Background:
To evaluate the efficacy of Epley’s maneuver plus betahistine in the management of patients with posterior canal benign paroxysmal positional vertigo (PC-BPPV).
Methods:
Electronic databases including PubMed, Embase, Web of Science, Cochrane Library, Chinese National Knowledge Infrastructure, and Wanfang were searched from their inception to April, 2022. The effect size was analyzed by calculating the pooled risk ratio estimates of efficacy rate, recurrence rate, and standardized mean differences (SMD) of dizziness handicap inventory (DHI) score with a 95% confidence interval (CI). Sensitive analysis was performed simultaneously.
Results:
A total of 9 randomized controlled trials with 860 PC-BPPV patients were included in the meta-analysis, in which 432 were treated with Epley’s maneuver plus betahistine, and 428 received Epley’s maneuver alone. The meta-analysis revealed that Epley’s maneuver plus betahistine significantly improved DHI score than Epley’s maneuver alone (SMD = −0.61, 95% CI −0.96 to −0.26, P = .001). In addition, both Epley’s maneuver plus betahistine and Epley’s maneuver groups had comparable outcomes in efficacy rate and recurrence rate.
Conclusion:
This meta-analysis shows that Epley’s maneuver plus betahistine in PC-BPPV patients had favorable effects on DHI score.
Keywords: betahistine, Epley’s maneuver, meta-analysis, posterior canal benign paroxysmal positional vertigo
1. Introduction
Posterior canal benign paroxysmal positional vertigo (PC-BPPV) is a disorder of the inner ear characterized by repeated episodes triggered by head position changes in the direction of gravity with abrupt onset and rapid decrease.[1] It occurs most often in people age 50 and older, but can occur at any age, with a highly variable prevalence of 10.7-64/100,000.[2] The most common symptoms are positionally-triggered vertigo, dizziness, unsteadiness, and loss of balance and nausea.[3] The triggers of PC-BPPV are often not clear. However, cases may be associated with trauma, migraine, other inner ear problems, diabetes, osteoporosis, and lying in bed for long periods.[4] Clinically, the 2 most common BPPV variants are posterior canal BPPV and lateral canal BPPV.[5] The posterior canal is the most commonly affected site (88–90%) of BPPV because of the lowest position among the 3 canals, with the right ear predominating.[6] There are 2 possible mechanisms: otolith debris from the urtcular macula becomes attached to the canal cupula (cupulolithiasis), and free-floating otoconia in the canal (canalithiasis). The crystals cause one canal cupula to be abnormally stimulated causing vertigo with nystagmus on a change in head position.[7] It finally causes vertigo and nystagmus due to the movement of the head.
Although PC-BPPV may resolve spontaneously without treatment, up to half of the patients still need extra testing or treatment and a longer time to resolve.[8] Epley’s maneuver, as one of canalith repositioning procedure, has been proposed to be the most successful method, particularly in the treatment of PC-BPPV. Through a series of head movements, the crystals are returned to the utricle, where they are either absorbed or eliminated by the endolymphatic sac.[9] However, some studies report that there is still a specific recurrence rate within 1 year after single and simple repositioning maneuvers.[10] In other words, long-term and lasting improvement in symptoms may require a combination of other treatments including medical treatment or surgery. Therapy with betahistine is currently used to treat various vestibular disorders of peripheral and central origin and is especially effective for the symptoms of vestibular vertigo. Betahistine, as a histamine H1 agonist and H3 antagonist pharmacologically, relieves the inner ear vestibular hair cells by improving circulation in the cochlear stria vascularis and reducing excessive endolymphatic pressure.[11] However, there is no evidence for systematic clinical evaluation of efficacy in PC-BPPV. This study aimed to investigate the efficacy and safety of a medical treatment of betahistine administered together with Epley’s repositioning maneuvers in patients with PC-BPPV.
2. Materials and Methods
We conducted this systematic review and meta-analysis accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis.[12]
2.1. Ethical notice
This study did not require ethical approval because no original data were collected in this systematic review.
2.2. Literature search
Electronic databases including PubMed, Embase, Web of Science, Cochrane library, Chinese National Knowledge Infrastructure, and Wanfang Databases were searched from their inception to Apirl, 2022 to identify eligible studies about the effectiveness of betahistine in addition to Epley’s maneuver in PC-BPPV patients. The search strategies were (“benign paroxysmal positional vertigo” OR “BPPV”) AND (“betahistine”) AND (“Epley”). No language restrictions in the current study. Reference lists of retrieved articles were also screened.
