Summary
Background
The UK's ‘First do no harm’ report highlighted missed opportunities to prevent harm and emphasised the need to incorporate patient voices into healthcare. Due to concerns about, and the subsequent suspension, of vaginal mesh for urinary incontinence thousands of women face the decision about mesh removal surgery. The aim of this study was to explore and understand the experience of living with complications attributed to vaginal mesh surgery so that this knowledge can contribute to improvements in care for those considering mesh, or mesh removal, surgery.
Methods
This study was embedded in the ‘PURSUE’ study which explored the experiences of 74 people with urogynaecological conditions in the UK (30th April 2021–17th December 2021). Of these 74 people, fifteen women reported complications that they attributed to vaginal mesh surgery. We used the six stages of reflexive thematic analysis to conceptualise these fifteen accounts.
Findings
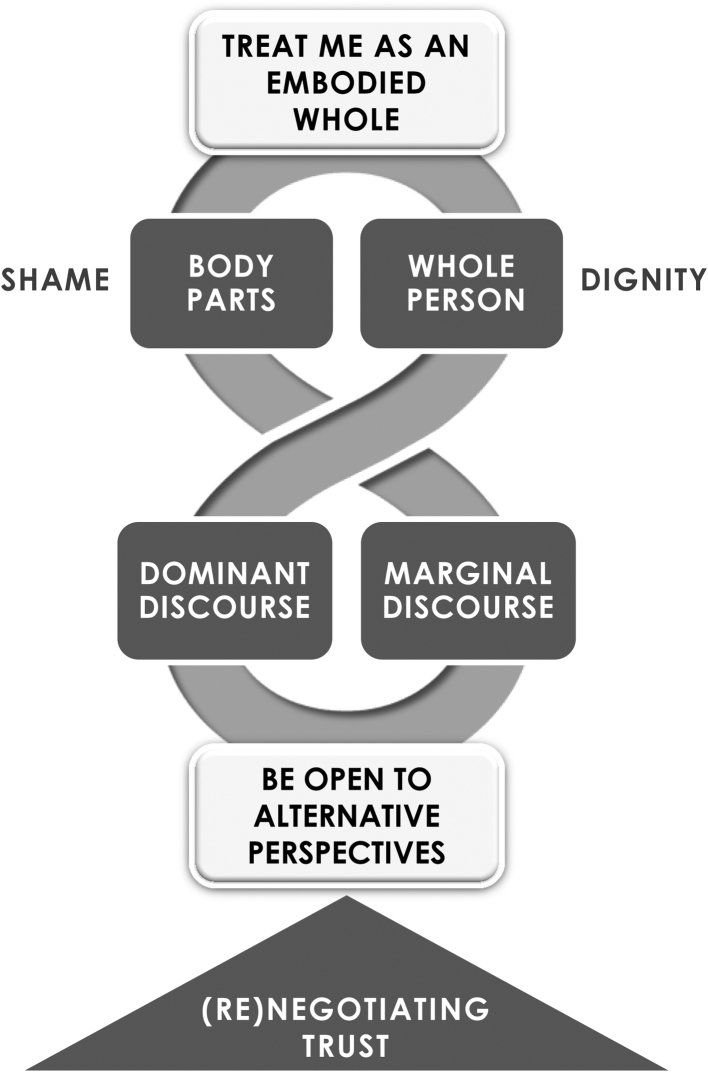
Our conceptual model anchors eight themes around two dualities: (1) body parts versus body whole, (2) dominant discourse versus marginal discourse. Our themes indicate that trust can be established through: (1) embodied healthcare that focuses on connecting with patients’ lived experience, (2) dialectic communication that recognises patient experiences and remains open to alternative perspectives.
Interpretation
This study raises some important issues for education and practice. Our findings can translate to other health settings where treatments aimed to provide care have caused harm.
Funding
NIHR Policy Research Programme (NIHR202450).
Keywords: Qualitative research, Urogynaecology, Stress urinary incontinence, Tension-free vaginal Tape, Social science
Research in context.
Evidence before this study
We searched MEDLINE, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and PsycINFO from database inception up until March 6, 2023, without language restrictions, and identified a systematic review and thematic synthesis of qualitative research on women's experiences of and perspectives on vaginal mesh surgery. This review indicates that discounting women's experiences has the potential for harm. The review did not include a qualitative interview study of this experience in the UK.
Added value of this study
Quality healthcare for those considering mesh removal surgery is centred on trust, promoted by (1) connecting with patients’ lived experience, and (2) dialectic communication that recognises and regards patient experiences.
Implications of all the available evidence
Failure to consider patients as embodied individuals (who might have alternative perspectives) can lead to lost trust and subsequent harm. This raises some important issues for healthcare education, policy, and practice, and should be a consideration in joint decision-making across conditions.
