Abstract
Background
Although current studies have identified sleep disorders as an independent risk factor for suicide, the relationship between sleep disorders and suicide risk has not been well established. This study explored whether anxiety and depressive symptoms are used as mediators to participate in the impact of sleep quality on suicide risk.
Methods
This is a cross-sectional study. We administered a psychological questionnaire to the participants, using a combination of self-assessment and psychiatrist assessment.Sleep quality, suicide risk, level of anxiety and depressive symptoms were assessed by PSQI, NGASR, SAS and SDS.The study subjects were 391 hospitalized COVID-19 patients from Wuhan hospitals. We used model 6 in the PROCESS (version 3.5) plug-in of SPSS software to conduct mediation test with sleep quality as the independent variable, suicide risk as the dependent variable, level of anxiety and depressive symptoms as intermediate variables.
Results
The severity of anxiety and depressive symptoms and the risk of suicide in the sleep disorder group (63.15 ± 13.71, 59.85 ± 13.38, 6.52 ± 3.67) were higher than those in the non-sleep disorder group (49.83 ± 13.14, 44.87 ± 10.19, 2.87 ± 3.26) (P < 0.001). The mediation model works well, The total indirect effect was 0.22 (95%CI = [0.17, 0.28]), and the direct effect was 0.16 (95%CI = [0.08, 0.24]).
Limitations
This study used a self-assessment scale.
Conclusions
Anxiety and depressive symptoms played a chain mediating role between sleep quality and suicide risk.
Keywords: COVID-19, Sleep quality, Suicide risk, Depressive symptom, Anxiety symptom, Mediation
Highlights
-
•
Sleep quality were positively associated with suicide risk in COVID-19 patients.
-
•
Anxiety and depressive symptoms acted as a chain mediating role between sleep quality and suicide risk.
-
•
By reducing symptoms of anxiety and depression, thereby improving sleep quality, and thus reducing the risk of suicide.。
1. Introduction
The COVID-19 pandemic has triggered all kinds of mental health issues, including sleep disorders, anxiety, depression, suicide, and more [[1], [2], [3], [4]]. During the pandemic, COVID-19 patients may be a group with a higher psychological burden, with a higher prevalence of sleep disorders, depression, anxiety, and a higher risk of suicide compared to the rest of the population [4,5]. A meta-analysis in China found that 34% of COVID-19 patients had sleep disorders, 45% had depression, and 47% had anxiety disorders [6]. Suicide is one of the leading causes of death worldwide and a major public health problem [7]. According to the WHO, 800,000 people die by suicide each year, with a suicide rate of 10.7 per 100,000 people [8]. Despite efforts to develop new interventions, suicide rates have been rising over the past two decades [9]. There are indications that isolation, loneliness, and stigma may increase the risk of suicide for COVID-19 patients [10,11]. Sleep disorders, including insomnia, daytime sleepiness, and sleep-related movement [12], can have a serious impact on people's mental health [13]. Several previous studies have suggested that sleep disorders are an independent risk factor for suicidal behavior [2,14,15]. Insomnia and nightmares are associated with an increased risk of suicide, according to a systematic review [16]. A study of military veterans showed that taking sleep medication significantly reduced the risk of suicide attempts in patients with sleep disorders [17].
But further research is needed to understand the relationship between sleep quality and suicide [15]. At the same time, current studies on psychological problems during the COVID-19 pandemic mainly focus on non-COVID-19 populations, and there are few studies on COVID-19 patients [6]. In addition, previous research focused on exploring the link between sleep quality and suicide risk, but factors that could moderate the relationship were neglected. Therefore, the identification of preventable intermediate factors may provide new directions for early intervention in suicide.
1.1. Review literature
The emotional problem may be one potential factor linking suicide risk to sleep [18]. Current research has shown that sleep is closely related to mental disorders such as anxiety and depression [2,19]. It is worth noting that sleep disorders can often predict the occurrence of anxiety and depression. Sleep disorders, such as insomnia, can cause the dysfunction of the biological sleep-wake system, which leads to the interruption of the emotional regulation process and then causes emotional problems [15]. Longitudinal studies indicate that sleep disturbance is not only a prodromal symptom of depression but also an independent risk factor for subsequent depression relapse [20]. It is well known that anxiety and depression can be risk factors for suicide [21]. Emotional problems have been shown to be associated with an increased risk of suicide in studies of different populations [22]. Therefore, emotional problems, such as anxiety and depression, may play an intermediary role between sleep disorders and suicide risk [15]. A study of Canadian military personnel identified depressive symptoms as an intermediary in sleep disorders, trauma-related nightmares, and suicidal ideation [23]. Another study of 972 adults on a crowdsourcing website showed that emotional regulation mediated nightmares and suicide risk [24].
