Abstract
Carcinoma prostate is the second most common malignancy in males. It starts with a relatively indolent course and maybe asymptomatic during the initial stages. However, metastasis is highly common in Carcinoma prostate. The sites of metastases include bone, lung, liver, pleura and adrenals with cutaneous metastasis being one of the rarest sites being less than 1%. In our case report we present one such rare finding of Carcinoma prostate with cutaneous metastasis.
Keywords: Carcinoma prostate, cutaneous metastasis, rare cases
INTRODUCTION
Carcinoma prostate is the second-most common malignancy in males.[1] It starts with a relatively indolent course and is often asymptomatic during the initial stages. However, depending on the treatment, patient’s compliance, and the Gleason score of the disease, the prostate cancer metastasizes in many cases. The sites of metastases include bone (90%), lung (46%), liver (25%), pleura (21%), and adrenals (13%), with cutaneous metastasis (0.36%) being one of the rarest sites.[2,3] There are only a few cases of cutaneous metastasis reported in the medical literature till date.
CASE REPORT
A 64-year-old male, known case of carcinoma prostate since 2016, reported to our department in 2022. The patient had LUTs, clinically malignant prostate, and raised prostate-specific antigen (PSA) (15.31 ng/ml), for which he underwent prostate biopsy in March 2016. The biopsy was suggestive of poorly differentiated adenocarcinoma with Gleason score of 4 + 5. The patient was then started on antiandrogen therapy (bicalutamide), and bilateral orchidectomy was done in September 2016. No documents of metastatic workup were available with the patient. He was then lost to follow-up. He again presented elsewhere with complaints of LUTS in 2019. For this, he underwent channel TURP. Again, he was lost to follow-up for 2 years. Then, he presented to AIIMS Jodhpur, Urology department in 2022 with complaints of hematuria on and off for 5 days and decreased urine output with few violaceous nontender nodules present over the right groin region for the past 20 days [Figure 1]. There were no other complaints. The nodules were firm and noncompressible. Hard lymph nodes were palpated on both sides in the inguinal regions. On evaluation, the patient had bilateral hydroureteronephrosis and deranged KFT. The PSA level was 436.26 ng/ml. The patient underwent bilateral nephrostomy placement, excisional biopsy of skin lesion, and was discharged after 2 days when kidney function started normalizing.
Figure 1.

Clinical photograph of skin metastasis
The patient underwent metastatic workup after kidney function normalized. Bone scan was done suggestive of extensive osteoblastic skeletal metastases at the skull (multifocal), bilateral clavicles, sternum, bilateral scapula, proximal 1/3rd of the right humerus, multiple bilateral ribs, multiple cervico-dorso-lumbar vertebrae, pelvis (multiple focal), and sacrum. Contrast-enhanced computed tomography of the thorax, abdomen, and pelvis was done, which was suggestive of inguinal and iliac lymphadenopathy, multiple skeletal metastases, dermal deposits in the lower abdomen, and deposits in the left iliacus muscle. On follow-up, the skin lesion turned out to be metastatic deposits, and on immunohistochemistry testing, the lesions were positive for PSA [Figure 2]. In this case of metastatic castration resistant prostate carcinoma docetaxel based chemotherapy was given to the patient in view of non-compliant attitude of the patient. Secondarily due to economic constraints, use of expensive antiandrogen drugs such as enzalutamide or abiraterone was deferred as first line treatment.
Figure 2.
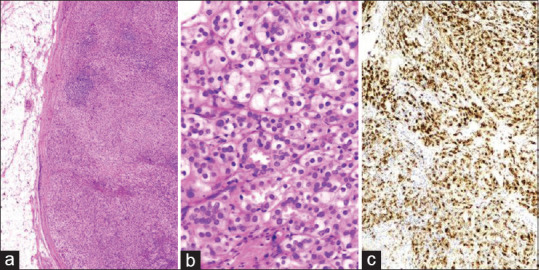
(a) Photomicrograph of skin nodule showing tumor cells arranged in a nesting pattern (H and E, ×40), with occasional germinal center is identified. (b) High-power view shows the glandular architecture of the tumor with individual tumor cells having hyperchromatic nuclei and eosinophilic to clear cytoplasm (H and E, ×400). (c) The tumor cells showed diffuse cytoplasmic immunopositivity for PSA (IHC, ×100). H and E: Hematoxylin and eosin, IHC: Immunohistochemistry, PSA: Prostate-specific antigen
DISCUSSION
