Abstract
Aims
The aim of this study was to estimate the global burden of atrial fibrillation (AF)/atrial flutter (AFL) and its attributable risk factors from 1990 to 2019.
Methods and results
The data on AF/AFL were retrieved from the Global Burden of Disease Study (GBD) 2019. Incidence, disability-adjusted life years (DALYs), and deaths were metrics used to measure AF/AFL burden. The population attributable fractions (PAFs) were used to calculate the percentage contributions of major potential risk factors to age-standardized AF/AFL death. The analysis was performed between 1990 and 2019. Globally, in 2019, there were 4.7 million [95% uncertainty interval (UI): 3.6 to 6.0] incident cases, 8.4 million (95% UI: 6.7 to 10.5) DALYs cases, and 0.32 million (95% UI: 0.27 to 0.36) deaths of AF/AFL. The burden of AF/AFL in 2019 and their temporal trends from 1990 to 2019 varied widely due to gender, Socio-Demographic Index (SDI) quintile, and geographical location. Among all potential risk factors, age-standardized AF/AFL death worldwide in 2019 were primarily attributable to high systolic blood pressure [34.0% (95% UI: 27.3 to 41.0)], followed by high body mass index [20.2% (95% UI: 11.2 to 31.2)], alcohol use [7.4% (95% UI: 5.8 to 9.0)], smoking [4.3% (95% UI: 2.9 to 5.9)], diet high in sodium [4.2% (95% UI: 0.8 to 10.5)], and lead exposure [2.3% (95% UI: 1.3 to 3.4)].
Conclusion
Our study showed that AF/AFL is still a major public health concern. Despite the advancements in the prevention and treatment of AF/AFL, especially in regions in the relatively SDI quintile, the burden of AF/AFL in regions in lower SDI quintile is increasing. Since AF/AFL is largely preventable and treatable, there is an urgent need to implement more cost-effective strategies and interventions to address modifiable risk factors, especially in regions with high or increased AF/AFL burden.
Keywords: Global burden, Atrial fibrillation/atrial flutter, Incidence, Deaths, Disability-adjusted life years, Risk factors
What’s new?
Accurate assessment of the current burden and attributable risk factors for atrial fibrillation (AF)/atrial flutter (AFL) is critical for developing effective control and prevention strategies.
Previous studies from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2017 have reported the global burden of AF/AFL. To our knowledge, no updated study has provided detailed estimates on various factors like the incidence, disability-adjusted life years, deaths, and major risk factors of AF/AFL in all regions over time.
In this study, we provide a revised report on AF/AFL based on the latest GBD 2019 study, Our study provides a comparable and comprehensive overview of the updated global burden of AF/AFL and its attributable risk factors from 1990 to 2019.
Introduction
Atrial fibrillation (AF)/atrial flutter (AFL) is the most common type of clinical tachyarrhythmia. The AF/AFL cases are prevalent worldwide and continuously rising due to the rapidly aging population. The AF/AFL affects the quality of the patient's life and increases the susceptibility to severe complications such as myocardial infarction, heart failure, stroke, and ultimately death.1,2 The AF/AFL-related deaths were as high as 287 241 in 20173 and remains one of the leading causes of death worldwide. While the age-standardized AF/AFL death rate has declined by 2.53% over the past few decades, the absolute number of disability-adjusted life years (DALYs) due to AF/AFL globally increased from 1990 to 2019 and has risen to 5.97 million people.4 The AF/AFL has become a leading cause of disability worldwide, and post-AF/AFL care and the economic costs of treatment are substantial. In the United States of America (USA), ∼3–5 million people suffer from AF/AFL, and as the population ages, it is expected to affect more than 8 million people by 2050.5 In Europe, the prevalent cases of AF are projected to increase from a current estimate of 8.8 million to ∼18 million in 2060.6 The medical costs of managing individual AF patients are extremely high. Direct cost estimates range from $2000 to 14 200 per patient-year in the USA and from €450 to 3000 in Europe.7 AF/AFL is likely to become a serious public health concern and will increase the financial burden on society in the future.
It is necessary to accurately assess the current burden and attributable risk factors for AF/AFL, which is crucial to the development of effective control and prevention strategies. Although the previous studies3,4 from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2017 have reported the global burden of AF/AFL, to our knowledge, no updated study has provided a detailed report about various factors like the incidence, DALYs, deaths and major risk factors of AF/AFL in all regions over time. Therefore, in the study, based on the latest GBD 2019 estimates, we expanded and updated the previous study to provide comparable and comprehensive information on the global burden of AF/AFL and its attributable risk factors from 1990 to 2019.
Methods
Data sources
Raw data were obtained from the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 database, a web-based tool using the Global Health Data Exchange query tool (http://ghdx.healthdata.org/gbd-results-tool). The detailed contents and methodology uesd by GBD 2019 have been published previously.8,9 The waiver of informed consent was reviewed and approved by the University of Washington Institutional Review Board due to the use of deidentified aggregated data in GBD 2019.
Definitions
The International Classification of Diseases and Injuries (ICD-9 and ICD-10) was used to identify AF/AFL. All cardiovascular diseases coded as 427.3–427.32 in the ICD-9 and I48–I48.92 in the ICD-10 were identified as AF/AFL in the study. Similar to previous GBD studies,3,4,9 electrocardiogram was used to diagnose AF/AFL.
Years of life lost (YLLs) were calculated as the standard life expectancy at the age of death multiplied by the number of deaths. Years lived with disability (YLDs) was estimated as the number of YLLs to health, weighted by disability weight for severity. The sum of YLLs and YLDs due to premature death of the population was considered as DALYs.
The Socio-Demographic Index (SDI), which ranges from 0 (worst) to 1 (best), was an aggregated indicator that quantifies development in each location year.8,9 It was calculated on the basis of the lagged distribution of income per capita, the average education level of individuals aged 15 years and older, and the total fertility rate under 25 years. The threshold for the SDI quintile was calculated using estimates for countries with a population of more than 1 million.8,9 According to SDI quintiles, 195 countries and regions were divided into high SDI, high–middle SDI, middle SDI, low–middle SDI, and low SDI quintiles.8,9
The risk factors for AF/AFL were identified based on the following criteria: adequate evidence for the cause of AF/AFL, availability of exposure data, and the possibility of modification.3,9,10 In GBD 2019, six risk factors, i.e. high body mass index, high systolic blood pressure, smoking, alcohol use, diets high in sodium, and lead exposure, contributed to AF/AFL-related death. The exact definition of these risk factors and methods for quantifying the percentage contribution of these risk factors to AF/AFL-related death has been published in previous studies.3,9,10
Statistical analysis
We estimated counts, age-standardized rate (ASR) per 100 000 people, and percentage change in ASR with 95% uncertainty interval (UI) to quantify GBD 2019 AF/AFL burden metrics such as prevalence, incidence, DALYs, and deaths and reported by global, gender, SDI quintile, and geographical location. The ASR was calculated by directly standardizing the global age structure.11 UI were calculated based on 1000 draw-level estimates for each parameter. 95% UI was defined as the 25th and 975th values across all 1000 draws. It is important to note that AF/AFL does not directly lead to death but could cause complications such as stroke or heart failure, which indirectly contribute to the increased risk of AF/AFL-related mortality. Therefore, the crude case fatality rate in patients with AF/AFL is not an appropriate metric, mortality due to AF/AFL is preferred. The AF/AFL-related death rate was statistically estimated and modelled using a comprehensive multi-parameter method, which obtained statistical significance through the combination of various national covariates. The population attribution fractions (PAFs) represent the proportion of age-standardized AF/AFL-related death rate, which will reduce if risk factor exposure is reduced to the theoretical minimum. The PAFs were calculated based on the percentage contributions of the major risk factors to age-standardized AF/AFL-related death rate.3,9,10 The PAFs for each risk factor includes all burdens that can be directly or indirectly attributed to that risk factor. Therefore, the cumulative impact of risk factors is not a simple addition to their personal contributions. When PAFs are summarized across multiple risk factors, mediation adjustment is required. For all estimates, 95% UI excluding zero represents statistical significance. The analysis was performed between 1990 and 2019.