It should not be ignored that anxiety and depression are often comorbidities, and there is a positive correlation between them. More severe depressive symptoms are often accompanied by more severe anxiety symptoms [6].
1.2. Research questions
Therefore, we found that anxiety and depressive symptoms may play a chain mediating role between sleep quality and suicide risk. However, there are few types of researches on this. In this study, participants' sleep quality, suicide risk, anxiety, and depressive symptoms were investigated by a psychological questionnaire, and SPSS software was used as mediating test. The main research questions are: (1) whether sleep quality is associated with suicide risk in COVID-19 patients. (2) Whether anxiety and depressive symptoms play a chain mediating role between sleep quality and suicide risk in COVID-19 patients. To investigate psychological problems in COVID-19 patients and the impact of sleep disorders on suicide risk.
1.3. Model hypothesis
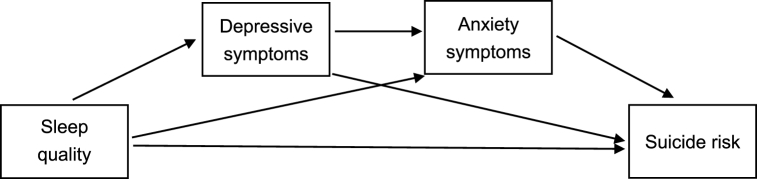
Therefore, we hypothesized that anxiety and depressive symptoms play a chaining mediating role between sleep quality and suicide risk in COVID-19 patients, as detailed in the conceptual model shown in Fig. 1.
H1
Suicide risk, depressive symptoms, anxiety symptoms, and sleep quality were significantly associated with the other three, respectively.
H2
Sleep quality positively predicts suicide risk in COVID-19 patients.
H3
Sleep quality affects suicide risk in COVID-19 patients through anxiety symptoms.
H4
Sleep quality influences suicide risk in COVID-19 patients through depressive symptoms.
H5
Sleep quality influences the risk of suicide in COVID-19 patients through the chain-mediating effect of anxiety and depressive symptoms.
Finally, this study confirmed the above hypothesis, demonstrating that anxiety and depressive symptoms play a chain mediating role between sleep quality and suicide risk.
Fig. 1.
Hypothesized conceptual model of the chain mediation.
2. Methods
2.1. Study object and data collection
Participants were COVID-19 inpatients from the Department of Infectious Diseases of Wuhan First Hospital and Fever Ward 12, 14, and 15 of Houhu Hospital of Wuhan Central Hospital, Hubei Province, China. We conducted a psychological questionnaire survey on these patients from January 2, 2020, to March 10, 2020, using a combination of self-assessment and psychiatrist assessment. Before the investigation, all researchers were trained on measurement tools and survey processes, and a consistency test was conducted after the investigation. Patients with a prior history of mental or psychological illness were excluded. Finally, 371 valid data were obtained, of which 46 patients were determined to have sleep disorders. Informed consent from the patient was obtained prior to the investigation. This study was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University.
2.2. Measures
2.2.1. Sleep quality
Pittsburgh Sleep Quality Index (PSQI) was used to measure sleep quality. It consists of 18 scoring questions, including 7 main components of sleep quality, the time required to fall asleep, total sleep time, sleep efficiency, sleep disorders, hypnotic drugs, and daytime dysfunction. Each component is scored according to grades 0–3, and the total score of each component is the PSQI total score, which ranged from 0 to 21. Higher scores indicate poorer sleep quality. BUYSSE proposed that “Good” sleep quality is 0–5 points, “ok” sleep quality is 6–10 points, “average” sleep quality is 11–15 points, and “poor” sleep quality is 16–21 points [25]. The scale has good reliability and validity (Cronbach’s α = 0.85) [26]. In our research, scores between 16 and 21 were considered to have sleep disorders.
2.2.2. Suicide risk
To evaluate suicide risk, we used the Nurses' Global Assessment of Suicide Risk Scale (NGASR), which is a reliable tool for assessing suicide risk, especially for patients with acute psychosis [[27], [28], [29]]. It includes 15 items, such as feelings of hopelessness, plans to take suicide action a history of attempted suicide, and so on, and each item has two answers: “yes” and “no”, and “no” counts as 0 points, and “yes” counts as 1 or 3 points according to the bonus rule. Finally, the total score is obtained under the extra points rules. A higher score means a higher risk of suicide. Low risk ≤5 points, medium risk 6–8 points, high risk 9–11 points, extremely high risk ≥12 points [30].
