Abstract
A 36-year-old male patient presented with a firm swelling in the left lacrimal sac region with a history of recurrent episodes of acute dacryocystitis, which partly resolved with systemic antibiotics. Computed tomography showed diffuse soft tissue mass without bony erosion in the same area. Incisional biopsy confirmed diffuse large cell lymphoma of non-Hodgkin's type by histopathology and immunohistochemistry. Oncologists did not detect systemic involvement, and the patient received six cycles of cyclophosphamide, hydroxydaunorubicin, oncovin, and prednisolone (CHOP). Epiphora was resolved, and no recurrence of the lesion was seen with subsequent dacryocystorhinostomy with intubation and was in good health for up to 3 years of follow-up. Although primary lacrimal sac lymphoma is a rare entity, high suspicion, and prompt action in atypical cases can save lives from aggressive diffuse large cell lymphoma.
Keywords: Acute dacryocystitis, CHOP therapy, dacryocystorhinostomy, diffuse large cell lymphoma
Introduction
Despite infection being the primary ailment of the lacrimal drainage system, neoplasms affecting the system cannot be ignored. Tumors of the lacrimal sac, however relatively rare and may be primary, secondary, or metastatic. Most Lacrimal neoplasms are epithelial in origin, and squamous cell carcinoma is the most common one.[1] Lymphomas of the lacrimal sac are rare,[2] and the primary one is rarer. The vast majority of lacrimal lymphomas are either secondary or metastatic. Histopathologically, non-Hodgkin's B-cell lymphomas are the most familiar type of lymphoma in the lacrimal drainage system.[1] In the UK, diffuse large B-cell lymphoma (DLBCL) and extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma) are common histological types of primary lacrimal sac lymphoma.[3] But in Japan, the most reported primary lymphoma in the lacrimal sac is DLBCL.[4]
Case Report
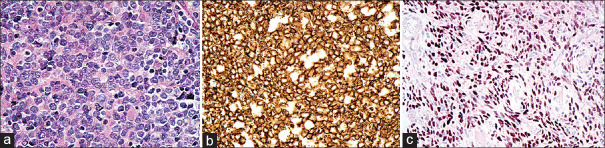
A 36-year-old male presented with recurrent episodes of painful swelling in the left lacrimal sac area and was treated with systemic antibiotics, considering the case as acute dacryocystitis [Figure 1], several times. The left lacrimal sac was swollen, firm, and moderately painful. Visual acuity was 20/20 with normal anterior and posterior segment findings in both eyes. Computed tomography of the orbit showed diffuse soft tissue mass, which took contrast without any bony erosion in the left lacrimal sac region [Figure 1]. An incisional biopsy was performed due to a diagnostic dilemma. Subsequent histopathology and immunohistochemistry confirmed the diagnosis as diffuse large cell lymphoma of non-Hodgkin's type of left lacrimal sac. An oncologist consultation was done, and no systemic involvement was detected. The patient was treated with six cycles of CHOP therapy (cyclophosphamide, hydroxydaunorubicin, oncovin, and prednisolone) which caused complete resolution of the lesion. The dacryocystorhinostomy surgery with intubation was performed, and the tube was removed after 3 months. During follow-up over 3 additional years, no epiphora or recurrences were observed.
Figure 1:
Clinical picture. (a) Acute swelling in the lacrimal area. (b) CT showing diffuse lesion in the lacrimal region extending to mid-orbit. (c) After receiving CHOP therapy and DCR operation. CT: Computed tomography, DCR: Dacryocystorhinostomy
Discussion
Acute dacryocystitis is the acute inflammation or infection of the lacrimal sac characterized by redness, tenderness, and swelling over the sac area and epiphora. The reported patient had recurrent episodes of similar features, treated with antibiotics and anti-inflammatory drugs on each episode. He responded well with acute pain relief each time, but mild tenderness and swelling persisted. The presentation mimicked acute dacryocystitis, which may be due to associated inflammation or concomitant infection which blocked the lacrimal passage. The presence of a relatively firm swelling was suspicious of a neoplasm within the lacrimal sac.
Lacrimal sac neoplasms are rare but life-threatening. It may be primary, secondary, or metastatic. Tumors of the lacrimal drainage system may be epithelial (73%)[1] or nonepithelial and either benign or malignant. Among nonepithelial tumors, lymphoproliferative tumors account for approximately 2%–8% of lacrimal sac tumors and more commonly arise secondary to systemic spread in a patient with leukemia or lymphoma. Primary lymphoma of the lacrimal sac is extremely rare.[2]
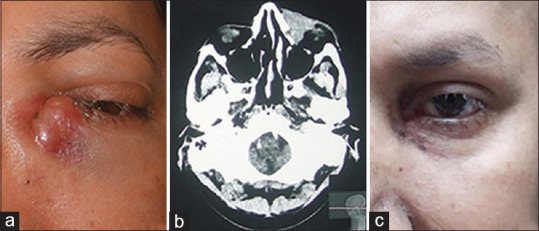
Histopathologically, primary lymphoma of the lacrimal drainage system is usually a non-Hodgkin's B-cell lesion. Extranodal marginal zone lymphoma of MALT is the most common tumor in ocular adnexa, accounting for 50%–70%.[5] On another hand, DLBCL is one of the most common systemic high-grade lymphomas (30%)[6] if compared with primary orbital and periorbital DLBCL (7%–21%).[7] Sjö et al. reported an equal number of cases of diffuse large cell lymphoma (DLBCL) and MALT lymphoma of the lacrimal sac, five cases of each out of 15 cases in a study from the UK.[3] However, DLBCL was the most reported case from Japan.[4] Histopathology and immunohistochemistry study of our case was positive for cluster of differentiation 20 (CD20) and signal transducer and activator of transcription 6 [Figure 2]. According to the WHO classification, it was diffuse large cell lymphoma.
