Abstract
Objective:
To compare the Simple Nutrition Screening Tool (SNST) with other nutritional screening tools [Nutrition Risk Screening 2002 (NRS-2002), Nutrition Risk index (NRI)], nutritional assessment parameters, and the Subjective Global Assessment (SGA) in surgical patients.
Methods:
A comparative observational study with a total of 122 surgical patients. Patients were assessed during the first 24 h of admission in the ward from January to July 2022 using the NRI, NRS-2002, SNST, body mass index (BMI), mid-upper arm circumferences (MUAC), albumin serum, hemoglobin level, total lymphocyte count (TLC), and SGA. Sensitivity, specificity and predictive values were calculated to evaluate NRI, NRS-2002, SNST, BMI, MUAC, albumin, hemoglobin, TLC compared to SGA.
Results:
The screening tools identified a high nutritional risk in surgical patients from 58.2%-72.1%. Meanwhile, about 29.5% to 71.3% was affected by malnutrition based on nutritional assessment tools. There were significant associations between the type of disease, the screening tools, the anthropometric parameters, albumin, TLC as well and SGA (p<0.05). The SNST has a good category among the nutritional screening tools with sensitivity and specificity >80%, as well as area under the curve >0.8.
Conclusions:
There were significant associations for screening (NRS-2002, SNST) and nutritional assessment tools (BMI, MUAC, albumin) compared with SGA. Both these tools can be used to determine the risk of malnutrition in surgical patients.
Keywords: Nutritional status, nutrition assessment, subjective global assessment, surgery
Abstract
Amaç:
Cerrahi hastalarda Basit Beslenme Tarama Aracını (SNST) diğer beslenme tarama araçları [Beslenme Riski Taraması 2002 (NRS-2002), Beslenme Riski indeksi (NRI)], beslenme değerlendirme parametreleri ve Subjektif Global Değerlendirme (SGA) ile karşılaştırmaktır.
Yöntemler:
Çalışmamız toplam 122 cerrahi hasta ile karşılaştırmalı bir gözlemsel çalışmadır. Hastalar, Ocak-Temmuz 2022 arasında hastaneye yatışlarının ilk 24 saatinde NRI, NRS-2002, SNST, vücut kitle indeksi (VKİ) orta-üst kol çevresi (MUAC), albumin serumu, hemoglobin seviyesi, toplam lenfosit sayısı (TLC) ve SGA kullanılarak değerlendirildi. NRI, NRS-2002, SNST, VKİ, MUAC, albumin, hemoglobin ve TLC’yi SGA’ya kıyasla değerlendirmek için sensitivite, spesifite ve prediktif değerler hesaplandı.
Bulgular:
Tarama araçları ile cerrahi hastalarda %58,2 ila %72,1 arasında yüksek bir beslenme riski belirlendi. Bu arada, beslenme değerlendirme araçlarına göre hastaların yaklaşık %29,5 ila %71,3’ünün yetersiz beslenmeden etkilendiği görüldü. Hastalık tipi, tarama araçları, antropometrik parametreler, albumin, TLC ve SGA arasında anlamlı ilişki vardı (p<0,05). SNST >%80 duyarlılık ve özgüllük ve eğri altındaki alan >0,8 ile beslenme tarama araçları arasında iyi bir yere sahiptir.
Sonuçlar:
SGA ile karşılaştırıldığında tarama (NRS-2002, SNST) ve beslenme değerlendirme araçları (VKİ, MUAC, albumin) açısından anlamlı ilişkiler bulunmuştur. Bu araçların her ikisi de cerrahi hastalarda yetersiz beslenme riskini belirlemek için kullanılabilir.
Keywords: Beslenme durumu, beslenme değerlendirmesi, subjektif global değerlendirme, cerrahi
INTRODUCTION
Malnutrition among hospitalized patients was very common and was more likely to occur in surgical patients who must be recovered. A systematic review reported that among surgical patients, the prevalence of malnutrition was high (>40%)1. The untreated malnutrition was proven to be manifested in a longer length of hospital stay2 and postoperative complications, poor outcome, major surgical stress, and trauma, that triggered catabolism3. The preventive action should be performed by determining the risk of malnutrition status to tackle malnutrition among surgical patients. The risk of malnutrition should be examined within 1 to 24 h of the patient’s admission to the hospital through nutritional screening to differentiate whether the patients were at risk of malnutrition or not.
