Summary
As wildfire risks have elevated due to climate change, the health risks that toxicants from fire smoke pose to wildland firefighters have been exacerbated. Recently, the International Agency for Research on Cancer (IARC) has reclassified wildland firefighters’ occupational exposure as carcinogenic to humans (Group 1). Wildfire smoke contributes to an increased risk of cancer and cardiovascular disease, yet wildland firefighters have inadequate respiratory protection. The economic cost of wildland fires has risen concurrently, as illustrated by the appropriation of $45 billion for wildfire management over FYs 2011–2020 by the U.S. Congress. Occupational epidemiological studies of wildland firefighters are crucial for minimizing health risks; however, they must account for the mixture of exposures in wildfire smoke. This review focuses on four aspects of wildland firefighters’ health risks at the wildland-urban interface: 1) economic costs and health impact, 2) respiratory protection, 3) multipollutant mixtures, and 4) proactive management of wildfires.
Keywords: Wildfire, Wildland-urban interface (WUI), Firefighter, Multi-pollutant mixtures of fire smoke, Occupational and environmental health, Exposure assessment, Prescribed burn
Introduction
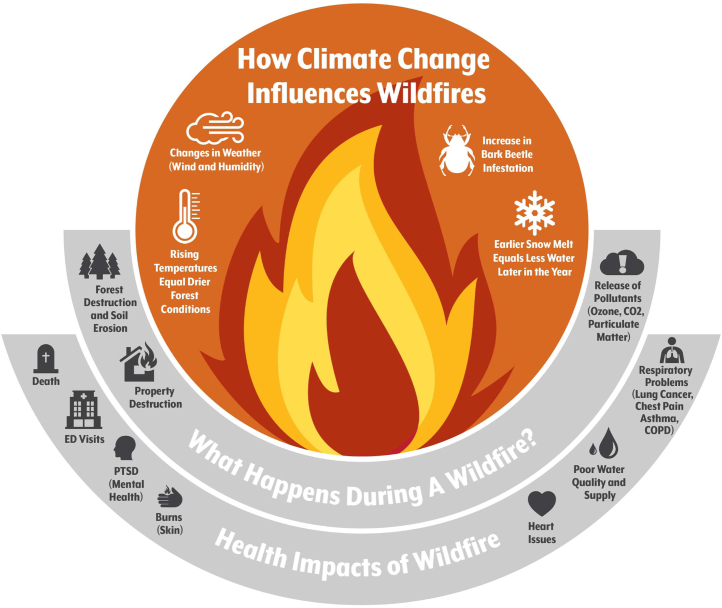
In June of 2022, the International Agency for Research on Cancer (IARC) reclassified the occupational exposure of structural and wildland firefighters as carcinogenic to humans (Group 1), the highest hazard category.1 Previously, the occupational exposure of firefighters was classified as possibly carcinogenic to humans (Group 2B). However, the toxicity of the working environment of firefighters, in particular, the wildland and the wildland-urban interface (WUI), has been exacerbated over the past 15 years by the escalating climate crisis. In 2015, the Paris Agreement was established to limit global warming and climate change, following which the United Nations and researchers around the world collaborated on an annual report, the Lancet Countdown. The 6th report, the most current, described the emerging health profile of the changing climate as code red because 72% of countries have experienced an increase in human exposure to wildfires.2 It has become more common for news media around the world to report on wildland fires because of climate change. Strikingly, the fires are often described as record-breaking, whether in terms of size of the burn, level of emissions, or even number of fatalities per year. Climate change alterations in wind patterns, temperatures, and levels of moisture around the globe affect the likelihood and magnitude of wildfires. Changes in the climate or weather patterns, including drought, are increasing the risk of wildland fires and the risk of co-morbidity from poor air quality (Fig. 1). Thus, for a considerable number of media around the world, the fight against wildland fires, including the devastating Brazilian wildfire of 2020, in which 77 million acres were burnt, has become daily news.3
Fig. 1.
The impact of climate change on wildfire behavior and human health.