Introduction
Permanent medical devices are implanted for a wide range of indications across many medical specialties. There have been several high-profile device safety issues raised, owing in part to the host immune response to synthetic materials.1, 2, 3 Vaginal mesh surgery involves the placement of a polypropylene surgical implant to treat pelvic organ prolapses (POP) or stress urinary incontinence (SUI). These are highly prevalent conditions which have a profound impact on lives, and for which many women undergo surgery.4,5 Developed in the late 1990's, vaginal mesh implants were heralded as an effective and safe alternative to traditional techniques that had been associated with high rates of failure and morbidity.6
The synthetic mid-urethral sling vaginal mesh implant was considered by many to have become the gold-standard surgical treatment for SUI.7,8 However, within a decade of widespread adoption, concerns developed due to adverse events such as pain, dyspareunia, incontinence, mesh exposure, haemorrhage, organ perforation, and infection.8, 9, 10 In many countries, public concern led to a cascade of governmental reviews and regulatory warnings, suspension of procedures, litigation, and an increasing body of literature highlighting potential harm.11,12 Patient concerns were supported by a limited body of qualitative research from the USA,13,14 Australia,15 New Zealand,16 and the UK.17 In the UK, public concern was such that the use of vaginal mesh to treat SUI is suspended until further notice. Although these concerns might lead to revision surgery or mesh removal,10 there is limited outcome data or consensus guidance to support patients on what to do about complications from mesh surgery.18 As a result, thousands of women around the world face a dilemma about surgical removal or expectant management, and specialist mesh centres across the UK have been commissioned by NHS England, Scotland, Wales, and HSC Northern Ireland in 2021.
The ‘First do no harm’ or Cumberlege report by the UK's Independent Medicines and Medical Devices Safety Review looked at the issue of vaginal mesh for SUI and highlighted missed opportunities to prevent harm in healthcare, with patients feeling as if they have been ‘dismissed, overlooked and ignored’.2 The report emphasised the need to incorporate patient voices into healthcare, resonating with the recent Women's Health Strategy for England.19 However, there is limited qualitative data aimed at understanding patients experiences of negotiating healthcare following complications from vaginal mesh. In 2021, following the publication of the Cumberlege report,2 the National Institute for Health and Social Care Research (NIHR) Policy Research Programme commissioned us to undertake an in-depth qualitative exploration of people's experiences of living with urogynaecological conditions to inform health and social care improvements in the UK.20 Our study included experiences of those who told us that they had been injured by vaginal mesh.
The aim of this study was to explore and understand the experience of living with complications attributed to vaginal mesh surgery so that this knowledge can contribute to improvements in care for those considering mesh, or mesh removal, surgery. We report themes from women experiencing complications from vaginal mesh surgery, and conceptualise these through a social science lens.
Methods
Patient and public involvement statement
The study was designed and analysed with the input of ten people with lived experience of the urogynaecological conditions.
Ethics approval and consent to participate
The study was approved by Berkshire National Research Ethics Service Committee (South Central) under reference 12/SC/0495.
Study design
The data is drawn from a UK qualitative study (n = 74) that explored the experiences of living with, and being treated for, urogynaecological conditions.20 We report findings from 15 women who reported complications following vaginal mesh surgery for SUI. We recruited UK adults living with urogynaecological conditions through multiple sources (30th April 2021–17th December 2021): NHS sites; advertisements, support groups, social media, and advisory panel members; snowball sampling; and working with health advocacy organisations and groups focused on inclusive gynaecological health care.
Qualitative data collection
Three social scientists conducted semi-structured interviews, either as online video calls or by telephone. We invited participants to tell us about their experiences and used a topic guide to prompt discussion (Table 1). This guide was developed from qualitative research syntheses21, 22, 23, 24 in collaboration with a steering group, and was piloted on two people with lived experience. The interviews started with an invitation to tell their story in their own way – “I'm going to ask you tell me a bit about your experiences with (…). You can say as much or as little as you want, and you can start at any point in your story”. With consent, all interviews were recorded and transcribed verbatim by approved transcribers compliant with data security policies. We checked each transcript against the recording for accuracy. Names and places were removed for de-identification. We gave participants the opportunity to read and mark any sections which they would like to expand or redact. This form of ‘respondent validation’ is a strategy to ensure trustworthiness of research.25
Table 1.
Interview schedule: example questions.
| Interview schedule: example questions |
|---|
|
Analysis
We used the six stages of reflexive thematic analysis to develop themes that cut across participants: (a) familiarisation; (b) coding; (c) generate initial themes; (d) develop and review themes; (e) refining and naming themes; (f) writing up. This provides a flexible method for distilling data into themes organised around a central idea.26 Reflexive thematic analysis goes beyond topic description and values the researchers’ interpretive lens. Interview transcripts were uploaded to NVivo 12 Software for qualitative analysis. The first author coded each transcript, a process that involves assigning a short phrase to a unit of meaning. Two researchers then discussed whether the assigned code did justice to the meaning. The aim of discussion was not to agree on a ‘correct code’ but to make sure that valuable nuance was not lost. The codes were then organised into themes around a central idea. Working in close collaboration during weekly meetings, the research team developed themes through constant comparison and discussion. This process facilitates the development of ideas by comparing similarities and differences across data.26 The research team included social scientists, a physiotherapist and hospital senior manager, and a urogynaecology surgeon, working alongside ten PPI members to refine the themes. Our analysis was influenced by conceptual approaches to qualitative research,27 which aim to offer insight through theorising. Again, working as a team during a series of meetings, we designed a conceptual model that integrated the themes into a storyline.
Role of the funding source
The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The funders had no role in: the collection, analysis, and interpretation of data; the writing of the report; and the decision to submit the paper for publication. All authors approved the final version to be published and all authors had access to anonymised coding reports.
Results
We recruited 74 people with a range of urogynaecological conditions into the PURSUE study. Eighteen had undergone Tension-free Vaginal Tape (TVT) or TVT-obturator (TVT-O) vaginal mesh surgery to treat SUI, fifteen of whom told us that they had been injured by mesh.
