INTRODUCTION
Evaluating lower-limb walking symmetry can help clinicians establish functional limitations, track changes over time, and assess effectiveness of rehabilitation techniques.1 Walking symmetry between prosthetic and intact limbs is often viewed as a measure of improved rehabilitation in individuals who use unilateral lower-limb prostheses (IULLPs),2 such as transtibial and transfemoral prostheses. Walking symmetry has been associated with increased balance,3–5 decreased fall risk,6 and decreased risk of developing musculoskeletal overuse injuries, such as osteoarthritis.7 Confidence in walking and balance tasks have been shown to improve community participation and quality of life.6,8 Therefore, increasing walking symmetry has the potential to improve functional mobility and quality of life in IULLPs.
Several reviews have discussed walking symmetry in IULLPs. In 2004, a review examined the influence of prosthetic componentry on kinematics, kinetics, and electromyography.9 Reviews on lumbopelvic parameters,10 standing balance,4 and the influence of muscle strength on balance5 also exist. Reviews on gait training15 and suspension systems11 have been shown to influence walking symmetry, and a review in 2011 identified the most common kinematic parameters studied in IULLPs.12 However, a review normalizing kinematic walking symmetry data across studies to inform clinical considerations in this population is lacking from the literature. Normalized walking symmetry data summarized from research in IULLPs can provide quantitative baseline characteristics to better inform clinical decision making.
Translating research findings into clinical care was identified as a 2020 research priority by the American Academy of Orthotists and Prosthetists, highlighting the importance of narrowing the barrier that exists between research data and clinical application.13 However, research studies have been difficult to compare, posing a barrier to translating research findings into clinical practice. Research studies typically have small sample sizes and differences in objectives, participant demographics, kinematic parameters, and mathematical analysis of symmetry.14 As a result, consensus among clinical practitioners has largely been based on observational effects rather than research findings.9 In order to translate kinematic walking symmetry research findings into clinical care, data need to be comparable, which can be achieved by normalizing research data across studies. Normative, or reference, values for symmetry have not been identified across current literature and could provide clinicians evidence-based rehabilitation targets by level of limb loss and payer justification for certain prosthetic componentry.
Therefore, the objective of this review was to normalize kinematic walking symmetry data in IULLPs by level of limb loss and prosthetic factors to inform considerations in clinical practice and future research. The most common participant demographics, kinematic parameters, and mathematical analysis of symmetry were identified. Then, data were normalized across studies using the most common mathematical analysis of symmetry for the five most common parameters identified in this review. Considerations for designing future kinematic walking symmetry studies are also provided to help promote clinical translation.
METHODS
A search was performed on March 18, 2020, in PubMed, Scopus, and Google Scholar to encompass literature from the year 2000. References from identified studies were also examined for inclusion.
The following search terms were used:
PubMed: (spatiotemporal) AND transtibial OR transfemoral AND prosth* AND unilateral AND symmetry OR asymmetry; (kinematic) AND transtibial AND prosth* AND unilateral AND symmetry OR asymmetry
Scopus: interlimb AND kinematic AND prosth* AND symmetry AND unilateral AND transtibial OR “below knee” OR transfemoral OR “above knee”
Google Scholar: kinematic OR spatiotemporal AND prosth* AND symmetry OR asymmetry OR “symmetry index” AND unilateral AND transtibial OR “below knee” AND transfemoral OR “above knee” AND gait OR ambulation -running -sprinting -powered -stair -ramp -incline -slope
Studies were selected based on the following inclusion criteria (Figure 1):
Adult population (defined as 18 or older) who used unilateral transtibial or transfemoral prostheses
Kinematic symmetry data were reported between the prosthetic and intact limbs
Participants walked on a level surface (ground or treadmill)
Fig. 1:
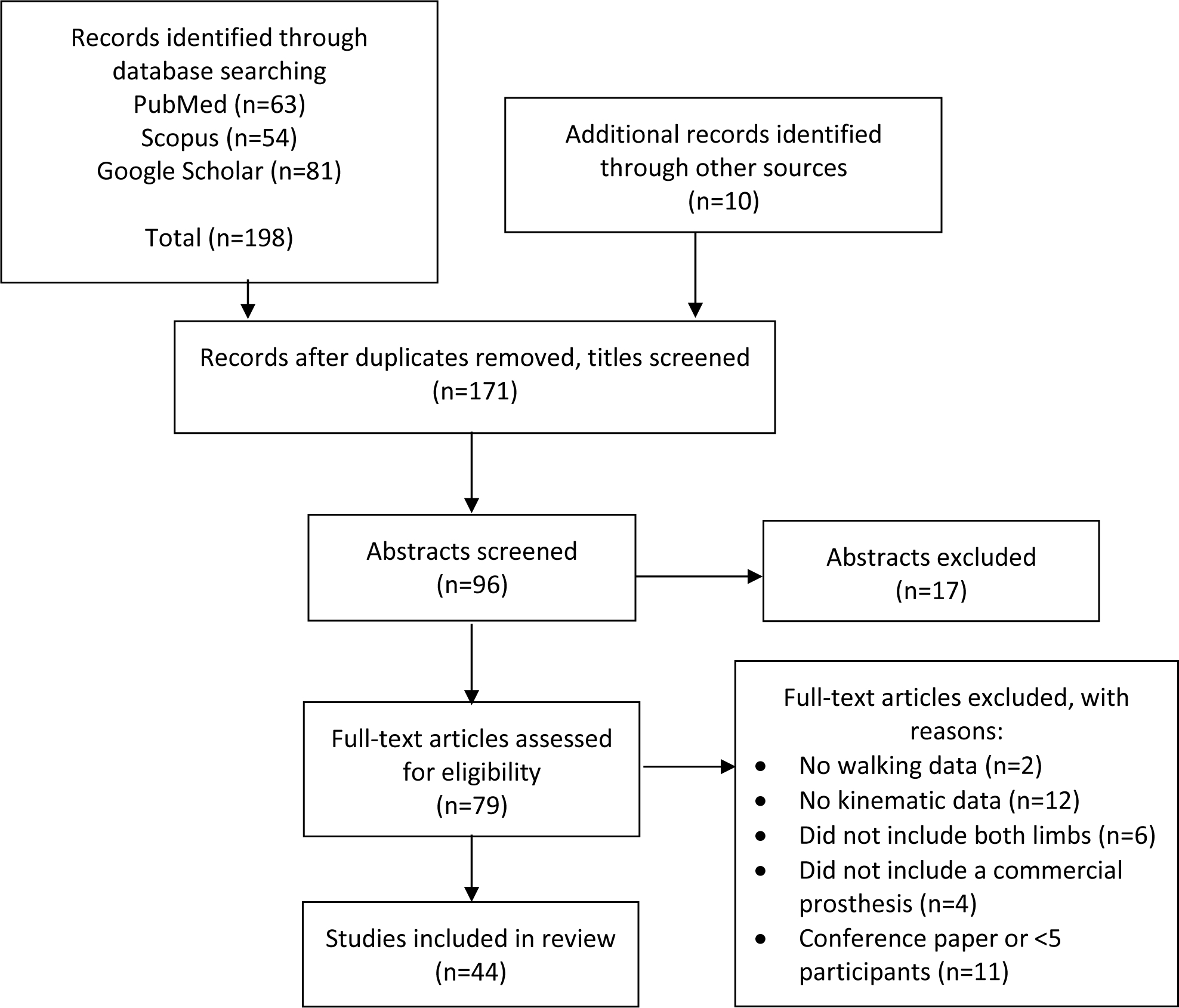
Flow diagram of inclusion process.
Studies were excluded based on the following criteria:
Case reports (defined as less than 5 participants)
Conference papers
Novel development or testing of prosthetic components not commonly prescribed in clinical practice
Participants performed movement tasks other than walking (e.g., stairs, running)
Computer modeling was used in place of participant testing
Many studies included in this review investigated parameters other than kinematics such as kinetics, energy consumption, or patient preference. Several studies also investigated movement tasks other than walking, such as traversing stairs or inclines, navigating turns, or performing sit-to-stand transitions. Only the portions of each study that met the inclusion criteria were discussed in this review.
The most common participant demographics, kinematic parameters, and mathematical analysis of symmetry were identified across studies. Findings by level of limb loss and prosthetic factors were then determined by using the most common mathematical analysis of symmetry identified in this review to recalculate symmetry data across studies for the five most common kinematic parameters in this review.
Normalizing data typically involves recalculating values to a range between 0 and 1.15 This review normalized data to a range between 0 and 100% between-limb symmetry across studies. Several conversions were made to report results consistently. All spatiotemporal units were converted to meters (m) and seconds (s). The most common mathematical analysis of symmetry in this review was Eq. 1, which provides asymmetry percentages.
| Eq. 1 |
I represents the intact limb and P represents the prosthetic limb. Perfect symmetry is a value of 0% and perfect asymmetry is a value of either 100% if intact limb values are greater or −100% if prosthetic limb values are greater. Therefore, an absolute value of 100 – Eq. 1 was used to provide symmetry percentages, resulting in 100% representing perfect symmetry and 0% representing perfect asymmetry.
Out of the 44 studies included in this review, 34 studies could be converted to normalized symmetry values. The remaining 10 studies could not be normalized because symmetry was examined through ratio scales or waveform analysis, and did not provide prosthetic and intact limb values necessary for recalculation using Eq. 1.15–24
RESULTS
This review included 44 studies after applying inclusion and exclusion criteria. Table 1 summarizes each study by objective, participant demographics, prosthetic componentry of participants, kinematic parameters measured, and mathematical analysis of symmetry. Results are reported in the following sections: participant demographics, kinematic parameters, and mathematical analysis of symmetry.
Table 1.
