Abstract
What is already known about this topic?
Cancer patients are more vulnerable and have higher mortality rates from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) than the general population; however, coverage for booster doses of the coronavirus disease 2019 (COVID-19) vaccine was low among cancer patients in China.
What is added by this report?
Overall, 32.0% and 56.4% of cancer patients from four Provincial Level Administrative Divisions (PLADs) expressed hesitancy toward the first and second booster doses, respectively. Factors negatively associated with hesitancy to receive booster doses included positive attitudes, perceived support, and higher exposure to COVID-19 vaccination information. Conversely, postvaccination fatigue was positively associated with vaccine hesitancy.
What are the implications for public health practice?
Improved COVID-19 vaccination coverage is needed to promote health for cancer patients.
Keywords: Cancer Patients, COVID-19 Vaccine, Booster Doses, Vaccine Hesitancy
Recent concerns have been raised about waning protection against coronavirus disease 2019 (COVID-19) after completing the two-dose primary vaccination series (1). Cancer patients have been found to have higher mortality from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) than the general population, but only 52% [95% confidence interval (CI): 35%–70%] of this population were willing to accept the COVID-19 vaccine (2). To date, no study has evaluated the hesitancy of cancer patients to receive the booster doses of the COVID-19 vaccines in China. A multicenter cross-sectional study was conducted in four Chinese cities. Medical staff approached all cancer inpatients aged 18 years or above, and 893 patients completed a face-to-face interview. This study was based on a sub-sample of 525 participants who completed the primary vaccination series. Logistic regression models were fitted to identify the factors associated with vaccine hesitancy. Among the participants, 32.0% and 56.4% were hesitant to receive the first and second COVID-19 vaccine booster doses. Positive attitudes, perceived support from significant others and perceived behavioral control related to the booster dose, higher exposure to COVID-19 vaccination information, and thoughtful consideration about the veracity of COVID-19-specific information were associated with lower hesitancy to receive the booster doses. Vaccination fatigue was positively associated with vaccine hesitancy. Cancer patients in China were more hesitant than the general population to receive COVID-19 vaccine booster doses. Health sectors should advocate the benefits of vaccination with COVID-19 booster doses to cancer patients, which would improve the coverage and promote health.
In Chinese mainland, the National Guideline recommends a third dose of COVID-19 vaccine as a booster for cancer patients six months after completing the two-dose primary vaccination series (3). Many cancer patients may be hesitant to receive the booster doses. A previous study identified some factors associated with hesitancy to complete the primary vaccination series among cancer patients (4). Vaccine fatigue, which is defined as people’s inaction towards vaccine instruction due to perceived burden and burnout (5), could be a factor in this hesitancy. Thoughtful consideration of the veracity of the information may mitigate the negative impact of misinformation related to COVID-19 and COVID-19 vaccination. This study examined the effects of sociodemographics, cancer-related characteristics, perceptions, vaccine fatigue, and media influences associated with vaccine hesitancy.
This was a multicenter, cross-sectional study of cancer patients in four Chinese cities from four Provincial Level Administrative Divisions (PLADs) (Changzhi, Hohhot, Urumqi, and Shenzhen) conducted between May and June 2022. All study sites adhered to the national guideline and recommended a third dose of the COVID-19 vaccine as a booster for cancer patients (3).