Surgical patients are at a risk of malnutrition, but the incidence in these patients is also quite high at 50-88%4,5,6. A previous study of surgical patients showed that 50% was affected by malnutrition and showed a relationship between nutrition and surgery outcome6. Similarly, it has been reported that the criteria of the Global Leadership Initiative on Malnutrition (GLIM) are related to poor clinical outcomes after emerging gastrointestinal (GI) surgery that affect the length of stay (LOS) with increased morbidity, mortality, and an increase in hospital costs7.
Patients who are at risk of malnutrition will enroll in the nutritional assessment to determine the nutritional status. The indicators for surgical patients’ malnutrition are weight loss >10-15% for 6 months, body mass index <18.5 kg/m2, Subjective Global Assessment (SGA) grade C or Nutrition Risk Screening (NRS) 2002 >5, and serum albumin <3.0 g/dL3.
Nutritional screening tools are used to distinguish between individuals that are at risk of malnutrition and those that are not. Patients that are at risk of malnutrition will be given further intervention by a nutritionist. Meanwhile, nutritional assessment determines the status of the patient by identifying clinically relevant malnutrition and monitoring changes in nutritional status. Furthermore, the nutritional assessment includes anthropometric, biochemical, physical-clinical measurements as well as the dietary history8.
Nutritional screening is the first phase in determining the risk of malnutrition in patients and is performed within 1 to 24 h after the patient is hospitalized. Currently, several nutritional screening tools have been developed to identify malnutrition risk and each has advantages and disadvantages. There are also various screening tools used for surgical patients, such as Nutritional Risk index (NRI) and NRS-2002, which have been tested in several previous studies5,9,10. The Simple Nutrition Screening Tool (SNST) with six questions identifies patients at risk of malnutrition in Indonesia11,12. In adult patients, the elderly, hemodialysis, diabetes mellitus, and people with cancer, research on nutritional screening using SNST has been conducted12,13,14,15,16. However, no study has shown that SNST can be used to assess the risk of malnutrition in surgical patients compared with other screening tools.
The SGA is a nutritional assessment tool that considers predictors of complications, such as poor wound healing and infection and in severely malnourished patients, which is associated with a longer LOS4. Furthermore, SGA is a tool for assessing nutritional status with a comprehensive method originally developed for assessing surgical patients4. However, nutritional assessment using other methods, such as anthropometry and biochemistry in surgical patients has advantages and disadvantages. Therefore, the comparison of anthropometric and biochemical parameters with SGA is necessary as a comprehensive method for determining the nutritional status of surgical patients. Therefore, this study aimed to compare the SNST with other nutritional screening tools (NRS-2022, NRI), nutritional assessment parameters, and the SGA in surgical patients.
MATERIALS and METHODS
Study Design and Subjects
This was an observational study conducted using a cross-sectional design. The inclusion criteria were adult surgical patients undergoing surgery GI procedures [GI cancer surgery, hernia surgery and repair, esophagus and foregut (upper GI) surgery, gallbladder surgery, liver and bile duct surgery, pancreas surgery, etc.] and non-GI procedures (orthopedics, urology, neurology, etc.) with medical diagnose cancer and non-cancer (diabetes mellitus, cholelithiasis, close fracture, etc.), that hospitalized from January to July 2020, able to communicate, were evaluated within the first 24 h of admission. The exclusion criteria for this study were patients who had mental disorders and pregnant women. Additionally, all participants provided informed consent before being enrolled in the study. Approval was granted by the Ethics Committee of the Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, and Dr. Sardjito General Hospital (ref. no.: KE/FK/0883/EC/2019, approval date: July 31, 2019).
Data Collection
Within 24 h after admission, nutritional screening tools (NRI, NRS-2002, SNST), assessments (anthropometric, biochemical), and SGA were administered by trained staff to all surgery patients. Anthropometric measurements were carried out directly. Meanwhile, a questionnaire form was provided for measuring SGA and nutritional screening, and the data of the patient was obtained from the medical records.