2.2.3. .Depressive symptoms
Depressive symptoms were accessed by using SDS (Self-rating Depression Scale), which is a valuable tool for screening clinically significant depression [31]. It contains 20 items, each item is divided into four grades according to the frequency of symptoms. The sum of the scores of each item is the total rough score, the total rough score × 1.25, and the integer part is the standard score. As the score increases, the degree of depressive symptoms becomes more severe. The standard score of ≤49 means no depressive symptoms, 50–59 means mild depressive symptoms, 60–69 means moderate depressive symptoms, and ≥70 means severe depressive symptoms [32].
2.2.4. Anxiety symptoms
We used SAS (Self-rating Anxiety Scale) to determine anxiety symptoms, and SAS has proved to be an effective tool for the assessment of anxiety symptoms [33]. It has 20 items and is scored on a scale of 1–4. The standard score is calculated by adding the scores for each of the 20 items and multiplying them by 1.25 to get the integer part. The higher the standard score, the more severe the anxiety symptoms. A score below 50 is considered no anxiety symptoms, 50–59 is considered mild anxiety symptoms, 60–69 is considered moderate anxiety symptoms, and above 69 is considered severe anxiety symptoms [34].
2.3. Statistical analyses
All our statistical analyses were carried out using SPSS software (version 26). First, Harman's single-factor test was adopted to test common method biases in the raw data. Second, to explore and summarize the variables, participants were divided into a sleep disorder group and a non-sleep disorder group for descriptive statistics. An independent sample T-test was used for measurement data satisfying normal distribution, and the results were expressed as M ± SD. The enumeration data were compared between groups using the χ 2 test, and the results were expressed as n (%). Third, we employed Pearson correlation analysis to analyze the participants' NGASR total score, SDS total score, SAS total score, PSQI total score, and age to determine the correlation between suicide risk, anxiety symptoms, depressive symptoms, and sleep quality. As the correlation coefficient gets closer to 1, the correlation between variables becomes stronger [35]. Finally, based on the hypothesis, we selected the Bootstrap method of the SPSS plug-in PROCESS (version 3.5) developed by Andrew F Hayes for mediation analysis of relevant variables, which is specially developed for testing complex models [36]. We chose model 6, with sleep quality as the independent variable, suicide risk as the dependent variable, depressive symptoms, and anxiety symptoms as the intermediary variables, and age as the covariate. In case CI (95%) does not contain 0, the mediating effect is significant. In this study, statistical significance was defined as P < 0.05.
3. Results
3.1. Common method deviation test
The outcomes showed that there were 22 components with characteristic roots greater than 1, and the variance explanation rate of the first component was 25.26%, which was less than the critical standard of 40%, indicating that the common method bias of this study was not obvious.
3.2. Descriptive analysis
The distribution characteristics of the participants were summarized in Table 1. Of the 371 COVID-19 patients, 46 (12.4%) suffered from sleep disorders. Compared with the non-sleep disorder group, the proportion of history of the physical disease (P < 0.001) and age (p = 0.003) were larger and older in the sleep disorder group, and there was no significant difference in gender (p = 0.092), an education level (p = 0.562) and city of work (p = 0.594) between the two groups. The severity of depressive symptoms and anxiety symptoms and the risk of suicide in the sleep disorder group were higher than those in the other group. (all p < 0.001).
Table 1.
Descriptive analysis
| Sleep disorders (N=46) | Non-sleep disorders (N=325) | P | |
|---|---|---|---|
| Age | 40.63±8.48 | 36.23±9.56 | 0.003 |
| Sex | |||
| male | 7 (15.2%) | 87 (26.8%) | 0.092 |
| Female | 39 (84.8%) | 238 (73.2%) | |
| History of physical illness | |||
| With | 15(32.6%) | 37 (11.4%) | <0.001 |
| Without | 31(67.4%) | 288 (88.6%) | |
| Education level | |||
| Bachelor degree and below | 29(63%) | 113(34.8%) | 0.562 |
| Master degree and above | 63(37%) | 212(65.2%) | |
| Work city | |||
| Wuhan | 46 (100%) | 323 (99.4%) | 0.594 |
| Non-Wuhan | 0 | 2 (0.6%) | |
| Depressive symptoms | 63.15±13.71 | 49.83±13.14 | <0.001 |
| Anxiety symptoms | 59.85±13.38 | 44.87±10.19 | <0.001 |
| Suicide risk | 6.52±3.67 | 2.87±3.26 | <0.001 |
3.3. Correlation between variables
Correlation analysis demonstrated that suicide risk was positively and significantly correlated with depressive symptoms (P < 0.001), anxiety symptoms (P < 0.001), sleep quality (P < 0.001), and age (P < 0.01). Depressive symptoms were obviously and positively correlated with anxiety symptoms (P < 0.001) and sleep quality (P < 0.001), but not remarkably correlated with age (P > 0.05). Anxiety symptoms were notably and positively correlated with sleep quality (P < 0.001), but not appreciably correlated with age (P > 0.05). Sleep quality and age (P < 0.01) were positively and outstandingly correlated (see Table 2). H1 was confirmed.