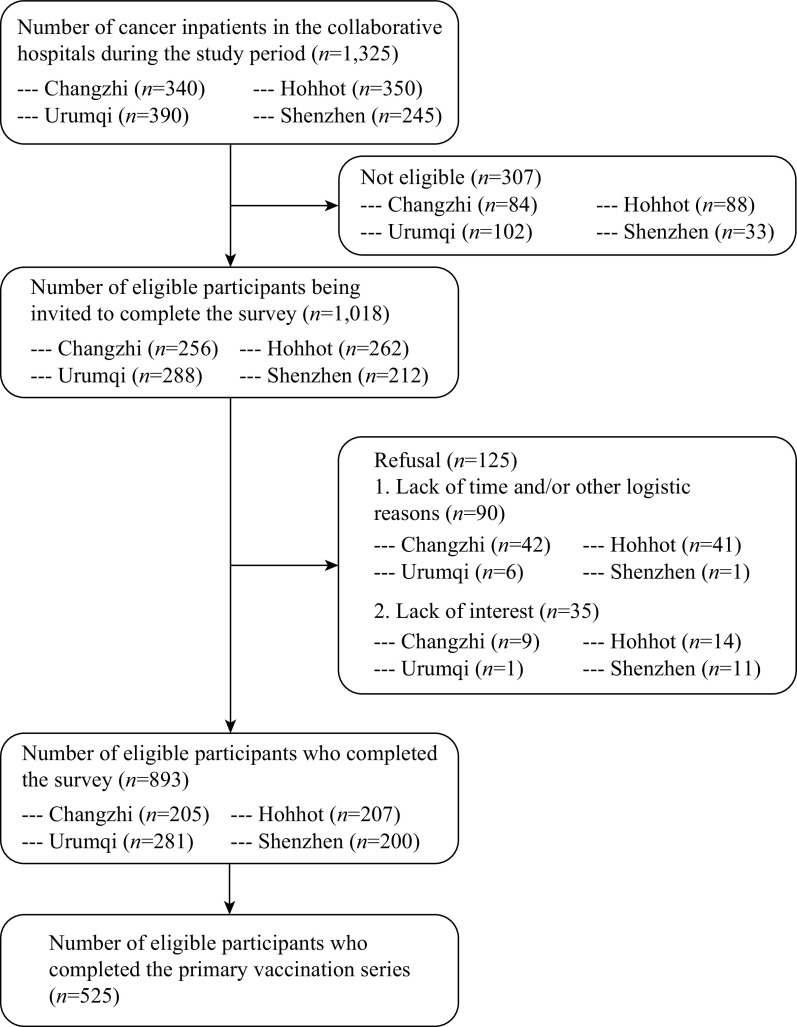
Participants of the original study were included if they met the following criteria: 1) cancer patients who were hospitalized in the four participating hospitals during the study period, 2) aged 18 years or above, and 3) willing to provide written informed consent to complete the survey. Exclusion criteria included: 1) critical illness or intensive care unit admission, 2) a diagnosis of lymphoma, leukemia, mental illness, or taking medication for mental illness, or 3) dementia or inability to communicate effectively with the investigators. Medical staff from the selected hospitals approached all cancer inpatients, screened their eligibility, briefed them about the study, and invited them to participate in a face-to-face interview. No incentives were provided. The data collection procedures are shown in Figure 1. Ethics approval was obtained from the Institutional Review Board of Changzhi Medical College (reference: RT2022027).
Figure 1.
The data collection procedures of this study.
Participants reported sociodemographic information, and medical staff extracted cancer-related characteristics and presence of other chronic diseases from medical records. We first asked whether participants had received the first booster dose, and for those who had not, we further asked their likelihood of receiving it (response categories: 1=very unlikely, 2=unlikely, 3=neutral, 4=likely, and 5=very likely). Since China has not yet provided the second booster dose, we asked all participants their likelihood of receiving it if it is available (response categories: 1=very unlikely, 2=unlikely, 3=neutral, 4=likely, and 5=very likely). Vaccine hesitancy was defined as “very unlikely,” “unlikely,” or “neutral.” We used the Theory of Planned Behavior (TPB) to measure perceptions related to COVID-19 vaccine booster dose (6). We used the 3-item Positive Attitude Scale and modified the 5-item Negative Attitude Scale, both of which were validated in older Chinese adults (7). In addition, perceived subjective norm and perceived behavioral control were measured by two single-item scales validated in the Chinese population (8). Vaccine fatigue was measured by a single item (“You are tired of receiving COVID-19 vaccination over and over again”). We adopted four items validated in the Chinese population to measure media influences related to COVID-19 and COVID-19 vaccination (8). A validated single item assessed the frequency of thoughtful consideration about the veracity of COVID-19 specific information. The Cronbach’s alpha of the Positive Attitude Scale, Negative Attitude Scale, and the Media Exposure Scale was 0.90, 0.84, and 0.90, respectively.
