Abstract
What is already known about this topic?
Tropical cyclone (TC) has a substantial and adverse impact on non-accidental mortality. However, whether heterogeneity exists when examining deaths from sub-causes and how TC impacts non-accidental mortality in the short term remain unclear.
What is added by this report?
This study found substantial associations at lag 0 between TC exposure and circulatory and respiratory mortality. TC exposures were associated with increased risks for several mortality sub-causes at lag 0 day, including ischemic heart disease, myocardial infarction, cardiac arrest, cerebrovascular disease, stroke, chronic obstructive pulmonary disease, and Parkinson’s disease.
What are the implications for public health practice?
This finding suggests an urgent need to expand the public health focus of natural disaster management to include non-accidental mortality and sub-causes.
Keywords: Tropical cyclones, Mortality risk, non-accidental diseases
Tropical cyclone (TC) is significantly and adversely associated with both accidental and non-accidental mortality (1-2). Additionally, accidental deaths from drowning, physical trauma, and electrocution during TCs have been well characterized in epidemiologic studies. However, whether heterogeneity exists in TC-associated risk for non-accidental mortality sub-causes remains unclear. Recognizing non-accidental mortality sub-causes susceptible to TCs is essential for devising mitigation. While the longer-term effect of TCs on non-accidental mortality, such as circulatory mortality, has been recognized (2), little is known about the short-term non-accidental mortality risk of TCs.
TC’s complex features generally stimulate cascading responses affecting non-accidental disease mortality (3). There is evidence that TC could substantially increase the risk of non-accidental mortality. The associated risks could result from several pathways; for example, TC can cause problems in accessing medical care (3), can damage infrastructure including public transportation and utility systems, and can increase exposure to other hazards like extreme heat.
We examined short-term associations of TC with mortality outcomes in China. China’s relatively high daily mortality enables the statistical analysis of rare health outcomes (4). Specifically, we aimed to 1) quantify TC-associated mortality risk and identify sensitive sub-causes; 2) recognize vulnerable sub-population and regions.
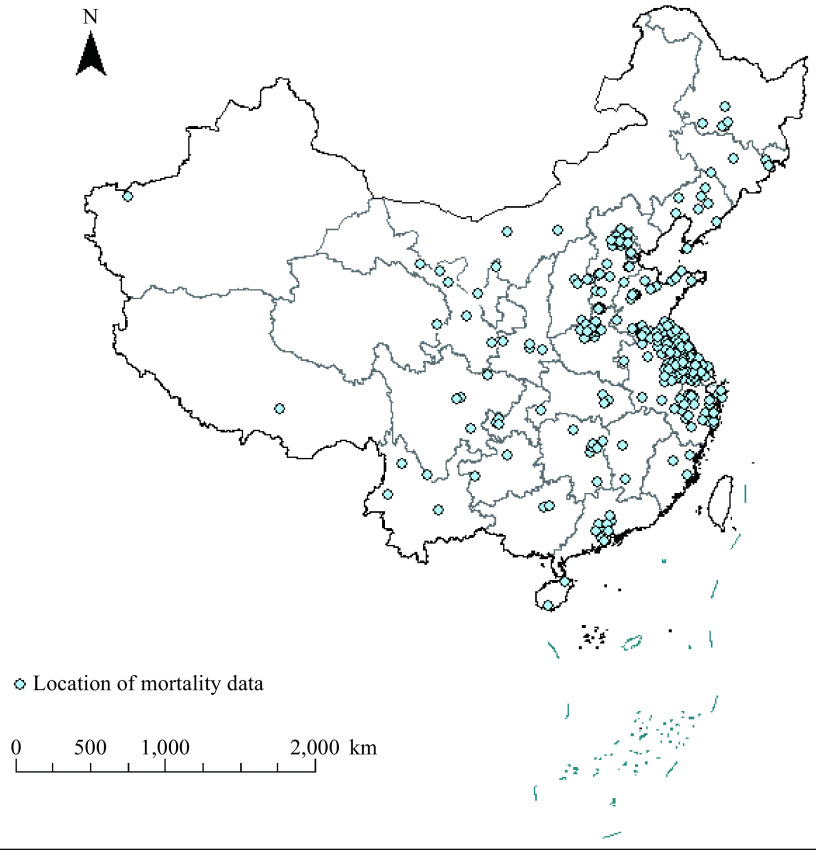
From the China Mortality Surveillance System of the National Center for Chronic and Noncommunicable Disease Control and Prevention, China CDC, we obtained mortality data, including residents’ daily mortality for 280 Chinese counties from 1 January 2013 to 31 December 2018 (Supplementary Figure S1, available in https://weekly.chinacdc.cn/). The International Classification of Diseases classified mortality data, 10th Revision (ICD–10), including all-cause (A00–Z99), non-accidental (A00–R99), accidental (V00–X56), circulatory (I00–I99), and respiratory diseases (J00–J99). We also included mortality data due to 18 sub-causes (Supplementary Table S1, available in https://weekly.chinacdc.cn/).
We obtained TCs data from the Tropical Cyclone Information Center of the China Meteorological Administration. For each TC event, we classified a county as exposed if the storm’s central track came within 60 km of the county’s geographic center (Supplementary Figure S2, available in https://weekly.chinacdc.cn/). Meteorological data were collected from the European Centre for Medium-Range Weather Forecasts.
A case-crossover study design was used to examine the county-level association between TCs and mortality. Each exposed day was matched to five unexposed days by county. We considered TC-associated risk up to six following days (1). Using the matched multi-county data, we fit generalized linear mixed-effect models (GLMMs) with a Poisson distribution to estimate TC-associated mortality risk (expressed as rate ratio, RR), adjusting for potential confounders. An unconstrained distributed lag function was used for the TC exposure variable. A county-specific random intercept was included.
We performed stratified analyses by sex, age, and the subset of counties by TC exposure frequency. We conducted sensitivity analyses to investigate the model’s robustness. All the statistical analyses were completed using R (Version 3.6.1, The R Foundation for Statistical Computing). More details are provided in the Supplementary Materials.
China was hit by forty-six TCs during 2013–2018 (Figure 1). 153 out of 280 counties were exposed to at least one TC and were analyzed. Southeast coastal areas were frequently affected (Figure 1). The total counts of all-cause mortality were 4,147 and 20,062 on TC-exposed days and selected five reference days, respectively (Table 1).
Figure 1.
