Abstract
Testicular metastasis are rare findings and bilateral metastasis of testes are extremely rare. Here we are describing for the first time a case of bilateral testicular metastasis in a patient with a known ileocecal valve NET using an in-depth ultra-sound studying including microvascular flow imaging (MV-flow), ultra-sound new technique, able to detect small vessel slow-signal.
Keywords: Bilateral testicular metastases, Ileocecal NET, Testicular tumor, Multiparametric US, MV-flow imaging
Introduction
Neuroendocrine tumors (NETs) are slow-growing malignancies occurring most frequently in the gastrointestinal tract and bronchopulmonary system. The gastrointestinal ones occur mostly in the small bowel (41.8% of gastrointestinal carcinoids), especially in the ileum (47.3% of small bowel carcinoids) [1].
The main target of metastases from small bowel NET are the liver and the regional lymph nodes [2], on the contrary testes represent very unusual sites. Ultrasound (US) imaging is the method of choice to examine the scrotum, providing information about volume, echotexture, tissue stiffness, macrovascularization and microvascularization, essential in the diagnosis of testicular tumors [3].
Besides, microvascular flow imaging (MVFI; MV-FlowTM, Samsung Medison Co., Ltd., Seoul, Korea), a new Doppler microvascular imaging, has been used for detecting slow blood flow, increasing confidence in the evaluation of the lesion vascularity [4].
Case report
Here describe the case of a 59 years old male, with a story of ileocecal valve NET (G1) treated with ileal resection and ileocolic anastomosis, with multiple metastatic liver lesions showed at computed tomography (CT). He presented a nonpainful palpable mass in the right testicle. Performed a US examination on RS85 ultrasound scanner (Samsung Medison Co., Ltd.) using LA2-14A linear array transducer. Performing B-mode scan, examined the testes in the sagittal and transversal axes finding multiple homogenously hypoechoic or isoechoic nodular masses with regular shape in both testes, the greater ones about 10 mm with a peripheral halo, (Fig. 1) that showed predominantly peripheral hypervascularity at color-doppler (CDUS) (Fig. 2) and yellow areas, as intermediate elasticity stiffer than the surrounding parenchyma, at real-time sonoelastography (RTSE) (Fig. 3). The masses were also detected by MV-flow imaging and showed the presence of peripheral and central microvascular structures (Fig. 4). Then performed contrast-enhanced ultrasonography (CEUS) (Fig. 5) with a 2.4 mL contrast medium (SonoVue, Bracco Imaging, Milan, Italy) administered intravenously in the antecubital vein followed by a 0.9% saline flush (10 ml). It showed a late contrast enhancement of the masses, considered hypervascularization. All the described findings were highly suggestive for metastases, so the patient underwent a positron emission tomography (PET) that revealed an increased fluorodeoxyglucose (FDG) uptake in both testes, as well as liver and bone.
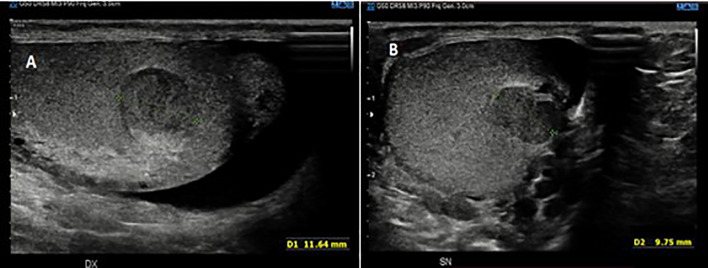
Fig. 1.