Frequency distributions of all variables were measured, and the mean and standard deviation (SD) of the scale and item scores were presented. Reliability tests were used to obtain the Cronbach's alpha for the scales. Hesitancy to receive the first and second COVID-19 vaccine booster doses were used as dependent variables, and univariate logistic regression models were used to examine significant associations between background characteristics and dependent variables. Perceptions, vaccine fatigue, and media influence were used as independent variables, and associations between one of these independent variables and the dependent variables with adjustments for significant background characteristics were assessed using adjusted odds ratios (AORs) and their corresponding CIs. There were no missing values for the participants who completed the primary vaccination series. Data analysis was conducted using IBM SPSS Statistics (version 26.0, IBM Corp., Armonk, NY, USA) and P<0.05 was considered statistically significant.
A total of 893 participants provided written informed consent and completed the interview. Of the 525 eligible cancer patients who completed primary COVID-19 vaccination, 41.8% were over 60 years old and 55.8% were male. The most common type of cancer was lung cancer (20.8%), followed by colorectal cancer (18.5%), and 6.7% had metastatic cancers. Most participants (93.0%) were under cancer treatment. In addition to cancers, 21.5% had at least one other chronic disease (Table 1). Of the participants, 49.9% had received the first COVID-19 booster dose. Of those who had not yet received the first booster dose, 36.1% intended to get vaccinated. The prevalence of hesitancy to receive the first and the second booster doses was 32.0% and 56.4%, respectively (Supplementary Table S1, available in https://weekly.chinacdc.cn/).
Table 1. Background characteristics of 525 participants who completed the primary COVID-19 vaccination series.
| Background characteristic | No. of participants | Percentage (%) |
| Sociodemographic characteristics | ||
| Age group in years | ||
| 18–45 | 87 | 16.6 |
| 46–60 | 219 | 41.7 |
| 61–75 | 194 | 37.0 |
| >75 | 25 | 4.8 |
| Gender | ||
| Male | 293 | 55.8 |
| Female | 232 | 44.2 |
| Ethnicity | ||
| Han majority | 426 | 81.1 |
| Other ethnic minority groups | 99 | 18.9 |
| Education level | ||
| Junior high school and below | 338 | 64.4 |
| High school education or equivalent | 102 | 19.4 |
| College-level and above | 85 | 16.2 |
| Relationship status | ||
| Single/divorced/widowed | 39 | 7.4 |
| Married | 486 | 92.6 |
| Employment status | ||
| Full-time | 138 | 26.3 |
| Part-time/self-employed/unemployed/retired/students | 387 | 73.7 |
| Characteristics of cancer | ||
| Type of cancer | ||
| Lung cancer | 109 | 20.8 |
| Gastric cancer | 66 | 12.6 |
| Liver cancer | 15 | 2.9 |
| Breast cancer | 30 | 5.7 |
| Colorectal cancer | 97 | 18.5 |
| Esophageal cancer | 26 | 5.0 |
| Ovarian cancer | 43 | 8.2 |
| Other types of cancer | 139 | 26.5 |
| Metastatic cancers | ||
| No | 490 | 93.3 |
| Yes | 35 | 6.7 |
| Current treatment for cancer | ||
| Untreated patients | 17 | 3.2 |
| Chemotherapy only | 338 | 64.4 |
| Radiotherapy only | 89 | 17.0 |
| Immunotherapy only | 12 | 2.3 |
| Chemotherapy and radiotherapy | 34 | 6.5 |
| Immunotherapy and chemotherapy/radiotherapy | 15 | 2.9 |
| Treatment completion | 20 | 3.8 |
| Presence of other chronic diseases | ||
| Diabetes mellitus | 30 | 5.7 |
| Hypertension and/or hyperlipidemia | 73 | 13.9 |
| Chronic cardiovascular diseases | 13 | 2.5 |
| Chronic respiratory diseases | 4 | 0.8 |
| Chronic liver and/or kidney diseases | 7 | 1.3 |
| Other chronic diseases | 15 | 2.9 |
In the univariate analysis, cancer patients who were ethnic minorities had lower hesitancy to receive the first COVID-19 vaccine booster dose (Supplementary Table S2, available in https://weekly.chinacdc.cn/). After adjusting for significant background characteristics listed in Supplementary Table S2, positive attitudes toward the booster dose (AOR: 0.83 & 0.66), perceived higher support from significant others (AOR: 0.55 & 0.40), perceived higher behavioral control to take up the booster dose (AOR: 0.51 & 0.25), higher exposure to information related to COVID-19 vaccination (AOR: 0.94 & 0.90), and thoughtful consideration about the veracity of COVID-19-specific information (AOR: 0.65 & 0.52) were associated with lower hesitancy to receive the first and the second booster doses (Table 2). Vaccination fatigue was also positively associated with hesitancy to receive the first and second booster doses (AOR: 1.36 & 1.52). Additionally, hesitancy to receive the first booster dose was associated with higher hesitancy for the second booster dose (AOR: 14.05).