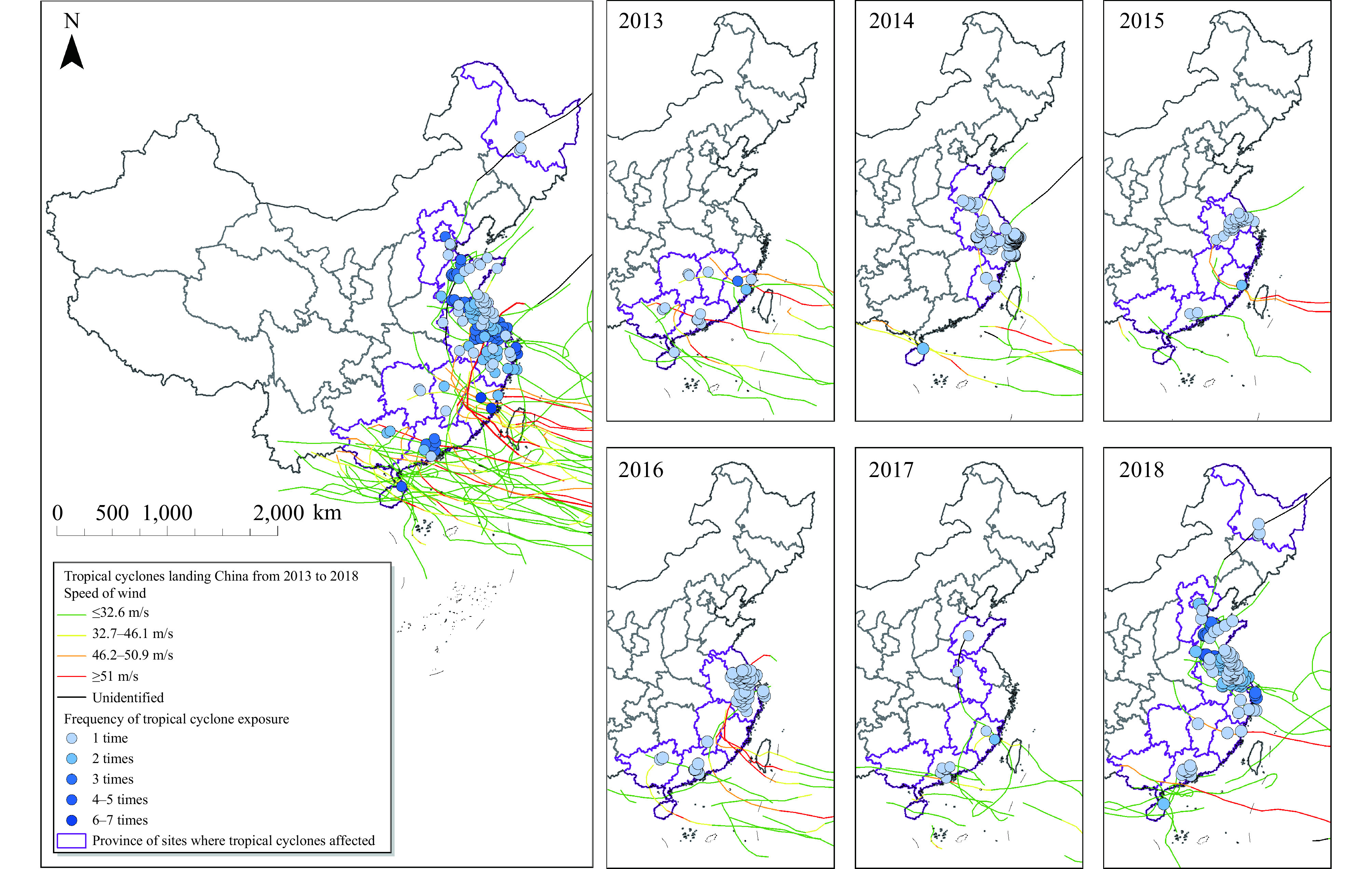
Spatial distribution of 153 eastern Chinese counties (blue circles) that were exposed to at least one tropical cyclone over the study period (2013–2018).
Note: Curves show the tracks of the 46 tropical cyclones that made landfall on China continent in this period; color of storm tracks denotes the maximum wind speed. Color of the circle in each county indicates the frequency of tropical cyclone exposures during the study period.
Table 1. Summary statistics of daily mortality on tropical cyclone exposure days and reference days (exposure∶reference=1∶5) in 153 Chinese counties (2013–2018).
| Variable | Exposure days (N=336) | Reference days (N=1,680) | |||||||
| Total | Mean±SD | Median (P25, P75) | Maximum | Total | Mean±SD | Median (P25, P75) | Maximum | ||
| Note: N=the number of TC exposure days. | |||||||||
| All-cause | 4,147 | 12.3±7.9 | 10 (7, 17) | 48 | 20,062 | 11.9±7.6 | 10 (6, 16) | 43 | |
| Cause-specific | |||||||||
| Non-accidental | 3,844 | 11.4±7.3 | 10 (6, 15) | 40 | 18,472 | 11.0±7.0 | 10 (6, 15) | 39 | |
| Accidental | 303 | 0.9±1.2 | 1 (0, 1) | 8 | 1,590 | 1.0±1.2 | 1 (0, 1) | 7 | |
| Circulatory disease | 1,648 | 4.9±3.9 | 4 (2, 7) | 26 | 7,557 | 4.5±3.4 | 4 (2, 6) | 24 | |
| Respiratory disease | 449 | 1.3±1.5 | 1 (0, 2) | 8 | 2,323 | 1.4±1.5 | 1 (0, 2) | 8 | |
| Sex | |||||||||
| Male | 2,405 | 7.2±4.9 | 6 (4, 10) | 28 | 11,471 | 6.8±4.6 | 6 (3, 10) | 28 | |
| Female | 1,742 | 5.2±3.7 | 4 (2, 7) | 20 | 8,591 | 5.1±3.8 | 4 (2, 7) | 23 | |
| Age (years) | |||||||||
| 0–64 | 964 | 2.9±2.4 | 2 (1, 4) | 17 | 4,826 | 2.9±2.3 | 2 (1, 4) | 14 | |
| 65–74 | 802 | 2.4±2.1 | 2 (1, 3) | 11 | 3,907 | 2.3±2.0 | 2 (1, 3) | 12 | |
| >75 | 2,381 | 7.1±5.0 | 6 (3, 10) | 24 | 11,329 | 6.7±4.8 | 6 (3, 9) | 29 | |
Compared with reference days, TC-associated RRs for all-cause and non-accidental mortality were 1.07 [95% confidence interval (CI): 1.03–1.10] and 1.08 (95% CI: 1.04–1.11) at lag 0 day (the exposure day), respectively. Although accidental mortality did not increase on the TC-exposed day, it did by the third day following exposure (RR=1.18, 95% CI: 1.06–1.30). We found significant associations at lag 0 between TC exposure and circulatory mortality (RR=1.12, 95% CI: 1.06–1.18) and respiratory mortality (1.12, 95% CI: 1.01–1.23) (Supplementary Table S2, Supplementary Figure S3, available in https://weekly.chinacdc.cn/). Effect estimates from sensitivity analyses were consistent with the primary ones (Supplementary Table S3, available in https://weekly.chinacdc.cn/).
TC was associated with increased risks for several mortality sub-causes at lag 0 day, including ischemic heart disease, myocardial infarction (MI), cardiac arrest, cerebrovascular disease, stroke, chronic obstructive pulmonary disease (COPD), and Parkinson’s disease; for example, MI mortality risk increased by 15% (Figure 2). The estimated RRs remained elevated for mortality due to cardiac arrest, cerebrovascular disease, and stroke in the subsequent 2–3 days. We also observed appreciable lagged effects for lower respiratory infection, asthma,influenza, and pneumonia (Figure 2).
Figure 2.