The BMI was calculated using the weight and height of the patients [BMI = weight (kg)/height (m2)] and was classified as malnourished when <18.5 kg/m2 17. Furthermore, the mid-upper arm circumference (MUAC) was measured using a met-line in the middle of the upper arm and was categorized as malnourished when <23.5 cm18. The SGA was based on changes in diet intake, estimated weight loss, clinical history, and a physical examination. Meanwhile, SGA was selected as the gold standard, and the results were grouped into moderately (B) and severely (C) malnourished as well as well-nourished (A) to enable comparisons between groups5.
Biochemical data were obtained from the patient’s medical record. Albumin levels ranging between 3.5-5.0 g/dL indicate good nutrition for both genders and a total lymphocyte count (TLC) less than 1500 cells/mm3 indicates malnutrition19,20,21. Furthermore, the hemoglobin (Hb) level was compared with the reference value for men (13 g/dL) and women (12 g/dL)19.
The NRI was derived from serum albumin, and the ratio of actual to normal weight was specially developed for surgical patients. Therefore, the formula used for the NRI was [15.19× serum albumin (g/dL) +41.7× actual weight (kg)/usual weight (kg)], while the results were grouped into 2 categories and were classified as the risk of malnutrition (low, medium, high), and the score was below 100 to enable comparisons15. The NRS-2002 includes a nutritional score based on BMI, food intake, weight loss, disease severity, and an age adjustment for patients >70 years old. Patients with a final score of ≥3 were classified to be at risk of malnutrition9. Furthermore, the SNST had six questions, required no anthropometric measurements and completed within a short time for each respondent. The SNST questions were as follows: 1) Does the patient appear thin? 2) Do your clothes appear looser? 3) Have you recently lost weight unintentionally (within the last six months)? 4) Have you cut back on your food intake in the last few weeks? 5) Do you feel weak, sluggish, or powerless? and 6) Do you have a disease that causes you to change the amount or type of food you eat? The patient is at a risk of malnutrition when the final score is ≥3 12.
Statistical Analysis
The data were analyzed using the SPSS 23.0 statistical software. Furthermore, qualitative data were expressed as frequencies and in percentage, while quantitative with a normal distribution were expressed as the mean ± standard deviation and median (minimum-maximum) for non-normally distributed data. Meanwhile, the comparison between patient characteristics, nutritional screening tools (NRI, NRS-2002, and SNST), and nutritional assessments (BMI, MUAC, albumin, Hb, and TLC) with SGA were analyzed using chi-square test, Student’s t-test, or Mann-Whitney U test as appropriated. The receiver operating characteristic (ROC) analysis was used to determine the cut-off point of the diagnostic test using a graph depicting the bargaining between sensitivity and specificity. A p-value <0.05 was defined as the level of significance.
The validity (sensitivity, specificity) was calculated to assess the comparative value of the nutritional screening tools. The area under the curve (AUC) was also calculated as part of the validity test to obtain the discrimination value that determines the precision of the screening tool to detect malnutrition. Additionally, the validity grade test followed the recommended cut points for sensitivity and specificity as well as AUC, ‘poor’, sensitivity or specificity <50%, with AUC <0.6; ‘fair’, sensitivity or specificity >80% but both >50%, with AUC 0.6-0.8; as well as ‘good’, sensitivity and specificity > 80%, AUC >0.812,22,23.