All mesh-injured participants were white, heterosexual, cis-gender women, aged between 48 and 78 years from England, Wales, and Northern Ireland. All reported having (or having had) urinary incontinence, with a further ten also reporting prolapse, and eight having had a hysterectomy. One participant was single, and all others were partnered or married. Thirteen participants had given birth to at least one child. Eight were living on a household annual income of less than £30,000. Table 2 shows the Index of Multiple Deprivation (IMD) based on postcode. IMD ranks neighbourhoods in England from 1 (most deprived area) to 32,844 (least deprived area) based on several indices of deprivation. These are then divided into equal groups to calculate the IMD decile (Table 2). Six participants had a university degree; the highest educational attainment for five participants was sixth form (or equivalent), and GCSE for two participants. Fourteen participants identified with having a disability; seven said their disability was solely related to mesh-injury.
Table 2.
Description of participants.
| Reported previous surgerya | Mesh exposure | Intervention planned | Age (years) | POP | Parity | Index of multiple deprivation decileb |
|---|---|---|---|---|---|---|
| TVT for UI | Yes | Partial removal | 48 | No | 4 | 10 |
| TVT for UI | Not known | Partial removal | 75 | Yes | 1 | c |
| TVT for UI | Yes | Partial removal | 51 | No | 2 | c |
| TVT for UI | Yes | Partial removal/awaiting full | 65 | No | 2 | 8 |
| TVT for UI | Yes | Partial removal/awaiting full | 55 | Yes | 2 | 7 |
| TVT for UI | Yes | Partial removal/awaiting full | 66 | No | 0 | 5 |
| TVT for UI | Yes | Partial removal/awaiting full | 49 | Yes | 1 | 5 |
| TVT for UI | Yes | Awaiting mesh removal consult | 52 | Yes | 0 | 7 |
| TVT for UI | Not known | Awaiting mesh removal consult | 59 | Yes | 4 | 6 |
| TVTO for UI | Yes | Removal | 62 | No | 2 | 8 |
| TVTO for UI | Not known | Awaiting mesh removal consult | 61 | Yes | 2 | 4 |
| TVTO for UI | Not known | Awaiting mesh removal consult | 52 | Yes | 3 | 7 |
| TVTO for UI | No | None | 78 | Yes | 3 | 6 |
| Mixed, including TVT and hysterectomy | Not known | Awaiting mesh removal consult | 72 | Yes | 2 | 6 |
| Mixed, including TVT and hysterectomy | Yes | Awaiting mesh removal consult | 49 | Yes | 1 | 4 |
This is based on participant reported surgery and we have not correlated with case notes/medical records.
IMD ranks neighbourhoods in England from 1 (most deprived area) to 32,844 (least deprived area) based on several indices of deprivation. These are then divided into equal groups to calculate the IMD decile.
IMD data not available outside England.
We report eight themes drawn from 52 initial subthemes (Supplementary material) illustrated with verbatim narrative, and a conceptual model.
Incontinence steals your dignity
Participants described the humiliation of urine leakage that was the context for surgery, and which could also become a barrier to discussions about surgical complications. They described the impact on their sense of dignity, or worth. The shame, taboo, and stigma around incontinence played a part in the decision to have mesh surgery, and the decision to remove it. Participants felt “ashamed”, “dirty”, “humiliated”, and “mortified”, because of lost bladder control.
[Incontinence] was very difficult for me to manage especially in front of my two teenage boys … I was walking along and found I was completely incontinent, or sitting in the car after a day out with the boys and completely wet the car seat … it was mortifying … they are mortified too.
Whilst some experienced reprieve from incontinence after vaginal mesh (sometimes for many years), others found minimal improvement or that incontinence returned soon after. Participants found it difficult to talk about surgical complications and this could be a barrier to care or support.
I tried to cover it up that I had actually had transvaginal tape … I didn't want people to know that maybe I could wet myself … it all stems from this one thing that started in your vagina. Really hard … How do you start conversations like that? It limits your ability to converse with anybody about where your pain is.
Mesh surgery has stolen me
Participants described the physical, social, and emotional impacts of damage attributed to mesh. For some, pain was at the core of this experience: “I cry out in pain”. Pain could be “deep”, “drilling”, “like needles” “agonising”, “excruciating”. Participants felt exhausted from no rest or sleep. Some felt “robbed” of present and future selves, and were getting “no joy out of living”: “shrouded in a miserable cloak”. Some were hit hard financially, or relied on benefits or a partner's income. There was a deep-felt rage and anguish that “this [harm] has been done to me”.
I can't see how there's gonna be any future … I can't see how the mesh improves … and my whole life, I could end up with no help whatsoever except living on benefits … it's psychologically having to deal with the fact that you're gonna get worse. It's scary … it's frightening … [it's] massive how hopeless you feel.
Some felt “heartbroken” by the impact on relationships, and some felt “utterly alone”. Being unable to want, enjoy, or have sex could be a “real life changer”: some were sad or embarrassed to ask their partner to “get a move on”. Some explained that mesh had “eroded” into their vagina and injured their partner's penis. Some felt they were missing out on being mum, or felt guilty for “letting children down”. Others had “dropped out of the mainstream of life” as people “drifted away”.
It gets boring for people … when someone's heard that someone's suddenly gone into hospital, they all rush around and want to come and see them and give them flowers [but] … people get bored with it, and they're not interested, and you sort of get dropped out of your social set.