Results
The GBD estimates on AF/AFL were available from GBD 2019 Data Input Sources Tool website (http://ghdx.healthdata.org/gbd-results-tool, accessed on May 2022). In 2019, AF/AFL affected ∼60.0 million (95% UI 45.7 to 75.3) people worldwide, an increase of 111.0% (95% UI: 107.4 to 115.5) from 28.3 million (95% UI: 21.5 to 36.2) in 1990. The incident cases of AF/AFL were 4.7 million (95% UI: 3.6 to 6.0) in 2019, an increase of 104.0% (95% UI: 100.3 to 108.8) from 2.3 million (95% UI: 1.8 to 3.0) in 1990. However, the age-standardized incidence rate of AF/AFL decreased by 2.5% (95% UI: −3.6 to 1.2) from 1990 to 2019. The largest decreases in age-standardized incidence rate was seen in countries in the high–middle SDI quintile [−4.1% (95% UI: −5.6 to −2.6)] (Table 1). Globally, the number of AF/AFL-related deaths in 2019 was 0.32 million (95% UI: 0.27 to 0.36), an increase of 169.4% (95% UI: 143.8 to 189.2) compared with 1990. The age-standardized rate of AF/AFL-related deaths in 2019 also increased by 2.0% (95% UI: −6.5 to 8.7) compared with 1990, with the greatest increases occurring in countries in the low–middle SDI quintile [21.6% (95% UI: −0.9 to 45.6)] (Table 1). In addition, AF/AFL contributed to 8.4 million (95% UI: 6.7 to 10.5) DALYs cases globally in 2019, an increase of 126.6% (95% UI: 111.1 to 145.4) compared with 1990. Despite the increases, from 1990 to 2019, the age-standardized DALYs rate decreased by 0% (95% UI: −0.1 to 0), with the largest decreases in countries in the high–middle SDI quintile [−0.1% (95% UI: −0.1 to 0.0)] (Table 1).
Table 1.
Counts and age-standardized incidence, deaths, and DALYs rates of AF/AFL in 2019, and their percentage change in ASR form 1990 to 2019, by sex, SDI quintile, and GBD region
| Incidence (95% UI) | Deaths (95% UI) | DALYs (95% UI) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2019 counts | 2019 ASR per 100 000 people | Percentage change in ASR, 1990–2019 | 2019 counts | 2019 ASR per 100 000 people | Percentage change in ASR, 1990–2019 | 2019 counts | 2019 ASR per 100 000 people | Percentage change in ASR, 1990–2019 | |
| Global | 4 720 324 (3 644 331 to 5 961 597) | 57.1 (44.1 to 71.9) | −2.5% (−3.6 to −1.2) | 315 337 (267 964 to 361 014) | 4.4 (3.7 to 5.0) | 2.0% (−6.5 to 8.7) | 8 393 635 (6 693 984 to 10 541 461) | 107.1 (86.2 to 133.7) | 0%(−0.1 to 0) |
| Sex | |||||||||
| ȃMale | 2 376 460 (3 010 747 to 1 837 669) | 60.8 (47.1 to 76.3) | −4.4% (−5.7 to −2.9) | 121 548 (148 261 to 97 352) | 4.3 (3.5 to 5.3) | 4.9% (−9.0 to 16.2) | 3 956 017 (5 050 017 to 3 087 374) | 114.1 (90.1 to 144.1) | 0% (−0.1 to 0) |
| ȃFemale | 2 343 863 (2 973 621 to 1 796 329) | 53.5 (41.1 to 67.7) | −0.3% (−1.5 to 1.5) | 193 789 (224 867 to 160 729) | 4.4 (3.7 to 5.1) | 0.8% (−9.0 to 9.2) | 4 437 618 (5 539 382 to 3 574 324) | 101.0 (81.3 to 126.0) | 0% (−0.1 to 0) |
| SDI quintiles | |||||||||
| ȃLow SDI | 207 391 (158 050 to 265 306) | 42 (31.8 to 53.7) | −1.7% (−3.2 to −0.1) | 13 160 (9591 to 16 006) | 4.3 (3.1 to 5.2) | 15.4% (−5.4 to 42.5) | 370 883 (291 504 to 456 045) | 91.9 (71.9 to 111.6) | 0.1% (0 to 0.2) |
| ȃLow–middle SDI | 733 952 (558 001 to 935 186) | 54.7 (41.5 to 69.8) | 0.8% (−0.2 to 1.8) | 38 423 (32 144 to 44 622) | 4.2 (3.5 to 4.9) | 21.6% (−0.9 to 45.6) | 1 173 891 (929 505 to 1 468 081) | 101.0 (81.2 to 123.9) | 0.1% (0 to 0.2) |
| ȃMiddle SDI | 1 347 018 (1 024 382 to 1 717 860) | 54.3 (41.2 to 69.0) | −0.9% (−1.8 to 0.0) | 69 793 (59 854 to 80 804) | 4.1 (3.5 to 4.7) | 7.7% (−7.1 to 25.3) | 2 113 471 (1 653 609 to 2 694 931) | 97.9 (78.1 to 122.7) | 0% (0 to 0.1) |
| ȃHigh–middle SDI | 1 194 911 (912 920 to 1 531 244) | 58 (44.6 to 74.2) | −4.1% (−5.6 to −2.6) | 83 844 (70 923 to 100 863) | 4.5 (3.8 to 5.4) | −3.8% (−12.3 to 3.4) | 2 214 107 (1 734 630 to 2 823 347) | 110.2 (86.7 to 140.1) | −0.1% (−0.1 to 0) |
| ȃHigh SDI | 1 235 202 (976 182 to 1 518 125) | 69.2 (55.4 to 85.2) | −3.1% (−7.3 to 1.8) | 109 926 (86 254 to 132 025) | 4.6 (3.7 to 5.5) | −0.2% (−10.6 to 5.8) | 2 517 229 (2 012 613 to 3 144 013) | 122.6 (97.3 to 153.6) | 0% (−0.1 to 0) |
| GBD regions | |||||||||
| ȃAndean Latin America | 8085 (6052 to 10 360) | 14.8 (11.1 to 19.2) | 8.9% (4.8 to 13) | 2239 (1804 to 2717) | 4.3 (3.5 to 5.2) | −2.1% (−20.6 to 21.3) | 33 839 (28 083 to 40 058) | 63.6 (52.7 to 75.2) | 0% (−0.2 to 0.2) |
| ȃAustralasia | 42 634 (32 397 to 54 822) | 90.4 (69.7 to 114.5) | −8.4% (−12.4 to −3.9) | 4082 (3258 to 4977) | 6.9 (5.5 to 8.3) | −7.1% (−14.3 to 6.5) | 89 702 (71 277 to 113 671) | 168.3 (132.5 to 214.3) | −0.1% (−0.1 to 0) |