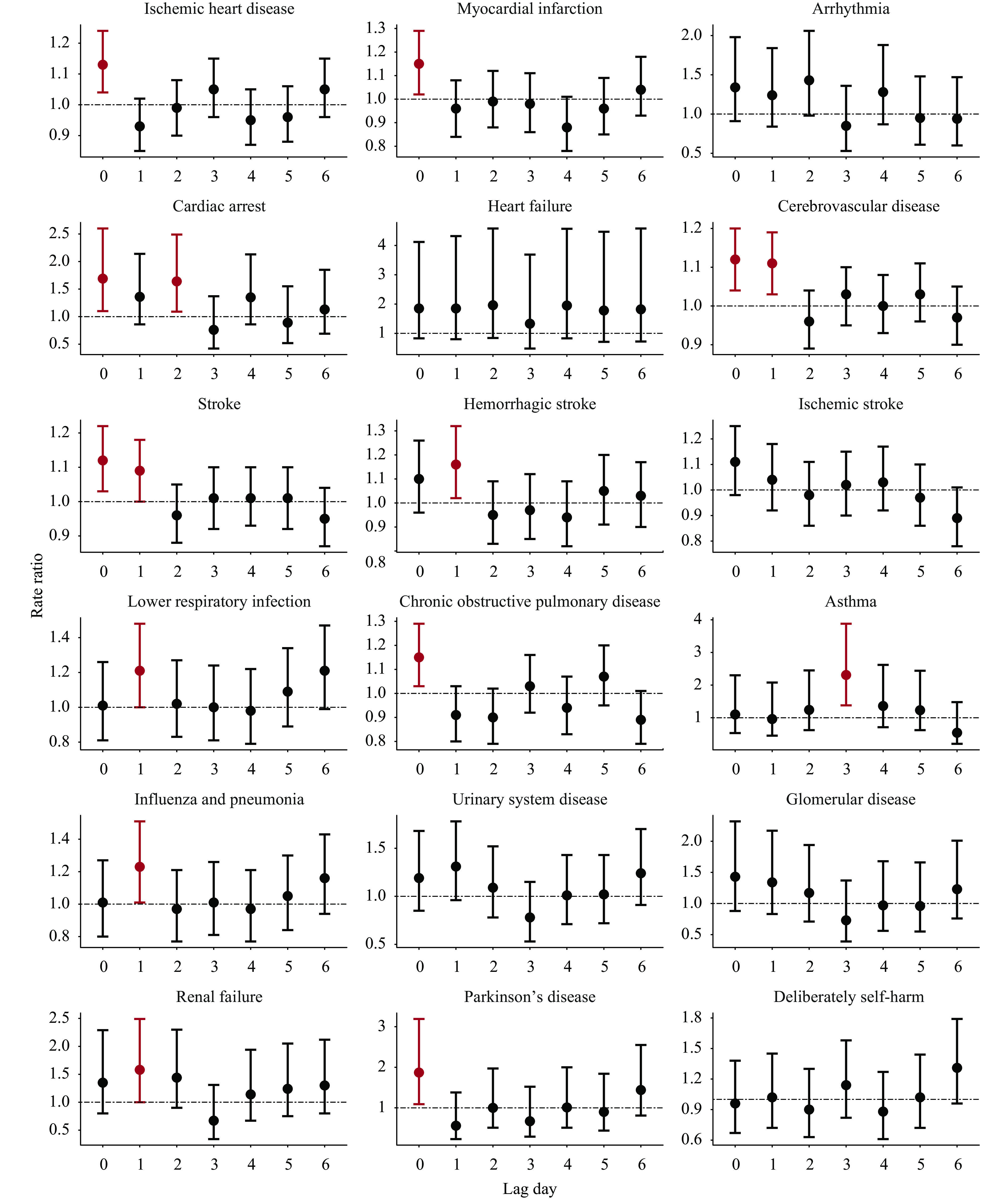
Lag-specific rate ratio of sub-cause mortality associated with tropical cyclone exposure, on average across all exposed counties.
Males had a higher TC-associated risk for accidental and circulatory mortality than females but lower for respiratory mortality (Supplementary Figure S4, available in https://weekly.chinacdc.cn/). The difference in risk estimates by sex was not statistically significant. Residents aged 65–74 years presented a significantly lower respiratory mortality risk than those younger than 65 and older than 74 years. We observed a higher cardiorespiratory mortality risk in counties that experienced ≥3 TC events than in those experiencing 1–2 events and lower accidental mortality risks, though the difference was not significant (Supplementary Figure S4).
DISCUSSION
To the best of our knowledge, this is the first multi-center, multi-event study examining the short-term associations of TCs with many mortality outcomes in China. Among residents in 153 Chinese counties during 2013–2018, TCs were associated with elevated risks for several non-accidental mortality, especially circulatory and respiratory sub-causes. TCs were also associated with renal failure and Parkinson’s disease mortality. Our findings suggest an urgent need to expand the public health focus of natural disaster management to include non-accidental mortality outcomes.
Two similar Chinese studies existed but on a much smaller scale. One study reported a RR of 1.05 (95% CI: 0.96–1.16) for circulatory mortality associated with TCs in Guangzhou (2008–2011) (5). The other indicated elevated mortality risk during the two years following Typhoon Morakot (2009) in Taiwan (6). These reported longer-term TC-associated mortality risks were consistent with western studies (2). However, TC-associated circulatory mortality risk was much more substantial in the short term, with a 12% increase on the TC-exposed day in this study and a 1.2% increase in the following month from a previous study (2). Our findings complement the limited knowledge by providing evidence of TC’s short-term circulatory mortality risk, focusing on a time scale relevant to rapid public health response.
Mortality due to several circulatory diseases markedly increased in association with TC. TC immediately impacted cardiac arrest and MI mortality. It is known that TC may have a longer-term effect on MI; for example, 30-day MI mortality increased by 31% during Hurricane Sandy in New Jersey (7). We found MI mortality increased by 15% on TC-exposed days, suggesting a short-term risk of TC. Psychological stress after TC exposure may help explain the elevated risk associated with TC. TC occurrences typically generate psychological stress for affected individuals, provoking physiological responses. Among these responses, the hypothalamic-pituitary-adrenocortical and autonomic nervous system responses primarily contribute to cardiovascular disease development (8). Stress may also trigger stroke, a possible explanation of TC-associated increased risk of cerebrovascular disease and stroke mortality (9). Our findings suggest an urgent need to expand the public health focus of TC management to include circulatory sub-causes.
Accidental deaths (like drowning and being hit by falling tree limbs) often occur during TC (10). We only observed increased accidental mortality risk at lag day 3 (RR=1.18). During TCs, fatal injuries or drowning often occur in heavily impacted areas where strong winds and severe rainfalls may block roads and damage communications. Therefore, the rescue teams might not arrive in time, and the deceased had to be determined a few days later. It may also be possible that it took several days to find and identify all accidental deaths caused by TCs. Furthermore, though insignificant, TC-associated accidental mortality risk was higher in males than females, which is consistent with previous findings. For example, the ratio of males to females was 1.87/1.00 among victims of Hurricane Sandy. Occupation type by sex might be a reason for this result, as men dominate some jobs (like bus drivers and rescue team members) with higher health risks than others during TCs.
TC was also associated with an increased mortality risk due to lower respiratory infections, COPD, influenza and pneumonia, renal failure, and urinary system diseases. While the underlying mechanism is not adequately understood, TCs likely affect mortality through damaging infrastructure (3). First, TCs can damage transportation and communication infrastructure, which may impede people from seeking medical treatment. Beyond that, utilities and power outages play a crucial role in increasing the risk of death for patients relying on electrically powered medical technologies like ventilators and oxygen, especially for those at hospitals who are particularly vulnerable to the impact of power outage (3).
Parkinson’s disease mortality significantly increased on TC days but not in the next few days. External shocks and movement difficulties may partly explain the elevated mortality risks. According to a previous study on TCs’ effects on Parkinson’s disease in American older adults, the hospitalization rate for Parkinson’s disease increased in the week after TCs (2). It can be possible that patients with severe Parkinson’s disease might be extremely fragile to the impacts of tropical cyclones and more likely to die than those who had less severe conditions and could be hospitalized in the following days.
Our study has some limitations. First, exposure misclassification may exist. Previous research has evaluated TC-associated health risks in America using a multi-hazard-based exposure assessment (1–2). Distance from a storm track effectively captured some signal of TC’s health risk (1). Future research is needed to develop alternative methods of TC exposure assessment in China. Second, confounding residuals may be possible. We used a matched design by county; county-level confounding factors that were time-invariant could be controlled at the study design stage. However, some county-level confounders (such as socioeconomic characteristics) could be time-variant. So confounding residuals may exist in the results (2).
Our findings offer practical implications. Firstly, it is crucial to improve TC’s early warning system, which should be able to alarm vulnerable individuals to take proper measures. The authorities should provide adequate medical resources for affected residents, especially people with TC-associated sensitive diseases. Also, the public should be well educated about TC’s health risk.
Conflicts of interest
No conflicts of interest.