I feel dehumanised, like meat
This theme explores the female body as dehumanised “meat” or “body parts”. Participants used words such as “butchered”; “I woke-up in agony”, “my sheets were soaked in blood”, as if “something had been slaughtered”. Some felt that they had not been fully informed and had therefore not consented to surgery.
I was bleeding all over the floor, and running down my legs, it was everywhere, I was covered in blood … I saw the consultant before she butchered me … [and said] “when you get me in there, please remember that I'm a human being, I'm not a lump of meat.” I'm not just a body, I am a person … they start cutting and I think we lose our humanity; we are just another piece of meat to be processed.
There was a sense that surgery had been “done to me”, and of being left to “fend for myself”. Some remembered being discharged with uncontrolled pain, or a urinary catheter, or having to improvise at home with sanitary pads to stem bleeding. Participants described mesh as “sharp”, “cutting”, “hard”, “barbed”, “a razor”. The mesh was felt to “attack” from the inside, causing autoimmune reactions. Others described post-surgical infections or abscesses, or being left to “rot on the inside”.
Just this awful smell all the time. It smells like … wet hay. It's a terrible smell. But you just can't do anything to get rid of … you have this god almighty smell that follows you around all the time because everything's rotting on the inside.
Participants felt outraged that their surgeon had described vaginal mesh as a “ribbon”, “tape” or “sling”, whilst implanting “hard” and “brittle” mesh into their “soft” body. Some felt that both the manufacturers and surgeons had known the risks. Some felt treated like “guinea pigs” and were incredulous that this had happened to so many without alarms being raised. Some were concerned about incentives, feeling that women had been treated as “cash cows”.
I am more than the sum of my body parts
Participants described the need to be treated as a human-being, not as body part. Good care was considered to look beyond compartments to see the whole. Participants wanted health professionals to understand that they were dealing with the basic tenets of human dignity, and to be cared for as fellow humans.
You make something a speciality and everything else gets forgotten … this is a big issue for this person that's in front of you. What we're looking at are the basics of dignity really, being able to pass urine, faeces … you bring sex into it … these are basic things in people's lives but they're big things … It doesn't cost anything to be nice and understanding and [to] acknowledge that this has a big impact on a person's life.
Participants juggled multifaceted lives that had not always been kind. Some had experienced childhood trauma. Some were living with “off-the-scale” caring roles. A good healthcare professional was described as someone who “is nice to me”, “hears my story”, “stands by me” and “cares”, even if they “can't treat”.
It's not all about medicine, it's about communication … body language as well as the spoken word … By dismissing somebody or not listening to them, you've completely put them on edge for the next time they have to go and see a professional because my trust is gone. And it doesn't matter how lovely and how nice the next professional person is, I have now got doubts in my head.
I blindly trusted the surgeon
This theme explores the impact of lost trust on decisions going forward. Some had become sceptical, and said that trust would be “hard to win back”. Some avoided healthcare altogether. Participants felt “lied to”, “conned” or “tricked” into surgery, and felt that transparency should underpin treatment decision-making.
When people lose trust, they're not gonna come to you and that has a massive knock-on effect … I will avoid going. I would rather sit and struggle … there are really kind, loving people that work within the health service. But you need to be knowledgeable about what you're saying yes to ‘cos I was blind and just walked in and put my trust into people.
Participants felt angry that vaginal mesh had been “sold to them” as “gold standard”, saying that risks had been underplayed: “it was billed as quick and easy”. Some felt that, driven by desperation, they had been gullible and not heard “warning bells”: “people who used to sell snake oil were very convincing”. Some felt angry that they had not been told about other treatment options.
I feel cross and angry with the surgeon who put it in, who I completely and utterly trusted … he downplayed any complications, he reassured me that he was the expert … he didn't tell me there were other options available at the time. And so really did I have a fully informed decision and consent? I consented to his truth.
The medical professionals stuck fast to the medical discourse
This theme describes encountering an infallible and inflexible medical way of knowing. Participants felt that the medical community “denied” that symptoms were caused by mesh. Some felt treated as if they were “neurotic”, or “hysterical”. Participants described the medical community as a “buddy system” or “members club” where everybody “covers each other's back”. Some recorded consultations or took a “witness”, concerned that details were omitted in medical notes to “cover things up”.
[The notes] say, “I discussed that with her” … when that wasn't actually mentioned on your recording of the meeting … and yet in the letter that goes back to your GP, it says, “We discussed …” No, we didn't. You have to say that to cover your own risk factors, but you didn't discuss it with me … It just makes your blood boil.
Participants did not feel encouraged to ask questions, or allowed to contribute knowledge. Some felt that, even when asked their opinion, the professional “talked over” them. There was a sense that doctors were “stuck in their ways”, and that symptoms were disregarded as “a natural part of being a woman”.
You feel as if you're not believed, they look at you as if you're a time waster. They've made up their minds what's wrong with you, and half the time they're looking at you as if you've just walked out of the local mental institution … thinking, ‘Oh well here we go again, some hypochondriac patient … she's got everything under the sun’
Healthcare professionals are fallible
This theme describes health professionals as fallible humans who share the same foibles, vulnerability, and liability to error as other human-beings. Some felt that whilst “most health professionals are great”, “it only takes one to rock the boat”. Some wondered whether NHS staff were “just worn down” because of limited resources.