<Image from Esposito, C. Wildfires, shut-downs, and behavior change: 2020 has been a big year for air quality and health. Colorado Health Institute, accessed Nov. 2022, https://www.coloradohealthinstitute.org>
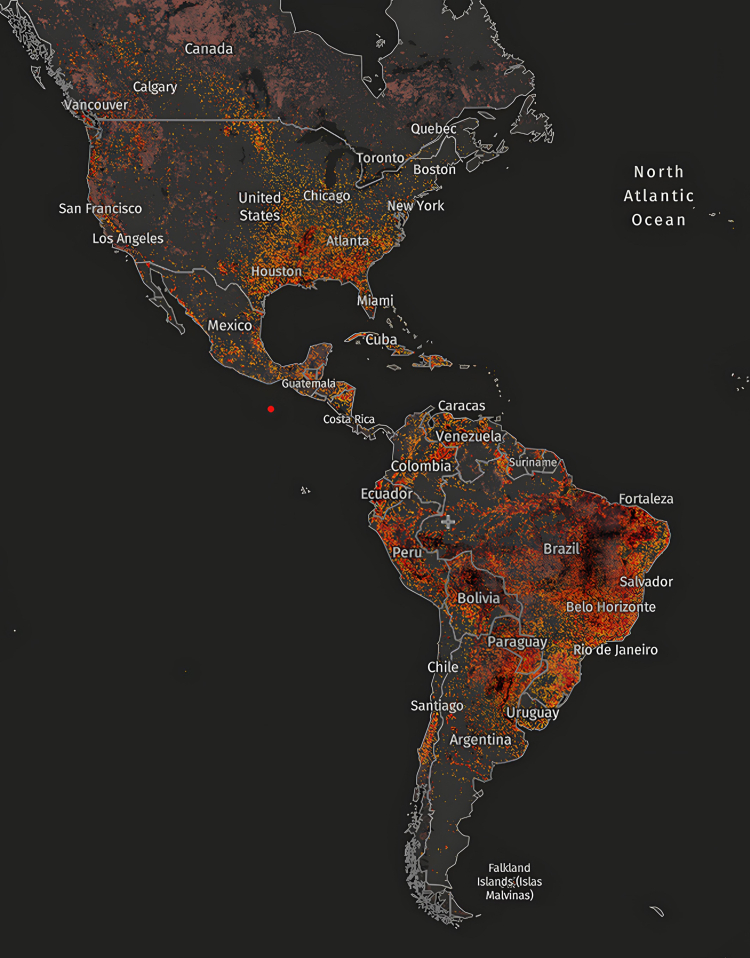
Furthermore, WUI fires have increased exposure to hazardous fire emissions from the combustion of man-made materials. The WUI is a hybrid of structural and wildland fire zones, or “the area where structures and other human developments meet or intermingle with undeveloped wildland fuels”.4 Thus, in the WUI, a fire burns homes and structures as well as the wildland, thereby consuming man-made materials in addition to natural fuels. From 2000 to 2016, the WUI in the U.S. increased rapidly, exhibiting 62% growth from 30.8 to 50 million houses, or roughly 350,000 new houses per year.5 Also during the same period, 15% of the WUI fires occurred in the Western U.S.6 In the top 10 wildfire-prone states, all located in the Western U.S., an estimated 4.5 million properties are at a high to extreme wildfire risk.7 Our understanding of exposure to contaminants from these fuels at wildfires is extensive. Yet, evidence-based studies have been inconclusive so far regarding adverse health effects because they do not use control populations or study long-term effects. An exposure assessment is the foremost step that should be taken. Most previous studies of health effects used questionnaires, secondary databases from fixed and temporary ground monitors, mathematical models, or satellite-based remote (Fig. 2) sensors to investigate exposure-response estimates. While monitoring data from remote sensing is available for long time periods in large areas on a global scale,8 the resulting exposure profiles lack accuracy and detail, leading to exposure misclassifications. Thus, a comprehensive health-relevant exposure assessment in the field is necessary for direct measurement and monitoring. From this perspective, we discuss the costs of fighting wildfires and the health impacts of exposure to wildfire smoke, the respiratory protection used by wildland firefighters, the effects of exposure to multi-pollutant mixtures on firefighters' health, and the proactive management of wildfires by prescribed fires.
Fig. 2.