SUPPLEMENTARY MATERIAL
Tropical Cyclone (TC)
A tropical cyclone is an intense circular storm that originates over warm tropical oceans which often threatens human health and has devastating impacts on society (1).
Mortality Data
This study obtained mortality data from the China Mortality Surveillance System of the National Center for Chronic and Noncommunicable Disease Control and Prevention, China CDC. The data include daily mortality counts for residents living in 280 Chinese counties (locations shown in Supplementary Figure S1) from January 1, 2013 to December 31, 2018. The International Classification of Diseases classified mortality data, 10th Revision (ICD–10), including all-cause (ICD–10, A00–R99), non-accidental (ICD–10, A00–R99), accidental (ICD–10, V00–X56), circulatory (ICD–10, I00–I99), and respiratory (ICD–10, J00–J99). We also included mortality data due to 18 sub-causes in our analysis, with details in Supplementary Table S1. Residential population data was obtained from the Sixth National Census in 2010.
Figure S1.
Locations of 280 counties with mortality data.
TC Data
TC exposure data was collected from the Tropical Cyclone Information Center of China Meteorological Administration (http://tcdata.typhoon.org.cn/). This database includes the track and maximum wind speed of TCs that made landfall in China. For each TC event during the study period, we classified a county as exposed if the storm’s central track came within 60 km of the county’s geographic center (2). When a county was assessed as exposed, the exposure date was determined as the date the storm came closest to that county.
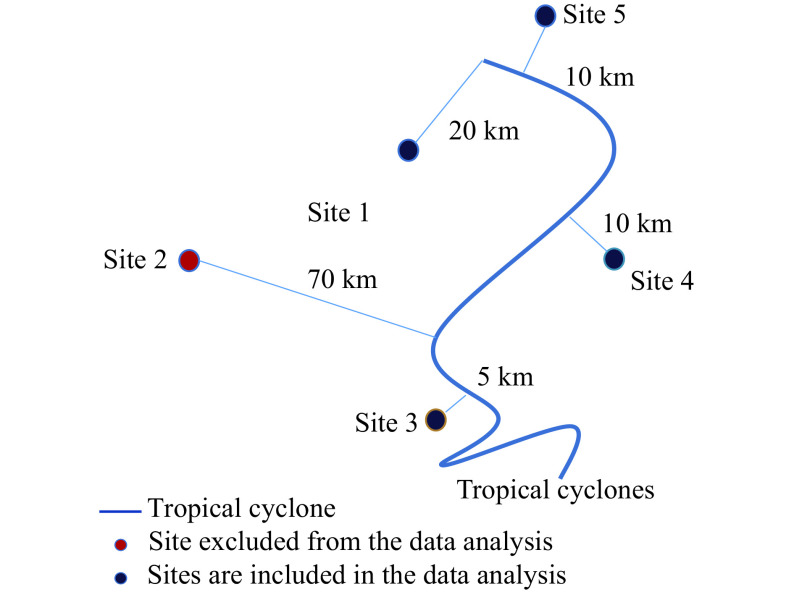
TC Exposure
For each tropical cyclone during the study period, we classified a county as exposed if the storm’s central track came within 60 km of the county’s geographic center. When a county was classified as exposed, the exposure date was determined as the date the storm came closest to that county. An example denoting the definition of tropical cyclone-exposed counties is shown in Supplementary Figure S2.
Figure S2.
An example showing the definition of tropical cyclone exposed counties.
In Supplementary Figure S2, the curve shows the track of a tropical cyclone. Circles show five counties (i.e., sites 1, 2, 3, 4, 5) along the storm track. The lines connecting the circles and the curve show the distances between each county’s geographic center and the tropical cyclone’s track. The distances for sites 1, 3, 4, and 5 were less than 60 km; these sites were included in the data analysis. Site 2 was excluded from the data analysis, as the distance (70 km) was greater than 60 km.
Meteorological Data
Meteorological data (mean temperature and mean relative humidity data) were collected from the European Centre for Medium-Range Weather Forecasts (ECMWF, https://apps.ecmwf.int/datasets/). For each county, we aggregated the hourly data from ECMFW to generate a daily measure for our study period.
Statistical Model
We used a case-crossover study design to examine county-level associations between TC exposure and mortality risk. For counties exposed to at least one TC event, we matched each exposed day to five unexposed days randomly selected from a candidate pool of days which were: 1) in the same county; 2) in a different year; 3) the same day of the year as the TC exposure day; and 4) not within a seven-day window of another TC exposure day. Since TCs typically occur in seasons when ambient temperature is high, we also excluded as potential controls days with daily maximum temperature exceeding 35 ℃ (the threshold of defining a high temperature day based on China Meteorological Administration) to reduce possible confounding from extreme heat. We considered TC-associated risk up to six days following the TC exposure day (in full, a seven-day period we refer to as the “exposure period”).
Following an approach that we previously developed, with the matched multi-county data, we fit generalized linear mixed-effect models (GLMMs) with a Poisson distribution to estimate the mortality risk associated with TC exposure. We fit the model separately for each mortality outcome. We adjusted for potential confounding effects due to long-term time trend and weather conditions. The model equation for the GLMMs is:
 |
1 |
where  is the daily mortality count for county c on day t;
is the daily mortality count for county c on day t;  is the total residential population of county c based on the 2010 census data, which is included as an offset term;
is the total residential population of county c based on the 2010 census data, which is included as an offset term;  is the model intercept;
is the model intercept;  is a random intercept for county c, included to account for within-county correlations;
is a random intercept for county c, included to account for within-county correlations;  is unconstrained distributed lag function for TC exposure
is unconstrained distributed lag function for TC exposure  .
.  is a vector of length 7 of coefficients from day t to lag day l;
is a vector of length 7 of coefficients from day t to lag day l;  is an indicator variable denoting whether a given day at lag day l from day t is within TC exposure or within the matched reference period in county c;
is an indicator variable denoting whether a given day at lag day l from day t is within TC exposure or within the matched reference period in county c;  is year for day t for county c to control for a linear long-term trend in mortality rates over study years;
is year for day t for county c to control for a linear long-term trend in mortality rates over study years;  is the linear coefficients for year;
is the linear coefficients for year;  is the daily mean temperature for county c on day t;
is the daily mean temperature for county c on day t;  is the coefficient for mean temperature;
is the coefficient for mean temperature;  is the daily average relative humidity for county c on day t;
is the daily average relative humidity for county c on day t;  is the coefficient for relative humidity. We calculated rate ratio (RR) of tropical cyclone exposure on mortality outcomes at each lag day based on the estimated
is the coefficient for relative humidity. We calculated rate ratio (RR) of tropical cyclone exposure on mortality outcomes at each lag day based on the estimated  .
.
Stratified Analysis
We performed secondary analyses by fitting the same model for 1) the population stratified by sex (male and female) and age (≤64, 65–74, and ≥75 years old); and 2) TC exposure frequency (counties experienced 1–2 TC events and ≥3 events) during our study period (3). The Z test was used to compare the two effect estimates derived from subgroup analysis:
 |
2 |
Where  and
and  were coefficient estimates from subgroups (e.g., males and females);
were coefficient estimates from subgroups (e.g., males and females);  and
and  were the corresponding standard error for coefficients. P values for the Z test were reported and shown with the results.
were the corresponding standard error for coefficients. P values for the Z test were reported and shown with the results.
Sensitivity Analysis
We conducted sensitivity analyses to investigate the robustness of our results. First, instead of selecting five reference periods for each exposed period, we tested using three and six referent periods. Second, to account for potential confounding effects due to spatial variation, we replaced the random effect for county with a fixed effect by including an indicator variable of county in a generalized linear model. All the statistical analyses were completed using R (Version 3.6.1, The Foundation for Statistical Computing). Several R packages were used in statistical analyses, including “dlnm”, “dplyr”, “MASS”, “purrr”, “lme4” and “splines”.