2.3. Inclusion and exclusion criteria
Inclusion criteria were Population: adults aged 18 years and older who were diagnosed as PC-BPPV; Intervention: Epley’s Maneuver plus Betahistine; Comparison: Epley’s Maneuver; Outcomes: Reporting available outcomes including recurrence, efficiency rate, and dizziness handicap inventory (DHI) score; Study: randomized controlled trials. The exclusion criteria were reviews, conference abstracts, and case reports; unavailable or insufficient outcomes; duplicate publications. The DHI is the gold standard for evaluating the therapeutic effect of PC-BPPV. It consists of 25 items designed to determine dizziness-dependent changes grouped into 3 domains: Functional, emotional, and physical.
2.4. Data extraction and quality assessment
Two researchers independently collected available data, and inconsistencies were consulted by a third researcher. We extracted the following data: name of the first author, publication year, country, sample size, gender, age, intervention, and outcome. The Cochrane Collaboration risk of bias tool was used to assess the quality of included studies.
2.5. Statistical analysis
All statistical analyses were conducted using the software of Stata 12.0 (STATA, College Station, TX). The pooled risk ratio (RR) with 95% confidential interval (CI) and standardized mean differences (SMD) with 95% CI was calculated to evaluate the effect size of the outcomes. The statistical heterogeneity between studies was determined by the Cochran Q test and I2 test. If P < .05 or I2 > 50%, it indicated a significant heterogeneity across studies, and a randomized-effects model was used; otherwise, a fixed-effects model was used. Publication bias or small-study effects were examined by Beger’s funnel plot and Egger’s test. Sensitivity analysis was also performed to verify the robustness of the results. Subgroup analysis was conducted according to the treatment period.
3. Result
3.1. Characterization of the selected studies
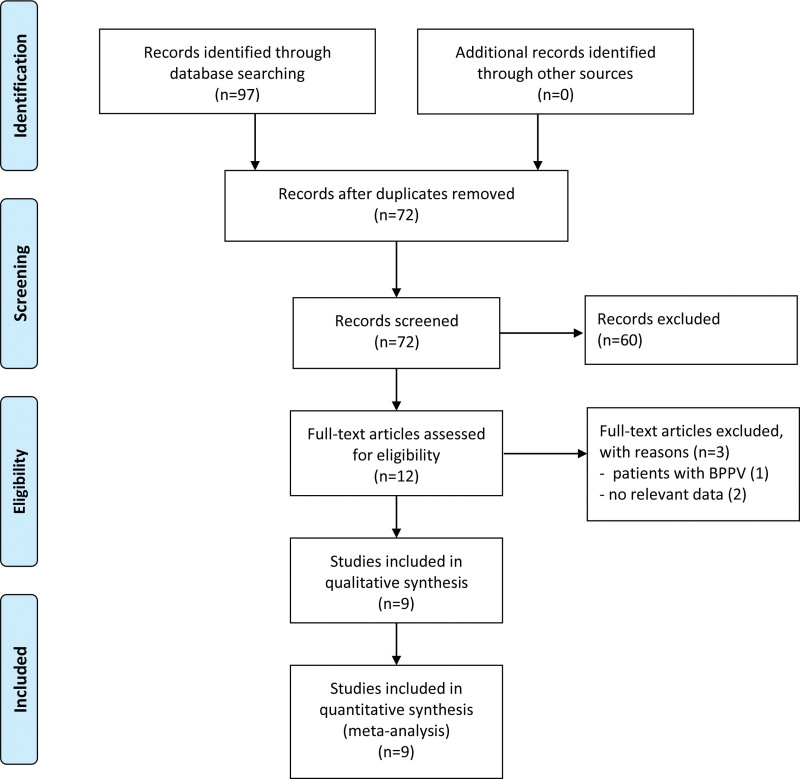
The details of the selection process are shown in Figure 1. Through search of electronic databases, 97 records were initially identified, in which 25 articles were excluded due to duplication. The remaining 72 studies were screening the title and abstract, and 60 were excluded based on selection criteria. Then, 12 studies were potentially eligible for full-text screening. 3 articles were further excluded for the following reasons: not reported relevant data (n = 2); the participants were not diagnosed with PC-BPPV (n = 1). Finally, a total of 9 studies[13–21] with 860 PC-BPPV patients were finally included in the meta-analysis, in which 432 were treated with Epley’s maneuver + betahistine, and 428 received Epley’s maneuver alone. Studies were conducted in Turkey, Iran, Pakistan, and China (Table 1).
Figure 1.
Study selection flowchart for meta-analysis. BPPV = benign paroxysmal positional vertigo.
Table 1.
