 | 1 | 2 | 1 | 2 | ||
| MBC/MIC | 4 | 4 | 4 | 0.125 | 2 | 4 | 2 | 4 | ||
Values are expressed (µg/mL) as means ± SEM.; PA: Pseudomonas aeruginosa (ATCC01); SA: Staphylococcus aureus (ATCC25922); ECs: Escherichia coli (ATCC10536); KP: Klessiella pneumonae (ATCC13883); SF: Shigella flexineri; SD: Shigella dysenteria; Stm: Salmonella typhimurium; ST: Salmonella typhi (ATCC6539); SE: Salmonella enteritidis. ND: not determined. MIC = Minimum inhibitory concentration; MBC = Minimum bactericidal concentration; MBC/MIC; The ratio MBC/MIC determine the bactericidal (MBC/MIC ≤ 4) or bacteriostatic (MBC/MIC > 4) effects of extracts. Cipro: Ciprofloxacin, Amox: Amoxicillin.
2.2.2. Antifungal Evaluation
The antifungal activity of the EtOH leaf extract, hexane, and AcOEt fractions as well as all the isolated compounds were evaluated against the four fungal strains Candida albicans, Candida krusei, Candida parasilosis, and Cryptococcus neoformans following a standard protocol. Table 4 shows the antifungal activity of leaf extract, fractions, and some isolated compounds. The leaf extract was found to be inactive against all the tested strains, whereas the hexane fraction evoked moderate activity against C. parasilosis with the MIC value of 250 µg/mL and a fungicidal effect with a ratio MFC/MIC of 2. Compound 12 highlighted moderate activity against C. krusei with an MIC value of 62.5 µg/mL, weak activity against C. parasilosis and C. neoformans with MIC values of 125 µg/mL, and fungicidal effects with MFC/MIC ratios of 4, 2, and 2, respectively. Compound 3 showed moderate activity against C. parasilosis with an MIC value of 62.5 µg/mL, weak activity against C. albicans and C. neoformans with MIC values of 125 µg/mL, and fungicidal effects with MFC/MIC ratios of 2, 4, and 2, respectively. Compound 6 revealed weak activity against C. parasilosis and C. neoformans with MIC values of 125 µg/mL and fungicidal effects with MFC/MIC ratio of 2 each. Compound 8 was evaluated with moderate activity against C. albicans with an MIC value of 62.5 µg/mL, weak activity against C. krusei with an MIC value of 125 µg/mL, and fungicidal effects with MFC/MIC ratios of 4 and 2, respectively. The other compounds were found to be either weakly active or inactive on the tested strains.
Table 4.
Minimal inhibitory and fungicidal concentration (MIC and MFC) of ethanolic leaf extract, hexane fraction, and 11 isolated compounds of X. stuhlmannii.
| Yeasts Strains | |||||
|---|---|---|---|---|---|
| Tested Substances | Parameters | CA | CK | CP | CN |
| Leaf extract | MIC | >500 | >500 | >500 | >500 |
| MFC | ND | ND | ND | ND | |
| MFC/MIC | ND | ND | ND | ND | |
| 12 | MIC | >125 | 62.5 | 125 | 125 |
| MFC | ND | 250 | 250 | 250 | |
| MFC/MIC | ND | 4 | 2 | 2 | |
| 3 | MIC | 125 | >125 | 62.5 | 125 |
| MFC | 250 | ND | 250 | 250 | |
| MFC/MIC | 2 | ND | 4 | 2 | |
| 6 | MIC | >125 | >125 | 125 | 125 |
| MFC | ND | ND | 250 | 250 | |
| MFC/MIC | ND | ND | 2 | 2 | |
| 8 | MIC | 62.5 | 125 | >125 | >125 |
| MFC | 250 | 250 | ND | ND | |
| MFC/MIC | 4 | 2 | ND | ND | |
| 2 | MIC | >125 | 125 | >125 | 125 |
| MFC | ND | 250 | ND | 250 | |
| MFC/MIC | ND | 2 | ND | 2 | |
| Hexane fraction | MIC | >500 | >500 | 125 | >500 |
| MFC | ND | ND | 250 | ND | |
| MFC/MIC | ND | ND | 2 | ND | |
| 13 | MIC | >125 | 125 | >125 | >125 |
| MFC | ND | 250 | ND | ND | |
| MFC/MIC | ND | 2 | ND | ND | |
| 11 | MIC | >125 | 125 | 125 | >125 |
| MFC | ND | 250 | 250 | ND | |
| MFC/MIC | ND | 2 | 2 | ND | |
| Nysta | MIC | 0.5 | 0.25 | 1 | 0.25 |
| MFC | 2 | 1 | 2 | 1 | |
| MFC/MIC | 4 | 0.25 | 2 | 0.25 | |
Values are expressed (in µg/mL) as means ± SEM. Minimum inhibitory concentrations (MIC); Minimum fungicidal concentrations (MFC). CA: Candida albicans, CK: Candida krusei, CP: Candida parasilosis, CN = Cryptococcus neoformans; Nysta: Nystatin.
