Abstract
Media reports frequently cite observational studies and meta-analyses to promote the reputed cardiovascular benefits of moderate alcohol consumption, however it is unclear whether public opinion or drinking behavior align with these reports. We administered an anonymous, single-center, 35-question, cross-sectional survey among patients hospitalized for acute cardiac illnesses from June to September 2019 who were eligible for cardiac rehabilitation. We assessed patient opinions toward alcohol use, perceptions of alcohol’s health impact, and role of media in forming these beliefs. We hypothesized that drinking habits are associated with beliefs about the health benefits of alcohol consumption. Of 300 patients approached, 290 (97%) completed the survey. Most (69%) reported having heard moderate alcohol use is heart healthy from one or more sources including: TV (61%), family/friends (33%), newspapers (21%) and internet (10%) although only 19% reported believing these reports. In total, 12 (4%) patients reported intentionally increasing alcohol intake due to the reported beneficial health effects. There was a strong association between binge drinking and increasing alcohol use to improve cardiac health [OR 8.8 (95% CI 2.7, 29)]. Given the known cardiotoxic effects of alcohol, particularly in large doses, strategies aimed at population-based education regarding the unhealthy cardiovascular impact of alcohol use is needed, especially among binge drinkers.
Keywords: Alcohol Use Disorder, Patient Opinion, Cardiovascular Disease
INTRODUCTION
Moderate alcohol use, defined as up to one drink per day for women and two drinks daily for men1 (based on 2020–2025 US Dietary Guidelines for Americans), has been linked to cardiovascular benefits in a variety of older observational studies and meta-analyses.2–5 More recent research has concluded that alcohol confers no health benefit and that no level of use is safe.6–9 Furthermore, even a single episode of binge drinking reverses the cardiovascular benefits that have been touted with low volume alcohol use.2,10 Heavy alcohol use, particularly binge drinking, is associated with increased risk of myocardial infarction, heart failure, stroke, and cancer.11–13 Nevertheless, the idea that moderate alcohol use is healthy remains pervasive in the media, which averages 20 incidents of alcohol consumption within 1 hour of television.14 Given the increasing prevalence of binge drinking15 it is important to determine whether patient opinion, which may be related to these reports, is associated with drinking habits. Little is known about patient’s perceptions of alcohol’s health impact or whether these perceptions impact alcohol intake. We surveyed patients hospitalized with heart disease regarding their opinions on alcohol’s health effects and whether they had heard moderate alcohol use was beneficial. We assessed the frequency with which they increased alcohol intake due to the purported heart health benefits and any intended changes to drinking habits following hospitalization.
METHODS
This article uses additional data from an anonymous, single-center, patient-level survey among consecutive patients hospitalized for acute cardiac illnesses at Baystate Medical Center, a tertiary care center in Western Massachusetts.16 From June to September 2019, we approached patients aged 18 years or older who were admitted to the hospital with acute coronary syndrome, atherosclerotic peripheral vascular disease, or chronic systolic heart failure, as well as those undergoing coronary artery bypass grafting, percutaneous coronary intervention, and/or heart valve repair/replacement. Exclusion criteria were minimal, and only excluded those cognitively unable to complete the survey, too frail to participate in cardiac rehabilitation, or who spoke a non-English/Spanish language. The survey was translated into Spanish by certified translators and a Spanish-fluent team member (TM) approached eligible Spanish-speaking patients.
To maximize response rate, we took several steps to anonymize the survey. First, no links to the name or medical record of participants were made. Second, patients were specifically instructed to not write any identifying information on the survey. At the end of each week, the lists of eligible patients were destroyed. No protected health information was retrieved or recorded from the electronic medical record. To confirm eligibility, charts were reviewed by phase 1 cardiac rehabilitation staff to ensure the admitting diagnosis and survey eligibility.
Once eligibility was verified, a team member solicited participation from the patient. When a patient declined, they were no longer approached. When patients were unavailable, the team member revisited them up to 3 additional times to request participation. Survey intent was explained to patients, both written and verbally. Participation was voluntary and without compensation. Patients could skip any questions if they preferred not to respond. The Institutional Review Board of Baystate Medical Center deemed survey completion to be adequate evidence of informed consent and approved the protocol. Completed surveys were collected and managed via REDCap electronic data capture tools hosted at Tufts Medical Center.
Complete details of the survey can be found in a prior publication.16 In short, section one was the validated Alcohol Use Disorders Identification Test (AUDIT). The next section contained unique questions primarily aimed at assessing patient belief regarding alcohol’s effects on health. The final section provided demographic information. Hazardous drinking was defined as an AUDIT score ≥ 8, and binge drinking was defined as ≥ 5 alcoholic drinks for males or > 4 drinks for females on any single occasion.17,18 “Unhealthy drinking” was defined as hazardous use or binge drinking. Anyone with an AUDIT ≥1 but did not exhibit binge drinking or hazardous use classified as “low risk consumers”. “Non-drinker” was defined by an AUDIT of 0.
In this study, we were primarily interested in patient opinion of moderate alcohol use’s effect on cardiac health and whether this was related to the amount of alcohol consumed. To better appreciate how patient opinion was formed, we explored the sources (media, healthcare professional, word of mouth) from which patients had obtained health information about alcohol. The potential influence of these beliefs on drinking behavior was assessed through the questions “How much does any reported health benefits of moderate alcohol consumption influence your drinking habits?” and “How often in the past year have you felt that you should not drink alcohol but justified having a drink because of reported heart health benefits?” If a patient drank more alcohol than they subjectively thought appropriate due to purported heart health benefits more frequently than once a month, this was considered to be “cardiac justification” of increased alcohol use. Furthermore, we sought to gauge how drinking behavior would be theoretically influenced if a cardiologist told them moderate alcohol use was heart healthy.