Characteristics of the included studies.
| Author and year | Country | Gender (M/F) | Sample size (T/C) | Intervention | Control | Dose | Main outcome |
|---|---|---|---|---|---|---|---|
| Sayin 2020 | Turkey | 42/58 | 50/50 | Epley maneuver + betahistine | Epley maneuver | 24 mg, twice times/d | DHI, efficiency rate |
| Jalali 2020 | Iran | 34/44 | 39/39 | Epley maneuver + betahistine | Epley maneuver | 16 mg, 3 times/d | DHI |
| Guneri 2012 | Turkey | NA | 24/26 | Epley maneuver + betahistine | Epley maneuver + placebo | 24 mg, twice times/d | DHI, efficiency rate |
| Muhammad 2021 | Pakistan | 38/56 | 47/47 | Epley maneuver + betahistine | Epley maneuver | 24 mg, twice times/d | Efficiency rate |
| Ugurlu 2012 | Turkey | NA | 20/20 | Epley maneuver + betahistine | Epley maneuver | 24 mg, twice times/d | Recurrence rate |
| İnan 2019 | Turkey | 23/25 | 24/24 | Epley maneuver + betahistine | Epley maneuver | 24 mg, twice times/d | DHI |
| Wang 2015 | China | 85/87 | 86/86 | Epley maneuver + betahistine | Epley maneuver + placebo | 12 mg, 3 times/d | Efficiency rate |
| Li 2021 | China | 66/84 | 75/75 | Epley maneuver + betahistine | Epley maneuver | 12 mg, 3 times/d | DHI, efficiency rate, recurrence rate |
| Hong 2012 | China | 42/86 | 67/61 | Epley maneuver + betahistine | Epley maneuver | 12 mg, 3 times/d | efficiency rate |
C = control, DHI = dizziness handicap inventory, F = female, M = male, T = treatment.
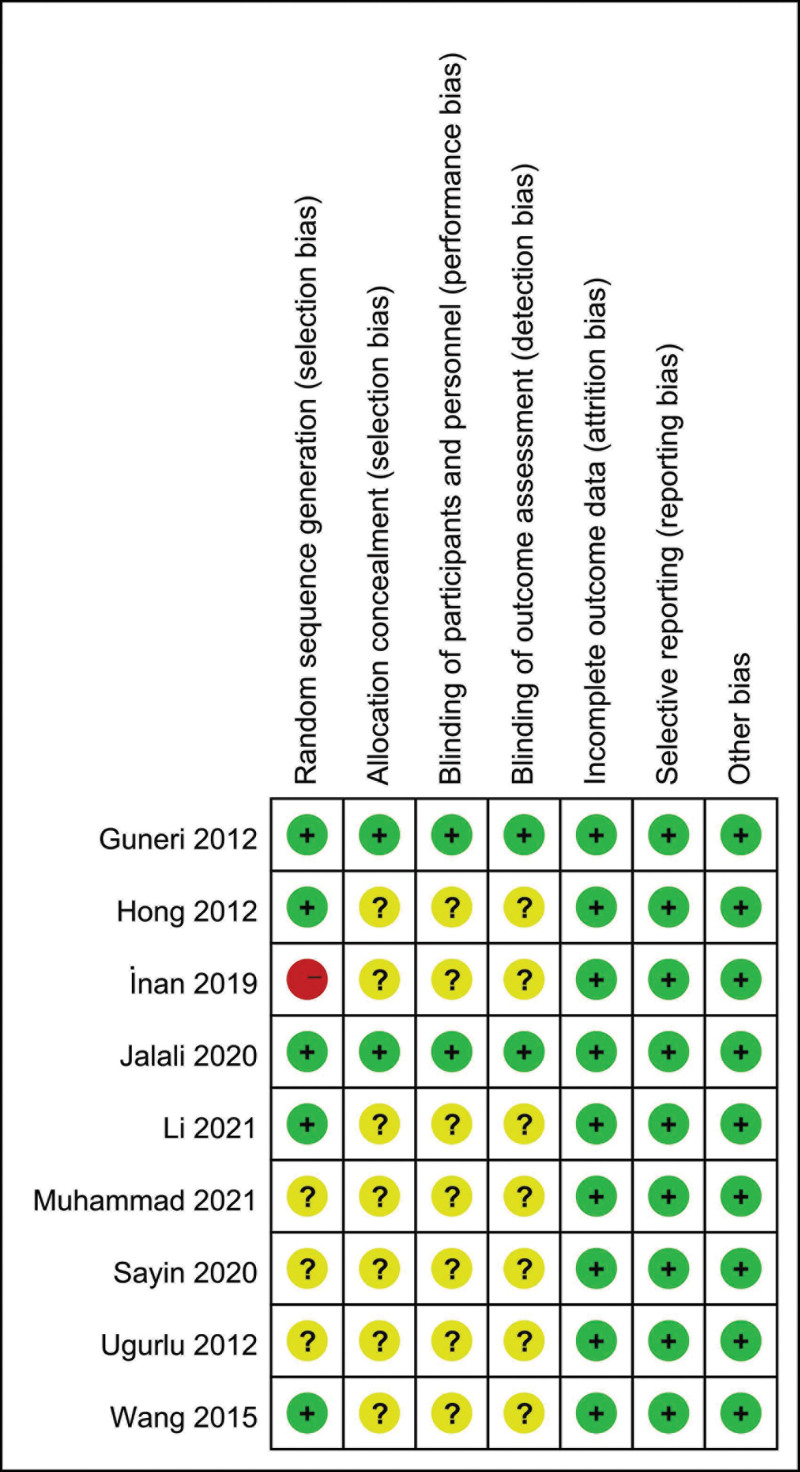
3.2. Quality assessment of the selected studies
According to the Cochrane evaluation system, one study[15] did not mention random sequence generation, 3 studies[18–20] did not mention the method of random sequence generation. Seven studies[14–20] didn’t report allocation concealment, blinding of participants and personnel, and blinding of outcome assessment. Two studies[13,21] were double-blind, randomized, controlled clinical trials. Quality results are summarized in Figure 2.