2.2.3. Antioxidant Evaluation
It has been demonstrated that more than one method is necessary to elucidate the antioxidant capacity of samples because these assays differ in the principles and experimental conditions. In this study, the antioxidant activity of the ethanolic leaf extract, hexane, and AcOEt fractions as well as the isolated compounds were tested using the radical scavenging activities and reducing power as listed in Table 5. The ethanolic leaf extract showed significant scavenging activity against 2,2-azino-bis (3-ethylbenzothiazoline-6-sulfonic acid) (ABTS) with RSa50 of 13.44 ± 0.82 and 2,2-dipheny-1-picrylhydrazyl (DPPH) with RSa50 of 14.97 ± 0.86 µg/mL, while a poor reducing power was observed within the ferric reducing antioxidant power (FRAP) assay. These results suggest that the ethanol leaf extract contains compounds that could act as a free radical scavenger that is, capable of donating hydrogen or electron to a free radical in order to stabilize the odd electron which is responsible for radical’s reactivity [27]. The fractions and isolated compounds were found to be either weakly active or inactive. The absence of activity in the isolated compounds may be due to the lack of proton donors in almost all their structures.
Table 5.
Radical scavenging activity (DPPH and ABTS) and ferric reducing power (FRAP) of ethanolic leaf extract and isolates.
| Tests Materials | DPPH (RSa50 (µg/mL)) | ABTS (RSa50 (µg/mL)) | FRAP (RC50 (µg/mL)) |
|---|---|---|---|
| Leaf extract | 16.36 ± 0.77 b | 13.44 ± 0.82 b | 39.85 ± 0.96 d |
| 12 | 17.93 ± 0.82 b | 35.20 ± 0.88 d | 24.09 ± 0.41 b |
| 6 | 14.97 ± 0.86 b | 22.31 ± 1.20 b | 25.31 ± 0.52 d |
| 5 | 24.29 ± 2.03 c | 17.41 ± 1.00 b | 15.07 ± 0.41 b |
| 7 | 19.10 ± 1.50 c | 14.41 ± 0.24 b | 19.50 ± 4.50 b |
| Vitamin C | 8.92 ± 0.06 a | 2.71 ± 0.08 a | 13.94 ± 0.07 a |
Values are expressed as mean ± SEM. Along each column, values with the same letter superscripts are not significantly different, Bonferroni test (p > 0.05). RSa50 of DPPH and ABTS in µg/mL; RC50 of FRAP in µg/mL.
Although the known compounds displayed either weak or no activity in this work, griffonianone D (7) was reported to possess anti-inflammatory effects in different experimental models of inflammation [11], while ichthynone (9) displayed a weak cytotoxic effect on cancer cells. [28]. Formonotin (10) was reported to exhibit anticancer activity [29], whereas maximaisoflavone B (13) and abrusprecatin (14) exhibit weak antiplasmodial activities [19,30]. To the best of our knowledge, no biological activity is reported for odoratin (6), conrauinone (8), 7-O-geranylformononetin (11), and conrauinone C (12).
