Abstract
Background
Compared to the classic open technique, limited exposure techniques have the advantages of less scar pain, more grip and pinch strength, and earlier return to daily life. We evaluated the effectiveness and safety of our novel method of minimally invasive carpal tunnel release using a hook knife through a small transverse carpal incision.
Methods
This study included 111 carpal tunnel decompressions in 78 patients who underwent carpal tunnel release from January 2017 to December 2018. We performed carpal tunnel release using a hook knife through a small transverse incision just proximal to the wrist crease under local infiltration of lidocaine with tourniquet inflation in the upper arm. All patients were tolerable during the procedure and discharged following the procedure on the same day.
Results
At an average of 29.4 months of follow-up (range, 12–51 months), all but one patient (99%) revealed complete or near complete symptomatic recovery. The average of the symptom severity score on the Boston questionnaire was 1.31 ± 0.30 and the average of the functional status score was 1.19 ± 0.26. The final mean Quick Disabilities of the Arm, Shoulder, and Hand questionnaire (QuickDASH) score was 8.66 (range, 2–39). There was no superficial palmar arch injury or nerve injury of the palmar cutaneous branch, recurrent motor branch, or median nerve itself as a complication of the procedure. No patient showed any wound infection or wound dehiscence.
Conclusions
Our carpal tunnel release using a hook knife through a small transverse carpal incision performed by an experienced surgeon is a safe and reliable method that is expected to have the benefits of simplicity and minimal invasiveness.
Keywords: Carpal tunnel syndrome, Carpal tunnel release, Median neuropathy, Small transverse incision, Hook knife
Carpal tunnel syndrome (CTS) is by far the most common cause of compressive mononeuropathy. The prevalence rate is estimated at 3.8% of the general population.1) It is more common in patients over the age of 55 years.2) Carpal tunnel release (CTR) is a treatment of choice when conservative treatment fails.3)
The surgery for CTS is to reduce the pressure within the carpal tunnel by releasing flexor retinaculum. The classic open technique, endoscopic technique, and limited incision technique have been used as reliable procedures.1,4,5,6,7,8) Compared to the traditional open incision technique, the endoscopic and mini-open methods have the merits of less scar tenderness, more grip and pinch strength, and earlier return to activities of daily life (ADL) and work, although the hazards of injury of adjacent neurovascular structures and incomplete release are still controversial.9,10,11) The mini-open technique (limited longitudinal incision technique) has recently emerged as the most popular technique due to its simplicity.5,8) However, it still uses the incision on the carpal base, which can result in painful palmar scarring. The purpose of this study was to introduce our novel technique for CTR using a hook knife through a small transverse carpal incision and describe clinical outcomes.
METHODS
This study was approved by the Institutional Review Board (No. KC18RESI0102) and all procedures were performed with informed consent from the patients.
We performed 130 carpal tunnel decompressions through a small transverse incision just proximal to the wrist crease in 93 patients during the 2-year period between January 2017 and December 2018 at a day surgery center. A curved hemostat and a hook knife were used for flexor retinaculum release. We excluded 19 wrists in 15 patients because of the short follow-up period (less than 12 months, 8 wrists in 6 patients), lack of functional evaluation (4 wrists in 3 patients), and/or combined disease in the ipsilateral upper limb (7 wrists in 6 patients). Finally, 111 surgically managed wrists with CTS in 78 patients were reviewed retrospectively in this study (Table 1).
Table 1. Demographics of Study Population.
| Variable | Value | |
|---|---|---|
| Sex (male : female) | 11 : 67 | |
| Mean age (yr) | 58.9 (33–83) | |
| Mean tourniquet time (min) | 8.99 (4–16) | |
| Side involved (no. of patients) | ||
| Bilateral | 33 | |
| Right | 21 | |
| Left | 24 | |
| EMG grade by AAEM classification (no. of wrists) | ||
| Mild | 13 | |
| Moderate | 54 | |
| Severe | 44 | |
Values are presented as number or mean (range).
EMG: electromyography, AAEM: American Association of Electrodiagnostic Medicine.
The inclusion criterion for the participants in this study was idiopathic CTS that was confirmed by electrodiagnostic testing and that failed to respond to conservative treatment. The mean follow-up period was 30.2 months (range, 12–66 months). The mean age at surgery was 58.9 years (range, 33–83 years). There were 11 men (15 wrists) and 67 women (96 wrists). Thirty-three patients had surgeries in both wrists. Preoperative electrodiagnostic evaluation by the American Association of Electrodiagnostic Medicine classification showed mild CTS in 13 wrists, moderate CTS in 54 wrists, and severe CTS in 44 wrists.12) We performed CTR using a hook knife through a small transverse incision just proximal to the wrist crease under the local infiltration of lidocaine with tourniquet inflation in the upper arm.13) All patients were tolerable during the procedure and discharged following the procedure on the same day.