Table S1. Descriptive analysis of cause-specific mortality on case and control days.
| Disease (ICD code) | Case | Control | |||||||||||
| Mean | SD | q25 | q50 | q75 | Max | Mean | SD | q25 | q50 | q75 | Max | ||
| Note: The ratio of case to control is 1 to 5. In the analysis, tropical events (case) and reference days (control) are 336 days and 1,680 days from 2013 to 2018, respectively. Minority of daily mortality for both case and control is 0. | |||||||||||||
| All (A00-Z99) | 12.34 | 7.87 | 7 | 10 | 17 | 48 | 11.94 | 7.58 | 6 | 10 | 16 | 43 | |
| Non-accidental (A00-R99) | 11.44 | 7.26 | 6 | 10 | 15 | 40 | 11.00 | 6.96 | 6 | 10 | 15 | 39 | |
| Accidental (V00-X58) | 0.90 | 1.23 | 0 | 1 | 1 | 8 | 0.95 | 1.21 | 0 | 1 | 1 | 7 | |
| Circulatory (I00-I99) | 4.90 | 3.87 | 2 | 4 | 7 | 26 | 4.50 | 3.39 | 2 | 4 | 6 | 24 | |
| Hypertensive heart disease (I10-I15) | 0.35 | 0.83 | 0 | 0 | 0 | 10 | 0.38 | 0.75 | 0 | 0 | 1 | 6 | |
| Ischemic heart disease (I20-I25) | 1.76 | 1.89 | 0 | 1 | 3 | 13 | 1.59 | 1.76 | 0 | 1 | 2 | 11 | |
| Myocardial infarction (I21-I23) | 1.02 | 1.44 | 0 | 1 | 2 | 12 | 0.93 | 1.33 | 0 | 0 | 1 | 10 | |
| Arrhythmia (I44-I49) | 0.08 | 0.30 | 0 | 0 | 0 | 2 | 0.06 | 0.24 | 0 | 0 | 0 | 2 | |
| Cardiac arrest (I46) | 0.07 | 0.28 | 0 | 0 | 0 | 2 | 0.04 | 0.21 | 0 | 0 | 0 | 2 | |
| Heart failure (I50) | 0.02 | 0.20 | 0 | 0 | 0 | 3 | 0.01 | 0.11 | 0 | 0 | 0 | 1 | |
| Cerebrovascular disease (I60-I69) | 2.56 | 2.42 | 1 | 2 | 4 | 16 | 2.33 | 2.14 | 1 | 2 | 3 | 15 | |
| Stroke (I60-I64) | 1.83 | 2.12 | 0 | 1 | 3 | 16 | 1.76 | 1.83 | 0 | 1 | 3 | 14 | |
| Hemorrhagic stroke (I60-I61) | 0.73 | 1.11 | 0 | 0 | 1 | 7 | 0.75 | 1.00 | 0 | 0 | 1 | 8 | |
| Ischemic stroke (I63) | 0.92 | 1.23 | 0 | 1 | 1 | 9 | 0.84 | 1.09 | 0 | 1 | 1 | 8 | |
| Respiratory (J00-J99) | 1.34 | 1.52 | 0 | 1 | 2 | 8 | 1.38 | 1.51 | 0 | 1 | 2 | 8 | |
| Lower respiratory infection (J12-J18&J20-J22) | 0.26 | 0.58 | 0 | 0 | 0 | 4 | 0.29 | 0.66 | 0 | 0 | 0 | 5 | |
| Chronic obstructive pulmonary disease (J41-J44) | 0.98 | 1.37 | 0 | 1 | 1 | 8 | 0.98 | 1.32 | 0 | 1 | 1 | 7 | |
| Asthma (J45-J46) | 0.02 | 0.15 | 0 | 0 | 0 | 1 | 0.03 | 0.19 | 0 | 0 | 0 | 2 | |
| Influenza and pneumonia (J09-J18) | 0.23 | 0.52 | 0 | 0 | 0 | 3 | 0.27 | 0.61 | 0 | 0 | 0 | 5 | |
| Digestive (K00-K93) | 0.24 | 0.55 | 0 | 0 | 0 | 4 | 0.21 | 0.47 | 0 | 0 | 0 | 2 | |
| Nervous (G00-G99) | 0.19 | 0.48 | 0 | 0 | 0 | 3 | 0.20 | 0.49 | 0 | 0 | 0 | 5 | |
| Parkinson's disease (G20-G21) | 0.05 | 0.21 | 0 | 0 | 0 | 1 | 0.02 | 0.15 | 0 | 0 | 0 | 1 | |
| Genitourinary (N00-N99) | 0.12 | 0.35 | 0 | 0 | 0 | 2 | 0.11 | 0.34 | 0 | 0 | 0 | 3 | |
| Urinary system disease (N00-N39) | 0.11 | 0.34 | 0 | 0 | 0 | 2 | 0.10 | 0.33 | 0 | 0 | 0 | 2 | |
| Glomerular disease (N00-N08) | 0.05 | 0.23 | 0 | 0 | 0 | 1 | 0.05 | 0.22 | 0 | 0 | 0 | 2 | |
| Renal failure (N17-N19) | 0.05 | 0.23 | 0 | 0 | 0 | 2 | 0.04 | 0.21 | 0 | 0 | 0 | 2 | |
| Deliberately self-harm (X60-X84) | 0.10 | 0.31 | 0 | 0 | 0 | 2 | 0.10 | 0.34 | 0 | 0 | 0 | 2 | |
Table S2. Numerical results from main model.