| ȃCaribbean | 15 388 (11 495 to 19 899) | 29.7 (22.2 to 38.4) | 1.3% (−0.9 to 3.6) | 2500 (2064 to 3049) | 4.7 (3.9 to 5.8) | 6.2% (−7.2 to 21.7) | 43 197 (36 148 to 51 752) | 83.3 (69.7 to 99.8) | 0% (0 to 0.2) |
| ȃCentral Asia | 51 004 (38 434 to 65 518) | 64.8 (49.6 to 82.7) | 2.0% (−0.4 to 4.5) | 2467 (2144 to 3301) | 5.7 (4.9 to 7.7) | 58.7% (15.7 to 97.4) | 81 519 (63 510 to 104 678) | 138.3 (109.6 to 176.3) | 0.3% (0.1 to 0.4) |
| ȃCentral Europe | 142 513 (108 565 to 183 042) | 70.6 (54.2 to 89.8) | 1.9% (0.1 to 3.6) | 10 882 (9017 to 12 840) | 4.8 (4.0 to 5.7) | 7.0% (−6.1 to 18.3) | 302 864 (237 301 to 385 693) | 136.0 (106.5 to 173.3) | 0% (−0.1 to 0.1) |
| ȃCentral Latin America | 73 686 (55 668 to 95 265) | 31.8 (23.8 to 41.2) | −0.1% (−1.9 to 13.4) | 9907 (8079 to 12 667) | 4.6 (3.7 to 5.8) | 2.2% (−10.6 to 14.0) | 185 647 (152 660 to 228 151) | 82.8 (68.3 to 101.9) | 0% (−0.1 to 0.1) |
| ȃCentral Sub-Saharan Africa | 16 185 (12 341 to 20 967) | 32.2 (24.4 to 41.5) | −2.5% (−5.8 to 0.9) | 1651 (1054 to 2389) | 5.6 (3.5 to 8.2) | 12.6% (−14.6 to 0.0) | 40 758 (28 803 to 53 877) | 104.2 (72.9 to 138.1) | 0.1% (−0.1 to 0.3) |
| ȃEast Asia | 1 202 906 (907 838 to 1 545 466) | 57.4 (43.7 to 73) | 3.9%(2.4 to 5.4) | 54 066 (45 777 to 62 320) | 3.8 (3.2 to 4.4) | −4.6% (−21.2 to 17.5) | 1 793 188 (1 356 400 to 2 304 890) | 96.8 (75.1 to 122.6) | 0% (−0.1 to 0.1) |
| ȃEastern Europe | 253 918 (193 148 to 325 654) | 74.4 (57.2 to 95.3) | 8.8% (7.2 to 10.5) | 15 982 (13 463 to 20 894) | 4.6 (3.9 to 6.0) | 14.6% (−1.3 to 29.3) | 481 406 (368 863 to 621 279) | 136.6 (104.8 to 177.1) | 0.1% (0.1 to 0.2) |
| ȃEastern Sub-Saharan Africa | 30 351 (23 226 to 38 666) | 19.9 (15.2 to 25.6) | 2.2% (1.0 to 3.5) | 4485 (2872 to 5572) | 4.7 (3.0 to 5.9) | 10.9% (−11.0 to 39.7) | 94 303 (66 626 to 115 072) | 77.1 (53.3 to 94.3) | 0.1% (−0.1 to 0.3) |
| ȃHigh-income Asia Pacific | 77 896 (59 594 to 99 918) | 21.1 (16.3 to 27.2) | −21.5% (−23.4 to −18.8) | 15 307 (11 653 to 20 615) | 2.4 (1.9 to 3.2) | −20.5% (−30.3 to −11.5) | 265 228 (212 780 to 329 103) | 53.5 (43.1 to 66.6) | −0.2% (−0.2 to −0.1) |
| ȃHigh-income North America | 675 439 (539 471 to 822 528) | 108.5 (87.6 to 131.4) | 13.9% (5.1 to 19.1) | 36 444 (29 295 to 44 399) | 5.0 (4.0 to 6.0) | 22.9% (12.8 to 27.9) | 1 059 274 (837 806 to 1 336 169) | 160.2 (125.7 to 202.7) | 0.1% (0.1 to 0.2) |
| ȃNorth Africa and Middle East | 173 921 (133 004 to 221 692) | 41.9 (31.7 to 53.6) | 0.3% (−1.4 to 1.8) | 10 505 (8922 to 12 765) | 3.7 (3.1 to 4.3) | 5.1% (−11.7 to 41.4) | 289 998 (229 100 to 361 786) | 81.6 (65.1 to 100.8) | 0% (−0.1 to 0.2) |
| ȃOceania | 3970 (2996 to 5098) | 59.3 (44.9 to 75.2) | 2.3% (−1.0 to 5.4) | 171 (129 to 228) | 4.2 (3.2 to 5.5) | 3.7% (−17.2 to 29.1) | 6579 (5066 to 8433) | 116.6 (91.1 to 148.0) | 0.1% (−0.1 to 0.2) |
| ȃSouth Asia | 851 084 (645 139 to 1 089 231) | 61.4 (46.5 to 78.0) | 2.2% (1.2 to 3.0) | 36 619 (28 652 to 45 926) | 4.1 (3.2 to 5.1) | 23.1% (−8.6 to 59.8) | 1 257 580 (971 301 to 1 609 102) | 106.1 (82.9 to 132.9) | 0.1% (0 to 0.2) |
| ȃSoutheast Asia | 378 094 (288 272 to 482 012) | 62.8 (47.5 to 79.6) | 2.4% (1.3 to 3.8) | 16 028 (13 357 to 19 305) | 4.0 (3.3 to 4.8) | 25.1% (0.7 to 50.1) | 544 420 (417 735 to 695 212) | 105.7 (82.2 to 133.5) | 0.1% (0 to 0.2) |
| ȃSouthern Latin America | 34 681 (26 262 to 44 620) | 41.8 (31.8 to 53.4) | 2.6% (−1.7 to 6.4) | 4639 (3866 to 6055) | 5.3 (4.4 to 6.9) | 8.1% (−3.6 to 23.8) | 86 620 (71 626 to 107 603) | 101.0 (83.3 to 125.8) | 0.1% (0 to 0.1) |
| ȃSouthern Sub-Saharan Africa | 20 372 (15 608 to 26 060) | 37.1 (28.2 to 47.6) | −0.9% (−2.6 to 0.8) | 1440 (1258 to 1587) | 3.9 (3.4 to 4.4) | 26.9% (11.7 to 44.8) | 36 881 (30 132 to 45 192) | 79.2 (65.8 to 95.7) | 0.1% (0 to 0.2) |
| ȃTropical Latin America | 107 861 (81 577 to 138 989) | 44.8 (33.8 to 57.8) | 3.1% (1.4 to 4.9) | 11 051 (8832 to 13 043) | 5.0 (4.0 to 5.9) | 5.4% (−9.3 to 13.0) | 235 075 (193 674 to 285 763) | 102.3 (84.3 to 124.3) | 0% (−0.1 to 0.1) |
| ȃWestern Europe | 495 118 (378 485– to 631 497) | 63 (48.4 to 79.8) | −13.4% (−15.3 to −11.6) | 69 928 (55 541 to 84 441) | 5.8 (4.6 to 7.0) | −0.2% (−14.4 to 7.8) | 1 347 220 (1 087 687 to 1 676 380) | 132.8 (105.9 to 168.1) | −0.1% (−0.2 to 0) |
| ȃWestern Sub-Saharan Africa | 65 217 (49 907 to 83 723) | 36 (27.3 to 46.2) | 1.4% (0.6 to 2.4) | 4944 (4097 to 5799) | 4.7 (3.9 to 5.6) | 5.5% (−27.8 to 30.1) | 118 338 (94 717 to 145 563) | 86.2 (70.0 to 103.2) | 0% (−0.2 to 0.2) |
Data in parentheses are 95% uncertainty interval.