Continuous variables were reported as means while categorical data was summarized with frequencies and proportions. For univariable analysis, chi-square, ANOVA, or odds ratio were employed for categorical variables with 95% confidence intervals and t-tests for continuous variables. We used a 5-point Likert scale of “strongly disagree” (1), “neutral” (3), and “strongly agree” (5) or “much lower” (1), “about right” (3), and “much higher” (5) for some questions and then averaged the numerical values of these responses. For the analysis of questions directed at patients who drink at least some alcohol, we excluded non-drinkers to improve the statistical validity of the comparison between the low-risk consumers and unhealthy drinkers.
Finally, to better assess risk factors associated with “cardiac justification” of increased alcohol use, we identified patient characteristics associated with this variable. Because of small numbers, multivariable prediction modeling was not possible due to unstable estimates. Only univariable associations with drinking habits were reported with the associated odds ratio and 95% confidence interval for categorial data. A p-value of <0.05 was considered significant. The software used for analysis was JMP 12.01 (SAS, Cary NC).
RESULTS
Over 4 months, team members approached 300 patients, of whom 290 (97%) completed the survey. Participants were mostly male, white, overweight, with a mean age of 69 (Table 1). The rate of unhealthy drinking was 18% (n=53). When comparing unhealthy drinkers to both non-drinkers and low-risk consumers, unhealthy drinkers were more likely to be younger, male, and to use tobacco, but less likely to have type 2 diabetes mellitus and obstructive sleep apnea. (Table 1). Spanish speaking patients were likely to be either non-drinkers or unhealthy drinkers.
Table 1.
Characteristics of patients surveyed by alcohol use status
| Variables | All Patients (n=290) | Never Drinkers (n=86) | Low-risk consumers (n=151) | Unhealthy drinkers (n=53) | p-value |
|---|---|---|---|---|---|
|
| |||||
| Age in years, mean, ± SD | 68 ± 11 | 71 ± 11 | 70 ± 11 | 62 ± 13 | <0.001 |
| Sex (male) | 203 (70%) | 51 (59%) | 103 (68%) | 49 (93%) | <0.001 |
| Body mass index (kg/m2) | 29 ± 6 | 30 ± 7 | 29 ± 5 | 30 ± 6 | 0.07 |