Overview of 44 studies included in this review.
| Author, Year | Objectives | Participants | Prosthesis Components | Kinematic Parameters | Assessment of Symmetry |
|---|---|---|---|---|---|
| 1. Astrom and Stenstrom, 2004 | Investigate effects of using a polyurethane liner on gait and socket comfort | 7 TT (4M 3F); Vascular (4), Nonvascular (3); Age (mean 46, range 23–71 years) | Prescribed silicone liners: Iceross(5), EVA(2); polyurethane liner used for study; Feet: Conventional (5), Flex(2) | Spatiotemporal: WS, StepL, StepT, SLS; Joint angles: Knee ROM during step period, Knee ROM at LR, Knee varus/valgus during stance |
((I-P)/ (.5*(I+P)) *100 |
| 2. Bai et al., 2017 | Kinematic and biomimetic assessment of a hydraulic ankle/foot (Echelon) compared with a fixed prosthetic ankle/foot (Esprit) | 5 TF (all M); Age (range 27–65 years): 12 Controls (5M 7F); Age (mean 26 SD 2 years) |
Knee: KX06(2), Linx(2), IP(1); Feet: Echelon VT(1), Elan(2), Linx(2); fitted with Echelon (hydraulic) and Esprit (fixed) for study | Spatiotemporal: WS, StepL, StanceT, StrideL; Joint angles: Ankle PF peak, Ankle DF peak, Ankle MS Eversion |
Statistical comparison |
| 3. Bateni and Olney, 2002 | Identify kinematic characteristics of gait in TT and compare results to other studies | 5 TT (all M); Trauma(all); Age (range 32–77 years) | Foot: SAFE foot (all) | Spatiotemporal: WS, StrideL, StrideT, StanceT, DLS Time; Joint angles: Knee ROM, Hip ROM |
Statistical comparison |
| 4. Carse et al., 2020 | Identify differences in gait symmetry between NA and established unilateral TF mechanical knee users and characterize common gait deviations in TF group | 60 TF or KD IULLPs (49M 11F); Trauma(32), Infection(7), PAD w/o diabetes(7), PAD w/diabetes(1), Tumor(8), Other(5); Age (mean 51.1 SD 15.2 years); K2(10), K3(31), K4(18); 10 Controls (5M 5F) |
Sockets: IsC(37) Quad(19), Distal end bearing(4); Suspension: Seal-in(18), Total suction(15), Pin(9), Waist belts(13), Other(5) Knee: Polycentric(20), Hydraulic yielding(15), Stance (weight) activated(19), Single axis (alignment controlled)(1), Hand operated knee lock(2), Semi-automatic knee lock(1), Fluid controlled hydraulic(1), Other(1) | WS, StepL, StepT, BoS, COM deviation | Ratio |
| 5. Chow et al., 2006 | Investigate effects of anteroposterior translations and tilts in prosthesis alignment on gait symmetry | 7 TT (6M 1F); Age (range 32–58 years) | Sockets: PTB and SACH; some originally used exoskeletal designs; all used endoskeletal designs for study | Spatiotemporal: StepL, StanceT; Joint angles: Knee Flex at LR, Time to Knee Flex at LR, Max Knee Flex during Swing, Time to Max Knee Flex during Swing, Knee ROM |
(I-P) /(.5*(I+P))*100; absolute value |
| 6. Clemens et al., 2020 | Measurement of gait symmetry and repeatability using IMUs | 128 total IULLPs; 65 TT (34M and 31F) Age (mean 51 SD 14.1 years) 63 TF (27M and 36F) Age (mean 47.9 SD 16.2 years) |
NR | Thigh: Segmental Symmetry Score (SSS) and Segmental Repeatability Score (SRS); Shank: Segmental Symmetry Score and Segmental Repeatability Score; sagittal angular velocities of the thigh and shank |
100 − (100 ∗ x/y) where x is the average Angular Velocity Difference value, and y is the threshold of symmetry |
| 7. Cutti et al., 2018 | Determine reference values for gait temporal asymmetry | 60 K3-K4 total IULLPs; Trauma(all); 23 TT Age (mean 44 SD 14 years); 37 TF Age (mean 46 SD 10 years): 10 Controls |
Knee: Mechanical (12-including TotalKnee 2100(5), 3R60(2), Mauch(2)), C-leg (25); Feet: Vari-flex or Vari-flex LP foot, 1C40, Truestep, Esprit | StepT, StanceT | Ratio; StepT= I/P, StanceT= I/P |
| 8. Darter et al., 2013 | Investigate if home-based treadmill training improves gait performance in established unilateral TF MPK users | 8 TF; Trauma or Cancer; Age (mean 41.4 SD 12.1 years) | Knee: MPKs | StepL, StanceT | Ratio; StepL= longer/shorter, StanceT = P/I |
| 9. Darter et al., 2017 | Investigate locomotor adaptability on a split belt treadmill | 10 TT (all M); Trauma(all); Age (mean 32.2 range 23–39): 8 Controls |
Suspension: Suction with sleeve(8), Pin lock(1), Elevated vacuum(1) Feet: Vari-flex XC(5), Soleus Tactical(3), Re-flex Rotate(1), Kinterra(1) |
StepL, StanceT, Limb Excursion | (fast-slow)/ (fast + slow) |
| 10. De Asha and Buckley, 2015 | Investigate effects of walking speed on minimum toe clearance, and the temporal relationship between minimum clearance and peak swing-foot velocity | 10 TT (all M) Age (mean 48 SD 11.7 years) | Feet: Esprit | Minimum toe-ground clearance, Peak Swing Velocity | Statistical comparison |
| 11. Gholizadeh et al., 2014 | Investigate effects of suction and pin/lock suspension systems on gait performance | 10 TT; Trauma(5) Diabetes(5); Age (mean 45.8 SD 14.4 years); K2(4) K3(6) | Each participant used each suspension: Iceross Dermo Liner with pin lock, Iceross seal-in suction; Feet: Flex foot | Spatiotemporal: WS, StepL, StrideL, StanceT and SwingT; Joint Angles: Hip Position IC, Max Hip Ext, Hip ROM, Knee Position IC, Max Knee Flex Stance, Max Knee Flex Swing, Knee ROM, Ankle Position IC, Max Ankle PF Stance, Max Ankle PF Swing, Max Ankle DF Stance, Ankle ROM |
((I-P) / (.5*(I+P))) *100 |
| 12. Gholizadeh et al., 2020 | Compare effects of unity suspension system on gait between vacuum on and off conditions | 12 TT (11M 1F); Trauma(8), Diabetes(3), Infection(1); Age (mean 57.2 SD 15.3 years); K3(10) and K4(2) | Suspension: Pin-lock(9), Suction(2); fit with Unity elevated vacuum suspension and Pro-flex XC foot for study | Spatiotemporal: WS, StepL, Step width, StepT, StrideL, StrideT, StanceT, SwingT, SLS Time, DLS Time; Joint Angles: Hip ROM, Peak Hip Flex early Stance, Knee ROM, Peak Knee Flex Swing, Knee Flex IC, Ankle ROM, Peak Ankle PF early Stance, Peak Ankle DF Stance |
((I-P) / (.5*(I+P))) *100 |
| 13. Graham et al., 2007 | Compare gait symmetry between conventional (Multiflex) and ESAR(Vari-flex) prosthetic feet in high-functioning TF | 6 TF (all M): Age (range 34–50) | Knee: Blatchford stabilized with pneumatic swing phase control(1), IP (5); Feet: Multiflex(all); Foot changed to Vari-flex for study | Spatiotemporal: StepL, StanceT; Joint Angles: Ankle DF Late Stance, Knee Flex Midswing, Hip Flex Late Swing, Hip Ext Late Stance, Transverse Pelvic Rotation |
Ratio |
| 14. Hak et al., 2014 | Determine if stepping asymmetry might be functional in terms of gait stability | 10 TT (9M 1F); Trauma(8), Dysvascular(1), Other(1); Age (range 21–66) | Socket: TSB(1) PTB(9); Feet: Axtion(1), Elite VT(1), 1C40(3), Vari-flex EVO(2), Fusion(1), Celsus(1), Propiofoot(1) | StepL, FFP, Trunk Progression | (I / ((I+P)/2)*100 |
| 15. Hekmatfard et al., 2013 | Investigate effects of four prosthetic mass conditions on spatiotemporal knee kinematics | 10 TF (all M); Trauma(all); Age (range 27.2–60) | Socket: IC; Suspension: belt; Knee: single axis w/ext. assist; Foot: single axis | WS, Cadence, walking distance, StepL, StrideL, Step speed, gait cycle duration, Stance T, SwingT, COM | Statistical comparison |
| 16. Highsmith et al., 2010 | Determine differences in spatiotemporal parameters between transtibial and transfemoral IULLPs | 15 total IULLPs; 7 TT (all M); Trauma(3), PVD(3), Tumor(1); Age (range 32–70 years) 8 TF (all M); Trauma(all); Age (range 21–72 years) |
Suspension: shuttle lock(7-all TT), suction(6), seal-in (2) Knees: C-Leg(6), Rheo(1), Plie(1); Feet: Trustep(1), Proprio(1), Perfect stride II(1), Vari-flex(2), Renegade(2), Ceterus(1), 1C40(2), Reflex-VSP(1), ESAR foot where brand not indicated(2), Journey(1), Luxon Max(1) | WS, Cadence, StepL, Step width, StepT | ((I-P) / (I+P)) |
| 17. Houdijk et al., 2018 | Compare StepL symmetry and MoS between Vari-flex to SACH prosthetic feet | 15 TT (all M); Trauma(all); Age (mean 55.8 SD 11.1 years); K3(all) | all originally used ESAR foot; Feet: Variflex vs SACH foot | StepL, backward MoS | Statistical comparison |
| 18. Johansson et al., 2005 | Compare kinematics between the Mauch hydraulic knee, C-Leg MPK, and Rheo MPK | 8 TF LLPs (7M 1F); Trauma(3), Infection(2), Cancer(2), Congenital(1); Age (range 29–54 years) | Suspension: suction(6), silesian belt(1), pin-lock(1) | WS, StepL, StepT, SLS Time, DLS Time | Statistical comparison |
| 19. Kahle and Highsmith, 2014 | Compare gait, balance, and subjective analysis between IsC and brimless TF socket designs with vacuum assisted suspension | 10 TF (8M 2F); Trauma(7), PVD(2), Sarcoma(1); Age (mean 42.9 years) | Same liner, pump, knee, and foot utilized in both conditions; Knee: SAFE(1), C-leg(9); Feet: ESAR | WS, StepL, StepT, BoS width, SLS Time, DLS Time, Swing Time, StanceT | ((I-P) / (I+P)) |