Fire incidence map of the Americas. Each red dot indicates a spot where one of National Aeronautics and Space Administration (NASA)'s satellites detected a fire between August 2022 and November 2022.
<Image from Visible Infrared Imaging Radiometer Suite (VIIRS) Active Fires Global Forest Watch Open Data Portal, accessed Nov. 2022, https://www.globalforestwatch.org>
Costs of fighting wildfires in the U.S.
The overall federal budget set by the U.S. Congress contains an annual appropriation for the management of wildland fires. Congress funds all wildland fire-related activities on lands administered by the Department of the Interior and managed by the Office of Wildland Fire. Four bureaus are involved in managing wildland fires—the Bureau of Indian Affairs, the Bureau of Land Management, the National Park Service, and the U.S. Fish and Wildlife Service—as well as the U.S. Forest Service, a federal agency under the Department of Agriculture. For fiscal years 2011–2020, Congress appropriated a total of $45 billion for wildfire management.9 The FY2020 appropriation was over $6 billion, the highest appropriation to date. In addition, in the FY2023 appropriation specified $3 billion in adjustments for wildfire suppression.10 These recent actions imply that the federal government recognizes the significant impact of wildfires and thereby highlights the broad scope of research needed to address the unique challenges of wildfire-related activities, including the health of wildland firefighters.
Health impacts of exposure to wildfire smoke among U.S. firefighters
Over 82 million Americans have experienced poor air quality at the moderate level (PM2.5 15–35 μg/m3). Of those people, 10 million have experienced unhealthy air quality (PM2.5 > 35 μg/m3), which is defined as more than 10 days of exposure to wildfire smoke.11 Consequently, the mortality burden attributable to PM2.5 from chronic wildland fire smoke is ∼216,000 deaths annually.12 Navarro and colleagues13 have estimated that over a 25-year period, a firefighter working long seasons has an additional risk of 43% for lung cancer and 30% for cardiovascular disease. These findings are consistent with an earlier self-report subclinical study that showed significant links between more experienced wildland firefighters and a higher risk of hypertension and heart arrhythmias.14 Acute wildfire-smoke related PM2.5 increases all-cause mortality by 0.26% per year.8 More specifically, the exposure–response relationship has indicated that the 3-day moving average of wildfire smoke-related PM2.5 was significantly associated with mortality. The relative risks initially increase with respect to PM2.5 concentration for all-cause and cardiovascular mortality, levelling out at around 20 μg/m³.8 This relationship is more significant for respiratory mortality, as a marked increase in risk is observed at concentrations greater than 30 μg/m³.8 To the best of our knowledge, wildland firefighters have been underrepresented in occupational epidemiological studies, as the cohorts tend to consist of structure (mainly career) firefighters in metropolitan areas. Overall, U.S. firefighters have increased incidence and mortality risks associated with cancer and non-malignant respiratory diseases. For example, NIOSH-funded studies have reported excess cancer incidence (SMR = 1.09, 95% CI 1.06–1.12) and mortality rates (SMR = 1.14, 95% CI 1.10–1.18) for firefighters.15,16 The recently updated NIOSH mortality study confirms that firefighters are at an increased risk for all types of cancer (SMR = 1.12; 95% CI 1.08–1.16) compared with the general population.17
Respiratory protection for wildland firefighters
Most exposure-associated health research focuses on structural firefighters, particularly in live fire training, while wildland firefighters are less likely to be specifically addressed. Thus, their exposure profile is less well understood. Direct evaluations of the functional performance of respirators for wildland firefighters are disjointed because wildland firefighters do not use respiratory protection such as a self-contained breathing apparatus (SCBA) for several reasons. First, wildland firefighters spend extended periods of time at prescribed burns and incident wildfires, averaging from 8 to 13 h. Yet a SCBA cylinder only lasts 30–60 min, and carrying extra cylinders that weigh 30 lbs is impractical. Second, carrying a SCBA would drain the energy of a wildland firefighter due to its weight, limit the carrying capacity for other tools and supplies, increase the risk of falling on uneven terrain because of potential body unbalance,18 and cause heat stress under environmental thermal conditions.19 Third, wildland firefighters cover extensive areas, often requiring them to be mobile instead of staying in one spot. Thus, the weight and mobility of respirators are significant factors affecting the performance of wildland firefighters. Instead, wildland firefighters sometimes wear NIOSH-approved N95 filtering facepiece respirators (assigned protection factor [APF] = 10) and/or cotton bandanas (i.e., Nomex® shrouds/balaclavas) or often, nothing. These practices are insufficient for avoiding inhalation exposure because none of these options supply fresh air and/or oxygen and hence provide little protection against the gas phase of smoke contaminants. The N95 respirator has been suggested to be the only one that can provide protection against particulate-phase contaminants.20