Figure 2.
Quality assessment of the selected studies.
3.2. Meta-analysis results
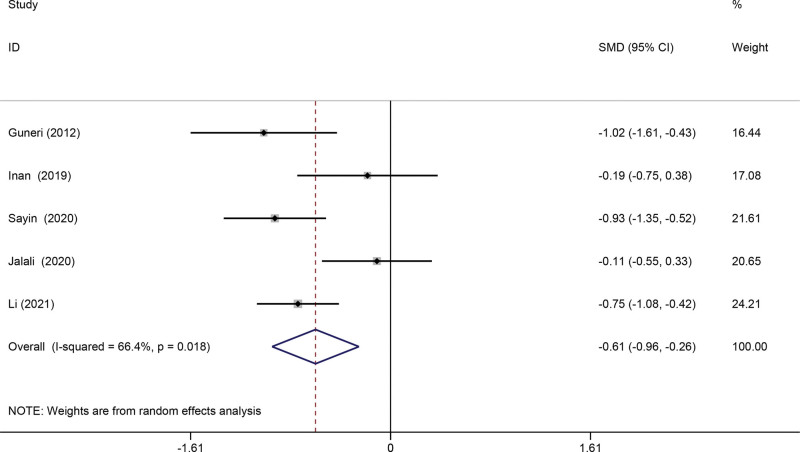
3.2.1. DHI score.
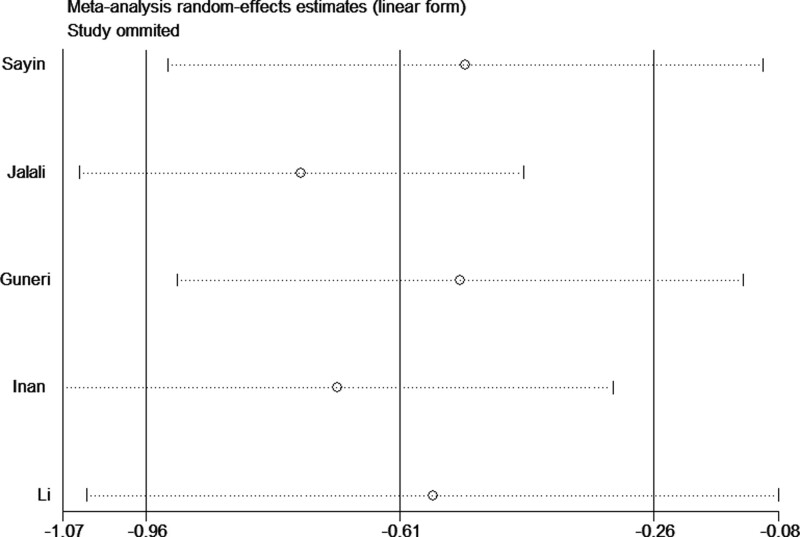
Five studies[13,15–17,19] reported DHI score after treatment. The randomized-effects model was adopted, because of the significant heterogeneity (I2 = 66.4%, P = .018). In the pooled analysis, Epley’s maneuver plus betahistine treatment could significantly improve DHI score than Epley’s maneuver alone (SMD = −0.61, 95% CI −0.96 to −0.26, P = .001) (Fig. 3). Sensitivity analyses revealed that consistent results were obtained after removing every study one by one, which indicated reliability and stability of our results. After the removal of the study of Jalali et al based on sensitivity analysis, the heterogeneity became insignificant (I2 = 44.3%, P = .146), suggesting that the source of high heterogeneity may be from the study of Jalali et al (Fig. 4). To determine potential publication bias of the literature, we performed Beger’s and Egger’s test which found there was no publication bias (Beger’s P = 1.000, Egger’s P = .725).