Surgical Procedure
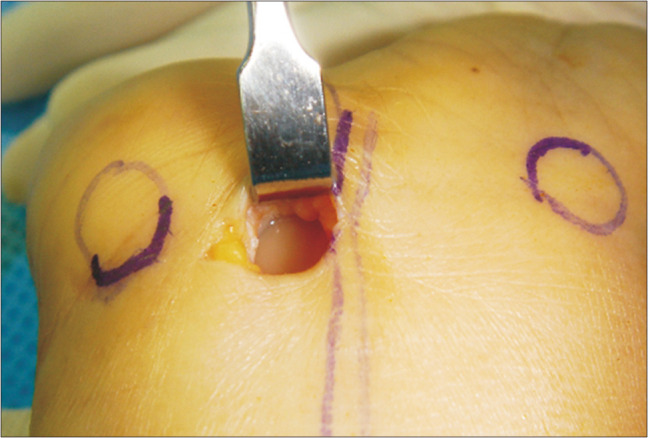
Two simple instruments, a hook knife and a curved hemostat, were used for percutaneous CTR (Fig. 1). We used the surface landmarks (Fig. 2) of the scaphoid tuberosity, pisiform, palmaris longus tendon, and the intersection between the Kaplan’s cardinal line and ring finger axis. The line connecting the proximal margin of the scaphoid tuberosity and pisiform is the proximal edge of the flexor retinaculum, and the intersection between the Kaplan’s cardinal line and ring finger axis is the distal edge of the flexor retinaculum. Carpal tunnel was accessed with the tip of a curved hemostat through the 1-cm-long transverse incision just proximal to the wrist crease between the palmaris longus and flexor carpi ulnaris tendon. The curved hemostat tip was advanced distally while keeping the contact to the undersurface of the flexor retinaculum and the radial border of the hook of hamate to avoid injury to the underlying and radial ward structures, such as recurrent motor branch of the median nerve or proper median nerve. The tip of the hemostat was palpated over the distal edge of the flexor retinaculum and marked with a marking pen as the starting point of retrograde release of the flexor retinaculum (Fig. 3). A space for hook knife passage was made by a couple of withdrawals of the hemostat with slightly widened jaws. A hook knife (Smith & Nephew Acufex instrumentation for Knee Arthroscopy: Hook, 3.0 mm Straight, Disposable) was introduced into the carpal tunnel, while similarly maintaining contact to the undersurface of flexor retinaculum, and the distal edge of the flexor retinaculum was hooked. As a starting procedure, about 1 cm of the distal edge of the flexor retinaculum was first released using back-and-pro motions of the hook knife in a longitudinal direction, which is the most difficult portion of the flexor retinaculum to release when only the distal portion of the flexor retinaculum remains unreleased. Next, the remaining main proximal part of the flexor retinaculum was released with two or three passages of the retrograde hook knife in a distal to proximal direction. Complete release of the flexor retinaculum was confirmed by the free passage of the curved hemostat tip from the distal edge of the flexor retinaculum to the proximal incision site without any resistance. After the release, the inner side of the carpal tunnel was inspected through an incision with an aid of retractors (Fig. 4). At this time, any active bleeding from vascular injury was checked after deflation of the tourniquet. The incision wound was closed with two stitches and a light compressive dressing was applied. In rare cases of absent palmaris longus tendon, we used the transverse incision between the middle finger axis and flexor carpi ulnaris tendon. The mean tourniquet time was 9 minutes (range, 4–16 minutes). Active motion of the hand and the fingers was encouraged immediately. A return to ADL was allowed from a couple of days after surgery and a return to work or sport activities was allowed from 3 to 4 weeks after surgery, based on each patient’s work demands.
Fig. 1. (A) Two simple instruments used for percutaneous carpal tunnel release. (B) The tip of the hook knife (black arrow: blade side of the hook knife) and the curved hemostat (round circle) are appropriate for retrograde release and palpating undersurface of the transverse carpal ligament. (C) A close-up photograph of the tip of the hook knife. (D) A close-up photograph of the tip of the curved hemostat.
Fig. 2. Surface landmarks: the intersection (X) between the Kaplan’s cardinal line (A) and the ring finger axis (B) is the distal edge of the flexor retinaculum. PL: palmaris longus, Ic: incision, St: scaphoid tuberosity, Ps: pisiform.