| 20. Kaufman et al., 2012 | Compare gait asymmetry between TF of mechanical and MPKs | 15 TF (12M 3F); Trauma(7), Cancer(6), PVD(1), Congenital(1); Age (mean 42 range 26–57 years); K3 and K4: 20 NA (9M 11F); Age (mean 26 SD 9 years) |
Knee: session one with mechanical fluid controlled knee prosthesis (Mauch SNS(11), CaTech(2), Black Max(1), Total Knee 2000(1)); session 2 with Otto Bock C-Leg; Feet: kept same; Luxon Max(5), Dynamic Plus(1), College Park(1), Axtion(8) | Hip Stance, Hip Swing, Knee Stance, Knee Swing, Ankle Stance, Ankle Swing | Entire waveform analysis; singular value decomposition; subtracted the mean value from every value in the waveform |
| 21. Keklicek et al., 2019 | Compare gait variability and symmetry between trained individuals TT and TF | 25 total IULLPs; 14 TT (12M 2F); 11 TF (4M 7F); Trauma(all): 14 Controls (8M 6F) |
Knee: mechanical knee joint (Otto Bock 3R15); Feet: dynamic (Otto Bock 1D10) for both TT and TF Amps | StepL, StepL % Variability, StanceT, Ambulation Index Score (relative to 100 based on foot-to-foot time distribution ratio and average step cycle) | Statistical comparison |
| 22. Kovac et al., 2010 | Investigate spatial, temporal and kinematic characteristics in traumatic TT amputee gait | 12 TT (all M); Trauma(all); Age (mean 40.25 SD 6 years): 12 Controls; Age (mean 37.46 SD 5.25 years) |
Feet: Dynamic foot(7), Greissenger foot(2), Flex foot(2) | WS, Cadence, StepL, StrideL, StrideT, Swing Velocity, StanceT, SwingT, DLS Time | Statistical comparison |
| 23. Marinakis, 2004 | Compare interlimb symmetry in the early rehabilitation stage between two different prosthetic feet (Greissenger Plus and SACH) | 9 TT (all M); Trauma (all); Age (mean 54.3 years SD 2.1 years): 13 Controls (all M); Age (mean 52.3 years SD 11.3 years) |
PTB socket with removable prosthetic liner (all); used Greissenger Plus and SACH for study | Spatiotemporal: WS, Cadence, StepL, StepT, StanceT, StrideT, %StrideT (division of StanceT by the StrideT and multiplied by 100); Joint Angles: Hip ROM, Knee ROM, Ankle ROM |
Method 1: 100* min(P,I)/max(P,I); Method 2: 100-((100*(P-I)) /(.5*(P+I))) for absolute difference; Method 3: 100-(P-I)(*50/max(P,I)-min(P,I))) |
| 24. Mattes et al., 2000 | Investigate walking symmetry after matching prosthetic and intact limb inertial properties | 6 TT; Age (mean 35 SD 12 years); Trauma(3), Blood Clot(1), Cancer(1), Congenital(1) | NR | StepL, SwingT, StanceT | ((P-I) / (.5*(P+I))) *100 |
| 25. Mishra et al., 2019 | Compare kinematic gait symmetry between the Jaipur knee joint to each participant’s prescribed prosthesis | 11 TF (9M 2F); Age (mean 45 range 26–66 years); Trauma(8), PVD(2), Cancer(1) | Knee: Jaipur used in study; prescribed prostheses NR | Hip ROM, Knee ROM, Ankle ROM; all separated into swing and stance | Entire waveform analysis; singular value decomposition; subtracted the mean value from every value in the waveform |
| 26. Moore, 2016 | Compare StanceT asymmetry between hydraulic ankle units(Avalon for K2 and Echelon for K3) and previous prescription | 13 total IULLPs; 7 TT; 6 TF; K3(6) K2(7) | Feet: K2 level= originally used Multiflex(12). K3 level= on the Multiflex(3), Javelin(2), Dynamic Response (1), Re-flex VSP(1), Seattle Lite-foot(1), Elite Blade(1), 1D10(1); Echelon (K3) and Avalon (K2) feet for study | StanceT | Statistical comparison |
| 27. Morgan et al., 201683 | Compare effects of a concurrent cognitive task on walking between TF MPK users and NA | 14 TF (9M 5F); Trauma(8) Tumor(3) Vascular(1) Infection(2); Age (mean 53.8 SD 13.6 years): 14 Controls |
Suspension: suction, seal-in, or pin-locking liners; Knee: all MPK= C-Leg, Genium, X2 | WS, Cadence, Step Width, StepT, StrideL | Absolute value of the difference between right and left |
| 28. Moylan et al., 2015 | Investigate effects of increased prosthetic mass on gait symmetry in dysvascular TF | 10 TF (9M 1F); PVD(all); Age (mean 64 range 52–78 years); No assistive device(2), Cane(3), Walker(3), Rollator(2) | Suspension: suction(3), silesian belt(7); Knee: Mauch SNS(4), Locked(6) Foot: SACH(4), Single axis(4), Multi-axis(2) | StepL, StepT, Step Width, SLS Time | ((I-P) / (I+P)) |
| 29. Nadollek et al., 2002 | Investigate the relationship between quiet stance ability, strength of the hip abductor muscles, and gait | 22 TT; PVD(10), Diabetic complications(12); Age (mean 71.7 range 54–86 years) | Socket: PTB or patella tendon supracondylar prosthesis; Suspension: cuff, silicone liner, or shuttle lock | WS, Cadence, StepL, StrideL, Stance: Swing Ratio, DLS Time | Statistical comparison |
| 30. Nolan et al., 2003 | Compare WS gait symmetry between TF, TT, and NA | 8 total IULLPs; 4 TT Age (mean 29 SD 18.9 years); 4 TF Age (mean 31.5 SD 10.9 years); Trauma(all): 6 Controls (32.2 SD 9.3 years) |
Knee: hinge knee prosthesis with SACH foot(all TF); Feet: SACH foot(all TT) | StepT, StanceT, SwingT | (I-P)/ (.5*(I+P)) *100; absolute value |
| 31. Orekhov et al., 2019 | Investigate knee joint biomechanics in gait, cycling, and elliptical training | 10 TT (7M 3F); Age (mean 32.2 SD 6.7 years): 10 Controls; Age (range 20–26 years) |
Foot: Vari-Flex; (8) originally used this foot | Max MS Knee Flex Angle (and timing), Max Swing Knee Flex Angle (and timing) | Statistical comparison |
| 32. Petersen et al., 2010 | Compare gait symmetry between the C-leg MPK and hydraulic 3R60 in TF | 5 TF (4M 1F); Trauma(3), Cancer(2); Age (range 26–48 years) | Socket: IsC(4), Stump end bearing socket(1); Knee: C-leg and 3R60 (all originally used C-Leg but had past experience with hydraulic knees) Feet: Pacifica LP(1), Renegade(1), C-Walk(1), Axtion(1), Flex-foot(1) | StepL, StanceT, SLS Time, Temporal Symmetry % (calculated from duration of stance phase), Spatial Symmetry % (calculated from step length) | ((I-P)/ (.5*(I+P)) * 100; absolute value |
| 33. Roerdink et al., 2012 | Determine if StepL asymmetry should be measured in conjunction with FFP and trunk progression | 3 TT (2M 1F); Vascular(1), Trauma (2); Age (range 29–68): 7 TF (1F 6 M); Vascular(4), Trauma(3); Age (range 50–68) |
Knees= 3R60(2), OFM1(1), 3R33(1), Hybrid Knee N1-C311(1), 3R106(1), C-leg(1); Feet: Multiflex(2), 1D10/1D11(4), 1C30 Trias(1), Vari-flex with EVO(1), Flex-Foot Assure(1), C-Walk 1C40(1) | StepL, FFP, Trunk Progression | ((P-I)/(P+I)) * 100 |
| 34. Rowe, 2014 | Determine if music improves self-regulated walking in terms of cadence and gait symmetry in TT with nontraumatic amputations | 17 TT (15M 2F); Vascular(10), Congenital(5), Complications following trauma(2); Age (mean 52.2 SD 12.9 years) | Participants using microprocessor or carbon fiber spring feet not included | WS, Cadence, StepL, StepT, SLS Time | ((P-I)/ (.5*(P+I))) *100 |
| 35. Schaarschmidt et al., 2012 | Compare gait symmetry between the C-Leg MPK and the hydraulic 3R80 in TF | 5 TF; Trauma(all); Age (mean 42.6 SD 13.4 years) | Knees: C-Leg (all, all had prior experience with mechanical knees) Feet: C-Walk | StepT, StanceT, SLS Time, DLS time | ((P-I)/ (.5*(P+I))) *100 |
| 36. Segal et al., 2006 | Compare gait symmetry between the C-Leg MPK and the Mauch SNS hydraulic knee after 3 month acclimation periods with each knee | 8 TF (7M 1F); Age (mean 29 years) 6 Controls (all M) |
Socket: thermoplastic(4),carbon fiber(4); Suspension: pin(6), suction(2); Knees: C-Leg (all), Mauch SNS (all); Feet of C-Leg users: Dynamic Plus(5), C-Walk(1), LuXon Max(2); Feet of Mauch SNS users: Seattle Lite Foot(5), Flex Walk Foot(3) | Spatiotemporal: WS, StepL; Joint Angles: Max Knee Flex in early stance, Knee Flex at opposite heel strike, Max Knee Flex during Swing |
Statistical comparison |
| 37. Sjodahl et al., 2002 | Compare gait in the sagittal plane before and after special gait re-education | 9 TF (5M 4F); Trauma or Tumor; Age (mean 33 range 16–51 years): 18 total Controls; 9 Controls (all M); Age (mean 33 range 21–47 years): 9 NA (all F); Age (mean 39 range 25–52 years) |
Socket: IsC(3), Quad(6) Knee: Total knee mechanical(3), Aqua pend pneumatic(3), T-Ling pneumatic(1), Mauch knee hydraulic(1), Vaxjo knee hydraulic(1) Feet: Seattle foot(2), Flex foot(6), Multiflex(1), Multiaxis Vaxjo foot(1) | Spatiotemporal: WS, Cadence, StepL, SLS Time, DLS Time; Joint Angles: Hip Flex ROM, Knee Flex ROM, Ankle ROM |
Statistical comparison |