Figure 3.
Forest plots of the comparison of DHI score between Epley’s maneuver plus betahistine and Epley’s maneuver alone. CI = confidence interval, DHI = dizziness handicap inventory, SMD = standardized mean differences.
Figure 4.
Sensitivity analysis of DHI score. DHI = dizziness handicap inventory.
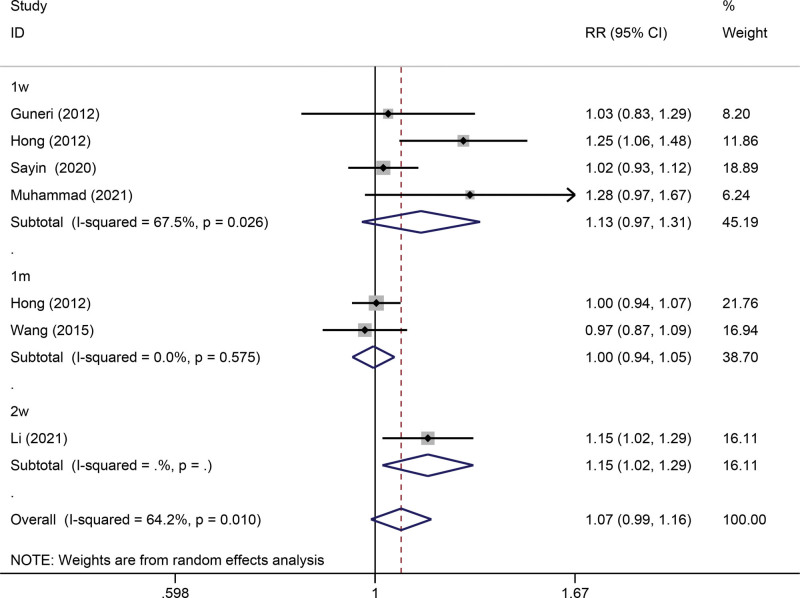
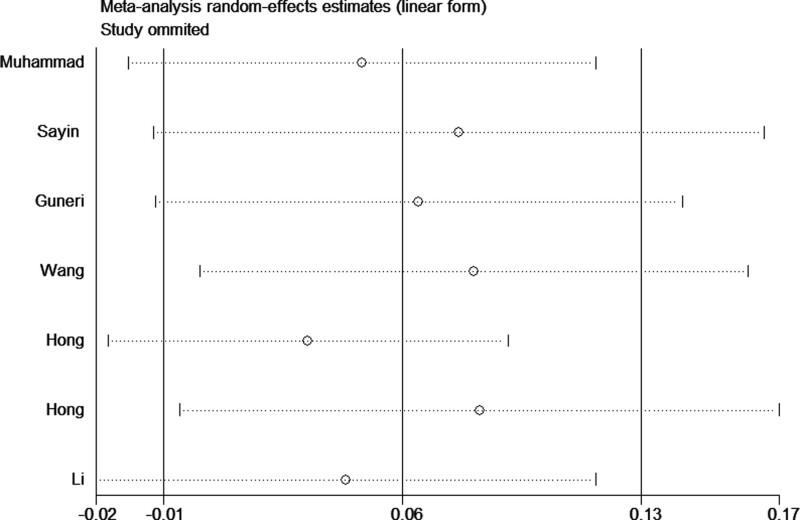
3.2.2. Efficacy rate.
Six articles[13,14,17–19,21] assessed the efficacy rate after treatment. The randomized-effects model analysis showed no significant difference was observed in efficiency rate between the 2 groups (RR = 1.07, 95% CI 0.99–1.16, P = .092) (Fig. 5). However, a substantial amount of heterogeneity (I2 = 64.2%, P = .010). Consistent results were obtained after the removal of any single study, suggesting that our result was reliable (Fig. 6). In addition, subgroups were stratified based on follow-up (1 weeks, 2 weeks, and 1 month). Subgroup analysis showed that maneuver + betahistine treatment could improve efficiency rate when treatment 2 weeks (Fig. 6). In addition, Beger’s (P = .099) and Egger’s test (P = .133) indicated there was no publication bias.
Figure 5.
Forest plots of the comparison of efficacy rate between Epley’s maneuver plus betahistine and Epley’s maneuver alone. CI = confidence interval, RR = risk ratio.
Figure 6.
Sensitivity analysis of efficacy rate.