US gray-scale image shows nodular masses with diameter about 10 mm with regular shape and a peripheral halo in right (a) and left (b) testicles
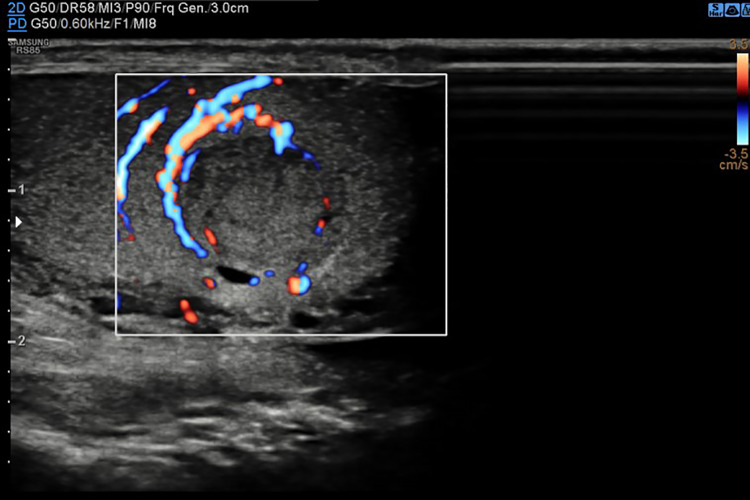
Fig. 2.
US color-Doppler image shows peripheral vascularization of the mass
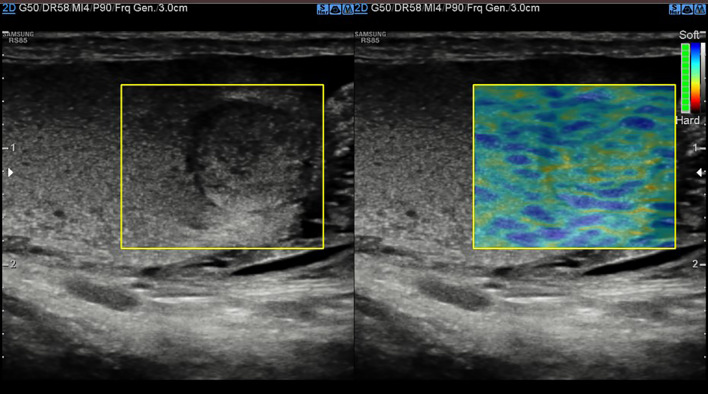
Fig. 3.
US image shows intermediate elasticity stiffer at real-time sonoelastography (RTSE)
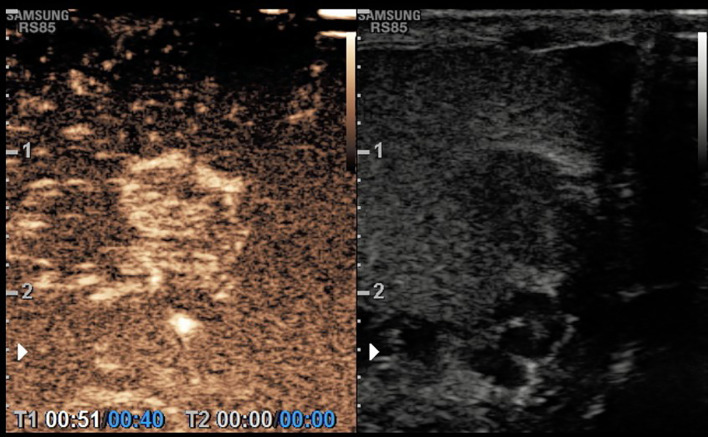
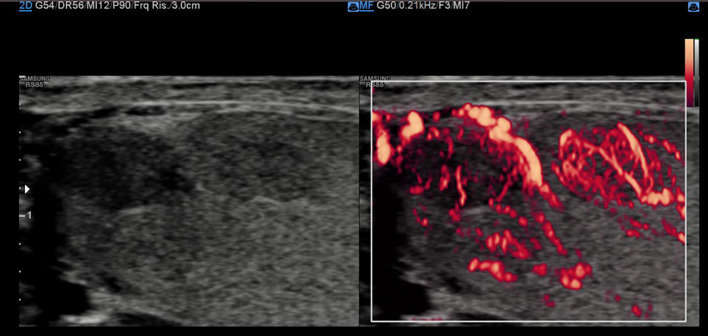
Fig. 4.
contrast-enhanced ultrasonography (CEUS) image shows contrast enhancement of the mass
Fig. 5.