| Cause of death | Rate ratio (95% confidence interval) | ||||||
|
Lag 0
(Exposure day) |
Lag 1 | Lag 2 | Lag 3 | Lag 4 | Lag 5 | Lag 6 | |
| All-cause | 1.07 (1.03, 1.10) |
1.01 (0.98, 1.05) |
0.99 (0.96, 1.02) |
1.02 (0.99, 1.05) |
0.95 (0.92, 0.98) |
1.03 (1.00, 1.07) |
0.99 (0.96, 1.02) |
| Non-accidental | 1.08 (1.04, 1.11) |
1.02 (0.99, 1.06) |
0.98 (0.95, 1.01) |
1.01 (0.97, 1.04) |
0.95 (0.92, 0.99) |
1.03 (1.00, 1.07) |
0.99 (0.96, 1.03) |
| Accidental | 0.94 (0.83, 1.06) |
0.95 (0.85, 1.07) |
1.07 (0.96, 1.19) |
1.18 (1.06, 1.3) |
0.92 (0.82, 1.04) |
1.06 (0.95, 1.18) |
0.97 (0.87, 1.09) |
| Circulatory | 1.12 (1.06, 1.18) |
1.05 (0.99, 1.10) |
0.98 (0.93, 1.04) |
1.01 (0.96, 1.06) |
0.99 (0.94, 1.04) |
1.01 (0.96, 1.07) |
1.00 (0.95, 1.05) |
| Respiratory | 1.12 (1.01, 1.23) |
0.98 (0.89, 1.09) |
0.95 (0.86, 1.05) |
1.05 (0.95, 1.16) |
0.96 (0.86, 1.06) |
1.06 (0.96, 1.17) |
0.97 (0.87, 1.07) |
| Digestive | 1.13 (0.90, 1.41) |
1.03 (0.82, 1.30) |
0.98 (0.78, 1.25) |
1.06 (0.85, 1.34) |
0.82 (0.64, 1.07) |
0.98 (0.78, 1.25) |
1.14 (0.91, 1.42) |
| Nervous | 1.08 (0.83, 1.40) |
0.87 (0.66, 1.15) |
1.08 (0.84, 1.38) |
0.86 (0.66, 1.14) |
0.68 (0.5, 0.93) |
0.95 (0.73, 1.24) |
1.13 (0.89, 1.45) |
| Genitourinary | 1.22 (0.88, 1.70) |
1.28 (0.94, 1.74) |
1.07 (0.77, 1.49) |
0.77 (0.53, 1.14) |
0.96 (0.68, 1.37) |
1.06 (0.76, 1.48) |
1.22 (0.90, 1.66) |
| Hypertensive heart disease | 1.01 (0.84, 1.23) |
1.11 (0.94, 1.33) |
1.02 (0.85, 1.22) |
0.79 (0.65, 0.97) |
1.02 (0.85, 1.22) |
0.98 (0.81, 1.18) |
0.84 (0.69, 1.02) |
| Ischemic heart disease | 1.13 (1.04, 1.24) |
0.93 (0.85, 1.02) |
0.99 (0.9, 1.08) |
1.05 (0.96, 1.15) |
0.95 (0.87, 1.05) |
0.96 (0.88, 1.06) |
1.05 (0.96, 1.15) |
| Myocardial infarction | 1.15 (1.02, 1.29) |
0.96 (0.84, 1.08) |
0.99 (0.88, 1.12) |
0.98 (0.86, 1.11) |
0.88 (0.78, 1.01) |
0.96 (0.85, 1.09) |
1.04 (0.93, 1.18) |
| Arrhythmia | 1.34 (0.91, 1.98) |
1.24 (0.84, 1.84) |
1.43 (0.98, 2.06) |
0.85 (0.53, 1.36) |
1.28 (0.87, 1.88) |
0.95 (0.61, 1.48) |
0.94 (0.60, 1.47) |
| Cardiac arrest | 1.69 (1.10, 2.60) |
1.36 (0.86, 2.14) |
1.64 (1.09, 2.49) |
0.76 (0.42, 1.37) |
1.35 (0.86, 2.13) |
0.89 (0.52, 1.55) |
1.13 (0.69, 1.85) |
| Heart failure | 1.85 (0.83, 4.12) |
1.85 (0.80, 4.32) |
1.96 (0.84, 4.58) |
1.33 (0.48, 3.69) |
1.95 (0.83, 4.57) |
1.78 (0.71, 4.47) |
1.82 (0.72, 4.58) |
| Cerebrovascular disease | 1.12 (1.04, 1.20) |
1.11 (1.03, 1.19) |
0.96 (0.89, 1.04) |
1.03 (0.95, 1.10) |
1.00 (0.93, 1.08) |
1.03 (0.96, 1.11) |
0.97 (0.90, 1.05) |
| Stroke | 1.12 (1.03, 1.22) |
1.09 (1.00, 1.18) |
0.96 (0.88, 1.05) |
1.01 (0.92, 1.10) |
1.01 (0.93, 1.10) |
1.01 (0.92, 1.10) |
0.95 (0.87, 1.04) |
| Hemorrhagic stroke | 1.1 (0.96, 1.26) |
1.16 (1.02, 1.32) |
0.95 (0.83, 1.09) |
0.97 (0.85, 1.12) |
0.94 (0.82, 1.09) |
1.05 (0.91, 1.20) |
1.03 (0.90, 1.17) |
| Ischemic stroke | 1.11 (0.98, 1.25) |
1.04 (0.92, 1.18) |
0.98 (0.86, 1.11) |
1.02 (0.90, 1.15) |
1.03 (0.92, 1.17) |
0.97 (0.86, 1.10) |
0.89 (0.78, 1.01) |
| Lower respiratory infection | 1.01 (0.81, 1.26) |
1.21 (1.00, 1.48) |
1.02 (0.83, 1.27) |
1.00 (0.81, 1.24) |
0.98 (0.79, 1.22) |
1.09 (0.89, 1.34) |
1.21 (0.99, 1.47) |
| Chronic obstructive pulmonary disease (COPD) |
1.15 (1.03, 1.29) |
0.91 (0.80, 1.03) |
0.90 (0.79, 1.02) |
1.03 (0.92, 1.16) |
0.94 (0.83, 1.07) |
1.07 (0.95, 1.20) |
0.89 (0.79, 1.01) |
| Asthma | 1.10 (0.53, 2.30) |
0.96 (0.45, 2.08) |
1.24 (0.62, 2.45) |
2.31 (1.38, 3.88) |
1.36 (0.71, 2.62) |
1.23 (0.62, 2.44) |
0.54 (0.20, 1.48) |
| Influenza and pneumonia | 1.01 (0.80, 1.27) |
1.23 (1.01, 1.51) |
0.97 (0.77, 1.21) |
1.01 (0.81, 1.26) |
0.97 (0.77, 1.21) |
1.05 (0.84, 1.30) |
1.16 (0.94, 1.43) |
| Parkinson's disease | 1.87 (1.09, 3.19) |
0.56 (0.23, 1.38) |
1.00 (0.51, 1.97) |
0.67 (0.29, 1.52) |
1.01 (0.51, 2.00) |
0.90 (0.44, 1.84) |
1.44 (0.81, 2.55) |
| Urinary system disease | 1.19 (0.85, 1.68) |
1.31 (0.96, 1.78) |
1.09 (0.78, 1.52) |
0.78 (0.53, 1.15) |
1.01 (0.71, 1.43) |
1.02 (0.72, 1.43) |
1.24 (0.91, 1.70) |
| Glomerular disease | 1.43 (0.88, 2.32) |
1.34 (0.83, 2.17) |
1.17 (0.71, 1.94) |
0.73 (0.39, 1.37) |
0.97 (0.56, 1.68) |
0.96 (0.55, 1.66) |
1.23 (0.76, 2.01) |
| Renal failure | 1.35 (0.80, 2.29) |
1.58 (1.00, 2.49) |
1.44 (0.90, 2.30) |
0.67 (0.34, 1.31) |
1.14 (0.67, 1.94) |
1.24 (0.75, 2.05) |
1.30 (0.80, 2.12) |
| Deliberately self-harm | 0.96 (0.67, 1.38) |
1.02 (0.72, 1.45) |
0.90 (0.63, 1.30) |
1.14 (0.82, 1.58) |
0.88 (0.61, 1.27) |
1.02 (0.72, 1.44) |
1.31 (0.96, 1.79) |
Table S3. Results from sensitive analysis.