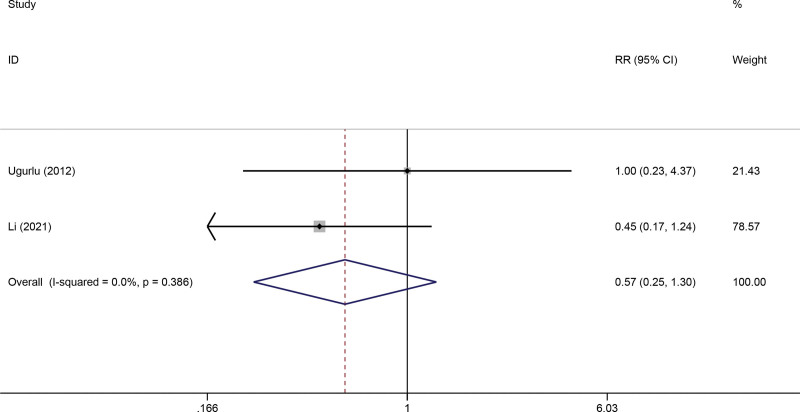
3.2.3. Recurrence rate.
Two studies[17,20] reported the recurrence rate after treatment. There was no heterogeneity in 2 articles (I2 = 0%; P = .386). The fixed effect model analysis showed no significant difference was observed in the recurrence rate between the 2 groups (RR = 0.57, 95% CI 0.25–1.30, P = .181) (Fig. 7).
Figure 7.
Forest plots of the comparison of recurrence rate between Epley’s maneuver plus betahistine and Epley’s maneuver alone. CI = confidence interval, RR = risk ratio.
4. Discussion
Repositioning maneuver is the first choice for PC-BPPV treatment with definite curative effect, but a considerable proportion of patients still have nonspecific symptoms such as dizziness and instability after successful repositioning, which lasts from several days to several months, leading to an adverse impact on patient’s daily life and social participation.[22] Drug treatment is mainly used clinically for the residual symptoms after reduction, but the conclusions of these studies are inconsistent.
Betahistine, a weak agonist for H1 receptors and an antagonist for H3 receptors, is the main treatment option for Ménière’s disease.[23] The main effect of betahistine is to improve the microcirculation of the inner ear with vasodilation.[24] Currently, it is used to treat various vestibular disorders as well as several other conditions, including tinnitus.[25] Some physicians advise PC-BPPV patients to take betahistine to relieve dizziness after the repositioning maneuver. However, the exact clinical effect of betahistine is ambiguous. Several studies showed that Betahistine is effective in reducing the frequency and severity of vertigo and improving vertigo-related symptoms. Mira et al[26] proved that betahistine improves the quality of life of patients with peripheric vestibular vertigo by decreasing attack frequency and dizziness and ameliorating the general condition of the patients. Kaur and Shamanna[27] carried out a study of 90 subjects consisting of 30 treated with the Epley’s maneuver plus betahistine, 30 treated with the Epley’s maneuver alone, and 30 treated with betahistine alone, and then made the conclusion that the effect of Epley’s maneuver + betahistine group is better than others. Cavaliere et al[28] clinical study of 103 people showed that betahistine add-on therapy resulted in faster recovery compared to the respective maneuver alone. Of course, there are still some opposite opinions. Therefore, it is necessary to comprehensively and systematically evaluate the therapeutic effect of betahistine after repositioning treatment.
In our study, we try to evaluate the effectiveness of Eply’s maneuver plus betahistine in PC-BPPV management. With the systematic analysis of 860 patients from 9 different studies, we find that Epley’s maneuver + betahistine treatment could significantly improve DHI score than Epley’s maneuver alone. However, the efficiency rate and recurrence rate show no significant difference. The significant difference in DHI score indicates that the effectiveness of Eply’s maneuver plus betahistine is better than Epley’s maneuver alone. Though there is no significant difference in efficiency rate and recurrence rate, it doesn’t mean the combination therapy is ineffective. Many factors, such as gender, age and some complications, including osteoporosis, hypertension, diabetes mellitus can influence the efficiency rate and recurrence rate. Chen et al reported that the female gender increased the risk of PC-BPPV recurrence, possibly related to osteoporosis in older women due to estrogen deficiency.[29,30] Besides, patients with osteoporosis were more likely to relapse.[31] Therefore, treatment of osteoporosis may have a preventive effect on the recurrence of PC-BPPV in older women, thereby reducing the potential recurrence rate at the same time. Considering the related factors, a more detailed subgroup classification should be taken in further study.
Our study still has some limitations and shortages. Firstly, the data is still relatively small and may not provide sufficient power to estimate the efficiency and recurrence rate. Secondly, as a type of retrospective study, a meta-analysis may encounter recall or selection bias, possibly influencing the reliability of our study results. Therefore, more studies with larger sample sizes and detailed subgroup classification are needed to provide a more representative statistical analysis accurately.