Table 2. Factors associated with hesitancy to receive the first and second booster doses of the COVID-19 vaccine (N=525).
| Characteristic |
Hesitancy to receive the
third dose of COVID-19 vaccine |
Hesitancy to receive the
fourth dose of COVID-19 vaccine |
|||||||
| OR (95% CI) | P value |
AOR*
(95% CI) |
P value | OR (95% CI) | P value |
AOR*
(95% CI) |
P value | ||
| Abbreviation: OR=crude odds ratio; AOR=adjusted odds ratio; CI=confidence interval; NA=not applicable. * Adjusted for significant background characteristics listed in Supplementary Table S2. | |||||||||
| Individual-level variables | |||||||||
| Positive attitude scale | 0.83 (0.76, 0.92) |
<0.001 | 0.83 (0.76, 0.92) |
<0.001 | 0.65 (0.60, 0.74) |
<0.001 | 0.66 (0.60, 0.74) |
<0.001 | |
| Negative attitude scale | 1.01 (0.97, 1.06) |
0.553 | 1.01 (0.97, 1.06) |
0.560 | 1.03 (0.99, 1.08) |
0.147 | 1.03 (0.99, 1.08) |
0.195 | |
| Perceived subjective norms | 0.54 (0.43, 0.67) |
<0.001 | 0.55 (0.44, 0.69) |
<0.001 | 0.39 (0.30, 0.49) |
<0.001 | 0.40 (0.31, 0.51) |
<0.001 | |
| Perceived behavioral control | 0.54 (0.43, 0.67) |
<0.001 | 0.51 (0.40, 0.63) |
<0.001 | 0.25 (0.19, 0.34) |
<0.001 | 0.25 (0.19, 0.34) |
<0.001 | |
| Vaccination fatigue (tired of receiving COVID-19 vaccination over and over again) | 1.34 (1.18, 1.58) |
<0.001 | 1.36 (1.18, 1.58) |
<0.001 | 1.48 (1.28, 1.71) |
<0.001 | 1.52 (1.31, 1.78) |
<0.001 | |
| Hesitancy to receive the third dose of COVID-19 vaccine | NA | NA | NA | NA | 14.05 (7.94, 24.79) |
<0.001 | 14.05 (8.05, 24.52) |
<0.001 | |
| Interpersonal variables | |||||||||
| Media exposure scale | 0.93 (0.89, 0.99) |
0.012 | 0.94 (0.89, 0.99) |
0.033 | 0.90 (0.85, 0.95) |
<0.001 | 0.90 (0.85, 0.95) |
<0.001 | |
| Frequency of thoughtful consideration about veracity of COVID-19-specific information | 0.64 (0.53, 0.77) |
<0.001 | 0.65 (0.54, 0.79) |
<0.001 | 0.51 (0.42, 0.62) |
<0.001 | 0.52 (0.43, 0.64) |
<0.001 | |
DISCUSSION
This is the first study to investigate hesitancy to receive the first and second COVID-19 vaccine booster doses among cancer patients. This study has several strengths, including its coverage of different geographic regions in China, its large sample size, and its examination of potential determinants at different levels. The level of hesitancy to receive the first COVID-19 vaccine booster dose among our participants was much higher than that of the general population in China (9).