| Spanish speaking | 12 (4%) | 7 (8%) | 1 (1%) | 4 (8%) | 0.008 |
| Race | 0.05 | ||||
| Non-Hispanic White | 253 (87%) | 66 (76%) | 140 (93%) | 47 (89%) | |
| Asian | 3 (1%) | 2 (2%) | 1 (1%) | 0 | |
| Black | 12 (4%) | 5 (7%) | 5 (7%) | 2 (4%) | |
| Hispanic / Latino | 20 (7%) | 12 (14%) | 4 (3%) | 4 (8%) | |
| Native American | 1 (<1%) | 0 | 1 (1%) | 0 | |
| Other | 1 (<1%) | 1 (1%) | 0 | 0 | |
| Prior medical conditions† | |||||
| Hypertension | 239 (82%) | 77 (90%) | 123 (81%) | 39 (74%) | 0.051 |
| Hyperlipidemia | 214 (74%) | 67 (78%) | 110 (72%) | 37 (70%) | 0.53 |
| Type II diabetes mellitus | 135 (47%) | 50 (58%) | 68 (45%) | 17 (32%) | 0.01 |
| Stroke | 35 (12%) | 10 (11%) | 16 (11%) | 9 (17%) | 0.47 |
| Heart failure | 76 (26%) | 29 (34%) | 35 (23%) | 12 (23%) | 0.17 |
| Peripheral vascular disease | 26 (9%) | 11 (13%) | 12 (8%) | 3 (6%) | 0.29 |
| Myocardial infarction | 92 (32%) | 29 (33%) | 49 (32%) | 14 (26%) | 0.64 |
| Obstructive sleep apnea | 69 (24%) | 27 (31%) | 35 (23%) | 7 (13%) | 0.048 |
| Atrial fibrillation | 73 (25%) | 23 (27%) | 42 (28%) | 8 (15%) | 0.17 |
| Chronic kidney disease | 56 (19%) | 20 (23%) | 28 (19%) | 8 (15%) | 0.46 |
| Cirrhosis | 4 (1%) | 0 | 2 (1%) | 2 (4%) | 0.18 |
| Pancreatitis | 11 (4%) | 2 (2%) | 8 (5%) | 1 (2%) | 0.37 |
| Cancer | 40 (14%) | 13 (15%) | 21 (14%) | 6 (11%) | 0.81 |
| None of the above | 7 (2%) | 3 (4%) | 3 (2%) | 1 (2%) | 0.74 |
| Reason for Admission† | |||||
| Myocardial infarction | 101 (35%) | 32 (37%) | 48 (32%) | 21 (40%) | 0.50 |
| Coronary artery bypass grafting | 52 (18%) | 14 (16%) | 27 (18%) | 11 (21%) | 0.80 |
| Percutaneous coronary intervention | 47 (16%) | 11 (13%) | 27 (18%) | 9 (17%) | 0.58 |
| Stable angina pectoris | 3 (1%) | 1 (1%) | 2 (1%) | 0 | 0.70 |
| Peripheral vascular disease | 1 (<1%) | 0 | 1 (<1%) | 0 | 0.63 |
| Chronic heart failure | 55 (19%) | 20 (23%) | 27 (18%) | 8 (15%) | 0.44 |
| Heart valve repair / replacement | 39 (14%) | 11 (13%) | 22 (15%) | 6 (11%) | 0.81 |
| Education level | 0.52 | ||||
| Did not graduate High School | 37 (13%) | 13 (15%) | 15 (10%) | 9 (17%) | |
| Graduate High School | 108 (38%) | 35 (42%) | 53 (35%) | 20 (38%) | |
| Some college | 50 (17%) | 12 (14%) | 28 (19%) | 10 (19%) | |
| Associate degree | 35 (12%) | 12 (14%) | 19 (13%) | 4 (7.6%) | |