RESULTS
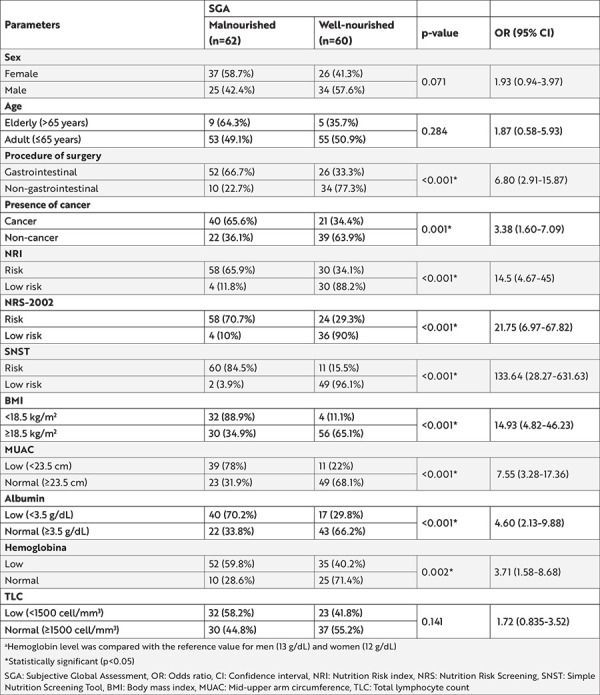
Three of the 125 surgical patient subjects in this study were excluded because anthropometric measurements such as MUAC and body weight could not be taken due to ascites and edema. A full anthropometric examination could not be performed on some people due of leg wounds. Out of 122 patients, 63 (51.6%) were women with a mean age of 49.62±14.19 and 61 subjects (50%) were diagnosed with cancer. This study showed that there was a difference in the prevalence of the risk of malnutrition. The nutritional screening tools by NRI, NRS-2002, and SNST identified the patient at a risk of malnutrition to be in the range of 72%, 67%, and 58%, respectively, while BMI, MUAC, Albumin, TLC, and Hb identified patients at the risk of malnutrition to be in the range of 29%, 41%, 47%, 45%, and 71% respectively. The comparison between the characteristics of the patient’s and their nutritional parameter results with SGA as the reference method are presented in Table 1. The results showed that there were significant correlations between the procedure of the surgery, presence of cancer, the 3 screening tools, anthropometric parameters, and albumin compared with SGA (p<0.05). According to the SGA, patients who underwent GI tract surgery had a 6.8 times (95% confidence interval 2.91-15.87) higher risk of malnutrition than patients who underwent non-digestive tract surgery.
Table 1. Patient characteristics at hospital admission.
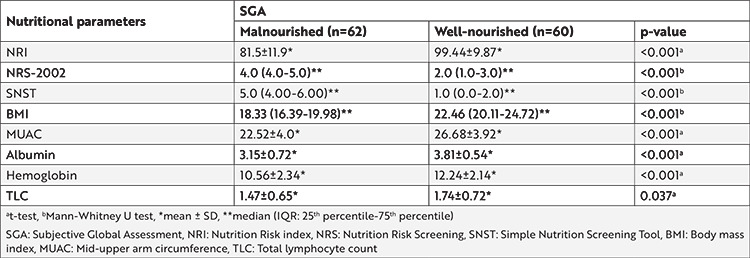
The differences in the mean score of the nutritional parameters (NRI and NRS-2002) with the nutritional status based on the SGA are shown in Table 2. Based on the results, there were significant correlations between SGA and the screening tools, anthropometric parameters, albumin, and Hb (p<0.001). Additionally, TLC also correlated significantly with SGA, but the association was weak compared with the others (p<0.05). Table 2 also shows that patients at risk of malnutrition had lower average value for the NRI and objective parameters (Hb, TLC, albumin, BMI, and MUAC) compared with patients without malnutrition. Patients at risk of malnutrition had a higher average of SNST and NRS-2002 scores than patients who were not at risk of malnutrition.
Table 2. Comparison of nutritional screening tools, anthropometric, biochemical measurement and SGA at hospital admission.
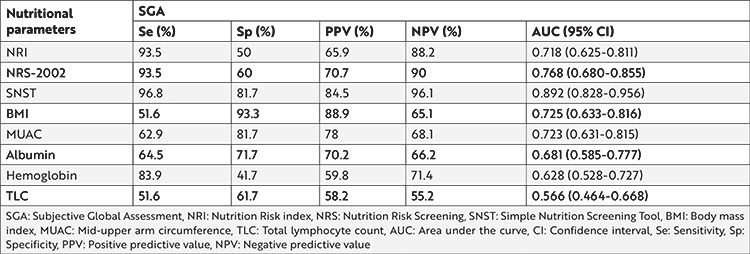
The accuracy of each nutritional parameter for identifying malnutrition as determined by the SGA is shown in Table 3. SNST had the highest sensitivity (96.8%), specificity (81.7%), and negative predictive value (96.1%), while BMI had the highest positive predictive value (88.9%). The other two screening tools also had high sensitivity, but lower sensitivity compared to SNST. Additionally, NRI and NRS-2002 had 93.5% sensitivity as well as 50% and 60% specificity respectively. The SNST has a good category among the nutritional screening tools with sensitivity and specificity >80%, as well as AUC >0.8.
Table 3. The accuracy of screening and assessment tools in detecting malnutrition (as determined by Subjective Global Assessment).