This study provided practical implications for developing health promotion. Addressing vaccination fatigue may be beneficial for future health promotion for cancer patients. Rapid changes in policies and recommendations related to COVID-19 booster doses caused confusion among the general public (5). This confusion was further exacerbated when health authorities recommended the second booster dose. Modifying perceptions related to COVID-19 vaccine booster doses is also important. Updated evidence of booster doses in reducing mortality and severe consequences caused by COVID-19 among cancer patients should be disseminated in an accessible manner. Future programs might consider involving significant others of cancer patients to create a subjective norm favoring COVID-19 vaccine booster doses uptake. Healthcare workers may facilitate cancer patients to form a plan to receive a booster dose during clinical visits, which may help to improve perceived behavioral control. Higher exposure to topics related to COVID-19 vaccination and the Omicron variant was associated with lower hesitancy to receive booster doses. Health authorities should consider using these mass media channels to disseminate messages promoting booster doses. Similar to the findings among the general population in China, thoughtful consideration played an essential role in reducing hesitancy to receive booster doses. Thoughtful consideration could mitigate the negative impacts of misinformation on vaccine hesitancy (8).
This study has several limitations. First, our findings could not be generalized to all cancer patients, as we only targeted inpatients. Second, the sample was selected conveniently and could not represent all cancer patients in China. Third, we could not obtain the characteristics of cancer patients who refused to join the study, leading to selection bias. Additionally, this was a cross-sectional survey and could not establish a causal relationship. To address vaccination fatigue, modify perceptions related to booster doses, disseminate booster dose promotion messages through mass media, and improve thoughtful consideration of the veracity of COVID-19-related information might be helpful strategies.
SUPPLEMENTARY MATERIAL
Table S1. Hesitancy to receive COVID-19 vaccine booster doses and descriptive statistics of independent variables of interest (among 525 participants who completed the primary vaccination series).
| Hesitancy to receive COVID-19 vaccine booster doses and individual-level variables | No. of participants | Percentage (%) |
| Abbreviation: COVID-19=coronavirus disease 2019; SD=standard deviation. * Positive Attitude Scale. 3 items. Cronbach’s alpha: 0.90. Exploratory factor analysis identified one factor, explaining 83.38% of total variance. † Negative Attitude Scale. 5 items. Cronbach’s alpha: 0.84. Exploratory factor analysis identified one factor, explaining 72.05% of total variance. § Media Exposure Scale, 4 items, Cronbach’s alpha: 0.90, one factor was identified by exploratory factor analysis, explaining 76.39% of total variance. | ||
| Hesitancy to receive COVID-19 vaccine booster doses | ||
| Uptake of the first COVID-19 vaccine booster dose (the third dose) | ||
| No | 263 | 50.1 |
| Yes | 262 | 49.9 |
| Behavioral intention to receive the first COVID-19 vaccine booster dose (among participants who had not received it, n=263) | ||