AF/AFL, atrial fibrillation and atrial flutter; ASR, age-standardized rate; DALYs, disability-adjusted life years; GBD, Global Burden of Disease, Injuries, and Risk Factors Study; SDI, Socio-Demographic Index; UI, uncertainty interval.
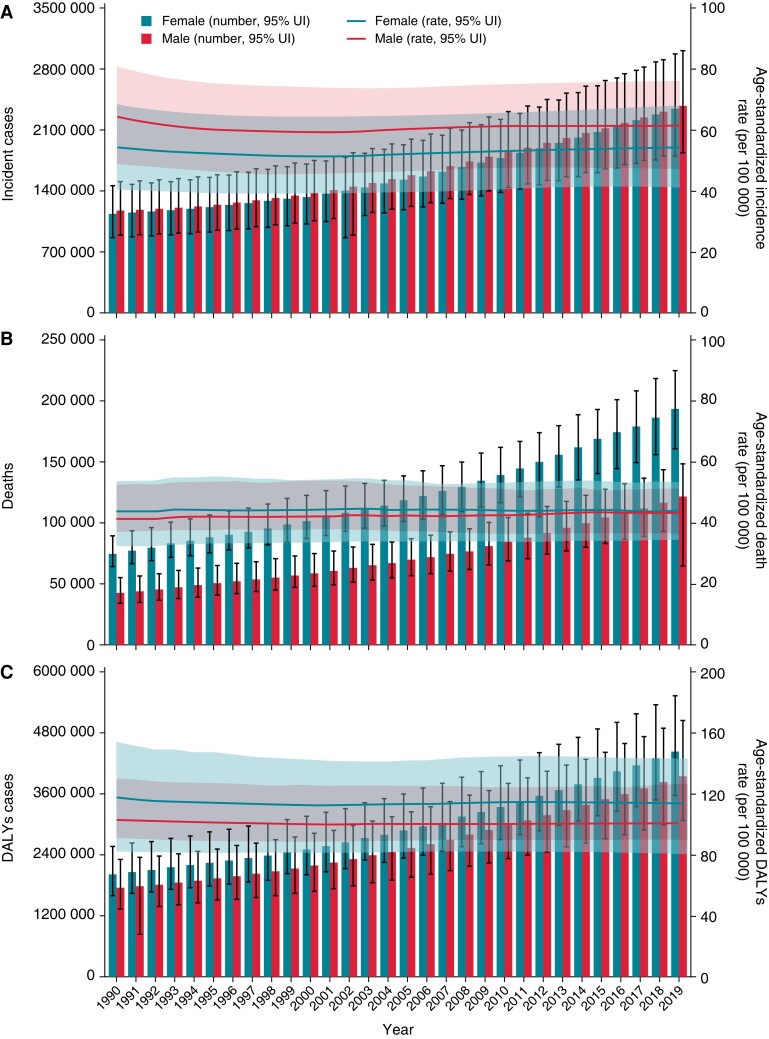
By sex, in 2019, there were more incident cases of AF/AFL in males than in females, with a higher age-standardized incidence rate of AF/AFL seen in males than in females (Figure 1A). Conversely, there were more deaths due to AF/AFL in females than in males, with a higher age-standardized death rate of AF/AFL observed in females than in males (Figure 1B). Additionally, DALYs cases due to AF/AFL were higher in females than males, while the higher age-standardized DALYs rate of AFAFL was seen in males than in females in 2019 (Figure 1C). Consistent with counts and ASRs of incident, DALYs, and deaths in 2019, those results were also seen across all years (Figure 1).
Figure 1.
Trends in numbers and age-standardized rates of incident cases (A), deaths (B), and disability-adjusted life years cases (C) of atrial fibrillation/atrial flutter at the global level, 1990–2019. Error bars indicate the 95% uncertainty interval (UI) for numbers. Shading indicates the 95% UI for rates.