| Model | Cause of death | Rate ratio (95% confidence interval) | ||||||
|
Lag 0
(Exposure day) |
Lag 1 | Lag 2 | Lag 3 | Lag 4 | Lag 5 | Lag 6 | ||
| Notes: Model 1 and Model 2 have the same specifications as the main model, using three and six reference periods, respectively; Model 3 is a generalized linear model (GLM) to control year, population, temperature, relative humidity, and a fixed effect of county (rather than the random effect of county used in the main model). | ||||||||
| Model 1 (3 reference periods) |
All-cause | 1.07 (1.04, 1.11) |
1.02 (0.99, 1.05) |
0.99 (0.96, 1.03) |
1.03 (0.99, 1.06) |
0.96 (0.93, 0.99) |
1.04 (1.01, 1.07) |
1.00 (0.97, 1.03) |
| Non-accidental | 1.09 (1.05, 1.13) |
1.03 (0.99, 1.07) |
0.99 (0.95, 1.02) |
1.01 (0.98, 1.05) |
0.96 (0.93, 1.00) |
1.04 (1.00, 1.08) |
1.00 (0.97, 1.04) |
|
| Accidental | 0.90 (0.79, 1.01) |
0.93 (0.83, 1.05) |
1.05 (0.94, 1.17) |
1.15 (1.04, 1.28) |
0.90 (0.8, 1.02) |
1.04 (0.93, 1.16) |
0.96 (0.85, 1.07) |
|
| Circulatory disease | 1.14 (1.08, 1.20) |
1.06 (1.00, 1.12) |
0.99 (0.94, 1.05) |
1.02 (0.97, 1.08) |
1.00 (0.95, 1.06) |
1.02 (0.97, 1.08) |
1.01 (0.96, 1.07) |
|
| Respiratory disease | 1.13 (1.02, 1.24) |
0.99 (0.89, 1.09) |
0.95 (0.86, 1.05) |
1.05 (0.95, 1.16) |
0.96 (0.86, 1.06) |
1.06 (0.96, 1.18) |
0.97 (0.87, 1.08) |
|
| Model 2 (6 reference periods) |
All-cause | 1.06 (1.03, 1.10) |
1.02 (0.98, 1.05) |
0.99 (0.96, 1.02) |
1.02 (0.99, 1.06) |
0.95 (0.92, 0.99) |
1.04 (1.00, 1.07) |
1.00 (0.96, 1.03) |
| Non-accidental | 1.08 (1.04, 1.11) |
1.02 (0.99, 1.06) |
0.99 (0.95, 1.02) |
1.01 (0.98, 1.05) |
0.96 (0.93, 0.99) |
1.04 (1.00, 1.07) |
1.00 (0.97, 1.03) |
|
| Accidental | 0.90 (0.80, 1.02) |
0.94 (0.83, 1.05) |
1.05 (0.95, 1.17) |
1.16 (1.04, 1.28) |
0.91 (0.81, 1.02) |
1.04 (0.94, 1.16) |
0.96 (0.86, 1.07) |
|
| Circulatory disease | 1.13 (1.08, 1.19) |
1.06 (1.01, 1.12) |
1.00 (0.94, 1.05) |
1.02 (0.97, 1.08) |
1.00 (0.95, 1.06) |
1.02 (0.97, 1.08) |
1.01 (0.96, 1.07) |
|
| Respiratory disease | 1.11 (1.01, 1.22) |
0.97 (0.88, 1.08) |
0.94 (0.85, 1.04) |
1.04 (0.94, 1.15) |
0.95 (0.85, 1.05) |
1.05 (0.95, 1.16) |
0.96 (0.87, 1.06) |
|
| Model 3 (GLM with county) |
All-cause | 1.08 (1.03, 1.13) |
1.02 (0.98, 1.07) |
0.99 (0.95, 1.04) |
1.03 (0.98, 1.08) |
0.96 (0.92, 1.01) |
1.04 (1.00, 1.10) |
1.01 (0.96, 1.06) |
| Non-accidental | 1.09 (1.04, 1.15) |
1.03 (0.98, 1.08) |
0.98 (0.94, 1.03) |
1.01 (0.96, 1.06) |
0.97 (0.92, 1.02) |
1.04 (0.99, 1.10) |
1.01 (0.96, 1.06) |
|
| Accidental | 0.92 (0.81, 1.05) |
0.95 (0.84, 1.08) |
1.08 (0.96, 1.22) |
1.19 (1.06, 1.33) |
0.91 (0.80, 1.04) |
1.06 (0.94, 1.20) |
0.98 (0.86, 1.11) |
|
| Circulatory disease | 1.16 (1.09, 1.24) |
1.06 (0.99, 1.13) |
0.98 (0.91, 1.05) |
1.01 (0.95, 1.08) |
1.01 (0.94, 1.08) |
1.02 (0.95, 1.09) |
1.00 (0.94, 1.07) |
|
| Respiratory disease | 1.13 (1.01, 1.26) |
1.01 (0.90, 1.14) |
0.97 (0.86, 1.1) |
1.07 (0.95, 1.20) |
0.99 (0.88, 1.11) |
1.10 (0.98, 1.23) |
1.01 (0.90, 1.14) |
|
Figure S3.
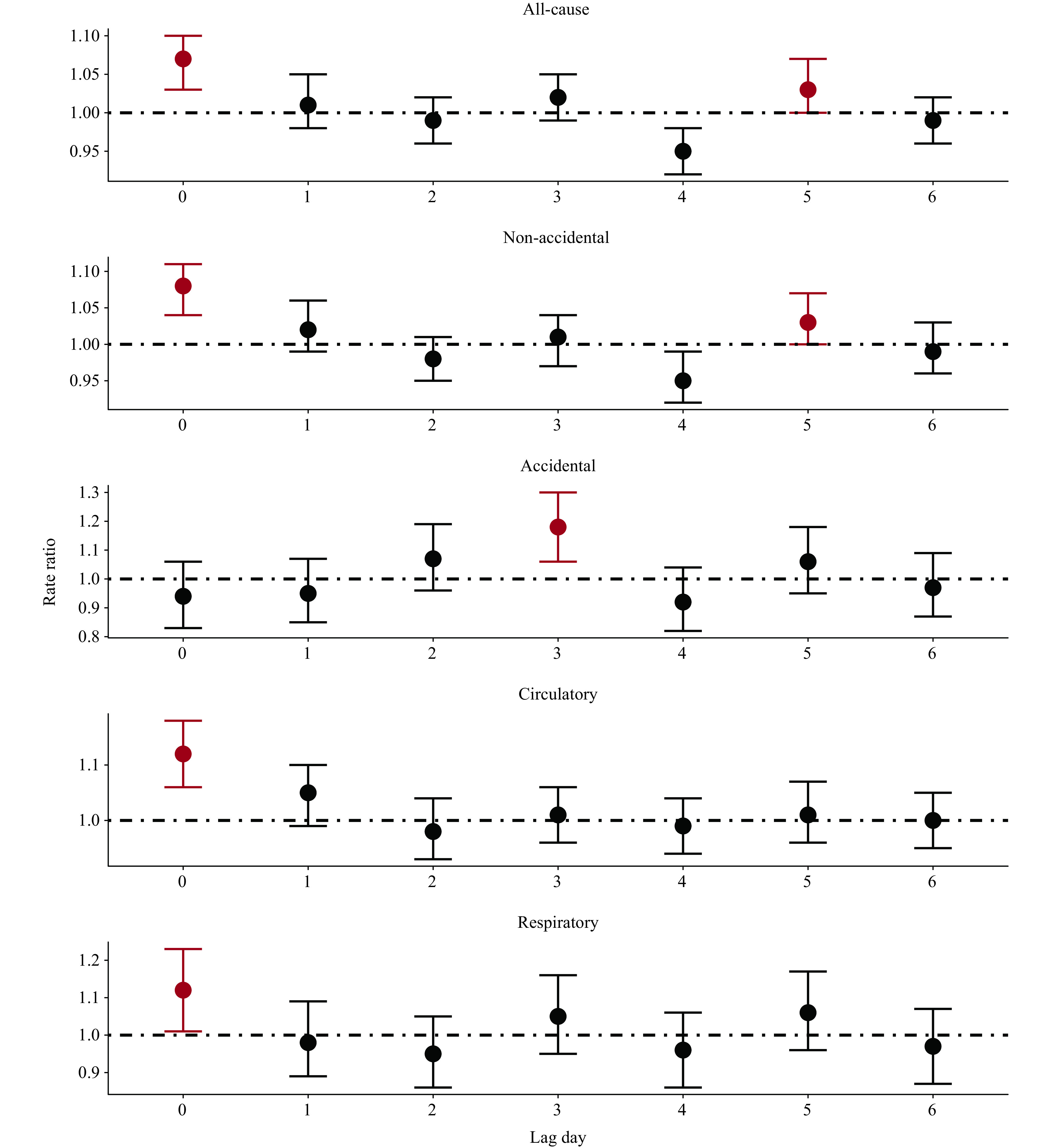
Lag-specific rate ratio for all-cause and broad cause mortality associated with tropical cyclone exposure, on average across tropical cyclone-exposed counties.
Figure S4.