DISCUSSION
Based on the characteristics of the patient, some that experienced the GI surgery were at a risk of malnutrition than those in the non-GI area. These results are consistent with the study of Mosquera et al.24 (2016), indicating that patients who received digestive surgery are at risk of malnutrition, which can increase the length of postoperative stay (LOS) longer, more severe complications, higher costs, readmission rates, and death in the hospital. The risk of malnutrition was higher in surgical patients diagnosed with cancer. Furthermore, this is due to the imbalance between the patient’s nutritional needs, the requirement of the tumor, and the availability of nutrients. When this persists for a long time, it results in cachexia and increases the risk of mortality and morbidity25. Meanwhile, due to the lack of an adequate sample of people over 65 years of age, the patient’s age did not show significant results, given that other studies have presented a significant correlation between age and malnutrition in elderly patients26.
The SNST, which was developed in the Indonesian population, was one of the screening tool used in this study. The SNST has been tested against other screening tools recommended by the Academy of Nutrition and Dietetics, namely the Malnutrition Screening Tool, Malnutrition Universal Screening Tool, NRS-2002, and Short Nutritional Assessment Questionnaire in adult patient populations in Indonesia12,27. According to the findings, all of these nutrition screening tools are appropriate for predicting malnutrition in hospitalized patients in Indonesia. As a result, we conducted a study on surgical patients using SNST, NRS-2002 (a grade II screening tool with fair strength and recommended by the ESPEN consensus), NRI (a surgical nutritional screening tool), and nutritional assessment tool, in comparison to SGA as the gold standard.
SNST has higher values for the validity results. Additionally, SNST has previously been tested and has high validity compared with other nutritional screening tools. This is partly because most Indonesians rarely perform routine weight checks at home. Therefore, tools such as SNST, which have no questions on weight loss, are usually more suitable to be used11. Furthermore, several studies have proven that SNST is suitable as an alternative screening tool in hospitals because it is considered valid and reliable in determining the risk of malnutrition in patients11,12,13.
Although NRI has a high sensitivity value as well as a fair AUC, the specificity value does not exceed 50%. This suggests that NRI may not be specific in predicting surgical patients at a risk of malnutrition. This is in line with the research carried out by Kyle et al.8 (2006), which stated that the NRI may not be specific for diagnosing malnutrition in all hospitalized patients.
The prevalence of anemic surgical patients is quite high in this study, but this is not supported by the results of the Hb validity test as a marker of malnutrition risk, which is in the poor category due to a specificity value of <50%. This is consistent with the comparison of patients with low Hb levels, which indicates a high risk of malnutrition. Moreover, anemia is frequently caused by tumor-induced blood loss, with increased cytokine activity resulting in decreased iron absorption and increased hepcidin use, causing chronic anemia28.
Our findings showed that the screening tools can identify surgical patients at risk of malnutrition. BMI, MUAC, albumin, and Hb had significant results for identifying the risk of malnutrition compared with SGA. They can be used to determine the nutritional risk and nutritional status in surgical patients during hospitalization. However, when compared to other parameters, the area under the ROC curve for the SNST and NRS-2002 performs good and fair validity according to the category, implying that the SNST and NRS-2002 are the best screening tool for detecting the risk of malnutrition. It has been shown that single parameters are insufficient to assess the nutritional risk because nutritional risk depends on several factors, including objective and subjective clinical parameters that are sensitive to change. NRS-2002 and SNST assess current conditions, stable conditions (weight loss), decreased conditions (intake), and severity of disease29. Nutritional screening tools attempt to record objective and subjective clinical parameters sensitive to these changes.
This study has limitations in such a way that the number of patients over 65 years needs to be increased as the number was not proportional to the number of patients below 65 years. Additionally, the patient’s pre-treatment history should be included as this criterion tends to affect the patient’s current condition and its relationship with the incidence of malnutrition in surgical patients. Furthermore, the GLIM phenotypic criteria of involuntary weight loss, reduction in muscle mass, and etiological reduction in food intake were not used. Another limitation is that this study only performed nutritional screening when the patients were newly admitted without observing any surgical complications.
CONCLUSION
There were significant associations for screening (NRS-2002, SNST) and nutritional assessment tools (BMI, MUAC, albumin) compared with SGA. Therefore, both the tools will consistently identify surgical patients at the risk of malnutrition in such a way that nutrition care can be initiated promptly.