| 38. Smith and Martin, 2013 | Investigate effects of prosthetic mass distribution on walking symmetry | 6 TT (5M 1 F); Trauma(5) Congenital bone disease(1); Age (mean 47 SD 16 years) | Feet: Genesis(1), College Park(3), Flex-foot(2) | StanceT, SwingT, Max Knee Angular Velocity during Swing, Max Thigh Angular Velocity during Swing | ((P-I) / (.5*(P+I))) *100 |
| 39. Supan et al., 2010 | Investigate effects of a Talux prosthetic foot on gait parameters of nonvascular TT | 10 TT (7M 3F); Nonvascular(all); Age (range 34–62 years) | Talux (3 originally used Talux) | Spatiotemporal: WS, Cadence, StepL, StepT, %SLS, StanceT; Joint Angles: Hip Position at IC, Hip Max Ext, Hip ROM, Knee Position at IC, Knee Max Flex at Stance, Knee Max Ext at Stance, Knee Max Swing Flex, Knee ROM, Ankle Position at IC, Ankle Max PF at Stance, Ankle Max DF at Stance, Ankle Max PF at Swing, Ankle ROM, Foot Progression Angle at IC, Foot Progression Angle Min at Swing, Foot Progression Angle ROM |
Statistical comparison |
| 40. Svoboda and Janura, 2007 | Investigate effects of prosthetic alignment (DF and PF) and prosthetic foot length changes (shorter and longer) on temporal symmetry of I and P limbs | 11 TT (all M); Age (mean 58 SD 9.47 years) | Feet: all dynamic feet characterized by a smooth rollover during gait and intended for second level activity users | StanceT, SwingT, %Stance (StanceT/duration of gait cycle) | ((I-P) / (I+P)) * 100 |
| 41. Uchytil et al., 2014 | Compare spatiotemporal parameters between the Rheo MPK and the Mauch SNS hydraulic knee in TF | 8 TF (4M 4F); Age (mean 38.2 SD 6.1 years); K3(all) 10 Controls (8M 2F); Age (mean 27.6 SD 5.2 years) |
All used ischial containment and SACH foot; Knees: Rheo MPK, Mauch SNS hydraulic knee | StepL, StepT, StanceT, SwingT | ((I-P)/ (.5*(I+P)) * 100 |
| 42. Uchytil et al., 2017 | Compare pelvis and lower limb joint angles in TF Rheo MPK and hydraulic knee joint users | 11 TF (6M 5F); Trauma(3), Cancer(7),; Age (mean 39.2 SD 10.1 years): 10 Controls (8M 2F); Age (mean 27.6 SD 5.2 years) |
All used IsC socket and SACH foot; Knee: Rheo MPK, Hydraulic | Pelvis: Min Pelvic Tilt, Min Pelvic Obliquity, Max Pelvic Obliquity, Max Rot; Hip: Flex IC, Max Ext in Stance, Max Flex in Swing, Max Add in Stance, Max Abd in Swing, Max Int Rot in Stance, Max Ext Rot in Swing; Knee: Flex at IC, Max Flex during LR, Max Ext Stance, Max Flex Swing, Max IR in Stance, Max ER in Swing |
((I-P) / (I+P)) * 100 |
| 43. Xu et al., 2017 | Investigate effects of vacuum level on gait characteristics in TT of elevated vacuum suspension | 9 TT; Trauma(5), Vascular(1), Other(3); Age (mean 51.1 SD 16.1 years); K3(7) and K4(2): 9 Controls; Age (mean 27.8 SD 3.7 years) |
all originally used elevated vacuum suspension | Spatiotemporal: WS, Cadence, StepL, StepT, StanceT, SLS Time, DLS Time; Joint Angles: Hip Ext Stance, Hip Abd Swing, Hip ER Swing, Hip ROM Sagittal, Hip ROM Frontal, Hip ROM Transverse, Knee Flex Swing, Knee ROM Sagittal, Knee ROM Frontal, Knee ROM Transverse, Ankle DF Stance, Ankle PF Swing, Ankle ROM Sagittal |
Statistical comparison |
| 44. Yang et al., 2018 | Compare gait patterns between two different shapes of ESAR prosthetic feet: 1C30 Trias and 1C60 Triton (has split forefoot and heel wedge) in TT | 10 TT; Age (mean 63.8 SD 2.49 years); K2(4) and K3(6) | 1C30 Trias, 1C60 Triton; none originally used ESAR feet | Spatiotemporal: WS, Cadence, StepL, Step Width, StanceT, SwingT; Stance: Swing Ratio Joint Angles: Hip Ext at TS, Hip Flex at Midswing, Knee Flex at TS, Knee Flex at Midswing, Ankle PF at IC, Ankle DF at MS, Ankle PF at TS, Ankle Pronation at early MS, Ankle Supination at onset of Preswing |
Statistical comparison |
Abbreviations: TT= individuals who use transtibial prostheses, TF= individuals who use transfemoral prostheses, IULLPs= individuals who use unilateral lower-limb prostheses, M= male, F= female, I= intact, P= prosthetic, SD= standard deviation, ESAR= energy storage and return, PTB= patellar tendon bearing, SACH= solid ankle cushion heel, MPK= microprocessor knee, IsC= ischial containment, WS= walking speed, StepL= step length, StepT= step time, StrideL= stride length, StrideT= stride time, StanceT= stance time, SwingT= swing time, SLS= single limb support, DLS= double limb support, BoS= base of support, MoS= margin of stability, FFP= forward foot placement, COM= center of mass, ROM= range of motion, Min= minimum, Max= maximum, PF= plantarflexion, DF= dorsiflexion, Flex= flexion, Ext= extension, Add= adduction, Abd= abduction, IR= internal rotation, ER= external rotation, IC= initial contact, MS= midstance, LR= loading response, TS= terminal stance.
Liner manufacturer: Iceross (Ossur, Reykjavik, Iceland).
Knee manufacturers: KX06, Linx, IP, CaTech, Black Max (Blatchford, USA, Canada, and UK); Jaipur Knee (BMVSS organization, Jaipur, India); Hybrid Knee N1-C311 (Nabtesco, Kobe, Japan); Rheo, Total Knee 2000, Total Knee 2100, Mauch SNS, OFM (Ossur, Reykjavik, Iceland); C-leg, Genium, X2, 3R60, 3R15, 3R33, 3R106, Aqua Knee (Ottobock, Duderstadt, Germany); SAFE (ST&G, California, USA).
Foot manufacturers: Foot manufacturers: Echelon, Echelon VT, Elan, Linx, Esprit, Multiflex, Javelin, Elite Blade, Avalon (Blatchford, USA, Canada, UK); Celsus, Truestep, Soleus Tactical (College Park, MI, USA); Genesis II (MICA Manufacturing Corp, WA, USA); Kinterra, Pacifica LP, Renegade (Freedom Innovations, CA, USA); Vari-flex, Vari-flex LP, Vari-flex XC, Vari-flex EVO, Pro-flex XC, Propiofoot, Reflex VSP, Reflex Rotate, Flex-foot, Flex-foot Assure, Talux (Ossur, Reykjavik, Iceland); Axtion, 1C30 Trias, 1C60 Triton, 1C40 C-Walk, 1D10, 1D11, Greissenger Plus, LuXon Max (Otto Bock, Duderstadt, Germany); Seattle Lite-foot (Trulife, USA, Canada, UK, Ireland); Fusion (Willowwood, OH, USA).
PARTICIPANT DEMOGRAPHICS
The highest number of IULLPs in a single study was 128,25 followed by 60 in two studies.15,16 However, 84.1% of studies included 15 or less IULLPs, and 61.4% of studies included 10 or less IULLPs. Half of studies included both females and males (n=22, where n indicates the number of studies) and several studies only included males (n=12) or did not report sex (n=10). The mean age of IULLPs ranged from 29.0 to 71.7 years. IULLPs with traumatic etiologies were included in over twice as many studies (n = 31) as those with vascular etiologies (n=15). Eleven studies did not report the etiology of participants.
Functional activity levels are assigned to IULLPs based on ambulation potential, and defined by Medicare as K-levels (K0-K4).26 No studies included in this review had IULLPs at K0 or K1 functional activity levels. Therefore, this review defines lower functional activity as K2, and higher functional activity as K3 or K4. Only six studies included at least one IULLP at a lower functional activity level of K2,15,17,18,27–29 while the remaining studies included IULLPs at higher functional levels of K3 or K4.
KINEMATIC PARAMETERS
The most common spatiotemporal parameters were step length (n=31) and stance time (n=27). The most common joint angle parameters were sagittal plane range of motion (RoM) at the hip (n=12), knee (n=16), and ankle (n=12). Few studies investigated all five of these parameters (n=8).
The most common equipment used to assess symmetry was motion capture (n=29), followed by the GaitRite system (n=5), instrumented insoles (n=2), instrumented treadmills (n=3), and inertial measurement units (IMUs) (n=1).
MATHEMATICAL ANALYSIS OF SYMMETRY
Symmetry index equations were most commonly used to assess interlimb symmetry (n= 20). The most common equation, which provides an asymmetry value, was Eq. 1 (n=6). Many studies did not directly calculate symmetry, but used statistical comparison (n=16), ratio scales (n=5), waveform analysis (n=2), or developed their own measures of symmetry (n=1) to examine differences between limbs.
FINDINGS BY LEVEL OF LIMB LOSS AND PROSTHETIC FACTORS
Findings by level of limb loss and prosthetic factors are summarized by differences between limbs in metric units (seconds, meters, degrees) in Table 2 and normalized symmetry percentages in Table 3. Individual study values used to calculate summaries in Tables 2 and 3 can be found in Supplementary Data Tables. Individuals who used unilateral transtibial prostheses were most frequently included (n=27), followed by individuals who used unilateral transfemoral prostheses (n=25), and individuals without limb loss were included as a control group in 15 studies. Individuals without limb loss tended to have the most symmetry, followed by individuals who used transtibial prostheses, then individuals who used transfemoral prostheses.