Table 2.
Analysis of related variables
| M± SD | Suicide risk | Depressive symptoms | Anxiety symptoms | Sleep quality | Age | |
|---|---|---|---|---|---|---|
| Suicide risk | 3.32±3.52 | 1 | ||||
| Depressive symptoms | 51.48±13.90 | 0.59∗∗∗ | 1 | |||
| Anxiety symptoms | 46.73±11.71 | 0.60∗∗∗ | 0.80∗∗∗ | 1 | ||
| Sleep quality | 9.46±4.53 | 0.50∗∗∗ | 0.48∗∗∗ | 0.60∗∗∗ | 1 | |
| Age | 36.78±9.53 | 0.16∗∗ | 0.04 | 0.07 | 0.16∗∗ | 1 |
illustrate significant correlation (P<0.01)
illustrate significant correlation (P<0.001)
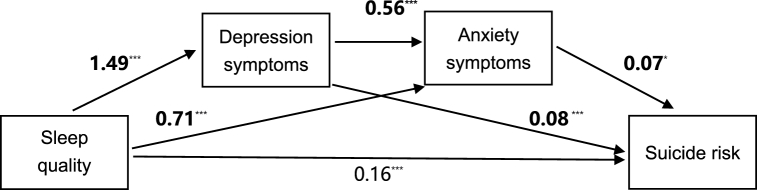
3.4. The mediation analysis
The analysis results of PROCESS (version 3.5) were presented in Table 3 and Fig. 2. After controlling for age, sleep quality could positively predict depressive symptoms (β = 1.49, SE = 0.14, T = 10.51, P < 0.001), anxiety symptoms (β = 0.71, SE = 0.09, T = 8.36, P < 0.001), and suicide risk (β = 0.16, SE = 0.04, T = 4.17, P < 0.001). Depressive symptoms could cause severe anxiety symptoms (β = 0.56, SE = 0.03, T = 20.54, P < 0.001) and an increased risk of suicide (β = 0.08, SE = 0.02, T = 4.71, P < 0.001). Anxiety symptoms actively promoted the risk of suicide (β = 0.07, SE = 0.02, T = 7.10, P < 0.05). The upshots displayed that the model fits well. Specifically, the effect of sleep quality on suicide risk is mainly through the following four pathways: (1) Sleep disordesr → Suicide risk. This confirmed H2. (2) Sleep quality → Anxiety symptoms → Suicide risk. This affirmed H3. (3) Sleep disordesr → Depressive symptoms →Suicide risk. This proved H4. (4) Sleep quality → Depressive symptoms → Anxiety symptoms → Suicide risk. This verified H5.
Table 3.
Predictive relationship between variables
| Outcome variable | Predictor variable | β | SE | T | CI(95%) |
R2 | F | |
|---|---|---|---|---|---|---|---|---|
| LLCI | ULCI | |||||||
| Depressive symptoms | Sleep quality | 1.49∗∗∗ | 0.14 | 10.51 | 1.21 | 1.77 | 0.23 | 55.55 |
| Age | -0.06 | 0.07 | -0.90 | -0.19 | 0.07 | |||
| Anxiety symptoms | Sleep quality | 0.71∗∗∗ | 0.09 | 8.36 | 0.55 | 0.88 | 0.70 | 286.68 |
| Depressive symptoms | 0.56∗∗∗ | 0.03 | 20.54 | 0.51 | 0.62 | |||
| Age | 0.01 | 0.04 | 0.02 | 0.07 | 0.07 | |||
| Suicide risk | Sleep quality | 0.16∗∗∗ | 0.04 | 4.17 | 0.08 | 0.24 | 0.44 | 70.67 |
| Depressive symptoms | 0.08 ∗∗∗ | 0.02 | 4.71 | 0.05 | 0.11 | |||
| Anxiety symptoms | 0.07∗ | 0.02 | 7.10 | 0.02 | 0.11 | |||
| Age | 0.04∗ | 0.01 | 2.44 | 0.01 | 0.06 | |||
illustrate significant correlation (P<0.05)
illustrate significant correlation (P<0.001)
Fig. 2.