| Bachelor’s Degree | 32 (11%) | 6 (7%) | 20 (13%) | 6 (11%) | |
| Advanced degree | 20 (7%) | 6 (7%) | 10 (7%) | 4 (7.6%) | |
| Doctorate | 5 (2%) | 0 | 5 (3%) | 0 | |
| Education High School or less | 145 (50%) | 48 (57%) | 68 (45%) | 29 (55%) | 0.18 |
| Income Level (n=225) | 0.43 | ||||
| < $20,000 | 45 (20%) | 14 (22%) | 21 (18%) | 10 (23%) | |
| $20,000-$34,999 | 49 (21%) | 15 (23%) | 27 (23%) | 7 (16%) | |
| $35,000-$49,999 | 51 (23%) | 17 (26%) | 27 (24%) | 7 (16%) | |
| $50,000-$74,999 | 51 (23%) | 14 (22%) | 25 (22%) | 12 (28%) | |
| $75,000-$99,999 | 22 (9%) | 4 (6%) | 11 (9%) | 7 (16%) | |
| >$100,000 | 7 (3%) | 0 | 6 (5%) | 1 (2%) | |
| Income <$50,000 | 145 (64%) | 46 (72%) | 75 (64%) | 24 (54%) | 0.19 |
| Tobacco use within 30 days of admission | 62 (22%) | 5 (6%) | 37 (25%) | 20 (38%) | <0.001 |
Data reported as frequency (n, %) or mean ± standard deviation.
More than one response was considered acceptable.
Among all surveyed, 68% (n=198) reported having heard that moderate alcohol use was beneficial for heart health though fewer patients (n=54, 19%) believed this. Drinking status was marginally associated with belief that moderate use was heart healthy (never drinkers=2.4±1.0, low-risk consumers=2.6±1.1, unhealthy drinkers=2.8±1.0, See Figure 1). Moreover, patient opinion regarding the medical definition of “moderate drinking” showed unhealthy drinkers were more likely to believe the definition should be higher to some degree (never drinkers=2.0±0.9, low-risk consumers=2.4±0.9, unhealthy drinkers=3.1±1.0, p<0.001, Figure 2). When asked if moderate consumption was beneficial for general health, 20% agreed, with no significant difference among groups (Table 2). Accordingly, when comparing low-risk consumers to unhealthy drinkers, there was no difference in prevalence of having increased drinking amount based on the general health benefits, (Table 3.)
Figure 1.
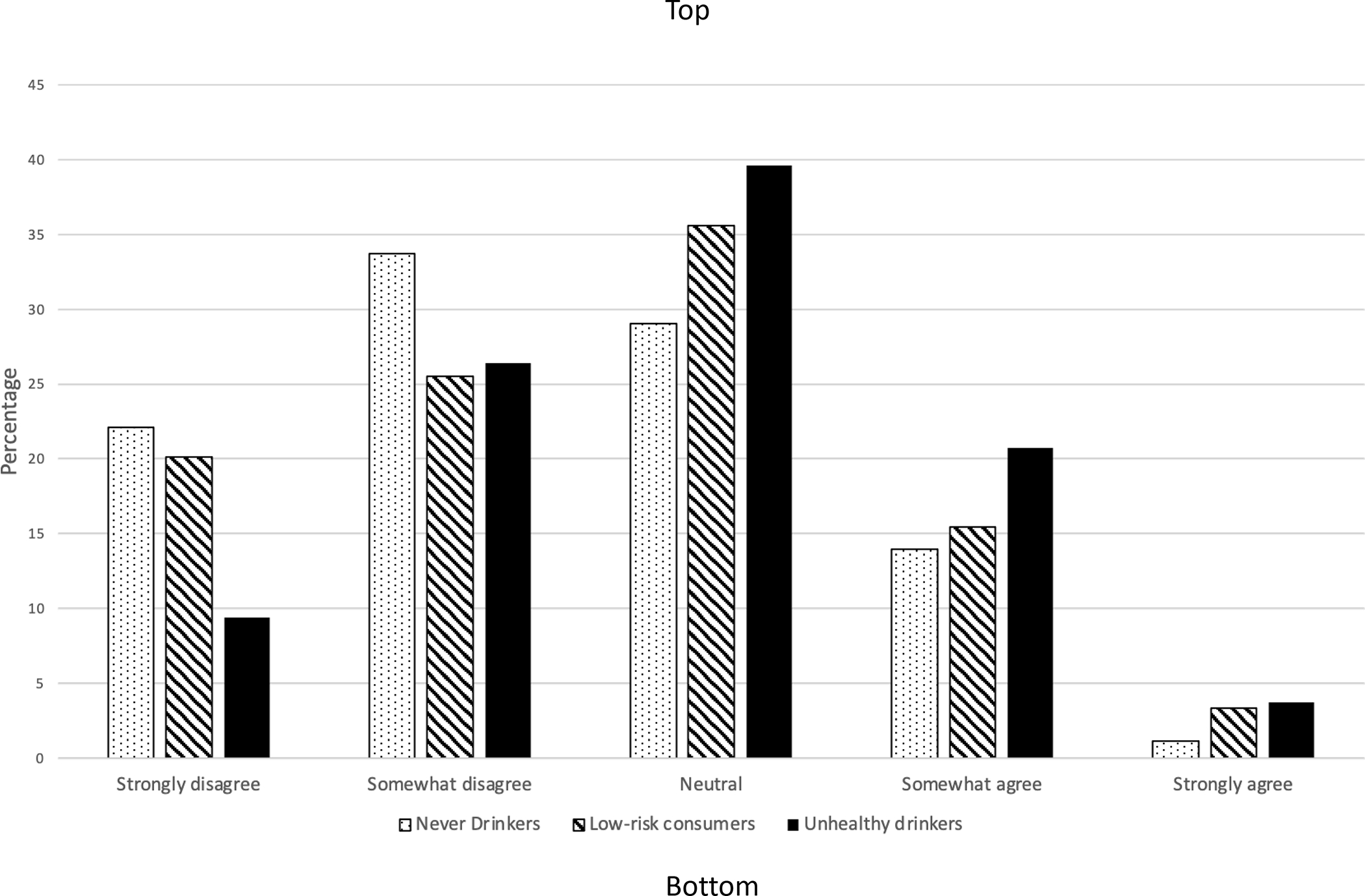
Responses of patients, separated based on drinking status, regarding their agreement or disagreement with the statement “moderate alcohol use is heart healthy” (P=0.052).
Figure 2.
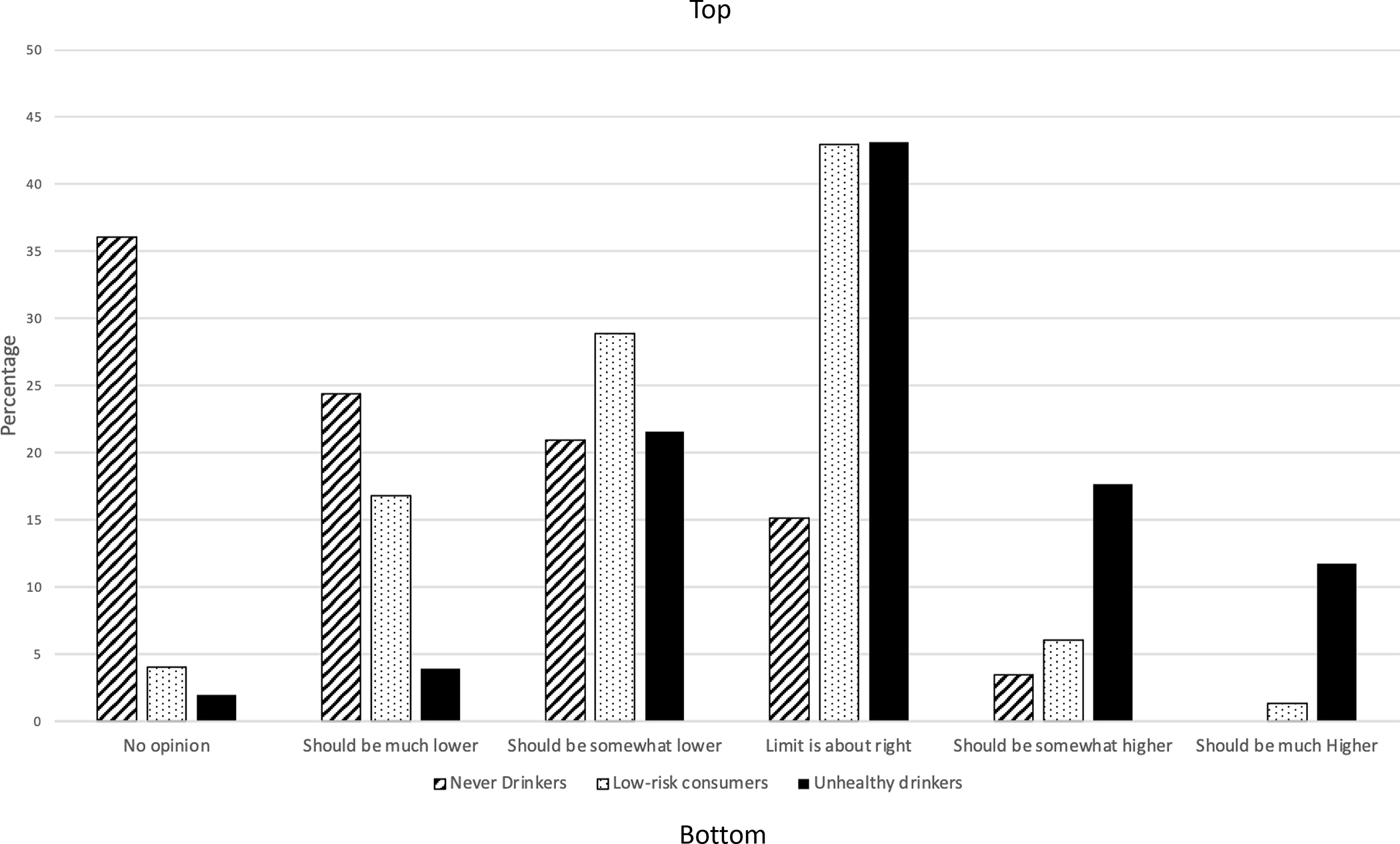
Bar graph reflecting patient’s opinion on the definition of “moderate alcohol use” as ≤1 drink daily for women or ≤2 daily for men., separated by drinking status (P<0.001).
