Abstract
Older adults with a chronic health condition (e.g., hypertension) use various self-management methods. Healthcare technologies have the potential to support health self-management. However, it is necessary to understand the acceptance of these technologies as a precursor to older adults’ adoption and integration into their health plan. Our focus was on the factors older adults with hypertension initially consider when introduced to three new healthcare technologies that might support their health self-management. We compared their considerations for a blood pressure monitor, an electronic pillbox, and a multifunction robot to simulate incrementally more complex technologies. Twenty-three participants (aged 65–84) completed four questionnaires and a semi-structured interview. The interview transcripts were analyzed using a thematic analysis approach. We identified the factors that were frequently mentioned among the participants for each of the three healthcare technologies. The factors that older adults initially considered were familiarity, perceived benefits, perceived ease of use, perceived need for oneself, relative advantage, complexity, and perceived need for others. Upon further reflection, participants considered advice acceptance, compatibility, convenience, facilitating conditions, perceived usefulness, privacy, subjective norm, and trust. We integrated the factors that older adults considered into the Healthcare Technology Acceptance Model (H-TAM), which elucidates the complexity of healthcare technology acceptance and provides guidance for future explorations.
Keywords: healthcare technology, older adults, technology acceptance
Introduction
Imagine Mrs. S, who is 85 years old, has hypertension, and her doctor has recommended that she manage her health by using a technology that can support her health self-management. What will influence her willingness to accept or not accept this new healthcare technology? Mrs. S. forms a behavioral intention that is likely influenced by numerous factors. She may decide to try it, decide not to try it, or decide to obtain more information. Knowing what she considers can provide insights for introducing new technologies into the lives of older adults.
Behavioral intentions are defined as, “indications of how hard people are willing to try, of how much of an effort they are planning to exert, in order to perform the behavior” (Ajzen, 1991: 181). The stronger the behavioral intentions are, the more likely the person is to engage in that behavior later. Intentions to accept are the first step towards the adoption of the technology. As such, behavioral intentions are included in models and theories related to the acceptance of a specific behavior (Ajzen, 1991; Davis, 1989; Venkatesh and Morris 2005) across time (Lee, Kozar and Larsen, 2003) and disciplines (King and He, 2006).
The Technology Acceptance Model (TAM; Davis, 1989) was one of the original models that focused on how perceived usefulness, perceived ease of use, and social norm influenced the acceptance of information systems. Since the development of this model, there have been many extensions across different technologies (Kim and Garrison, 2009; Lee and Lehto, 2013). The Unified Theory of Acceptance and Use of Technology (UTAUT; Venkatesh et al., 2003) is an extension of TAM that unified eight different models and theories (e.g., Theory of Planned Behavior, Social Cognitive Theory, Diffusion of Innovations Theory). Venkatesh and colleagues (2012) later developed UTAUT2, which added hedonic motivation, price value, and habit as predictors of technology acceptance. The TAM, UTAUT, and UTAUT2 were developed and validated primarily in the context of accepting an information system by consumers, with limited inclusion of different technologies by older adults.
With the increasing number of older adults worldwide (United States Department of Health and Human Services, 2018), it is essential to understand what will influence their intentions to accept new technologies, given that information and computing technologies are becoming more pervasive. The Senior Technology Acceptance Model (STAM; Chen and Chan, 2014) focused on older adults’ acceptance of gerontechnology and extended previous models and theories of acceptance. Chen and Chan (2014: 636) defined gerontechnology as, “…electronic or digital products or services that can increase independent living and social participation of older persons in relatively good health, comfort, and safety” (Chen and Chan, 2014: 636). In other words, the technology used in older adults’ daily lives. The categories of technologies studied were housing and daily living technology; community technology; education and recreation technology; and healthcare technology. Although the STAM focused on older adults, it did not expand on the acceptance of healthcare technologies specifically, nor did it systematically assess the role of the novelty and complexity of the technologies.
In the United States, many older adults are managing at least one chronic health condition (National Council on Aging, 2017). In our example of Mrs. S., she has hypertension, which is known as the silent killer and is one of the leading preventable chronic conditions among older adults (National Council on Aging, 2017). A health behavior change can support older adults with the self-management of hypertension (e.g., properly taking medications and knowing blood pressure numbers; American Heart Association, 2017). Additionally, healthcare technologies could also support older adults in the self-management of their hypertension. However, technology tools will only be useful if older adults are willing to use them.
Exemplar factors of older adults’ acceptance of technologies are cognition (Chen and Chan, 2011; Czaja et al., 2006), ease of learning and use (Renaud and Biljon, 2008), and perceived cost (Lee and Coughlin, 2015). However, these studies did not focus specifically on healthcare technologies, for which other factors may influence acceptance. One example is the role of advice acceptance.
The term ‘advice acceptance’ in communication sciences was defined by D’Angelo & D’Angelo (2018: 198) as “Recommendation for action in response to a problem.”. Advice acceptance may be particularly relevant to health behavior changes, and perhaps healthcare technology acceptance, given the tradition of relying on healthcare providers for health-related decisions. Moreover, people may be more likely to ask other people for advice (e.g., family and friends) related to health decisions that can affect the advice recipient’s longevity.
For individuals with chronic and preventable diseases such as hypertension, if advice is given to them properly, and it is accepted, they may improve their health behaviors (D’Angelo and D’Angelo, 2018). Although advice acceptance has been shown to affect health behaviors, it has not been incorporated into theories of technology acceptance, nor has it been studied in the context of healthcare technologies. Therefore, the goals of the present study were to address the following research questions:
- What are older adults’ initial considerations about new healthcare technologies?
- Do their considerations change depending on the complexity of the technology?
Upon further reflection, what are the additional considerations that older adults mention when deciding whether to adopt a healthcare technology?
We provided participants with scenarios to simulate a situation wherein they might be faced with deciding whether to use healthcare technology. We recruited participants who had been diagnosed with hypertension and described three different technologies varying in complexity that might support their health self-management (a new blood pressure monitor, an electronic pillbox, or a multifunction robot). We then asked them a series of interview questions designed to elicit their willingness to try these technologies. The questions probed a subset of the UTAUT2 model as well as aspects of advice acceptance. We included price value to understand whether the participants would be interested in buying the technology and their perceptions of cost. We did not include hedonic motivation and habit due to the scope of the study.
Method
Participants
A sample of 24 older adults (65 to 84), 16 females and 7 males, was recruited over the phone from the Illinois Health and Engagement through the Lifespan Project (I-HELP; central Illinois) participant registry and the TechSAge Rehabilitation Engineering Research Center participant registry (greater Atlanta area). Participants were prescreened to ensure that they met the following inclusion criteria: fluent in English, lived independently, self-reported diagnosis of hypertension, and a score of twenty-one or higher on the Modified Telephone Interview for Cognitive Status (TICS-M; de Jager, Budge and Clarke, 2003). One participant was removed due to an incomplete audio recording of the interview.