Table 2:
Differences Between Prosthetic and Intact Limbs
| Summary | Step Length Differences (m): | Stance Time Differences (s): | Stance Time Differences (% gait cycle): | Overall Hip RoM Differences (°): | Overall Knee RoM Differences (°): | Overall Ankle RoM Differences (°): |
|---|---|---|---|---|---|---|
|
| ||||||
| Ranges by Level of Limb Loss | Control= 0.003 – 0.01 | Control= 0.001 – 0.02 | Control= 0.71 | Control= NR | Control= 1.5 | Control= NR |
| TT= 0.01 – 0.12 | TT= 0.01 – 0.04 | TT= 0.07 – 5.15 | TT= 0.63 – 3.05 | TT= 1.43 – 14.6 | TT= 0.8 – 12.2 | |
| TF= 0.008 – 0.164 | TF= 0.01 – 0.24 | TF= 5.0 – 20.7 | TF= 3.72 – 19.0 | TF= 1.01 – 16.7 | TF= 2.4 – 7.7 | |
|
| ||||||
| Ranges by Prosthetic Feet | SACH= 0.05 | SACH= NR | SACH= NR | SACH= NR | SACH= NR | SACH= NR |
| ESAR= 0.01 – 0.13 | ESAR= 0.04 – 0.07 | ESAR= 0.3 – 8.0 | ESAR= 0.63 – 1.47 | ESAR= 1.43 – 3.19 | ESAR= 2.4 – 12.2 | |
|
| ||||||
| Ranges by Prosthetic Knees | Hydraulic= 0.04 – 0.09 | Hydraulic= 0.07 – 0.11 | Hydraulic= 7.4 | Hydraulic= 8.75 | Hydraulic= 1.01 – 13.4 | Hydraulic= NR |
| MPKs= 0.03 –0.07 | MPKs= 0.03 – 0.13 | MPKs= 5.3 | MPKs= 3.72 | MPKs= 1.26 – 16.74 | MPKs= NR | |
Table 2: Summary of studies (31 total) that reported raw values for prosthetic and intact limbs or differences between limbs in meters (m), seconds (s), % of the gait cycle, or degrees (°) for step length, stance time, or overall sagittal range of motion (RoM) at the hip, knee, and ankle. Studies that measured stance time either reported values in seconds or % of the gait cycle, so these are reported separately. Results are taken from level ground walking conditions at self-selected walking speeds. Baseline conditions and intermediate walking speeds were chosen if multiple conditions or speeds were tested. Normalized symmetry percentages calculated from these raw values are reported in Table 3. NR= not reported, TT= individuals who use unilateral transtibial prostheses, TF= individuals who use unilateral transfemoral prostheses, IULLPs= individuals who use unilateral lower-limb prostheses, SACH= solid ankle cushion heel, ESAR= energy storage and return, MPK= microprocessor knee.
Table 3:
Normalized Symmetry Percentages
| Step Length (% Symmetry from m) | Stance Time (% Symmetry from s) | Stance Time (% Symmetry from % gait cycle) | Overall Sagittal Hip RoM (% Symmetry from °) | Overall Sagittal Knee RoM (% Symmetry from °) | Overall Sagittal Ankle RoM (% Symmetry from °) | |
|---|---|---|---|---|---|---|
|
| ||||||
| Ranges by Level of Limb Loss | Control= 97.0 – 99.6 | Control= 97.2 – 99.8 | Control= 98.6 | Control= NR | Control= 96.2 | Control= NR |
| TT= 81.3 – 98.0 | TT= 78.9 – 98.8 | TT= 81.3 – 99.9 | TT= 85.7 – 99.8 | TT= 70.8 – 97.8 | TT= 23.7 – 96.1 | |
| TF= 66.4 – 98.5 | TF= 74.5 – 98.4 | TF= 58.6 – 91.6 | TF= 55.0 – 91.9 | TF= 70.5 – 98.2 | TF= 53.2 – 83.2 | |
|
| ||||||
| Ranges by Prosthetic Feet | SACH= NR | SACH= 78.9 | SACH= NR | SACH= 85.7 | SACH= 84.9 | SACH= 23.7 |
| ESAR= 81.6 – 97.3 | ESAR= 97.0 | ESAR= 87.1 – 99.5 | ESAR= 89.0 – 98.5 | ESAR= 91.4 – 97.8 | ESAR= 44.5 – 83.2 | |
|
| ||||||
| Ranges by Prosthetic Knees | Hydraulic= 86.6 – 94.2 | Hydraulic= 74.7 – 91.2 | Hydraulic= 88.2 | Hydraulic= 82.6 | Hydraulic= 77.8 – 98.2 | Hydraulic= NR |
| MPKs= 90.3 – 95.9 | MPKs= 71.4 – 96.0 | MPKs= 91.6 | MPKs= 91.6 | MPKs= 70.5 – 97.7 | MPKs= NR | |
Table 3: Summary of studies (34 total) that could be converted to percentages using 100- Eq. 1. Studies that measured stance time either reported values in seconds or % of the gait cycle, so these are reported separately. Results are taken from level ground walking conditions at self-selected walking speeds. Baseline conditions and intermediate walking speeds were chosen if multiple conditions or speeds were tested. NR= not reported, TT= individuals who use unilateral transtibial prostheses, TF= individuals who use unilateral transfemoral prostheses, IULLPs= individuals who use unilateral lower-limb prostheses, SACH= solid ankle cushion heel, ESAR= energy storage and return, MPK= microprocessor knee.
Half of studies included in this review investigated the influence of prosthetic factors on symmetry (n=22). Specifically, these studies investigated prosthetic factors of as suspension (n=5), alignment (n=2), foot componentry (n=6), and knee componentry (n=9). Suspension and alignment studies compared liners (n=1), transfemoral socket designs (n=1), transtibial suspension methods (n=3), and transtibial alignments (n=2). Foot componentry studies compared energy storage and return (ESAR) to non-ESAR feet (n=3), two different shapes of ESAR feet (n=1), and hydraulic feet to non-hydraulic feet (n=2). Knee componentry studies compared hydraulic knees to microprocessor knees (MPKs; n=5).
DISCUSSION
The objective of this review was to normalize kinematic walking symmetry data in IULLPs by level of limb loss and prosthetic factors to inform considerations in clinical practice and future research. Symmetry tended to decrease as the level of limb loss became more proximal and increase with more advanced prosthetic foot and knee componentry. However, it should be noted studies primarily included 10 or fewer individuals who were less than 65 years of age, had traumatic etiologies, and ambulated at higher functional levels of K3 or K4. While these findings are not novel, this review provides normative symmetry values by level of limb loss and prosthetic componentry as well as considerations for future research in this population, such as including larger sample sizes and individuals who are over 65 years of age, have diabetic etiologies, and ambulate at K2 functional levels to reflect clinical considerations for the majority of IULLPs.
PARTICIPANT DEMOGRAPHICS
Functional activity level, age, and etiology can influence decisions regarding rehabilitation goals in IULLPs. Most IULLPs included in this review were individuals who were less than 65 years of age, had traumatic etiologies, and ambulated at higher functional levels of K3 or K4.
The six studies that included at least one IULLP at a lower functional level of K2 provided normalized symmetry values of 86.2– 97.2% for step length, 92.2– 99.5% for stance time, 96.4– 97.1% for hip RoM, 77.0– 97.8% for knee RoM, and 44.5– 96.1% for ankle RoM. These values were in line with studies that did not include K2 participants, which is not surprising considering few participants were classified as K2 in each of these studies.
General literature has found that walking symmetry declines with age in individuals without limb loss from ≥90% to 80–85% in individuals over 65 years of age.30,31 Many individuals with limb loss are over 65 years of age, and vascular etiologies are the primary cause of amputation.32 Yet, IULLPs 65 years of age or older with vascular etiologies were only included in 12 and 15 studies, respectively. Only two studies exclusively included older IULLPs with vascular etiologies, with mean ages of 64 and 71.7 years.17,28 One study could not be normalized, and the other only measured step length in individuals who used transtibial prostheses, providing normalized symmetry values of 96.6%. In contrast, 10 studies exclusively included IULLPs with traumatic etiologies with mean ages ranging 30 to 45 years across studies.16,22,23,33–39 Normalized symmetry values ranged 89.5– 98.5% for step length, 74.5– 98.4% for stance time, 92.9% for hip RoM, and 87.9% for knee RoM, which were comparable to individuals without limb loss.16,23,34,35
Therefore, IULLPs who are older adults, have vascular etiologies, or ambulate at lower functional activity levels may differ compared to IULLPs that were included in this review. Collecting kinematic walking symmetry data from individuals with these demographic characteristics can help inform clinical considerations in a way that accurately represents the majority of IULLPs.
KINEMATIC PARAMETERS
The most commonly investigated parameters identified in this review, specifically step length, stance time, and knee RoM, were in line with a previous review of individuals who used transtibial prostheses.12 Future studies could include these parameters to improve comparison of findings across studies.
MATHEMATICAL ANALYSIS OF SYMMETRY
The most common mathematical analysis of symmetry in this review were symmetry index equations (n= 18), with the most common equation being Eq. 1 (n=6), or a derivation of Eq. 1 (n=4). This equation was first described by Robinson et al. (1987) and then Herzog et al. (1989) in individuals without limb loss using right and left limbs, rather than prosthetic and intact limbs. Therefore, when applying this equation to IULLPs, it is up to the authors whether to use the prosthetic or intact limb as the reference value. Three studies instead calculated the absolute value of Eq. 1 to obtain only positive values.35,40,41 Absolute values eliminate the need for a reference value, but also eliminate the distinction of which limb had higher or lower values. In this case, researchers could include both absolute percent symmetry values alongside the original data values (Table 2 and Table 3) to ease comparisons across studies.42
Additionally, one study used three different analyses for calculating symmetry with various statistical significance depending on the equation used,43 and one developed symmetry scores based on thigh and shank angular velocity data collected from inertial measurement units.25 These symmetry values were consistent with studies including similar demographics. Until these newly developed equations are consistently used or considered a better representation of symmetry, it is suggested that future studies analyze kinematic walking symmetry data using Eq. 1, in addition to the newly developed equations, to ease comparisons of findings across studies.