Chain intermediary model. * illustrate significant correlation (P < 0.05; *** illustrate significant correlation (P < 0.001).
The consequents of mediation analysis demonstrated that the indirect effect of the path with depression as the mediating variable was 0.12 (95% CI = [0.07, 0.17]), and the effect ratio was 31.58%. When anxiety was the mediating variable, the indirect effect was 0.05 (95% CI = [0.02, 0.08]), and the effect ratio was 13.16%. When depression and anxiety were used as mediator variables, the indirect effect was 0.05 (95%CI = [0.02, 0.10]), and the effect ratio was 13.16%. The total indirect effect was 0.22 (95%CI = [0.17, 0.28]), and the effect amount was 57.9%. The direct effect ratio was 0.16 (95% CI = [0.08, 0.24), and the effect ratio was 42.1% (see Table 4).
Table 4.
The effect of each path
| Model | Effect | Effect ratio | Boot SE | CI(95%) |
|
|---|---|---|---|---|---|
| LLCI | ULCI | ||||
| Sleep disordesr→ Depressive symptoms →Suicide risk |
1.49*0.08=0.12 | 31.58% | 0.03 | 0.07 | 0.17 |
| Sleep quality →Anxiety symptoms →Suicide risk |
0.71*0.07=0.05 | 13.16% | 0.02 | 0.02 | 0.08 |
| Sleep quality→ Depressive symptoms →Anxiety symptoms →Suicide risk |
1.49*0.56*0.07=0.05 | 13.16% | 0.02 | 0.02 | 0.10 |
| Indirect effect | 0.22 | 57.90% | 0.03 | 0.17 | 0.28 |
4. Discussion
In this study, we used a chained mediation model to investigate the impact of sleep quality on suicide risk in COVID-19 patients. We found that anxiety and depressive symptoms play a partial chain mediating role between sleep quality and the risk of suicide. The more severe the sleep quality, the more it triggered depressive symptoms, which in turn triggered anxiety symptoms, which increased the risk of suicide.
The study found that 12.4% of COVID-19 patients suffered from sleep disorders. A survey of 5153 COVID-19 patients by Jiawen Deng et al. found that the prevalence of sleep disorders was 34% [37]. The results of the two studies were not comparable because of differences in the definition and measurement of sleep disorders. Our finding that sleep disorders were a risk factor for suicide risk is consistent with previous studies [38,39]. This study aimed to explore the internal mechanism between sleep quality and suicide risk. We drew the following conclusions: First of all, sleep quality can directly affect patients' risk of suicide. Second, sleep quality could affect suicide risk by affecting depressive symptoms. On the one hand, the results are consistent with a prospective cohort study of 38,786 participants in Sweden, which found that depression played a partial mediator role between insomnia and suicide risk in short sleep Settings [37]. On the other hand, the results differ from those of Anna Karin Hedstrom et al. who suggested that nightmares predicted depression but had no effect on suicide rates [40]. The inconsistencies may be due to differences in study subjects, measurement tools, social context (our study was conducted during a particular period of the COVID-19 pandemic), and the fact that we studied the effect of sleep disorders (including nightmares and other factors) on suicide risk, while they focused on nightmares. Thirdly, anxiety symptoms also played an incomplete mediating role between sleep quality and suicide risk, confirming previous studies [18]. Finally, this study also found that there was a chain mechanism between sleep quality and suicide risk. The worse the sleep quality, the more it triggered depressive symptoms, which in turn triggered anxiety symptoms, which increased the risk of suicide. Poor sleep quality can lead to dysfunction of the biological sleep-wake system, weaken the emotional regulation ability of individuals, and make individuals experience more negative emotions (such as depression and anxiety) [41], thus increasing the risk of suicide.
This study was the first to explore the internal mechanism of sleep quality and suicide risk in patients with COVID-19. Although it had obvious advantages, it also had certain limitations. First, in addition to considering the relationship between mood symptoms in sleep quality and suicide risk, we should also consider the role of serotonin dysfunction, sleep hopelessness, and cognitive deficits [15]. The various factors may be interrelated and their combined effects should be considered in future studies. Second, due to the difficulty in data collection of COVID-19 patients, the samples we collected were concentrated in Wuhan, China. Follow-up studies should be conducted on patients in other parts of China and abroad. Third, the self-assessment scale is used in this study. Since people have different willingness and understanding abilities to fill in the scale, plus the strong subjectivity of the self-assessment scale, some errors will be caused. Although our data were professionally evaluated by psychiatrists and tested for common methodological bias, it still reduced the accuracy of the results. Fourth, COVID-19 patients are a special group of people, and it remains to be seen whether our findings can be generally applied to other groups of people.