Materials
The ten-item Technology Readiness Index 2.0 (TRI 2.0; Parasuraman and Colby, 2014) measured one’s readiness to embrace new technology using a five-point Likert scale (1= strongly disagree, and 5= strongly agree). The 36-item Technology Experience Profile (TEP; Barg-Walkow, Mitzner, and Rogers, 2014) assessed the participants’ familiarity and experience with everyday technologies within the last 12 months on a five-point Likert scale (1= not sure and 5=used frequently). The Demographics and Health Questionnaire (Czaja et al., 2006) collected information about the participants’ general demographic information (e.g., age, sex, ethnicity, living arrangement), occupational status, and general subjective health. Lastly, the 18-item Multi-Dimensional Health Locus of Control Form C (MHLC-C; Wallston, Stein and Smith, 1994) assessed health/medical condition beliefs about their control over their illness or disease. Participants were asked to circle a number representing their agreement on a six-point Likert scale (1=strongly disagree, and 6=strongly agree).
The healthcare technology acceptance semi-structured interview script was developed by the research team for this study to assess opinions and beliefs regarding factors related to acceptance of healthcare technologies (the full script is available from the authors; for more details, see Author, 2019). The interview script consisted of three scenarios related to the description of three healthcare technologies (i.e., a blood pressure monitor, electronic pillbox, and a multifunctional robot; see Figure 1). The least complex technology was the blood pressure monitor. The purpose of the blood pressure monitor was to take one’s blood pressure and record the numbers shown. The next-most complex was the electronic pillbox focused on administering medication and reminding the user to take it at a time that they previously set. The multifunctional healthcare robot was the most complex healthcare technology out of the three and could distribute medication and check one’s blood pressure. Each healthcare technology included different aspects of self-managing hypertension based on the novelty and/or complexity (set up) of the technology. Questions included in the interview script were asked for each of the three healthcare technologies to understand older adults’ intentions to accept a new healthcare technology and to learn of any factors that may be important to older adults and healthcare technology acceptance.
Figure 1.
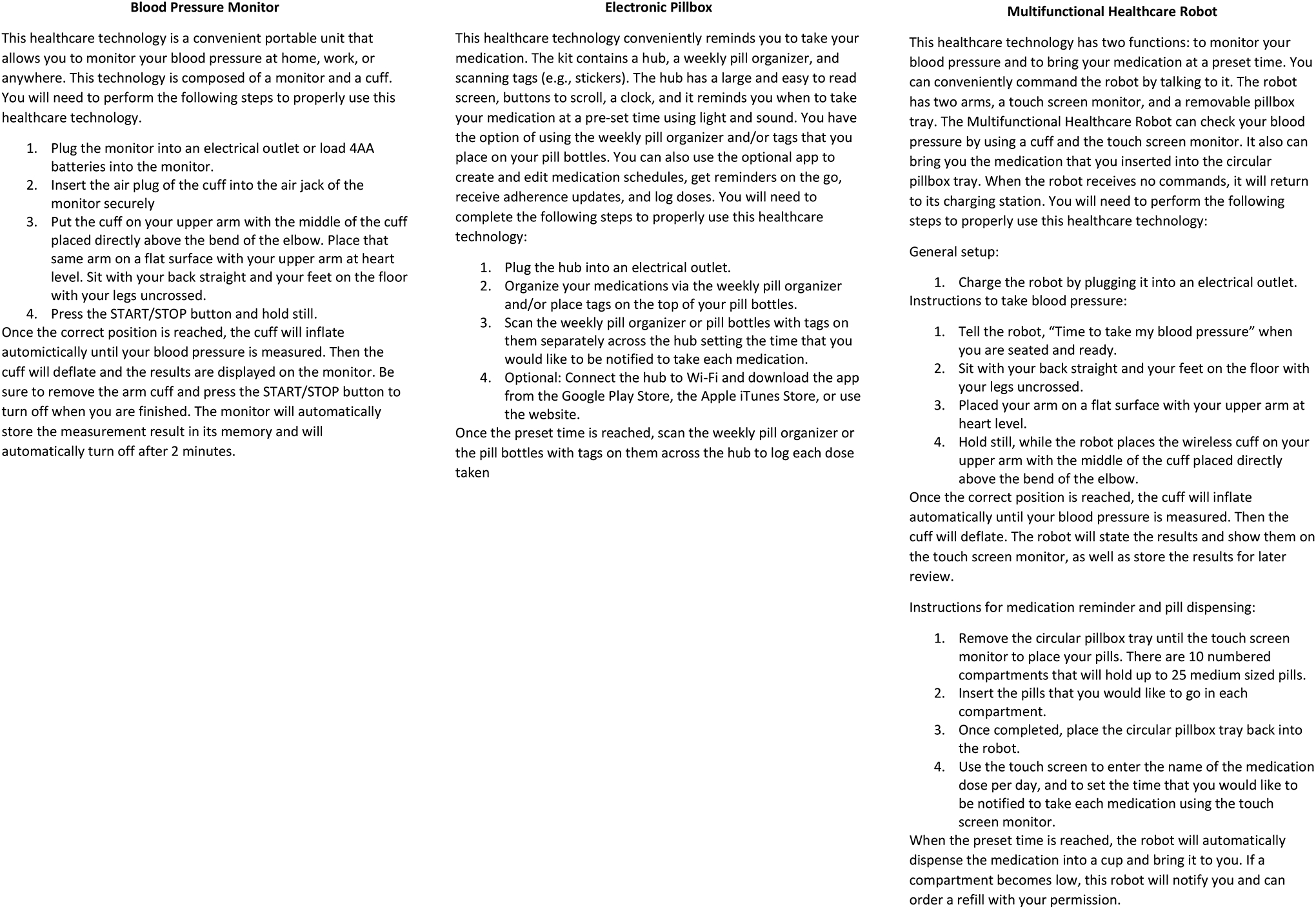
Descriptions of Healthcare Technologies Provided To Participants
Procedure
Participants were scheduled for in-person or remote interviews based on their preference. This study lasted for 1.5 hours for both in-person and remote interviews. In-person interview participants provided informed consent then completed two questionnaires (i.e., TRI 2.0 and TEP), the semi-structured interview, a 5-minute break, and then the remaining questionnaires (i.e., Demographics and Health; MHLC-C). Remote participants were sent an email containing a link to Qualtrics, an online survey company, to provide their informed consent. Once the informed consent form was signed, participants were able to complete all four questionnaires using Qualtrics. Once completed, the research team contacted participants to schedule the telephone interview.
Each interview was conducted by one research member, audio-recorded to be transcribed, and analyzed later. During the interview, in-person participants were given a written description of the healthcare technology to follow the scenario as the interviewer read the description aloud. Remote participants were sent an email before the semi-structured interview that included the three descriptions of the healthcare technologies to read during the interview. To control for order effects, the discussion of the technologies was counterbalanced across participants.