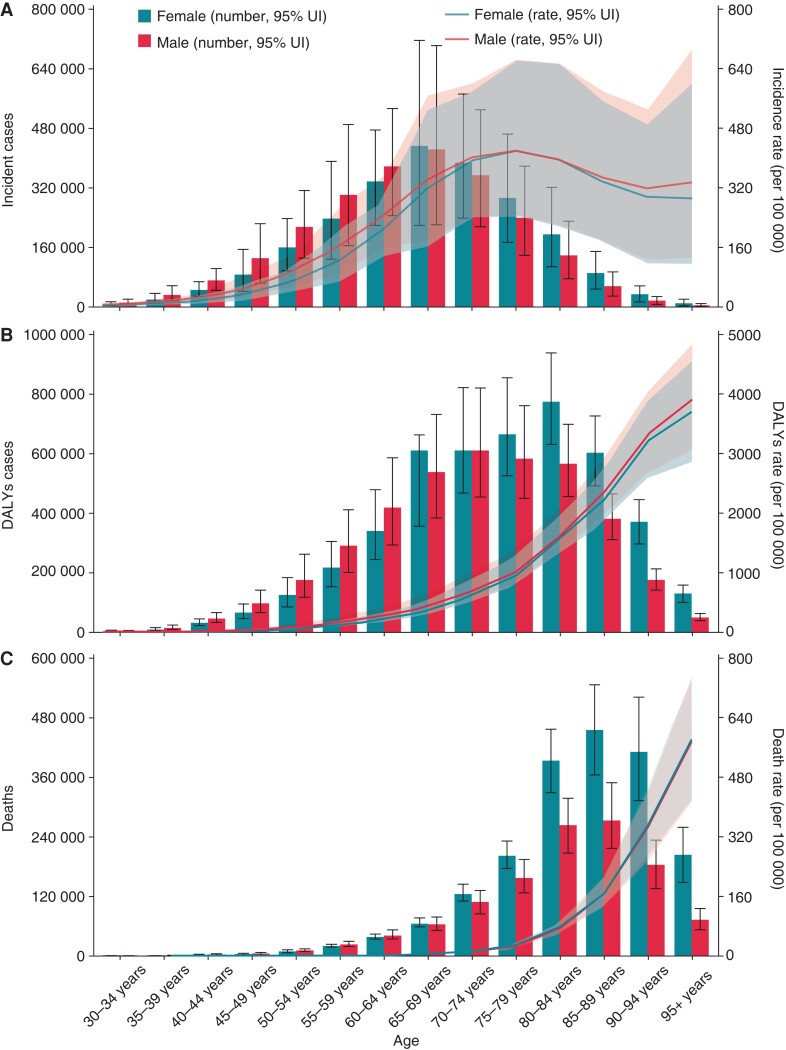
Age-specific counts and rates of incident cases, DALY cases, and deaths for AF/AFL by sex in 2019 were shown in Figure 2. The incident cases of AF/AFL peaked betweeen the 65–69 years in both sexes, with higher incident cases in males aged younger than 65 years and in females aged older than 65 years (Figure 2A). The number of DALYs due to AF/AFL peaked at between the 70–74 years in males and between the 80–84 years in females, and the number was higher in males than in females in the same age group until the 70–74 years (Figure 2B). The number of deaths due to AF/AFL peaked between the 85–89 years in both sexes, and females in the same age group have more deaths than males after the 65–69 years. The age-specific DALYs and death rates of AF/AFL increased with age in both sexes. However, the age-specific incidence rate decreased after the 75–79 years in both sexes.
Figure 2.
Age-specific numbers and rates of incident cases (A), disability-adjusted life years cases (B), and deaths (C) of atrial fibrillation/atrial flutter by sex, 2019. Error bars indicate the 95% uncertainty interval (UI) for numbers. Shading indicates the 95% UI for rates.
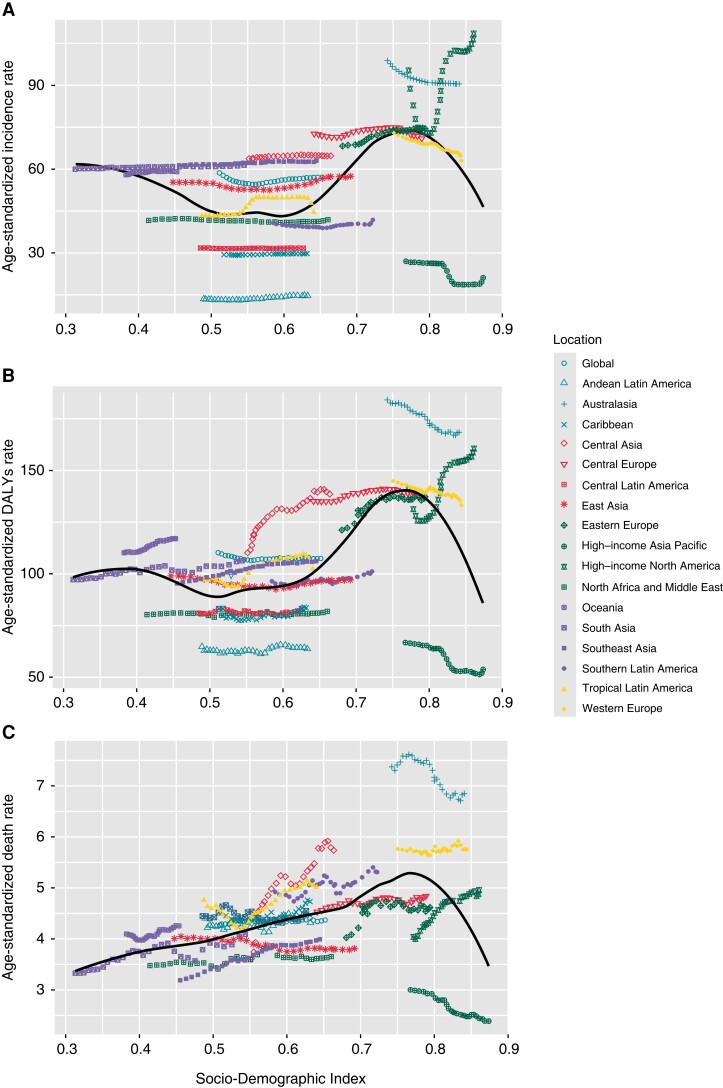
By SDI quintile, in 2019, age-standardized incidence, DALYs, and death rates of AF/AFL tended to be higher in regions (except for high-income Asia Pacific) in the higher SDI quintile, whereas the opposite results were seen in regions with in the low SDI quintile and high-income Asia Pacific (Table 1, Figure 3). From 1990 to 2019, ASRs of incidence, DALYs, and deaths of AF/AFL showed stable trends at the lower end of the SDI scale, whereas the largest increase and the largest decrease were all observed at the higher end of the SDI scale. Across 21 GBD regions, in 2019, the highest age-standardized incidence rate of AF/AFL was seen in high-income North America [108.5 (95% UI: 87.6 to 131.4) per 100 000 people], whereas the lowest age-standardized incidence rate was observed in Andean Latin America [14.8 (95% UI: 11.1 to 19.2) per 100 000 people] (Table 1, Figure 3A). The highest age-standardized DALYs [168.3 (95% UI: 132.5 to 214.3) per 100 000 people] and deaths [6.9 (95% UI: 5.5 to 8.3) per 100 000 people] rates were observed in Australasia, whereas the lowest ASRs of DALYs [53.5 (95% UI: 43.1 to 66.6) per 100 000 people] and deaths [2.4 (95% UI: 1.9–3.2) per 100 000 people] were seen in high-income Asia Pacific (Table 1, Figure3B and C). From 1990 to 2019, The largest drop and the largest rise in age-standardized incidence rate were seen in high-income Asia Pacific [−21.5% (95% UI: −23.4 to −11.8)] and high-income North America1 [3.9% (95% UI: 5.1 to 19.1)], respectively (Table 1, Figure 3A). The largest drop in age-standardized DALYs [−0.2% (95% UI: −0.2 to −0.1)] and death [−20.5% (95% UI: −30.3 to −11.5)] rates were all observed in the high-income Asia Pacific, whereas the largest rise in age-standardized DALYs [0.3% (95% UI: 0.1 to 0.4)] and death [58.7% (95% UI: 15.7 to 97.4)] rates were seen in Central Asia (Table 1, Figure 3B and C ).
Figure 3.
Trend in age-standardized incidence (A), disability-adjusted life years (B), and death (B) rates of atrial fibrillation/atrial flutter globally and for 21 GBD regions by socio-demographic index, 1990–2019. For each region, points from left to right depict estimates from each year from 1990 to 2019. GBD, Global Burden of Disease, Injuries, and Risk Factors Study.
