Introduction
Dengue fever (DF) is transmitted to humans by the bite of infected female Aedes mosquito, usually Aedes aegypti.
After the incubation period, symptoms follow three phases: Febrile, critical, and recovery. Hemorrhagic manifestations are often seen during the critical phase.[1]
We describe a case of acute macular neuroretinopathy (AMN),[2,3] branch vein vasculitis, and neurosensory detachment presenting as a consequence of DF.
Case Report
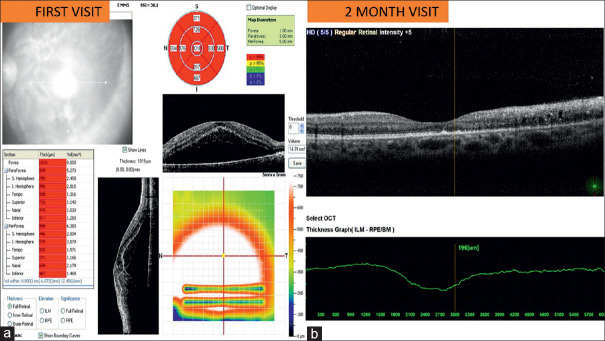
A 28-year-old male presented with complaint of blurring of vision in the left eye (LE) and headache for 15 days. He had a history of DF 22 days before the presentation. The DF was confirmed by positive immunoglobulin M enzyme-linked immunosorbent assay serology for the Dengue virus. His best-corrected-visual-acuity (BCVA) was (right eye [RE]) 6/9 and (LE) finger counting 0.5 m. On examination, (LE) fundus revealed focal constriction of arteries and veins, soft exudates, dot-blot and flame-shaped hemorrhages in branch vein distribution, attempt at macular fan formation, and area of macular edema [Figure 1]. (LE) optical coherence tomography (OCT) revealed neurosensory detachment with cystoid macular edema [Figure 2]. Central macular thickness was 1018 μ.
Figure 1:
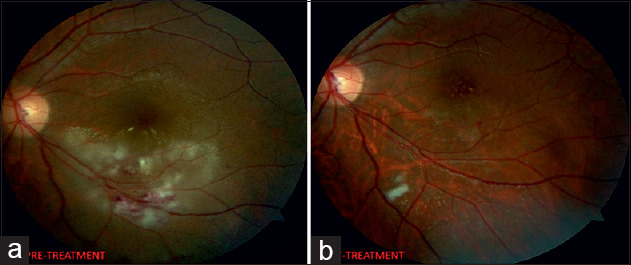
Left eye. (a) Branch vein vasculitis, macular oedema (first-visit). (b) Resolution of features (final-visit)
Figure 2:
Optical-coherence-tomography. (a) Left eye First-visit: neurosensory detachment. (b) Two months: Cystoid macular edema, subfoveal hyperreflectivity, and disruption of the external limiting membrane, the ellipsoid zone, and interdigitation zone in the foveal region. Features suggestive of acute macular neuroretinopathy
Complete blood count revealed platelet count: 84,000 (thrombocytopenia). Based on history, thrombocytopenia and clinical findings, diagnosis of dengue retinopathy was made. The patient was given intravitreal triamcinolone acetonide (4 mg/0.1 ml).[4]
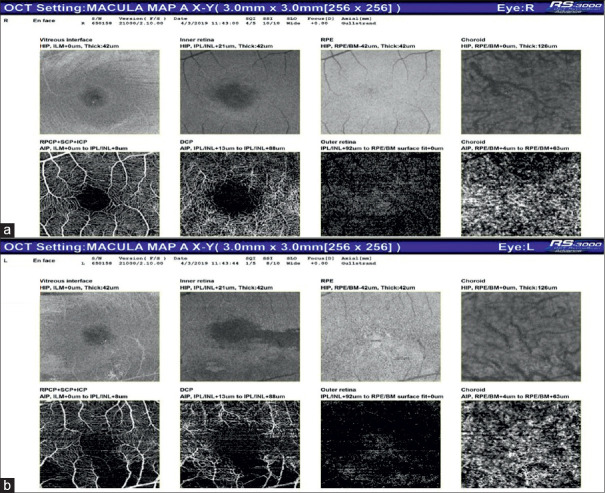
At 2 months, BCVA (RE) was 6/6 and (LE) 6/18. Since (LE) visual acuity did not normalize, fundus fluorescein angiography (FA) and OCT angiography (OCTA) were done. FA LE showed normal foveal avascular zone (noted in the early phase of angiogram), few areas of the delayed filling (inferotemporal vascular arcade) with capillary leakage. Disc leakage was also noted [Figure 3]. OCT showed cystoid spaces, intraretinal exudates with back-shadowing, disruption of the external limiting membrane, the ellipsoid zone, and the interdigitation zone in the foveal region. There was the subfoveal area of hyperreflectivity and retinal thinning [Figure 4]. (RE) OCTA was normal. OCTA (LE) showed distortion of retinal superficial and deep capillary plexus (SCP-DCP) inferotemporal to foveal center [Figure 5]. The features on OCT and OCTA were suggestive of AMN.