Prior to the interview, the interviewer confirmed that the recorder was being turned on with the interviewee. During the interview, the researcher read the description of the technology, followed by the participant reviewing the description at their own pace. Once the participant finished reviewing the description, the researcher asked questions from the interview script. Additionally, the interviewer used general probes when necessary to elicit more information from the participants (e.g., “What makes you feel this way?”). The recorder was turned off once the interview was completed. Once all parts of the study were completed, participants were compensated via an Amazon gift card for their time and debriefed.
Qualitative data analysis
The analysis of the qualitative data in this study was conducted by a three-member coding team, composed of a primary coder and two secondary coders to minimize research bias. Each member had a background in applied health, focusing on utilizing technology to support older adults.
The recorded audio files from each interview were transcribed using Scribie, a website tool that transcribes audio/video files, and then checked for accuracy by the coding team. Once the transcriptions were completed, the coding team used MAXQDA, a qualitative and mixed methods data analysis software, to segment the transcripts and later applied the coding scheme.
The coding scheme utilized for this study was developed using a combined conceptually driven and data-driven approach to capture factors from the literature as well as factors that emerged from the interviews with the participants (Mitzner, Bixter, and Rogers, 2016). The primary coder reviewed the technology acceptance literature to develop the preliminary codes and subcodes using a top-down approach. Once completed, the primary coder segmented the transcripts into units of analysis.
The unit of analysis was a complete response of one question, referred to as a segment. During the coding process, each segment was coded based on the pre-defined subcodes. Researchers extracted the message delivered in each segment and matched it to the most appropriate sub-codes. A segment could be coded into one or more subcodes, depending on the relatability of the content to the subcodes definition. On the other hand, if no part of the segment related to any subcodes definition or the segment was too general, it was coded under ‘other’ or ‘general.’
For reliability purposes with coding, MAXQDA calculated inter-rater reliability using Cohen’s Kappa, which represents the percentage of agreement between the primary coder and the secondary coders (Brennan and Prediger, 1981). The research team conducted rounds of independent coding on two randomly selected transcripts until inter-rater reliability of 80 per cent or higher was achieved between the primary coder and the two secondary coders. According to Banerjee and colleagues (1999), an agreement above 75 per cent represents excellent agreement beyond chance.
During the independent coding rounds, the coding team discussed any discrepancies that resulted in a low inter-rater reliability percentage and adapted the coding scheme as needed. Throughout this discussion, the coding team used a data-driven approach to develop an exhaustive list of codes and subcodes previously noted in the preliminary list. Also, they combined similar codes and subcodes that emerged during the development of the coding scheme.
Once inter-rater reliability above 80 per cent was achieved among the coding team, transcripts were divided and coded independently. The primary coder analyzed 14 transcripts, and the two secondary coders each analyzed seven transcripts. Additional details and the complete coding scheme are provided in Author (2019); here, we focus on a subset of the data.
Results
Participant Characteristics
The characteristics of the 23 older adults (mean age 75; SD=4.18) are presented in Table 1. On average, participants noted that they were not sure what the health technologies (i.e., medication reminder device and health management software) listed in the TEP were. Overall, participants felt optimistic about technology (positive benefits). However, they also felt innovative (wanting to experiment, learn, and talk about the technology), discomfort (perceived lack of control), and insecure (technology can result in adverse impacts) on average.
Table 1.
Participant Demographics and Health Descriptive Information
| Factor | Options | Frequency or Mean | SD |
|---|---|---|---|
| Demographics | Frequency | ||
| Sex | Female | n = 16 | |
| Male | n = 7 | ||
| Race | Black/African American | n = 1 | |
| White/Caucasian | n = 22 | ||
| Education | Less than high school graduate | n = 1 | |
| High school graduate/GED | n = 5 | ||
| Some or in-progress college/Associates degree | n = 3 | ||
| Bachelor’s degree (BA/BS) | n = 5 | ||
| Master’s degree | n = 6 | ||
| Doctoral degree | n = 3 | ||
| Yearly Household Income | Less than $25,000 | n = 6 | |
| $25,000–$49,999 | n = 7 | ||
| $50,000–$74,999 | n = 4 | ||
| $75,000 or more | n = 4 | ||
| Do not wish to answer | n = 2 | ||
| Background Questionnairea | Mean | SD | |
| General Health | “In general, would you say your health is…” | M= 3.44 | 0.75 |
| Health Compared to Others | “Compared to other people your own age, would you say your health is…” | M= 3.61 | 0.72 |
| Technical Readiness Index 2.0b | Mean | SD | |
| Optimism | M=3.88 | 1.21 | |
| Innovativeness | M=2.92 | 1.18 | |
| Discomfort | M=3.12 | 1.26 | |
| Insecurity | M=3.44 | 1.17 | |
| Multidimensional Health Locus of Control – Form Cb | Mean | SD | |
| Internal | M=24.04 | 5.17 | |
| Chance | M=20.39 | 6.49 | |
| Doctors | M=15.65 | 2.10 | |
| Other People | M=8.52 | 2.83 | |
| Technology Experience Profilec | Mean | SD | |
| Health Technology (e.g., Blood Pressure Monitor, Digital Thermometer, Heart Rate Monitor) | M=0.85 | 1.13 | |
| Technical Readiness Index 2.0d | Mean | SD | |
| Optimism | M=3.88 | 1.21 | |
| Innovativeness | M=2.92 | 1.18 | |
| Discomfort | M=3.12 | 1.26 | |
| Insecurity | M=3.44 | 1.17 | |
The scoring index for the background questionnaire: 1=Poor, 2=Fair, 3=Good, 4= Very Good, 5= Excellent
The scoring index for the Multidimensional Health Locus of Control-Form C: 6 to 14 = Low Inclination, 15 to 22 = Moderate Inclination, 23 to 30 = Strong Inclination
The scoring index for the Technology Experience Profile: 0=Never Used, 1=Used Once, 2=Occasionally Used, 3=Frequently Used
The scoring index for the Technology Readiness Index 2.0: 1=strongly disagree, 5=strongly agree
Initial Considerations
Our first general research objective was to understand, “What are older adults’ initial considerations about new healthcare technologies?” and “Do their considerations change depending on the complexity of the technology?” We addressed this through the thematic analysis of the participants’ initial responses during the interview; they received the descriptions of each of the technologies. The following sections will address the initial considerations for each healthcare technology to illustrate how these initial considerations varied based on complexity.
Blood Pressure Monitor.
When presented with a new blood pressure monitor, the primary considerations from the participants were: familiarity, perceived benefits, perceived ease of use, and perceived need for oneself (Table 2). Familiarity, the most frequently mentioned factor, was defined as “past experiences with related products.” Thus, familiarity with the blood pressure monitor was not surprising given that participants had hypertension and may already have a method to monitor their blood pressure to support their health self-management. One participant mentioned this, “…I think most people start out a bit familiar…[because] they’ve had it done when they have checkups.” Another participant stated, “Because it’s very similar to what I’m doing already. I’m familiar with it. I know how to do it.”
Table 2.