Overall, this meta-analysis shows that Epley’s maneuver plus betahistine in PC-BPPV patients resulted in improvements DHI score, but no impact on efficacy rate and recurrence rate.
Acknowledgments
This article does not contain any studies with human participants or animals performed by any of the authors.
Author contributions
Conceptualization: Wei Li, Jinqiang Sun, Yanqiu Zhang.
Data curation: Wei Li, Jinqiang Sun, Zeqi Zhao, Jifeng Xu.
Formal analysis: Wei Li, Jinqiang Sun, Zeqi Zhao, Jifeng Xu, Hao Wang, Rui Ding.
Investigation: Yanqiu Zhang.
Methodology: Wei Li, Jinqiang Sun.
Software: Wei Li, Jinqiang Sun.
Supervision: Yanqiu Zhang.
Validation: Wei Li, Jinqiang Sun, Zeqi Zhao, Jifeng Xu, Hao Wang, Rui Ding.
Visualization: Wei Li, Jinqiang Sun, Zeqi Zhao, Jifeng Xu, Hao Wang, Rui Ding.
Writing – original draft: Wei Li, Jinqiang Sun, Yanqiu Zhang.
Writing – review & editing: Wei Li, Jinqiang Sun, Yanqiu Zhang.
Abbreviations:
- CI
- confidence interval
- DHI
- dizziness handicap inventory
- PC-BPPV
- posterior canal benign paroxysmal positional vertigo
- RR
- risk ratio
- SMD
- standardized mean differences
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Li W, Sun J, Zhao Z, Xu J, Wang H, Ding R, Zhang Y. Efficacy of Epley’s maneuver plus betahistine in the management of PC-BPPV: A systematic review and meta-analysis. Medicine 2023;102:13(e33421).
Contributor Information
Wei Li, Email: lili78163@163.com.
Jinqiang Sun, Email: sunhongsh_6@163.com.
Zeqi Zhao, Email: zeqi_zhao@163.com.
Jifeng Xu, Email: xujifengfeng@163.com.
Hao Wang, Email: wanghaowwwhhh@163.com.
Rui Ding, Email: dingandrui@163.com.
References
- [1].Bhattacharyya N, Gubbels SP, Schwartz SR, et al. Clinical practice guideline: benign paroxysmal positional vertigo (update). Otolaryngol Head Neck Surg. 2017;156(3_suppl):S1–47. [DOI] [PubMed] [Google Scholar]
- [2].You P, Instrum R, Parnes L. Benign paroxysmal positional vertigo. Laryngoscope Investig Otolaryngol. 2019;4:116–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].von Brevern M, Bertholon P, Brandt T, et al. Benign paroxysmal positional vertigo: diagnostic criteria consensus document of the committee for the classification of vestibular disorders of the barany society. Acta Otorrinolaringol Esp (Engl Ed). 2017;68:349–60. [DOI] [PubMed] [Google Scholar]
- [4].Bhattacharyya N, Hollingsworth DB, Mahoney K, et al. Plain language summary: benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2017;156:417–25. [DOI] [PubMed] [Google Scholar]
- [5].Nuti D, Masini M, Mandala M. Benign paroxysmal positional vertigo and its variants. Handb Clin Neurol. 2016;137:241–56. [DOI] [PubMed] [Google Scholar]
- [6].Korres S, Balatsouras DG, Kaberos A, et al. Occurrence of semicircular canal involvement in benign paroxysmal positional vertigo. Otol Neurotol. 2002;23:926–32. [DOI] [PubMed] [Google Scholar]
- [7].Talaat HS, Abuhadied G, Talaat AS, et al. Low bone mineral density and vitamin D deficiency in patients with benign positional paroxysmal vertigo. Eur Arch Otorhinolaryngol. 2015;272:2249–53. [DOI] [PubMed] [Google Scholar]
- [8].Oh HJ, Kim JS, Han BI, et al. Predicting a successful treatment in posterior canal benign paroxysmal positional vertigo. Neurology. 2007;68:1219–22. [DOI] [PubMed] [Google Scholar]
- [9].Piromchai P, Eamudomkarn N, Srirompotong S, et al. The efficacy of a home treatment program combined with office-based canalith repositioning procedure for benign paroxysmal positional vertigo-a randomized controlled trial. Otol Neurotol. 2019;40:951–6. [DOI] [PubMed] [Google Scholar]
- [10].Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014;12:CD003162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Martinez DM. The effect of Serc (betahistine hydrochloride) on the circulation of the inner ear in experimental animals. Acta Otolaryngol Suppl. 1972;305:29–47. [DOI] [PubMed] [Google Scholar]
- [12].Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Guneri EA, Kustutan O. The effects of betahistine in addition to epley maneuver in posterior canal benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2012;146:104–8. [DOI] [PubMed] [Google Scholar]