The medical profession is such an amazing profession … but it just takes a few people to rock the boat and completely make it come tumbling down in someone else's eyes … the trouble is, it's those few that impact you in a negative way that become the forefront of everything.
Participants felt that health professionals must be accountable, “admit”, “learn from” and “apologise for” mistakes.
[The air ambulance team do] an instant ‘debrief’ after an incident, especially quite a nasty one … and it's never a criticism of anybody, it's just learning points … we could've done it a different way … they really go for it. They don't hold back on anything … they all take it and walk away and then come back the next day.
Seeking another way of knowing in communitas
This theme explores a sense of solidarity and bonding, or communitas, forged in online communities and sustained by the collective marginality of those existing together in a liminal space or “wilderness”. In communitas, participants found their way out of the wilderness and no longer felt alone or “mad”.
Hearing other people stories … I think it might have been first on there where I realised that this could probably be all to do with mesh … I'm reading somebody else's story and I think, ‘that's me’ … but it just gave me that real ‘I'm not going mad’: because I felt as though I was.
Some experienced personal growth through communitas. There was a sense that “the internet has made us wiser” and that “I will no longer take any nonsense”. Participants felt a duty of advocacy towards the community, and did not want anyone one else to “go through this”. There were also those who needed to “switch off” from the community, which did not always feel supportive or reassuring.
Over time, that fear has lessened, and the anxiety has reduced, but sometimes the researching stuff also is a double-edged sword, and sometimes it makes you more anxious and more fearful in the short term.
Between a rock and a hard place
Participants described the difficult decision to have mesh (fully or partially) removed. Some felt like they were “living in limbo” or “treading water” whilst waiting for a mesh complications consultation, “pushed from pillar to post”: an “endless conveyor belt” of “humiliating tests” and “red tape” with no one really knowing what to do. Some were concerned that they were reliant on those who “15 years ago might have been putting the mesh in”. The decision was described as “Russian Roulette”: “I am frightened if I take it out; I am frightened if I don't”. Some felt certain that they wanted the mesh completely removed to prevent “further damage”, even if it would be like “taking fish bones out of chewing gum”. Others were scared about complications, of needing further surgery, or of becoming incontinent again.
I'm scared. I know there are risks … but there are also risks of keeping it inside … I just want to get rid of this foreign body that should've never been there … psychologically it would be great to know that I haven't got this foreign body inside me anymore.
Lost trust made it difficult to know “whose hands to put my life in”, and some sought second (sometimes conflicting) opinions in private care.
He offered to just cover up the mesh, the exposed mesh, or just trim a little bit off and cover it up. And was very anti-doing anything more than that … to have a full removal, or even a partial removal. The risks of that are not inconsequential … Who to trust? Which surgeon do I go with? Who do I trust to do it? Who's got the most experience? … I feel like I'm in between a rock and a hard place.
Our findings indicate the need for a (re)negotiation of trust. Our conceptual model (Fig. 1) represents a complex process anchored around two dualities. First, whilst recognising that we are body parts, finding trust means simultaneously being regarded as a whole person. Second, we illustrate a tension between the dominant (medical) discourse and a marginal (online) discourse. Our model indicates that (a) treating patients as embodied people, and (b) being open to alternative perspectives would help to rebuild trust.
Fig. 1.
Conceptual model: (re)negotiating trust. This figure represents our conceptual model. We see a process anchored around two dualities placed on a lemniscate (body parts/whole person: dominant discourse/marginal discourse). (Re)negotiating trust requires the clinician to negotiate these dualities by (a) treating the patient with dignity as an embodied whole and not focusing solely on body parts, and (b) being open to alternative perspectives rather than remaining fixed on the dominant discourse.
Discussion
This qualitative exploration was embedded in a qualitative study of 74 self-selected people with urogynaecological conditions. This report incorporates the voices of 15 who told us that they had been injured by vaginal mesh. We aimed to encapsulate their experiences so that healthcare systems can evolve through understanding. Our findings indicate a breakdown of trust, highlight areas needing repair, and include a request from women to treat me as an embodied whole. We found that trust is promoted by dialectic rather than didactic, or instructive communication, where clinicians and health systems must be open to alternative perspectives.
Our findings highlight barriers that impact on decision-making regarding mesh removal. Participants described how communication around surgery can be far from satisfactory. The UK's General Medical Council (GMC) guidelines encourage clinicians to “find out what matters to patients”28 and not make assumptions about what a person needs to know about their condition or treatments. Participants emphasised the need to be fully informed and involved in decisions. Although some recognised that withholding information might aim to “protect” the patient, there was a sense that withholding information served no protective function and eroded trust. Our findings re-iterate the need for fully informed consent in healthcare. As such, the GMC strongly affirm that patients should be involved, and supported, in treatment decisions. In the context of vaginal mesh surgery,2 the failure to recognise, acknowledge and apologise for harm is an important message, supported by our data. The GMC and Nursing and Midwifery Council confirm that apologising is not admitting legal liability and can be the right thing to do.29
We found that trust was at the heart of ‘good’ healthcare. However, trust is not straightforward: ‘blind’ trust can become a barrier to communication if no information is exchanged, whereas ‘broken’ trust can stimulate communication if a patient is more inclined to press for information.30 To gain trust requires different ways of ‘knowing’: Frank31 compares two of the ancient Greek branches of knowledge: Episteme and Phronesis. Episteme, the ideal for scientific knowledge, is concerned with establishing universal context invariant laws. Phronesis or wisdom, forged through experience and relationships, is concerned with moral life and human dignity.31 Our findings highlight the need for this relational knowledge, and we suggest that undervaluing Phronesis as a source of knowledge in healthcare has risks. In the context of mesh removal, we also found that a third branch of knowledge, Techne (meaning ‘craft’ knowledge) was integral when choosing a surgeon.