Table 2.
Responses to Select Questions regarding the Health Impact of Alcohol Use
| How strongly do you agree or disagree that “moderate alcohol consumption is beneficial for my general health?” | |||
|
| |||
| P=0.15 | Never drinkers | Low-risk consumers | Unhealthy Drinkers |
| Strongly disagree | 20 (24%) | 45 (19%) | 4 (8%) |
| Somewhat disagree | 30 (35%) | 81 (35%) | 18 (34%) |
| Neutral | 25 (29%) | 74 (32%) | 17 (32%) |
| Somewhat agree | 10 (12%) | 31 (13%) | 11 (21%) |
| Strongly agree | 0 | 3 (1.3%) | 3 (6%) |
| “If a heart doctor told you moderate alcohol use was heart healthy, how likely would you be to change your alcohol use?” | |||
|
| |||
| P< 0.001 | Never drinkers | Low-risk consumers | Unhealthy Drinkers |
| I don’t drink and wouldn’t start | 75 (87%) | 12 (8%) | 1 (2%) |
| Significantly decrease my alcohol use | 0 | 2 (1%) | 2 (4%) |
| Somewhat decrease my alcohol use | 0 | 6 (4%) | 4 (8%) |
| No change in alcohol use | 1 (1%) | 97 (64%) | 30 (57%) |
| Somewhat increase my alcohol use | 9 (10%) | 28 (19%) | 13 (25%) |
| Significantly increase my alcohol use | 1 (1%) | 6 (4%) | 3 (6%) |
Table 3.
Responses to Questions regarding Alcohol and Health Benefits
| On a scale of 1-5, how much does any reported health benefits of moderate alcohol consumption influence your drinking habits? | ||
|
| ||
| P=0.87 | Low-risk/former consumers (n=151) | Unhealthy Drinkers (n=53) |
| I don’t drink and it doesn’t influence me | 16 (11%) | 3 (6%) |
| Makes me decrease my alcohol use | 10 (7%) | 4 (8%) |
| I drink, but it doesn’t influence me | 116 (77%) | 43 (81%) |
| Makes me increase alcohol use | 9 (6%) | 3 (6%) |
| “Now that you have been hospitalized for a heart issue, on a scale of 1-5, how are you mostly likely to change your alcohol use?” | ||
|
| ||
| P< 0.001 | Low-risk/former consumers | Unhealthy Drinkers |
| I don’t drink and wouldn’t start | 16 (11%) | 1 (2%) |
| Significantly decrease my alcohol use | 8 (5%) | 12 (23%) |
| Somewhat decrease my alcohol use | 17 (11%) | 17 (32%) |
| No change in alcohol use | 108 (72%) | 22 (42%) |
| Increase my alcohol use | 2 (1%) | 1 (2%) |
The most common source for hearing that alcohol possesses heart health benefits was TV (61%), followed by family/friends (33%), newspaper (21%), internet (10%), healthcare provider (6%), social media (6%), and unknown (12%). (Figure 3) There was no difference in the source based on age or drinking status (p=0.65). Of the 54 individuals who believed moderate alcohol use was heart healthy, 18 (33%) reported having heard this from a healthcare provider. Among the various kinds of alcohol, red wine (78%) was considered the most likely possess heart health benefits, followed by white wine (30%). Unhealthy drinkers were more likely to report beer as having a heart health benefit compared to low-risk/non consumers (13% vs 6.9%, p=0.045). No other differences were observed among other alcohol types in these two groups.
Figure 3.
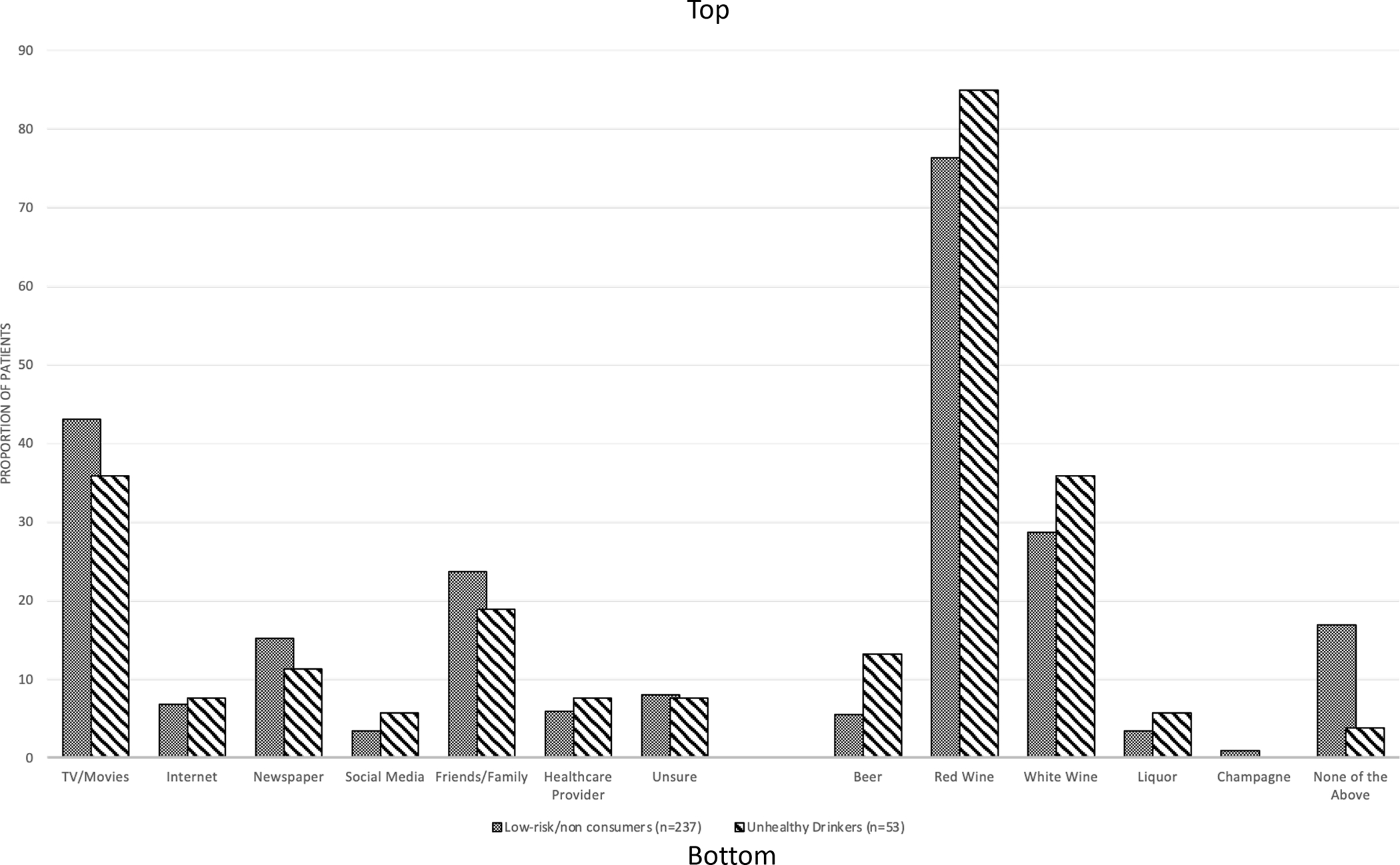