Fig. 3. Through the 1-cm-long transverse incision at just proximal to the wrist crease between the palmaris longus and flexor carpi ulnaris tendon, the carpal tunnel was accessed with the tip of the curved hemostat and the distal edge of the flexor retinaculum was confirmed.

Fig. 4. After release, the inner side of the carpal tunnel was inspected through the incision with an aid of retractors.
Outcome Evaluation
The following outcomes were evaluated: status of symptomatic recovery, symptom severity, and functional evaluation by Boston Questionnaire,14) Quick Disabilities of the Arm, Shoulder, and Hand questionnaire (QuickDASH) score,15,16) postoperative scar tenderness and pillar pain, and complications related to the surgical procedure.
The subjective symptomatic recovery from tingling sensation and night burning was divided into five categories: symptom-free (no tingling sensation or night burning at all), good (more than 90% recovery from the preoperative status), remained (less than 50% of initial symptoms remained), persistent (more than 50% of initial symptoms remained), and aggravated (occurrence of symptoms more severe than preoperative symptoms). The symptom severity was evaluated with a five-point scale: 1 (normal), 2 (slight), 3 (moderate), 4 (severe), and 5 (very severe).
The postoperative functional status was evaluated with Boston Questionnaire and QuickDASH, which is the shortened version of the Disabilities of the Arm, Shoulder and Hand score. Boston Questionnaire has two main categories: the Symptom Severity Scale (SSS) and the Functional Status Scale (FSS). The SSS has 11 questions and the FSS has 8 activities. The response to each item may range from 1 point to 5 points, and the scale is scored by calculating the mean score.14,17) The QuickDASH consists of 11-item measure of upper extremity–related disability.16) The result score ranges from 0 (no disability) to 100 (most severe disability). We checked the final Boston Questionnaire and QuickDASH scores at 1 year after operation. In the case of patients who had symptomatic comorbidities in the affected hand or wrist at the evaluation time, we rather delayed functional evaluation to the next visit, while trying to resolve comorbidities. Any recorded or experienced surgery-related complications were assessed. For patients with missing clinical and functional follow-up at 1 year after surgery, an additional phone survey was used.
RESULTS
At an average of 29.4 months follow-up, all but one patient (99%) revealed complete (symptom-free) or near complete (good) symptomatic recovery from tingling sensation or night burning (Table 2). This one 79-year-old patient had remaining tingling sensation in the hand at 26 months after surgery. The remaining symptoms were likely caused by cervical radiculopathy, but she did not want to get further evaluation before her death of other causes. Symptom severity of tingling sensation or night-burning score at the last follow-up was normal in 59 wrists, slight discomfort was noted in 51 wrists, and moderate discomfort was observed in 1 wrist. Satisfactory symptomatic recovery was obtained in all but one wrist. The score of the SSS of Boston Questionnaire (11 items) was 1.31 ± 0.30 and the score of the FSS (8 items) was 1.19 ± 0.26. We used QuickDASH (11 items) score to estimate the severity of symptoms and upper extremity function. The final mean QuickDASH score was 8.66 (range, 2–39) (Table 2).
Table 2. Summary of Outcomes.
| Subjective symptomatic recovery | Value | |
|---|---|---|
| Symptom-free | 46 (41.4) | |
| Good | 64 (57.7) | |
| Remained | 1 (0.9) | |
| Persistent | 0 | |
| Aggravated | 0 | |
| Symptom severity score | ||
| Normal | 59 (53.2) | |
| Mild | 51 (45.9) | |
| Moderate | 1 (0.9) | |
| Severe | 0 | |
| Very severe | 0 | |
| QuickDASH score | 8.66 (2–39) | |
| Boston questionnaire | ||
| Symptom score | 1.31 ± 0.30 | |
| Function score | 1.19 ± 0.26 | |
Values are presented as number (%), mean (range), or mean ± standard deviation.
QuickDASH: Quick Disabilities of the Arm, Shoulder, and Hand questionnaire.
During the first month after surgery, most patients complained of mild pain and tenderness on the carpal base, the area of flexor retinaculum released, which then gradually improved within additional couple of months. On visiting 2–4 weeks after surgery, about one third of the patients still showed mild tenderness on the surgical incision site, but there was no case with remained tenderness except in a couple of ones showing keloid characteristics at the 3-month follow-up.
Complications
There was no superficial palmar arch (SPA) injury or nerve injury of the palmar cutaneous branch, recurrent motor branch, or median nerve itself as a complication of the procedure. No patient showed any wound infection or wound dehiscence. Three wrists in 2 patients showed temporary complex regional pain syndrome symptoms, which were resolved spontaneously with emotional support, medications, and physical therapies over weeks to months. There was no recurrence. No reoperation was required.