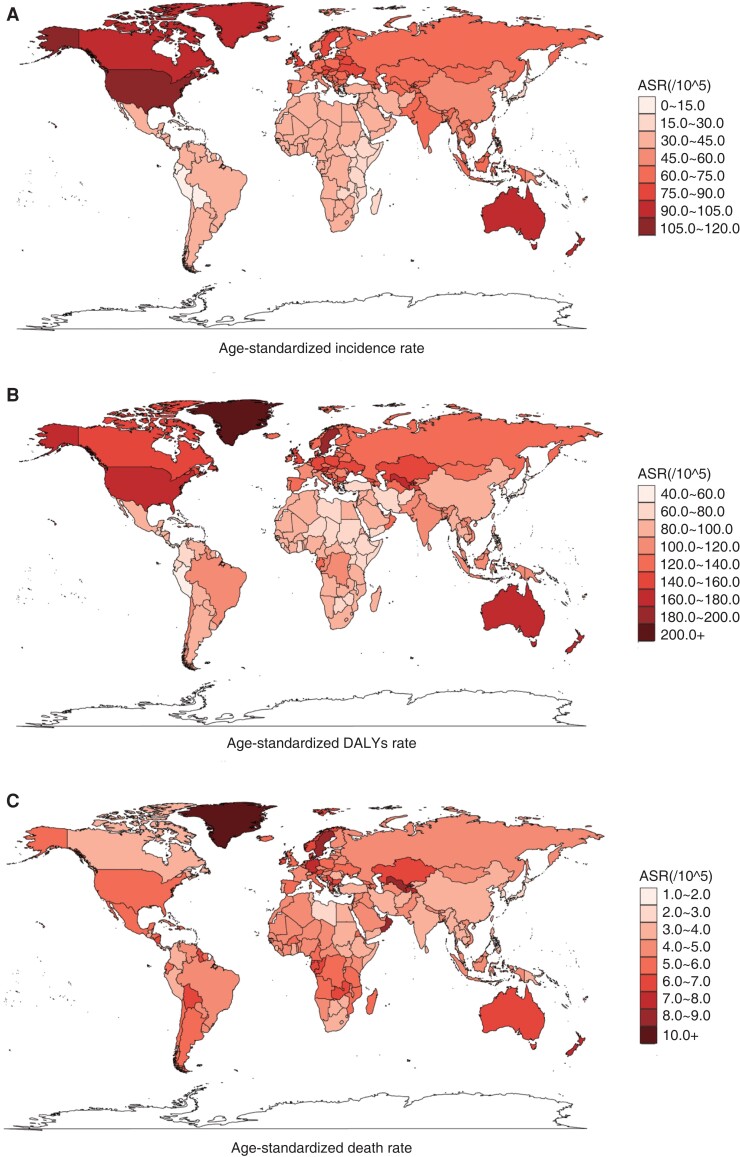
Across all countries, in 2019, the USA had the global highest age-standardized incidence rate [109.5 (95% UI: 89.0 to 131.9) per 100 000 people], while Bolivia (Plurinational State of) had the lowest age-standardized incidence rate [14.4 (95% UI: 10.7 to 18.7) per 100 000 people]. The global highest age-standardized DALYs [250.6 (95% UI: 205.8 to 313.7) per 100 000 people] and death [14.4 (95% UI: 11.3 to 19.4) per 100 000 people] rates of AF/AFL were seen in Montenegro, whereas the lowest age-standardized death [2.0 (95% UI: 1.4 to 2.4) per 100 000 people] and DALYs [51.9 (95UI: 40.1 to 67.0)] rates were observed in Singapore (Figure 4 and Supplementary material online, Table S1). From 1990 to 2019, the countries with the largest drop in age-standardized incidence, death, and DALYs rates were seen in Japan [−25.8% (95% UI: −28.2 to −22.4)], Guam [−47.3% (95% UI: −59.6 to −31.9)] and Bermuda [−20.7% (95% UI: −31.1 to −7.7)]. While the countries with the largest rise in age-standardized incidence, death and DALYs rates were seen in Ecuador [22.5% (95% UI: 13.4 to 31.9)], Uzbekistan [211.3% (95% UI: 69.6 to 347.1)] and Uzbekistan [75.0% (95% UI: 37.7 to 120.4)], respectively (Figure 4 and Supplementary material online, Table S1). Notably, China had the global largest number of incident cases [1.2 million (95% UI: 0.9 to 1.5)], DALYs cases [1.7 million (95% UI: 1.3 to 2.2)], and deaths [51.7 thousand (95% UI: 43.6 to 60.1)] due to AF/AFL in 2019. Compared with other countries, from 1990 to 2019, the global number of DALYs and deaths due to AF/AFL had the largest increase in China, increasing by ∼121.6% (95% UI: 111.5 to 132.0) and 169.4% (95% UI: 143.8 to 189.2), respectively.
Figure 4.
Age-standardized incidence (A), DALYs (B), and death (C) rates of is atrial fibrillation /atrial flutter across 195 countries and territories for both sexes, 2019. DALYs, disability-adjusted life years.