The genitourinary malignancies rarely metastasize to the skin, with <1% occurrence.[4] The occurrence of prostatic malignancy metastasizing to the skin is even rarer, and about 100 cases are reported in the English medical literature. Among the various histopathologic variants, adenocarcinoma is the source in 91% of cutaneous metastasis cases. Other variants with decreasing order of cutaneous metastasis include small cell carcinoma (3.8%), transitional cell carcinoma (2.6%), and mucinous adenoma subtype with signet ring cells (1.3%).[5-10] It has been observed that the cases those metastasized to the skin had high Gleason scores and the worst prognosis. Pertaining to these observations, our case histologically was adenocarcinoma prostate and had a Gleason score of 4 + 5. The skin lesions usually start with insidious onset nontender fleshy nodules of varying colors. Our patient had a similar presentation with pink nontender nodules, which were insidious onset and without any other associated symptoms pertaining to these lesions. The sites of involvement have been reported to vary vastly. It has been seen to be associated with metastasis at other places as well. In our patient, including skin, he had multiple skeletal metastases. Because the cutaneous metastasis in prostate cancer is very rare, commenting on the natural course is difficult. Wang et al. have reported that for cutaneous metastatic tumors, therapeutic options include local excision and intralesional chemotherapy.[11] However, in a case report of chest wall cutaneous metastasis by Mak et al., palliative radiotherapy of 18 Gy in three fractions was delivered to the left chest wall.[12] So far, no definitive treatment protocols for cutaneous metastasis in carcinoma prostate have been listed. In our case, we could excise the cutaneous metastases in toto keeping adequate free margins. It has been seen that metastasis usually spells a grave prognosis, and isolated cutaneous metastasis is yet to be seen; hence, until now, such cases have only limited survival, with one case reported by Marquis and Benson surviving 3.5 years following cutaneous metastasis.[13]
CONCLUSION
Cutaneous metastasis in prostate cancer is an extremely rare incident. Isolated cutaneous metastasis is yet to be seen. So far, the prognosis remains grave until further development in the definitive management strategy of such a rare scenario.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient’s legal guardian has given the consent for images and other clinical information to be reported in the journal. The patient’s legal guardian understands that name and initials will not be published, and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics. 2018:GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Bubendorf L, Schöpfer A, Wagner U, Sauter G, Moch H, Willi N, et al. Metastatic patterns of prostate cancer:An autopsy study of 1,589 patients. Hum Pathol. 2000;31:578–83. doi: 10.1053/hp.2000.6698. [DOI] [PubMed] [Google Scholar]
- 3.Gandaglia G, Abdollah F, Schiffmann J, Trudeau V, Shariat SF, Kim SP, et al. Distribution of metastatic sites in patients with prostate cancer: A population-based analysis. Prostate. 2014;74:210–6. doi: 10.1002/pros.22742. [DOI] [PubMed] [Google Scholar]
- 4.Mueller TJ, Wu H, Greenberg RE, Hudes G, Topham N, Lessin SR, et al. Cutaneous metastases from genitourinary malignancies. Urology. 2004;63:1021–6. doi: 10.1016/j.urology.2004.01.014. [DOI] [PubMed] [Google Scholar]
- 5.Cecen K, Karadag MA, Demir A, Kocaaslan R. Small cell carcinoma of the prostate presenting with skin metastasis: A case report. J Med Case Rep. 2014;8:146. doi: 10.1186/1752-1947-8-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kraft Rovere R, Silva de Lima A, Casemiro KP. A case of small-cell prostate cancer with a metastasis to the scalp. Jpn J Clin Oncol. 2013;43:1156. doi: 10.1093/jjco/hyt165. [DOI] [PubMed] [Google Scholar]
- 7.Yildirim Y, Akcay Y, Ozyilkan O, Celasun B. Prostate small cell carcinoma and skin metastases: A rare entity. Med Princ Pract. 2008;17:250–2. doi: 10.1159/000117801. [DOI] [PubMed] [Google Scholar]
- 8.Mishra VC, Tindall SF. Case report –Cutaneous metastasis from a primary transitional cell carcinoma of prostate. Int Urol Nephrol. 2001;33:507. doi: 10.1023/a:1019598702924. [DOI] [PubMed] [Google Scholar]
- 9.Razvi M, Fifer R, Berkson B. Occult transitional cell carcinoma of the prostate presenting as skin metastasis. J Urol. 1975;113:734–5. doi: 10.1016/s0022-5347(17)59568-3. [DOI] [PubMed] [Google Scholar]
- 10.López-Navarro N, López-Sánchez JC, Pérez-Enríquez JE, Bosch RJ, Herrera E. Atypical skin metastases of mucinous adenocarcinoma of the prostate with signet ring cells. Actas Dermosifiliogr. 2009;100:338–41. [PubMed] [Google Scholar]
- 11.Wang SQ, Mecca PS, Myskowski PL, Slovin SF. Scrotal and penile papules and plaques as the initial manifestation of a cutaneous metastasis of adenocarcinoma of the prostate:Case report and review of the literature. J Cutan Pathol. 2008;35:681–4. doi: 10.1111/j.1600-0560.2007.00873.x. [DOI] [PubMed] [Google Scholar]
- 12.Mak Gabriel, Chin M, Nahar N, De Souza P. “Cutaneous metastasis of prostate carcinoma treated with radiotherapy: A case presentation.” BMC Research Notes 7, no. 1 (December 2014) p. 505. https://doi.org/10.1186/1756-0500-7-505. [DOI] [PMC free article] [PubMed]
- 13.Marquis W, Benson R. Long-term survival with skin metastases from carcinoma of prostate. Urology. 1980;16:407–8. doi: 10.1016/0090-4295(80)90152-1. [DOI] [PubMed] [Google Scholar]