Bar graph representing the sources from which patients reported having heard moderate alcohol use is good for heart health as well as which type of alcohol, if any, they reported as most likely to provide a heart health benefits.
A few patients (n=12) endorsed drinking more alcohol than they felt appropriate based on the reported cardiac health benefits (cardiac justification). Unhealthy drinkers were more likely than low-risk consumers to report cardiac justification within the past month (13% vs 2.1%, OR 7.1 (95% CI [2.1, 13.2]), p<0.001). Similarly, cardiac justification was associated with hazardous drinking, binge drinking, and belief that the definition of moderate alcohol use should be somewhat or much higher. No association was found based on age or male sex, but there was a trend with believing that red wine is healthy (Table 4).
Table 4.
Selected Variables Associated with Drinking Excess Alcohol Based on the Heart Health Effects
| All other Patients (n=278) | Cardiac Justification of increased alcohol (n=12) | Odds Ratio (95% Confidence Interval) | p-value | |
|---|---|---|---|---|
|
| ||||
| Age | 68 ± 12 | 70 ± 15 | 0.75 | |
| Male sex | 193 (69%) | 10 (83%) | 2.2 (0.48 to 10) | 0.30 |
| Hazardous drinking (AUDIT≥8) | 46 (17%) | 7 (58) | 7.0 (2.1 to 23) | 0.002 |
| Binge drinking | 38 (14%) | 7 (58%) | 8.8 (2.7 to 29) | <0001 |
| Belief that alcohol limit should be somewhat/much higher | 22 (8%) | 7 (58%) | 16 (4.6 to 54) | <0.001 |
| Red wine perceived as healthy | 214 (77%) | 12 (100%) | * | 0.06 |
Odds ratio could not be computed due to 100% agreement among patients with regular justification.
Most patients (80%) reported intending to make minimal or no changes to their alcohol intake after discharge and most low-risk/non consumers reported no intention to change alcohol use. (Table 3). However, only 55% (29 of 53) of unhealthy drinkers planned to decrease alcohol consumption. Although the association only trended towards significance, fewer unhealthy drinkers planned to attend cardiac rehabilitation after discharge (38% vs 52%, p=0.062).
In the hypothetical question that a cardiologist or cardiac surgeon indicated that moderate alcohol use was heart healthy, most patients anticipated they would ignore such advice, but a few, including 10% of non-drinkers, would consume more alcohol. Unhealthy drinkers were more likely than low-risk consumers to report a plan to increase consumption (Table 2).
DISCUSSION
Among nearly 300 patients hospitalized for acute cardiac illness, approximately two-thirds had heard from at least one source, most commonly media or family/friends, that moderate alcohol use was heart healthy. Though many fewer individuals reported believing the purported heart health benefits, more than 2/3 of those who reported this opinion arrived at this conclusion without input from healthcare providers. As such, and in agreement with another study on the topic,19 many patients’ beliefs about alcohol’s health impact does not appear to be based on information provided by healthcare providers and may be influenced by unreliable sources.