Of the respiratory protection equipment used by firefighters, the SCBA has the highest APF (=10,000). An APF of 10,000 indicates that the concentration of contaminants in the outside air is expected to be reduced at least 10,000 times inside the SCBA. Various studies have characterised the effectiveness of SCBAs by fire stage (i.e., knockdown vs. overhaul). Using both spirometry and serum pneumoproteins, one study concluded that the overhaul process could potentially decrease lung function in the absence of an SCBA or air-purifying respirator.21 More recent studies have campaigned for firefighters to wear SCBAs during overhauls because they tend to take them off as soon as knockdown is completed.22 The National Fire Protection Association (NFPA) 1852: Standard on Selection, Care, and Maintenance of Open-Circuit Self-Contained Breathing Apparatus addresses practices for SCBA protective equipment; however, only interior structural firefighters are subject to this standard. The only standard that addresses respirators for wildland firefighters is NFPA 1984: Standard on Respirators for Wildland Firefighting Operations. However, it focusses more on safety specifications (i.e., labelling, design, and performance of respirators) for manufacturers than for firefighters. The most recent edition (2022) has been updated to recommend that respiratory protection equipment be considered “when a large number of WUI firefighters are exposed to a variety of respiratory hazards and when medical and health concerns increase for firefighters exposed to products of combustion in WUI firefighting conditions”. Yet, the standard is still vague. Thus, although research does show that wildland firefighters are exposed to hazards from smoke, there is no approved respiratory protection for wildland firefighting and no commercially available respirators that meet the immediate need to protect them from both airborne exposures and heat stress. The U.S. Department of Homeland Security has developed a prototype scarf-type respiratory protection system that integrates filter cartridges, a powered air purifying respirator (PAPR), and charcoal sorbent for wildland firefighters. However, universal acceptance of the new system by wildland firefighters will take time.
Multi-pollutant mixture exposures from smoke at wildfires
Studies over the past 30 years have focussed on exposure quantification and potential health effects. In 1992, the Harrison group in CA conducted the first study to quantify exposure to wildland fire smoke,23 measuring health-relevant occupational exposure levels to smoke during fire suppression. Since then, it has been well-documented that wildfire smoke is comprised of many individual pollutants, including polycyclic aromatic hydrocarbons (PAHs), volatile organic compounds (VOCs, i.e., acrolein, benzene, formaldehyde), carbon monoxide, nitrogen dioxide, PM2.5, and more. To the best of our knowledge, most earlier studies assessed one pollutant at a time, yet wildland firefighters are exposed to a combination of pollutants. Assessing multi-pollutant mixture exposure from wildland fire smoke, including overall effect estimation of the mixture, toxic agent identification associated with the health outcome, and the association between outcome and a priori-defined group, is a relatively new area of research.24 As fires in a WUI zone mix smoke from both structural (i.e., synthetic products) and wildland (i.e., pure biomass) fuel materials, the dimensions of the exposure matrix are complex. Of the various methods for assessing multi-pollutant mixture exposure, Bayesian approaches including Bayesian Kernel Machine Regression (BKMR), Bayesian Multiple Index Model (BMIM), and Bayesian Variable Selection Model (BVSM) have been widely studied and applied, as prior information on exposure effects can be incorporated into the models.25 In addition to Bayesian approaches, quantile regression and penalised regression approaches are also available for mixture exposures analysis.25 For field assessments, the task performed, type of structural fire in WUI, type of vegetation, size of burned areas, and duration of fire suppression can be recorded. Also, the toxic equivalency factor,26 the lung/air and blood/air and partition coefficients for estimating inhalation exposure risks,27 and the IARC classification of toxicants can be included to assess the overall effect of multi-pollutant mixture exposure on firefighters’ health.