The influence of Cartesian dualism, conceptualising the mind and the body as separate entities, in western medicine has been culturally pervasive. Our findings support the argument that a shift to embodiment32 as a guiding philosophy would navigate us towards more trusting relationships. Embodiment, whilst recognising that we are physical bodies, shifts the focus of understanding to lived experience. We argue that the skills needed for ‘embodied’ healthcare are integral, not an adjunct, to effective care. This raises some important issues for clinical education and practice.
A dialectic, rather than didactic, way of knowing does not frame contradictory ideas as threatening; knowledge flourishes at the interface of opposing ideas. Turner places idea conflict within a positive frame, suggesting that society cannot progress, or even ‘function’, without a ‘dialectic’ tension between thesis and antithesis.33 Participants found themselves on the margins of normative medical discourse and needed to find validation, information, and support in ‘communitas’.33 Here, in an ambiguous limbo or ‘liminality’, some discovered ‘unprecedented potency’ for social action, as witnessed by the Cumberlege report.2 There were, however, those did not find solace in this space.
There are only a limited number of studies that explore the experience of vaginal mesh surgery.34 Our findings resonate with qualitative studies highlighting the profound impact on physical and social self as a potential complication of vaginal mesh.13, 14, 15, 16, 17 Our findings also resonate with a review highlighting potential harm from disregarding women's voices and failure to fully inform. Motamedi and colleagues argue that ‘epistemic injustice’ – whereby ‘a person's contribution to the production of knowledge is unrecognised or unjustly excluded, dismissed, or relegated to a lower status’ – is an ethical issue for careful consideration in healthcare.34
Many lives have been changed positively by vaginal mesh, and this is supported by evidence indicating high satisfaction rates following vaginal mesh slings for SUI.35 Yet large meta-analyses have highlighted uncertainty regarding long term effectiveness and safety of such surgical procedures, and have concluded that a better understanding of complications is ‘imperative’: this includes reporting and recording complications in national databases.36 Population data from Scotland concluded that nearly 1 in 10 women undergoing vaginal mesh insertion for SUI experience a complication peri-operatively within 30-days or up to five years9: although, in the same population, the risk of complications appear to be lower for vaginal mesh procedures compared to non-mesh alternatives.10 More recent large population studies in England with ten-year follow-up following surgery for SUI corroborate lower rates of re-operation following vaginal mesh insertion as versus non-mesh procedures. However, the authors emphasise the need for long-term patient-reported outcome data in this context: reoperation is but one outcome, and its importance to patients has not been well-studied.37
A criticism made of qualitative research is that it is biased, having a ‘tendency, inclination, or leaning towards a particular perspective’. However, qualitative research is not designed to test intervention effectiveness, and its truth is not grounded on representative or normally distributed samples.38 Qualitative research is underpinned by a different epistemological foundation about what makes things true, and sees truth in people's unique perspectives: it draws on small purposive samples to give voice to lived experience, and to develop ideas from ‘information rich’ (rather than statistically representative) samples.26 Future research to explore experiences of those who are satisfied following vaginal mesh surgery, or focusing on specific procedures, ages, or communities would give additional insight. For example, an exploration of the complex decision to remove mesh or leave it in situ, from the perspective of patient and health professional. We did not have access to medical records as participants were self-selected from multiple community, online, and healthcare sources. Participants did not therefore always describe, or know, the specific details of their vaginal mesh surgery.
A sociological exploration of surgical decision-making for mesh suggests that the widespread use of vaginal mesh resulted from a health professional mindline (36) of ‘fixing anatomy’, which meant that vaginal mesh ‘made so much sense’. They suggest that a shift to an alternative mindline ‘anchored in patient experience’ requires profound changes in how we assess the need for, and outcome of, surgery. This shift may have implications for professional identity as it is ‘intertwined with surgeons' embodied, and painstakingly acquired, skills’.39 Differentiating anatomy, or indeed pathology, from the experience of a condition may help us to understand the areas of miscommunication that led to widespread mesh use, and has important implications for clinical education in the future.
The issues surrounding vaginal mesh have impacts for many areas of clinical medicine, but also implications for device development and innovation, the role of industry, healthcare provision, autonomy, women's rights, and health education. Our findings provide important insights into experiences that, if placed at the centre of healthcare systems, will ensure safer and more inclusive healthcare. Qualitative enquiry and the social sciences can make a positive contribution to healthcare education, practice, and policy. Drawing from a group of women with unique experiences of harm from vaginal mesh surgery, our findings support an embodied and dialectic approach in healthcare interactions that can re (build) trust and contribute to effective and shared decision making in a range of contexts. Our findings may translate to other health setting where treatments aimed to care have caused harm.
Contributors
All authors made a substantial contribution to the conception or design of the work and the acquisition, analysis, or interpretation of data for the work. FT drafted the first version of the manuscript which was critically revised by AM, KB and MIK for important intellectual content. All authors approved the final version to be published. All authors agree to be accountable for the work, and in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. FT and AM verified and had access to the original transcripts, and all authors had access to anonymised coding reports.