US image shows masses neo-vascularity at MV-flow image
Discussion and Conclusion
Testicular metastasis is uncommon findings with an incidence of 0.9% in all testicular tumors [5]. Even more uncommon are bilateral testicular metastasis, most of them reported from prostatic carcinoma [6].
Only a few cases of metastasis from ileocecal carcinoid were reported in the literature at this moment and, to our knowledge, bilateral testicular metastasis from ileocecal carcinoid has never been previously reported.
The US is the modality of choice to study the scrotum, with almost 100% sensitivity combined with history and physical examination [7]. Most testicular malignancy typically occur as nonpainful masses without specific features that differentiate primary from secondary tumors;
the multiparametric US can help to define some differences among the subtypes. According to Huang et al. [8], seminoma appears at the gray-scale US as a solid round homogeneous low-reflectivity, at CDUS shows vascularity within the lesion and on CEUS there is a rapid enhancement in the mass with a rapid washout of the contrast, but with the persistence of the abnormal crossing vessels within the lesion. The non-seminomatous germ-cell tumors on B-mode images may be inhomogeneous, with areas of increased echogenicity, calcification and cysts, CDUS may or may not show increased vascularity, on CEUS individual microbubbles may be seen within the lesion in a haphazard pattern. Metastatic masses can appear as focal or multifocal hypoechoic nodular lesions with a halo [9] with internal vascularity within the lesions at CDUS confirmed at CEUS with internal and peripheral contrast enhancement. All the lesions demonstrate an intermediate-hard elasticity stiffer on RTSE. The metastatic mass features found in our patient were similar to the ones described in the literature: homogenously hypoechoic nodular masses with a peripheral halo and predominantly peripheral hypervascularity at CDUS, an intermediate elasticity stiffer at RTSE and a late contrast enhancement on CEUS. Besides, we performed the MV-flow imaging, for the first time on the testicles to our knowledge. This specific technique, already used in a limited number of studies [10–12] was able to depict the microvascular structures due to tumoral neoangiogenesis within the lesions.
Similar techniques to study testicular blood slow-flow were already reported using different scanner brands. Rocher et al. [13] described the feasibility of ultrasensitive Doppler (USD) on the Aixplorer US system (SuperSonic Imagine, Aix-en-Provence, France) that improved the detection of vascular architecture or the absence of any vessels in different testicular lesions. Lee et al. [14] used superb microvascular imaging (SMI) technique, on the Aplio 500 (Toshiba Medical System Corporation, Tokyo, Japan) to detect the perfusion difference between normal and undescended testes in young children.