DISCUSSION
Open carpal tunnel decompression under the direct visualization of the flexor retinaculum and surrounding structures can avoid the continuation or recurrence of symptoms resulting from incomplete release, and it can also reduce complications of major neurovascular structure injuries by easily detecting and coping with anatomical abnormalities.18,19) The complication rates of open decompression are about 1%–2% of cases, and major vascular and nerve injury is relatively rare.9,20,21) Initially, decompression using an endoscope or a mini-open technique led to more incomplete releases or neurovascular injuries compared to the conventional open incision method, with a reported rate of 1.8%–4.8% of cases.22,23,24) However, the incidence of complications is not higher than 2% when minimally invasive release is performed by an experienced surgeon.25,26,27,28,29,30)
Carpal tunnel decompression using endoscopic or mini-open methods is not suitable for conditions such as combined space occupying lesions, inflammatory diseases involving the proliferation of flexor tendon synovium, and fibrous adhesion or anatomical deformity caused by previous trauma or surgery. Such conditions should be excluded in the application of mini-open methods during preoperative evaluation.31,32,33,34)
We initially developed our procedure as an endoscope-assisted procedure for the visualization of structures in the carpal tunnel. In the case of idiopathic CTS, the only necessary procedure to decompress carpal tunnel is the release of flexor retinaculum, which is a superficial structure with anatomic consistency.35) By a couple of passages of a hook knife, we could safely release flexor retinaculum without any endoscopic assistance. Therefore, we converted our previous endoscope-assisted procedure to the present minimally invasive simple one. The advantages of our procedure include that it does not require any specific equipment, is more simple and quicker than endoscopic techniques, and is easy to perform on an outpatient base without hospitalization.
Median nerve neurolysis and flexor tenosynovectomy could have a role in symptom improvement in selective cases. Possible indications of neurolysis are (1) refractory or severe symptoms, (2) marked thenar muscle atrophy, (3) noted scarring on epineurium and around the fascicles. However, no consistent benefit from neurolysis has been obtained and it may harm the median nerve related to mechanical neurovascular injuries and additional fibrosis. So routine use of neurolysis or epineurotomy is not warranted.36) Debulking the carpal tunnel and removing any potential space occupying tissue is the rationale of flexor tenosynovectomy during CTR. On flexor retinaculum release, routine tenosynovectomy is not beneficial and associated with increased rates of infection. It can be indicated only in invasive, proliferative tenosynovitis (rhematoid arthritis, gout, tuberculosis), and markedly thickened tenosynovium from amyloid deposition in dialysis patients.36)
Recent studies using a hook knife through a mini-transverse incision have been conducted by Wang et al.37) and Ma et al.38) They used similar instruments as a bush-hook without an endoscope under local anesthesia. The results were as good as ours without any complication. However, the mean hospitalization period was over 3 days, which was longer than our outpatient procedure and the mean follow-up period was relatively short (6.8 months).
The most likely concerned structures during a mini-open release are the SPA and the variation of median nerve anatomy in the carpal tunnel such as a trans-ligamentous type motor branch and a motor branch originating from the ulnar border of median nerve.19,36,39) SPA is located about 12 mm (range, 4.0–18.0 mm) away from the distal end of the flexor retinaculum on the extension line of the longitudinal axis of the ring finger, and it is enclosed in fat tissue with the distal part of the flexor retinaculum.40) To avoid SPA injury during flexor retinaculum release, finding the exact point of hooking is important, which is guided by palpation of the tip of hemostat at the just distal margin of the flexor retinaculum on initial passage. The communicating branches between the median and ulnar nerves appear at about 67%–80% of the population, and they are often located within a few millimeters of the distal end of the flexor retinaculum or at a more proximal site than the distal end, which can be damaged during flexor retinaculum release.41,42) Another concerned structure is a bifid median nerve, which has been reported in four variation types: (1) thenar branch variations in relation to the transverse carpal ligament, (2) accessory branches at the distal carpal tunnel, (3) high division of the median nerve, and (4) accessory branches proximal to the carpal tunnel.39) To avoid injury to these structures, it is also important to advance either the tip of a hemostat or a hook knife in line with the longitudinal axis of the ring finger, while keeping in contact with the undersurface of the flexor retinaculum, and to place the tip of the hook knife accurately on the marked target point just distal to the distal edge of the flexor retinaculum.19,39) From our experience, it is likely that the superficially located flexor retinaculum can be released effectively and safely without the complications of incomplete release or major neurovascular injury. The main tips and pearls are using anatomical surface landmarks, intraoperative verification of structures, maintaining the exact location and upright orientation of instruments used within the safety zone, and maintaining the contact between the tips of instruments and the undersurface of flexor retinaculum during passage. The initial passage of a curved hemostat while the tip of it keeping in contact with the undersurface of flexor retinaculum might push any structures at risk such as communicating branches between the median and ulnar nerves, motor branch of median nerve, and bifid median nerve dorsally.