Footnotes
Ethics
Ethics Committee Approval: Approval was granted by the Ethics Committee of the Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, and Dr. Sardjito General Hospital (ref. no.: KE/FK/0883/EC/2019, approval date: July 31, 2019).
Informed Consent: All participants provided informed consent before being enrolled in the study.
Peer-review: Externally and internally peer-reviewed.
Author Contributions
Surgical and Medical Practices: S.S., A.S.S., D.K.C., A.I.R., A.Y.H., Consept: S.S., A.Y.H., Design: S.S., A.Y.H., Data Collection and/or Processing: A.S.S., D.K.C., A.I.R., Analysis and/or Interpretation: S.S., A.S.S., Literature Search: S.S., A.S.S., D.K.C., A.I.R., Writing: S.S., A.S.S.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: Grant from Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada Yogyakarta.
References
- 1.Inciong JFB, Chaudhary A, Hsu HS, et al. Hospital malnutrition in northeast and southeast Asia: A systematic literature review. Clin Nutr ESPEN. 2020;39:30–45. doi: 10.1016/j.clnesp.2020.06.001. [DOI] [PubMed] [Google Scholar]
- 2.Nigatu YD, Gebreyesus SH, Allard JP, Endris BS. The effect of malnutrition at admission on length of hospital stay among adult patients in developing country: A prospective cohort study. Clin Nutr ESPEN. 2021;41:217–24. doi: 10.1016/j.clnesp.2020.12.013. [DOI] [PubMed] [Google Scholar]
- 3.Weimann A, Braga M, Carli F, et al. ESPEN practical guideline: Clinical nutrition in surgery. Clin Nutr. 2021;40:4745–61. doi: 10.1016/j.clnu.2021.03.031. [DOI] [PubMed] [Google Scholar]
- 4.Detsky AS, Mclaughlin JR, Baker JP, et al. What is Subjective Global Assessment of Nutritional Status? J Parenter Enter Nutr. 1987;11:8–13. doi: 10.1177/014860718701100108. [DOI] [PubMed] [Google Scholar]
- 5.Almeida AI, Correia M, Camilo M, Ravasco P. Nutritional risk screening in surgery: Valid, feasible, easy! Clin Nutr. 2012;31:206–11. doi: 10.1016/j.clnu.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Andonovska B, Kuzmanovska BK, Andonovski AG, Kartalov AB, Petrovska-Cvetkovska D. Malnutrition in the surgical patients. Sanamed. 2016;11:229–37. [Google Scholar]
- 7.Haines KL, Lao W, Ngyen BP, et al. Evaluation of Malnutrition via Modified GLIM Criteria for in Patients Undergoing Emergent Gastrointestinal Surgery. Clin Nutr. 2021;40:1367–75. doi: 10.1016/j.clnu.2020.08.026. [DOI] [PubMed] [Google Scholar]
- 8.Kyle UG, Kossovsky MP, Karsegard VL, Pichard C. Comparison of tools for nutritional assessment and screening at hospital admission: A population study. Clin Nutr. 2006;25:409–17. doi: 10.1016/j.clnu.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Kondrup J, Rasmussen HH, Hamberg O, Stanga Z; Ad Hoc ESPEN Working Group. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22:321–36. doi: 10.1016/s0261-5614(02)00214-5. [DOI] [PubMed] [Google Scholar]
- 10.Pokharel N, Katwal G, Adhikari SK. Comparison of preoperative Nutritional Risk Index and Body Mass Index for predicting immediate postoperative outcomes following major gastrointestinal surgery: Cohort-study. Ann Med Surg (Long) 2019;48:53–8. doi: 10.1016/j.amsu.2019.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hadi H, Hakimi M, Asdie AH. Development, validation and reliability of the simple nutrition screening tool (SNST) for adult hospital patient in Indonesia. Pakistan J Nutr. 2014;13:157–63. [Google Scholar]
- 12.Hadi H, Hakimi M, Asdie AH. Comparison of Nutrition Screening and Assessment Parameters in Predicting Length of Hospital Stay. J Nutr Med Diet Care. 2018;4:1–9. [Google Scholar]
- 13.Mayasari M, Lestariana W. Simple nutritional screening tool (SNST) has good validity to identify risk of malnutrition on hospitalized elderly patients. Pakistan J Nutr. 2014;13:573–8. [Google Scholar]