FINDINGS BY LEVEL OF LIMB LOSS
In agreement with research prior to 2000,48–51 individuals without limb loss tended to show the most symmetrical gait with values over 90% (97.0– 99.8%), followed by individuals who used transtibial prostheses (70.8– 98.5%), while individuals who used transfemoral prostheses tended to show the least symmetrical gait (53.2– 98.5%).
Spatiotemporal Parameters
Step lengths tended to be longer on the prosthetic limb compared to the intact limb, with more symmetry in individuals who used transtibial prostheses than transfemoral prostheses. Two studies in this review suggested step length differences between prosthetic and intact limbs might be functional compensations to preserve backward margin of stability during double limb support.48,49
Stance times tended to be shorter on the prosthetic limb compared to the intact limb, with more symmetry in individuals who used transtibial prostheses than transfemoral prostheses. Three studies in this review compared stance time symmetries, and found the greatest symmetry in individuals without limb loss, followed by individuals who used transtibial prostheses (89.7– 93.4%), and then individuals who used transfemoral prostheses (58.6– 74.5%).16,34,35 However, individuals without limb loss and individuals who used transtibial prostheses tended to have similar amounts of symmetry in studies included in this review. Individuals who used transfemoral prostheses tended to have the widest range of symmetry across studies with the lowest minimum values.
Joint Angle Parameters
In a study of 78 individuals without limb loss, the ankle was the least symmetrical joint (88.0– 94.0%) compared to the knee (96.0– 98.0%) and hip (96.0– 98.0%).50 The ankle was also the least symmetrical joint for all IULLPs in this review (Table 3). Transtibial values for normalized symmetry averaged 64.7% (23.7– 96.1%) at the ankle compared to 87.7% (70.8– 97.8%) at the knee and 97.8% (85.7– 99.8%) at the hip. Transfemoral values for normalized symmetry averaged 68.2% (53.2– 83.2%) at the ankle compared to 86.0% (70.5– 98.2%) at the knee and 73.3% (55.0– 91.9%) at the hip. The prosthetic foot had less ankle plantarflexion compared to the intact limb in individuals who used transtibial prostheses.43,51–54 This agrees with previous research,55–57 and supports the idea that the intact limb may compensate for lack of plantarflexion in the prosthetic foot.14,58–62Ankle symmetry was not reported in any study included in this review for individuals without limb loss.
FINDINGS BY PROSTHETIC FACTORS
Prosthetic factors are discussed by studies that examined suspension and alignment, foot componentry, and knee componentry. The influence of suspension and alignment findings on symmetry were inconclusive for the five normalized kinematic parameters. ESAR and hydraulic feet tended to show increased symmetry compared to non-ESAR and non-hydraulic feet.18,19,37,43,51 MPKs tended to show increased symmetry compared to non-MPKs.16,20,41,63,64
Suspension and Alignment
Spatiotemporal Parameters
Suspension systems are typically considered the most critical part of a prosthesis, since it provides direct contact between an individual’s prosthesis and residual limb. Individuals who used transtibial prostheses had decreased gait variability when participants wore a polyurethane liner compared to their previous liner, but had no difference in step length or stance time symmetry.65 Individuals who used transfemoral prostheses had more symmetrical step lengths with a wider base of support while wearing an ischial containment socket (98.0%) compared to a brimless socket with vacuum suspension (92.0%).66 Individuals who used transtibial prostheses showed increased step length and stance time symmetry, though not statistically significant, with suction suspension (93.2%) compared to pin-lock suspension (86.2%),29 and increased step lengths with vacuum suspension (91.9– 95.8%) compared to without vacuum (91.5%).54,67,68
Prosthetists optimize prosthetic alignment by observing an individual’s gait and make prosthetic adjustments to increase symmetry between prosthetic and intact limbs. Misalignment of the prosthesis can negatively influence gait and cause residual limb irritation. One study found stance time symmetry was consistent across alignment conditions,40 but another found stance time was least symmetrical during the optimal alignment condition.69 Both investigated individuals who used transtibial prostheses. Differences in findings may be explained by prosthetic design and foot componentry. In the study that found stance time symmetry was consistent across alignment conditions,40 some participants typically ambulated with an exoskeletal prosthesis, but used an endoskeletal prosthesis for the study. Participants in this study also used SACH feet, while participants used ESAR feet in the study that found stance time was least symmetrical during the optimal alignment condition.69
Joint Angle Parameters
Transtibial suspension studies found almost identical hip RoM symmetry across pin-lock, suction, and vacuum suspensions.29,67 Astrom and Stenstrom (2004) found no differences in knee symmetry when participants used polyurethane liners compared to their prescribed liners. Chow et al. (2006) determined knee flexion at loading response had the least relevance in determining acceptable alignment. One study found pin-lock suspension (84.4%)showed significantly increased knee joint symmetry compared to suction suspension (77.0%),29 and one study found differences in knee RoM between vacuum on (97.0%) and off (97.6%) conditions were almost identical.54,67 Ankle symmetry had less than a 1% difference between pin-lock and suction suspensions,29 and almost identical values between vacuum on and off conditions.54,67
Foot Componentry
Spatiotemporal Parameters
Studies agreed ESAR and hydraulic feet increased step length and stance time symmetry compared to non-ESAR and non-hydraulic feet.16,18,19,37,43,51 Yang et al. (2018) found the ESAR foot with split forefoot and heel wedge (97.3%) slightly increased step length symmetry compared to an ESAR foot without those features (94.2%). Moore (2016) results could not be normalized but found hydraulic feet significantly increased symmetry in comparison to non-hydraulic feet regardless of whether participants used transtibial or transfemoral prostheses or ambulated at lower or higher functional activity levels.
Joint Angle Parameters
Hip, knee, and ankle symmetry increased when individuals who used transtibial prostheses ambulated with an ESAR foot compared to a SACH foot. The ankle showed the most prominent differences between ESAR (63.5%) and SACH (23.7%) feet.43 Findings were consistent across three different equations Marinakis (2004) used to calculate results. Yang et al. (2018) showed the ESAR foot with split forefoot and heel wedge (60.8%) increased ankle dorsiflexion symmetry between limbs compared to the ESAR foot without those features (44.5%) throughout the gait cycle. Bai et al. (2017) found the non-hydraulic foot (83.2%) had increased ankle symmetry compared to the hydraulic foot (53.2%) throughout the gait cycle.
Knee Componentry
Spatiotemporal Parameters
Several studies found participants had increased step length symmetry with MPKs compared to hydraulic knees64,70 while other studies found no significant differences.41,71 These conflicting findings may be explained by prosthesis accommodation times. Studies that found significant differences had accommodation times of 3 months or stated each participant used the prosthetic knee for at least two years prior to testing, while studies that found no significant differences had accommodation times of 1 week or 10 hours. A previous review concluded proper accommodation times are important in determining findings that are reflective of long-term use and allowing clinicians to make appropriate prosthetic decisions.72
Stance time symmetry findings were also conflicting. One study found MPKs increased stance time symmetry compared to hydraulic knees,41 while another found the opposite,39 and two other studies found no significant differences.64,71 Conflicting findings may be explained by selection of hydraulic knee componentry. The study that found MPKs increased stance time symmetry tested hydraulic 3R60 knees (Ottobock, Duderstadt, Germany), while the study that found the opposite tested hydraulic 3R80 knees (Ottobock, Duderstadt, Germany), and both studies with no significant differences tested hydraulic Mauch SNS knees (Ossur, Reykjavik, Iceland). Conflicting step length and stance time findings were in line with a clinical practice guideline stating spatiotemporal parameters may not be primary indications for prosthetic knee joint selection due to comparable symmetries among knees.73
Joint Angle Parameters
MPKs (91.6%) tended to increase hip RoM symmetry compared to non-MPKs (82.6%), but showed similar amounts of knee RoM symmetry with MPKs (70.5– 97.7%) compared to non-MPKs (77.8– 98.2%).20,63,64 One study using waveform analysis found MPKs had more stance phase symmetry in all three joints compared to a variety of non-MPKs, though findings were not statistically signifcant.20 Another study found MPKs had more symmetry in all three joints across the gait cycle compared to hydraulic knees, with most increased symmetry at the hip.63 Finally, participants had more knee angle symmetry with MPKs compared to hydraulic knees after three-month acclimation periods to each knee. No studies that compared prosthetic knee componentry reported ankle symmetry or RoM.
CLINICAL CONSIDERATIONS
Walking symmetry is not typically quantified in clinical practice. Instead, prosthetists use observational gait analysis to observe kinematic symmetry parameters, such as step length or joint RoM, to make prosthetic adjustments and inform treatment plans. Effectiveness of using observational gait analysis can be dependent on subjective factors such as practitioner experience, user fatigue, or time allotted for the appointment. Observational gait analysis could be supplemented by translating kinematic walking symmetry research findings into clinical practice.
Motion capture was most commonly used to measure kinematic parameters in this review. While motion capture typically quantifies symmetry in research settings, it can be impractical to use in clinic for several reasons: high costs, lack of portability, and the need for specialized personnel.14 Some studies used equipment such as gait mats or inertial measurement units to collect data outside of research lab settings. As portable and wearable equipment becomes more ubiquitous and cost effective, clinicians and researchers may find this equipment more practical.
Clinicians can use normalized data summarized in this review, particularly the Table 2 summary of differences between prosthetic and intact limbs in metric units, as reference values for step length, stance time, and sagittal plane hip, knee, and ankle range of motion. These values provide evidence-based data that can be used to guide thresholds of symmetry in rehabilitation and justify ESAR feet and MPKs for active adults under 65 years of age with traumatic etiologies to insurance payers.
LIMITATIONS AND FUTURE RESEARCH
This review focused on kinematic symmetry due to ease of translation to observational gait analysis in clinical practice, and several researchers have noted kinematics alone should not be the sole determinant of gait symmetry.16,74 The majority of studies included in this review measured parameters other than kinematics such as kinetics, muscle strength, patient preference, or energy consumption, which should also be assessed. Furthermore, this review only included studies that measured walking. Other movement tasks such as sit-to-stand transitions, turns, and navigating inclines, declines, or uneven terrain are also important activities of daily living that should be examined in future research.