The incomplete release of flexor retinaculum could be an issue in minimal incision techniques. However, from our experience, careful retrograde passages of a curved hemostat tip after each release allowed us to assess the release status in detail, and tiny unreleased portion could be recognized in a very accurate manner. Complete release could be surely verified in our procedure.
The principal finding is that our novel method of minimally invasive CTR using a hook knife through a small transverse incision achieved similar symptomatic resolution and minimal adverse events compared to those of other mini-open techniques (endoscopic and limited longitudinal incision techniques) (Table 3).38,43,44,45) Moreover, it is simpler than endoscopic procedures and is expected to involve less postoperative pillar pain and scar tenderness as it avoids the need to make an incision on the palmar carpal base.
Table 3. Comparison with Other Mini-Open Surgeries.
| Variable | Limited longitudinal carpal tunnel release43) | Endoscopic release44) | Ultrasound-guided release45) | Mini-transverse incision with a bush hook37) | This study |
|---|---|---|---|---|---|
| Case (hand) | 134 | 97 | 61 | 85 | 111 |
| Mean follow-up period (mo) | 3 | 12 | 20 | 6.6 | 29.4 |
| Symptomatic recovery (%) | NA | NA | 93 | 92.9 | 99 |
| BCTQ-S | 1.55 | 1.8 | 1.2 | 1.3 | 1.31 |
| BCTQ-F | 1.45 | 1.7 | 1.1 | 1.3 | 1.19 |
| QuickDASH | NA | 7.5 | 2.3 | N/A | 8.66 |
| Return to work | NA | 18 day | NA | 8.5 day | 2–4 wk |
| Wound problem (%) | 4.48 | 0 | 0.16 | 0 | 0 |
| Major nerve injury | 0 | 0 | 0 | 0 | 0 |
| Structural damage (arteries, tendons) | 0 | 0 | 0 | 0 | 0 |
| CRPS | NA | 0 | NA | NA | 2.7 (temporal) |
| Recurrence | 0 | NA | 1 | NA | 0 |
NA: not applicable, BCTQ-S: Boston Carpal Tunnel Questionnaire symptom severity score, BCTQ-F: Boston Carpal Tunnel Questionnaire functional status score, QuickDASH: Quick Disabilities of the Arm, Shoulder, and Hand questionnaire, CRPS: complex regional pain syndrome.
Previous studies support that the postoperative SSS and FSS of Boston Questionnaires and QuickDASH score are correlated with outcomes of carpal tunnel decompression, such as patients’ satisfaction.17,46,47) Our study showed comparable to better functional outcomes than those in other reports on mini-open surgeries (Table 3).38,43,44,45) In other studies, the postoperative QuickDASH scores demonstrated persistent upper limb disabilities.47,48) Our excellent results in terms of QuickDASH and Boston Questionnaires scores might be related to our effort to exclude the influence of comorbidities through the selection of a better time point of evaluation and the pre-introduction of an evaluation focusing on CTS itself during self-assessment or telephone interviews.
Surgical release of carpal tunnel can be performed with or without a tourniquet. Wide awake local anesthesia and no tourniquet (WALANT) is gaining popularity. Although most patients were tolerable to a brief period of tourniquet use, some patients complained of discomfort associated with tourniquet pressure. WALENT surgery maybe a good alternative to CTR under local anesthesia with a tourniquet.49,50,51)
We found some disadvantages of this technique, one of which is the learning curve of our novel technique. We recommend sufficient preparation with cadaver workshop and awareness of the risk factors of the procedure when applying this technique. Limitation of indications is another drawback of our technique. It is not suitable for space-occupying lesions, proliferative tenosynovitis, stiff/fused wrists, or in patients with previous CTR. However, we did not face any difficulty applying our technique to idiopathic CTS or even to patients with rheumatoid arthritis or chronic renal failure as an initial procedure.
There are some limitations regarding the study design of this report. First, this is a retrospective case series study with no comparative group and no preoperative functional evaluation data, so future works comparing different surgical procedures based on prospective randomized controlled trials with pre- and postoperative evaluations should be considered. Second, we solely focused on the safety and reliability of our novel procedure in this study and did not compare the postoperative pain or the return time to ADL or work of our group to those of groups managed with other methods. Third, in some cases, we incorporated telephone interviews using questionnaires in the final functional assessment.
In conclusion, our CTR performed by an experienced surgeon using a hook knife through a small transverse carpal incision is a safe and reliable method with the expected benefits of simplicity and minimal invasiveness.