Initial Reactions Associated with Use of Blood Pressure Monitor
| Category | n (%) | Sample Quotes |
|---|---|---|
| Familiarity | 16 (43%) | , “…I’m already familiar with taking my blood pressure…” |
| Perceived Benefits | 8 (22%) | “Using [the blood pressure monitor] is gonna help me maintain my health and my ability to live longer.” |
| Perceived Ease of Use | 7 (19%) | “Itseems easy…” |
| Perceived Need for Oneself | 6 (16%) | “I think that’s what I need.” |
Note. There were 37 total comments included in the percentages. Total comments for each category differ based on the comment type.
The next most frequently discussed factor was perceived benefit, such as how the beneficial attributes of the blood pressure monitor can improve one’s health. Perceived benefit was defined as “knowing the concrete benefits of using technology.” The participants could see the potential value, perhaps due to their familiarity with blood pressure monitors. One participant expressed the various possibilities that could come from using the blood pressure monitor, stating, “Well of course keeping a record of what your blood pressure is according to what your doctor had told you to do. You would be able to tell whether it’s going up or down too high maybe it would tell you not to eat so much salt if it got too high.”
Similarly, perceived ease of use, which was defined as “the degree of ease associated with the use of the healthcare technology,” was mentioned in their initial comments, perhaps also connected to familiarity. One of the participants stated, “Well, it’s relatively easy to use. It’s easy to understand it too. You are in control of what you’re doing, it’s keeping track of the information so that makes it easy to… look back and see what your blood pressure is doing.” Some participants even stated that they had or used something similar in their environment. For example, one participant stated that the blood pressure monitor is “Quite easy. I like it. I did it this morning. It was a piece of cake.”
Lastly, participants perceived that they needed the blood pressure monitor for themselves. The perceived need was not surprising due to the participants managing their hypertension and keeping track of their blood pressure. One participant answered, “I do. I just need to get one.” when asked if they believed that they need to use the blood pressure monitor.
Electronic Pillbox.
In contrast to the blood pressure monitor, participants considered different factors for the electronic pillbox: relative advantage, perceived need for others, and complexity (Table 3). With pillboxes being a standard method for medication management, the first factor under consideration for an electronic pillbox was whether it was better or worse than their current method. This most discussed factor was relative advantage, defined as “the degree to which a technological factor is perceived as providing greater benefit.” Many participants perceived the electronic pillbox to be more effective than their current method of managing their medications. For example, “If I had it and it worked for me, yes. I would. I think that is a little bit more accurate than what I’m doing now.”
Table 3.
Initial Reaction Factors Associated with Use of an Electronic Pillbox
| Category | n (%) | Sample Quotes |
|---|---|---|
| Relative Advantage | 8 (36%) | “It’s just much simpler to do the way I do it.” |
| Complexity | 7 (32%) | “it’s a little too complex over the long run.” |
| Perceived Need for Others | 7 (32%) | “I think it would probably be good for some people, but I don’t think I, myself, am ready for that.” |
Note. There were 22 comments included in the percentages. Total comments for each category differ based on the comment type.
The participants saw the electronic pillbox as being complex when compared to their current method of managing their medication—particularly describing their current method as simple and that it may be useful for those that have a more complicated schedule. An example of the electronic pillbox being perceived as complex is, “Too complicated…because my system is simple and this…seems to me just adding more complication to my system. My needs. If your needs were more complicated this might simplify it.”
Although participants perceived the electronic pillbox as being more effective than their current method, many of the participants believed that it would fit the needs of other people rather than themselves, especially if the participant had a simplified method or if others had various limitations. One participant stated, “…definitely would be very helpful for people who maybe their… memory has gotten a little bit faulty and they perhaps don’t remember when they take it when they took it if they took it, etcetera.” Some participants merely did not believe that the electronic pillbox would be useful for them. For example, “I’m sure it could be useful for the right person I’m not sure I’m that right person though.”
Multifunctional Healthcare Robot.
As observed for the electronic pillbox, complexity and perceived need for others were two factors that were considered for the multifunctional healthcare robot (Table 4). Perhaps not surprisingly, as this was the most complex technology presented to the participants. Specifically, one participant stated, “I think it would be difficult. I mean if I’m so sick…I wouldn’t wanna mess with it. You know, and if I’m well enough I can just do it on my own. So, I think this is something I would never use.”
Table 4.
Initial Reaction Factors Associated with Use of a Multifunctional Healthcare Robot
| Category | n (%) | Quotes |
|---|---|---|
| Complexity | 5 (56%) | “It might be simpler to have a non-multifunctional thing….” |
| Perceived Need for Others | 4 (44%) | “Well, I think it would be a good reminder for people that don’t take their blood pressure at a regular basis like they’re supposed to…” |
Note. There were 9 comments included in the percentages. Total comments for each category differ based on the comment type.
The multifunctional healthcare robot was also perceived as filling a possible need for others but not for oneself. Stating, “I believe it would improve the health of someone who needed it. I don’t need it…” Another example of perceived need for others illustrated how people that might need the multifunctional healthcare robot compared to ‘average’ senior citizens:
“Well, you know depending on how much mobility the person has the robot might be better for somebody with say limited mobility not you know quite as independent as others. But for your average I would say senior citizen that is not you know dealing with a lot of medical problems no.”
Each health technology had factors associated with the participants’ initial considerations, with the number of factors considered decreasing as the technology became more complex. The blood pressure monitor, the least complex, elicited four factors of consideration: familiarity, perceived benefits, perceived ease of use, and perceived need for oneself. The electronic pillbox and the multifunctional healthcare robot elicited three and two factors, respectively, two of which they had in common – complexity and perceived need for others. The third factor considered for the electronic pillbox was relative advantage. Although there were various specific factors that participants initially considered, other factors emerged upon further consideration.
Additional Considerations
The second research objective was to understand, “Upon further reflection, what are the additional considerations that older adults mention when deciding whether to adopt a healthcare technology?” To address this, we conducted a thematic analysis to understand what factors emerged in the ensuing discussion.
In addition to the initial factors, there were eight others that the participants considered when presented with a new healthcare technology (Table 5). Each factor that emerged consisted of 2–4 different themes (i.e., positive and negative). The following sections describe these additional factors in alphabetical order to ensure factors with the same names are grouped (e.g., advice acceptance).
Table 5.