Figure 2:
Histopathological feature. (a) H and E: Diffuse infiltration of atypical centroblast-type lymphoid cells. (b) The atypical centroblast-type lymphoid cells are positive for B-cell marker CD20. In addition, brown is positive membranous staining. (c) STAT6: Immunocytochemistry shows that every tumor cells express the STAT6 protein. Brown is positive staining. CD20: Cluster of differentiate 20, STAT6: Signal transducer and activator of transcription 6
If we consider the diagnostic age, our patient was diagnosed at a younger age than the previously reported case series, where the median age of diagnosis was 71 years (range 45–95 years).[3] Frequent presenting symptoms of lacrimal sac lymphoma are epiphora (85%), lacrimal sac area swelling (79%), and dacryocystitis (21%) of chronic variety[3] but here patient presented with recurrent episodes of acute dacryocystitis.
The literature search also showed that DLBCL has clinical, histopathological, immunohistochemical, and genetic heterogeneity, that's why it is unlikely to represent a single disease process and has a variable prognosis.[6] Due to this nature, all patients should have a complete workup to rule out systemic lymphoma. After appropriate staging, treatment for the condition continues to involve chemotherapy, typically an anthracycline-based regimen such as CHOP (cyclophosphamide, adriamycin, vincristine, and prednisolone) and/or radiotherapy. Newer immunotherapies such as anti-CD20 antibodies may revolutionize the management of the condition and improve the overall prognosis.[6,8] The reported patient was evaluated by an oncologist and treated with six cycles of CHOP therapy. Diffuse large cell lymphoma is typically high-grade lymphoma, but it is potentially curable.[3] The survival rate of the patient depends on the lesion, whether localized or not. One cohort study of 37 patients with orbital DLBCL showed a high 5-year survival rate of 90.9%.[9] An advanced disease does not provide such a favorable survival rate. Our patient had a localized lesion, and after proper treatment, he was symptom and recurrence-free in 3 years of follow-up. Proper staging and treatment can save a life in case of aggressive DLBCL. Although, primary lacrimal sac lymphoma is a rare entity; a high suspicion and prompt decision-making are needed in atypical cases.
Statement of ethics
The patient gave his informed consent for publication of this case report (text and photographs). The study protocol was approved by the institute's review board.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Yanoff M, Sassani J. Ocular Pathology. 8th. New York: Elsevier; 2018. pp. 232–3. [Google Scholar]
- 2.Litschel R, Siano M, Tasman AJ, Cogliatti S. Nasolacrimal duct obstruction caused by lymphoproliferative infiltration in the course of chronic lymphocytic leukemia. Allergy Rhinol (Providence) 2015;6:191–4. doi: 10.2500/ar.2015.6.0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sjö LD, Ralfkiaer E, Juhl BR, Prause JU, Kivelä T, Auw-Haedrich C, et al. Primary lymphoma of the lacrimal sac: An EORTC ophthalmic oncology task force study. Br J Ophthalmol. 2006;90:1004–9. doi: 10.1136/bjo.2006.090589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kakutani S, Takahashi Y, Valencia MR, Kakizaki H. Diffuse large B-Cell lymphoma of the lacrimal sac in a Japanese patient. Case Rep Ophthalmol. 2018;9:516–9. doi: 10.1159/000495745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coupland SE, Hellmich M, Auw-Haedrich C, Lee WR, Stein H. Prognostic value of cell-cycle markers in ocular adnexal lymphoma: An assessment of 230 cases. Graefes Arch Clin Exp Ophthalmol. 2004;242:130–45. doi: 10.1007/s00417-003-0831-5. [DOI] [PubMed] [Google Scholar]
- 6.Hunt KE, Reichard KK. Diffuse large B-cell lymphoma. Arch Pathol Lab Med. 2008;132:118–24. doi: 10.5858/2008-132-118-DLBL. [DOI] [PubMed] [Google Scholar]
- 7.Sullivan TJ, Whitehead K, Williamson R, Grimes D, Schlect D, Brown I, et al. Lymphoproliferative disease of the ocular adnexa: A clinical and pathologic study with statistical analysis of 69 patients. Ophthalmic Plast Reconstr Surg. 2005;21:177–88. doi: 10.1097/01.iop.0000159173.42243.ad. [DOI] [PubMed] [Google Scholar]
- 8.Sullivan TJ, Grimes D, Bunce I. Monoclonal antibody treatment of orbital lymphoma. Ophthalmic Plast Reconstr Surg. 2004;20:103–6. doi: 10.1097/01.iop.0000115594.98470.ac. [DOI] [PubMed] [Google Scholar]
- 9.Madge SN, McCormick A, Patel I, Hatef E, Menon V, Prabhakaran VC, et al. Ocular adnexal diffuse large B-cell lymphoma: Local disease correlates with better outcomes. Eye (Lond) 2010;24:954–61. doi: 10.1038/eye.2009.283. [DOI] [PubMed] [Google Scholar]