CONFLICT OF INTERESTS
No potential conflict of interest relevant to this article was reported.
ACKNOWLEDGEMENTS
This work was performed at Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea.
References
- 1.Kaleff PR, de Lima MS, Fernandes YB, Honorato DJ, Vargas AA, Honorato DC. Carpal tunnel syndrome: treatment with small transverse incision. Arq Neuropsiquiatr. 2010;68(1):93–97. doi: 10.1590/s0004-282x2010000100020. [DOI] [PubMed] [Google Scholar]
- 2.Fung BW, Tang CY, Fung BK. Does aging matter?: the efficacy of carpal tunnel release in the elderly. Arch Plast Surg. 2015;42(3):278–281. doi: 10.5999/aps.2015.42.3.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katz JN, Losina E, Amick BC, 3rd, Fossel AH, Bessette L, Keller RB. Predictors of outcomes of carpal tunnel release. Arthritis Rheum. 2001;44(5):1184–1193. doi: 10.1002/1529-0131(200105)44:5<1184::AID-ANR202>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 4.Chern TC, Kuo LC, Shao CJ, Wu TT, Wu KC, Jou IM. Ultrasonographically guided percutaneous carpal tunnel release: early clinical experiences and outcomes. Arthroscopy. 2015;31(12):2400–2410. doi: 10.1016/j.arthro.2015.06.023. [DOI] [PubMed] [Google Scholar]
- 5.Lee H, Jackson TA. Carpal tunnel release through a limited skin incision under direct visualization using a new instrument, the carposcope. Plast Reconstr Surg. 1996;98(2):313–320. doi: 10.1097/00006534-199608000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Mintalucci DJ, Leinberry CF., Jr Open versus endoscopic carpal tunnel release. Orthop Clin North Am. 2012;43(4):431–437. doi: 10.1016/j.ocl.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 7.Petrover D, Richette P. Treatment of carpal tunnel syndrome: from ultrasonography to ultrasound guided carpal tunnel release. Joint Bone Spine. 2018;85(5):545–552. doi: 10.1016/j.jbspin.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Tarallo M, Fino P, Sorvillo V, Parisi P, Scuderi N. Comparative analysis between minimal access versus traditional accesses in carpal tunnel syndrome: a perspective randomised study. J Plast Reconstr Aesthet Surg. 2014;67(2):237–243. doi: 10.1016/j.bjps.2013.10.033. [DOI] [PubMed] [Google Scholar]
- 9.Karl JW, Gancarczyk SM, Strauch RJ. Complications of carpal tunnel release. Orthop Clin North Am. 2016;47(2):425–433. doi: 10.1016/j.ocl.2015.09.015. [DOI] [PubMed] [Google Scholar]
- 10.Malhotra R, Kiran EK, Dua A, Mallinath SG, Bhan S. Endoscopic versus open carpal tunnel release: a short-term comparative study. Indian J Orthop. 2007;41(1):57–61. doi: 10.4103/0019-5413.30527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schmelzer RE, Della Rocca GJ, Caplin DA. Endoscopic carpal tunnel release: a review of 753 cases in 486 patients. Plast Reconstr Surg. 2006;117(1):177–185. doi: 10.1097/01.prs.0000194910.30455.16. [DOI] [PubMed] [Google Scholar]
- 12.Storm S, Beaver SK, Giardino N, et al. Compliance with electrodiagnostic guidelines for patients undergoing carpal tunnel release. Arch Phys Med Rehabil. 2005;86(1):8–11. doi: 10.1016/j.apmr.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 13.Chung YG, Kim YS, Kim JM, Kim DH, Choi SW, Kim SJ. Percutaneous carpal tunnel release using curved hemostat and meniscectomy hook knife. J Korean Orthop Assoc. 2004;39(7):819–824. [Google Scholar]
- 14.Levine DW, Simmons BP, Koris MJ, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75(11):1585–1592. doi: 10.2106/00004623-199311000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Hudak PL, Amadio PC, Bombardier C The Upper Extremity Collaborative Group (UECG) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected] Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 16.Beaton DE, Wright JG, Katz JN Upper Extremity Collaborative Group. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(5):1038–1046. doi: 10.2106/JBJS.D.02060. [DOI] [PubMed] [Google Scholar]