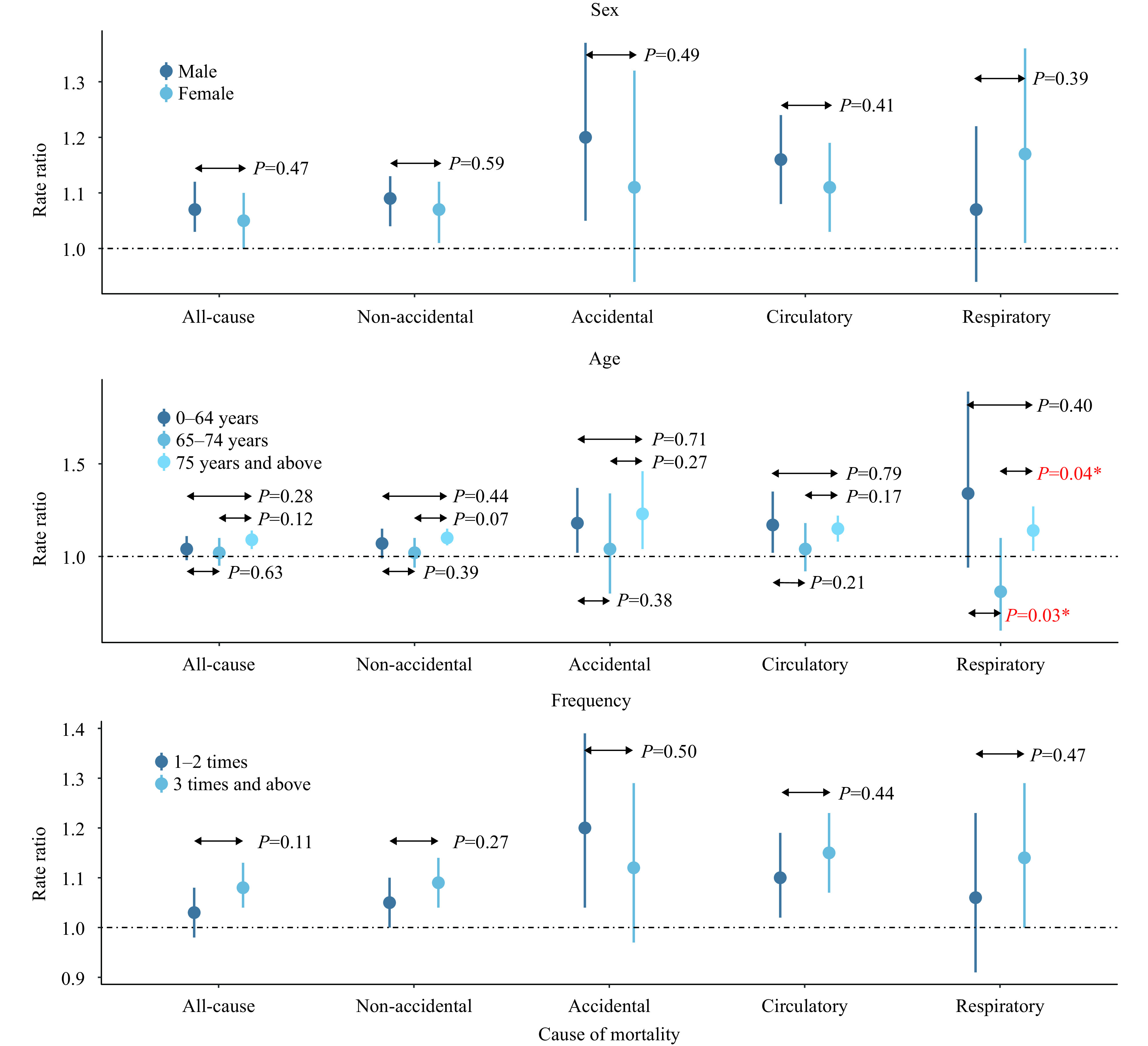
Rate ratio (RR) of mortality associated with tropical cyclone exposure stratified by sex, age, and tropical cyclones’ frequency in the county over the study period. RRs were estimated at lag 3 for accidental mortality and lag 0 for other mortality outcomes.
REFERENCES
Shultz JM, Russell J, Espinel Z. Epidemiology of tropical cyclones: the dynamics of disaster, disease, and development. Epidemiol Rev 2005.27(1):21 − 35. https://doi.org/10.1093/epirev/mxi011.
Grabich SC, Horney J, Konrad C, Lobdell DT. Measuring the storm: methods of quantifying hurricane exposure with pregnancy outcomes. Nat Hazards Rev 2016;17(1):06015002. http://dx.doi.org/10.1061/(ASCE)NH.1527-6996.0000204.
Sun ZY, Chen C, Yan ML, Shi WY, Wang JN, Ban J, et al. Heat wave characteristics, mortality and effect modification by temperature zones: a time-series study in 130 counties of China. Int J Epidemiol 2020;49(6):1813 − 22. http://dx.doi.org/10.1093/ije/dyaa104.
Funding Statement
This project has received funding from the National Natural Science Foundation of China (92043301)
References
- 1.Yan ML, Wilson A, Dominici F, Wang Y, Al-Hamdan M, Crosson W, et al Tropical cyclone exposures and risks of emergency medicare hospital admission for cardiorespiratory diseases in 175 urban United States counties, 1999-2010. Epidemiology. 2021;32(3):315–26. doi: 10.1097/EDE.0000000000001337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parks RM, Benavides J, Anderson GB, Nethery RC, Navas-Acien A, Dominici F, et al Association of tropical cyclones with county-level mortality in the US. JAMA. 2022;327(10):946–55. doi: 10.1001/jama.2022.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lane K, Charles-Guzman K, Wheeler K, Abid Z, Graber N, Matte T Health effects of coastal storms and flooding in urban areas: a review and vulnerability assessment. J Environ Public Health. 2013;2013:913064. doi: 10.1155/2013/913064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ban J, Xu DD, Mike ZH, Sun QH, Chen C, Wang WT, et al The effect of high temperature on cause-specific mortality: A multi-county analysis in China. Environ Int. 2017;106:19–26. doi: 10.1016/j.Envint.2017.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang X, Gou HM, Kang RH, Wang W, Ma W Effects of typhoon on mortality and burden of disease of residents in Yuexiu district of Guangzhou from 2008 to 2011. J Environ Health. 2015;32(4):315–8. doi: 10.16241/J.Cnki.1001-5914.2015.04.010. [DOI] [Google Scholar]
- 6.Shih HI, Chao YZ, Huang YT, Tu YT, Sung TC, Wang JD, et al Increased medical visits and mortality among adults with cardiovascular diseases in severely affected areas after Typhoon Morakot. Int J Environ Res Public Health. 2020;17(18):6531. doi: 10.3390/ijerph17186531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swerdel JN, Janevic TM, Cosgrove NM, Kostis JB, Myocardial Infarction Data Acquisition System (MIDAS 24) Study Group The effect of hurricane sandy on cardiovascular events in New Jersey. J Am Heart Assoc. 2014;3(6):e001354. doi: 10.1161/JAHA.114.001354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kivimäki M, Steptoe A Effects of stress on the development and progression of cardiovascular disease. Nat Rev Cardiol, 2018;15(4):215–29. doi: 10.1038/nrcardio.2017.189. [DOI] [PubMed] [Google Scholar]
- 9.Smyth A, O’Donnell M, Hankey GJ, Rangarajan S, Lopez-Jaramillo P, Xavier D, et al Anger or emotional upset and heavy physical exertion as triggers of stroke: the INTERSTROKE study. Eur Heart J. 2022;43(3):202–9. doi: 10.1093/eurheartj/ehab738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rappaport EN, Blanchard BW Fatalities in the United States indirectly associated with Atlantic tropical cyclones. Bull Am Meteor Soc. 2016;97(7):1139–48. doi: 10.1175/BAMS-D-15-00042.1. [DOI] [Google Scholar]