| Likelihood of outcomes: unlikely to neutral | 168 | 63.9 |
| Highly probable | 95 | 36.1 |
| Hesitancy to receive the first COVID-19 vaccine booster dose (the third dose) | ||
| No | 357 | 68.0 |
| Yes | 168 | 32.0 |
| Hesitancy to receive the second COVID-19 vaccine booster dose (the fourth dose) | ||
| No | 229 | 43.6 |
| Yes | 296 | 56.4 |
| Individual-level variables | ||
| Positive attitudes toward COVID-19 vaccine booster dose, n (%) agree/strongly agree | ||
| Receiving a booster dose can maintain your antibody level and strengthen the protection against COVID-19 | 289 | 51.2 |
| A booster dose is highly effective in protecting you from COVID-19 variants of concern (e.g., Omicron) | 190 | 36.2 |
| A booster dose is highly effective in preventing severe consequences of COVID-19 | 253 | 48.2 |
| Positive attitude scale*, Mean (SD) | 10.8 | (2.1) |
| Negative attitudes toward COVID-19 vaccine booster dose, n (%) agree/strongly agree | ||
| The protection offered by COVID-19 vaccine booster dose is weaker among people with cancers | 184 | 35.0 |
| Cancer therapy would reduce the protection of COVID-19 vaccine booster dose | 167 | 31.8 |
| The side effects of COVID-19 vaccine booster dose are more severe among people with cancers | 195 | 37.1 |
| The duration of protection of COVID-19 vaccine booster dose is shorter among people with cancers | 101 | 19.2 |
| COVID-19 vaccine booster dose would negatively affect the control of cancers | 191 | 36.4 |
| Negative attitude scale†, Mean (SD) | 16.1 | (4.0) |
| Perceived subjective norm related to COVID-19 vaccine booster dose, n (%), agree/strongly agree | ||
| People who are important to you, such as family members or healthcare providers, would likely support you in receiving a booster dose | 190 | 36.2 |
| Item score, Mean (SD) | 3.2 | (0.9) |
| Perceived behavioral control to receive a COVID-19 vaccine booster dose, agree/strongly agree | ||
| Receiving a COVID-19 vaccine booster dose is easy for you if you want to | 253 | 48.2 |
| Item score, Mean (SD) | 3.4 | (0.9) |
| Vaccination fatigue: n (%) agree/strongly agree | ||
| You are tired of receiving COVID-19 vaccination over and over again | 90 | 17.1 |
| Item score, Mean (SD) | 2.5 | (1.3) |
| Media influences related to COVID-19 and COVID-19 vaccination | ||
| Frequency of exposure to the following contents on TV, radio, newspaper, and internet, n (%) sometimes/always | ||
| Infectivity of the Omicron variant of COVID-19 | 407 | 77.5 |
| Risk of having severe consequences or death is relatively low following infection of the Omicron variant of COVID-19 | 341 | 65.0 |
| COVID-19 pandemic is not under control after COVID-19 vaccination rollout | 283 | 53.9 |
| Some people contract COVID-19 after completion of their primary vaccine series | 314 | 59.8 |
| Media exposure scale§, Mean (SD) | 11.1 | (3.4) |
| Frequency of thoughtful consideration about veracity of COVID-19-specific information | ||
| Almost never | 102 | 19.4 |
| Seldom | 108 | 20.6 |
| Sometimes | 206 | 39.2 |
| Always | 109 | 20.8 |
| Item score, Mean (SD) | 2.6 | (1.0) |
Table S2. Associations between background characteristics and hesitancy to receive the first and second booster doses of the COVID-19 vaccine among 525 participants who completed the primary vaccination series.
| Characteristic | Hesitancy to receive the first COVID-19 vaccine booster dose | Hesitancy to receive the second COVID-19 vaccine booster dose | |||||