- 17.Sancmis M, Cavit A, Cakici I, Ozcanli H, Uysal H. Is Boston questionnaire an alternative to electromyography for evaluation of the surgical outcome for carpal tunnel syndrome? Turk J Phys Med Rehabil. 2020;66(3):336–342. doi: 10.5606/tftrd.2020.3136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gillig JD, White SD, Rachel JN. Acute carpal tunnel syndrome: a review of current literature. Orthop Clin North Am. 2016;47(3):599–607. doi: 10.1016/j.ocl.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 19.Henry BM, Zwinczewska H, Roy J, et al. The prevalence of anatomical variations of the median nerve in the carpal tunnel: a systematic review and meta-analysis. PLoS One. 2015;10(8):e0136477. doi: 10.1371/journal.pone.0136477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee DH, Masear VR, Meyer RD, Stevens DM, Colgin S. Endoscopic carpal tunnel release: a cadaveric study. J Hand Surg Am. 1992;17(6):1003–1008. doi: 10.1016/s0363-5023(09)91046-2. [DOI] [PubMed] [Google Scholar]
- 21.Kuschner SH, Brien WW, Johnson D, Gellman H. Complications associated with carpal tunnel release. Orthop Rev. 1991;20(4):346–352. [PubMed] [Google Scholar]
- 22.Agee JM, McCarroll HR, Jr, Tortosa RD, Berry DA, Szabo RM, Peimer CA. Endoscopic release of the carpal tunnel: a randomized prospective multicenter study. J Hand Surg Am. 1992;17(6):987–995. doi: 10.1016/s0363-5023(09)91044-9. [DOI] [PubMed] [Google Scholar]
- 23.Bozentka DJ, Osterman AL. Complications of endoscopic carpal tunnel release. Hand Clin. 1995;11(1):91–95. [PubMed] [Google Scholar]
- 24.Brown RA, Gelberman RH, Seiler JG, 3rd, et al. Carpal tunnel release: a prospective, randomized assessment of open and endoscopic methods. J Bone Joint Surg Am. 1993;75(9):1265–1275. doi: 10.2106/00004623-199309000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Benson LS, Bare AA, Nagle DJ, Harder VS, Williams CS, Visotsky JL. Complications of endoscopic and open carpal tunnel release. Arthroscopy. 2006;22(9):919–924. doi: 10.1016/j.arthro.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 26.Agee JM, Peimer CA, Pyrek JD, Walsh WE. Endoscopic carpal tunnel release: a prospective study of complications and surgical experience. J Hand Surg Am. 1995;20(2):165–172. doi: 10.1016/S0363-5023(05)80001-2. [DOI] [PubMed] [Google Scholar]
- 27.Chow JC. Endoscopic release of the carpal ligament for carpal tunnel syndrome: long-term results using the Chow technique. Arthroscopy. 1999;15(4):417–421. doi: 10.1016/s0749-8063(99)70060-5. [DOI] [PubMed] [Google Scholar]
- 28.Thoma A, Veltri K, Haines T, Duku E. A systematic review of reviews comparing the effectiveness of endoscopic and open carpal tunnel decompression. Plast Reconstr Surg. 2004;113(4):1184–1191. doi: 10.1097/01.prs.0000110202.08818.c1. [DOI] [PubMed] [Google Scholar]
- 29.Devana SK, Jensen AR, Yamaguchi KT, et al. Trends and complications in open versus endoscopic carpal tunnel release in private payer and medicare patient populations. Hand (N Y) 2019;14(4):455–461. doi: 10.1177/1558944717751196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kang HJ, Koh IH, Lee TJ, Choi YR. Endoscopic carpal tunnel release is preferred over mini-open despite similar outcome: a randomized trial. Clin Orthop Relat Res. 2013;471(5):1548–1554. doi: 10.1007/s11999-012-2666-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kendall WW. Results of treatment of severe carpal tunnel syndrome without internal neurolysis of the median nerve. J Bone Joint Surg Am. 1988;70(1):151. [PubMed] [Google Scholar]
- 32.Mackinnon SE, McCabe S, Murray JF, et al. Internal neurolysis fails to improve the results of primary carpal tunnel decompression. J Hand Surg Am. 1991;16(2):211–218. doi: 10.1016/s0363-5023(10)80099-1. [DOI] [PubMed] [Google Scholar]
- 33.Steinberg DR. Surgical release of the carpal tunnel. Hand Clin. 2002;18(2):291–298. doi: 10.1016/s0749-0712(01)00011-7. [DOI] [PubMed] [Google Scholar]
- 34.Shin EK. Endoscopic versus open carpal tunnel release. Curr Rev Musculoskelet Med. 2019;12(4):509–514. doi: 10.1007/s12178-019-09584-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Keith MW, Masear V, Chung KC, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on the treatment of carpal tunnel syndrome. J Bone Joint Surg Am. 2010;92(1):218–219. doi: 10.2106/JBJS.I.00642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mirza MA, King ET., Jr Newer techniques of carpal tunnel release. Orthop Clin North Am. 1996;27(2):355–371. [PubMed] [Google Scholar]