Proactive role of prescribed burns
Wildland firefighters are responsible for the fire management of natural fuels.20 U.S. fire departments responded to 1.4 million fires in 2020, which corresponds to one fire response every 23 s.28 Of these fires, 277,000 (20% of total fires) occurred in wildlands, including brush, grass, and forest fires, while 490,000 (35% of total fires) occurred in structures. Although the frequency of fire incidents in wildlands is lower than that in structures, a natural ecosystem takes longer to recover post-fire, and the total loss is relatively higher in a wildland fire. In 2019–2020, 5800 homes were destroyed, and 97,000 buildings were threatened by only four major wildfires on the West Coast. Over the last decade, 2011–2021, more than 82 million acres were burned and destroyed by the 660,000 wildfires that occurred. In 2021 alone, ∼59,000 wildfires across the nation consumed 7.1 million acres,29 with an estimated insured loss of at least $45 billion from the top ten costliest wildland fires.7 Thus, training to fight wildfires safely and proactively in a controlled operational fire environment, such as a prescribed burn, is critical for wildland firefighters. Prescribed burns are intentionally set for the purpose of reducing wildfire risks by burning accumulated combustible natural fuels during favorable meteoric conditions, thereby controlling wildfire hazards and the availability of parched vegetation within designated boundaries. Prescribed burns are used extensively throughout the U.S. as part of a comprehensive fire management strategy. Over the past two decades (1998–2018), the number of prescribed burns has grown from 4277 to 450,335, approximately a 100-fold increase.29 The number of acres subject to prescribed burns has also increased over the same period by a factor of 7, from 0.9 to 6.4 million. During this period, a total of 57 million acres have been burned by prescribed burns, an acreage equivalent in size to the state of Minnesota. The latest survey conducted by state forestry agencies reported that 2019 was the first year in which the number of prescribed burns totalled over 10 million acres.30 Increasing the number of prescribed fires to manage wildland fires rather than suppressing them aggressively can promote adaptive resilience as the climate continues to warm. Specifically, prescribed fires, ignited under cooler and moister conditions than typical wildfires, can reduce natural fuels and minimize the risk of uncontrolled forest wildfires near communities.6 In contrast to wildfires, the risks of prescribed fires are relatively low because the latter are successfully contained within planned perimeters and often produce fewer toxins with lesser exposure given that most of the fuels are natural—forest, grass, or brush, etc. Promoting more prescribed fires near the WUI with residential communities is an important step toward addressing the ongoing crisis of increasing wildfires.
Conclusions
We anticipate that health risks to firefighters from wildfire smoke will continue rising based on the ongoing climate change and the increased acreage of WUI. While wildfire is unavoidable, we can reduce the extent of toxicant exposures by conducting more prescribed burns, which help minimize the frequency and risk of uncontrolled emergency wildfires. We can also reduce the extent of exposure by designing more effective respiratory protection for wildland firefighters. Wildland firefighters are exposed to hazards from fire smoke, and our understanding of exposure to individual contaminants at wildfires is extensive. Yet, fire smoke is complex, often consisting of mixed smoke toxicants, and the WUI is a more complicated environment than that of either structural or wildland fires. Multi-pollutant mixture exposure assessment is one of the most important steps that must be taken, as statistical tools are readily available.
Contributors
Conceptualization–JH; data curation–JH; formal analysis–N/A; funding acquisition–NSC, MZ, ZL, JH; investigation–NSC, MZ, RJA, ZL, CX, XX, JH; methodology–NSC, MZ, RJA, ZL, CX, XX, JH; project administration–NSC, MZ, RJA, ZL, CX, XX, JH; resources–NSC, MZ, RJA, ZL, CX, XX, JH; software–JH; supervision–JH; validation–NSC, MZ, RJA, ZL, CX, XX, JH; visualization–N/A; writing-original draft–JH; and writing-review and editing–NSC, MZ, RJA, ZL, CX, XX, JH.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
The authors declare no conflict of interest.