Additional Factors Considered by Older Adults upon Further Reflection
| Factors | Comment Type n (%) | Quotes | Frequencies by Healthcare Technology |
|---|---|---|---|
| Advice Acceptance from Family (n=54) | Positive 33 (61%) | “ Some of my family members know what the results of high blood pressure or hypertension is. So that’s why. And I would listen to [them] because we’ve all experienced it, what it does.” |
BP (n= 15)
EPB (n=7) MHR (n=11) |
| Negative 21 (39%) | “They’re not healthcare professionals.” |
BP (n= 4)
EPB (n=8) MHR (n=9) |
|
| Advice Acceptance from Friends (n=51) | Positive 22 (43%) | “I would listen to my friends…when my friends and I start talking about different things that kill us, we pay attention to each other [because] we know from personal experience with family members or whatever. We pay attention to each other” |
BP (n=8)
EPB (n=9) MHR (n=5) |
| Negative 29 (57%) | “I really don’t care what friends…have to say about any healthcare technology or procedure.” |
BP (n=6)
EPB (n=10) MHR (n=13) |
|
| Advice Acceptance from Healthcare Provider (n=64) | Positive 53 (83%) | “Because if you trust your healthcare provider, then you would be more willing to do this type of thing or use this type of thing.” |
BP (n=21)
EPB (n=15) MHR (n=17) |
| Negative 11 (17%) | “there would have to be a good reason because, like I say, the method that I use seems to be working well” |
BP (n=1)
EPB (n=5) MHR (n=5) |
|
| Compatibility (n=67) | Compatible 50 (75%) | “…people are taking a pill is a daily routine kind of a thing so this is just a little bit of an augmentation or reminder or helper to make it work” |
BP (n=17)
EPB (n=19) MHR (n=14) |
| Incompatible 17 (25%) | “I don’t worry about my.blood pressure on a daily basis” |
BP (n=3)
EPB (n=5) MHR (n=9) |
|
| Convenience (n=77) | Convenient 49 (64%) | “… it is more convenient than say going to the drug store or Sams or Walmart…. So it’s convenient [because] it’s at home.” |
BP (n=21)
EPB (n=17) MHR (n=11) |
| Inconvenient 28 (36%) | “Seems like that would take and awfully lot of time” |
BP (n=2)
EPB (n=12) MHR (n=14) |
|
| Facilitating Conditions (n=85) | Support 42 (49%) | “I would use it on my own. I would probably have some professional help. My son help[s] me set it up, but yes.” |
BP (n=6)
EPB (n=12) MHR (n=24) |
| No support 43 (51%) | “[Because] I know how to do it.” |
BP (n=19)
EPB (n=13) MHR (n=11) |
|
| Perceived Usefulness (n=75) | Useful 66 (88%) | “I think that’s useful…” |
BP (n=26)
EPB (n=20) MHR (n=20) |
| Not Useful 9 (12%) | “I’m not convinced that it’s that useful” |
BP (n=1)
EPB (n=4) MHR (n=4) |
|
| Privacy (n=70) | Invades privacy 7 (10%) | “I think I wouldfeel watched… ” |
BP (n=0)
EPB (n=2) MHR (n=5) |
| Privacy is not an issue 40 (57%) | “I think it would be pretty secure… ” |
BP (n=18)
EPB (n=12) MHR (n=10) |
|
| Lack of privacy concern 23 (33%) | “I’m just not inclined to worry about that kind of thing. Actually, I guess I have nothing to be secret about…” |
BP (n=4)
EPB (n=9) MHR (n=10) |
|
| Subjective Norm Family (n=68) | Positive 50 (74%) | “My family is whatever you think is best for you, we’re for it” |
BP (n=17)
EPB (n=18) MHR (n=15) |
| Negative 7 (10%) | “They [would] laugh at me” |
BP (n=0)
EPB (n=3) MHR (n=4) |
|
| Not sure/Do not care 11 (16%) | “Chances are good they wouldn’t know because we don’t really talk about health issues.” |
BP (n=4)
EPB (n=3) MHR (n=4) |
|
| Subjective Norm Friends (n=68) | Positive 33 (48%) | “They would be fascinated.” |
BP (n=11)
EPB (n=10) MHR (n=12) |
| Negative 8 (12%) | “They’d think I was crazy.” |
BP (n=1)
EPB (n=2) MHR (n=5) |
|
| Not sure/Do not care 27 (40%) | “I really don’t give a crap what my friends think.” |
BP (n=10)
EPB (n=12) MHR (n=5) |
|
| Subjective Norm Healthcare Provider (n=69) | Positive 48 (70%) | “I think they’d be delighted if it would improve the compliance” |
BP (n=19)
EPB (n=15) MHR (n=14) |
| Negative 5 (7%) | “Probably would have some of the same concerns I expressed with it.” |
BP (n=0)
EPB (n=2) MHR (n=3) |
|
| Not sure/Do not care 16 (23%) | “I don’t have a clue. I really don’t know…” |
BP (n=3)
EPB (n=8) MHR (n=5) |
|
| Trust (n=97) | Trust in technology 41 (42%) | “It’s just like the one.the nurse puts on. [You] know. It’s probably FDA approved or whatever.” |
BP (n=16)
EPB (n=15) MHR (n=10) |
| Trust in person 18 (19%) | “Because I trust my doctor and if he says that I need to do something I will do it.” |
BP (n=3)
EPB (n=8) MHR (n=7) |
|
| Conditional trust 22 (23%) | “Once I know that it’s calibrated properly, yes.” |
BP (n=7)
EPB (n=7) MHR (n=8) |
|
| Lack of trust 16 (16%) | “I don’t trust it and I don’t think I need it.” |
BP (n=1)
EPB (n=3) MHR (n=12) |
Note. Frequency of comment types are a combination of the three healthcare technologies. BP is blood pressure monitor, EPH is electronic pillbox, and MHR is multifunctional health robot.
Advice acceptance in this study focused on whether older adults would accept or not accept the advice from a significant other (i.e., family members, friends, and healthcare providers) to use healthcare technology. Discussions on advice acceptance had a higher frequency of positive comments towards accepting advice from healthcare providers and family members than friends. The participants stated more positive comments towards healthcare providers due to trusting their healthcare provider and their expertise. Similarly, the participants stated positive comments towards family members due to their relationships and the part that their family members played in their health management. Conversely, the participants mentioned more negative comments towards accepting advice from friends, reportedly caring less about their opinions.
Conversations about compatibility focused on how healthcare technology would be compatible with one’s current lifestyle. With the participants already having their methods to self-manage their health, how would these technologies fit in their lives? Most of the conversations focused on how the healthcare technologies were compatible--focusing on how they could incorporate the technologies into their lives with minimal effort to use them.
When considering if the healthcare technologies would make their lives easier or harder, the participants stated more frequently that the healthcare technologies appeared convenient to use. They also focus on the position they were currently in, within their lives, or the amount of time needed to use the healthcare technologies.
Facilitating conditions were considered as receiving instructional or physical support to use healthcare technologies. There was no difference regarding whether the participants perceived that they would want support or not want support. The participants who mentioned that they would like support wanted to have someone there to help them or some type of instructions to follow. The participants who did not want support reported that they were comfortable using the healthcare technologies.
Another factor centered on how older adults perceived the technology to be useful. Given that healthcare technologies are commonly used to support self-management of hypertension, it is no surprise that most of the participants in this study perceived that healthcare technologies would be useful. Many focused on how healthcare technologies are generally useful, whereas others focused on the benefits of using healthcare technologies.