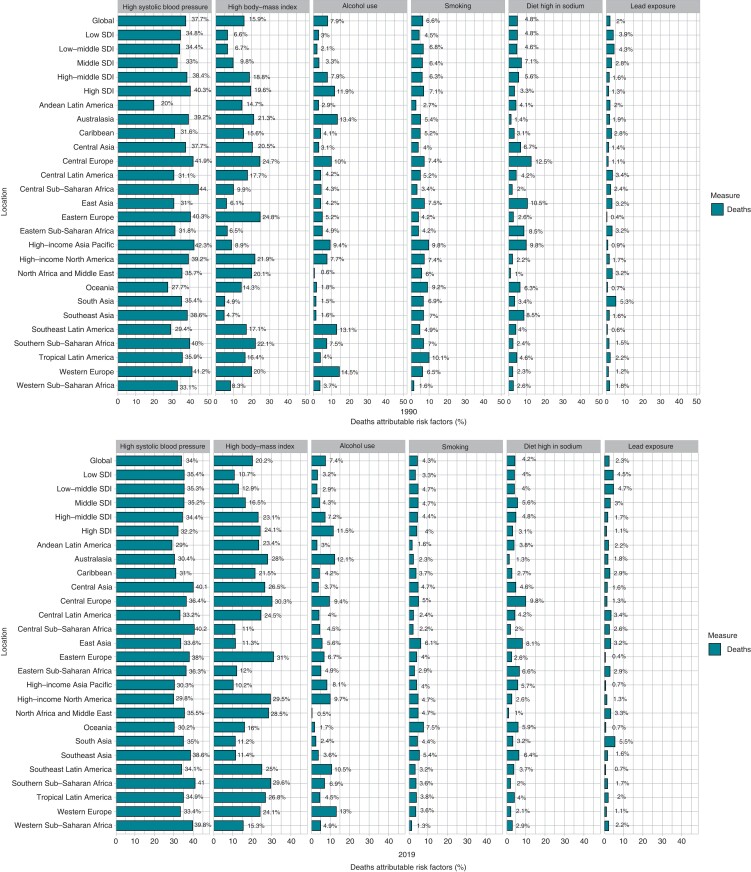
Among all potential risk factors in GBD 2019, age-standardized AF/AFL death worldwide was primarily attributable to high systolic blood pressure [34.0% (95% UI: 27.3 to 41.0)], followed by high body mass index [20.2% (95% UI: 11.2 to 31.2)], alcohol use [7.4% (95% UI: 5.8 to 9.0)], smoking [4.3% (95% UI: 2.9 to 5.9)], diets high in sodium [4.2% (95% UI: 0.8 to 10.5)], and lead exposure [2.3% (95% UI: 1.3 to 3.4)]. The percentage contribution of these risk factors to age-standardized AF/AFL death by gender, SDI quintile, and GBD region were shown in Figure 5 and Supplementary material online, Table S2. With the exception of a few regions, the percentage contribution of high body mass index and high systolic blood pressure to AF/AFL age-standardized death affected females more than males. Conversely, the percentage contribution of smoking, lead exposure and alcohol use to age-standardized AF/AFL death affected males more than females. For diets high in sodium, in addition to Eastern Sub-Saharan Africa, the percentage contribution of age-standardized AF/AFL death also affected males more than females. Across SDI quintiles, the contribution percentage of high systolic blood pressure, high sodium diet, and smoking to age-standardized AF/AFL death was similar in each SDI. The largest percentage contribution of high body mass index and alcohol use to age-standardized AF/AFL death was seen in countries in high–middle SDI quintile and high SDI quintile in both sexes. Conversely, the largest percentage contribution of lead exposure to age-standardized AF/AFL death was observed in countries in the low SDI quintile and low–middle SDI quintile. Globally, from 1990 to 2019, the percentage contribution of high body mass index and lead exposure to age-standardized AF/AFL death trended upwards in both sexes, while other risk factors trended downwards in both sexes.
Figure 5.
Percentage contributions of major risk factors to age-standardized death of atrial fibrillation/atrial flutter, 1990–2019. SDI, Socio-Demographic Index.
Discussion
Our results indicated that AF/AFL remains a significant health burden globally, with more than 60.0 million AF/AFL survivors in 2019. Although the age-standardized incidence and prevalence rates of AF/AFL declined from 1990 to 2019, its absolute number has more than doubled, possibly due to population growth and aging, advanced diagnostic techniques, and increased awareness of AF/AFL. The absolute number of AF/AFL deaths and DALY cases has also increased significantly, possibly attributable to undiagnosed asymptomatic or paroxysmal AF/AFL and lack of standardized treatment for AF/AFL. Notably, our results showed that DALYs cases and deaths of AF/AFL increased faster than the prevalent cases and incident cases. Therefore, it is not only necessary to detect AF/AFL as early as possible, but also urgently to develop more effective treatment measures to actively treat AF/AFL.
Consistent with GBD 2017 analysis3,4 of AF/AFL, our results also indicated that the number of AF/AFL-related DALYs and deaths was higher in females than in males in 2019, whereas the opposite result was seen in AF/AFL-related incidence. Recent studies2,12,13 have shown that females have more complications and mortality due to AF/AFL than males, and female patients are less likely to use rhythm control strategies, including less antiarrhythmic therapy, less cardioversion, and less catheter ablation. Therefore, more attention should be paid to rhythm control strategies and complications treatment in females with AF/AFL. A 50-year follow-up study found that age was the strongest risk factor for developing AF/AFL compared with sex, smoking, alcohol, hypertension, body mass index, significant heart murmur, left ventricular hypertrophy, myocardial infarction, and heart failure. As shown in our study, the incidence of AF/AFL peaked in the elderly. Notably, the rates of AF/AFL-related death and DALYs have risen sharply in the elderly, suggesting that the management of AF/AFL in the elderly is far from adequate. Unlike the analysis of AF/AFL in GBD 2017,3,4 our results showed incidence and death rates of AF/AFL tend to be younger in females. Therefore, while focusing on AF/AFL in the elderly, the diagnosis and treatment of AF/AFL in young women should not be ignored.
Similar to GBD 2017 analysis of AF/AFL,3,4 the temporal trends in the age-standardized incidence, DALYs, and death rates of AF/AFL varied significantly by SDI quintile. Socio-Demographic Index is mainly composed of years of education, per capita income level, and total fertility rate. Therefore, social factors have an important influence on the age-standardized incidence, DALYs and death rates, and changes in AF/AFL. Regions should formulate corresponding strategies according to their own situation. High SDI regions had a higher age-standardized incidence rate, while low SDI regions had lower age-standardized incidence rate, suggesting that a larger proportion of people in low SDI regions had undetectable AF/AFL. Therefore, more patients with AF/AFL, especially those with paroxysmal or asymptomatic AF/AFL, are diagnosed early and accurately. Age-standardized incidence, DALYs, and death rates increased in regions with low SDI regions. This may be attributable to treatment strategies, including the use of new oral anticoagulants, left atrial appendage closure, and catheter or cryogenic balloon ablation, which are unevenly distributed across socioeconomic settings in different regions. Although the age-standardized incidence and DALY rates decreased significantly in the high SDI region, the age-standardized death rate increased significantly in the low SDI region. In recent years, we have made great achievements in the AF/AFL burden of high SDI areas, but we have neglected the AF/AFL management of low SDI areas. In the future, we need to strengthen the prevention, diagnosis, and treatment of AF/AFL in low SDI areas.
A series of literature reviews showed that active management of AF/AFL modifiable factors, such as hypertension, obesity, smoking, and alcohol abuse, can prevent AF/AFL14,15 and improve its prognosis.16 Therefore, a variety of efforts are still needed to prevent and treat these risk factors. Previous studies have shown that obesity is an independent predictor of AF/AFL in healthy fertile young women,17 and obesity is strongly associated with diabetes and hypertension.18 Therefore, obesity in adults are at the highest risk of developing AF/AFL. A meta-analysis19 of 4 371 714 participants showed that AF/AFL was associated with all-cause mortality in females. Therefore, in order to reduce the percentage contribution of high body mass index and high systolic blood pressure to age-standardized AF/AFL death in females.
Policymakers should not only prevent females from developing high body mass index and high systolic blood pressure as soon as possible but also regulate the management of AF/AFL in females. Smoking, diets high in sodium, and alcohol use usually represent an unhealthy lifestyle in males, and lead exposure represents a poor working environment in males. Males should try to avoid these risk factors to decrease the percentage contribution to age-standardized AF/AFL death. Previous GBD studies3 found the percentage contribution of these risk factors to age-standardized AF/AFL death was mainly seen in countries with high–middle SDI quintile. The present study showed that the percentage contribution of these risk factors to age-standardized AF/AFL death was observed in countries with each SDI. Thus, we should pay attention to the risk factors of each SDI quintile.