- 14.Susetyowati S, Djarwoto B, Faza F. Nutrition Screening Tools as Predictor of Malnutrition for Hemodialysis. Saudi J Kidney Dis Transpl. 2017;28:1307–13. doi: 10.4103/1319-2442.220871. [DOI] [PubMed] [Google Scholar]
- 15.Rohimah BB, Sugiarto S, Probandari AA, Wiboworini BB. Comparison of a Simple Nutrition Screening Tool (SNST) Compared with Subjective Global Assessment (SGA) in Body Mass Index (BMI) Assessments of Type 2 Diabetic Patients Validation of SNST Versus BMI in T2 Diabetes. Pakistan J Nutr. 2016;15:412–8. [Google Scholar]
- 16.Susetyowati S, Sarasati RM, Rizqi F, Sanubari NDG, Nuraini A. Determining the Valid Tools to Screen Malnutrition in Cancer Patients: A Comparison to Patient Generated-Subjective Global Assessment (PG-SGA) J Gizi Indones (The Indones J Nutr) 2022;11:49–56. [Google Scholar]
- 17.WHO Expert Consultation No authors listed. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 18.Van Tonder E, Mace L, Steenkamp L, Tydeman-Edwards R, Gerber K, Friskin D. Mid-upper arm circumference (MUAC) as a feasible tool in detecting adult malnutrition. South African J Clin Nutr. 2019;32:93–8. [Google Scholar]
- 19.Raymond J, Morrow K. Krause and Mahan’s Food & The Nutrition Care Process Krause and Mahan’s Food & The Nutrition Care Process 15th ed. Vol. 68, Elsevier. Philadelpia: Saunders. 2020:p 1216. [Google Scholar]
- 20.Bharadwaj S, Ginoya S, Tandon P, et al. Malnutrition: Laboratory markers vs nutritional assessment. Gastroenterol Rep (Oxf) 2016;4:272–80. doi: 10.1093/gastro/gow013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Omran ML, Morley JE. Assessment of protein energy malnutrition in older persons, part II: laboratory evaluation. Nutrition. 2000;16:131–40. doi: 10.1016/s0899-9007(99)00251-8. [DOI] [PubMed] [Google Scholar]
- 22.Power L, Mullally D, Gibney ER, et al. A review of the validity of malnutrition screening tools used in older adults in community and healthcare settings - A MaNuEL study. Clin Nutr ESPEN. 2018;24:1–13. doi: 10.1016/j.clnesp.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Allard JP, Keller H, Gramlich L, Jeejeebhoy KN, Laporte M, Duerksen DR. GLIM criteria has fair sensitivity and specificity for diagnosing malnutrition when using SGA as comparator. Clin Nutr. 2020;39:2771–7. doi: 10.1016/j.clnu.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 24.Mosquera C, Koutlas NJ, Edwards KC, et al. Impact of malnutrition on gastrointestinal surgical patients. J Surg Res. 2016;205:95–101. doi: 10.1016/j.jss.2016.05.030. [DOI] [PubMed] [Google Scholar]
- 25.Arends J, Bachmann P, Baracos V, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2017;36:11–48. doi: 10.1016/j.clnu.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 26.Yu Z, Kong D, Peng J, Wang Z, Chen Y. Association of malnutrition with all-cause mortality in the elderly population: A 6-year cohort study. Nutr Metab Cardiovasc Dis. 2021;31:52–9. doi: 10.1016/j.numecd.2020.08.004. [DOI] [PubMed] [Google Scholar]
- 27.Skipper A, Coltman A, Tomesko J, et al. Position of the Academy of Nutrition and Dietetics: Malnutrition (Undernutrition) Screening Tools for All Adults. J Acad Nutr Diet. 2020;120:709–13. doi: 10.1016/j.jand.2019.09.011. [DOI] [PubMed] [Google Scholar]
- 28.Randi ML, Bertozzi I, Santarossa C, et al. Prevalence and Causes of Anemia in Hospitalized Patients: Impact on Diseases Outcome. J Clin Med. 2020;9:950. doi: 10.3390/jcm9040950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rasmussen HH, Holst M, Kondrup J. Measuring nutritional risk in hospitals. Clin Epidemiol. 2010;2:209–16. doi: 10.2147/CLEP.S11265. [DOI] [PMC free article] [PubMed] [Google Scholar]