|
Prevalence of vaccine hesitancy n/N (%) |
OR (95% CI) | P value |
Prevalence of vaccine hesitancy n/N (%) |
OR (95% CI) | P value | ||
| Abbreviation: COVID-19=coronavirus disease 2019; OR=crude odds ratio; CI=confidence interval. | |||||||
| Age group in years | |||||||
| 18–45 | 29/87 (33.3) | 1.0 | 48/87 (44.2) | 1.0 | |||
| 46–60 | 68/219 (31.1) | 0.90 (0.53, 1.53) | 0.699 | 125/219 (57.1) | 1.08 (0.66, 1.78) | 0.762 | |
| 61–75 | 62/194 (32.0) | 0.94 (0.55, 1.61) | 0.820 | 106/194 (54.6) | 0.98 (0.59, 1.63) | 0.934 | |
| >75 | 9/25 (36.0) | 1.13 (0.44, 2.85) | 0.804 | 17/25 (68.0) | 1.73 (0.67, 4.42) | 0.255 | |
| Gender | |||||||
| Male | 93/293 (31.7) | 1.0 | 151/293 (51.5) | 1.0 | |||
| Female | 75/232 (32.3) | 1.03 (0.71, 1.49) | 0.886 | 145/232 (62.5) | 1.57 (1.10, 2.23) | 0.012 | |
| Ethnicity | |||||||
| Han majority | 146/426 (34.3) | 1.0 | 254/426 (59.6) | 1.0 | |||
| Other ethnic minority groups | 22/99 (22.2) | 0.55 (0.35, 0.92) | 0.022 | 42/99 (42.4) | 0.50 (0.32, 0.78) | 0.002 | |
| Education level | |||||||
| Junior high school and below | 112/338 (33.1) | 1.0 | 198/338 (58.6) | 1.0 | |||
| High school education or equivalent | 31/102 (30.4) | 0.88 (0.55, 1.42) | 0.604 | 54/102 (52.9) | 0.80 (0.51, 1.24) | 0.313 | |
| College-level and above | 25/85 (29.4) | 0.84 (0.50, 1.41) | 0.512 | 44/85 (51.8) | 0.76 (0.47, 1.22) | 0.257 | |
| Relationship status | |||||||
| Single/divorced/widowed | 10/39 (25.6) | 1.0 | 20/39 (51.3) | 1.0 | |||
| Married | 158/486 (32.5) | 1.40 (0.66, 2.94) | 0.378 | 276/486 (56.8) | 1.25 (0.65, 2.40) | 0.505 | |
| Employment status | |||||||
| Full-time | 46/138 (33.3) | 1.0 | 86/138 (62.3) | 1.0 | |||
| Part-time/self-employed/ Unemployed/retired/students |
122/387 (31.5) | 0.92 (0.61, 1.39) | 0.696 | 210/387 (54.3) | 0.72 (0.48, 1.07) | 0.102 | |
| Type of cancer | |||||||
| Lung cancer | 34/109 (31.2) | 1.0 | 55/109 (50.5) | 1.0 | |||
| Gastric cancer | 20/66 (30.3) | 0.96 (0.49, 1.86) | 0.902 | 36/66 (54.5) | 1.18 (0.64, 2.18) | 0.600 | |
| Liver cancer | 6/15 (40.0) | 1.47 (0.49, 4.46) | 0.496 | 12/15 (80.0) | 3.93 (1.05, 14.70) | 0.042 | |
| Breast cancer | 12/30 (40.0) | 1.47 (0.64, 3.39) | 0.366 | 24/30 (80.0) | 3.93 (1.48, 10.36) | 0.006 | |
| Colorectal cancer | 39/97 (40.2) | 1.48 (0.84, 2.63) | 0.178 | 64/97 (66.0) | 1.90 (1.08, 3.35) | 0.025 | |
| Esophageal cancer | 6/26 (23.1) | 0.66 (0.24, 1.60) | 0.418 | 12/26 (46.2) | 0.84 (0.36, 1.98) | 0.693 | |
| Ovarian cancer | 13/43 (30.2) | 0.96 (0.44, 2.06) | 0.908 | 26/43 (60.5) | 0.91 (0.55, 1.51) | 0.724 | |
| Other types of cancer | 39/139 (27.3) | 0.83 (0.48, 1.44) | 0.507 | 67/139 (48.2) | 1.50 (0.73, 3.08) | 0.267 | |
| Metastatic cancers | |||||||
| No | 161/490 (32.9) | 1.0 | 280/490 (57.1) | 1.0 | |||
| Yes | 7/35 (20.0) | 0.51 (0.22, 1.20) | 0.121 | 16/35 (45.7) | 0.63 (0.32, 1.26) | 0.191 | |
| Current treatment for cancer | |||||||
| Untreated patients | 4/17 (23.5) | 1.0 | 10/17 (58.8) | 1.0 | |||
| Chemotherapy only | 127/338 (37.6) | 1.96 (0.62, 6.13) | 0.250 | 212/338 (62.7) | 1.18 (0.44, 3.17) | 0.746 | |
| Radiotherapy only | 14/89 (15.7) | 0.61 (0.17, 2.13) | 0.436 | 34/89 (38.2) | 0.43 (0.15, 1.24) | 0.120 | |
| Immunotherapy only | 4/12 (33.3) | 1.63 (0.32, 8.40) | 0.562 | 6/12 (50.0) | 0.70 (0.16, 3.10) | 0.638 | |
| Chemotherapy and radiotherapy | 7/34 (20.6) | 0.84 (0.21, 3.40) | 0.810 | 14/34 (41.2) | 0.49 (0.15, 1.60) | 0.237 | |