Several considerations can be applied to future studies regarding information collected from participants. Length of time since amputation was often assumed to reflect gait consistency. However, gait consistency could also be influenced by prosthetic socket or alignment changes, regardless of a participant’s time since amputation. Collecting the data since last prosthetic fitting, adjustment, or alignment may be a more accurate way to determine the consistency of a participant’s gait pattern than time since amputation. Additionally, testing clinically appropriate components with adequate accommodation time is necessary to determine findings that accurately inform clinical decisions.
Considerations for data collection and analysis could also be applied to future research. Future studies could use normalized values provided in this review as a reference for their findings and include the most common kinematic parameters and mathematical analysis of symmetry identified in this review to improve comparisons across studies. Studies could include larger sample sizes of IULLPs with a wide variety of demographics, which may be more feasible as portable and wearable equipment becomes more ubiquitous.
Several topics for future research were identified in this review. Collecting pelvic and trunk symmetry could improve understanding of gait deviations that contribute to commonly reported secondary health conditions such as low back pain in IULLPs.10,75,76 No studies included in this review directly examined differences in gait symmetry by age or etiology, examined ankle symmetry in individuals who used transfemoral prostheses, or compared componentry intended for individuals with lower activity levels.
CONCLUSIONS
This review normalized kinematic walking symmetry data in IULLPs by level of limb loss and prosthetic factors to provide considerations for clinical practice, and also provided considerations to promote clinical translation in future research. Individuals without limb loss had the most symmetry, followed by individuals who used transtibial prostheses, then individuals who used transfemoral prostheses in step length, stance time, and lower-limb sagittal RoM parameters. Componentry intended for individuals with higher activity levels, such as ESAR feet and MPKs, tended to increase symmetry. However, the majority of studies included 10 or fewer individuals, young adult IULLPs with traumatic etiologies who used componentry intended for higher activity levels. Clinicians can use normalized values in this study to guide thresholds for walking symmetry during rehabilitation, and future research can include larger sample sizes and individuals who are older, have vascular etiologies, or use componentry intended for lower activity levels to help promote translation of research findings into clinical practice for the majority of IULLPs. Identifying reference values reflective of the majority to IULLPs could ultimately help clinicians elevate the standard of care for individuals with lower-limb loss.
Supplementary Material
ACKNOWLEDGMENTS
This work was written while the first author was supported by the National Institutes of Health/National Institute on Aging (T32 AG020494) and the Institute for Healthy Aging.
Footnotes
Conflicts of Interest:
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Viteckova S, Kutilek P, Svoboda Z, et al. Gait symmetry measures: A review of current and prospective methods. Biomed Signal Process Control 2018; 42: 89–100. [Google Scholar]
- 2.Michael JW. Modern Prosthetic Knee Mechanisms: Clin Orthop 1999; 361: 39–47. [DOI] [PubMed] [Google Scholar]
- 3.Hof AL, van Bockel RM, Schoppen T, et al. Control of lateral balance in walking. Gait Posture 2007; 25: 250–258. [DOI] [PubMed] [Google Scholar]
- 4.Ku PX, Abu Osman NA, Wan Abas WAB. Balance control in lower extremity amputees during quiet standing: A systematic review. Gait Posture 2014; 39: 672–682. [DOI] [PubMed] [Google Scholar]
- 5.van Velzen JM, van Bennekom CA, Polomski W, et al. Physical capacity and walking ability after lower limb amputation: a systematic review. Clin Rehabil 2006; 20: 999–1016. [DOI] [PubMed] [Google Scholar]
- 6.Miller WC, Deathe AB, Speechley M, et al. The influence of falling, fear of falling, and balance confidence on prosthetic mobility and social activity among individuals with a lower extremity amputation. Arch Phys Med Rehabil 2001; 82: 1238–1244. [DOI] [PubMed] [Google Scholar]
- 7.Kulkarni J, Adams J, Thomas E, et al. Association between amputation, arthritis and osteopenia in British male war veterans with major lower limb amputations. Clin Rehabil 1998; 12: 348–353. [DOI] [PubMed] [Google Scholar]
- 8.Asano M, Rushton P, Miller WC, et al. Predictors of quality of life among individuals who have a lower limb amputation. Prosthet Orthot Int 2008; 32: 231–243. [DOI] [PubMed] [Google Scholar]
- 9.van der van der Linde H, Hofstad CJ, Geurts ACH, et al. A systematic literature review of the effect of different prosthetic components on human functioning with a lower-limb prosthesis. J Rehabil Res Dev 2004; 41: 555. [DOI] [PubMed] [Google Scholar]
- 10.Devan H, Hendrick P, Ribeiro DC, et al. Asymmetrical movements of the lumbopelvic region: Is this a potential mechanism for low back pain in people with lower limb amputation? Med Hypotheses 2014; 82: 77–85. [DOI] [PubMed] [Google Scholar]
- 11.Gholizadeh H, Abu Osman NA, Eshraghi A, et al. Transtibial prosthesis suspension systems: Systematic review of literature. Clin Biomech 2014; 29: 87–97. [DOI] [PubMed] [Google Scholar]
- 12.Sagawa Y, Turcot K, Armand S, et al. Biomechanics and physiological parameters during gait in lower-limb amputees: A systematic review. Gait Posture 2011; 33: 511–526. [DOI] [PubMed] [Google Scholar]
- 13.Research Priorities 2020, https://www.oandp.org/page/research-priorities-2020.
- 14.Gard SA. Use of Quantitative Gait Analysis for the Evaluation of Prosthetic Walking Performance. J Prosthet Orthot 2006; 18: 93–104. [Google Scholar]
- 15.Carse B, Scott H, Brady L, et al. A characterisation of established unilateral transfemoral amputee gait using 3D kinematics, kinetics and oxygen consumption measures. Gait Posture 2020; 75: 98–104. [DOI] [PubMed] [Google Scholar]
- 16.Cutti AG, Verni G, Migliore GL, et al. Reference values for gait temporal and loading symmetry of lower-limb amputees can help in refocusing rehabilitation targets. J NeuroEngineering Rehabil 2018; 15: 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moylan B, Paner R, Pauley T, et al. Impact of Increased Prosthetic Mass on Gait Symmetry in Dysvascular Transfemoral Amputees: A Randomized Prospective Double-Blind Crossover Trial. J Prosthet Orthot 2015; 27: 63–67. [Google Scholar]
- 18.Moore R Effect on Stance Phase Timing Asymmetry in Individuals with Amputation Using Hydraulic Ankle Units: J Prosthet Orthot 2016; 28: 44–48. [Google Scholar]
- 19.Graham LE, Datta D, Heller B, et al. A Comparative Study of Conventional and Energy-Storing Prosthetic Feet in High-Functioning Transfemoral Amputees. Arch Phys Med Rehabil 2007; 88: 801–806. [DOI] [PubMed] [Google Scholar]
- 20.Kaufman KR, Frittoli S, Frigo CA. Gait asymmetry of transfemoral amputees using mechanical and microprocessor-controlled prosthetic knees. Clin Biomech 2012; 27: 460–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mishra P, Singh S, Ranjan V, et al. Performance Evaluation of Jaipur Knee Joint through Kinematics and Kinetics Gait Symmetry with Unilateral Transfemoral Indian Amputees. J Med Syst 2019; 43: 55. [DOI] [PubMed] [Google Scholar]
- 22.Highsmith MJ, Schulz BW, Hart-Hughes S, et al. Differences in the Spatiotemporal Parameters of Transtibial and Transfemoral Amputee Gait: JPO J Prosthet Orthot 2010; 22: 26–30. [Google Scholar]
- 23.Darter BJ, Bastian AJ, Wolf EJ, et al. Locomotor adaptability in persons with unilateral transtibial amputation. PLOS ONE 2017; 12: e0181120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Asha AR, Buckley JG. The effects of walking speed on minimum toe clearance and on the temporal relationship between minimum clearance and peak swing-foot velocity in unilateral trans-tibial amputees. Prosthet Orthot Int 2015; 39: 120–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clemens S, Kim KJ, Gailey R, et al. Inertial sensor-based measures of gait symmetry and repeatability in people with unilateral lower limb amputation. Clin Biomech 2020; 72: 102–107. [DOI] [PubMed] [Google Scholar]
- 26.Balk E, Gazula AMG. Table 1, Lower limb extremity prosthesis Medicare Functional Classification Levels (K levels). In: Lower Limb Prostheses: Measurement Instruments, Comparison of Component Effects by Subgroups, and Long-Term Outcomes. Rockville, MD: Agency for Healthcare Research and Quality (US), https://www.ncbi.nlm.nih.gov/books/NBK531517/table/ch2.tab1/. [PubMed] [Google Scholar]
- 27.Yang JR, Yang HS, Ahn DH, et al. Differences in Gait Patterns of Unilateral Transtibial Amputees With Two Types of Energy Storing Prosthetic Feet. Ann Rehabil Med 2018; 42: 609–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nadollek H, Brauer S, Isles R. Outcomes after trans-tibial amputation: the relationship between quiet stance ability, strength of hip abductor muscles and gait. Physiother Res Int 2002; 7: 203–214. [DOI] [PubMed] [Google Scholar]