- 37.Wang D, Ma T, Hu Y, Zhao X, Song L. Effectiveness and safety of surgical treatment of carpal tunnel syndrome via a mini-transverse incision and a bush hook versus a mid-palmar small longitudinal incision. J Orthop Surg Res. 2022;17(1):75. doi: 10.1186/s13018-022-02967-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ma T, Wang D, Hu Y, Zhao X, Wang W, Song L. Mini-transverse incision using a novel bush-hook versus conventional open incision for treatment of carpal tunnel syndrome: a prospective study. J Orthop Surg Res. 2021;16(1):462. doi: 10.1186/s13018-021-02608-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lanz U. Anatomical variations of the median nerve in the carpal tunnel. J Hand Surg Am. 1977;2(1):44–53. doi: 10.1016/s0363-5023(77)80009-9. [DOI] [PubMed] [Google Scholar]
- 40.Omokawa S, Tanaka Y, Ryu J, Suzuki J, Kish VL. Anatomy of the ulnar artery as it relates to the transverse carpal ligament. J Hand Surg Am. 2002;27(1):101–104. doi: 10.1053/jhsu.2002.30077. [DOI] [PubMed] [Google Scholar]
- 41.Bas H, Kleinert JM. Anatomic variations in sensory innervation of the hand and digits. J Hand Surg Am. 1999;24(6):1171–1184. doi: 10.1053/jhsu.1999.1171. [DOI] [PubMed] [Google Scholar]
- 42.Meals RA, Shaner M. Variations in digital sensory patterns: a study of the ulnar nerve-median nerve palmar communicating branch. J Hand Surg Am. 1983;8(4):411–414. doi: 10.1016/s0363-5023(83)80200-7. [DOI] [PubMed] [Google Scholar]
- 43.Mack EM, Callinan NJ, Reams M, Bohn DC, Chmielewski TL. Patient-reported outcomes after open carpal tunnel release using a standard protocol with 1 hand therapy visit. J Hand Ther. 2017;30(1):58–64. doi: 10.1016/j.jht.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 44.Trumble TE, Diao E, Abrams RA, Gilbert-Anderson MM. Single-portal endoscopic carpal tunnel release compared with open release : a prospective, randomized trial. J Bone Joint Surg Am. 2002;84(7):1107–1115. doi: 10.2106/00004623-200207000-00003. [DOI] [PubMed] [Google Scholar]
- 45.Kamel SI, Freid B, Pomeranz C, Halpern EJ, Nazarian LN. Minimally invasive ultrasound-guided carpal tunnel release improves long-term clinical outcomes in carpal tunnel syndrome. AJR Am J Roentgenol. 2021;217(2):460–468. doi: 10.2214/AJR.20.24383. [DOI] [PubMed] [Google Scholar]
- 46.Ozer K, Malay S, Toker S, Chung KC. Minimal clinically important difference of carpal tunnel release in diabetic and nondiabetic patients. Plast Reconstr Surg. 2013;131(6):1279–1285. doi: 10.1097/PRS.0b013e31828bd6ec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Clement ND, Duckworth AD, Jenkins PJ, McEachan JE. Interpretation of the QuickDASH score after open carpal tunnel decompression: threshold values associated with patient satisfaction. J Hand Surg Eur Vol. 2016;41(6):624–631. doi: 10.1177/1753193415622341. [DOI] [PubMed] [Google Scholar]
- 48.Atroshi I, Lyren PE, Ornstein E, Gummesson C. The six-item CTS symptoms scale and palmar pain scale in carpal tunnel syndrome. J Hand Surg Am. 2011;36(5):788–794. doi: 10.1016/j.jhsa.2011.02.021. [DOI] [PubMed] [Google Scholar]
- 49.Castro Magtoto IJ, Alagar DL. Wide awake local anesthesia no tourniquet: a pilot study for carpal tunnel release in the philippine orthopedic center. J Hand Surg Asian Pac Vol. 2019;24(4):389–391. doi: 10.1142/S2424835519500486. [DOI] [PubMed] [Google Scholar]
- 50.Sraj S. Carpal tunnel release with wide awake local anesthesia and no tourniquet: with versus without epinephrine. Hand (N Y) 2021;16(5):592–594. doi: 10.1177/1558944719890038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sasor SE, Cook JA, Duquette SP, et al. Tourniquet use in wide-awake carpal tunnel release. Hand (N Y) 2020;15(1):59–63. doi: 10.1177/1558944718787853. [DOI] [PMC free article] [PubMed] [Google Scholar]