While a dearth of healthcare provider-patient counseling regarding alcohol may contribute to this phenomenon16, these results suggest that unhealthy drinkers are highly sensitive to messages conveying alcohol’s purported health benefit, and appear prone to using this information to justify high levels of alcohol consumption. The root cause of why some individuals appear susceptible is unknown but may be due to increased exposure to reports or confirmation bias. Prior studies found that focused coverage of a product in media reinforces an individual’s intention to purchase and consume the product, they also recognized the detrimental impact that this finding could have when applied to alcohol.20,21 The prevalence of alcohol promoting messages, including in social media,14 may be powerful enough to influence a person’s drinking habits. Prior research has found that viewing or posting alcohol-related content on social media is associated with higher rates of excessive alcohol consumption.22,23
Here, patient opinion of alcohol’s cardiac health effect was strongly correlated with alcohol consumption. However, no association was detected between alcohol consumption and opinion of alcohol’s effect on general health. Prior studies suggested that unhealthy drinkers often formed positive associations, which reinforced increase consumption, in response to hearing about alcohol’s beneficial cardiac effects.19,24 That said, causal direction is uncertain, it is possible heavier alcohol consumption led to behavior-justifying cognitive distortions that augmented perceptions of alcohol’s cardiac benefits. Additionally, prior studies found that those with unhealthy alcohol consumption often perceive higher intake as being responsible and not excessive.25 Our data supports this notion as unhealthy drinkers believed the limit for moderate use should be higher. Notably, patients’ responses to our questions demonstrated hesitancy to attend cardiac rehabilitation and readiness to increase intake if a cardiologist endorsed moderate alcohol use as heart healthy. Together this suggests confirmation bias may be a factor as it seems that individuals who consume excessive amounts of alcohol seek out reasons to justify high consumption, despite guidelines recommending limited use.26 Notably our findings also support established guidelines and a recent policy briefing from The World Heart Foundation indicating that clinicians should never counsel non-drinkers should to start drinking.1,9 We found that some non-drinkers would begin drinking if counseled to begin for cardiovascular health benefits.
While the effects of moderate alcohol use on heart health continue to be debated, the detrimental effects of heavy alcohol use on cardiovascular health are widely accepted.15 Given trends toward increases in binge and hazardous drinking rates,6 which were exacerbated by the COVID-19 pandemic,27,28 it is essential that clinicians identify and address hazardous drinking. Re-education of unhealthy drinkers regarding alcohol’s negative overall and cardiac health impact should be a focus. Cardiologists and heart surgeons have an opportunity to address this situation effectively during acute cardiac episodes, which represent “teachable moments” during which the patient population might be more receptive to advice to change unhealthy behaviors. Specifically, providers could counter common media messages of alcohol’s purported benefits with the findings of current, peer-reviewed studies.
Excess alcohol use is an underappreciated risk factor among the cardiac patient population, and action from clinicians seems necessary but so far insufficient.16 Individual education in clinic encounters would be more effective if aligned with media messages, but providers should be prepared to specifically counter the misinformation conveyed through media sources. Furthermore, prior studies suggest a multifaceted approach to re-education efforts could be helpful.11 Media could have influence as reduced exposure to misinformation about alcohol’s health effects may lead to decreased justification among problem drinkers. Moreover, the media can have a profound impact by shifting focus to the hazards of alcohol use. Similar changes regarding the way media approach this topic have been recommended in other countries too.29
This study has several strengths and weaknesses.16 The participation rate was very high, with a 97% completion rate, most likely due to the anonymity and ease of the survey. The principal weakness is that this cross-sectional survey has limited ability to determine causal direction, i.e., whether unhealthy drinkers were influenced by media reports to consume more alcohol, or if this group was more likely to remember hearing these reports or endorse alcohol’s benefits because they drank. It is subject to recall bias, i.e., quantification of alcohol consumed was self-reported from memory. Additionally, because cardiac justification was observed in only 4% of our sample, the confidence intervals around these associations in Table 4 are wide, and these point estimates should be primarily considered exploratory.
While this single center study of hospitalized patients with cardiac illness may be limited in generalizability, it does confirm and extend the findings of a study which found that those who perceived alcohol as heart healthy consumed more alcohol.19 Together, these studies suggest a need for population-based re-education about alcohol’s heart health effects.
In this single-center study of hospitalized patients, many patients, especially unhealthy drinkers, believed moderate alcohol use was heart healthy despite having never discussed it with a physician or used debunked, reputed heart effects to justify excess alcohol use. Given, the known cardiotoxic effects, our study highlights the importance of identifying unhealthy drinkers in the cardiac population and providing education about the harms of excess drinking.
FUNDING
Dr. Quinn Pack is supported by a grant from the National Heart, Lung and Blood Institute of the National Institutes of Health of Bethesda, MD under award number 1K23HL135440, as well as by the Research Pilot Award Program from Baystate Medical Center.
Footnotes
CONFLICTS/DISCLOSURES
All authors report no conflicts of interest.