5. Conclusion
This study aims to explore the relationship between sleep quality and suicide risk in COVID-19 patients, as well as its influencing factors and mechanisms, so as to provide a reference for the literature. Our main conclusions are as follows: (1) Sleep quality in COVID-19 patients is closely associated with suicide risk. (2) Depression and anxiety symptoms in COVID-19 patients are chain mediators between sleep quality and suicide risk.
This study highlights the importance of not only paying attention to the physical health of COVID-19 patients, but also their mental health. This study also offers a new possibility for suicide prevention among COVID-19 patients——preventing and treating depression and anxiety with the goal of actively preventing and treating sleep disorders, thereby reducing patients' risk of suicide. Our findings enrich our understanding of how COVID-19 patients can reduce their risk of suicide during the COVID-19 pandemic and fill a gap in the research on the underlying mechanism of suicide risk in COVID-19 patients. However, more similar studies in different populations are needed to confirm this idea in the future. In addition, further research is needed to investigate the effects of serotonergic dysfunction, cognitive impairment, and other factors between sleep quality and suicide risk.
Author contribution statement
Yang Yiyue; Gu Kaiqi: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Wang Rujie; Liu Honghong; Ming Xu; Feng Yingxue; Peng Yijing; Chen Yu; Ji Yuanyuan: Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Ma Jing; Li Dongxiao; Lu Yue: Analyzed and interpreted the data.
Funding statement
This work was supported by Joint project of Chongqing Health Commission and Science and Technology Bureau [2020FYYX180].
Data availability statement
The data that has been used is confidential.
Declaration of interest’s statement
The authors declare no conflict of interest.
Acknowledgments
We express our heartfelt thanks to all the participants.
References
- 1.Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020 Jun;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. Epub 2020 Apr 15. PMID: 32304649; PMCID: PMC7159850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2020 Jun;70:124. doi: 10.1016/j.sleep.2020.04.019. Epub 2020 Apr 25. PMID: 32408252; PMCID: PMC7195057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020 Mar 6;33(2) doi: 10.1136/gpsych-2020-100213. Erratum in: Gen Psychiatr. 2020 Apr 27;33(2):e100213corr1. PMID: 32215365; PMCID: PMC7061893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hossain M.M., Tasnim S., Sultana A., Faizah F., Mazumder H., Zou L., McKyer E.L.J., Ahmed H.U., Ma P. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020 Jun 23;9:636. doi: 10.12688/f1000research.24457.1. PMID: 33093946; PMCID: PMC7549174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020 Oct 1;113(10):707–712. doi: 10.1093/qjmed/hcaa202. PMID: 32539153; PMCID: PMC7313777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deng J., Zhou F., Hou W., Silver Z., Wong C.Y., Chang O., Huang E., Zuo Q.K. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann. N. Y. Acad. Sci. 2021 Feb;1486(1):90–111. doi: 10.1111/nyas.14506. Epub 2020 Oct 2. PMID: 33009668; PMCID: PMC7675607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization Suicide. 2019. https://www.who.int/en/news-room/fact-sheets/detail/suicide
- 8.WHO Suicide prevention. 2020. https://www.who.int/mental_health/prevention/suicide/suicideprevent/en/
- 9.Hedegaard H., Curtin S.C., Warner M. Suicide rates in the United States continue to increase. NCHS Data Brief. 2018;(309):1–8. [PubMed] [Google Scholar]