3. Materials and Methods
3.1. General Experimental Procedures
HR-ESI were generated on either an Agilent 6220 TOF LCMS mass spectrometer (Agilent Technologies, Santa Clara, CA, USA) with perfluorokerosene as reference substance or Synapt G2-S (Waters, Manchester, UK, Details in the Supplementary Materials) for ESI-HR-MS. The NMR spectra were recorded at 500 MHz for 1H and 125 MHz for 13C, on Bruker DRX 500 or Avance NEO spectrometer with a cryo probe CTCI (1H/13C/15N) (Bruker, Rheinstetten, Germany) in CDCl3, C3D6O, and DMSO-d6. All the chemical shifts are given in ẟ (ppm) with reference tetramethylsilane (TMS) (Sigma-Aldrich, Munich, Germany) to the residual solvent signal, while coupling constants (J) were measured in Hz. Data processing and evaluation were performed using the Topspin Software Version 4.0.7 (Bruker, Rheinstetten, Germany). For the determination of the specific optical rotation, the polarimeter Jasco P-2000 (Jasco, Groß-Umstadt, Germany) digital polarimeter with a 5-cm cuvette was employed. The aperture was set to 1.8 mm. Column chromatography was performed using Sephadex LH-20 gel (Amersham Pharmacia Biotech, Uppsala, Sweden) and silica gel 60 (0.040–0.063 mm, Merck, Darmstadt, Germany). Preparative HPLC was performed on a Jasco System (Jasco, Groß-Umstadt, Germany, see details the Supplementary Materials). Thin layer chromatography (TLC) was carried out on silica gel 60 F254 (Merck, Darmstadt, Germany) plates developed with hexane-EtOAc, EtOAc, and EtOAc-MeOH. While spots were detected by spraying with 10% H2SO4 reagent followed by heating. The molecular composition of the isolated compounds was identified by accurate mass determinations. All reagents used were of analytical grade.
3.2. Plant Material
The leaves of X. stuhlmannii were collected in Tonga, west region of Cameroon, in November 2020. The plant was identified by Tacham Walter of National Herbarium of the Cameroon, where a voucher specimen (No. 6011/SRF/CAM) has been deposited.
3.3. Extraction and Isolation
The air-dried leaves of X. Stuhlmannii (1.5 kg) were powdered prior to being extracted with EtOH (10 L × 3) at room temperature. The filter solution was concentrated in vacuo to afford leaf crude extract (130.0 g). The crude extract was suspended in water and partitioned with n-hexane (Hex), EtOAc, and MeOH (1 L, three times, each) to yield n-hexane (HF, 50.8 g), EtOAc (EF, 30.4g), and MeOH (MF, 15.6 g) fractions, respectively. The EtOAc fraction which contained less chlorophyll was further investigated. An aliquot of 28.0 g of the EtOAc fraction was subjected to silica gel column chromatography (CC) (100 × 5 cm) and eluted with gradients of n-hexane-EtOAc (from 1:9 to 100:00 (v/v)) and EtOAc-MeOH (from 5:95 to 15:85 (v/v)), 1 L each. The resulting subfractions were grouped into four fractions FA1-FA4, on the basis of their TLC profiles. Subfraction FA1 (100.5 mg, Hex–EtOAc (4:1, v/v)), was further chromatographed on silica gel (100 × 2.5 cm) with an isocratic solvent system of Hex–EtOAc (85:15, v/v) to give compounds 6 (10.2 mg), 8 (15.1 mg), and 11 (30.3 mg). Subfraction FA2 (90.5 mg, Hex–EtOAc (7:3, v/v)), was further chromatographed by Sephadex LH-20 cc (100 × 2.5 cm) with 100% MeOH (500 mL) to yield compounds 2 (8.15 mg) and 12 (12.25 mg), also subfractions FA2a (20.15 mg) and FA2b (10.25 mg). Subfraction FA2a was purified by HPLC using a preparative RP-C18 column (CH3CN− H2O, 55:45), to yield compound 1 (15.2 mg), whereas FA2b was purified by preparative silica gel TLC with a solvent system of Hex–EtOAc (3:2, v/v) to give compounds 13 (6.1 mg). Subfraction FA3 (200.5 mg, Hex–EtOAc (3:2, v/v)), was further chromatographed by Sephadex LH-20 column chromatography (100 × 2.5 cm) with 100% MeOH (400 mL) to give subfractions FA3a (25.4 mg), FA3b (20.3 mg), and FA3c (10.5 mg). Subfraction FA3a was purified by HPLC using a preparative RP-C18 column (CH3CN− H2O, 55:45) to yield compounds 7 (8.2 mg) and 10 (8.3 mg). Using the same conditions mentioned above, FA3b was purified by HPLC using a preparative RP-C18 column (CH3CN− H2O, 55:45) to yield compounds 5 (10.6 mg) and 9 (5.2 mg), whereas FA3c was purified by preparative silica gel TLC with a solvent system of Hex–EtOAc (1:1, v/v) to give compound 14 (7.5 mg). FA4 (80.5 mg, Hex–EtOAc (3:7, v/v)), was further chromatographed by Sephadex LH-20 column chromatography (100 × 2.5 cm) with 100% MeOH (400 mL), then preparative silica gel TLC with a solvent system of Hex–EtOAc (3:7, v/v) to give compounds 3 (12.5 mg) and 4 (10.1 mg).