Acknowledgments
The Federal Emergency Management Agency/Fire Prevention and Safety (FEMA/FP&S) Program of the U.S. Department of Homeland Security (EMW-2018-FP-00668) has provided support for NSC, MZ, and ZL. JH was supported by the Centers for Disease Control and Prevention (CDC)/National Institute for Occupational Safety and Health (NIOSH) (K01OH011891).
Role of funding source: The perspectives and conclusions in this manuscript are those of the authors and do not necessarily represent the views of the funding agencies. The funders have played no role in this research.
References
- 1.Demers P.A., DeMarini D.M., Fent K.W., et al. Carcinogenicity of occupational exposure as a firefighter. Lancet Oncol. 2022;2045(22):4–5. doi: 10.1016/S1470-2045(22)00390-4. [DOI] [PubMed] [Google Scholar]
- 2.Romanello M., McGushin A., Di Napoli C., et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet. 2021;398(10311):1619–1662. doi: 10.1016/S0140-6736(21)01787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pivello V.R., Vieira I., Christianini A.V., et al. Understanding Brazil's catastrophic fires: causes, consequences and policy needed to prevent future tragedies. Perspect Ecol Conserv. 2021;19(3):233–255. [Google Scholar]
- 4.Radeloff V.C., Hammer R.B., Stewart S.I., Fried J.S., Holcomb S.S., McKeefry J.F. The wildland–urban interface in the United States. Ecol Appl. 2005;15(3):799–805. [Google Scholar]
- 5.Burke M., Driscoll A., Heft-Neal S., Xue J., Burney J., Wara M. The changing risk and burden of wildfire in the United States. Proc Natl Acad Sci U S A. 2021;118(2):1–6. doi: 10.1073/pnas.2011048118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schoennagel T., Balch J.K., Brenkert-Smith H., et al. Adapt to more wildfire in western North American forests as climate changes. Proc Natl Acad Sci U S A. 2017;114(18):4582–4590. doi: 10.1073/pnas.1617464114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Insurance Information Institute . 2021. Verisk wildfire risk analytics used data from fireLine®, Verisk's wildfire risk management tool.https://www.iii.org/fact-statistic/facts-statistics-wildfires# Available from: [Google Scholar]
- 8.Chen G., Guo Y., Yue X., et al. Mortality risk attributable to wildfire-related PM2·5 pollution: a global time series study in 749 locations. Lancet Planet Health. 2021;5(9):e579–e587. doi: 10.1016/S2542-5196(21)00200-X. [DOI] [PubMed] [Google Scholar]
- 9.Hoover K. Federal wildfire management: ten-year funding trends and issues (FY2011-FY2020) Congr Res Serv. 2020 Report No. R46583. [Google Scholar]
- 10.U.S. Government Publishing Office . U.S. Office of Management and Budget; Washington, DC: 2022. Budget of the U.S. government fiscal year 2023 (ISBN 978-0-16-095232-6) [Google Scholar]
- 11.Rappold A.G., Reyes J., Pouliot G., Cascio W.E., Diaz-Sanchez D. Community vulnerability to health impacts of wildland fire smoke exposure. Environ Sci Technol. 2017;51(12):6674–6682. doi: 10.1021/acs.est.6b06200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O'Dell K., Bilsback K., Ford B., et al. Estimated mortality and morbidity attributable to smoke plumes in the United States: not just a western US problem. Geohealth. 2021;5(9):1–17. doi: 10.1029/2021GH000457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Navarro K.M., Kleinman M.T., Mackay C.E., et al. Wildland firefighter smoke exposure and risk of lung cancer and cardiovascular disease mortality. Environ Res. 2019;173:462–468. doi: 10.1016/j.envres.2019.03.060. [DOI] [PubMed] [Google Scholar]
- 14.Semmens E.O., Domitrovich J., Conway K., Noonan C.W. A cross-sectional survey of occupational history as a wildland firefighter and health. Am J Ind Med. 2016;59(4):330–335. doi: 10.1002/ajim.22566. [DOI] [PubMed] [Google Scholar]