With technologies gradually becoming more ingrained in our lives, privacy is a common concern. Three types of comments emerged from the data: invading their privacy, not being an issue, and lacking concern. Fifty-seven per cent of the comments focused on how privacy was not an issue to them. The second comment that was frequently mentioned was related to a lack of privacy concern. Many did not understand how these technologies would invade their privacy. However, others mentioned that the technology would invade their privacy generally or that it was dependent on how it was set up.
Subjective norm focused on how older adults perceive their significant others want them to either use or not use healthcare technologies. Like advice acceptance, the participants believed that their family members and their healthcare providers would react more positively to them using these healthcare technologies. However, the participants perceived that their friends would react positively towards them using the healthcare technologies, but they were also not sure, nor did they care much how they reacted. This contrast was due to the personal relationships that the participants had with their friends. Some of the participants conversed with their friends about their health conditions and felt they would receive support to use the healthcare technologies. Others did not converse with their friends about their health conditions, and some noted that they did not have any close friends.
Lastly, the participants considered trust a factor that influenced whether to accept a new healthcare technology. There were four types of comments: trust in the technology, trust in the person, conditional trust, and lack of trust. One reason participants trusted the technology was due to their personal experiences. Others trusted the technology once they knew that issues would not arise in the future. Some participants trusted the person, specifically their healthcare providers, who told them to use the technology. Others lacked trust due to generally just not trusting the healthcare technologies or the perceptions that the participants had of the healthcare technologies.
Discussion
This study aimed to understand what older adults consider when they are introduced to new healthcare technology. As the world becomes more technologically advanced, older adults have little choice but to accept these healthcare technologies. Their initial considerations likely influence later actual usage of future healthcare technologies that are introduced into their lives.
The older adults’ initial considerations in the interviews included various factors, but we included the major themes that were frequently stated (i.e., four or more times). These themes regarding the initial considerations about the healthcare technologies discussed in this study varied across the three technologies, with some similarities between the electronic pillbox and the multifunctional healthcare robot, which were presumably the more complex.
The three technologies used in this studied varied in complexity but were similar to what individuals might use to help self-manage their hypertension. Thematic analysis of the older adults’ initial considerations yielded seven themes: familiarity, perceived benefits, perceived ease of use, perceived need for oneself, relative advantage, complexity, perceived need for others. Overall, there were more comments for the more familiar and less complex healthcare technology (Kim, Mannino and Nieschwietz, 2009). For example, familiarity was only associated with the blood pressure monitor, and perceived need for others was associated with both the electronic pillbox and the multifunctional healthcare robot.
The four predictors commonly used in theoretical models of acceptance are perceived usefulness, perceived ease of use, social influence, and facilitating conditions. In UTAUT, the terms used were performance expectancy (perceived usefulness), effort expectancy (perceived ease of use), social influence, and facilitating conditions. These four predictors were defined by developing an exhaustive list from prior models and theories. For example, effort expectancy was developed using perceived ease of use, complexity, and ease of use (Venkatesh et al., 2003).
UTAUT2 incorporated new predictors (i.e., cost), which resulted in seven predictors that are said to lead to behavioral intentions. As previously stated, although this theory was based on acceptance, it did not focus on healthcare technologies and older adults. Therefore, this study aimed to understand if the factors considered in this study are consistent with the predictors in UTAUT2. In this study, some factors emerged that were not incorporated into UTAUT2, such as perceived need, perceived benefits, familiarity, trust, and advice acceptance.
Older adults may not accept a technology, regardless of the type, if they believe they do not need it (Czaja et al., 2013; Lorenzen-Huber et al., 2011). Perceived need, in this study, is the belief that technical assistance is needed for oneself or others. For example, older adults may believe that they currently need technology due to the possibility of it supporting them at that moment. Another example would include older adults not believing that they need the technology, but it could be useful for someone else. Previous research found that accepting a technology is least likely if technological assistance does not support the person’s current needs (Thielke et al., 2012).
The term perceived benefit is included in the definition of price value from UTAUT2 (Venkatesh et al., 2012). Nevertheless, price value is not adequately defined, independent of perceived benefit. If older adults know the concrete benefits of using a technology (Jimison et al., 2008), this can increase the chance of adoption (Mitzner et al., 2010). Knowledge of the concrete benefits and perceiving the benefits of using that technology as advantageous, may reduce concerns about using that technology (Peek et al., 2014).
When the technology itself is familiar, perhaps due to past experiences with similar products, it can influence behavioral intentions (Mahmood et al., 2008). Exposure to technologies by older adults is explicitly negatively correlated with their age (Lee and Coughlin, 2015). Thus, if novel technologies are familiar and can be gradually introduced to older adults, usage may be more successful (Jimison et al., 2008).
Older adults’ perceptions of trust can influence how complex older adults perceive the technology to be. When there is a lack of trust, especially in the information the technology provides, it becomes a barrier to accepting the technology (Jimison et al., 2008). Without understanding if they can trust the technology or person with their privacy or that it is safe can deter older adults from accepting the technology.
Advice acceptance is a novel term in the technology acceptance literature, providing a focus on older adults accepting advice from a significant other in their care network to use a specific healthcare technology. Current models and theories of technology acceptance have predictors (i.e., social influence) that focus on how others perceive the user or the support the user receives from their family members and friends. Although there are common socially related predictors in the technology acceptance literature, most do not explicitly include receiving advice from people that can influence the user’s acceptance.
In the context of recommending healthcare technologies to support a health behavior change, the recommendation must come from someone knowledgeable on the subject and match the advice recipient’s information (Van Swol and Sniezek, 2011). This match between the advice recipient and the advice-giver increases the advice recipient’s confidence about the advice. Thus, if the advice-giver in the interaction appears to be confident, it is more likely that advice recipients will accept it. To understand the role of advice acceptance in the acceptance of healthcare technology, the care network, persons closely associated and trusted (i.e., healthcare provider, family, and friends), were considered.
We developed a conceptual model, the Healthcare Technology Acceptance Model (H-TAM; see Figure 2; for more detail see Harris, 2019), to illustrate the factors that older adults considered when introduced to healthcare technologies. The bolded and italicized factors in H-TAM represented factors that are not commonly included in technology acceptance models. These factors were considered by the older adults we interviewed in the contexts of their intentions to adopt a new healthcare technology. The factors at the bottom of the conceptual model (e.g., sex and age) are moderators that are commonly found in technology acceptance models. Lastly, there are two types of lines in H-TAM. The solid lines represent relationships found in the literature, and the dotted lines represent hypothesized relationships. Privacy and trust in the technology are both hypothesized to relate to complexity and familiarity. With the addition of various factors and hypothesized relationships, the present data illustrated that a broader view of acceptance is needed for this context.
Figure 2.