Stuhlmannione A (1). Yellow powder; HRESI-MS m/z 387.1081 [M+H]+ (calcd. for C20H19O8 m/z 387.1080); 1H-NMR (500 MHz, CDCl3) and 13C-NMR (125 MHz, CDCl3): see Table 1.
Stuhlmannione B (2). Yellow powder; HRESI-MS m/z 421.2023 [M+H]+ (calcd. for C26H29O5 m/z 421.2015); 1H-NMR (500 MHz, CDCl3) and 13C-NMR (125 MHz, CDCl3): see Table 1.
Stuhlmarotenoid A (3). Yellow powder; [α]D = 0°; HRESI-MS m/z 477.1931 [M-H2O-H]+ (calcd. For C28H29O7 m/z477.1913); 1H-NMR (500 MHz, DMSO-d6) and 13C-NMR (125 MHz, DMSO-d6): see Table 2.
Stuhlmarotenoid B (4). Yellow powder; HRESI-MS m/z 493.1873 [M-H2O-H]+ (calcd. for C28H29O8 m/z 493.1862); 1H-NMR (500 MHz, DMSO-d6) and 13C-NMR (125 MHz, DMSO-d6): see Table 2.
Stuhlmarotenoid C (5). Brown oil; [α]D = 0°; HRESI-MS m/z 531.1630 [M+Na]+ (calcd. for C28H28O9Na m/z 531.1631); 1H-NMR (500 MHz, CDCl3) and 13C-NMR (125 MHz, CDCl3): see Table 2.
3.4. Biological Activities
3.4.1. Antibacterial Activity
The antibacterial activity was implemented against nine strains (Pseudomonas aeruginosa (ATCC01); Staphylococcus aureus (ATCC25922); Escherishia coli (ATCC10536); Klessiella pneumonae (ATCC13883); Shigella flexineri; Shigella dysenteria; Salmonella typhimurium; Salmonella typhi (ATCC6539), and Salmonella enteritidis). The broth microdilution method was used for susceptibility testing of bacteria species in 96-well microtiter sterile plates as previously described [26,31,32]. Briefly, the crude extracts were dissolved in 5% DMSO solution and diluted with Mueller Hinton broth to obtain a stock concentration of 2000 µg/mL for the extracts, 1000 µg/mL for fractions, and 500 µg/mL for the isolated compounds. This gave a concentration range of 1000–0.96 µg/mL, 500–0.96 µg/mL, and 250–0.96 µg/mL respectively. One hundred microliters of each bacterial suspension (containing about 1.5 × 106 CFU/mL) was added, respectively, to the wells containing the test samples and mixed thoroughly to give final concentrations ranging from 500 to 0.48 µg/mL for extract, 250 to 0.48 µg/mL for fraction, and 125 to 0.48 µg/mL for isolated compounds. Ciprofloxacin® (Bayer, Leverkusen, Germany) at concentration of 125–0.48 µg/mL was used as the standard reference. The assay microtiter plates were incubated at 37 °C for 24 h. Inhibitory concentrations of the extracts were detected after addition of 50 µL to 0.2 mg/mL p-iodonitrotetrazolium chloride (INT) (Sigma–Aldrich, Johannesburg, South Africa) and incubated at 37 °C for 30 min. These preparations were further incubated at 37 °C for 48 hrs, and bacterial growth was revealed by the addition of INT as mentioned above. The smallest concentration at which no color change was observed was considered as the MBC. The tests were performed in duplicates. The ratio MBC/MIC was calculated to determine the bactericidal (MBC/MIC ≤ 4) and bacteriostatic (MBC/MIC > 4) effects.
3.4.2. Antifungal Activity
The inocula of yeasts were prepared from 48 h old cultures by picking numerous colonies and suspending them in sterile saline (NaCl) solution (0.9%). Absorbance was read at 530 nm and adjusted with the saline solution to match that of a 0.5 McFarland standard solution, corresponding to about 106 yeast cells/mL (CLSI, CLSI, formerly national committee for clinical and laboratory standards, NCCLS, 2008). MIC of each extract was determined by using broth microdilution techniques according to the guidelines of CLSIfor yeasts (M27-A2). Stock solutions of the test extracts were prepared in 5% aqueous DMSO solution and diluted with sabouraud dextrose broth (SDB) to give a concentration of 1 mg/mL. This was serially diluted two-fold to obtain a concentration range of 500–0.24 μg/mL for extracts and 125–0.24 µg/mL for compounds. The final concentration of DMSO in the well was less than 1% (preliminary analysis with 1% DMSO did not inhibit the growth of the test organisms). The plates were covered with a sterile lid and incubated on the shaker at 37 °C for 48 h (for yeasts) or at 28 °C for 7 days (for dermatophytes) [33,34,35]. MICs were assessed visually after the corresponding incubation period and were taken as the lowest product concentration at which there was no or virtually no growth. The assay was repeated three times. Nystatin (for yeasts) and griseofulvin (for dermatophytes) were used as positive controls.