- [14].Hong J, Bi Y, Fang L. Research of association of modified Epley maneuver and betahistine for treating posterior semicircular canal benign paroxysmal positional vertigo. Chin General Pract. 2012;15:622–4. [Google Scholar]
- [15].İnan HC, Kiraç M. An evaluation of the effects of betahistine and dimenhydrinate on posterior canal benign paroxysmal positional vertigo. Turk Arch Otorhinolaryngol. 2019;57:191–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Jalali MM, Gerami H, Saberi A, et al. The impact of betahistine versus dimenhydrinate in the resolution of residual dizziness in patients with benign paroxysmal positional vertigo: a randomized clinical trial. Ann Otol Rhinol Laryngol. 2020;129:434–40. [DOI] [PubMed] [Google Scholar]
- [17].Li Y, Cui LP, Dong WR, et al. The clinical effects of betahistine mesilate tablets combined with manual reduction in treatment of benign paroxysmal positional vertigo. Hebei Med J. 2021;43:1350–3. [Google Scholar]
- [18].Muhammad T, Ahmed E, Habib M, et al. Comparison of effectiveness of Epley s maneuver only and Epley s maneuver plus betahistine in the management of benign paroxysmal positional vertigo. Pak J Med Health Sci. 2021;15:1254–6. [Google Scholar]
- [19].Sayin I, Koc RH, Temirbekov D, et al. Betahistine add-on therapy for treatment of subjects with posterior benign paroxysmal positional vertigo: a randomized controlled trial. Braz J Otorhinolaryngol. 2022;88:421–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Ugurlu B, Evcimik MF, Ozkurt FE, et al. Comparison of the effects of betahistine dihydrochloride and brandt-daroff exercises in addition to epley maneuver in the treatment of benign paroxysmal positional vertigo. J Int Adv Otol. 2012;8:45–50. [Google Scholar]
- [21].Wang K, Rong LQ, Zhu BL, et al. Epley maneuver associated with vertigo calming for treating posterior semicircular canal benign paroxysmal positional vertigo in young. Clin Med China. 2015;31:795–8. [Google Scholar]
- [22].Murdin L, Hussain K, Schilder AG. Betahistine for symptoms of vertigo. Cochrane Database Syst Rev. 2016;6:CD010696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Parfenov VA, Golyk VA, Matsnev EI, et al. Effectiveness of betahistine (48 mg/day) in patients with vestibular vertigo during routine practice: The VIRTUOSO study. PLoS One. 2017;12:e0174114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Lacour M. Betahistine treatment in managing vertigo and improving vestibular compensation: clarification. J Vestib Res. 2013;23:139–51. [DOI] [PubMed] [Google Scholar]
- [25].Ramos Alcocer R, Ledezma Rodriguez JG, Navas Romero A, et al. Use of betahistine in the treatment of peripheral vertigo. Acta Otolaryngol. 2015;135:1205–11. [DOI] [PubMed] [Google Scholar]
- [26].Mira E, Guidetti G, Ghilardi L, et al. Betahistine dihydrochloride in the treatment of peripheral vestibular vertigo. Eur Arch Otorhinolaryngol. 2003;260:73–7. [DOI] [PubMed] [Google Scholar]
- [27].Kaur J, Shamanna K. Management of benign paroxysmal positional vertigo: a comparative study between epleys manouvre and betahistine. Int Tinnitus J. 2017;21:30–4. [DOI] [PubMed] [Google Scholar]
- [28].Cavaliere M, Mottola G, Iemma M. Benign paroxysmal positional vertigo: a study of two manoeuvres with and without betahistine. Acta Otorhinolaryngol Ital. 2005;25:107–12. [PMC free article] [PubMed] [Google Scholar]
- [29].Chen J, Zhang S, Cui K, et al. Risk factors for benign paroxysmal positional vertigo recurrence: a systematic review and meta-analysis. J Neurol. 2021;268:4117–27. [DOI] [PubMed] [Google Scholar]
- [30].Yang H, Gu H, Sun W, et al. Estradiol deficiency is a risk factor for idiopathic benign paroxysmal positional vertigo in postmenopausal female patients. Laryngoscope. 2018;128:948–53. [DOI] [PubMed] [Google Scholar]
- [31].Vibert D, Kompis M, Hausler R. Benign paroxysmal positional vertigo in older women may be related to osteoporosis and osteopenia. Ann Otol Rhinol Laryngol. 2003;112:885–9. [DOI] [PubMed] [Google Scholar]