Data sharing statement
Data for this project are not currently available for access outside the study research team. The dataset may be shared when finalised to bona fide researchers following request to AM who was the principal applicant for funding source.
Declaration of interests
FT has received grants or contracts from Pfizer, NIHR Policy Research Programme and the CSP charitable trust.
MK is Chair of International Urogynaecological Association FTECP committee. AM has received grants or contracts from the Oliver Bird Fund, Nuffield Foundation: OBF/43985 and the HTA Project: NIHR127489. The other author declares that they have no competing interests beyond their funding source.
Acknowledgements
We gratefully acknowledge our co-applicants, research team, and PPI members, and all those who share their stories with us. This study was funded by the NIHR Policy Research Programme (NIHR202450).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2023.101918.
Appendix A. Supplementary data
References
- 1.Greco C. The Poly Implant Prothèse breast prostheses scandal: embodied risk and social suffering. Soc Sci Med. 2015;147:150–157. doi: 10.1016/j.socscimed.2015.10.068. [DOI] [PubMed] [Google Scholar]
- 2.IMMDSR . Crown copyright; 2020. First Do No Harm – The report of the Independent Medicines and Medical Devices Safety Review.https://www.immdsreview.org.uk/downloads/IMMDSReview_Web.pdf [DOI] [PubMed] [Google Scholar]
- 3.Cohen D. How safe are metal-on-metal hip implants? BMJ Br Med J (Clin Res Ed) 2012;344 doi: 10.1136/bmj.e1410. [DOI] [PubMed] [Google Scholar]
- 4.Slieker-ten Hove M.C., Pool-Goudzwaard A.L., Eijkemans M.J., Steegers-Theunissen R.P., Burger C.W., Vierhout M.E. The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(9):1037–1045. doi: 10.1007/s00192-009-0902-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith F.J., Holman C.D., Moorin R.E., Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–1100. doi: 10.1097/AOG.0b013e3181f73729. [DOI] [PubMed] [Google Scholar]
- 6.Olsen A.L., Smith V.J., Bergstrom J.O., Colling J.C., Clark A.L. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–506. doi: 10.1016/S0029-7844(97)00058-6. [DOI] [PubMed] [Google Scholar]
- 7.Petros P. Creating a gold standard surgical device: scientific discoveries leading to TVT and beyond: Ulf Ulmsten Memorial Lecture 2014. Int Urogynecol J. 2015;26(4):471–476. doi: 10.1007/s00192-015-2639-3. [DOI] [PubMed] [Google Scholar]
- 8.Muller P., Gurol-Urganci I., Thakar R., Ehrenstein M.R., Van Der Meulen J., Jha S. Impact of a mid-urethral synthetic mesh sling on long-term risk of systemic conditions in women with stress urinary incontinence: a national cohort study. BJOG An Int J Obstet Gynaecol. 2022;129(4):664–670. doi: 10.1111/1471-0528.16917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keltie K., Elneil S., Monga A., et al. Complications following vaginal mesh procedures for stress urinary incontinence: an 8 year study of 92,246 women. Sci Rep. 2017;7(1) doi: 10.1038/s41598-017-11821-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morling J.R., McAllister D.A., Agur W., et al. Adverse events after first, single, mesh and non-mesh surgical procedures for stress urinary incontinence and pelvic organ prolapse in Scotland, 1997-2016: a population-based cohort study. Lancet (London, England) 2017;389(10069):629–640. doi: 10.1016/S0140-6736(16)32572-7. [DOI] [PubMed] [Google Scholar]
- 11.2017. https://wwwgovscot/binaries/content/documents/govscot/publications/independent-report/2017/03/scottish-independent-review-use-safety-efficacy-transvaginal-mesh-implants-treatment-9781786528711/documents/00515856-pdf/00515856-pdf/govscot%3Adocument/00515856pdf GOV.Scotland. Scottish Independent Review of the use, safety and efficacy of transvaginal mesh implants in the treatment of stress urinary incontinence and pelvic organ prolapse in women.