Figure 3:
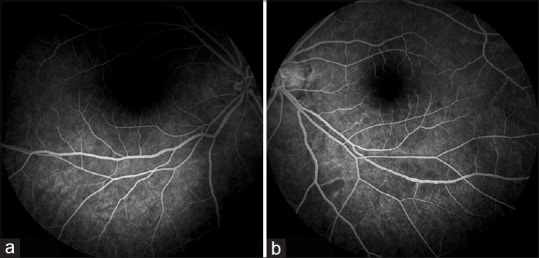
Fluorescein angiography. (a) Right eye and (b) left eye shows normal foveal-avascular-zone, few areas of the delayed filling (inferotemporal-vascular-arcade) with capillary leakage
Figure 4:
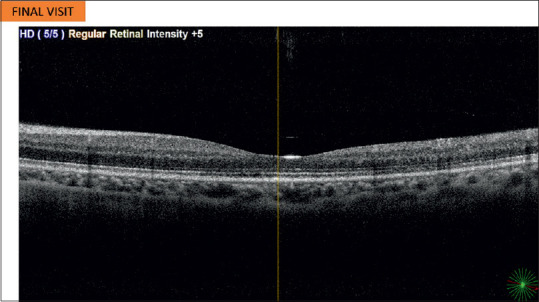
Optical coherence tomography final-visit left eye: Restoration of retinal layers with retinal thinning
Figure 5:
Optical coherence tomography-angiography (final-visit). (a) right eye: Normal. (b) left eye: Distortion of superficial and deep capillary plexus with preservation of retinal pigment epithelium and choroid
Six months visit revealed complete resolution of fundus features, visual acuity of both eyes on Snellen's 6/6, but with persistent micropsia. OCT revealed retinal thinning with the restoration of retinal layers. Distortion of SCP-DCP on OCTA persisted, which was the only persistent defect explaining the visual complaint of the patient [Figure 2].
Discussion
The OCTA changes in AMN associated with dengue, as seen in our patient, have been scarcely described.[5] In our case, the retinal pigment epithelium and choroid OCTA findings remained normal, thus suggesting that DF predominantly affected only outer retinal layers.
Dengue retinopathy typically occurs within a week of onset of DF. Intravitreal steroids can be used in treatment. FA, OCT, and OCTA are useful tools in the diagnosis and follow-up. Especially OCTA, which is noninvasive and can be used to study macular changes. Visual acuity may be restored but the quality of vision may be permanently affected due to permanent changes in the retinal capillary plexus.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initial s will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Halstead SB. Mosquito-borne hemorrhagic fevers of South-East Asia and the Western Pacific. Bull World Health Organ. 1966;35:17–33. [PMC free article] [PubMed] [Google Scholar]
- 2.Munk MR, Jampol LM, Cunha Souza E, de Andrade GC, Esmaili DD, Sarraf D, et al. New associations of classic acute macular neuroretinopathy. Br J Ophthalmol. 2016;100:389–94. doi: 10.1136/bjophthalmol-2015-306845. [DOI] [PubMed] [Google Scholar]
- 3.Aggarwal K, Agarwal A, Katoch D, Sharma M, Gupta V. Optical coherence tomography angiography features of acute macular neuroretinopathy in dengue fever. Indian J Ophthalmol. 2017;65:1235–8. doi: 10.4103/ijo.IJO_485_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bacsal KE, Chee SP, Cheng CL, Flores JV. Dengue-associated maculopathy. Arch Ophthalmol. 2007;125:501–10. doi: 10.1001/archopht.125.4.501. [DOI] [PubMed] [Google Scholar]
- 5.Velaitham P, Vijayasingham N. Central retinal vein occlusion concomitant with dengue fever. Int J Retina Vitreous. 2016;2:1. doi: 10.1186/s40942-016-0027-x. [DOI] [PMC free article] [PubMed] [Google Scholar]