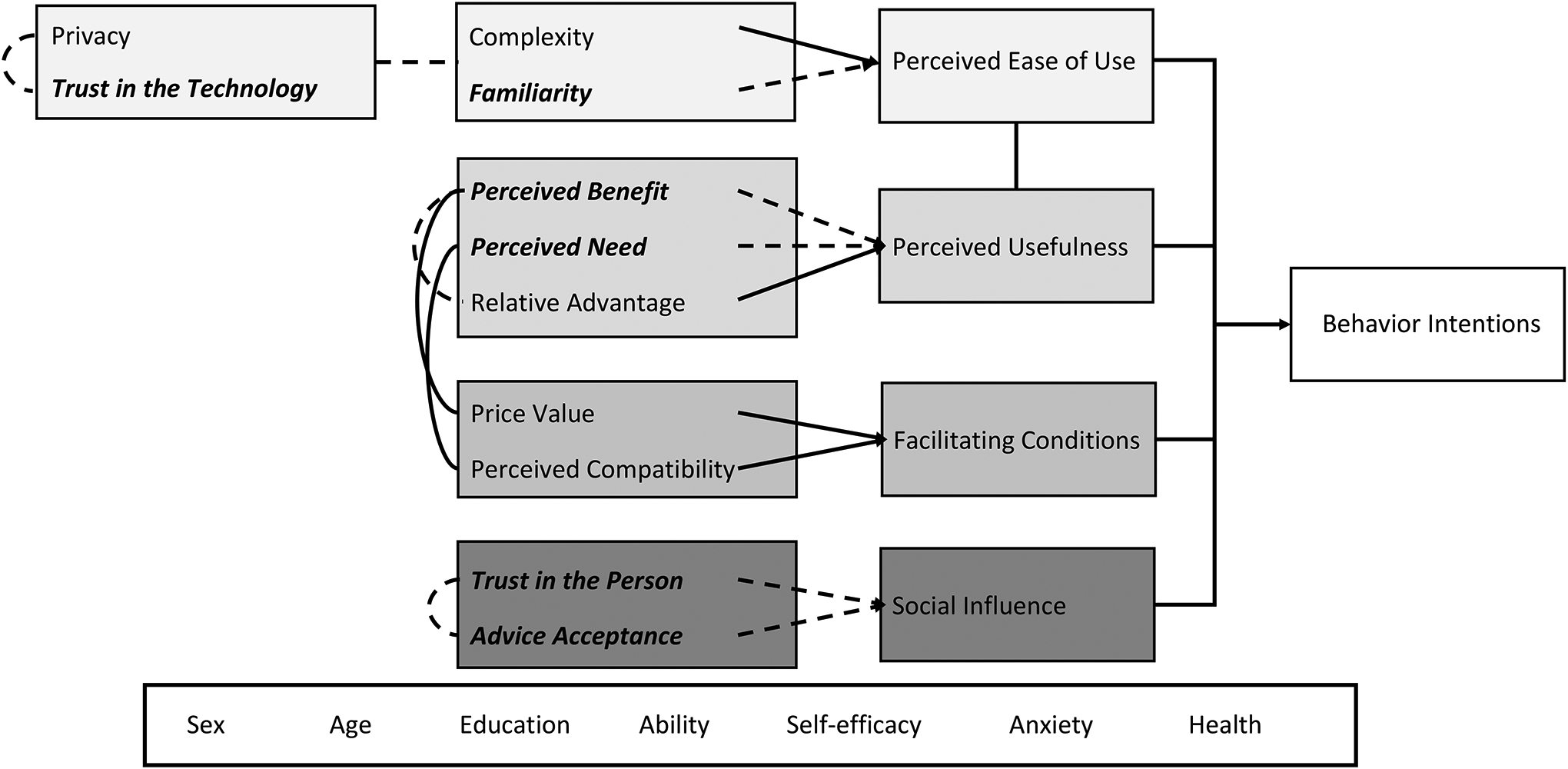
A Conceptual Healthcare Technology Acceptance Model (H-TAM)
These findings provided valuable insights about what older adults considered when presented with a new healthcare technology. Nevertheless, there are limitations to this study that should be noted. The sample of 23 participants is a reasonable number for qualitative research studies, but future studies should consider having a more extensive and diverse sample to ensure that the study represents the population. Having a larger sample would allow for a mixed-methods study to strengthen the generalizability and guide theory development. Specifically, looking quantitatively at how these factors predict older adults’ intentions to accept healthcare technologies can support introduction of technologies to support different health conditions that older adults are commonly susceptible to (i.e., cardiovascular disease). Future research should explore the dyad between the older adult and individuals in their care network to understand the complexities of the relationship and how it affects the older adults’ considerations.
Conclusion
Technology acceptance models are commonly used to understand the acceptability of various technologies by different groups of people. Our goal was to focus on older adults’ initial considerations when presented with new healthcare technologies and how these considerations compared to a well-known technology acceptance model (UTAUT2). There were seven themes that older adults initially considered when presented with new healthcare technologies and eight additional factors. Of these 15 factors, four were consistent across many technology acceptance models, including UTAUT2, such as perceived ease of use and perceived usefulness. The remaining factors are included in some models of technology acceptance (e.g., subjective norm), whereas are not. (e.g., advice acceptance and perceived need).
The Healthcare Technology Acceptance Model (H-TAM) was developed to illustrate the emergent factors in this study that are not included in current technology models. Future research should consider using quantitative methods to understand better how these factors interact with each other and their relationships with behavior intentions and acceptance—eventually informing future healthcare technology design, health behavior interventions that utilize healthcare technologies, and the adoption of healthcare technologies by older adults.
Acknowledgments.
This research was supported in part by a research supplement grant from the National Institute of Health (National Institute on Aging) Grant P01 AG17211 under the auspices of the Center for Research and Education on Aging and Technology Enhancement (CREATE). This research was conducted as part of a Master’s Thesis; thus, we would like to thank the committee members: Wendy A. Rogers, Shannon T. Mejía, and Andiara Schwingel. In addition to the committee members, we would like to acknowledge the students that supported this research study Olivia Kupiec and Danniel Rhee.
The authors would like to thank Olivia Kupiec, Danniel Rhee, and Claire Textor for their assistance on this study.
Footnotes
Ethical standards. This study was approved by the Institutional Review Board at the University of Illinois Urbana-Champaign (Protocol #17526)
Statement of conflict of interest: The authors declare no conflicts of interest.
References.