- 15.Daniels R.D., Kubale T.L., Yiin J.H., et al. Mortality and cancer incidence in a pooled cohort of US firefighters from San Francisco, Chicago and Philadelphia (1950-2009) Occup Environ Med. 2014;71:388–397. doi: 10.1136/oemed-2013-101662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daniels R.D., Bertke S., Dahm M.M., et al. Exposure-response relationships for select cancer and non-cancer health outcomes in a cohort of US firefighters from San Francisco, Chicago and Philadelphia (1950-2009) Occup Environ Med. 2015;72(10):699–706. doi: 10.1136/oemed-2014-102671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pinkerton L., Bertke S.J., Yiin J., et al. Mortality in a cohort of US firefighters from San Francisco, Chicago and Philadelphia: an update. Occup Environ Med. 2020;77(2):84–93. doi: 10.1136/oemed-2019-105962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Navarro K.M., Cisneros R., Noth E.M., et al. Occupational exposure to polycyclic aromatic hydrocarbon of wildland firefighters at prescribed and wildland fires. Environ Sci Technol. 2017;51(11):6461–6469. doi: 10.1021/acs.est.7b00950. [DOI] [PubMed] [Google Scholar]
- 19.NTDP . National Technology and Development Program. US Dep Agric For Serv; 2021. Wildland firefighter heat stress National Technology and Development Program Field Study; pp. 2051–2815. [Google Scholar]
- 20.Reinhardt T.E., Ottmar R.D. Baseline measurements of smoke exposure among wildland firefighters. J Occup Environ Hyg. 2004;1(9):593–606. doi: 10.1080/15459620490490101. [DOI] [PubMed] [Google Scholar]
- 21.Burgess J.L., Nanson C.J., Bolstad-johnson D.M., et al. Adverse respiratory effects following overhaul in firefighters. J Environ Monit. 2001;43(5):467–473. doi: 10.1097/00043764-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Fent K.W., Evans D., Booher D., et al. Volatile organic compounds off-gassing from firefighters' personal protective equipment ensembles after use. J Occup Environ Hyg. 2015;12(4):227–234. doi: 10.1080/15459624.2015.1025135. [DOI] [PubMed] [Google Scholar]
- 23.Liu D., Tager I.B., Balmes J.R., Harrison R.J. The effect of smoke inhalation on lung function and airway responsiveness in wildland fire fighters. Am Rev Respiatory Dis. 1992;146(6):1469–1473. doi: 10.1164/ajrccm/146.6.1469. [DOI] [PubMed] [Google Scholar]
- 24.Gibson E.A., Goldsmith J., Kioumourtzoglou M.-A. Complex mixtures, complex analyses: an emphasis on interpretable results. Curr Environ Heal Reports. 2019;6(2):53–61. doi: 10.1007/s40572-019-00229-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Joubert B.R., Kioumourtzoglou M.-A., Chamberlain T., et al. Powering research through innovative methods for mixtures in epidemiology (PRIME) program: novel and expanded statistical methods. Int J Environ Res Public Health. 2022;19(3) doi: 10.3390/ijerph19031378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nisbet I.C.T., LaGoy P.K. Toxic equivalency factors (TEFs) for polycyclic aromatic hydrocarbons (PAHs) Regul Toxicol Pharmacol. 1992;16(3):290–300. doi: 10.1016/0273-2300(92)90009-x. [DOI] [PubMed] [Google Scholar]
- 27.Dutta D., Chong N.S., Lim S.H. Endogenous volatile organic compounds in acute myeloid leukemia: origins and potential clinical applications. J Breath Res. 2018;12(3) doi: 10.1088/1752-7163/aab108. [DOI] [PubMed] [Google Scholar]
- 28.Aherns M., Evarts B. 2021. Fire loss in the United States during 2020. National fire protection association No. FLX10. [Google Scholar]
- 29.NICC . National Interagency Coordination Center, National Interagency Fire Center; Boise, Idaho: 2021. Wildland fire summary and statistics annual report 2021.https://www.nifc.gov/fire-information/statistics Available from: [Google Scholar]
- 30.Melvin M.A. 2020. National prescribed fire use report. National association of state foresters and coalition of prescribed fire councils technical bulletin 04-20. [Google Scholar]