| Immunotherapy and chemotherapy/radiotherapy | 5/15 (33.3) | 1.63 (0.34, 7.67) | 0.540 | 7/15 (46.7) | 0.61 (0.15, 2.49) | 0.493 | |
| Completion of treatment | 7/20 (35.0) | 1.75 (0.41, 7.45) | 0.449 | 13/20 (65.0) | 1.30 (0.34, 4.93) | 0.700 | |
| Presence of any other chronic diseases | |||||||
| No | 136/412 (33.0) | 1.0 | 242/412 (58.7) | 1.0 | |||
| Yes | 32/113 (28.3) | 0.80 (0.51, 1.27) | 0.344 | 54/113 (47.8) | 0.64 (0.42, 0.98) | 0.038 | |
Funding Statement
This study was supported by the National Natural Science Foundation of China (81872674), the Joint Foundation of Innovative Environment Construction of Autonomous Region of Xinjiang (#2019D01C326), and the Four “Batches” Innovation Project of Invigorating Medical Cause through Science and Technology of Shanxi Province (2022XM45), Shenzhen Science and Technology Innovation Committee Projects (No. JCYJ20220818102817038), the Scientific Research Foundation of Peking University Shenzhen Hospital (No. KYQD2022216)
Contributor Information
Jianzhou Yang, Email: jzyang@aliyun.com.
Zixin Wang, Email: wangzx@cuhk.edu.hk.
Junjie Xu, Email: xjjcmu@163.com.
References
- 1.Menni C, May A, Polidori L, Louca P, Wolf J, Capdevila J, et al COVID-19 vaccine waning and effectiveness and side-effects of boosters: a prospective community study from the ZOE COVID study. Lancet Infect Dis. 2022;22(7):1002–10. doi: 10.1016/S1473-3099(22)00146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhao Y, Du J, Li Z, Xu Z, Wu YX, Duan WS, et al It is time to improve the acceptance of COVID-19 vaccines among people with chronic diseases: a systematic review and meta-analysis. J Med Virol. 2023;95(2):e28509. doi: 10.1002/jmv.28509. [DOI] [PubMed] [Google Scholar]
- 3.National Health Commission of the People’s Republic of China. COVID-19 vaccination boosters. 2022. http://www.nhc.gov.cn/xcs/fkdt/202301/34d7d68ed30a4d249be6da9a43e6a8d7.shtml. [2023-2-1]. (In Chinese).
- 4.Chun JY, Kim SI, Park EY, Park SY, Koh SJ, Cha YJ, et al Cancer patients’ willingness to take COVID-19 vaccination: a nationwide multicenter survey in Korea. Cancers (Basel) 2021;13(15):3883. doi: 10.3390/cancers13153883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Su ZH, Cheshmehzangi A, McDonnell D, da Veiga CP, Xiang YT Mind the “vaccine fatigue”. Front Immunol. 2022;13:839433. doi: 10.3389/fimmu.2022.839433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ajzen I The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 7.Wang ZX, Fang Y, Yu FY, Chan PSF, Chen SY, Sun FH Facilitators and barriers to take up a COVID-19 vaccine booster dose among community-dwelling older adults in Hong Kong: a population-based random telephone survey. Vaccines (Basel) 2022;10(6):966. doi: 10.3390/VACCINES10060966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang KC, Fang Y, Chan PSF, Cao H, Chen HB, Hu T, et al Behavioral intention to get a booster dose of COVID-19 vaccine among Chinese factory workers. Int J Environ Res Public Health. 2022;19(9):5245. doi: 10.3390/ijerph19095245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qin CY, Wang RT, Tao LY, Liu M, Liu J Acceptance of a third dose of COVID-19 vaccine and associated factors in China based on health belief model: a national cross-sectional study. Vaccines (Basel) 2022;10(1):89. doi: 10.3390/VACCINES10010089. [DOI] [PMC free article] [PubMed] [Google Scholar]