- 10.Reger M.A., Stanley I.H., Joiner T.E. Suicide mortality and coronavirus disease 2019-A perfect storm? JAMA Psychiatr. 2020;77(11):1093–1094. doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- 11.Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O’Connor R.C., Pirkis J., COVID-19 Suicide Prevention Research Collaboration Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatr. 2020 Jun;7(6):468–471. doi: 10.1016/S2215-0366(20)30171-1. Epub 2020 Apr 21. PMID: 32330430; PMCID: PMC7173821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rémi J., Pollmächer T., Spiegelhalder K., Trenkwalder C., Young P. Sleep-related disorders in neurology and psychiatry. Dtsch Arztebl Int. 2019 Oct 11;116(41):681–688. doi: 10.3238/arztebl.2019.0681. PMID: 31709972; PMCID: PMC6865193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pavlova K.M., Latreille V. Sleep disorders. Am. J. Med. 2019 Mar;132(3):292–299. doi: 10.1016/j.amjmed.2018.09.021. Epub 2018 Oct 4. PMID: 30292731. [DOI] [PubMed] [Google Scholar]
- 14.Perlis M.L., Grandner M.A., Chakravorty S., Bernert R.A., Brown G.K., Thase M.E. Suicide and sleep: is it a bad thing to be awake when reason sleeps? Sleep Med. Rev. 2016 Oct;29:101–107. doi: 10.1016/j.smrv.2015.10.003. Epub 2015 Oct 19. PMID: 26706755; PMCID: PMC5070474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Woznica A.A., Carney C.E., Kuo J.R., Moss T.G. The insomnia and suicide link: toward an enhanced understanding of this relationship. Sleep Med. Rev. 2015 Aug;22:37–46. doi: 10.1016/j.smrv.2014.10.004. Epub 2014 Oct 16. PMID: 25454672. [DOI] [PubMed] [Google Scholar]
- 16.Russell K., Allan S., Beattie L., Bohan J., MacMahon K., Rasmussen S. Sleep problem, suicide and self-harm in university students: a systematic review. Sleep Med. Rev. 2019;44:58–69. doi: 10.1016/j.smrv.2018.12.008. [DOI] [PubMed] [Google Scholar]
- 17.Bishop T.M., Walsh P.G., Ashrafioun L., Lavigne J.E., Pigeon W.R. Sleep, suicide behaviors, and the protective role of sleep medicine. Sleep Med. 2020;66:264–270. doi: 10.1016/j.sleep.2019.07.016. [DOI] [PubMed] [Google Scholar]
- 18.Ward-Ciesielski E.F., Winer E.S., Drapeau C.W., Nadorff M.R. Examining components of emotion regulation in relation to sleep problems and suicide risk. J. Affect. Disord. 2018;241:41–48. doi: 10.1016/j.jad.2018.07.065. [DOI] [PubMed] [Google Scholar]
- 19.Ko Y., Moon J., Han S. Sleep duration is closely associated with suicidal ideation and suicide attempt in Korean adults: a nationwide cross-sectional study. Int. J. Environ. Res. Publ. Health. 2021;18(11):5594. doi: 10.3390/ijerph18115594. Published 2021 May 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fang H., Tu S., Sheng J., Shao A. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J. Cell Mol. Med. 2019 Apr;23(4):2324–2332. doi: 10.1111/jcmm.14170. Epub 2019 Feb 7. PMID: 30734486; PMCID: PMC6433686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bachmann S. Epidemiology of suicide and the psychiatric perspective. Int. J. Environ. Res. Publ. Health. 2018 Jul 6;15(7):1425. doi: 10.3390/ijerph15071425. PMID: 29986446; PMCID: PMC6068947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ghorbani Fatemeh, et al. The alexithymia, emotion regulation, emotion regulation difficulties, positive and negative affects, and suicidal risk in alcohol-dependent outpatients. Psychiatr. Res. 2017;252:223–230. doi: 10.1016/j.psychres.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 23.Don Richardson J., King L., St Cyr K., Shnaider P., Roth M.L., Ketcheson F., Balderson K., Elhai J.D. Depression and the relationship between sleep disturbances, nightmares, and suicidal ideation in treatment-seeking Canadian Armed Forces members and veterans. BMC Psychiatr. 2018 Jun 19;18(1):204. doi: 10.1186/s12888-018-1782-z. PMID: 29921268; PMCID: PMC6011186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ward-Ciesielski E.F., Winer E.S., Drapeau C.W., Nadorff M.R. Examining components of emotion regulation in relation to sleep problems and suicide risk. J. Affect. Disord. 2018 Dec 1;241:41–48. doi: 10.1016/j.jad.2018.07.065. Epub 2018 Jul 27. PMID: 30096591. [DOI] [PubMed] [Google Scholar]
- 25.Buysse D.J., Reynolds C.F., 3rd, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatr. Res. 1989 May;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. PMID: 2748771. [DOI] [PubMed] [Google Scholar]