- 12.FDA . The Food and Drug Administration; 2011. Urogynecologic Surgical Mesh: Update on the Safety and Effectiveness of Transvaginal Placement for Pelvic Organ Prolapse.https://wwwfdagov/files/medical%20devices/published/Urogynecologic-Surgical-Mesh--Update-on-the-Safety-and-Effectiveness-of-Transvaginal-Placement-for-Pelvic-Organ-Prolapse-%28July-2011%29pdf [Google Scholar]
- 13.Uberoi P., Lee W., Lucioni A., Kobashi K.C., Berry D.L., Lee U.J. Listening to women: a qualitative analysis of experiences after complications from mesh mid-urethral sling surgery. Urology. 2021;148:106–112. doi: 10.1016/j.urology.2020.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Dunn G.E., Hansen B.L., Egger M.J., et al. Changed women: the long-term impact of vaginal mesh complications. Female Pelvic Med Reconstr Surg. 2014;20(3):131–136. doi: 10.1097/SPV.0000000000000083. [DOI] [PubMed] [Google Scholar]
- 15.McKinlay K.A., Oxlad M. 'I have no life and neither do the ones watching me suffer': women's experiences of transvaginal mesh implant surgery. Psychol Health. 2022:1–22. doi: 10.1080/08870446.2022.2125513. [DOI] [PubMed] [Google Scholar]
- 16.Brown J.L. The experiences of seven women living with pelvic surgical mesh complications. Int Urogynecol J. 2020;31(4):823–829. doi: 10.1007/s00192-019-04155-w. [DOI] [PubMed] [Google Scholar]
- 17.Izett-Kay M.L., Lumb C., Cartwright R., et al. ‘What research was carried out on this vaginal mesh?’ Health-related concerns in women following mesh-augmented prolapse surgery: a thematic analysis. BJOG An Int J Obstet Gynaecol. 2021;128(1):131–139. doi: 10.1111/1471-0528.16331. [DOI] [PubMed] [Google Scholar]
- 18.Cundiff G.W., Quinlan D.J., van Rensburg J.A., Slack M. Foundation for an evidence-informed algorithm for treating pelvic floor mesh complications: a review. BJOG An Int J Obstet Gynaecol. 2018;125(8):1026–1037. doi: 10.1111/1471-0528.15148. [DOI] [PubMed] [Google Scholar]
- 19.Crown . 2022. Women's Health Strategy for England.https://wwwgovuk/government/publications/womens-health-strategy-for-england [Google Scholar]
- 20.McNiven A., Toye F. 2020. Understanding experiences of urogynaecological conditions and health services.https://wwwphcoxacuk/research/health-experiences/understanding-experiences-of-urogynaecological-conditions-and-health-services [Google Scholar]
- 21.Toye F., Pearl J., Vincent K., Barker K. A qualitative evidence synthesis using meta-ethnography to understand the experience of living with pelvic organ prolapse. Int Urogynecol J. 2020;31(12):2631–2644. doi: 10.1007/s00192-020-04494-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Izett-Kay M., Barker K.L., McNiven A., Toye F. Experiences of urinary tract infection: a systematic review and meta-ethnography. Neurourol Urodyn. 2022;41(3):724–739. doi: 10.1002/nau.24884. [DOI] [PubMed] [Google Scholar]
- 23.Toye F., Barker K.L. A meta-ethnography to understand the experience of living with urinary incontinence: ‘is it just part and parcel of life?’. BMC Urol. 2020;20(1):1. doi: 10.1186/s12894-019-0555-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Toye F., Seers K., Barker K. A meta-ethnography of patients' experiences of chronic pelvic pain: struggling to construct chronic pelvic pain as 'real. J Adv Nurs. 2014;70(12):2713–2727. doi: 10.1111/jan.12485. [DOI] [PubMed] [Google Scholar]
- 25.Lincoln N., Guba E. 1985. Naturalistic Inquiry. [Google Scholar]
- 26.Braun V., Clarke V. SAGE; UK: 2021. Thematic Analysis A Practical Guide. [Google Scholar]
- 27.Charmaz K. Sage Publications; London, UK: 2006. Constructing Grounded Theory. [Google Scholar]
- 28.GMC . General Medical Council; 2020. Guidance on professional standards and ethics for doctors Decision making and consent.https://www.gmc-uk.org/-/media/documents/gmc-guidance-for-doctors---decision-making-and-consent-english_pdf-84191055.pdf [Google Scholar]
- 29.GMC . General medical Council & Nursing and Midwifery Council; 2022. Openness and honesty when things go wrong: the professional duty of candour. updated. [Google Scholar]
- 30.Joseph-Williams N., Elwyn G., Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Counsel. 2014;94(3):291–309. doi: 10.1016/j.pec.2013.10.031. [DOI] [PubMed] [Google Scholar]
- 31.Frank A.W. Asking the right question about pain: narrative and Phronesis. Lit Med. 2004;23 doi: 10.1353/lm.2005.0003. (Number 2, Fall) [DOI] [PubMed] [Google Scholar]
- 32.Merleau-Ponty M. Routledge; Oxford, UK: 2012. Phenomenology of Perception. [Google Scholar]
- 33.Turner V. Routledge & Kegan Paul; London, UK: 1969. The ritual process: structure and anti-structure. [Google Scholar]
- 34.Motamedi M., Carter S.M., Degeling C. Women's experiences of and perspectives on transvaginal mesh surgery for stress urine incontinency and pelvic organ prolapse: a qualitative systematic review. Patient. 2022;15(2):157–169. doi: 10.1007/s40271-021-00547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Richter H.E., Albo M.E., Zyczynski H.M., et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;362(22):2066–2076. doi: 10.1056/NEJMoa0912658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Imamura M., Hudson J., Wallace S.A., et al. Surgical interventions for women with stress urinary incontinence: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2019;365:l1842. doi: 10.1136/bmj.l1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Muller P., Gurol-Urganci I., van der Meulen J., Thakar R., Jha S. Risk of reoperation 10 years after surgical treatment for stress urinary incontinence: a national population-based cohort study. Am J Obstet Gynecol. 2021;225(6):645.e1–645.e14. doi: 10.1016/j.ajog.2021.08.059. [DOI] [PubMed] [Google Scholar]
- 38.Braun V., Clarke V. SAGE Publications; 2021. Thematic analysis: A practical guide. ISBN 978-1-4739-5323-9. [Google Scholar]
- 39.Ducey A., Donoso C., Ross S., Robert M. From anatomy to patient experience in pelvic floor surgery: mindlines, evidence, responsibility, and transvaginal mesh. Soc Sci Med. 2020;260 doi: 10.1016/j.socscimed.2020.113151. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.