3.4.3. Antioxidant Activity
DPPH radical scavenging assay
The free radical scavenging activities of the sample were evaluated using the DPPH analysis as described by Noghogne et al. [36]. The radical scavenging activities of crude extract were evaluated through spectrophotometer using the 1,1-diphenyl-2-picrylhydrazyl (DPPH) free radical. When DPPH reacts with an antioxidant sample, which can donate hydrogen, it is reduced. The changes in color were measured at wave length 517 nm under UV/visible light spectrophotometer (Infinite M200, TECAN, Männedorf, Switzerland). The extract (1000 µg/mL) was two-fold serially diluted with methanol. Fifty microliters of the diluted extract (1000 µg/mL) in methanol were mixed with 150 µL of 0.02% of 2,2-diphenyl-1-picrylhydrazyl (DPPH) methanol solution, giving a final extract concentration range from 250 to 1.9531 µg/mL (250, 125, 62.5, 31.25, 15.625, 7.8125, 3.9062, and 1.9531 µg/mL). After 30 min of incubation in the dark at room temperature, the optical density was measured. Ascorbic acid (Vitamin C) was used as positive control. Each assay was done in triplicate, and the results recorded as the mean ± standard deviation (SD). The radical scavenging activity (RSA, %) was calculated as follows:
| (1) |
ABTS radical scavenging assay
The radical scavenging activities of the samples were evaluated spectrophotometrically using the 2,2′-azino-bis (3-ethylbenzothiazoline-6-sulphonic) acid (ABTS) free radical [37]. When ABTS reacts with an antioxidant compound, which can donate hydrogen, it is reduced. The changes in color were measured at 734 nm under UV/visible light spectrophotometer (Infinite M200 (TECAN, Männedorf, Switzerland). Pure methanol was used to calibrate the counter. The extract (1000 µg/mL) was twofold serially diluted with methanol. Twenty-five microliters of the diluted extract were mixed with seventy-five µL of 2,2′-azino-bis (3-ethylbenzothiazoline-6-sulphonic) acid (ABTS) methanol solution, to give a final extract concentration range of 250–1.9531 µg/mL (250, 125, 62.5, 31.25, 15.625, 7.8125, 3.9062, and 1.9531 µg/mL). After 30 min of incubation in the dark at room temperature, the optical densities were measured at 734 nm. Ascorbic acid (Vitamin C) was used as a control. Each assay was done in triplicate, and the results, recorded as the mean ± standard deviation (SD) of the three findings, were presented in tabular form. The radical scavenging activity (RSA, in %) was calculated as follows:
| (2) |
FRAP assay
The ferric reduction potential (conversion potential of Fe3+ to Fe2+) of the samples was determined according to the method described by Padmaja et al. [38]. Briefly, the samples were first dissolved as for the DPPH assay. 25 µL from each dilution was introduced into a new microplate, and 25 µL of 1.2 mg/mL Fe3+ solution was added. The plates were pre-incubated for 15 min at ambient temperature. After this time, 50 µL of 0.2% ortho-phenanthroline was added to obtain final extract concentrations of 250, 125, 62.5, 31.25, 15.625, 7.8125, 3.90625, and 1.95325 µg/mL. The reaction mixtures were further incubated for 15 min at ambient temperature after which the absorbance was measured at 505 nm under UV/visible light spectrophotometer (Infinite M200 TECAN, Männedorf, Switzerland) against the blank (made of 25 µL methanol + 25 µL Fe3+ + 50 µL ortho-phenanthroline). Ascorbic acid (Vitamin C) was used as a positive control. The assay was performed in triplicate. From the obtained OD (optical density), reducing percentages were calculated for each concentration and used to determine the RC50 from dose–response curves.