References
- 1.U.S. Department of Agriculture, U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025. 9th edition 2020:164. [Google Scholar]
- 2.Day E, Rudd JHF. Alcohol use disorders and the heart. Addiction 2019;114:1670–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mukamal KJ, Chen CM, Rao SR, Breslow RA. Alcohol Consumption and Cardiovascular Mortality among U.S. Adults, 1987–2002. J Am Coll Cardiol 2010;55. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3865979/. Accessed March 30, 2019. [DOI] [PMC free article] [PubMed]
- 4.Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 2011;342:d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dai J, Mukamal KJ, Krasnow RE, Swan GE, Reed T. Higher usual alcohol consumption was associated with a lower 41-y mortality risk from coronary artery disease in men independent of genetic and common environmental factors: the prospective NHLBI Twin Study. Am J Clin Nutr 2015, 102:31–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anon. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018;392:1015–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edenberg HJ. The Genetics of Alcohol Metabolism: Role of Alcohol Dehydrogenase and Aldehyde Dehydrogenase Variants. Alcohol Res Health 2007;30:5–13. [PMC free article] [PubMed] [Google Scholar]
- 8.Millwood IY, Walters RG, Mei XW, Guo Y, Yang L, Bian Z, Bennett DA, Chen Y, Dong C, Hu R, Zhou G, Yu B, Jia W, Parish S, Clarke R, Davey Smith G, Collins R, Holmes MV, Li L, Peto R, Chen Z. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in China. Lancet 2019;393:1831–1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anon. The Impact of Alcohol Consumption on Cardiovascular Health: Myths and Measures. Available at: https://world-heart-federation.org/wp-content/uploads/WHF-Policy-Brief-Alcohol.pdf. [DOI] [PMC free article] [PubMed]
- 10.Kalla A, Figueredo VM. Alcohol and cardiovascular disease in the geriatric population. Clin Cardiol 2017;40:444–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pletcher MJ, Varosy P, Kiefe CI, Lewis CE, Sidney S, Hulley SB. Alcohol consumption, binge drinking, and early coronary calcification: findings from the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol 2005;161:423–433. [DOI] [PubMed] [Google Scholar]
- 12.O’Keefe JH, Bybee KA, Lavie CJ. Alcohol and Cardiovascular Health: The Razor-Sharp Double-Edged Sword. J Am Coll Cardiol 2007;50:1009–1014. [DOI] [PubMed] [Google Scholar]
- 13.Malyutina S, Bobak M, Kurilovitch S, Gafarov V, Simonova G, Nikitin Y, Marmot M. Relation between heavy and binge drinking and all-cause and cardiovascular mortality in Novosibirsk, Russia: a prospective cohort study. The Lancet 2002;360:1448–1454. [DOI] [PubMed] [Google Scholar]
- 14.Keller-Hamilton B, Muff J, Blue T, Lu B, Slater MD, Roberts ME, Ferketich AK. Tobacco and Alcohol on Television: A Content Analysis of Male Adolescents’ Favorite Shows. Prev Chronic Dis 2018;15. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6219846/. Accessed May 13, 2021. [DOI] [PMC free article] [PubMed]
- 15.Hedden SL, Kennet J, Lipari R, Medley G, Tice P, Copello EAP, Kroutil LA. Key Substance Use and Mental Health Indicators in the United States: Results from the 2015. National Survey on Drug Use and Health. 2015:74. [Google Scholar]
- 16.Gobeil K, Medling T, Tavares P, Sawalha K, Abozenah M, Friedmann PD, Naimi T, Pack QR. Frequency of Hazardous and Binge Drinking Alcohol Among Hospitalized Cardiovascular Patients. Am J Cardiol 2021;153:119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol Drugs 1995;56:423–432. [DOI] [PubMed] [Google Scholar]
- 18.Anon. Drinking Levels Defined. National Institute on Alcohol Abuse and Alcoholism (NIAAA) 2011. Available at: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking. Accessed August 27, 2020. [Google Scholar]
- 19.Whitman IR, Pletcher MJ, Vittinghoff E, Imburgia KE, Maguire C, Bettencourt L, Sinha T, Parsnick T, Tison GH, Mulvanny CG, Olgin JE, Marcus GM. Perceptions, Information Sources, and Behavior Regarding Alcohol and Heart Health. Am J Cardiol 2015;116:642–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anon. Alcohol Control in Cuba: Preventing Countervailing Cultural and Mass Media Influences. Available at: https://mediccreview.org/alcohol-control-in-cuba-preventing-countervailing-cultural-and-mass-media-influences/. Accessed September 15, 2021. [DOI] [PubMed]
- 21.Valenzuela-Fernández L, Martínez-Troncoso C, Yáñez-Wieland F. Influence of Placement on Explicit and Implicit Memory of College Students. Comunicar: Revista Científica de Comunicación y Educación 2015;22:169–176. [Google Scholar]
- 22.Savolainen I, Oksanen A, Kaakinen M, Sirola A, Miller BL, Paek H-J, Zych I. The Association Between Social Media Use and Hazardous Alcohol Use Among Youths: A Four-Country Study. Alcohol Alcohol 2020;55:86–95. [DOI] [PubMed] [Google Scholar]
- 23.Moreno MA, Whitehill JM. Influence of Social Media on Alcohol Use in Adolescents and Young Adults. Alcohol Res Health 2014;36:91–100. [PMC free article] [PubMed] [Google Scholar]
- 24.Brown KG, Stautz K, Hollands GJ, Winpenny EM, Marteau TM. The Cognitive and Behavioural Impact of Alcohol Promoting and Alcohol Warning Advertisements: An Experimental Study. Alcohol Alcohol 2016;51:354–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Noel JK, Xuan Z, Babor TF. Perceptions of Alcohol Advertising among High Risk Drinkers. Subst Use Misuse 2018;53:1403–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. Global Strategy to reduce the harmful use of alcohol. Geneva: World Health Organization, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grossman ER, Benjamin-Neelon SE, Sonnenschein S. Alcohol Consumption during the COVID-19 Pandemic: A Cross-Sectional Survey of US Adults. Int J Environ Res Public Health 2020;17:9189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barbosa C, Cowell AJ, Dowd WN. Alcohol Consumption in Response to the COVID-19 Pandemic in the United States. J Addict Med 2021;15:341–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zachová K, Petruželka B, Barták M, Rogalewicz V. Media portrayal of alcohol does not match its real harm effects in the Czech Republic. Cent Eur J Public Health 2019;27 Suppl:S66–S73. [DOI] [PubMed] [Google Scholar]