- 29.Gholizadeh H, Abu Osman NA, Eshraghi A, et al. The Effects of Suction and Pin/Lock Suspension Systems on Transtibial Amputees’ Gait Performance. PLoS ONE 2014; 9: e94520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laroche DP, Cook SB, Mackala K. Strength Asymmetry Increases Gait Asymmetry and Variability in Older Women: Med Sci Sports Exerc 2012; 44: 2172–2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Skelton DA, Kennedy J, Rutherford OM. Explosive power and asymmetry in leg muscle function in frequent fallers and non-fallers aged over 65. Age Ageing 2002; 31: 1. [DOI] [PubMed] [Google Scholar]
- 32.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the Prevalence of Limb Loss in the United States: 2005 to 2050. Arch Phys Med Rehabil 2008; 89: 422–429. [DOI] [PubMed] [Google Scholar]
- 33.Bateni H, Olney SJ. Kinematic and Kinetic Variations of Below-Knee Amputee Gait: JPO J Prosthet Orthot 2002; 14: 2–10. [Google Scholar]
- 34.Keklicek H, Kirdi E, Yalcin A, et al. Comparison of gait variability and symmetry in trained individuals with transtibial and transfemoral limb loss. J Orthop Surg 2019; 27: 230949901983266. [DOI] [PubMed] [Google Scholar]
- 35.Nolan L, Wit A, Dudziñski K, et al. Adjustments in gait symmetry with walking speed in trans-femoral and trans-tibial amputees. Gait Posture 2003; 17: 142–151. [DOI] [PubMed] [Google Scholar]
- 36.Kovac I, Medved V, Ostojic L. Spatial, temporal and kinematic characteristics on traumatic transtibial amputee’s gait. Coll Antropol 2010; 34: 205–213. [PubMed] [Google Scholar]
- 37.Houdijk H, Wezenberg D, Hak L, et al. Energy storing and return prosthetic feet improve step length symmetry while preserving margins of stability in persons with transtibial amputation. J NeuroEngineering Rehabil 2018; 15: 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hekmatfard M, Farahmand F, Ebrahimi I. Effects of prosthetic mass distribution on the spatiotemporal characteristics and knee kinematics of transfemoral amputee locomotion. Gait Posture 2013; 37: 78–81. [DOI] [PubMed] [Google Scholar]
- 39.Schaarschmidt M, Lipfert SW, Meier-Gratz C, et al. Functional gait asymmetry of unilateral transfemoral amputees. Hum Mov Sci 2012; 31: 907–917. [DOI] [PubMed] [Google Scholar]
- 40.Chow DHK, Holmes AD, Lee CKL, et al. The Effect of Prosthesis Alignment on the Symmetry of Gait in Subjects with Unilateral Transtibial Amputation. Prosthet Orthot Int 2006; 30: 114–128. [DOI] [PubMed] [Google Scholar]
- 41.Petersen AO, Comins J, Alkjær T. Assessment of Gait Symmetry in Transfemoral Amputees Using C-Leg Compared With 3R60 Prosthetic Knees: JPO J Prosthet Orthot 2010; 22: 106–112. [Google Scholar]
- 42.Błażkiewicz M, Wiszomirska I, Wit A. Comparison of four methods of calculating the symmetry of spatial-temporal parameters of gait. Acta Bioeng Biomech 2014; 16: 29–35. [PubMed] [Google Scholar]
- 43.Marinakis GNS. Interlimb symmetry of traumatic unilateral transtibial amputees wearing two different prosthetic feet in the early rehabilitation stage. J Rehabil Res Dev 2004; 41: 581. [DOI] [PubMed] [Google Scholar]
- 44.Jaegers SMHJ, Arendzen JH, de Jongh HJ. Prosthetic gait of unilateral transfemoral amputees: A kinematic study. Arch Phys Med Rehabil 1995; 76: 736–743. [DOI] [PubMed] [Google Scholar]
- 45.Waters RL, Perry J, Antonelli D, et al. Energy cost of walking of amputees: the influence of level of amputation. J Bone Joint Surg Am 1976; 58: 42–46. [PubMed] [Google Scholar]
- 46.Zuniga EN, Leavitt LA, Calvert JC, et al. Gait patterns in above-knee amputees. Arch Phys Med Rehabil 1972; 53: 373–382. [PubMed] [Google Scholar]
- 47.James U, Oberg K. Prosthetic gait pattern in unilateral above-knee amputees. Scand J Rehabil Med 1973; 5: 35–50. [PubMed] [Google Scholar]
- 48.Roerdink M, Roeles S, van der Pas SCH, et al. Evaluating asymmetry in prosthetic gait with step-length asymmetry alone is flawed. Gait Posture 2012; 35: 446–451. [DOI] [PubMed] [Google Scholar]
- 49.Mattes SJ, Martin PE, Royer TD. Walking symmetry and energy cost in persons with unilateral transtibial amputations: Matching prosthetic and intact limb inertial properties. Arch Phys Med Rehabil 2000; 81: 561–568. [DOI] [PubMed] [Google Scholar]
- 50.Forczek W, Staszkiewicz R. An Evaluation of Symmetry in the Lower Limb Joints During the Able-Bodied Gait of Women and Men. J Hum Kinet 2012; 35: 47–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bai X, Ewins D, Crocombe AD, et al. Kinematic and biomimetic assessment of a hydraulic ankle/foot in level ground and camber walking. PLOS ONE 2017; 12: e0180836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sjödahl C, Jarnlo G-B, Söderberg B, et al. Kinematic and kinetic gait analysis in the sagittal plane of trans-femoral amputees before and after special gait re-education. Prosthet Orthot Int 2002; 26: 101–112. [DOI] [PubMed] [Google Scholar]
- 53.Supan T, Lebiedowska M, Dodson R, et al. The Effect of a Talux® Prosthetic Foot on Gait Parameters and Limb Loading of Nonvascular Transtibial Amputees: JPO J Prosthet Orthot 2010; 22: 43–52. [Google Scholar]
- 54.Xu H, Greenland K, Bloswick D, et al. Vacuum level effects on gait characteristics for unilateral transtibial amputees with elevated vacuum suspension. Clin Biomech 2017; 43: 95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Breaky J Gait of unilateral below-knee amputees. O&P Library Digital Resource, http://www.oandplibrary.org/op/1976_03_017.asp.
- 56.Dingwell JB, Davis BL, Frazder DM. Use of an instrumented treadmill for real-time gait symmetry evaluation and feedback in normal and trans-tibial amputee subjects. Prosthet Orthot Int 1996; 20: 101–110. [DOI] [PubMed] [Google Scholar]
- 57.Winter DA, Sienko SE. Biomechanics of below-knee amputee gait. J Biomech 1988; 21: 361–367. [DOI] [PubMed] [Google Scholar]
- 58.Boonstra AM, Schrama J The gait of unilateral transfemoral amputees. Gait Unilateral Transfemoral Amputees 1994; 26: 217–223. [PubMed] [Google Scholar]
- 59.Schmalz T, Blumentritt S, Jarasch R. Energy expenditure and biomechanical characteristics of lower limb amputee gait: Gait Posture 2002; 16: 255–263. [DOI] [PubMed] [Google Scholar]
- 60.Berger N Atlas of limb prosthetics: surgical, prosthetic rehabilitation principles. In: Analysis of amputee gait. St Louis: Mosby-Year Book, Inc., 1992. [Google Scholar]
- 61.Czerniecki JM. Rehabilitation in limb deficiency. 1. Gait and motion analysis. Arch Phys Med Rehabil 1996; 77: S3–S8. [DOI] [PubMed] [Google Scholar]
- 62.Neptune RR, Kautz SA, Zajac FE. Contributions of the individual ankle plantar flexors to support, forward progression and swing initiation during walking. J Biomech 2001; 34: 1387–1398. [DOI] [PubMed] [Google Scholar]
- 63.Uchytil J, Jandacka D, Farana R, et al. Kinematics of gait using bionic and hydraulic knee joints in transfemoral amputees. Acta Gymnica 2017; 47: 130–137. [Google Scholar]
- 64.Segal AD, Orendurff MS, Klute GK, et al. Kinematic and kinetic comparisons of transfemoral amputee gait using C-Leg and Mauch SNS prosthetic knees. J Rehabil Res Dev 2006; 43: 857. [DOI] [PubMed] [Google Scholar]
- 65.Åström I, Stenström A. Effect on gait and socket comfort in unilateral trans-tibial amputees after exchange to a polyurethane concept. Prosthet Orthot Int 2004; 28: 28–36. [DOI] [PubMed] [Google Scholar]
- 66.Kahle JT, Highsmith MJ. Transfemoral interfaces with vacuum assisted suspension comparison of gait, balance, and subjective analysis: Ischial containment versus brimless. Gait Posture 2014; 40: 315–320. [DOI] [PubMed] [Google Scholar]
- 67.Gholizadeh H, Lemaire ED, Sinitski EH, et al. Transtibial amputee gait with the unity suspension system. Disabil Rehabil Assist Technol 2020; 15: 350–356. [DOI] [PubMed] [Google Scholar]
- 68.Board WJ, Street GM, Caspers C. A comparison of trans-tibial amputee suction and vacuum socket conditions. Prosthet Orthot Int 2001; 25: 202–209. [DOI] [PubMed] [Google Scholar]
- 69.Svoboda Z, Janura M Temporal symmetry of sound and prosthetic limbs during transtibial amputee gait with various prosthetic alignment. Acta Gymn 2007; 37: 55–60. [Google Scholar]
- 70.Uchytil J, Jandacka D, Zahradnik D, et al. Temporal–spatial parameters of gait in transfemoral amputees: Comparison of bionic and mechanically passive knee joints. Prosthet Orthot Int 2014; 38: 199–203. [DOI] [PubMed] [Google Scholar]
- 71.Johansson JL, Sherrill DM, Riley PO, et al. A Clinical Comparison of Variable-Damping and Mechanically Passive Prosthetic Knee Devices: Am J Phys Med Rehabil 2005; 84: 563–575. [DOI] [PubMed] [Google Scholar]
- 72.Wanamaker AB, Andridge RR, Chaudhari AM. When to biomechanically examine a lower-limb amputee: A systematic review of accommodation times. Prosthet Orthot Int 2017; 41: 431–445. [DOI] [PubMed] [Google Scholar]
- 73.Stevens PM, Wurdeman SR. Prosthetic Knee Selection for Individuals with Unilateral Transfemoral Amputation: A Clinical Practice Guideline. J Prosthet Orthot 2019; 31: 2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Childers WL, Kogler GF. Symmetrical kinematics does not imply symmetrical kinetics in people with transtibial amputation using cycling model. J Rehabil Res Dev 2014; 51: 1243–1254. [DOI] [PubMed] [Google Scholar]
- 75.Devan H, Hendrick P, Hale L, et al. Exploring Factors Influencing Low Back Pain in People With Nondysvascular Lower Limb Amputation: A National Survey. PM&R 2017; 9: 949–959. [DOI] [PubMed] [Google Scholar]
- 76.Gailey R Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev 2008; 45: 15–30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