4. Conclusions
In summary, we have conducted the successful isolation of 15 compounds, including two new isoflavone derivatives (1–2) and three new rotenoid derivatives (3–5), together with nine known compounds (6–14) from X. stuhlmannii. The biological evaluations revealed that the leaf extract showed a general trend to exhibit weaker antibacterial and antifungal activities than the hexane fraction. From the evident results, compounds 3, 12, and 8 highlighted the greatest antibacterial and antifungal activities. However, no antioxidant activity was observed with the isolated compounds. From these results, further study may be done to confirm the use of the leaves in traditional folk medicine to treat diarrhoea, coccidiosis, endoparasites, fungal infections, and lethargic birds.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/molecules28062846/s1, Figure S1–S63: HRESIMS, 1D, and 2D NMR spectra of 1–5, HRESIMS, and 1D NMR spectra of 6–14, UPLC-ESI-TOF-MS, and preparative HPLC parameters.
Author Contributions
Conceptualization, A.G.B.A. and A.B.D.; methodology, L.B.K.M., W.D.T.T., J.J.W.K., A.K.N., Y.F., L.T.A., T.D.S. and A.G.B.A.; formal analysis, L.B.K.M., W.D.T.T., A.G.B.A., L.T.A. and T.D.S.; data curation, L.B.K.M., W.D.T.T., L.T.A. and T.D.S.; writing-original draft preparation, L.B.K.M., W.D.T.T. and T.D.S.; and funding acquisition, T.D.S. and A.B.D. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The supporting information can be found in the Supplementary Materials.
Conflicts of Interest
The authors declare no conflict of interest.
Sample Availability
Samples of the compounds are not available from the authors.
Funding Statement
This work was supported by the Alexander von Humboldt foundation.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Kumar P.R., Balakrishna C., Murali B., Gudipati R., Hota P.K., Chaudhary A.B., Shree A.J., Yennam S., Behera M. An efficient synthesis of 8-substituted odoratine derivatives by the suzuki coupling reaction. J. Chem. Sci. 2016;128:441–450. doi: 10.1007/s12039-016-1042-z. [DOI] [Google Scholar]
- 2.Rahman A.H.M.M., Parvin M.I.A. Study of medicinal uses on Fabaceae family at Rajshahi, Bangladesh. Res. Plant Sci. 2014;2:6–8. doi: 10.12691/plant-2-1-2. [DOI] [Google Scholar]
- 3.Sharma M., Kumar A. Leguminosae (Fabaceae) in tribal medicines. IC J. J. Pharmacogn. Phytochem. 2013;2:127–134. [Google Scholar]
- 4.Asase A., Oteng-Yeboah A.A., Odamtten G.T., Simmonds M.S.J. Ethnobotanical study of some Ghanaian anti-malarial plants. J. Ethnopharmacol. 2005;99:273–279. doi: 10.1016/j.jep.2005.02.020. [DOI] [PubMed] [Google Scholar]
- 5.Selemani M.A., Kazingizi L.F., Manzombe E., Bishi L.Y., Mureya C., Gwata T.T., Rwere F. Phytochemical characterization and in vitro antibacterial activity of Xeroderris Stuhlmannii (Taub.) Mendonca & E.P. Sousa bark extracts. S. Afr. J. Bot. 2021;142:344–351. doi: 10.1016/j.sajb.2021.07.006. [DOI] [Google Scholar]
- 6.Gosavi P.M., Ngan K.C., Yeo M.J.R., Su C., Li J., Lue N.Z., Hoenig S.M., Liau B.B. Profiling the landscape of drug resistance mutations in neosubstrates to molecular glue degraders. ACS Cent. Sci. 2022;8:417–429. doi: 10.1021/acscentsci.1c01603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peter C., Van Welzen K.C. The 11th Flora of Thailand meeting 1999 Leiden, The Netherlands. Thai Forest Bulletin. 1999;28:1–16. [Google Scholar]
- 8.Nakai K., Yoshimura T. African blackwood (Dalbergia melanoxylon) and other local Tanzanian tree species biological performance against subterranean termites and wood decay fungi. BioResources. 2020;15:2994–3005. doi: 10.15376/biores.15.2.2994-3005. [DOI] [Google Scholar]