In conclusion, the US is the method of choice to explore the scrotum since it is easily available, noninvasive, rapid to perform and economic. We believe that the multiparametric US is necessary in detecting as well as possible testicular abnormalities because every single technique can add useful information to improve the characterization of testicular lesions and to increase diagnostic confidence, especially for unusual findings as demonstrated in this case.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statements and Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki declaration of 1975, and its late amandments. Additional informed consented was obtained from all patients for which indentifyng information is not included in this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97(4):934–959. doi: 10.1002/cncr.11105. [DOI] [PubMed] [Google Scholar]
- 2.Riihimäki M, Hemminki A, Sundquist K, Sundquist J, Hemminki K. The epidemiology of metastases in neuroendocrine tumors. Int J Cancer. 2016;139(12):2679–2686. doi: 10.1002/ijc.30400. [DOI] [PubMed] [Google Scholar]
- 3.De Zordo T, Stronegger D, Pallwein-Prettner L, Harvey CJ, Pinggera G, Jaschke W, Aigner F, Frauscher F. Multiparametric ultrasonography of the testicles. Nat Rev Urol. 2013;10(3):135–148. doi: 10.1038/nrurol.2012.255. [DOI] [PubMed] [Google Scholar]
- 4.Kudo M, Tochio H. Intranodular blood supply correlates well with biological malignancy grade determined by tumor growth rate in pathologically proven hepatocellular carcinoma. Oncology. 2008;75(Suppl 1):55–64. doi: 10.1159/000173425. [DOI] [PubMed] [Google Scholar]
- 5.Dieckmann KP, Düe W, Loy V. Intrascrotal metastasis of renal cell carcinoma. Case reports and review of the literature. Eur Urol. 1988;15(3–4):297–301. doi: 10.1159/000473457. [DOI] [PubMed] [Google Scholar]
- 6.Manikandan R, Nathaniel C, Reeve N, Brough RJ. Bilateral testicular metastases from prostatic carcinoma. Int J Urol. 2006;13(4):476–477. doi: 10.1111/j.1442-2042.2006.01329.x. [DOI] [PubMed] [Google Scholar]
- 7.Tufano A, Flammia RS, Antonelli L, Minelli R, Franco G, Leonardo C, Cantisani V. The value of contrast-enhanced ultrasound (CEUS) in differentiating testicular masses: a systematic review and meta-analysis. Appl Sci. 2021;11:8990. doi: 10.3390/app11198990. [DOI] [Google Scholar]
- 8.Huang DY, Sidhu PS. Focal testicular lesions: colour Doppler ultrasound, contrast-enhanced ultrasound and tissue elastography as adjuvants to the diagnosis. Br J Radiol. 2012;85 Spec No 1(Spec Iss 1):S41–53. doi: 10.1259/bjr/30029741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang H, Ling W, Qiu T, Luo Y. Ultrasonographic features of testicular metastasis from renal clear cell carcinoma that mimics a seminoma: a case report. Medicine (Baltimore) 2018;97(40):e12728. doi: 10.1097/MD.0000000000012728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kang HJ, Lee JM, Jeon SK, Ryu H, Yoo J, Lee JK, Han JK. Microvascular flow imaging of residual or recurrent hepatocellular carcinoma after transarterial chemoembolization: comparison with color/power Doppler imaging. Korean J Radiol. 2019;20(7):1114–1123. doi: 10.3348/kjr.2018.0932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen X, Wei X, Zhao S, Huang H, Wang W, Qiu J, Chen X, Cheng C, Tian Z, Rychik J. Characterization of placental microvascular architecture by MV-flow imaging in normal and fetal growth-restricted pregnancies. J Ultrasound Med. 2020 doi: 10.1002/jum.15531. [DOI] [PubMed] [Google Scholar]
- 12.Dall'Asta A, Grisolia G, Volpe N, Schera G, Sorrentino F, Frusca T, Ghi T. Prenatal visualisation of the torcular herophili by means of a Doppler technology highly sensitive for low-velocity flow in the expert assessment of the posterior fossa: a prospective study. BJOG. 2020 doi: 10.1111/1471-0528.16392. [DOI] [PubMed] [Google Scholar]
- 13.Rocher L, Gennisson JL, Ferlicot S, Criton A, Albiges L, Izard V, Bellin MF, Correas JM. Testicular ultrasensitive Doppler preliminary experience: a feasibility study. Acta Radiol. 2018;59(3):346–354. doi: 10.1177/0284185117713350. [DOI] [PubMed] [Google Scholar]
- 14.Lee YS, Kim MJ, Han SW, Lee HS, Im YJ, Shin HJ, Lee MJ. Superb microvascular imaging for the detection of parenchymal perfusion in normal and undescended testes in young children. Eur J Radiol. 2016;85(3):649–656. doi: 10.1016/j.ejrad.2015.12.023. [DOI] [PubMed] [Google Scholar]