Limitations
The limitations of our study have to be discussed. First, although the ICD codes were widely accepted for obtaining information on AF/AFL cases, and the GBD 2019 methods have made great efforts to improve data quality, it may still affect the accuracy of in some cases. Second, despite improved diagnostic tools for AF/AFL, the large number of undiagnosed asymptomatic or paroxysmal AF/AFL in the population would lead us to underestimate the number of AF/AFL. Third, there are different types of AF/AFL, such as paroxysmal AF/AFL, persistent AF/AFL, and permanent AF/AFL, the GBD database does not recognize this complexity, only whether the population has AF/AFL classification. Finally, we only analysed the main risk factors associated with AF/AFL, and other risks of AF/AFL cannot be ignored.
Conclusions
Our study showed the burden of AF/AFL in 2019 and their temporal trends from 1990 to 2019 varied widely by gender, Socio-Demographic Index (SDI) quintile, and geographical location. Despite the advancements in the prevention and treatment of AF/AFL, especially in regions in relatively high SDI quintiles, the burden of AF/AFL in regions in the lower SDI is increasing. Since AF/AFL is largely preventable and treatable, there is an urgent need to implement more cost-effective strategies and interventions to address modifiable risk factors, especially in regions with high or increased AF/AFL burden.
Supplementary Material
Acknowledgements
The authors would like to thank all members of the Institute for Health Metrics and Evaluation (IHME) and all collaborators involved in GBD 2019 study.
Contributor Information
Xin-Jiang Dong, Department of Cardiology, Shanxi Cardiovascular Hospital, Yifen Road, Wanbailin District, Taiyuan 030000, China.
Bei-Bei Wang, Department of Cardiology, The First People’s Hospital of Jinzhong, Shuncheng Road, Yuci District, Jinzhong 030600, China.
Fei-Fei Hou, Department of Intensive Care Unit, Affiliated of Inner Mongolia Medical University, Tongdao North Road, Huimin District, Huhehaote 010000, China.
Yang Jiao, Department of Interventional Radiology, Shaanxi Provincial People’s Hospital, Youyi West Road, Beilin District, Xian 710000, China.
Hong-Wei Li, Department of Cardiology, Shanxi Cardiovascular Hospital, Yifen Road, Wanbailin District, Taiyuan 030000, China.
Shu-Ping Lv, Department of Cardiology, Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, Longcheng Road, Xiaodian District, Taiyuan 030032, China.
Fei-Hong Li, Department of Cardiology, Yantai Yeda Hospital, Taishan Road, Fushan District, Yantai 265599, China.
Supplementary material
Supplementary material is available at Europace online.
Authors’ contribution
X.-J.D. and B.-B.W. wrote the main manuscript text; F.-F.H. and Y.J. collected the data; H.-W.L., S.-P.L., and F.-H.L. prepared figures and tables; and all authors approved the manuscript.
Data availability
The data underlying this article were derived from sources in the public domain: Institute for Health Metrics and Evaluation, at http://ghdx.healthdata.org/gbd-results-tool, accessed on May 2022.
References
- 1. Ruddox V, Sandven I, Munkhaugen J, Skattebu J, Edvardsen T, Otterstad JE. Atrial fibrillation and the risk for myocardial infarction, all-cause mortality and heart failure: a systematic review and meta-analysis. Eur J Prev Cardiol 2017;24:1555–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stewart S, Hart C, Hole D, McMurray J. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med 2002;113:359–64. [DOI] [PubMed] [Google Scholar]
- 3. Dai H, Zhang Q, Much A, Maor E, Segev A, Beinart R. Global, regional, and national prevalence, incidence, mortality, and risk factors for atrial fibrillation, 1990–2017: results from the Global Burden of Disease Study 2017. Eur Heart J Qual Care Clin Outcomes 2021;7:574–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wang L, Ze F, Li J, Mi L, Han B, Niu H. Trends of global burden of atrial fibrillation/flutter from Global Burden of Disease Study 2017. Heart 2021;107:881–7. [DOI] [PubMed] [Google Scholar]
- 5. Naccarelli G, Varker H, Lin J, Schulman KL. Increasing prevalence of atrial fibrillation and flutter in the United States. Am J Cardiol 2009;104:1534–9. [DOI] [PubMed] [Google Scholar]
- 6. Krijthe B, Kunst A, Benjamin E, Lip G, Franco O, Hofman A. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur Heart J 2013;34:2746–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wolowacz S, Samuel M, Brennan V, Jasso-Mosqueda J, Gelder I. The cost of illness of atrial fibrillation: a systematic review of the recent literature. Europace 2011;13:1375–85. [DOI] [PubMed] [Google Scholar]
- 8. GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England) 2020;396:1204–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Roth G, Mensah G, Johnson C, Addolorato G, Ammirati E, GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol 2020;76:2982–3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet (London, England) 2020;396:1223–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo Cet al. . The trends in incidence of primary liver cancer caused by specific etiologies: results from the Global Burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol 2019;70:674–83. [DOI] [PubMed] [Google Scholar]
- 12. Westerman S, Wenger N. Gender differences in atrial fibrillation: a review of epidemiology, management, and outcomes. Curr Cardiol Rev 2019;15:136–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tian X, Xu Y, Yang Y. Gender differences in arrhythmias: focused on atrial fibrillation. J Cardiovasc Transl 2020;13:85–96. [DOI] [PubMed] [Google Scholar]
- 14. Allan V, Honarbakhsh S, Casas J, Wallace J, Hunter R, Schilling Ret al. . Are cardiovascular risk factors also associated with the incidence of atrial fibrillation? A systematic review and field synopsis of 23 factors in 32 population-based cohorts of 20 million participants. Thromb Haemost 2017;117:837–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gorenek B, Pelliccia A, Benjamin E, Boriani G, Crijns H, Fogel Ret al. . European Heart Rhythm Association (EHRA)/European Association of Cardiovascular Prevention and Rehabilitation (EACPR) position paper on how to prevent atrial fibrillation endorsed by the Heart Rhythm Society (HRS) and Asia Pacific Heart Rhythm Society (APHRS). Europace 2017;19:190–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Middeldorp M, Ariyaratnam J, Lau D, Sanders P. Lifestyle modifications for treatment of atrial fibrillation. Heart 2020;106:325–32. [DOI] [PubMed] [Google Scholar]
- 17. Karasoy D, Jensen T, Hansen M, Schmiegelow M, Lamberts M, Gislason Get al. . Obesity is a risk factor for atrial fibrillation among fertile young women: a nationwide cohort study. Europace 2013;15:781–6. [DOI] [PubMed] [Google Scholar]
- 18. Grundvold I, Bodegard J, Nilsson P, Svennblad B, Johansson G, Östgren C. Body weight and risk of atrial fibrillation in 7,169 patients with newly diagnosed type 2 diabetes; an observational study. Cardiovasc Diabetol 2015;14:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Emdin C, Wong C, Hsiao A, Altman D, Peters S, Woodward Met al. . Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: systematic review and meta-analysis of cohort studies. BMJ 2016;532:h7013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article were derived from sources in the public domain: Institute for Health Metrics and Evaluation, at http://ghdx.healthdata.org/gbd-results-tool, accessed on May 2022.