- 26.Tsai P.S., Wang S.Y., Wang M.Y., Su C.T., Yang T.T., Huang C.J., Fang S.C. Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual. Life Res. 2005 Oct;14(8):1943–1952. doi: 10.1007/s11136-005-4346-x. PMID: 16155782. [DOI] [PubMed] [Google Scholar]
- 27.Ferrara P., Terzoni S., D’Agostino A., Cutcliffe J.R., Pozo Falen Y., Corigliano S.E., Bonetti L., Destrebecq A., Gambini O. Psychometric properties of the Italian version of the Nurses' global assessment of suicide risk (NGASR) scale. Riv. Psichiatr. 2019 Jan-Feb;54(1):31–36. doi: 10.1708/3104.30938. PMID: 30760935. [DOI] [PubMed] [Google Scholar]
- 28.Façanha Jorge, et al. Assessment of suicide risk: validation of the Nurses' global assessment of suicide risk Index for the Portuguese population. Arch. Psychiatr. Nurs. 2016;30(4):470–475. doi: 10.1016/j.apnu.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 29.Kozel Bernd, et al. Inter-rater reliability of the German version of the Nurses' global assessment of suicide risk scale. Int. J. Ment. Health Nurs. 2016;25(5):409–417. doi: 10.1111/inm.12193. [DOI] [PubMed] [Google Scholar]
- 30.Cutcliffe J.R., Barker P. The Nurses' global assessment of suicide risk (NGASR): developing a tool for clinical practice. J. Psychiatr. Ment. Health Nurs. 2004 Aug;11(4):393–400. doi: 10.1111/j.1365-2850.2003.00721.x. PMID: 15255912. [DOI] [PubMed] [Google Scholar]
- 31.Dunstan D.A., Scott N. Clarification of the cut-off score for Zung’s self-rating depression scale. BMC Psychiatr. 2019 Jun 11;19(1):177. doi: 10.1186/s12888-019-2161-0. PMID: 31185948; PMCID: PMC6558728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zung W.W. From art to science. The diagnosis and treatment of depression. Arch. Gen. Psychiatr. 1973 Sep;29(3):328–337. doi: 10.1001/archpsyc.1973.04200030026004. PMID: 4724142. [DOI] [PubMed] [Google Scholar]
- 33.Dunstan D.A., Scott N. Norms for Zung’s self-rating anxiety scale. BMC Psychiatr. 2020 Feb 28;20(1):90. doi: 10.1186/s12888-019-2427-6. PMID: 32111187; PMCID: PMC7048044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zung W.W. A rating instrument for anxiety disorders. Psychosomatics. 1971 Nov-Dec;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. PMID: 5172928. [DOI] [PubMed] [Google Scholar]
- 35.Schober P., Boer C., Schwarte L.A. Correlation coefficients: appropriate use and interpretation. Anesth. Analg. 2018 May;126(5):1763–1768. doi: 10.1213/ANE.0000000000002864. PMID: 29481436. [DOI] [PubMed] [Google Scholar]
- 36.Hayes A.F. An Index and test of linear moderated mediation. Multivariate Behav. Res. 2015;50(1):1–22. doi: 10.1080/00273171.2014.962683. PMID: 26609740. [DOI] [PubMed] [Google Scholar]
- 37.Anna Karin H., Hössjer O., Bellocco R., Ye W., Trolle L.Y., Åkerstedt T. Insomnia in the context of short sleep increases suicide risk. Sleep. 2021 Apr 9;44(4) doi: 10.1093/sleep/zsaa245. PMID: 33216134; PMCID: PMC8033451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pigeon W.R., Pinquart M., Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J. Clin. Psychiatry. 2012;73(9):e1160–e1167. doi: 10.4088/JCP.11r07586. PMID: 23059158. [DOI] [PubMed] [Google Scholar]
- 39.McCall W.V., Blocker J.N., D’Agostino R., Jr., Kimball J., Boggs N., Lasater B., Rosenquist P.B. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Med. 2010;11(9):822–827. doi: 10.1016/j.sleep.2010.04.004. Epub 2010 May 15. PMID: 20478741; PMCID: PMC2936685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hedström A.K., Bellocco R., Hössjer O., Ye W., Trolle Lagerros Y., Åkerstedt T. The relationship between nightmares, depression and suicide. Sleep Med. 2021;77:1–6. doi: 10.1016/j.sleep.2020.11.018. Epub 2020 Nov 20. PMID: 33285395. [DOI] [PubMed] [Google Scholar]
- 41.Palagini L., Bastien C.H., Marazziti D., Ellis J.G., Riemann D. The key role of insomnia and sleep loss in the dysregulation of multiple systems involved in mood disorders: a proposed model. J. Sleep Res. 2019;28(6) doi: 10.1111/jsr.12841. Epub 2019 Apr 10. PMID: 30968511. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.