- American Heart Association (2017) Changes you can make to manage high blood pressure. American Heart Association Available online at https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure [Accessed June 2020]
- Ajzen I (1991) The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- Banerjee M, Capozzoli M, McSweeney L, and Sinha D (1999) Beyond kappa: A review of interrater agreement measures. Canadian Journal of Statistics, 27, 3–23. 10.2307/3315487 [DOI] [Google Scholar]
- Barg-Walkow LH, Mitzner TL and Rogers WA (2014) Technology Experience Profile (TEP): Assessment and Scoring Guide. (HFA-TR-1402) Atlanta, GA. [Google Scholar]
- Brennan RL and Prediger DJ (1981) Coefficient Kappa: Some Uses, Misuses, and Alternatives. Educational and Psychological Measurement, 41, 687–699. 10.1177/001316448104100307 [DOI] [Google Scholar]
- Chen K and Chan AHS (2014) Gerontechnology acceptance by elderly Hong Kong Chinese: A senior technology acceptance model (STAM). Ergonomics, 57, 635–652. 10.1080/00140139.2014.895855 [DOI] [PubMed] [Google Scholar]
- Czaja S, Beach S, Charness N and Schulz R (2013) Older adults and the adoption of healthcare technology: Opportunities and challenges. In Sixsmith A and Gutman G (eds.), Technologies for Active Aging. International Perspectives on Aging, vol 9. Springer, Boston, 27–46. 10.1007/978-1-4419-8348-0_3 [DOI] [Google Scholar]
- Czaja SJ, Charness N, Fisk AD, Hertzog C, Nair SN, Rogers WA, and Sharit J (2006) Factors Predicting the Use of Technology: Findings From the Center for Research and Education on Aging and Technology Enhancement (CREATE). Psychology and Aging, 21, 333–352. 10.1037/0882-7974.21.2.333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Angelo J and D’Angelo A-L (2018) Advice from healthcare professionals. In MacGeorge EL. and Van Swol LM. (eds.), The Oxford Handbook of Advice (Vol.1). The Oxford University Press, New York, 197–216. 10.1093/oxfordhb/9780190630188.013.10 [DOI] [Google Scholar]
- Davis FD (1989) Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Quarterly, 13, 319–340. JSTOR. 10.2307/249008 [DOI] [Google Scholar]
- de Jager CA, Budge MM, and Clarke R (2003) Utility of TICS-M for the assessment of cognitive function in older adults. International Journal of Geriatric Psychiatry, 18, 318–324. 10.1002/gps.830 [DOI] [PubMed] [Google Scholar]
- Harris MT (2019). Developing the Healthcare Technology Acceptance Model (H-TAM) for Older Adults [Unpublished master’s thesis]. University of Illinois Urbana-Champaign. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimison H, Gorman P, Woods S, Nygren P, Walker M, Norris S and Hersh W (2008) Barriers and drivers of health information technology use for the elderly, chronically ill, and underserved. Evidence Report/Technology Assessment, 175, 1–1422. [PMC free article] [PubMed] [Google Scholar]
- Kim HJ, Mannino M, and Nieschwietz RJ (2009) Information technology acceptance in the internal audit profession: Impact of technology features and complexity. International Journal of Accounting Information Systems, 10, 214–228. 10.1016/j.accinf.2009.09.001 [DOI] [Google Scholar]
- Kim S and Garrison G (2009) Investigating mobile wireless technology adoption: An extension of the technology acceptance model. Information Systems Frontiers, 11, 323–333. 10.1007/s10796-008-9073-8 [DOI] [Google Scholar]
- King WR and He J (2006) A meta-analysis of the technology acceptance model. Information & Management, 43, 740–755. 10.1016/j.im.2006.05.003 [DOI] [Google Scholar]
- Lee C and Coughlin JF (2015) PERSPECTIVE: Older Adults’ Adoption of Technology: An Integrated Approach to Identifying Determinants and Barriers. Journal of Product Innovation Management, 32, 747–759. 10.1111/jpim.12176 [DOI] [Google Scholar]
- Lee DY and Lehto MR (2013) User acceptance of YouTube for procedural learning: An extension of the Technology Acceptance Model. Computers & Education, 61, 193–208. 10.1016/j.compedu.2012.10.001 [DOI] [Google Scholar]
- Lee Y, Kozar KA and Larsen KRT (2003) The Technology Acceptance Model: Past, Present, and Future. Communications of the Association for Information Systems, 12. 10.17705/1CAIS.01250 [DOI] [Google Scholar]
- Lorenzen-Huber L, Boutain M, Camp LJ, Shankar K and Connelly KH (2011) Privacy, Technology, and Aging: A Proposed Framework. Ageing International, 36, 232–252. 10.1007/s12126-010-9083-y [DOI] [Google Scholar]
- Mahmood A, Yamamoto T, Lee M and Steggell C (2008) Perceptions and Use of Gerotechnology: Implications for Aging in Place. Journal of Housing for the Elderly, 22, 104–126. 10.1080/02763890802097144 [DOI] [Google Scholar]
- Mitzner TL, Bixter MT and Rogers WA (2016) Qualitative Research Procedures in the Human Factors and Aging Laboratory. (HFA-TR-1601). Atlanta, GA. [Google Scholar]
- National Council on Aging (2017) Top 10 Chronic Conditions in 65+ and what you can do to prevent or manage them. National Council on Aging Available online at https://www.ncoa.org/blog/10-common-chronic-diseases-prevention-tips/ [Accessed July 2020]
- Parasuraman A and Colby CL (2015) An Updated and Streamlined Technology Readiness Index: TRI 2.0. Journal of Service Research, 18, 59–74. 10.1177/1094670514539730 [DOI] [Google Scholar]
- Peek STM, Wouters EJM, van Hoof J, Luijkx KG, Boeije HR and Vrijhoef HJM (2014) Factors influencing acceptance of technology for aging in place: A systematic review. International Journal of Medical Informatics, 83, 235–248. 10.1016/j.ijmedinf.2014.01.004 [DOI] [PubMed] [Google Scholar]
- Renaud K and van Biljon J (2008) Predicting technology acceptance and adoption by the elderly: A qualitative study. Proceedings of the 2008 Annual Research Conference of the South African Institute of Computer Scientists and Information Technologists on IT Research in Developing Countries Riding the Wave of Technology - SAICSIT ‘08, 210–219. 10.1145/1456659.1456684 [DOI] [Google Scholar]
- Swol LM and Sniezek JA (2005) Factors affecting the acceptance of expert advice. British Journal of Social Psychology, 44, 443–461. 10.1348/014466604X17092 [DOI] [PubMed] [Google Scholar]
- Thielke S, Harniss M, Thompson H, Patel S, Demiris G and Johnson K (2012) Maslow’s Hierarchy of Human Needs and the Adoption of Health-Related Technologies for Older Adults. Ageing International, 37, 470–488. 10.1007/s12126-011-9121-4 [DOI] [Google Scholar]
- U.S. Department of Health and Human Services (2018) 2017 Profile of Older Americans. Administration for Community Living Available online at https://acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2017OlderAmericansProfile.pdf [Accessed July 2020]
- Venkatesh V, Morris MG, Davis GB and Davis FD (2003) User Acceptance of Information Technology: Toward a Unified View. MIS Quarterly, 27, 425–478. JSTOR. 10.2307/30036540 [DOI] [Google Scholar]
- Venkatesh V, Thong JYL and Xu X (2012) Consumer Acceptance and Use of Information Technology: Extending the Unified Theory of Acceptance and Use of Technology. MIS Quarterly, 36, 157–178. JSTOR. 10.2307/41410412 [DOI] [Google Scholar]
- Wallston KA, Stein MJ and Smith CA (1994) Form C of the MHLC Scales: A Condition-Specific Measure of Locus of Control. Journal of Personality Assessment, 63, 534–553. 10.1207/s15327752jpa6303_10 [DOI] [PubMed] [Google Scholar]