- 9.Ngarivhume T., Van’T Klooster C.I.E.A., De Jong J.T.V.M., Van Der Westhuizen J.H. Medicinal plants used by traditional healers for the treatment of malaria in the chipinge district in Zimbabwe. J. Ethnopharmacol. 2015;159:224–237. doi: 10.1016/j.jep.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 10.Maundu P.M., Tengnäs B. Useful Trees and Shrubs for Kenya. World Agroforestry Centre; Nairobi, Kenya: 2005. [Google Scholar]
- 11.Yankep E., Njamen D., Fotsing M.T., Fomum Z.T., Mbanya J.C., Giner R.M., Recio M.C., Máñez S., Ríos J.L. Griffonianone D, an isoflavone with anti-inflammatory activity from the root bark of Millettia Griffoniana. J. Nat. Prod. 2003;66:1288–1290. doi: 10.1021/np0205912. [DOI] [PubMed] [Google Scholar]
- 12.Fuendjiep V., Bernard B., Nkengfack A., Fomum T.Z., Sondengam B. Conrauinones A and B, two new isoflavones from stem bark of Millettia conraui. J. Nat. Prod. 1998;3864:380–383. doi: 10.1021/np970187g. [DOI] [PubMed] [Google Scholar]
- 13.Mai H.D.T., Nguyen T.T.O., Pham V.C., Litaudon M., Guéritte F., Tran D.T., Nguyen V.H. Cytotoxic prenylated isoflavone and bipterocarpan from Millettia Pachyloba. Planta Med. 2010;76:1739–1742. doi: 10.1055/s-0030-1249834. [DOI] [PubMed] [Google Scholar]
- 14.Tahara S., Eriko N., Ingham J.L., Junya M. Isoflavonoids from the root bark of Piscidia erythrina and a note on the structure of piscidone. Z. Naturforsch. 1989;44:905–913. [Google Scholar]
- 15.das Neves M.V.M., da Silva T.M.S., de Oliveira L.E., da Cunha E.V.L., Oliveira E.J. Isoflavone formononetin from red propolis acts as a fungicide against Candida sp. Braz. J. Microbiol. 2016;47:159–166. doi: 10.1016/j.bjm.2015.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Felpin F.X., Lory C., Sow H., Acherar S. Practical and efficient entry to isoflavones by Pd(0)/C-mediated suzuki-miyaura reaction. Total synthesis of geranylated isoflavones. Tetrahedron. 2007;63:3010–3016. doi: 10.1016/j.tet.2007.01.062. [DOI] [Google Scholar]
- 17.Fuendjiep V., Nkengfack A.E., Fomum Z.T., Sondengam B.L., Bodo B. Conrauinones C and D, two isoflavones from stem bark of Millettia conraui. Phytochemistry. 1998;47:113–115. doi: 10.1016/S0031-9422(97)00518-9. [DOI] [PubMed] [Google Scholar]
- 18.Rama M.S., Rao E.V. Maxima isoflavone J: A new O-prenylated isoflavone from Tephrosia maxima. J. Nat. Prod. 1985;48:967–968. doi: 10.1021/np50042a015. [DOI] [Google Scholar]
- 19.Li Y., Wu J.W., Tan H.B., Li B.L., Qiu S.X. Three new pterocarpans from the aerial Parts of Abrus precatorius. Nat. Prod. Res. 2020;34:1836–1844. doi: 10.1080/14786419.2018.1564293. [DOI] [PubMed] [Google Scholar]
- 20.Mabry T., Markham K., Thomas M. The Ultraviolet Spectra of Flavones and Flavonols. Springer; Berlin/Heidelberg, Germany: 1970. [Google Scholar]
- 21.Agrawal P.K., Bansal M.C. Carbon-13 NMR of flavonoids. Stud. Org. Chem. 1989;39:564. [Google Scholar]
- 22.Torres R., Faini F., Delle Monache F., Delle Monache G. Two new O-geranyl coumarins from the resinous exudate of Haplopappus multifolius. Fitoterapia. 2004;75:5–8. doi: 10.1016/j.fitote.2003.06.003. [DOI] [PubMed] [Google Scholar]
- 23.Lawson A.M. Ph.D. Thesis. University of Limoges; Limoges, France: 2006. Phytochemical Study of a Tropical Fabaceae, Lonchocarpus Nicou, Preliminary Biological Assessment. [Google Scholar]
- 24.Mathias L., Da Silva B.P., Mors W.B., Parente J.P. Isolation and structural elucidation of a novel rotenoid from the seeds of Clitoria fairchildiana. Nat. Prod. Res. 2005;19:325–329. doi: 10.1080/14786410412331272022. [DOI] [PubMed] [Google Scholar]
- 25.Micco S., Zampella A., D’Auria M., Festa C., Marino S., Riccio R., Butts C., Bifulco G. Plakilactones G and H from a marine sponge. Stereochemical determination of highly flexible systems by quantitative NMR-derived interproton distances combined with quantum mechanical calculations of 13C chemical shifts. J. Org. Chem. 2013;9:2940–2949. doi: 10.3762/bjoc.9.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Newton S.M., Lau C., Gurcha S.S., Besra S.G. The evaluation of forty-three plant species for in vitro antimycobacterial activities; Isolation of active constituents. J. Ethnopharmacol. 2002;79:57–67. doi: 10.1016/S0378-8741(01)00350-6. [DOI] [PubMed] [Google Scholar]
- 27.Akinpelu A., Aiyegoro A., Okoh I. The in vitro antioxidant property of methanolic extract of Afzelia africana (Smith.) J. Med. Plants Res. 2010;4:2022–2027. doi: 10.5897/jmpr10.484. [DOI] [Google Scholar]
- 28.Buyinza D., Yang L., Derese S., Ndakala A., Coghi P., Heydenreich M., Wong V., Möller H., Yenesew A. Cytotoxicity of isoflavones from Millettia dura. Nat. Prod. Res. 2019;35:2744–2747. doi: 10.1080/14786419.2019.1660335. [DOI] [PubMed] [Google Scholar]
- 29.Kai-Ching T., Tan L.T., Chan C.K., Hong S.L., Chan C.G., Yap W.S., Pusparajah P., Lee H.L., Goh B.H. Formononetin: A Review of Its Anticancer Potentials and Mechanisms. Front. Pharmacol. 2019;10:820. doi: 10.3389/fphar.2019.00820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Derese S., Barasa L., Akala H.M., Yusuf A.O., Kamau E., Heydenreich M., Yenesew A. Prenyloxyderrone from the stem bark of Millettia oblata ssp. and the antiplasmodial activities of isoflavones from some Millettia species. Phytochem. Lett. 2014;8:69–72. doi: 10.1016/j.phytol.2014.02.001. [DOI] [Google Scholar]
- 31.Mann C.M., Markham J.L. A new method for determining the minimum inhibitory concentration of essential oils. J. Appl. Microbiol. 1998;84:538–544. doi: 10.1046/j.1365-2672.1998.00379.x. [DOI] [PubMed] [Google Scholar]
- 32.Palomino J.C., Martin A., Camacho M.P.F. Resazurin microtiter assay plate: Simple and inexpensive method for detection of drug resistance in mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2002;46:2720–2722. doi: 10.1128/AAC.46.8.2720-2722.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eloff J.N. A sensitive and quick microplate method to determine the minimal inhibitory concentration of plant extracts for bacteria. Planta Med. 1998;64:711–713. doi: 10.1055/s-2006-957563. [DOI] [PubMed] [Google Scholar]
- 34.Souza E.L., Stamford T.L.M., Lima E.O., Trajano V.N. Effectiveness of Origanum vulgare L. essential oil to inhibit the growth of food spoiling seasts. Food Control. 2007;18:409–413. doi: 10.1016/j.foodcont.2005.11.008. [DOI] [Google Scholar]
- 35.Araújo F.M., Ribeiro P.R., Guedes M.L.S., Young M.C.M., Martins D. A new isoflavone glucoside and other compounds from Poiretia bahiana C. Mueller: Chemophenetics, fragmentation pattern and biogenetic implications. Fitoterapia. 2021;153:104977. doi: 10.1016/j.fitote.2021.104977. [DOI] [PubMed] [Google Scholar]
- 36.Noghogne L., Gatsing D., Fotso, Kodjio N., Sokoudjou J., Kuiate J. In vitro antisalmonellal and antioxidant properties of Mangifera indica L. stem bark crude extracts and fractions. Br. J. Pharm. Res. 2015;5:29–41. doi: 10.9734/BJPR/2015/13390. [DOI] [Google Scholar]
- 37.Silva S., Gomes L., Leitão F., Coelho A.V., Boas L.V. Phenolic compounds and antioxidant activity of Olea europaea L. fruits and leaves. Food Sci. Technol. Int. 2006;12:385–396. doi: 10.1177/1082013206070166. [DOI] [Google Scholar]
- 38.Padmaja M., Sravanthi M., Hemalatha K.P.J. Evaluation of antioxidant activity of two Indian medicinal plants. J. Phytol. 2011;3:86–91. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The supporting information can be found in the Supplementary Materials.